Abstract
The association between urbanicity and risk of schizophrenia is well established. The incidence of schizophrenia has been observed to increase in line with rising levels of urbanicity, as measured in terms of population size or density. This association is expressed as Incidence Rate Ratio (IRR), and the results are usually presented by comparing the most urban with the most rural environment. In this study, we undertook to express the effect of urbanicity on the risk of schizophrenia in a linear form and to perform a meta-analysis of all available evidence. We first employed a simple regression analysis of log (IRR) as given in each study on the urbanicity category, assuming a uniform distribution and a linear association. In order to obtain more accurate estimates, we developed a more sophisticated method that generates individual data points with simulation from the summary data presented in the original studies, and then fits a logistic regression model. The estimates from each study were combined with meta-analysis. Despite the challenges that arise from differences between studies as regards to the number and relative size of urbanicity levels, a linear association was observed between the logarithm of the odds of risk for schizophrenia and urbanicity. The risk for schizophrenia at the most urban environment was estimated to be 2.37 times higher than in the most rural environment. The same effect was found when studies measuring the risk for nonaffective psychosis were included.
Key words: schizophrenia, psychosis, review, urban environment
Introduction
A strong association between exposure to an urban environment and the development of schizophrenia has been supported by many studies, which provide evidence that this is not just an epiphenomenon of the social drift of patients with schizophrenia or differential service utilization.1 Although confounders could explain part of this association (because city life may be related to higher rates of substance abuse or ethnic minority status, which are risk factors for schizophrenia themselves), studies controlling for a wide range of possible confounders have confirmed this association.2
Since the initial study that suggested a link between urbanicity and schizophrenia,3 several replications have been conducted, mainly in Europe. Despite the different methodologies used for the measurement of urban exposure (population size or density), window of exposure (birth, upbringing, or illness onset), and disease definition (narrow schizophrenia or broad psychosis), they have mostly confirmed that living in urban environment increases the risk of developing schizophrenia. Furthermore, they suggest that the incidence of schizophrenia is associated with the degree of exposure to urban environment in terms of duration and severity.4 These studies have been summarised in 2 recent reviews.5,6
An estimate of the pooled effect of urbanicity on schizophrenia risk derived from these studies would be useful for developing risk prediction models. However, the variable number, size, and definition of the various exposure categories make meta-analysis difficult. For this reason most attempts to convey or summarise the findings compare the baseline rural with the most urban group, without regard to whether these categories are defined in a similar manner across studies.
The present study performs meta-analysis of relative risks for urbanicity of these studies pooling findings from all categories of urbanicity. We express the increased risk of schizophrenia relative to a continuous variable of the level of exposure to the risk factor (urbanicity index). This novel method could be applied to other underlying quantitative risk factors for schizophrenia or other diseases where the primary studies have used ordered comparison groups, like paternal age at birth or use of cannabis.
Methods
Studies were identified through a PubMed search up to December 2011, using search terms “schizophrenia” and “urban*” and through reference lists of all included studies and published reviews of schizophrenia risk and urbanicity.5–7 We included studies comparing incidence rates (IRs) of schizophrenia between different (at least 3) groups of urbanicity exposure. In order to avoid bias due to selective migration of individuals with psychosis and in line with previous evidence that the effect of urbanization operate before the time of illness onset,8 we included studies measuring urbanization prior to the earliest stage of the disease process (at birth or under 15 years of age). To avoid inaccuracies in the measurement of the at-risk population from which cases were drawn, we included only studies where the study populations were national or representative cohorts (eg, conscripts), and cases were identified from national registers of psychiatric disorders. In all studies, diagnosis of narrow schizophrenia and schizophrenia-like psychotic disorders was made according to the International Classification of Diseases (ICD) criteria (ICD-8 and ICD-9, 295; ICD-10, F20). When multiple studies with partially overlapping cohorts met our inclusion criteria, we took the larger study. Because only 4 studies met our primary inclusion criteria (table 1),9–13 we repeated the analysis with more liberal characteristics, which included studies with broader psychosis outcome, 2 comparison groups, and urbanicity exposure at the time of disease onset (see online supplementary material table 1).14–17 The Danish studies11,12 were supplemented with new, unpublished data provided by co-author Pedersen.
Table 1.
Characteristics of the Included Studies
| Study | Country | Cohort (Birth y) | Outcome (Follow-Up Period) | Case Identification | Number of Cases | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lewis et al., 19929 | Sweden | Conscript cohort (1949–1951) | Schiz ICD-8 295 (1970–1983) | Swedish National Register of Psychiatric Care | 268 | |||||
| Marcelis et al., 199810 | Netherlands | Population-based cohort (1942–1978) | Narrow schiz ICD-9 295 (1970–1992) | Dutch National Psychiatric Case Register | 5606 | |||||
| Harrison et al., 200313 | Sweden | Population-based cohort (1973–1980) | Schiz ICD-9 295, ICD-10 F20 (1989–1997) | Swedish Inpatient Discharge Register | 363 | |||||
| Denmark* | Denmark | Population-based cohort (1955–1993) | Schiz ICD-8 295, ICD-10 F20 (1970–2009) | Danish Psychiatric Case Register | 17389 |
In each study, we recorded the number of comparison groups defined by different levels of urbanicity, their size (number of cases and person-years of exposure investigated), and the incidence rate ratio (IRR) compared to the rural group, which was consistently used as the baseline. Studies reported both adjusted and crude IRRs, using different covariates to estimate adjusted IRR. We used the crude IRR, where available, or the IRR with the minimum adjustment (eg, age and sex). When person-years were not given, they were estimated from the number of cases and the IR in each group.
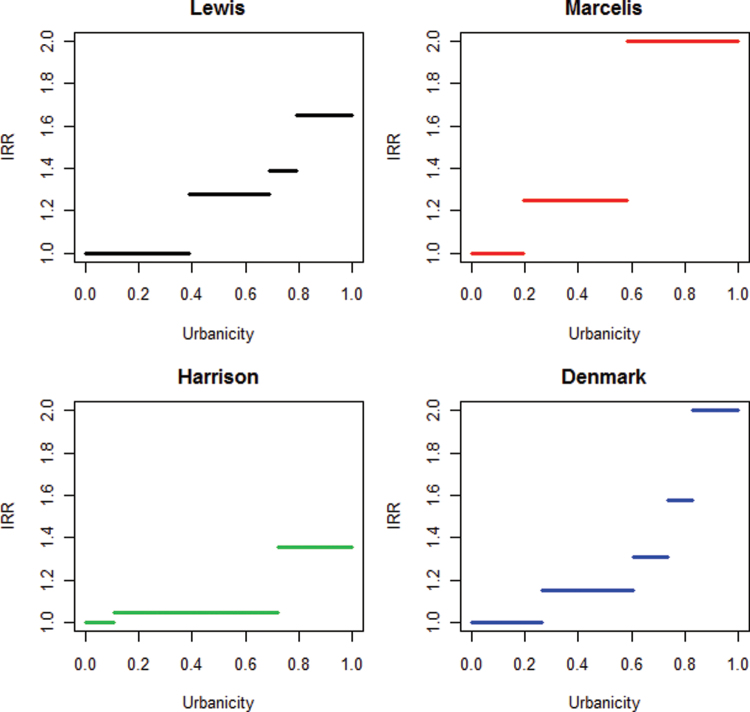
Urbanicity exposure was presented as an ordered variable in all studies although each study used different definitions of urbanicity (number of inhabitants or population density). We therefore assumed that urbanicity can be measured as a continuous variable and that any individual in the population can be assigned to a point along a uniformly distributed urbanicity scale [U(0, 1)], with 0 the most rural environment and 1 the most urban. For each study, this scale was divided in bins equal to the number of urbanicity exposure groups. The width of each bin was determined from the relevant ratio of person-years of exposure in each group (summarized in table 2 and figure 1).
Table 2.
Incidence Rate Ratios (IRR) of Schizophrenia by Urbanicity Exposure as Reported Comparative Epidemiologic Studies
| Study | Urbanicity Level | Person-Years | N Cases | IRa Estimated | IRR/OR Given (Adjusted)b | IRR Estimated (Unadjusted)c | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lewis | 1 | 266 000 | 83 | 31.20 | 1 | 1 | ||||||
| 2 | 203 500 | 81 | 39.80 | 1.26 | 1.275 | |||||||
| 3 | 694 00 | 30 | 43.23 | 1.37 | 1.386 | |||||||
| 4 | 144 000 | 74 | 51.39 | 1.57 | 1.648 | |||||||
| Marcelis | 1 | 1 792 000 | 717 | 40.01 | 1 | 1 | ||||||
| 2 | 3 586 000 | 1793 | 50.00 | 1.27 | 1.250 | |||||||
| 3 | 3 870 000 | 3096 | 80.00 | 1.97 | 1.999 | |||||||
| Harrison | 1 | 373 442 | 34 | 9.10 | 1 | 1 | ||||||
| 2 | 2 162 911 | 207 | 9.57 | 1.04 | 1.051 | |||||||
| 3 | 9 86 037 | 122 | 12.37 | 1.34 | 1.359 | |||||||
| Denmark | 1 | 13 338 462 | 3468 | 26.00 | 1 | 1 | ||||||
| 2 | 17 483 333 | 5245 | 30.00 | 1.14 | 1.154 | |||||||
| 3 | 6 394 118 | 2174 | 34.00 | 1.28 | 1.308 | |||||||
| 4 | 4 639 024 | 1902 | 41.00 | 1.4 | 1.577 | |||||||
| 5 | 8 846 154 | 4600 | 52.00 | 1.8 | 2 |
aIncidence Rate (per 100 000 person-years).
bAdjusted IRR/OR were given in the papers. The original studies used different covariates to adjust.
cUnadjusted IRR were estimated from N cases and person-years in each group. In Lewis et al. person-years were estimated from the given N cases and incidence.
Fig. 1.
Incidence Rate Ratio (IRR) of schizophrenia in different urbanicity levels. In each study, the number of horizontal lines corresponds to the number of urbanicity exposure groups, the length of each line on the x-axis (bin width) is analogous to the relevant size of the person-years at risk in each group, and the height on the y-axis corresponds to the given IRR with the baseline group always set at 1.
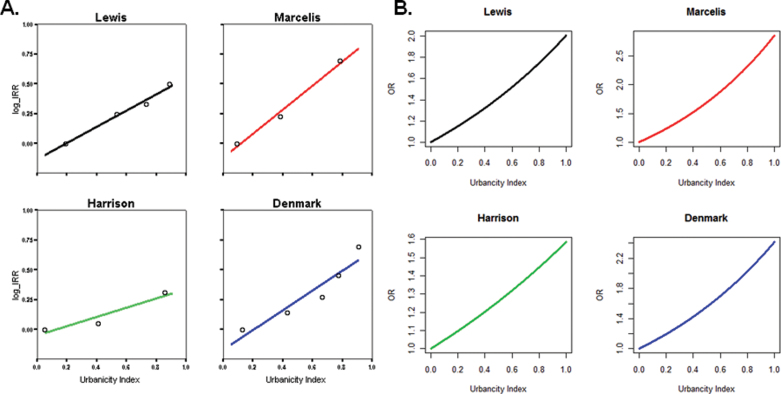
Mapping the urbanicity categories from each study to a common underlying urbanicity measure enables us to combine IRR estimates across studies. We used 2 methods to achieve this: firstly, we performed a regression of the log (IRR) against the corresponding urbanicity category (summary method) and secondly we used a simulation strategy to generate likely urbanicity levels compatible with data from schizophrenia cases and controls in the original study and fitted a logistic regression model to the data (simulation method).
Because all studies had monotonic (increasing) IRR across the urbanicity categories, a linear model for the effect of urbanicity on schizophrenia risk was chosen. In each study, we performed a linear regression of the logarithm of IRR on the mid-point of the corresponding urbanicity exposure bin. The IRR of schizophrenia of the most urban vs the least urban individuals is exp(IR1)/exp(IR0), where IR1 and IR0 refer to the estimated IR at urbanicity points 1 and 0. The above equals exp(IR1 −IR0), and because the range of the urbanicity scale has been defined as 1, this is equal to exp(b), where b is the regression coefficient.
For a more accurate estimation of the association we developed a method based on simulation, which makes use of the summary points given in each study. We simulated an urbanicity index value to each case and control based on the ranks of the uniform distribution and then fit a logistic regression model to these individual-level data. The logarithm of the odds of schizophrenia as a function of the urbanicity index is given by ln(P/1−P) = a + bx, where P is the probability of developing schizophrenia, x the urbanicity index between 0 and 1, a the intercept, and b the regression coefficient. The exponential of b is the odds ratio (OR) of schizophrenia between the most urban (x = 1) and the most rural (x = 0) individuals, which is directly comparable to the IRR of schizophrenia from the previous method. The probability of schizophrenia for an individual with urbanicity index value x is then given by P = e a+bx /(1 + e a+bx ). Simulations were repeated to estimate b, then the mean value of exp(b), and SE for each study used as an estimate of the OR for schizophrenia (for full details see online supplementary materials).
Meta-analysis was performed to produce a single estimate of the effect size of urbanicity as a risk factor of schizophrenia. The first method of estimating IRR used only the summary points from the original studies, so no meaningful SE were derived. For the simulation method, meta-analysis of the mean regression coefficients was performed, weighting studies by the SE of b. Heterogeneity between samples was assessed using Cochran’s Q and I2 statistics18 and estimates were combined with the Der-Simonian and Laird random-effects model.19 The analyses were carried out initially with studies meeting the strict inclusion criteria and, subsequently, with all studies identified with the relaxed criteria. In the second analysis, the Lewis et al study9 was excluded because the sample was included in the larger male cohort by Sundquist et al.16 Data were analyzed using SPSS version 15 (SPSS Inc. Chicago, Illinois), Stata release 10 (Stata Corp. 2007), and the R Project for Statistical Computing (www.r-project.org). The R scripts for the simulation method are available from the authors upon request.
Results
In total, we identified 4 studies that met our strict inclusion criteria (diagnosis of schizophrenia, more than 2 levels of urbanicity exposure, and premorbid measurement)9–13 and 4 additional studies14–17 that met our broader criteria (see online supplementary material table 1). These were conducted between 1974 and 2007 in 6 Western industrialized countries with predominantly European populations and comprised a total of 46 820 cases with psychosis.
Results for the summary method from each study are shown in table 3 and figure 2 and were very similar to study-specific OR for the simulation method. The estimated pooled OR from the simulation method for schizophrenia in the 4 studies that met strict criteria was 2.37 (95% confidence interval [CI] = 2.01–2.81). Estimates from individual studies were combined with the random-effects model because they were highly heterogeneous (Q = 16.6, P = .18, I2 = 82%). The effect was sustained when inclusion criteria were relaxed with the addition of urbanicity measured at residence and outcome measure including nonaffective psychosis. Analysis of all 8 studies that met the broader criteria gave similar results (OR = 2.38; CI = 1.6–3.5), with even higher heterogeneity (Q = 833, P = 0, I2 = 99%), resulting in a large CI. Forest plots from both analyses are presented in figure 1 of the online supplementary materials.
Table 3.
IRR/OR Estimated From Summary and Simulation Methods, With Pooled Estimates Obtained Through Meta-Analysis of Simulation Method Results
| Study | Summary Method: | Simulation Method: | ||||
|---|---|---|---|---|---|---|
| IRR | OR | 95% confidence Interval | ||||
| Strict criteria | ||||||
| Lewis | 1.98 | 2.01 | 1.32–3.07 | |||
| Marcelis | 2.74 | 2.87 | 2.61–3.15 | |||
| Harrison | 1.47 | 1.60 | 1.12–2.30 | |||
| Denmark | 2.29 | 2.42 | 2.29–2.55 | |||
| Pooled effect size | 2.38 | 2.01–2.81 | ||||
| Broad criteria | ||||||
| Eaton | 3.33 | 4.18 | 3.42–5.09 | |||
| Hauka | 1.06 | 1.06 | 1.00–1.12 | |||
| Sundquist-females | 3.57 | 3.93 | 3.44–4.46 | |||
| Sundquist-males | 3.08 | 3.34 | 2.94–3.80 | |||
| Weiser | 1.63 | 1.60 | 1.31–1.96 | |||
| Pooled effect size* | 2.39 | 1.62–3.51 | ||||
*Excluding study by Lewis et al.
Fig. 2.
Regression of IRR/OR against Urbanicity index with the summary and simulation method. (A). Summary method. In each study the urbanicity index is represented on x-axis and the logarithm of IRR on the y-axis. The circles correspond to the estimated IRR from the original studies as given in table 2. They are positioned in the middle of each bin on the x-axis. (B). Simulation method. Plot of the OR of schizophrenia as a function of the urbanicity index, estimated with logistic regression.
Discussion
Our study summarizes the effect of exposure to urban environment on the risk of developing schizophrenia. From published data, we found a consistent effect in that incidence of schizophrenia increased almost linearly with increase in urbanicity. This observation remained stable irrespective of the outcome measure (narrow schizophrenia or broad psychosis), the method of measuring urban environment (population size of place of residence or population density), and the time of exposure (birth and upbringing or onset of illness).
The pooled estimates of the effect of urbanicity on the incidence of schizophrenia or psychosis are clinically relevant for individualized estimation of the risk of developing schizophrenia. From a public health perspective, the results of this study can be useful for the design and provision of psychiatric services, eg, the estimation of local needs for psychiatric beds in hospitals, the development and relative size of community teams that target mainly psychosis such as early intervention services and assertive outreach teams.
The summary method used has intuitive appeal in its direct use of IRR estimates from the original studies, but the simulation study is required for CIs to be used in meta-analysis across studies. Strengths of the study include the use of all available published data (46 820 cases with psychosis in total), the expression of risk to develop schizophrenia in a linear form that can be applied in urbanized countries, and the development of a method to transform ordinal to linear exposure variables that can be used in other risk factors when there is a reasonable assumption that exposure has a linear effect on the outcome. The regression models applied here (linear regression for log(OR); logistic regression for OR) assume risk changes monotonically and in a linear relationship with the underlying quantitative trait of urbanicity. Different modeling strategies would be needed for disorders that exhibit a different relationship between risk and the underlying trait. The regression coefficients estimated do not rely on the arbitrary size of the most and least urban groups, and our estimates of the effect of urbanicity make use of all the data reported in the original studies.
Ideally, future studies should report both crude and adjusted IRs in each category. Common confounders available in all studies, like age, sex, and their interaction, should always be reported. When a continuous exposure variable is available, authors should try to make a prediction for the underling distribution (linear and exponential) and report regression coefficients in addition to the IRR of discrete categories. Finally, when discrete categories are produced from continuous exposure variables, groups should be almost equal in size to avoid large CI.
One limitation of our meta-analysis is that the validity and accuracy of our findings depend on the quality of the original studies. By using large epidemiological studies and strict inclusion criteria for the definition of cases, we attempted to select high-quality studies. However, the heterogeneity remained high, possibly due to the different IRs of schizophrenia between studies, and the different size of the baseline group and effect sizes were synthesized with the random-effects model. Of interest is the observation that our estimates of the effect of urbanicity including studies with both strict and relaxed criteria were similar. The pooled OR was based on crude (unadjusted) estimates of IRR from the original studies because they used different confounders for the estimation of adjusted IRR.
Another limitation of our meta-analysis is that although the original studies followed their cohort prospectively for the development of schizophrenia, in the absence of individual data, we estimated OR instead of IRR. However, given the rarity of the disease, we can make the reasonable assumption that the 2 approaches have minor differences.20 It is important to note that all studies were performed in developed countries with high levels of urbanicity, as measured by United Nations, Population Division (http://esa.un.org/unup/), and the US Census Bureau (http://www.census.gov/). Hence, we cannot make inferences about less urbanized or developing countries. One possibility that remains to be tested is that given the higher variability of exposure to urban environment, in countries with similar levels of development but less aggregation in cities, the effect of urbanicity could be larger.
The large effect of urbanicity on the risk of developing psychosis does not necessarily imply causation, but the level of exposure to urban environment remains a very important risk marker for schizophrenia and psychosis in general. Explanations for this association include differences in individual characteristics (eg, different levels of migration or family history), familial characteristics, selective migration, exposure to infections, exposure to pollutants, diet, and the social environment.21–24 Evidence from a Danish sibling design suggest that the causes responsible for these urban-rural differences are related to family-level factors although the influence of individual-level factors could not be ruled out.21 Neighbourhood effect, social fragmentation and deprivation, and other differences between life in cities and rural areas have been found to explain better the association of urbanicity with psychosis than individual differences.25 To be able to understand better the causes of this association and to make universal use of urbanicity as risk factor for schizophrenia, there is a need to extend the observation in developing countries with different sociodemographic structure.
Supplementary Material
Supplementary material is available at http:// schizophreniabulletin.oxfordjournals.org.
Funding
Guy’s and St Thomas’ Charity (R080529).
Supplementary Material
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.Tandon R, Keshavan MS, Nasrallah HA. Schizophrenia, “Just the Facts” What we know in 2008. 2. Epidemiology and etiology. Schizophr Res. 2008;102:1–18 doi: 10.1016/j.schres.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 2. van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature 2010. 468 203–212 [DOI] [PubMed] [Google Scholar]
- 3. Faris REL, Dunham , Dunham HW. Mental Disorders in Urban Areas. An ecological study of schizophrenia and other psychoses Chicago: University of Chicago Press; 1939. xxxviii, 270 [Google Scholar]
- 4. Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry 2001. 58 1039–1046 [DOI] [PubMed] [Google Scholar]
- 5. March D, Hatch SL, Morgan C, et al. Psychosis and place. Epidemiol Rev 2008. 30 84–100 [DOI] [PubMed] [Google Scholar]
- 6. Kelly BD, O’Callaghan E, Waddington JL, et al. Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophr Res 2010. 116 75–89 [DOI] [PubMed] [Google Scholar]
- 7. Pedersen CB. Urban-rural differences in the risk of schizophrenia Aarhus: National Centre for Register-based Research, Aarhus University; 2009. [Google Scholar]
- 8. Marcelis M, Takei N, van Os J. Urbanization and risk for schizophrenia: does the effect operate before or around the time of illness onset? Psychol Med 1999. 29 1197–1203 [DOI] [PubMed] [Google Scholar]
- 9. Lewis G, David A, Andréasson S, Allebeck P. Schizophrenia and city life. Lancet 1992. 340 137–140 [DOI] [PubMed] [Google Scholar]
- 10. Marcelis M, Navarro-Mateu F, Murray R, Selten JP, Van Os J. Urbanization and psychosis: a study of 1942-1978 birth cohorts in the Netherlands Psychol Med 1998. 28 871–879 [DOI] [PubMed] [Google Scholar]
- 11. Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med 1999. 340 603–608 [DOI] [PubMed] [Google Scholar]
- 12. Pedersen CB, Mortensen PB. Family history, place and season of birth as risk factors for schizophrenia in Denmark: a replication and reanalysis. Br J Psychiatry 2001. 179 46–52 [DOI] [PubMed] [Google Scholar]
- 13. Harrison G, Fouskakis D, Rasmussen F, Tynelius P, Sipos A, Gunnell D. Association between psychotic disorder and urban place of birth is not mediated by obstetric complications or childhood socio-economic position: a cohort study. Psychol Med 2003. 33 723–731 [DOI] [PubMed] [Google Scholar]
- 14. Eaton WW. Residence, social class, and schizophrenia. J Health Soc Behav 1974. 15 289–299 [PubMed] [Google Scholar]
- 15. Haukka J, Suvisaari J, Varilo T, Lonnqvist J. Regional variation in the incidence of schizophrenia in Finland: a study of birth cohorts born from 1950 to 1969 Psychol Med 2001. 31 1045–1053 [DOI] [PubMed] [Google Scholar]
- 16. Sundquist K, Frank G, Sundquist J. Urbanisation and incidence of psychosis and depression: follow-up study of 4.4 million women and men in Sweden. Br J Psychiatry 2004. 184 293–298 [DOI] [PubMed] [Google Scholar]
- 17. Weiser M, van Os J, Reichenberg A, et al. Social and cognitive functioning, urbanicity and risk for schizophrenia. Br J Psychiatry 2007. 191 320–324 [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003. 327 557–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986. 7 177–188 [DOI] [PubMed] [Google Scholar]
- 20. So HC, Sham PC. Effect size measures in genetic association studies and age-conditional risk prediction. Hum Hered 2010. 70 205–218 [DOI] [PubMed] [Google Scholar]
- 21. Pedersen CB, Mortensen PB. Are the cause(s) responsible for urban-rural differences in schizophrenia risk rooted in families or in individuals? Am J Epidemiol 2006. 163 971–978 [DOI] [PubMed] [Google Scholar]
- 22. Allardyce J, Boydell J, Van Os J, et al. Comparison of the incidence of schizophrenia in rural Dumfries and Galloway and urban Camberwell. Br J Psychiatry 2001. 179 335–339 [DOI] [PubMed] [Google Scholar]
- 23. Allardyce J, Boydell J. Review: the wider social environment and schizophrenia. Schizophr Bull 2006. 32 592–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Freeman H. Schizophrenia and city residence. Br J Psychiatry Suppl 1994. 39–50 [PubMed] [Google Scholar]
- 25. Zammit S, Lewis G, Rasbash J, Dalman C, Gustafsson JE, Allebeck P. Individuals, schools, and neighborhood: a multilevel longitudinal study of variation in incidence of psychotic disorders. Arch Gen Psychiatry 2010. 67 914–922 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.