Abstract
Objectives: Risk for psychosis is currently defined primarily on the basis of attenuated positive symptoms (APS), with no inclusion of the functional deficits characteristic of schizophrenia. Impaired social and role functioning have been of interest for reflecting poor outcome but far less is known about the developmental impact of these deficits as vulnerability or risk factors. Methods: Age-appropriate social and role functioning were prospectively assessed in 100 individuals at clinical high risk (CHR) for psychosis included in the 8-site North American Prodromal Longitudinal Study database. A nested case-control design was used to compare changes in social and role functioning in 26 individuals converting to psychosis shortly after baseline assessment and 24 converting over a year later. Individuals in each converter subgroup were directly matched to a non-converter at the same site, controlling for time to conversion, age, gender, and severity of baseline symptoms. Results: At baseline, CHR subjects who later became psychotic were significantly more likely to be impaired socially than matched non-converters. Onset of psychosis did not further disrupt social difficulties. Role functioning showed some of the same trends, but the overall pattern was not as consistent as for the social domain. Controlling for neurocognition did not change the pattern of group differences. Conclusions: Early impaired social functioning appears to be a risk factor for psychosis and, added to APS, could potentially contribute to accurate identification of CHR individuals and provide a new direction for early intervention to reduce long-term disability.
Keywords: clinical high risk, functional deficits, prodromal, social risk factors, functional outcome/attenuated positive symptoms
Introduction
Current findings suggest that psychosis prevention strategies are limited by their focus on late-emerging positive symptoms, a time when disability is already relatively well established.1 As a result of the emphasis on positive symptoms, most treatments targeting the prepsychotic or “prodromal” period consider a reduced rate of conversion to psychosis to be the outcome of interest. It is possible, however, that prevention would be markedly improved with a more comprehensive approach that involves developmentally earlier functional deficits. A major goal of the current study is to evaluate the extent to which early social and role (school/work) deficits appear to be stable risk factors for psychosis and are appropriate targets for early intervention.
Functional deficits (eg, inability to work or be an independent member of the community, social isolation, lack of self-care) are long-established characteristics of chronic psychosis2–4 and are typically reported to be nonresponsive to antipsychotic treatment, even when positive symptoms show marked improvement.5–7 In chronic patients, research has tended to focus on functional outcome, with particular interest directed at the association between early cognitive deficits and later impaired functioning.3,8–11 However, it is becoming increasingly clear that the development of functional difficulties is important in its own right, beyond its association with impaired cognition.12,13
Evidence has been found in genetic high risk, cohort, and first-episode studies that moderately impaired social and role functioning are often early preillness characteristics of individuals who will later develop psychosis.14–23 Social difficulties appear to have particular potential to contribute to prediction of schizophrenia.24–28 Based on this early data, Cornblatt et al29 proposed a neurodevelopmental model suggesting that the widely acknowledged vulnerability for later psychosis involves deficits in at least 4 domains (Cognitive-Affective-Social-Isolation-School /work problems) which are labeled the “CASIS” cluster. It is proposed that in many cases, this vulnerability is the necessary but not sufficient precondition for development of major psychotic disorders, especially schizophrenia. According to this view, individuals at true risk have long-standing social difficulties and impaired age-appropriate role functioning, including unsuccessful adaptation to school demands and later difficulties in becoming self-supporting. In this context, early school problems are considered the harbinger of later work difficulties and involve a broader set of skills than simply academic success. Emerging positive symptoms are considered developmentally independent processes that progress to chronic schizophrenia in the presence of some combination of CASIS deficits.
At present, little is known about the course and stability of functional deficits through the premorbid, prodromal, and postpsychosis phases of illness and the extent to which functioning is disrupted by the onset of psychosis. Early intervention may be especially important because social and role skills consolidate during late adolescence-early adulthood.30 In the data reported here, we evaluate the initial evidence from phase I of the North American Prodromal Longitudinal Study (NAPLS I) that social and role functioning are potentially long-standing risk factors that precede psychosis onset. Specifically, we hypothesize that: (1) at-risk individuals who go on to develop a psychosis will be more likely to display early functional impairments than will at-risk subjects who do not convert; (2) clinical stage does not influence impaired functioning; therefore, deficits will be comparable for those early vs late in the prodrome; and (3) evaluated prospectively emergence of full psychosis is not a major cause of impaired functioning.
Methods
Sample
The current study examines changes in social and role functioning in adolescents and young adults at clinical high risk (CHR) for schizophrenia, of whom about 35% converted to psychosis with follow-up over a period of 2½ years.25 The study protocols, informed consents, and data pooling procedures were approved by the institutional review boards (IRBs) of each of the 8 participating study sites which include: Calgary University; Emory University; Harvard Medical School; University of California, Los Angeles (UCLA); University of California, San Diego; University of North Carolina (UNC), Chapel Hill; Yale University; and the Zucker Hillside Hospital. At baseline, the NAPLS I consolidated database consisted of a total of 888 subjects who had been enrolled in 1 of the 8 consortium sites between 1998 and 2005. All participants signed IRB approved consent forms. Of these, 370 subjects were considered to be “prodromal” or at CHR according to the criteria specified by the structured interview of prodromal symptoms (SIPS).31 Most CHR individuals (97%) met criteria for the attenuated positive symptoms (APS) category requiring a moderate to severe (but not psychotic) rating on any one or more of 5 positive symptoms, including unusual thoughts, perceptual abnormalities, suspiciousness, grandiose ideas, and conceptual disorganization.
The NAPLS I database and follow-up conversion rates are detailed in several prior publications.25,32–34 The index sample (cases) for the present study consists of those CHR subjects who converted to psychosis over follow-up and who were assessed for social and role functioning both at baseline and shortly after conversion. Of 291 at-risk subjects with baseline and follow-up evaluations, 82 developed a psychotic disorder over the 2½-year follow-up period. Each converter was matched to a CHR participant who did not convert. To control for a range of confounding variables and possible site differences, a nested case-control design was used in which index subjects were matched to CHR non-converters at the same site.
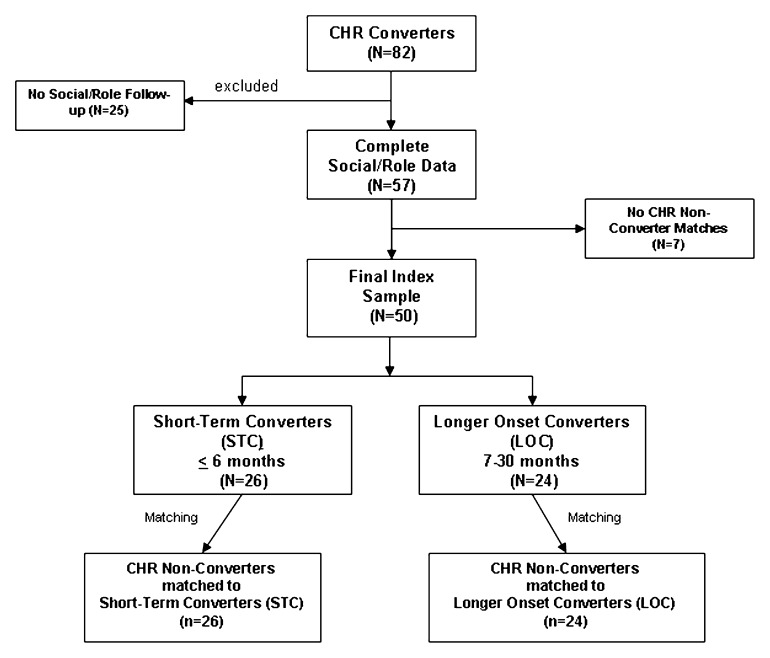
The sample matching or yoking process is described in figure 1. Of the initial 82 converters, 25 were excluded because they did not have follow-up functional ratings available (remaining n = 57). An additional 7 cases were eliminated because no appropriate within site matches were available, generating a final sample of 50 converters yoked to 50 CHR non-converters. For converters, the last follow-up contact was considered to be the rating done as closely following conversion as possible. Matched non-converters had a last functional assessment of similar duration to their yoked index case.
Fig. 1.
Flowchart indicating sample selection process, generating a total of 100 subjects, 50 index converters (divided into 26 short-term and 24 longer onset converters), and 50 matched clinical high risk (CHR) non-converters.
Based on the data available, converters fell into 1 of 2 different longitudinal groups: (1) subjects who developed a psychosis within 6 months of recruitment, referred to as short-term converters (STCs, n = 26), and individuals who took considerably longer to undergo conversion, ranging from 7 to 30 months labeled as longer onset converters (LOCs, n = 24). Both theoretical and practical reasons supported separate analysis of these 2 groups. Theoretically, STCs are considered to be individuals in the acute final stages of the prodrome, where psychosis is imminent. LOCs are assumed to be recruited in earlier stages of the prodrome because it takes substantially longer to convert (from 7 months to over 2 years). A question can then be raised as to whether individuals who convert early are actually more ill, verging on psychosis, compared with longer onset prodromal cases. This is especially relevant to clinical trials focusing on prevention because it may be considerably more difficult to “prevent” illness in individuals so close to onset. Empirically, the distribution of times to conversion supported a 6-month cut-off, with STCs, on average, converting at 1.98 months (SD = 1.43; range = 0.43–5.59) and LOCs mean time to conversion of 14.19 months (SD = 6.38; range = 6.02–32.82; see table 1). In addition to site and follow-up time point, all converter/nonconverter yoked pairs were matched for age, gender, and, as closely as possible, positive symptom severity at baseline. The matching process generated 26 STC pairs and 24 LOC pairs.
Table 1.
Demographic and Clinical Characteristics for Short-term and Longer Onset Converters Plus Matched CHR Non-converters
| Short Term | Longer Onset | |||||
| Converters (n = 26) | Non-converter (n = 26) | Converters (n = 24) | Non-converter (n = 24) | Test Statistic | P Values | |
| Research site, No. (%) | Site total | |||||
| UNC | 7 (26.9) | 7 (26.9) | 4 (16.7) | 4 (16.7) | 22 | |
| Emory | 0 (0) | 0 (0) | 1 (4.2) | 1 (4.2) | 2 | |
| LIJ | 1 (3.8) | 1 (3.8) | 2 (8.3) | 2 (8.3) | 6 | |
| Toronto | 2 (7.7) | 2 (7.7) | 5 (20.8) | 5 (20.8) | 14 | |
| UCLA | 0 (0) | 0 (0) | 6 (25.0) | 6 (25.0) | 12 | |
| UCSD | 2 (7.7) | 2 (7.7) | 4 (16.7) | 4 (16.7) | 12 | |
| Yale | 14 (53.8) | 14 (53.8) | 2 (8.3) | 2 (8.3) | 32 | |
| Age, y, mean (SD) | 18.46 (4.05) | 18.32 (3.95) | 17.99 (3.02) | 17.72 (3.01) | F 3,96 = 0.23 | .89 |
| Education, y, mean (SD) | 10.73 (2.52) | 10.92 (2.77) | 10.79 (2.54) | 10.43 (2.64) | F 3,96 = 0.15 | .93 |
| Currently enrolled in school, No. (%) | 19 (73.1) | 22 (84.6) | 18 (75.0) | 17 (70.8) | = 1.54 | .67 |
| Gender, No. (%) | ||||||
| Male | 16 (61.5) | 16 (61.5) | 16 (66.7) | 16 (66.7) | = 0.29 | .96 |
| Female | 10 (38.5) | 10 (38.5) | 8 (33.3) | 8 (33.3) | ||
| Race, No. (%) | ||||||
| White | 17 (65.4) | 21 (80.8) | 19 (79.2) | 19 (79.2) | = 2.19 | .53 |
| Ethnic origin, No. (%) | ||||||
| Hispanic | 3 (11.5) | 2 (7.7) | 3 (12.5) | 4 (16.7) | = 0.96 | .81 |
| SIPS score, mean (SD) | ||||||
| Positive | 14.85 (3.75) | 12.50 (3.35) | 13.25 (4.08) | 12.29 (4.47) | F 3,96 = 2.24 | .09 |
| Negative | 15.08 (6.67) | 11.42 (6.75) | 16.92 (7.28) | 9.08 (6.78) | F 3,96 = 6.44 | .001 |
| DSM-IV diagnoses | ||||||
| Mooda | 7 (36.8) | 6 (26.0) | 8 (40.0) | 9 (40.9) | = 1.63 | .65 |
| Mania | 0 (0.0) | 0 (0.0) | 1 (5.0) | 1 (4.5) | = 2.01 | .57 |
| Anxietyb | 4 (25.0) | 6 (25.0) | 4 (20.0) | 8 (36.4) | = 1.56 | .67 |
| Follow-up medication, No. (%) | ||||||
| No medication | 16 (61.5) | 12 (46.2) | 5 (20.8) | 9 (37.5) | ||
| Antipsychotics | 8 (30.8) | 4 (15.4) | 14 (58.3) | 7 (29.2) | = 10.83 | .01 |
| Antidepressants | 1 (3.8) | 8 (30.8) | 3 (12.5) | 7 (29.2) | = 8.49 | <.05 |
| Other medications | 1 (3.8) | 2 (7.7) | 2 (8.3) | 1 (4.2) | = 0.72 | .87 |
| Functioning | ||||||
| GF: social, mean (SD) | 5.46 (1.33) | 6.35 (1.29) | 5.21 (1.64) | 7.25 (1.60) | F 3,96 = 9.72 | <.001 |
| GF: role, mean (SD) | 6.04 (1.34) | 6.46 (1.50) | 4.96 (1.92) | 6.21 (1.89) | F 3,96 = 3.84 | .01 |
| Time to conversion/follow-up, months, mean (SD)c | 1.97 (1.43) | 2.88 (5.23) | 14.91 (6.37) | 12.00 (5.00) | F 3,96 = 41.21 | <.001 |
Note: CHR, clinical high risk; SIPS, structured interview for prodromal syndromes; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; UNC, University of North Carolina; LIJ, Long Island Jewish Health System; UCLA, University of California, Los Angeles; UCSD, University of California, San Diego. Group comparisons of demographic and clinical variables were performed using Pearson Chi-Square tests for categorical variables and one-way ANOVA for continuous variables. Results of post hoc Fisher's least significant difference tests are described in manuscript.
DSM-IV defined diagnosis of depression or dysthymia.
DSM-IV defined diagnosis of panic disorder, posttraumatic stress disorder , obsessive-compulsive disorder, generalized anxiety disorder, or phobias including simple phobias and social phobia.
Post hoc tests indicated that there was no difference in time to conversion/follow-up between converters and non-converters in either the short-term or longer onset groups.
Measures
In most cases, the measures administered at the 8 sites were sufficiently similar to be combined in the NAPLS I database.32 Measures of functioning, however, were an exception. Little commonality was found across sites in terms of specific instruments used to measure either social or role functioning. As discussed in more detail in Cornblatt et al,24 a different set of measures was used by each site and these varied considerably in targeted age range (child vs adult) and severity levels. Thus, to provide a common metric, 2 new global measures were developed to reflect functioning in at-risk adolescents and young adults who are not as severely impaired as more chronic patients. These 2 measures are referred to as the Global Functioning (GF) Scales, one measuring social skills (GF: social35) and the other measuring role (GF: role36). These scales were initially validated as part of collaboration between the Zucker Hillside and UCLA sites24 and were subsequently used as the common social/role measures across 7 of the 8 NAPLS sites (the Harvard site did not contribute to this data set). Ratings for each of the 2 GF scales were based on best estimates derived from all information available at each site. High interrater reliabilities were reported22 using this approach, along with construct and early predictive validity. Both measures have been used in several other prodromal11,25,33,37 and first-episode38 reports.
Description of the Social and Role Functioning Scales.
The GF:S and GF:R scales35,36 were designed to be complementary and broadly derived from the traditional Global Assessment of Functioning (GAF) format. For both scales, scores range from 1 to 10, with 10 indicating superior functioning and 1 representing extreme dysfunction. Scores around 6 typically characterize at-risk individuals,24 indicating moderately severe problems in functioning. Based on this distribution pattern, both scales have been dichotomized for the current analyses with scores of 1–6 indicating poor to moderately poor functioning and scores of 7–10 reflecting good functioning (the strategy also used by Cannon et al25).
Statistical Analyses
All analyses were conducted using SPSS 16.0 (SPSS Inc, Chicago, IL). Group comparisons of demographic and clinical variables were performed using Pearson Chi-Square tests for categorical variables and one-way ANOVA for continuous variables. Significant ANOVAs were followed by post hoc Fisher's least significant difference (LSD) tests.
Multinomial generalized estimating equations (GEE39–41) models for repeated measures were used to estimate the impact of conversion on functioning as well as the change in functioning from baseline to the last observation period. Follow-up time and conversion status (ie, converter vs matched non-converter) were included as the main explanatory variables in the GEE model, controlling for baseline positive and negative symptoms and medication. The variables entered into the GEE model as covariates were those that were significant at a 10% level in the univariate group analyses. An interaction term was also included in the model to evaluate whether the rate of change of functioning over follow-up was modified by conversion status. Social and role functioning were used as the primary dependent variables. An unstructured correlation matrix and robust estimation was used to protect against model misspecification. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using the cumulative logit link function, adjusted for all the covariates described above. One model was built for each of the domains of functioning (ie, social and role) separately for STC and LOC groups (for a total of 4 models). The GEE models generate cumulative predicted probabilities for poor functioning and are graphed on linear scales in figures 2 and 3 to optimize interpretability.
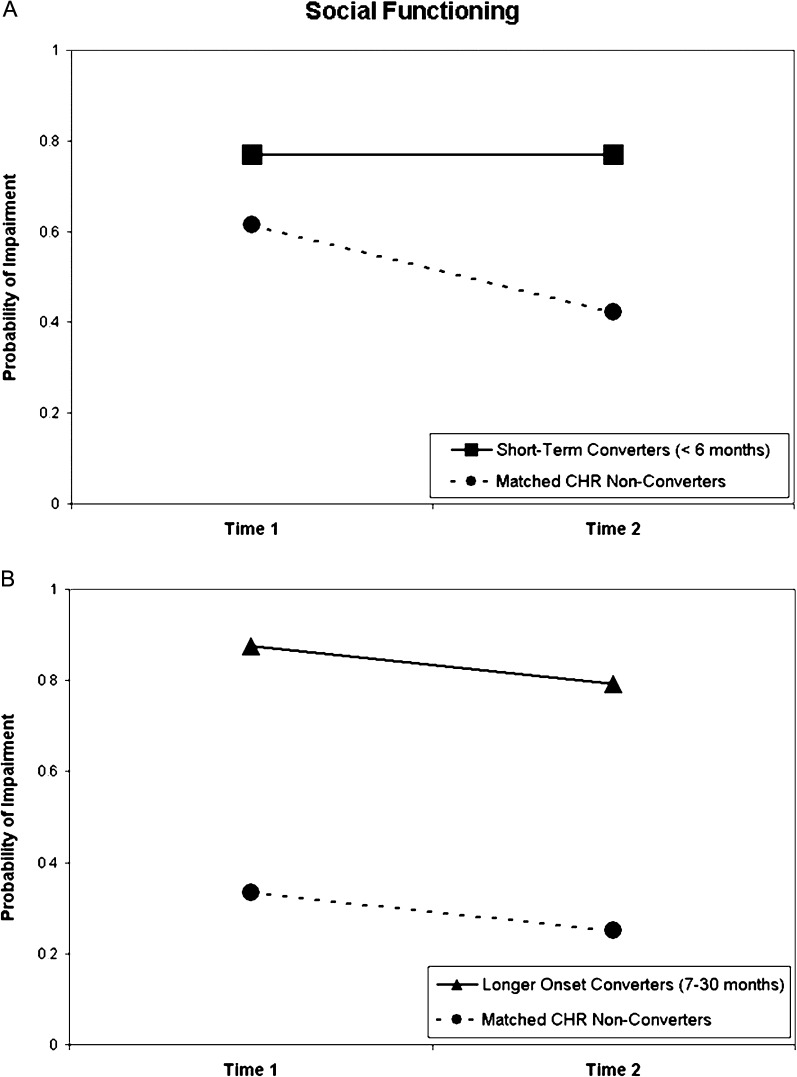
Fig. 2.
Probability of social impairment by conversion status for (A) short-term converters and matched CHR non-converters and (B) longer onset converters and matched CHR non-converters.
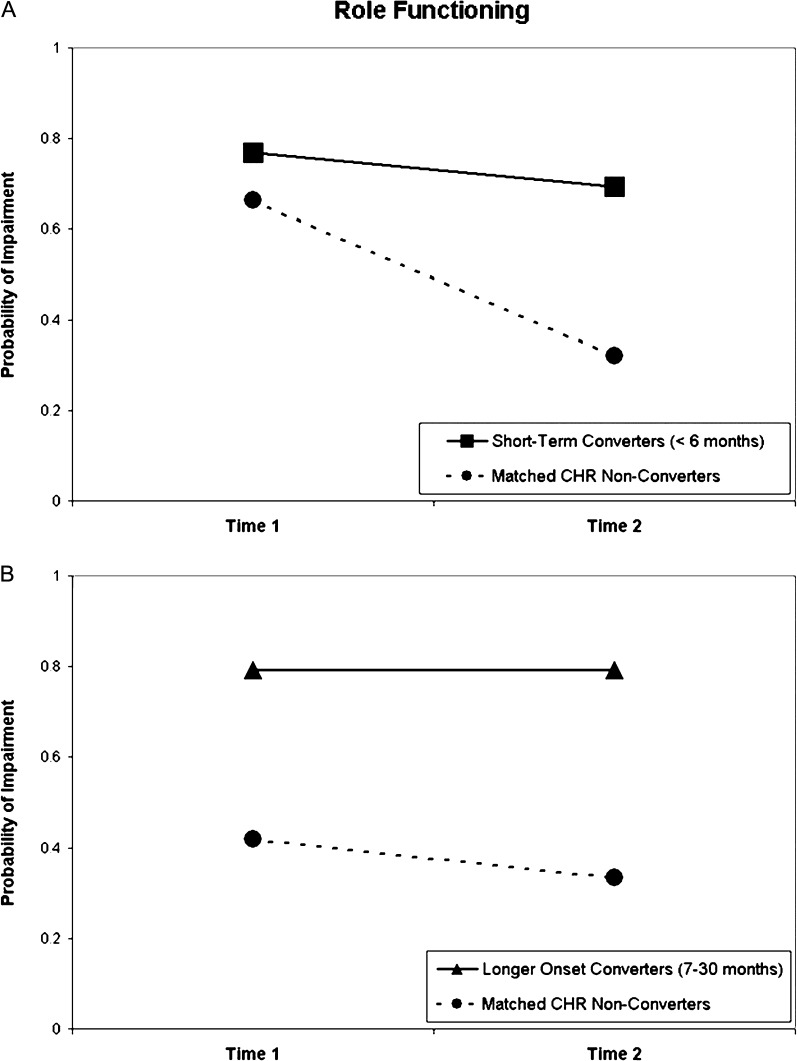
Fig. 3.
Probability of role impairment by conversion status for (A) short-term converters and matched CHR non-converters and (B) longer onset converters and matched CHR non-converters.
Results
Sample Characteristics
Demographic variables and clinical characteristics are presented in table 1. The majority of STC pairs came from 2 sites: UNC and Yale. The LOC pairs were more evenly divided among all 7 participating sites. Secondary matching variables worked quite well, with all 4 groups approximately 18 years of age and all 4 approximately 2/3rds male, consistent with the schizophrenia literature. In addition, there were no differences among the 4 groups in race, ethnicity, years of education, or school enrollment. For the sample overall, the majority of subjects were enrolled in high school or college.
Group Differences: Converters vs Non-converters
There were no systematic clinical differences between converters and non-converters at baseline, including rates of mood (depression or dysthymia), mania, and anxiety disorders (see table 1). There were also no differences in total positive symptom scores, as would be expected from matching, although non-converters did show a trend for lower positive symptoms compared with future converters. A major exception, however, was negative symptoms, which were not matched at baseline and showed a group difference (P < .01), with post hoc analyses indicating that LOCs had a higher level of negative symptoms than matched non-converters (Fisher's LSD test, P < .001).
In terms of the 2 domains of interest, social and role functioning, as indicated in table 1, both groups of converters were already significantly impaired at baseline relative to non-converters. Significant group differences were found for social functioning (P < .001) and post hoc analyses showed that both STCs and LOCs were significantly impaired relative to matched non-converters (P < .05 for both), with no differences between converter subgroups. For role functioning, LOCs were dramatically impaired at baseline relative to their matched non-converters and compared with the STC and non-converter groups (P < .01 for all).
Group Differences: STC vs LOC Subgroups
Overall, the 2 converter groups were not significantly different from each other on any of the baseline demographic features or clinical characteristics, with the exception of negative symptoms and role functioning. At baseline, LOCs had higher negative symptoms and lower role functioning when compared with STCs, with negative symptoms related to role functioning. At follow-up, there were no differences between converter groups in type of axis I psychotic disorders (see online supplementary table S1).
Medication
Patterns of medication over follow-up indicated that subjects in the longer onset group received more pharmacological treatment than those in short-term groups, suggesting a possible protective effect delaying onset. Moreover, the type of medication received was different for both converter groups compared with the nonconverter groups. Converters in both short-term and longer onset groups were treated significantly more often with antipsychotics and both non-converter groups more often with antidepressants.
Social Functioning
Table 2 presents the adjusted ORs derived from longitudinal models evaluating the association between conversion status and the likelihood of poor social and role functioning over time. All models are adjusted for positive and negative symptoms at baseline and medication treatment over follow-up. Baseline depression was not found to be a significant covariate, so it was not included in the GEE models. For social functioning, the odds of impairment are nearly 4 times greater in STCs (OR, 3.82; 95% CI, 1.08–13.51) and 5 times greater in LOCs (OR, 5.83; 95% CI, 1.15–29.54) than for matched non-converters. A separate GEE analysis, based on a smaller sample, found that the relationship between conversion and functioning was not affected when adjusting for baseline cognition (for more details, see online supplementary data and supplementary table S2).
Table 2.
Adjusted ORs and 95% CIs of the Occurrence of Poor Social and Role Functioning in CHR Patients Using Generalized Estimating Equations Models With Repeated Assessmentsa
| Social Functioning | Role Functioning | |||
| Short Term | Longer Onset | Short Term | Longer Onset | |
| Independent variables | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Conversion statusa | 3.82 (1.08–13.51)* | 5.83 (1.15–29.54)* | 4.12 (1.17–14.44)* | 3.26 (0.69–15.43) |
| Timeb | 2.23 (0.73–6.80) | 1.85 (0.42–8.17) | 4.90 (1.91–12.56)** | 1.62 (0.54–4.88) |
| Conversion × time | 0.45 (0.10–2.08) | 1.13 (0.11–11.89) | 0.32 (0.07–1.46) | 0.62 (0.10–3.86) |
| Follow-up medication | ||||
| Antipsychotics | 1.00 (0.24–4.18) | 1.10 (0.31–3.90) | 0.34 (0.06–1.82) | 0.53 (.130–2.17) |
| Antidepressants | 2.03 (0.71–5.80) | 1.30 (0.22–7.80) | 0.92 (0.21–3.97) | 1.68 (0.28–10.01) |
| SIPS score | ||||
| Positive | 0.98 (0.85–1.12) | 1.14 (0.95–1.36) | 0.99 (0.83–1.18) | 1.06 (0.93–1.21) |
| Negativec | 1.04 (0.93–1.16) | 1.40 (1.12–1.74)** | 1.14 (1.02–1.27)* | 1.23 (1.08–1.41)** |
Note: CHR, clinical high risk; SIPS, structured interview for prodromal syndromes. All covariates adjusted for in the model are listed as independent variables.
The reference group for conversion status was CHR matched controls.
The reference group for time was last observation period/psychosis onset.
Negative symptoms included avolition, decreased expression of emotions, decreased experience of emotions and self, and decreased ideational richness.
*P < .05, **P < .01.
Figure 2 illustrates the changes in probabilities of social impairment at baseline (time 1) and at follow-up (time 2). Figure 2A presents the data for STCs and matched non-converters and figure 2B for LOC subjects and matched non-converters. The higher the score, the greater the likelihood of poor functioning. Both groups of converters display high probabilities of social impairment (77%–87%) that are consistent over time, as indicated by the nonsignificant time effect and group × time interaction shown in table 2. The CHR non-converters in both matched subgroups show a far lower probability of impairment (group main effect, P < .05, table 2) with change nonsignificant but suggesting improvement. Considered overall, these findings indicate that converters, regardless of time to onset, are far more likely to be socially impaired at baseline than nonconverting CHR individuals and to remain so over time.
Role Functioning
As shown in table 2 and figures 3A and 3B, baseline differences and change over time for role functioning (ie, about two-thirds school performance, remaining third work, with no differences between the 2) are more inconsistent than found for social, especially for the yoked LOC groups. Analyses of the ORs for the STC vs non-converters presented in table 2 shows main effect for group (P < .05) and time (P < .01) and a nonsignificant group × time interaction after controlling for baseline symptoms and medication. Adjusted ORs for impaired role functioning associated with conversion in the STCs was 4.12 (95% CI, 1.17–14.44). As shown in figure 3A, both STCs (77%–69%) and matched non-converters (66%–32%) show significantly less likelihood that role will continue to be impaired over time (OR, 4.90; 95% CI, 1.91–12.56), indicating that for STCs, role problems fluctuate and are not directly associated with the onset of psychosis. This relationship was not affected by controlling for cognition (Supplementary table S2).
The findings for LOC comparisons are quite different than for STC. Initial analyses indicated that the longer onset converters were significantly impaired relative to non-converters in role functioning at baseline and follow-up. However, after controlling for covariates, there were no significant group or time main effects or interaction between time and group. Negative symptoms were the most significant covariate. An additional set of analyses were run controlling for cognition, but as in the case of STC role functioning and social functioning for both converter samples, controlling for cognition did not impact any of the comparisons. Thus, it is likely that negative symptoms differentially contributed to poor school/work performance in individuals requiring substantial follow-up prior to conversion.
Comments
Three findings from the current study support impaired social functioning to be an important risk factor for psychosis: (1) early social deficits are impaired in subjects at CHR who later developed psychosis compared with matched CHR subjects who did not convert to psychosis over follow-up; (2) impaired social functioning appears to be a long-standing trait that is stable over time; and (3) social functioning is independent of clinical state and, in particular, of emerging psychosis. As will be discussed, role functioning partially adheres to this pattern but not sufficiently to be conclusive about risk factor status.
Converters vs Non-converters.
Establishing that individuals destined to develop psychosis display deficits in functioning compared with those at the same baseline risk who do not convert is a first critical step in establishing risk factor status. This case was solidly made by the data presented here for social skills, which was impaired in the 2 converter samples under study relative to matched CHR non-converters at baseline. These findings are consistent with a number of previous studies indicating social difficulties to be characteristic of preschizophrenia individuals at early ages.17,22–26,28,30,42 The differences between converters and CHR non-converters in this study were not as consistent for impaired school performance (or early employment difficulties) and, for longer onset converters, seemed to be largely attributable to negative symptoms.
Stability of Functional Deficits.
Stability is an obvious requirement for a deficit to be considered a long-standing risk factor or trait. There are 2 ways in which the data reported here support the stability of social skill difficulties. First, evidence is provided cross-sectionally: comparable social deficits were displayed by individuals converting to psychosis shortly after intake (Short-term converters, late prodrome) and in those subjects remaining prodromal for many months prior to conversion (Longer onset converters, earlier prodrome). These data indicate that social problems are stable across phases of the prodrome. The findings for role functioning partially fit this cross-sectional pattern but, once again, are not as consistent as for social deficits. The second source of evidence for stability is the longitudinal prospective data indicating that there is little change in functioning from baseline through onset of psychosis for converters, and this observation holds comparably true for both social and role functioning. By contrast, nonconverting CHR subjects display improvement across time in role functioning, suggesting that repeated assessments might be one important means of separating true from false positive CHR identifications.
Independence From Clinical State.
The longitudinal data also strongly support the independence of functioning from clinical state. None of the clinical domains (baseline positive or negative symptoms, depression, or emergence of psychosis) influenced social skills, which appears to be a long-standing independent domain of functioning. Similarly, neither baseline positive symptoms nor the emergence of psychosis immediately impact role functioning, either at school or at work. This finding is consistent with Piskulic et al38 who reported that patients undergoing an initial psychotic episode are comparable in functioning with CHR subjects using the current GF measures. While role functioning typically worsens with chronicity, absence of change with the onset of psychosis in the current data supports the suggestion that this deterioration is likely due to a range of factors associated with illness, including hospitalization, medication, poor care, and a variety of environmental factors.13
Role vs Social Functioning.
A major difference between role and social functioning emerged when controlling for negative symptoms. Unlike social functioning, role difficulties appear to be related to negative symptoms in converters with relatively slow onset. The substantial differences in baseline role functioning displayed by LOCs compared with matched non-converters lost significance when controlled for baseline negative symptoms. Negative symptoms, however, did not similarly influence role in STCs. These findings suggest that the LOCs may be a somewhat different group of converters and may represent subjects with prominent negative symptoms and insidious course, who are likely to be seeking treatment for long-standing functional problems, very likely beginning in early school years. The findings reported here are in keeping with those previously reported in the larger Cannon et al25 study where role problems did not predict later psychosis independently of social deficits. However, the dramatic level of impairment of role functioning across LOCs suggests that rather than specifically predicting psychosis, this domain may be a critical predictor of long-term disability.
Comparison Between STC and LOC Subgroups.
Within the nested case-control design, the sample was divided into subjects who converted in 6–8 weeks after intake and individuals who required a year or more of follow-up before converting. Each group is compared with yoked non-converters to provide risk factor information controlling for confounds. However, additional information can be obtained by comparing the 2 converter groups directly with each other. A major theoretical interest is whether the short onset group includes individuals already actively transitioning to psychosis or who are possibly psychotic but too guarded when originally recruited to report the full extent of their symptoms at intake. By contrast, longer onset individuals might be more strictly prodromal. The results of this study appear to disprove this hypothesis and suggest that the 2 groups are very similar on most measures at baseline. There are no differences between converter groups in demographic variables, axis I diagnosis at baseline or follow-up, depression, positive symptoms, or social functioning at baseline. However, a key difference was found in that only the LOCs showed a direct link between role functioning and negative symptoms.
An additional, interesting difference between converter groups is in type of medication over follow-up. While the numbers are small and treatment was given in a nonrandomized noncontrolled context, 58% of LOCs vs 31% of STCs received antipsychotics over follow-up, suggesting that it is possible that treatment with antipsychotics delayed onset. In both cases, far fewer matched nonconverters were treated with antipsychotics. However, far more subjects in both CHR non-converter groups received antidepressants. This finding is consistent with the conclusions from the Cornblatt et al43 study suggesting that antidepressants are appropriate as a first-line treatment in many cases because they may be neuroprotective for those at true risk and are a more benign treatment for false positive CHR cases. However, these possibilities require evaluation in randomized controlled studies.
Relationship Between Neurocognition and Functioning.
While cognition was related to functioning, adjusting for baseline cognitive performance did not affect the pattern of group differences in either functional domain. This result is consistent with a recent study by Carrión et al44 that found cognition accounted for about 18–19% of the variance of functioning in adolescents at CHR for developing psychosis. Overall, this suggests that while cognition is an active component of functioning, it only explains some of the variance in long-term disability and implicates a number of other factors, some primarily environmental, for example lack of social services.13
A major strength of this study is the matched case-control design, which offsets a number of potential confounds, especially differences between sites. The primary drawback of this design, however, is that the full data set is not utilized. There were also more missing cognitive and follow-up clinical assessments than optimal, a problem largely resulting from combining sites that were originally designed and conducted independently of each other.
Implications of Findings.
Considered overall, these findings highlight the importance of early intervention. By initiating treatment early, possibly prior to the emergence of distinct positive symptoms, long-term functioning may be remediated and maintained. Early treatment is especially important because early to late adolescence is the developmental period during which social and role skills crystallize.30 Consistent with the model proposed by Cornblatt et al,29 improvement of the underlying vulnerability may, in itself, be a means of reducing the risk for later psychosis and, independently, limiting future functional disability. The findings reported suggest that a future direction should be to evaluate the extent to which adding long-standing social deficits to APS criteria may serve to improve the predictive validity of the CHR construct.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
National Institute of Mental Health (R01 MH061523, U01 MH081857 to Dr B.A.C.; R18 MH43518, U01 MH081928, P50 MH080272 to Dr L.S.; R01 MH65079 to Dr T.D.C.; RO1 MH062066, 5U01 MH081988 to Dr E.F.W.; R01 MH60720, K24 MH76191 to Dr K.S.C.; K05 MH01654 to Dr T.H.M.; U01 MH066069, P50 MH064065 to Dr D.O.P.; R18 MH 43518 to Dr M.T.; U01 MH74356, U01 MH082022, R41 MH083436 to Dr S.W.W.; and U01 MH066134 to Dr J.A.).
Acknowledgments
We thank the study participants for their time and effort. We also thank Jennifer Johnson, PhD (UCLA), Diane Kirsopp, BA (University of Toronto), and Roy Money, MS (Yale University) for their contributions to the NAPLS I database described in this article. The authors also thank Andrea Auther, PhD, Lauren Baskir, PhD, and Ruth Olsen, BS. Conflict of interest: Dr. Cornblatt was the original developer of the CPT-IP and has been an advisor for Bristol-Myers Squibb and Merck. Dr. Lencz has received consulting fees and/or honoraria from Eli Lilly, Merck, Clinical Data Inc., GoldenHelix, Inc., Guidepoint Global, and Cowen & Co. Dr. Carrión has not received funding from for-profit entities. Dr. Seidman has not received funding from for-profit entities in the past 12 months. In the past he received unrestricted educational support from Janssen Pharmaceuticals and has served as a consultant for Shire. Dr. Walker has not received funding from for-profit entities. Dr. Cannon has served as a consultant for Janssen Pharmaceuticals and Eli Lilly and Company. Dr. Cadenhead has not received funding from for-profit entities. Dr. McGlashan has served as a consultant for Eli Lilly and Company, Pfizer, Solvay/Wyeth, and Roche Pharmaceuticals. Dr. Perkins has received research funding from Janssen Pharmaceuticals and Dainippon Sumitomo Pharma in the past 12 months. In the past Dr. Perkins received research funding from AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Otsuka Pharmaceutical Co Ltd, Eli Lilly and Company, Janssen Pharmaceuticals, and Pfizer and consulting and educational fees from AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly and Company, Janssen Pharmaceuticals, GlaxoSmithKline, Forest Labs, Pfizer, and Shire. Dr. Tsuang has received research grants from Janssen Pharmaceuticals. Dr. Woods has received research funding support from multiple for-profit entities including UCB Pharma and Bristol- Myers Squibb and has consulted for Otsuka and Schering-Plough. Dr Woods has not served on speaker's bureaus. Dr. Heinssen is an employee of the nonprofit National Institutes of Health and has had no financial relationships with for-profit entities. Dr. Addington has served as a consultant for Pfizer, AstraZeneca Pharmaceuticals, and Janssen Pharmaceuticals.
References
- 1.Cornblatt B, Lencz T, Smith C, Auther A. Treatment of the schizophrenia prodrome. In: Tsuang MT, Stone WS, Lyons MJ, editors. Recognition and Prevention of Major Mental and Substance Use Disorders. 1st ed. Washington, DC: American Psychiatric Publishing; 2007. pp. 159–185. [Google Scholar]
- 2.Carpenter WT, Jr., Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145:578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- 3.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 4.Harvey PD, Reichenberg A, Bowie CR, Patterson TL, Heaton RK. The course of neuropsychological performance and functional capacity in older patients with schizophrenia: influences of previous history of long-term institutional stay. Biol Psychiatry. 2010;67:933–939. doi: 10.1016/j.biopsych.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamilton SH, Edgell ET, Revicki DA, Breier A. Functional outcomes in schizophrenia: a comparison of olanzapine and haloperidol in a European sample. Int Clin Psychopharmacol. 2000;15:245–255. doi: 10.1097/00004850-200015050-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bond GR, Kim HW, Meyer PS, et al. Response to vocational rehabilitation during treatment with first- or second-generation antipsychotics. Psychiatr Serv. 2004;55:59–66. doi: 10.1176/appi.ps.55.1.59. [DOI] [PubMed] [Google Scholar]
- 7.Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry. 2006;163:2080–2089. doi: 10.1176/ajp.2006.163.12.2080. [DOI] [PubMed] [Google Scholar]
- 8.Bellack AS, Gold JM, Buchanan RW. Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophr Bull. 1999;25:257–274. doi: 10.1093/oxfordjournals.schbul.a033377. [DOI] [PubMed] [Google Scholar]
- 9.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 10.Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Niendam TA, Bearden CE, Zinberg J, Johnson JK, O'Brien M, Cannon TD. The course of neurocognition and social functioning in individuals at ultra high risk for psychosis. Schizophr Bull. 2007;33:772–781. doi: 10.1093/schbul/sbm020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowie CR, Leung WW, Reichenberg A, et al. Predicting schizophrenia patients' real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008;63:505–511. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harvey PD, Helldin L, Bowie CR, et al. Performance-based measurement of functional disability in schizophrenia: a cross-national study in the United States and Sweden. Am J Psychiatry. 2009;166:821–827. doi: 10.1176/appi.ajp.2009.09010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res. 2008;99:119–124. doi: 10.1016/j.schres.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cannon M, Jones P, Huttunen MO, et al. School performance in Finnish children and later development of schizophrenia: a population-based longitudinal study. Arch Gen Psychiatry. 1999;56:457–463. doi: 10.1001/archpsyc.56.5.457. [DOI] [PubMed] [Google Scholar]
- 16.Done DJ, Crow TJ, Johnstone EC, Sacker A. Childhood antecedents of schizophrenia and affective illness: social adjustment at ages 7 and 11. BMJ. 1994;309:699–703. doi: 10.1136/bmj.309.6956.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dworkin RH, Green SR, Small NE, Warner ML, Cornblatt BA, Erlenmeyer-Kimling L. Positive and negative symptoms and social competence in adolescents at risk for schizophrenia and affective disorder. Am J Psychiatry. 1990;147:1234–1236. doi: 10.1176/ajp.147.9.1234. [DOI] [PubMed] [Google Scholar]
- 18.Dworkin RH, Lewis JA, Cornblatt BA, Erlenmeyer-Kimling L. Social competence deficits in adolescents at risk for schizophrenia. J Nerv Ment Dis. 1994;182:103–108. doi: 10.1097/00005053-199402000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Jones P, Rodgers B, Murray R, Marmot M. Child development risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet. 1994;344:1398–1402. doi: 10.1016/s0140-6736(94)90569-x. [DOI] [PubMed] [Google Scholar]
- 20.Hans SL, Auerbach JG, Asarnow JR, Styr B, Marcus J. Social adjustment of adolescents at risk for schizophrenia: the Jerusalem Infant Development Study. J Am Acad Child Adolesc Psychiatry. 2000;39:1406–1414. doi: 10.1097/00004583-200011000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Tarbox SI, Pogue-Geile MF. Development of social functioning in preschizophrenia children and adolescents: a systematic review. Psychol Bull. 2008;134:561–583. doi: 10.1037/0033-2909.34.4.561. [DOI] [PubMed] [Google Scholar]
- 22.Ruhrmann S, Schultze-Lutter F, Salokangas RK, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2010;67:241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- 23.Hafner H, Nowotny B. Epidemiology of early-onset schizophrenia. Eur Arch Psychiatry Clin Neurosci. 1995;245:80–92. doi: 10.1007/BF02190734. [DOI] [PubMed] [Google Scholar]
- 24.Cornblatt BA, Auther AM, Niendam T, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33:688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riecher-Rössler A, Pflueger MO, Aston J, et al. Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol Psychiatry. 2009;66:1023–1030. doi: 10.1016/j.biopsych.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 27.Ruhrmann S, Schultze-Lutter F, Klosterkotter J. Probably at-risk, but certainly ill—advocating the introduction of a psychosis spectrum disorder in DSM-V. Schizophr Res. 2010;120:23–37. doi: 10.1016/j.schres.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Velthorst E, Nieman DH, Linszen D, et al. Disability in people clinically at high risk of psychosis. Br J Psychiatry. 2010;197:278–284. doi: 10.1192/bjp.bp.109.075036. [DOI] [PubMed] [Google Scholar]
- 29.Cornblatt BA, Lencz T, Smith CW, Correll CU, Auther AM, Nakayama E. The schizophrenia prodrome revisited: a neurodevelopmental perspective. Schizophr Bull. 2003;29:633–651. doi: 10.1093/oxfordjournals.schbul.a007036. [DOI] [PubMed] [Google Scholar]
- 30.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–370. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 31.Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- 32.Addington J, Cadenhead KS, Cannon TD, et al. North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33:665–672. doi: 10.1093/schbul/sbl075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woods SW, Addington J, Cadenhead KS, et al. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009;35:894–908. doi: 10.1093/schbul/sbp027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seidman LJ, Giuliano AJ, Meyer EC, et al. Neuropsychology of the prodrome to psychosis in the NAPLS consortium: relationship to family history and conversion to psychosis. Arch Gen Psychiatry. 2010;67:578–588. doi: 10.1001/archgenpsychiatry.2010.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Auther A, Smith C, Cornblatt B. Global Functioning Scale: Social (GFS: Social) Glen Oaks, NY: Zucker-Hillside Hospital; 2006. [Google Scholar]
- 36.Niendam TA, Bearden CE, Johnson JK, Cannon TD. Global Functioning Scale: Role (GFS: Role) Los Angeles: University of California; 2006. [Google Scholar]
- 37.Addington J, Cornblatt BA, Cadenhead KS, et al. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011;168:800–805. doi: 10.1176/appi.ajp.2011.10081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piskulic D, Addington J, Auther A, Cornblatt BA. Using the global functioning social and role scales in a first-episode sample. Early Interv Psychiatry. 2011;5:219–223. doi: 10.1111/j.1751-7893.2011.00263.x. [DOI] [PubMed] [Google Scholar]
- 39.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 40.Diggle P, Liang K-Y, Zeger SL. Analysis of Longitudinal Data. New York, NY: Oxford University Press; 1994. [Google Scholar]
- 41.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 42.Corcoran CM, Kimhy D, Parrilla-Escobar MA, et al. The relationship of social function to depressive and negative symptoms in individuals at clinical high risk for psychosis. Psychol Med. 2011;41:251–261. doi: 10.1017/S0033291710000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cornblatt BA, Lencz T, Smith CW, et al. Can antidepressants be used to treat the schizophrenia prodrome? Results of a prospective, naturalistic treatment study of adolescents. J Clin Psychiatry. 2007;68:546–557. doi: 10.4088/jcp.v68n0410. [DOI] [PubMed] [Google Scholar]
- 44.Carrión RE, Goldberg TE, McLaughlin D, Auther AM, Correll CU, Cornblatt BA. Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am J Psychiatry. 2011;168:806–813. doi: 10.1176/appi.ajp.2011.10081209. [DOI] [PMC free article] [PubMed] [Google Scholar]