Abstract
Stromal–epithelial interaction is crucial to mediate normal prostate and prostate cancer (PCa) development. The indispensable roles of mesenchymal/stromal androgen receptor (AR) for the prostate organogenesis have been demonstrated by using tissue recombination from wild-type and testicular feminized mice. However, the stromal AR functions in the tumour microenvironment and the underlying mechanisms governing the interactions between the epithelium and stroma are not completely understood. Here, we have established the first animal model with AR deletion in stromal fibromuscular cells (dARKO, AR knockout in fibroblasts and smooth muscle cells) in the Pten+/− mouse model that can spontaneously develop prostatic intraepithelial neoplasia (PIN). We found that loss of stromal fibromuscular AR led to suppression of PIN lesion development with alleviation of epithelium proliferation and tumour-promoting microenvironments, including extracellular matrix (ECM) remodelling, immune cell infiltration and neovasculature formation due, in part, to the modulation of pro-inflammatory cytokines/chemokines. Finally, targeting stromal fibromuscular AR with the AR degradation enhancer, ASC-J9®, resulted in the reduction of PIN development/progression, which might provide a new approach to suppress PIN development.
Keywords: androgen receptor, PIN, prostate stroma, PTEN, tumour microenvironment
INTRODUCTION
Emerging evidence has shown that the tumour microenvironments play crucial roles in the prostate cancer (PCa) development/progression (Ammirante et al, 2010; Erez et al, 2010; Santos et al, 2009; Trimboli et al, 2009). The tumour stromal cells can foster the oncogenic epithelial cell growth through secretion of paracrine growth factors and providing a more favorable microenvironment for tumour growth. One line of evidence used tissue recombination to show that when initiated benign prostatic hyperplasia (BPH) epithelial cell line BPH-1 cells (immortalized by SV40-T antigen) were combined with normal fibroblasts or carcinoma associated fibroblasts (CAFs), large tumour growth only occurred in BPH-1 with CAFs recombinants. The results indicated that the tumourigenesis of BPH-1 cells required signalling support from CAFs, but not from normal fibroblasts (Cunha et al, 2002, 2003; Hayward et al, 2001). To determine the stromal androgen receptor (AR) roles in the elicitation of hormonal-mediated carcinogenesis, tissue recombinants from wild-type (Wt) or testicular feminized (Tfm) urogenital sinus mesenchyme (UGM) were mixed with BPH-1 cells following estradiol 17-beta (E2) + testosterone (T) treatment. The BPH-1 cells could undergo tumourigenesis and develop tumours only in the presence of functional mesenchymal AR (Cunha et al, 2002, 2003, 2004; Ricke et al, 2006). Furthermore, tissue recombinant result from PC-3 (prostate epithelium) and AR siRNA knockdown in WPMY-1 cells (prostate stroma) revealed that stromal AR is essential to support PC-3 cell growth, leading to larger tumour development (Niu et al, 2008a, b). Taken together, the previous studies using tissue recombination suggested that stromal AR could promote PCa development/progression. However, how stromal AR influences oncogenic epithelium cell growth, especially in the real physiological condition with intact immune systems in mice, is still unresolved.
The phosphatase and tensin homologue deleted from chromosome 10 (PTEN) or mutated in multiple advanced cancers (MMAC1) gene was originally identified as a tumour suppressor gene located at chromosome 10q23 (Myers et al, 1997). The PTEN gene is one of the most frequently mutated or deleted genes in various human cancers including lymphoid, breast, endometrial, glioblastoma and prostate (Bose et al, 1998; Wang et al, 2003; Webber et al, 1999). PTEN is a multifunctional phosphatase to dephosphorylate the substrate of phosphatidylinositol (3,4,5)-triphosphate (PIP3; Maehama & Dixon, 1998). By dephosphorylating the D3 position of PIP3, PTEN negatively regulates the PI3K pathway and triggers its downstream Akt activation. The lipid phosphatase activity and Akt activity were associated with tumour suppression (Goberdhan & Wilson, 2003; Li et al, 1997). PTEN mutations or deletions have been implicated in the PCa development (Gray et al, 1998; Whang et al, 1998), being present in 30% of primary prostate tumours (Dahia, 2000) and around 63% of metastatic human prostate tissue samples (Suzuki et al, 1998; Trotman et al, 2006, 2003). To approach the PTEN pathophysiological roles in PCa development, several PTEN mutant mouse lines have been established and characterized (Backman et al, 2004; Cully et al, 2006; Di Cristofano et al, 2001; Podsypanina et al, 1999; Trotman et al, 2003; Wang et al, 2003). Heterozygous PTEN mutant mice (Pten+/−) were reported to show prostatic intraepithelial neoplasia (PIN) lesions in the adult mice, however, PIN lesions never proceed to PCa or metastatic tumours, suggesting that loss of one allele of the PTEN gene is not sufficient to cause the onset of PCa (Chen et al, 2006; Park et al, 2002). The biallelic mutation of the PTEN gene or the 2nd hit of loss-of-function in tumour suppressor genes could promote advanced PCa progression (Abate-Shen et al, 2003; Chen et al, 2006; Kim et al, 2002; Wang et al, 2003). Histopathological phenotypes revealed that invasive adenocarcinoma was frequently observed in epithelial PTEN null mice older than 12 weeks (Wang et al, 2003). Other PTEN specific KO mice were concurrently established by breeding mouse mammary tumour virus-long terminal repeat promoter cre mice with floxed Pten mice, resulting in aberrant prostate morphology that exhibited high grade-PIN (HG-PIN) with frequent invasion into adjacent stromal compartments (Backman et al, 2004).
Since prostate stromal AR has a potential contribution to the PCa development, we characterized this stromal fibromuscular ARKO (dARKO) mouse model with PTEN haplo-insufficiency. Here, we identified that stromal fibromucular AR could regulate PIN lesion formation, epithelium proliferation and the tumour-promoting microenvironment in Pten+/− mice. Finally, targeting stromal fibromuscular AR via the AR degradation using ASC-J9® could yield the therapeutic effects through modulation of the stromal–epithelial interaction and alteration of the tumour-promoting microenvironments.
RESULTS
Generation and characterization of dARKO/Pten+/− mice lacking AR in cancer associated stromal cells
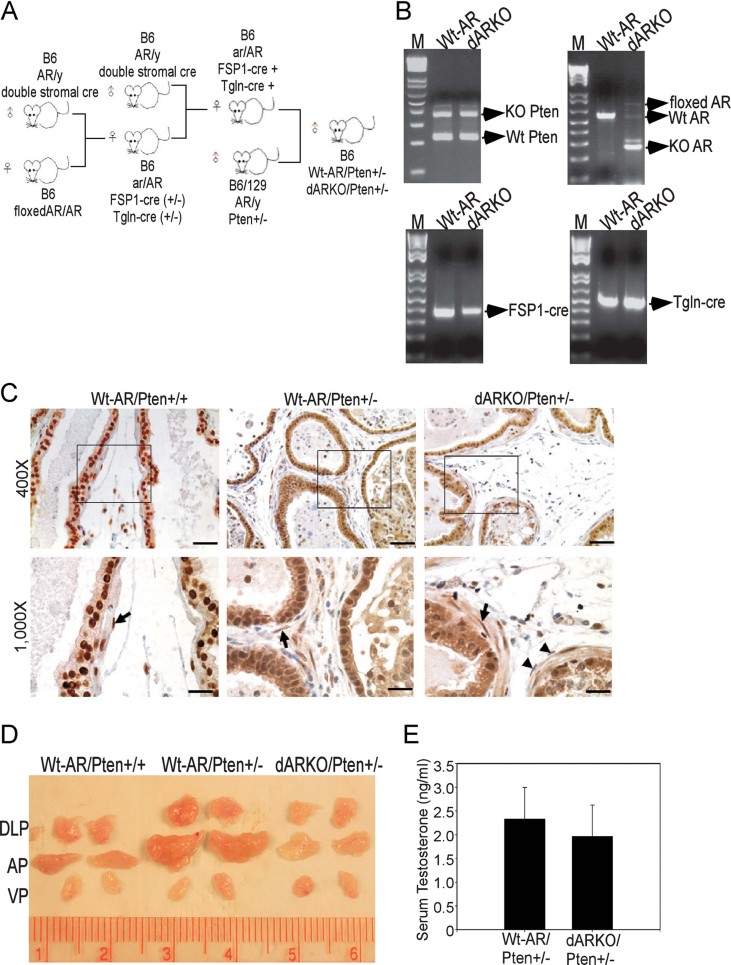
To dissect the stromal AR roles in prostate tumourigenesis, we generated a new mouse model (named as dARKO/Pten+/−) that has selective AR deletion in stromal cells (both fibroblasts and smooth muscle cells; Lai et al, 2012) via mating mice carrying FSP1-cre (Bhowmick et al, 2004) and transgelin cre (Tgln-cre; Li et al, 1996) with floxed AR mice (Yeh et al, 2002), then bred the resulting FSP1-cre/Tgln-cre/ARflox/+ mice with Pten+/− mice (see detailed mating strategy in Fig 1A). The tail genotyping results demonstrated the new dARKO/Pten+/− mice carried the transgenes, FSP1-cre, Tgln-cre, floxed AR allele and had PTEN heterozygosity (Fig 1B).
Figure 1. Generation and characterization of stromal fibromuscular ARKO in Pten+/− mice.
- Mating strategy of dARKO/Pten+/− mouse generation.
- Genotyping results of Wt-AR/Pten+/− and dARKO/Pten+/− mice by using 2–9/select, FSP1-cre, Tgln-cre and Pten primer sets. Tail genomic DNA was isolated from Wt-AR/Pten+/− and dARKO/Pten+/− mice and PCR genotyping was performed to identify Wt and deleted AR fragment, FSP1-cre, Tgln-cre and Pten alleles.
- DLPs from 9-month-old Wt-AR/Pten+/+, Wt-AR/Pten+/− and dARKO/Pten+/− mice were subjected to AR IHC staining. Arrows indicate the AR immunoreactive stromal cells and arrowheads represent the AR negative stromal cells. Epithelium from three different genotypes of mice all showed AR positive expressions. Data are presented as mean ± SEM. N = 5 mice per group. Scale Bars = 200 µm (400×) and 50 µm (1000×).
- Loss of stromal fibromuscular AR reduced prostate size in APs and DLPS of Pten+/− mice. The representative gross appearance from 9-month-old Wt-AR/Pten+/+, Wt-AR/Pten+/− and dARKO/Pten+/− mouse prostates.
- Serum testosterone was monitored by collecting the serum from 9-month-old Wt-AR/Pten+/− and dARKO/Pten+/− mice. The testosterone ELISA kit was used per the manufacturer's instructions. Data are presented as mean ± SEM. N = 5 mice per group.
Immunohistochemistry (IHC) staining of dorsolateral prostate (DLPs) lobes from Wt-AR/Pten+/+, Wt-AR/Pten+/− and dARKO/Pten+/− mice using an antibody against the AR C-terminal showed partial AR deletion, which was restricted to the stromal fibromuscular cells, but this deletion was not seen in the adjacent epithelium (Fig 1C).
Consistent with a previous report (Podsypanina et al, 1999), we found that in the Wt-AR/Pten+/− mice, the anterior-prostates (APs) and DLPs had larger size compared to those found in Wt-AR/Pten+/+ mice, indicating the development of PIN lesions (Chen et al, 2006; Park et al, 2002; Podsypanina et al, 1999). We then examined the effects of loss of stromal fibromuscular AR on PIN lesion development judged by prostate size. As shown in Fig 1D, we found the prostate size displayed significant reduction (APs and DLPs) in dARKO/Pten+/− mice, suggesting that stromal fibromuscular AR might play positive roles to promote PIN lesion development.
Furthermore, the serum testosterone levels were found to be similar between dARKO/Pten+/− mice and their Wt littermates, indicating that altered phenotypes (described in the next sections) found in the dARKO/Pten+/− mice were not due to the change of circulating testosterone (Fig 1E).
Collectively, results from Fig 1A–E showed that we successfully established the stromal dARKO mice with PTEN deficiency and also observed the reduced prostate size in dARKO/Pten+/− mice.
Loss of stromal fibromuscular AR diminished PIN lesion development
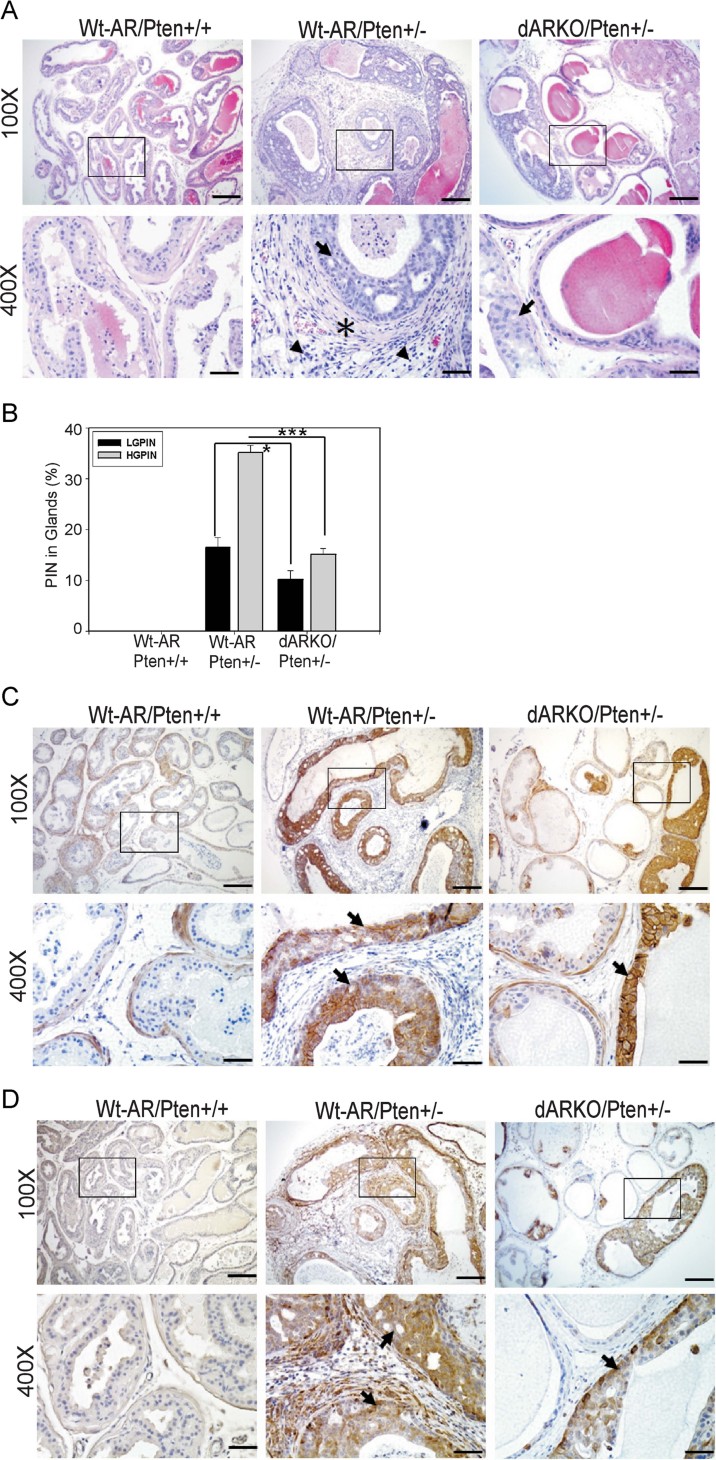
We then applied H&E staining to examine PIN lesions in 9-month-old Wt-AR/Pten+/− mice and found multicellular layered or cribriform structures of low-grade/high-grade-PIN (LG-/HG-PIN) prostate glands (Fig 2A arrows) as compared to a single layer of epithelial glandular structure in Wt-AR/Pten+/+ mice. This Pten+/− mouse is a germline mutation and the PIN lesion was concurrently observed in the proximal and distal regions of prostate ducts (Supporting Information Fig S1A and B arrows), which was distinct from using the cre-loxP system to knockout PTEN alleles in the prostate epithelium. Comparing two prostate epithelial specific cre mediated PTEN disruptions (PSA-cre and probasin-cre), the PSA-cre driven PTEN deletion caused hyperplasia was restricted to the distal luminal epithelial cells (Korsten et al, 2009). However, the probasin-cre mediated PTEN deletion caused tumour development arising from basal/stem cells in the proximal regions (Wang et al, 2006). Therefore, the phenotypes we observed from Pten+/− mice were not due to the differential effects of Pten gene loss in luminal or basal/stem epithelial cells.
Figure 2. Loss of stromal fibromuscular AR leads to diminished PIN lesion development.
N = 6–7 mice per group
- Histological examination of 9-month-old Wt-AR/Pten+/+, Wt-AR/Pten+/− and dARKO/Pten+/− mouse DLPs subjected to H&E staining. The PIN lesions are presented as multi-layered epithelium and typical cribriform structures pointed-out by arrows. The asterisk marks the reactive stroma surrounding the PIN lesions and arrowheads indicate infiltrated immune cells located in the stromal compartments. Scale Bars = 200 µm (100×) and 50 µm (400×).
- Quantification of LG-/HG-PIN in Wt-AR/Pten+/+, Wt-AR/Pten+/− and dARKO/Pten+/− mouse DLPs at 9-month-old (N = 5 mice for each group). Data are presented as mean ± SEM. *p < 0.05, ***p < 0.001.
- IHC staining against p-Akt at Ser473. Arrows indicate p-Akt positive epithelium. Scale Bars = 200 µm (100×) and 50 µm (400×).
- IHC staining of p-S6RP (Ser235/236). Arrows indicate p-S6RP positive epithelium. Scale Bars = 200 µm (100×) and 50 µm (400×).
Importantly, we found DLPs from dARKO/Pten+/− mice displayed diminished PIN formation as compared to those found in the Wt-AR/Pten+/− mice (Fig 2A and Supporting Information Fig S1). The LG-/HG-PIN lesion quantification results (Fig 2B) further confirmed that the loss of stromal fibromuscular AR not only reduced the PIN initiation, but also retarded the LG-PIN progression.
Loss of PTEN leads to activation of phospho-Akt (p-Akt), which can further trigger the downstream signals such as mammalian target of rapamycin (mTOR), forkhead box 01A (FOXO1A) and phosphorylated S6 Ribosomal Protein (p-S6RP) to influence PCa cell survival and cell cycle control (Trotman et al, 2006, 2003). Therefore, we applied p-Akt (at Ser 473) IHC staining and found the staining signal was significantly reduced in the dARKO/Pten+/− mice as compared to that found in Wt-AR/Pten+/− mice (Fig 2C arrows), implicating reduction of PIN formation. As expected, we also found similar results in p-S6RP (at Ser 235/236) IHC staining in the dARKO/Pten+/− mice (Fig 2D arrows).
Together, results from Fig 1D and Fig 2A–D clearly demonstrated that stromal fibromuscular AR played positive roles in promoting PIN lesion development. This positive role of stromal AR is in contrast to our earlier report showing negative roles of AR in basal/intermediate epithelial cells to suppress PCa progression/invasion and indicates a differential AR role depending on the cell type (Niu et al, 2008a, 2008b, 2010).
Stromal fibromuscular AR plays a positive role in promoting PIN development and modulates the tumour-promoting microenvironment
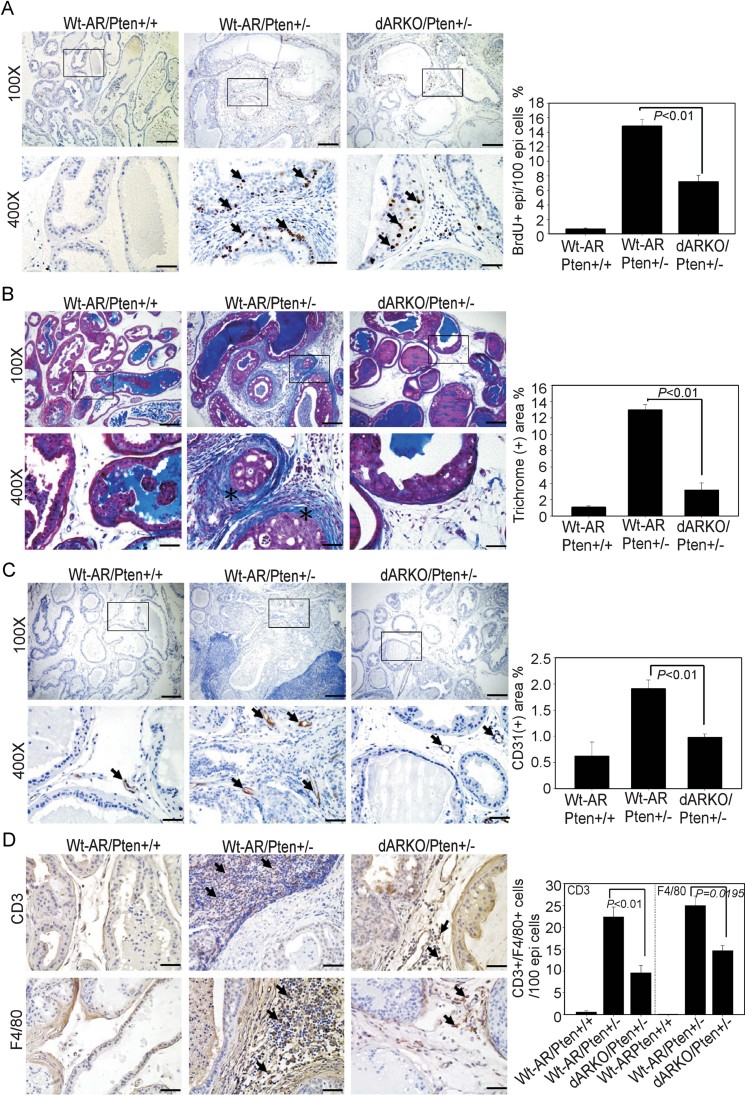
In order to dissect the possible mechanisms of how stromal fibromuscular AR could play a positive role in PIN development, we first examined its influences on the adjacent epithelial cell proliferation. The BrdU staining (for proliferation index) of epithelial cells was decreased in dARKO/Pten+/− mice as compared to that found in the Wt-AR/Pten+/− mice (Fig 3A arrows and quantitation in right panel), suggesting that epithelial cell proliferation within the PIN lesions still relied on stromal AR mediated signals.
Figure 3. Stromal fibromuscular AR regulates epithelium proliferation, ECM remodelling, neovasculature formation and immune cell infiltration in Pten deficient mice.
N = 6–7 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×). The quantification results are in the right panels of each figure.
- BrdU staining was used to evaluate proliferative cells. Arrows indicate BrdU positive cells.
- Wt-AR/Pten+/+, Wt-AR/Pten+/− and dARKO/Pten+/− mouse DLPs were subjected to Masson's Trichrome staining to measure deposited collagen fibers that stain blue colors (asterisks).
- CD31 IHC staining was used to identify endothelial cells. Arrows indicate CD31+ endothelial cells.
- CD3 and F4/80 IHC staining of DLPs from three genotypes of mice were used to characterize infiltrated T-cells and macrophages, respectively. Arrows indicate CD3+ staining T-cells (upper panel) and F4/80+ macrophages (lower panel).
Next, we characterized several features of the tumour-promoting microenvironments such as extracellular matrix (ECM) remodelling, angiogenesis and immune cell infiltration. We applied Mason's Trichrome staining to evaluate the ECM remodelling of collagen deposition, which has been suggested to play crucial roles in the tumour initiation and progression (Santos et al, 2009; Trimboli et al, 2009). We also found loss of stromal fibromuscular AR resulted in decreased collagen fiber accumulation in the dARKO/Pten+/− mice (Fig 3B asterisks and quantitation in right panel). Moreover, we used IHC staining with an antibody against CD31 (endothelial cell marker to monitor angiogenic status) to confirm that neovasculature formation was substantially decreased in the dARKO/Pten+/− mice (Fig 3C arrows and quantitation in right panel).
Chronic inflammation and/or recurrent infection have been suggested to be involved in the etiology of PCa development (Roseman et al, 1984). Early reports also showed that infiltrating immune cells frequently accompanied the PIN lesions, which suggested immune cells might contribute to the development of PIN and PCa (De Marzo et al, 1999; Putzi & De Marzo, 2000). As expected, using IHC staining with antibodies against CD3 (T-cell marker) and F4/80 (macrophage marker), we found infiltrating immune cells were associated with the PIN lesions in the Wt-AR/Pten+/− mice (Fig 3D). As expected, the infiltrating T-cells/macrophages were significantly reduced in the dARKO/Pten+/− mice (Fig 3D and quantitation in right panel).
Together, results from Fig 3A–D suggested that reduced PIN development in dARKO/Pten+/− mice may be due to the changes of the tumour microenvironments such as the alteration of ECM remodelling, angiogenesis and immune cells infiltration, partly due to the loss of stromal fibromuscular AR.
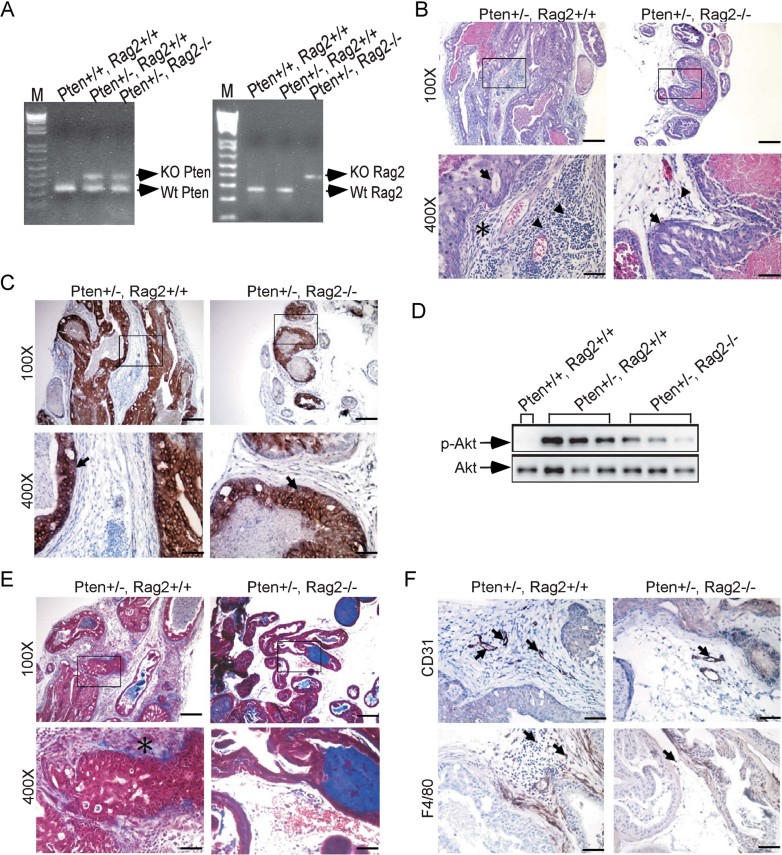
Abolishment of T-/B-cells in Pten+/− mice displays less PIN lesion development
According to the previous results in Figs 2 and 3, we found loss of stromal fibromuscular AR results in decreased PIN lesion and attenuation of tumour-promoting microenvironment. Then, we were interested to know whether infiltrating lymphocytes play any significant roles to promote or suppress PIN development, therefore, we established the Pten+/− mice with Rag2 gene deletion. In the Pten+/−, Rag2−/− mice, there are no mature T-/B-cells because Rag2 is essential for V(D)J rearrangement (Shinkai et al, 1992). Data on the generation of these mutant mice are provided in Fig 4A. We then characterized the PIN lesion in 7–8-month-old Pten+/−, Rag2+/+ and Pten+/−, Rag2−/− mice and found Pten+/−, Rag2−/− mice displayed PIN lesion reduction compared to Pten+/−, Rag2+/+ mice (Fig 4B). To further confirm the PIN lesion, we used p-AKT (at Ser 473) IHC staining (Fig 4C) as well as Western blotting (WB) from mouse DLPs (Fig 4D) and found similar results correlating with H&E staining. These results suggested that depletion of T-/B-cells infiltration and their mediated inflammatory response results in decreased PIN lesion formation.
Figure 4. Depletion of T-/B-cells attenuates PIN lesion formation in Pten+/− mice.
- Genotyping of Pten+/+, Rag2+/+; Pten+/−, Rag2+/+ and Pten+/−,Rag2−/− mice by using Pten and Rag2 primer sets. Tail genomic DNA was isolated and the PCR genotyping was performed to identify Wt or KO of Pten and Rag2 genes.
- H&E staining of 7–8-month-old Pten+/−, Rag2+/+ and Pten+/−, Rag2−/− mice. The PIN lesions are pointed-out by arrows and arrowheads indicate infiltrated immune cells located in the stromal compartments. The asterisk marks the reactive stroma. N = 4–5 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×).
- IHC staining of p-Akt at Ser473. Arrows indicate p-Akt positive epithelium. N = 4–5 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×).
- Proteins were extracted from DLPs of three genotypes of mice and p-Akt/Akt immunoblotting assays were used to determine the expression levels. The data are presented from one Pten+/+, Rag2+/+ mouse and three individual Pten+/−, Rag2+/+ or Pten+/−, Rag2−/− mice.
- Pten+/−, Rag2+/+ and Pten+/−, Rag2−/− mouse DLPs were subjected to Masson's Trichrome staining. The blue staining indicates collagen fibers (asterisk). N = 4–5 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×).
- CD31 and F4/80 IHC stainings were applied to detect endothelium and macrophages in the upper and lower panel, respectively. Arrows indicate CD31+ or F4/80 positive cells. N = 4–5 mice per group. Scale Bars = 50 µm (400×).
Furthermore, we analysed the tumour microenvironments by detection of collagen deposition (Fig 4E), neovasculature formation (Fig 4F; upper panels) and macrophage infiltration (Fig 4F; lower panels) and consistently each result showed a reduction in the Pten+/−, Rag2−/− mice compared to Pten+/−, Rag2+/+ mice.
Collectively, after removal of T-/B-cells in Pten+/− mice, we observed less PIN lesion accompanied by less tumour-promoting microenvironmental changes, suggesting that T and/or B-cells mediated inflammation may also contribute to the PIN devolvement.
Stromal fibromuscular AR regulates pro-inflammatory cytokines/chemokines to alter tumour microenvironment
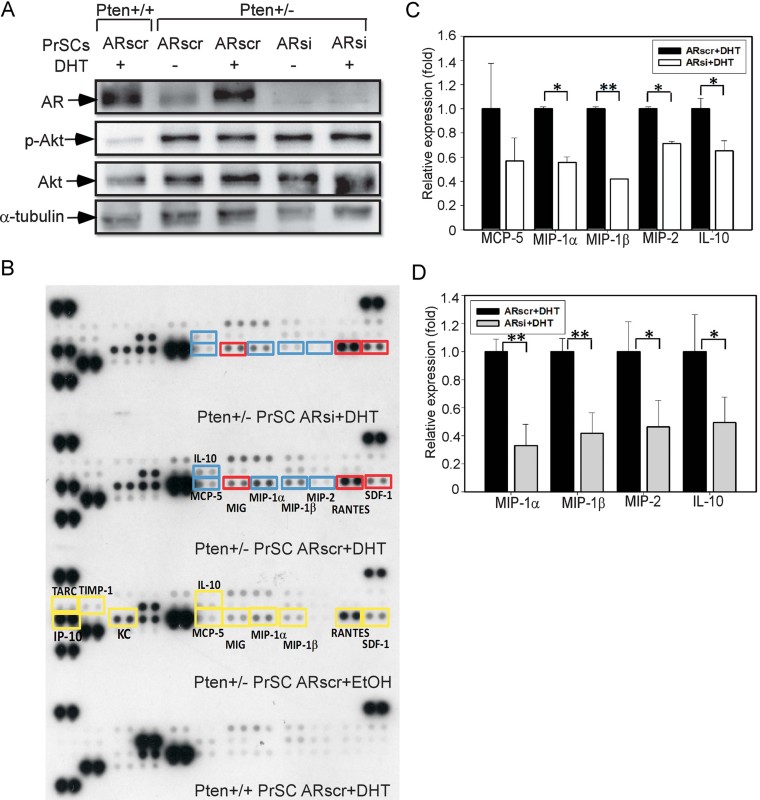
We have shown that loss of stromal fibromuscular AR led to decreased infiltrating T-cells/macrophages (Fig 3D) and depletion of T-/B-cells in Pten+/− mice also displayed a reduction of PIN lesion and attenuation of the tumour microenvironment (Fig 4). To explore the roles of immune cells mediated inflammation, which may contribute to the PIN development during prostate tumourigenesis (de Visser et al, 2006; Karin & Greten, 2005), we examined whether AR in cancer-associated fibroblasts (CAFs) was able to control pro-inflammatory cytokines/chemokines production to affect the immune cells recruitment. We used primary culture of prostate stromal cells (PrSCs) from DLPs of Pten+/+ and Pten+/− mice and used lentivirus carrying ARsiRNA (ARsi) to knockdown AR compared to ARscramble (ARscr) controls. As shown in Fig 5A, we successfully isolated the PrSCs from Pten+/+ and Pten+/− mouse prostates and established the AR siRNA knockdown stromal cells. The results showed that p-AKT (at Ser 473) expression was only elevated in the PrSCs isolated from Pten+/− mice, but not from Pten+/+ controls (Fig 5A).
Figure 5. Stromal fibromuscular AR controls pro-inflammatory cytokines/chemokines expression.
- Primary cultures of PrSCs from 22 to 24-week-old Pten+/− mouse DLPs were prepared and lentivirus carrying AR siRNA was used to knockdown AR. The AR scramble (ARscr) and ARsiRNA (ARsi) knockdown cells were then treated with EtOH or 10 nM DHT after following by immunoblotting against AR, p-Akt (at Ser 473), total Akt and α-tubulin. The stromal cell pools came from 5 to 6 mice.
- The ARscr or ARsi PrSCs were cultured with 10% CD-FBS medium for 2 days and then stimulated with EtOH or 10 nM DHT for another 1 day. The CM were collected and subjected to a pro-inflammatory cytokine array analysis according to the manufacturer's instructions. The yellow boxes indicate the cytokines that were increased in the Pten+/− PrSCs ARscr + EtOH or Pten+/− PrSCs ARscr + DHT group as compared to Pten+/+ PrSCs ARscr + DHT. The blue boxes indicate the reduction of cytokine level in Pten+/− PrSCs ARsi + DHT as compared to Pten+/− PrSCs ARscr + DHT. The red boxes indicate the elevation of cytokine level in Pten+/− PrSCs ARsi + DHT as compared to Pten+/− PrSCs ARscr + DHT. The primary PrSCs were pooled and collected from 5 to 6 mouse DLPs.
- Dot quantification results were determined using Biorad ChemiDoc™ XRS+ System. Each bar represents the mean ± SD of at least two dependent determinations performed in triplicate.
- Real-time PCR analysis was used to validate the cytokine changes in Pten+/− PrSCs ARscr and Pten+/− PrSCs ARsi in the presence of 10 nM DHT. Each bar represents the mean ± SD of at least two-independent determinations performed in triplicate.
Next, the conditioned media (CM) obtained from four groups of PrSCs isolated from Pten+/− DLPs was prepared: Pten+/+ ARscr+DHT treatment, Pten+/− ARscr + EtOH, Pten+/− ARscr + DHT and Pten+/− ARsi + DHT. The CM from each group was subjected to pro-inflammatory cytokine array analysis (Fig 5B) and we found Pten+/+ PrSCs showed little expression of any cytokines/chemokines. In contrast, Pten+/− PrSCs displayed significant up-regulation of several cytokines/chemokines: such as interferon gamma-induced protein (IP-10); keratinocyte-derived chemokine (KC); thymus and activation regulated chemokine (TARC); tissue inhibitor of metalloproteinase 1 (TIMP-1); monocyte chemotactic protein-5 (MCP-5); macrophage inflammatory protein-1α (MIP-1α); macrophage inflammatory protein-1β (MIP-1β); regulated upon activation, normal T-cell expressed and secreted (RANTES); stromal cell-derived factor-1 (SDF-1); and interleukin-10 (IL-10), compared to Pten+/+ controls (Fig 5B). Interestingly, we found the levels of MIP-1α, MIP1-β, MIP-2 and IL-10 were substantially reduced in Pten+/− ARsi + DHT group compared to Pten+/− ARscr + DHT, which was confirmed by dot-quantification (Fig 5C) and real-time PCR analysis (Fig 5D). The similar result was also seen in the Pten+/− PrSCs isolated from APs (Supporting Information Fig S2).
We then studied the mechanisms by which AR regulates the expression of MIP-1β, which was altered significantly in Pten+/− ARsi PrSCs (Fig 5). First, we surveyed the mouse MIP-1β 5 kb promoter region to identify the potential androgen responsive elements (AREs) by transcriptional element search system (TESS, U of Pennsylvania, Philadelphia, PA). Based on the survey results, we found the potential AREs (half-palindromic motif) mainly located within the 2 kb promoter region. Therefore, we performed the ChIP assay to examine whether AR can directly bind to the MIP-1β promoter region in mouse PrSCs. The partial mouse MIP-1β promoter region and the primer sets used to amplify AR-bound DNA are provided (Supporting Information Fig S3A). The results showed that AR failed to bind to the immunoprecipitated promoter regions of MIP-1β (Supporting Information Fig S3B, upper and middle panels), however, AR can bind to the keratinocyte growth factor promoter (Heitzer & DeFranco, 2006) that served as positive control (Supporting Information Fig S3B, lower panel). These results were further corroborated with mouse MIP-1β promoter luciferase assay. We constructed the mouse MIP-1β promoter (-1,989 to +68) into pGL3-basic vector and determined whether AR can activate the MIP-1β promoter. In Supporting Information Fig S4A, AR itself is not sufficient to turn-on the MIP-1β promoter, however, liganded AR can potentiate the IL-1β induced MIP-1β promoter activation, suggesting AR may cooperate with the IL-1β downstream mediator to activate MIP-1β promoter.
A previous report has demonstrated that NF-kappaB and C/EBPβ play crucial roles to activate chondrocyte (MIP-1α) CCL3 and (MIP-1β) CCL4 expressions after IL-1β stimulation (Zhang et al, 2010). Also, it has been known that NF-kappaB plays a critical role in several cytokines/chemokines regulation such as we identified MIP1-α and MIP-1β. To further dissect the regulatory role of AR-NF-kappaB on MIP-1β promoter, we pretreated with NF-kappaB inhibitor (BAY118082) prior to the IL-1β stimulation, leading to abolishment of promoter activation (In Supporting Information Fig S4A), indicating that NF-kappaB is essential to mediate IL-1β enhanced MIP-1β expression.
Taken together, we found loss of stromal AR leads to decreased MIP-1β expression and it appears that the regulation of AR on MIP-1β is unlikely through direct promoter binding. Instead, the cooperation with NF-kappaB to activate MIP-1β promoter may a play more important role for the AR-mediated regulation. Although it is also possible that AR may bind to the enhancer region of MIP-1β or modulate the co-occupied transcriptional factors to regulate MIP-1β expression, which needs further investigation.
Together, results from Fig 5A–D and Supporting Information Figs S3 and S4 suggested that stromal AR in CAFs was able to regulate pro-inflammatory cytokines/chemokines expression such as MIP-1α, MIP-1β, MIP-2 and IL-10, to affect immune cell recruitment and modulate inflammatory responses in Pten+/− mouse prostate. For the MIP-1β gene regulation, AR may cooperate with NF-KappaB to activate MIP-1β promoter after IL-1β stimulation, instead of directly binding to MIP-1β promoter.
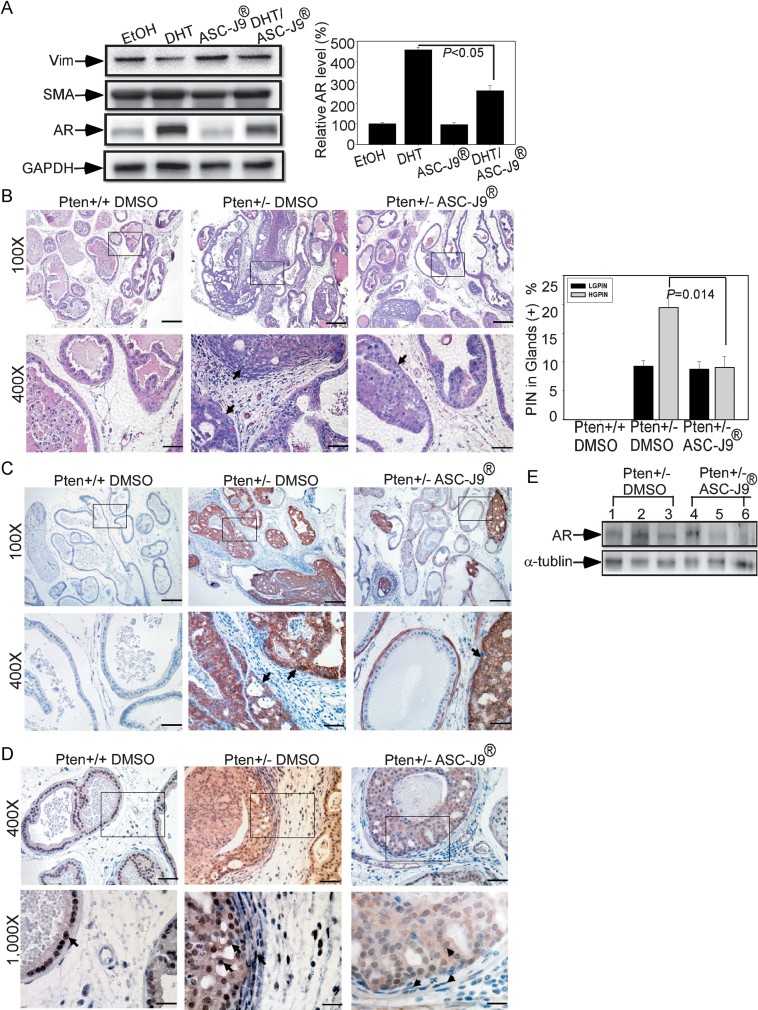
ASC-J9® suppresses PIN lesion development, in part, via stromal AR degradation
To further confirm the findings in Figs 2 and 3 showing that stromal AR can regulate PIN development and the tumour-promoting microenvironment, we used the AR degradation enhancer, ASC-J9®, which was developed to interrupt the interaction of AR and its coregulator ARA55 in stromal cells and ARA70 in luminal epithelial cells. This disruption might then lead to the degradation of AR and suppress AR-mediated cell growth (Lai et al., manuscript submitted). The potential therapeutic effects of ASC-J9® have been demonstrated in vitro and in vivo in several AR related diseases such as bladder cancer, liver cancer and spinal and bulbar muscular atrophy (SBMA) a motor-neuron disease (Miyamoto et al, 2007; Wu et al, 2010; Yang et al, 2007).
First, we used primary cultured of stromal cells from Pten+/− mice and treated with vehicle or ASC-J9® to show AR protein could be degraded (Fig 6A). To examine the in vivo effects of ASC-J9®, we injected DMSO-vehicle or ASC-J9® every other day starting with 6-month-old Pten+/− mice. After 2 months of injection, we harvested the prostate tissues and characterized the histology. The DLPs from ASC-J9® treated Pten+/− mice showed diminished PIN lesion formation, most markedly in HG-PIN as compared to vehicle treated Pten+/− mice (Fig 6B). The LG-/HG-PIN lesion quantification is also provided (Fig 6B, right panel). The PIN lesions were further examined by staining of p-Akt (Ser473) and the results were similar to the H&E staining data (Fig 6C). To ensure ASC-J9® can degrade AR in the Pten+/− mice, we employed AR IHC and prostate tissues WB to confirm ASC-J9® effects (Fig 6D–E). Note that ASC-J9® can also degrade luminal epithelial AR protein, therefore, we were able to observe decreased epithelial AR amounts in the ASC-J9® treated mouse prostate (Fig 6D).
Figure 6. ASC-J9® suppresses PIN lesion development via AR degradation.
- Primary cultures of PrSCs from Pten+/− mice were prepared. The PrSCs were cultured in 10% CD-FBS medium for 2 days and treated with EtOH, 10 nM DHT, 10 µM ASC-J9®, or DHT + ASC-J9® for 24 h. The protein extracts were harvested and subjected to WB analysis using antibodies against Vimentin (Vim), SMA, AR and GAPDH. The stromal cells were pooled from 5 to 6 Pten+/− mice at 22–24 weeks old. The quantification data of AR amounts are shown and normalized with GAPDH loading controls (right panel).
- ASC-J9® displays chemopreventative effects in Pten+/− mouse model. ASC-J9® was administrated to 6-month-old Pten+/− mice and the DLPs were harvested after 2 months treatment. Histological examination of 8-month-old Pten+/+ DMSO, Pten+/− DMSO and Pten+/− ASC-J9® treated mouse DLPs were subjected to H&E staining. The PIN lesions are pointed-out by arrows. Quantification results are shown in the right panel. N = 4–5 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×).
- p-Akt (Ser473) IHC staining in Pten+/+ DMSO, Pten+/− DMSO and Pten+/− ASC-J9® treated mouse DLPs were performed. Arrows indicate p-Akt positive staining in the PIN lesion. N = 4–5 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×).
- DLPs from the three groups of mice were subjected to AR IHC staining. Arrows indicate the AR immunoreactive cells and arrowheads show weaker intensity in ASC-J9® treated group. N = 4–5 mice per group. Scale Bars = 200 µm (100×) and 50 µm (400×).
- The DLPs tissue protein extracts were isolated from the three groups of mice and AR immunoblotting assay was used to determine AR expression. The data are presented from three individual Pten+/− DMSO and Pten+/− ASC-J9® treated mice.
Collectively, we demonstrated that ASC-J9® could reduce PIN lesion development in Pten+/− mice, at least in part, due to the stromal AR degradation.
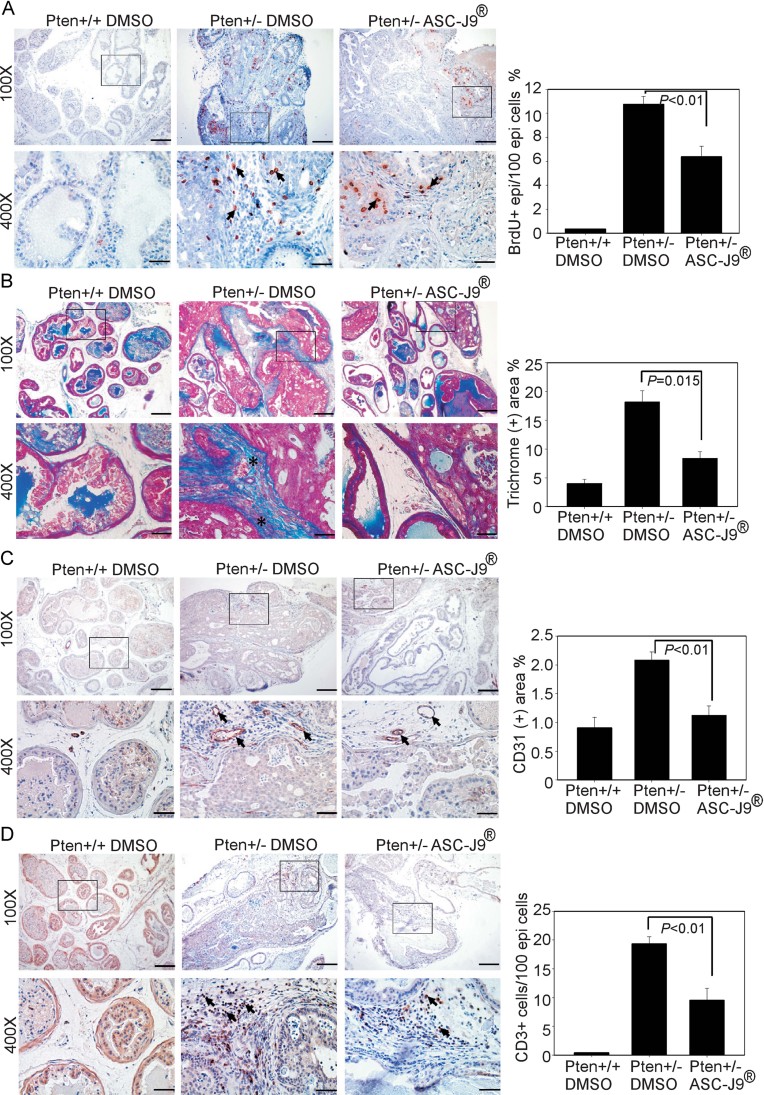
ASC-J9® impedes PIN lesion development and attenuates the tumour microenvironment in Pten+/− mice
We further utilized the BrdU incorporation assay to identify proliferating epithelial cells and the results indicated that Pten+/− mice with ASC-J9® treatment had markedly reduced proliferation signals within the PIN areas (Fig 7A; left panel and quantitation in right panel). Moreover, tumour microenvironmental characterization was conducted using staining with Mason's Trichrome, CD31 IHC and CD3 IHC (Fig 7B–D; left panels and quantitation in right panels) to show ASC-J9® also suppressed those changes.
Figure 7. ASC-J9® impedes PIN lesion development and alleviates tumour-promoting microenvironment in Pten+/− mice.
N = 5–6 mice per group.
- The DLPs from three treated groups of mice were subjected to histological characterization by BrdU staining (left panel) and the quantification results are provided in the right panel.
- Pten+/+ DMSO, Pten+/− DMSO and Pten+/− ASC-J9® treated mouse DLPs were subjected to Masson's Trichrome staining to measure deposited collagen fibers. The blue colors indicate collagen fibers defined by asterisks and quantification results are shown in the right panel.
- CD31 IHC staining. Arrows indicate CD31+ endothelial cells in the stromal compartment and quantification results are shown in the right panel.
- CD3 IHC staining. Arrows indicate CD3+ T-cells and quantification results are shown in the right panel.
Together, the phenotypic characterization results from Fig 6B–C and Fig 7A–D are consistent with data from mice lacking stromal fibromuscular AR (Figs 2 and 3) and demonstrated that injection of ASC-J9® into Pten+/− mice could effectively suppress PIN development with attenuation of the tumour microenvironment remodelling partially through stromal AR degradation.
DISCUSSION
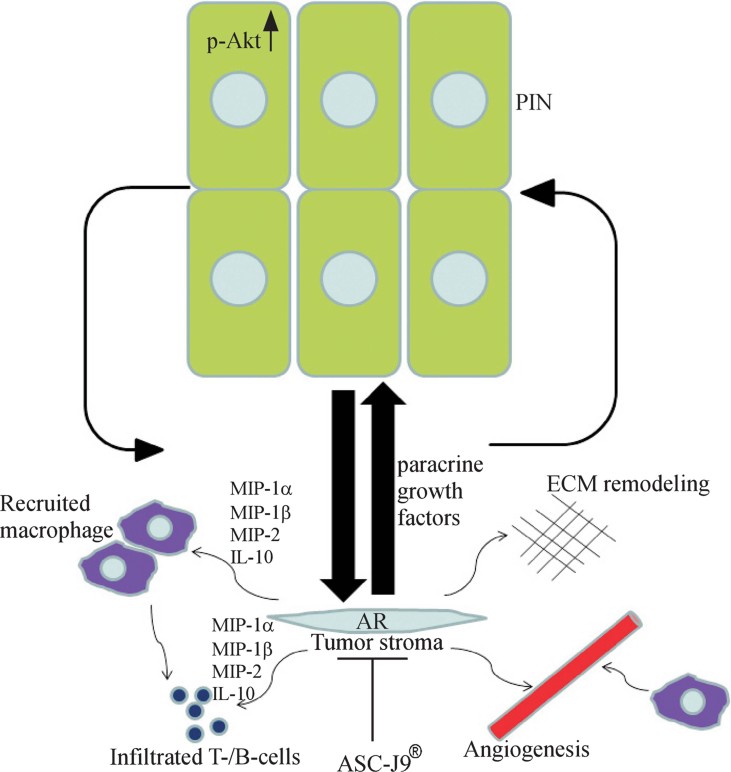
Reciprocal signalling between tumour cells and adjacent stromal cells plays pivotal roles in orchestrating the oncogenic epithelial cellular and molecular mechanisms. The cross-talk between tumours and various stromal cells in the PCa are still not fully understood. We developed the stromal fibromuscular ARKO mice to examine PCa initiation in Pten+/− mice. Our experimental results with these compound mutant mice highlight the crucial roles of stromal fibromuscular AR on the regulation of adjacent epithelial lesion development through a paracrine manner and re-organization of a favorable microenvironment. In this study, we also observed a reduction in collagen deposition, neovasculature formation and immune cells infiltration in this dARKO/Pten+/− mouse as the features of tumour-promoting microenvironments (Fig 8). Although we still did not have the direct evidence to support that those microenvironmental changes are exclusively due to the stromal AR deletion, it is likely that these changes are attributed to the intermixing effects of loss of stromal AR and reduction of PIN lesion in dARKO/Pten+/− mice. The oncogenic epithelium within the PIN lesion was also able to secrete growth factors and cytokines/chemokines to create a more favorable microenvironment including the ECM remodelling, angiogenesis and immune cell infiltration.
Figure 8. Stromal fibromuscular AR regulates PIN lesion through secretion of paracrine factors and alteration of surrounding microenvironments.
A proposed model for the roles of CAFs AR to mediate tumour-promoting microenvironment and cross-talk between different cell types in the PIN areas of Pten+/− mice, illustrating the functional roles of AR in the ECM remodelling, angiogenesis and tumour-promoting inflammatory response.
Emerging evidence of risk factors such as infectious agents and environmental factors have been proposed to precede the development of PIN lesions (De Marzo et al, 1999; De Marzo et al, 2007). Epidemiological studies also suggested that chronic inflammation and/or recurrent infection might contribute to prostate carcinogenesis (Grivennikov et al, 2010; Karin & Greten, 2005; Karin et al, 2006). Proliferative inflammatory atrophy (PIA) lesions of the glandular epithelial foci could be a connection between prostatitis and PIN or PCa (De Marzo et al, 2007; Palapattu et al, 2005). The inflammatory lesions in the aging prostate are frequently associated with atrophic epithelium and some fractions of epithelium undergo active proliferation, which may develop into PIN or PCa. In the molecular aspects, several genetic alteration such as glutathione S-transferase pi 1 (GSTP1), NKX3.1, p27 and PTEN have been regarded as the markers of PIN and PCa (Wagenlehner et al, 2007). Collectively, this epidemiological and genetic evidence might suggest a causative role of inflammation in the complicated process of prostate carcinogenesis, implicating the important contribution of immune cells in the prostate pathogenesis.
Regarding the functions of tumour associated stromal cells, tumour associated fibroblasts (TAFs) are distinguishable from normal fibroblasts and a subset of TAFs has been characterized as myofibroblasts based on the expression of smooth muscle α-actin (SMAα; Santos et al, 2009). TAFs in skin were demonstrated to be able to produce pro-inflammatory cytokines to foster epithelium growth, but the functions of TAFs in PCa are unclear (Erez et al, 2010). In addition to TAFs, B-cells residing in the skin were able to ‘educate’ normal fibroblasts to evolve into TAFs, which can produce various pro-inflammatory cytokines in order to evoke tumour initiation (Erez et al, 2010). Furthermore, the sensitivity to castration in PCa can be modulated through infiltrated B-cells derived lymphotoxin-epithelium engagement in the transgenic adenocarcinoma of the mouse prostate (TRAMP) mice (Ammirante et al, 2010). Overall, inflammatory responses from either infiltrated immune cells or TAFs may contribute, in part, to the PCa development. In this report, we demonstrated that AR in CAFs could modulate cytokines/chemokines production to affect the immune cells recruitment. Although we have not identified whether T-cells or B-cells are more important in mediating this tumour-promoting inflammatory response in Pten+/− mice, further studies by crossing T-cell or B-cell deficient mice with Pten+/− mice may provide direct answers to address this question.
As noted, tissue recombination experiments conducted in immunodeficient mice, which lack functional T- and B-cell mediated immune responses. The elicited T-/B-cells inflammation has been associated with the tumour progression through pro-inflammatory cytokine production and recruitment of macrophages (Balkwill et al, 2005; Coussens & Werb, 2002; Karin et al, 2006). Furthermore, subrenal capsule implementation of tissue recombinants provide enriched nutrition and ample oxygen supply for recombinants growth, however, this does not mimic the real in vivo prostate microenvironment. The ECM composition, basement membrane components and matrix/metalloproteinase factors are distinct between renal capsules and prostate. Therefore, by generating conditional stromal fibromuscular ARKO mice with the cre-loxP system, we can breed with other transgenic/KO mice such as TRAMP, Nkx3.1 KO, p53 KO and c-Myc transgenic mice to further understand stromal AR roles in vivo with intact immune systems.
Interestingly, a previous report has suggested that human prostate tumour samples with higher mesenchymal stem cells (MSCs) marker CD90 expression might contain the tumour-promoting potentials of CAFs (Zhao & Peehl, 2009). To characterize the MSCs population in the Pten+/− PrSCs and explore the potential AR regulation, we performed QPCR analysis to examine MSC markers (CD29, CD44 and CD90). The results showed that PrSCs isolated from Pten+/− mice expressed these three MSC markers, with higher expression in CD90 (Supporting Information Fig S5D). By using genetic knockout (WT vs. ARKO bone marrow-MSCs, BM-MSCs) or AR siRNA knockdown approach in Pten+/− PrSCs to disrupt AR expression (Supporting Information Fig S5A), we did not see ablation of AR could reverse these MSC marker expressions (Supporting Information Fig S5B–D). However, we could observe that loss of AR in BM-MSCs could enhance self-renewal by CFU-F assay (Supporting Information Fig S5E). Therefore, we reasoned that knockdown of stromal AR might increase MSCs population, which has the potential to promote PCa development, however, this may not happen in the dARKO-Pten+/− mice because dARKO-Pten+/− mice showed reduced PIN lesion.
Finally, the AR degradation enhancer, ASC-J9®, has been extensively examined in several types of cells such as motor neuronal cells, bladder cancer cells, hepatocarcinoma cells and macrophages in wound tissues (Lai et al, 2009; Ma et al, 2008; Miyamoto et al, 2007; Yang et al, 2007). The results demonstrated that ASC-J9® was able to degrade AR in those various cells to achieve therapeutic effects. Here, we evaluated the effects of ASC-J9® in Pten+/− mice and demonstrated ASC-J9® can reduce PIN development partially through stromal AR degradation. Taken together, our study not only elucidates the roles of stromal fibromuscular AR in prostate tumourigenesis via characterization of dARKO-Pten+/− mice, but also provides an alternative therapeutic candidate using implementation of ASC-J9® for early PCa intervention.
MATERIALS AND METHODS
Mice, cells and reagents
The floxed AR mice were generated by insertion of loxP sites flanking the exon-2 region of the AR gene in C57BL/6 background (Yeh et al, 2002). The FSP1-cre mice in C57BL/6 background were kindly provided by Dr. NA Bhowmick (Bhowmick et al, 2004). The transgelin cre (Tgln-cre) mice in C57BL/6/SJL background were purchased from Jackson Laboratory (Bar Harbor, ME). The stromal double cre mice were generated by mating male FSP1-cre mice with female Tgln-cre mice and backcrossed to a C57BL/6 background for more than 5–6 generations (Lai et al, 2012). Pten+/− mice were obtained from NCI (Bethesda, MD) in a B6/129 background. Rag2 KO mice were purchased from Taconic (Germantown, NY). Animal procedures were conducted in accordance with the protocols approved by the University of Rochester Committee on Animal Resources.
The primary cultured prostate stromal cells were prepared by cutting the prostates into small pieces (1 mm3) and further digested into single cells by using 1% collagenase (Roche). The primary cultured PrSCs were grown in DMEM/F12 (1:1) with 10% FBS, 1% penicillin/streptomycin, 1% l-glutamine and 1% insulin–transferrin–selenium (ITS; Gibco) and the mixed populations were collected for characterization.
ASC-J9® (5-hydroxy-1,7-bis(3,4-dimethoxyphenyl)-1,4,6-heptatrien-3-one) was a gift from AndroScience (San-Diego, CA) and was generated as described previously (Wu et al, 2010; Yang et al, 2007). ASC-J9® (dissolved in DMSO and diluted with corn oil) was i.p. injected into mice at a dose of 75 mg/kg every other day until the end of each study. Control mice received DMSO in corn oil only.
Histological and immunohistochemical analysis
Four percent of paraformaldehyde fixed prostates from individual genotypes of mice were subjected to paraffin embedding and sectioning (5 µm). To determine the phenotypic characterization of dARKO/Pten+/− mice, tissue sections were sequentially stained with H&E and IHC for characterization. For the BrdU incorporation assay, the BrdU injection protocol was described previously (Wu et al, 2007) and BrdU immunostaining was performed following the manufacturer's instructions (Invitrogen). The Masson's Trichrome staining kit was purchased from Sigma–Aldrich and used according to the manufacturer's instructions. For IHC staining, the antibodies against AR (C-19, Santa Cruz Biotechnology), PTEN (138G6, Cell Signaling), p-Akt at Ser473 (D9E, Cell Signaling), p-S6RP at Ser235/236 (91B2, Cell Signaling), vimentin (LN-6, Sigma–Aldrich), SMA (1A4, Sigma–aldrich), CD3 (Sigma–Aldrich), F4/80 (A3-1, Abcam) and anti-CD31 (Abcam) were used.
The paper explained
PROBLEM:
The interaction of epithelium and stroma plays a crucial role to determine the rodent and human prostate development. Although the tissue recombination has demonstrated that mesenchymal/stromal AR is indispensable for the rodent prostate organogenesis, the stromal AR function in the prostate cancer (PCa) development is still unclear especially under the real physiological condition such as in immune intact mice compared to tissue recombinants implanted into SCID mice. Here, we elucidated the importance of stromal AR in prostate tumourigenesis in PTEN deficient mice and dissected the mechanisms of cross-talk between stromal AR and adjacent oncogenic epithelium for prostatic intraepithelial neoplasia (PIN) development.
RESULTS:
Using a cre-loxP based conditional knockout system, we established a compound mutant mouse model, which has deleted AR in fibroblasts and smooth muscle cells with PTEN haploinsufficiency. By characterizing the phenotypes, we described that stromal AR is essential to control the epithelium proliferation and is able to modulate the surrounding tumour-promoting microenvironments. Those tumour-promoting microenvironmental features include the immune cell infiltration, angiogenesis and extracellular matrix (ECM) remodelling, which may contribute to the promotion of tumour initiation in Pten+/− mice. The data may only reflect PIN observed in the peripheral zone of human prostate.
IMPACT:
We have highlighted the critical role of stromal AR in the prostate tumourigenesis in mice with PTEN deletion, which frequently occurs in the human PCa patients. These valuable preclinical findings might not only advance our knowledge of the pathophysiological role of stromal AR, but also help us to develop a new therapeutic agent such as we used here, AR degradation enhancer, ASC-J9®. The successful clinical trials of this compound would be beneficial for patients who suffer from early stage PCa.
Serum testosterone detection
Mice of the indicated genotypes were killed at 9 months old, blood was drawn by cardiocenthesis and immediately assayed for serum testosterone concentration by an EIA kit following the manufacturer's instructions (Diagnostic Systems Laboratories).
Genotyping, RNA extraction, RT-PCR and real-time quantitative PCR analysis
Genomic DNA from mouse tails was purified by phenol/chloroform extraction and used as templates for PCR reactions to detect transgenes. Total RNA was prepared from cells with Trizol (Invitrogen) according to the manufacturer's instructions. cDNA synthesis was carried out by reverse transcriptase PCR (RT-PCR) with Superscript RNase H-reverse transcriptase (Invitrogen). Expression levels of AR, MIP-1α, MIP-1β, MIP-2 and IL-10 were determined by quantitative real-time PCR using iCycler real-time PCR amplifier (Bio-Rad Laboratories). The relative copy numbers of GAPDH were quantified and used for normalization. The ΔΔCT method was used to calculate relative differential expression between control and experimental groups. The primer sequences for QPCR are provided in the Supporting Information Table.
Pro-inflammatory cytokine array analysis
Primary cultures of prostate stromal cells from Pten+/− mouse prostates were prepared and lentivirus carrying ARscr or ARsiRNA was used as control or to knockdown AR, respectively. The CM from each treated group was collected and subjected to cytokines analysis. The proinflammtory cytokine array was obtained from R&D systems and performed according to the manufacturer's instructions.
Statistics
The data are presented as mean ± SEM. The student t-test was employed to compare two groups and one way ANOVA was used to compare more than two groups. p-Values of *p < 0.05; **p < 0.01; and ***p < 0.001 were considered statistically significant.
For more detailed Materials and Methods see the Supporting Information.
Acknowledgments
We thank Karen Wolf (George H. Whipple Lab, University of Rochester Medical Center, Rochester, NY, USA) for assistance in manuscript preparation and Spencer Vitkus (Department of Urology, University of Rochester Medical Center, NY, USA) for the insightful suggestions. This work was supported by NIH grants (CA127300, CA122840 and CA156700), George H. Whipple Professorship Endowment and Taiwan Department of Health Clinical Trial, Research Center of Excellence (DOH99-TD-B-111-004 to China Medical University, Taichung, Taiwan).
Supporting Information is available at EMBO Molecular Medicine online.
Conflict of interest statement: ASC-J9® was patented by the University of Rochester, the University of North Carolina, and AndroScience Corp., and then licensed to AndroScience Corp. Both the University of Rochester and C. Chang own royalties and equity in AndroScience Corp. The other authors declare that they have no conflict of interest.
Author contributions
KPL, SYa, SYe and CC designed the experiments; KPL, SYa and CKH performed the experiments; KPL and SYa analysed the data; KPL, SYe and CC wrote the paper.
Supplementaary material
Detailed facts of importance to specialist readers are published as ”Supporting Information”. Such documents are peer-reviewed, but not copy-edited or typeset. They are made available as submitted by the authors.
References
- Abate-Shen C, Banach-Petrosky WA, Sun X, Economides KD, Desai N, Gregg JP, Borowsky AD, Cardiff RD, Shen MM. Nkx3.1; Pten mutant mice develop invasive prostate adenocarcinoma and lymph node metastases. Cancer Res. 2003;63:3886–3890. [PubMed] [Google Scholar]
- Ammirante M, Luo JL, Grivennikov S, Nedospasov S, Karin M. B-cell-derived lymphotoxin promotes castration-resistant prostate cancer. Nature. 2010;464:302–305. doi: 10.1038/nature08782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backman SA, Ghazarian D, So K, Sanchez O, Wagner KU, Hennighausen L, Suzuki A, Tsao MS, Chapman WB, Stambolic V, et al. Early onset of neoplasia in the prostate and skin of mice with tissue-specific deletion of Pten. Proc Natl Acad Sci USA. 2004;101:1725–1730. doi: 10.1073/pnas.0308217100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balkwill F, Charles KA, Mantovani A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell. 2005;7:211–217. doi: 10.1016/j.ccr.2005.02.013. [DOI] [PubMed] [Google Scholar]
- Bhowmick NA, Chytil A, Plieth D, Gorska AE, Dumont N, Shappell S, Washington MK, Neilson EG, Moses HL. TGF-beta signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science. 2004;303:848–851. doi: 10.1126/science.1090922. [DOI] [PubMed] [Google Scholar]
- Bose S, Wang SI, Terry MB, Hibshoosh H, Parsons R. Allelic loss of chromosome 10q23 is associated with tumor progression in breast carcinomas. Oncogene. 1998;17:123–127. doi: 10.1038/sj.onc.1201940. [DOI] [PubMed] [Google Scholar]
- Chen ML, Xu PZ, Peng XD, Chen WS, Guzman G, Yang X, Di Cristofano A, Pandolfi PP, Hay N. The deficiency of Akt1 is sufficient to suppress tumor development in Pten+/− mice. Genes Dev. 2006;20:1569–1574. doi: 10.1101/gad.1395006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cully M, You H, Levine AJ, Mak TW. Beyond PTEN mutations: the PI3K pathway as an integrator of multiple inputs during tumorigenesis. Nat Rev Cancer. 2006;6:184–192. doi: 10.1038/nrc1819. [DOI] [PubMed] [Google Scholar]
- Cunha GR, Hayward SW, Wang YZ. Role of stroma in carcinogenesis of the prostate. Differentiation. 2002;70:473–485. doi: 10.1046/j.1432-0436.2002.700902.x. [DOI] [PubMed] [Google Scholar]
- Cunha GR, Hayward SW, Wang YZ, Ricke WA. Role of the stromal microenvironment in carcinogenesis of the prostate. Int J Cancer. 2003;107:1–10. doi: 10.1002/ijc.11335. [DOI] [PubMed] [Google Scholar]
- Cunha GR, Ricke W, Thomson A, Marker PC, Risbridger G, Hayward SW, Wang YZ, Donjacour AA, Kurita T. Hormonal, cellular, and molecular regulation of normal and neoplastic prostatic development. J Steroid Biochem Mol Biol. 2004;92:221–236. doi: 10.1016/j.jsbmb.2004.10.017. [DOI] [PubMed] [Google Scholar]
- Dahia PL. PTEN, a unique tumor suppressor gene. Endocr Relat Cancer. 2000;7:115–129. doi: 10.1677/erc.0.0070115. [DOI] [PubMed] [Google Scholar]
- De Marzo AM, Marchi VL, Epstein JI, Nelson WG. Proliferative inflammatory atrophy of the prostate: implications for prostatic carcinogenesis. Am J Pathol. 1999;155:1985–1992. doi: 10.1016/S0002-9440(10)65517-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Marzo AM, Nakai Y, Nelson WG. Inflammation, atrophy, and prostate carcinogenesis. Urol Oncol. 2007;25:398–400. doi: 10.1016/j.urolonc.2007.05.007. [DOI] [PubMed] [Google Scholar]
- de Visser KE, Eichten A, Coussens LM. Paradoxical roles of the immune system during cancer development. Nat Rev Cancer. 2006;6:24–37. doi: 10.1038/nrc1782. [DOI] [PubMed] [Google Scholar]
- Di Cristofano A, De Acetis M, Koff A, Cordon-Cardo C, Pandolfi PP. Pten and p27KIP1 cooperate in prostate cancer tumor suppression in the mouse. Nat Genet. 2001;27:222–224. doi: 10.1038/84879. [DOI] [PubMed] [Google Scholar]
- Erez N, Truitt M, Olson P, Hanahan D. Cancer-associated fibroblasts are activated in incipient neoplasia to orchestrate tumor-promoting inflammation in an NF-kappaB-dependent manner. Cancer Cell. 2010;17:135–147. doi: 10.1016/j.ccr.2009.12.041. [DOI] [PubMed] [Google Scholar]
- Goberdhan DC, Wilson C. PTEN: tumour suppressor, multifunctional growth regulator and more. Hum Mol Genet. 2003;12:R239–248. doi: 10.1093/hmg/ddg288. Spec No 2. [DOI] [PubMed] [Google Scholar]
- Gray IC, Stewart LM, Phillips SM, Hamilton JA, Gray NE, Watson GJ, Spurr NK, Snary D. Mutation and expression analysis of the putative prostate tumour-suppressor gene PTEN. Br J Cancer. 1998;78:1296–1300. doi: 10.1038/bjc.1998.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward SW, Wang Y, Cao M, Hom YK, Zhang B, Grossfeld GD, Sudilovsky D, Cunha GR. Malignant transformation in a nontumorigenic human prostatic epithelial cell line. Cancer Res. 2001;61:8135–8142. [PubMed] [Google Scholar]
- Heitzer MD, DeFranco DB. Hic-5/ARA55, a LIM domain-containing nuclear receptor coactivator expressed in prostate stromal cells. Cancer Res. 2006;66:7326–7333. doi: 10.1158/0008-5472.CAN-05-2379. [DOI] [PubMed] [Google Scholar]
- Karin M, Greten FR. NF-kappaB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005;5:749–759. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- Karin M, Lawrence T, Nizet V. Innate immunity gone awry: linking microbial infections to chronic inflammation and cancer. Cell. 2006;124:823–835. doi: 10.1016/j.cell.2006.02.016. [DOI] [PubMed] [Google Scholar]
- Kim MJ, Cardiff RD, Desai N, Banach-Petrosky WA, Parsons R, Shen MM, Abate-Shen C. Cooperativity of Nkx3.1 and Pten loss of function in a mouse model of prostate carcinogenesis. Proc Natl Acad Sci USA. 2002;99:2884–2889. doi: 10.1073/pnas.042688999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korsten H, Ziel-van der Made A, Ma X, van der Kwast T, Trapman J. Accumulating progenitor cells in the luminal epithelial cell layer are candidate tumor initiating cells in a Pten knockout mouse prostate cancer model. PLoS ONE. 2009;4:e5662. doi: 10.1371/journal.pone.0005662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai JJ, Lai KP, Chuang KH, Chang P, Yu IC, Lin WJ, Chang C. Monocyte/macrophage androgen receptor suppresses cutaneous wound healing in mice by enhancing local TNF-alpha expression. J Clin Invest. 2009;119:3739–3751. doi: 10.1172/JCI39335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai KP, Yamashita S, Vitkus S, Shyr CR, Yeh S, Chang C. Suppressed prostate epithelial development with impaired branching morphogenesis in mice lacking stromal fibromuscular androgen receptor. Mol Endocrinol. 2012;26:52–66. doi: 10.1210/me.2011-1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Miano JM, Mercer B, Olson EN. Expression of the SM22alpha promoter in transgenic mice provides evidence for distinct transcriptional regulatory programs in vascular and visceral smooth muscle cells. J Cell Biol. 1996;132:849–859. doi: 10.1083/jcb.132.5.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Yen C, Liaw D, Podsypanina K, Bose S, Wang SI, Puc J, Miliaresis C, Rodgers L, McCombie R, et al. PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer. Science. 1997;275:1943–1947. doi: 10.1126/science.275.5308.1943. [DOI] [PubMed] [Google Scholar]
- Ma WL, Hsu CL, Wu MH, Wu CT, Wu CC, Lai JJ, Jou YS, Chen CW, Yeh S, Chang C. Androgen receptor is a new potential therapeutic target for the treatment of hepatocellular carcinoma. Gastroenterology. 2008;135:947–955. doi: 10.1053/j.gastro.2008.05.046. 955. e941-e945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maehama T, Dixon JE. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J Biol Chem. 1998;273:13375–13378. doi: 10.1074/jbc.273.22.13375. [DOI] [PubMed] [Google Scholar]
- Miyamoto H, Yang Z, Chen YT, Ishiguro H, Uemura H, Kubota Y, Nagashima Y, Chang YJ, Hu YC, Tsai MY, et al. Promotion of bladder cancer development and progression by androgen receptor signals. J Natl Cancer Inst. 2007;99:558–568. doi: 10.1093/jnci/djk113. [DOI] [PubMed] [Google Scholar]
- Myers MP, Stolarov JP, Eng C, Li J, Wang SI, Wigler MH, Parsons R, Tonks NK. P-TEN, the tumor suppressor from human chromosome 10q23, is a dual-specificity phosphatase. Proc Natl Acad Sci USA. 1997;94:9052–9057. doi: 10.1073/pnas.94.17.9052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu Y, Altuwaijri S, Lai KP, Wu CT, Ricke WA, Messing EM, Yao J, Yeh S, Chang C. Androgen receptor is a tumor suppressor and proliferator in prostate cancer. Proc Natl Acad Sci USA. 2008a;105:12182–12187. doi: 10.1073/pnas.0804700105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu Y, Altuwaijri S, Yeh S, Lai KP, Yu S, Chuang KH, Huang SP, Lardy H, Chang C. Targeting the stromal androgen receptor in primary prostate tumors at earlier stages. Proc Natl Acad Sci USA. 2008b;105:12188–12193. doi: 10.1073/pnas.0804701105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu Y, Chang TM, Yeh S, Ma WL, Wang YZ, Chang C. Differential androgen receptor signals in different cells explain why androgen-deprivation therapy of prostate cancer fails. Oncogene. 2010;29:3593–3604. doi: 10.1038/onc.2010.121. [DOI] [PubMed] [Google Scholar]
- Palapattu GS, Sutcliffe S, Bastian PJ, Platz EA, De Marzo AM, Isaacs WB, Nelson WG. Prostate carcinogenesis and inflammation: emerging insights. Carcinogenesis. 2005;26:1170–1181. doi: 10.1093/carcin/bgh317. [DOI] [PubMed] [Google Scholar]
- Park JH, Walls JE, Galvez JJ, Kim M, Abate-Shen C, Shen MM, Cardiff RD. Prostatic intraepithelial neoplasia in genetically engineered mice. Am J Pathol. 2002;161:727–735. doi: 10.1016/S0002-9440(10)64228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsypanina K, Ellenson LH, Nemes A, Gu J, Tamura M, Yamada KM, Cordon-Cardo C, Catoretti G, Fisher PE, Parsons R. Mutation of Pten/Mmac1 in mice causes neoplasia in multiple organ systems. Proc Natl Acad Sci USA. 1999;96:1563–1568. doi: 10.1073/pnas.96.4.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putzi MJ, De Marzo AM. Morphologic transitions between proliferative inflammatory atrophy and high-grade prostatic intraepithelial neoplasia. Urology. 2000;56:828–832. doi: 10.1016/s0090-4295(00)00776-7. [DOI] [PubMed] [Google Scholar]
- Ricke WA, Ishii K, Ricke EA, Simko J, Wang Y, Hayward SW, Cunha GR. Steroid hormones stimulate human prostate cancer progression and metastasis. Int J Cancer. 2006;118:2123–2131. doi: 10.1002/ijc.21614. [DOI] [PubMed] [Google Scholar]
- Roseman DS, Ansell JS, Chapman WH. Sexually transmitted diseases and carcinogenesis. Urol Clin North Am. 1984;11:27–43. [PubMed] [Google Scholar]
- Santos AM, Jung J, Aziz N, Kissil JL, Pure E. Targeting fibroblast activation protein inhibits tumor stromagenesis and growth in mice. J Clin Invest. 2009;119:3613–3625. doi: 10.1172/JCI38988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinkai Y, Rathbun G, Lam KP, Oltz EM, Stewart V, Mendelsohn M, Charron J, Datta M, Young F, Stall AM, et al. RAG-2-deficient mice lack mature lymphocytes owing to inability to initiate V(D)J rearrangement. Cell. 1992;68:855–867. doi: 10.1016/0092-8674(92)90029-c. [DOI] [PubMed] [Google Scholar]
- Suzuki A, de la Pompa JL, Stambolic V, Elia AJ, Sasaki T, del Barco Barrantes I, Ho A, Wakeham A, Itie A, Khoo W, et al. High cancer susceptibility and embryonic lethality associated with mutation of the PTEN tumor suppressor gene in mice. Curr Biol. 1998;8:1169–1178. doi: 10.1016/s0960-9822(07)00488-5. [DOI] [PubMed] [Google Scholar]
- Trimboli AJ, Cantemir-Stone CZ, Li F, Wallace JA, Merchant A, Creasap N, Thompson JC, Caserta E, Wang H, Chong JL, et al. Pten in stromal fibroblasts suppresses mammary epithelial tumours. Nature. 2009;461:1084–1091. doi: 10.1038/nature08486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotman LC, Niki M, Dotan ZA, Koutcher JA, Di Cristofano A, Xiao A, Khoo AS, Roy-Burman P, Greenberg NM, Van Dyke T, et al. Pten dose dictates cancer progression in the prostate. PLoS Biol. 2003;1:E59. doi: 10.1371/journal.pbio.0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotman LC, Alimonti A, Scaglioni PP, Koutcher JA, Cordon-Cardo C, Pandolfi PP. Identification of a tumour suppressor network opposing nuclear Akt function. Nature. 2006;441:523–527. doi: 10.1038/nature04809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenlehner FM, Elkahwaji JE, Algaba F, Bjerklund-Johansen T, Naber KG, Hartung R, Weidner W. The role of inflammation and infection in the pathogenesis of prostate carcinoma. BJU Int. 2007;100:733–737. doi: 10.1111/j.1464-410X.2007.07091.x. [DOI] [PubMed] [Google Scholar]
- Wang S, Gao J, Lei Q, Rozengurt N, Pritchard C, Jiao J, Thomas GV, Li G, Roy-Burman P, Nelson PS, et al. Prostate-specific deletion of the murine Pten tumor suppressor gene leads to metastatic prostate cancer. Cancer Cell. 2003;4:209–221. doi: 10.1016/s1535-6108(03)00215-0. [DOI] [PubMed] [Google Scholar]
- Wang S, Garcia AJ, Wu M, Lawson DA, Witte ON, Wu H. Pten deletion leads to the expansion of a prostatic stem/progenitor cell subpopulation and tumor initiation. Proc Natl Acad Sci USA. 2006;103:1480–1485. doi: 10.1073/pnas.0510652103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber MM, Trakul N, Thraves PS, Bello-DeOcampo D, Chu WW, Storto PD, Huard TK, Rhim JS, Williams DE. A human prostatic stromal myofibroblast cell line WPMY-1: a model for stromal–epithelial interactions in prostatic neoplasia. Carcinogenesis. 1999;20:1185–1192. doi: 10.1093/carcin/20.7.1185. [DOI] [PubMed] [Google Scholar]
- Whang YE, Wu X, Suzuki H, Reiter RE, Tran C, Vessella RL, Said JW, Isaacs WB, Sawyers CL. Inactivation of the tumor suppressor PTEN/MMAC1 in advanced human prostate cancer through loss of expression. Proc Natl Acad Sci USA. 1998;95:5246–5250. doi: 10.1073/pnas.95.9.5246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu CT, Altuwaijri S, Ricke WA, Huang SP, Yeh S, Zhang C, Niu Y, Tsai MY, Chang C. Increased prostate cell proliferation and loss of cell differentiation in mice lacking prostate epithelial androgen receptor. Proc Natl Acad Sci USA. 2007;104:12679–12684. doi: 10.1073/pnas.0704940104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu MH, Ma WL, Hsu CL, Chen YL, Ou JH, Ryan CK, Hung YC, Yeh S, Chang C. Androgen receptor promotes hepatitis B virus-induced hepatocarcinogenesis through modulation of hepatitis B virus RNA transcription. Sci Transl Med. 2010;2:32ra35. doi: 10.1126/scitranslmed.3001143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z, Chang YJ, Yu IC, Yeh S, Wu CC, Miyamoto H, Merry DE, Sobue G, Chen LM, Chang SS, et al. ASC-J9 ameliorates spinal and bulbar muscular atrophy phenotype via degradation of androgen receptor. Nat Med. 2007;13:348–353. doi: 10.1038/nm1547. [DOI] [PubMed] [Google Scholar]
- Yeh S, Tsai MY, Xu Q, Mu XM, Lardy H, Huang KE, Lin H, Yeh SD, Altuwaijri S, Zhou X, et al. Generation and characterization of androgen receptor knockout (ARKO) mice: an in vivo model for the study of androgen functions in selective tissues. Proc Natl Acad Sci USA. 2002;99:13498–13503. doi: 10.1073/pnas.212474399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Bryan JL, DeLassus E, Chang LW, Liao W, Sandell LJ. CCAAT/Enhancer-binding protein {beta} and NF-{kappa}B mediate high level expression of chemokine genes CCL3 and CCL4 by human chondrocytes in response to IL-1{beta} J Biol Chem. 2010;285:33092–33103. doi: 10.1074/jbc.M110.130377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H, Peehl DM. Tumor-promoting phenotype of CD90hi prostate cancer-associated fibroblasts. Prostate. 2009;69:991–1000. doi: 10.1002/pros.20946. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.