Abstract
Background
In Malawi, as in other sub-Saharan African countries, nurses manage patients of all ages on antiretroviral treatment (ART). Nurse management of children is rarely studied. We compare ART prescribing between nurses and clinical officers during routine clinic visits at an urban, public clinic to inform policy in paediatric ART management.
Methods
Caregivers of children on first-line ART provided information about visit dates, pill counts, ART dosage and formulation to a nurse and, subsequently, to a clinical officer. Nurses and clinical officers independently calculated adherence, dosage based on body weight, and set next appointment date. Clinical officers, but not nurses, accessed an electronic data system that made the calculations for them based on information from prior visits, actual and expected pill consumption, and standard drug supplies. Nurses calculated with pen and paper. For numerical variables, Bland-Altman graphs plot differences of each nurse–clinical officer pair against the mean, show the 95% limits of agreement (LoA), and also show the mean difference across all reviews. Kappa statistics assess agreement for categorical variables.
Results
A total of 704 matched nurse–clinical officer reviews of 367 children attending the ART clinics between March and July 2010 were analyzed. Eight nurses and 18 clinical officers were involved; two nurses and five clinical officers managed 100 visits or more. Overall, there was a good agreement between the two cadres. Differences between nurses and clinical officers were within narrow LoA and mean differences showed little deviation from zero, indicating little skewing towards one cadre. LoA of adherence and morning and evening ART dosages varied from −24% to 24%, −0.4 to 0.4 and −0.41 to 0.40 tablets, respectively, with mean differences (95% CI) of 0.003 (−0.9, 0.91), −0.005 (−0.02, 0.01) and −0.009 (−0.02, 0.01). Next appointment calculations differed more between cadres with LoA from −40 to 42 days [mean difference: 0.96 days (95% CI:−0.6 to 2.5)], but agreement in the ART formulation prescribed was very good (kappa 0.93).
Conclusions
Nurses’ ART prescribing practices and calculations of adherence and next appointments are similar to clinical officers, although clinical officers used an electronic system. Our findings support the decision of Malawi's health officials to utilize nurses to manage paediatric ART patients.
Keywords: antiretroviral therapy, child, HIV, task shifting, nurse, adherence, medication safety, Malawi, sub-Saharan Africa
Background
Consistent adherence to dosing guidelines by health providers and patients is essential to reduce the likelihood of treatment failure from under dosing or drug toxicity from overdosing. Choosing the correct dosage is more challenging in children as it depends on close monitoring of growth through accurate height and weight. Despite the recognized need for additional caution with paediatric patients, errors during prescription, dispensing, administration and documentation of treatments are common [1–6]. Although several interventions to reduce errors show promise, including the use of electronic systems [7–10], in countries with few resources, treatment errors are a particular concern [11].
In the context of antiretroviral treatment (ART), correct dosing for children is critical as HIV drug resistance and treatment failure develop rapidly with poor adherence to treatment guidelines [12]. In response, non-government organizations [13–15], national programmes [16] and WHO [17,18] developed paediatric weight band-based dosing tools for different paediatric ART formulations to improve adherence of providers and patients. Several studies found these tools to be effective: simplification of paediatric ART by using fixed dose combination (FDC) tablets instead of syrups [19], reducing the number of pills per day [20] or modifying the ART initiation recommendations [21] help reduce dosing errors.
However, there are additional obstacles to correct ART dosing for children with HIV in low-resource settings where facilities with dedicated staff or capacity to care specifically for children may be limited or absent, and the demand for care is high. First, to increase access to ART, WHO promotes task shifting where non-specialist cadres take on responsibilities in the ART management [22]. Though nurse-led HIV care in Africa is common [22] and successful efforts in nurse-led ART management for adults are well documented [23], only few studies focus on paediatric HIV care [24,25]. Second, standardization of dosages and monthly supplies promote adherence assessment using pill counts and appointment scheduling. In adults, pill bottles usually contain standard supplies for one month. These quantities simplify the process for health workers to correctly calculate adherence, set appointment dates and determine when a patient is lost to follow up [26,27]. The situation in children is different: weight dependent dosages prevent packaging of standard monthly or two-month supplies. As a result, calculating appointment dates and adherence is more complicated and error prone, resulting in appointments on dates when patients have already run out of tablets or still have many remaining pills. Lastly, synchronization with caregivers’ visits is more complicated in a family-centred clinic setting when clinic staff tries to match children's visits with those of their guardians.
In Malawi, task shifting efforts from clinical officers to nurses help increase access to ART. Lighthouse Trust, the largest public provider of ART in Malawi's Central Region, pioneered this task shifting effort for adults. Currently, both clinical officers and nurses may become certified to start and follow up adult and paediatric patients on ART. Although guidelines allow for this task shifting effort, knowledge about nurse capacity for correct paediatric ART management is limited. Therefore, we designed an operational study to compare nurses’ prescriptions of paediatric ART, adherence calculation and next appointment date determination with their clinical officer peers who were supported by an electronic data system, the current standard of care at Lighthouse Trust.
Methods
Setting
Lighthouse Trust provides free ART to over 16,000 patients; about 6% of all patients are children aged <15 years. On average, eight nurses and eight clinical officers provide clinical services. They rotate in three- to six-month intervals between Lighthouse Trust's two ART sites, the Martin Preuss Centre (MPC) and the Lighthouse clinic at Kamuzu Central Hospital, providing the same core services to similar patient groups. In addition, clinical officers from other clinics support Lighthouse Trust as clinical attachments on a regular basis, mostly once a week. Nurses complete 70% of the approximately 8000 ART visits per month. They triage and screen adult patients for signs and symptoms, assess adherence by pill counting, issue ART and give new appointments. Clinical officers manage sick patients, initiate treatment, review patients not yet eligible for ART, and review all children and patients on non-standard ART regimens. Lighthouse uses an electronic data system (EDS) with touch-screen stations in reception, height/weight stations, review rooms and pharmacy for real-time data collection and the management of adult and paediatric patients [28]. The EDS suggests an ART regimen based on previous prescriptions, doses based on current body weight, calculates adherence based on expected and actual consumption of tablets, and sets next appointments based on standard monthly supplies, following the national ART guidelines [29]. Children are treated with generic fixed dose combinations (FDC) of d4T/3TC/NVP as adult split or generic paediatric FDC according to weight band-based tables and standard supplies [16].
Design
All nurses and clinical officers were previously trained on paediatric ART care as part of the national ART provider certification. All nurses underwent a two-hour refresher training on the paediatric dosing charts, adherence and appointment calculation and entered a three-day pilot phase with intense supervision by the study coordinator to clarify questions and to ensure that all operations followed the study protocol. All paediatric patients scheduled for a routine ART visit who consented first visited an ART nurse who filled a paper assessment form to determine nurse review eligibility (on standard first line continuation regimen, <15 years old, child present, clinically stable). Inclusion was independent of prior adherence. Children attending for acute clinical problems were sent straight to the clinical officer for review. For eligible patients, the same ART nurse asked a series of questions (directly to an older child or to the caregiver of a young child/infant) and completed the clinical checklist section of the same paper-based assessment (Box 1).
Box 1. Questions to caregivers related to the child's adherence, dose, formulation and next appointment for children on standard paediatric first line regimen using split adult or paediatric fixed dose combination antiretroviral therapy.
How many remaining ARV pills did the patient have last time?
How many pills received last time?
How many remaining ARV pills are brought today?
How many remaining ARV pills left at home today?
Date of the last ARV dispensing visit at the ART clinic?
Number of days since last dispensing visit?
What was the daily dose since last visit? (tabs per day, e.g. 1.25/day)
What is the adherence today in%? actual/expected consumption=[(Q1 +Q2)−(Q3+Q4)]/(Q6*Q7)
What dosage of the ART formulation would you prescribe today am [morning]? (indicate number of tablets)
What dosage of the ART formulation would you prescribe today pm [afternoon]? (indicate number of tablets)
Number of full ART tablets you would dispense today?
What is the date of the next appointment?
What ART formulation would you prescribe today? (paediatric FDC or split adult FDC)
Based on the responses, nurses made the calculation for Questions 8 to 13 with pen and paper as calculators may be unavailable in health centres. They used the formula provided in the national guidelines (additional file 1: Examples for calculation of adherence and next appointment) and the weight band-based dosing charts (additional file 2: Dosing charts for adult split Triomune tablets and Triomune baby tablets). After completion, caregivers and paediatric patients went immediately to clinical officers who were blinded to the nurses’ assessments. Clinical officers asked the child or caregiver the exact same questions asked previously by the nurses; clinical officers recorded answers to questions on an identical paper assessment form. Clinical officers entered the information for questions 8 to 13 into the EDS, which made the dosing, adherence, and next appointment date calculations for them, allowing an assessment of the nurses’ arithmetic skills. Thereafter, patients received their ART at the pharmacy according to the EDS information entered by the clinical officers. To ensure adherence to the study protocol a study coordinator made daily spot-checks in nurse and clinical officer rooms. Unique patient IDs linked nurses’ and clinical officers’ assessments and all forms were double entered into an Access database. Ethical clearance for the study was obtained from the Malawi Health Sciences Research Committee.
Data analysis
Characteristics of patients at ART initiation and involved staff were described using summary statistics and frequency tables. We used analysis of inter-rater agreement (kappa test) [30] to compare agreement of nurses’ and clinical officers’ responses regarding the choice of paediatric ART regimen and examined agreement of numerical variables of dose and adherence with the Bland Altman method [31]. Expression of dates as numerical values allowed calculation of means. For each nurse–clinical officer paired response, we calculated the difference of the values reported by the two cadres (y-axis) and plotted it against its mean (x-axis). Then, we calculated the mean of these differences (the mean difference) and the 95% confidence interval. The distance of the mean difference from zero indicates the trend in the differences of the responses towards one cadre. We calculated the area around the mean that covers 95% of the differences. The lower and upper boundaries of this area are referred to as 95% limits of agreement (LoA). The narrower the boundaries, the better is the agreement between the two cadres. Statistical analysis was performed in STATA 10.
Results
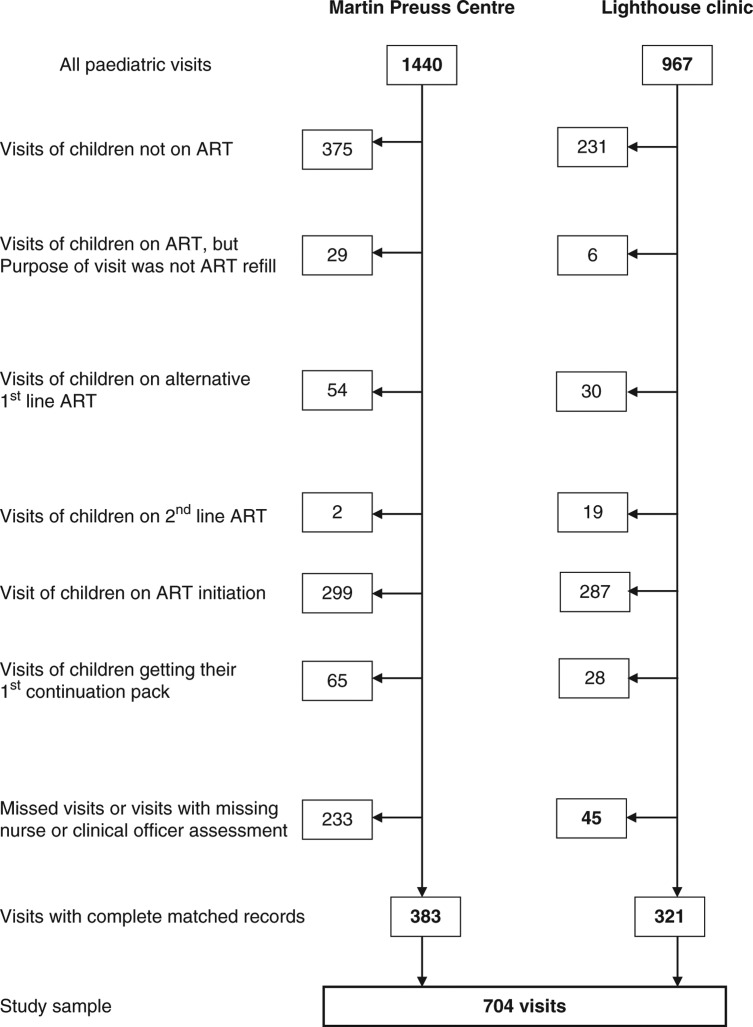
A total of 704 matched nurse and clinical officer reviews of 367 children attending the ART clinics at Lighthouse and MPC between 1st March and 30th July 2010 were included in the study (Figure 1). Approximately 20% of children had one visit, 15% had 4 or more visits. On average, children spent 7.11 minutes with the nurse and 7.39 minutes with the clinical officer. About 50% (190/367) were girls; the median (IQR) age at initiation was 8.4 (5.4, 11) years, and about one-third of patients at both sites were in WHO stage 3 at ART initiation (Table 1). The time on ART among children involved in the study differed between sites: at Lighthouse the median (IQR) was 1136 days (433, 1710), at MPC 422 days (269, 707). The study involved eight nurses and 18 clinicians. However, the workload was not distributed evenly: five nurses and five clinical officers managed 50 visits or more and two nurses and five clinical officers managed 100 visits or more (Table 2).
Figure 1.
Flowchart describing recruitment of study sample between 1st March and 30th July 2010 at Lighthouse Trust's two study sites.
Table 1.
Characteristics of patients at the time of initiation of antiretroviral treatment
| Characteristic | Number of children enrolled, n=376 |
|---|---|
| Agea | |
| 0 to <2 | 18 (4.8) |
| 2 to <5 | 63 (16.8) |
| 5 to <10 | 158 (42.0) |
| 10 to <15 | 131 (34.8) |
| Median (IQR) age in years | 8.4 (5.4, 11.0) |
| Female | 190 (50.5) |
| WHO stageb | |
| 1 | 4 (1.1) |
| 2 | 23 (6.1) |
| 3 | 228 (60.6) |
| 4 | 91 (24.2) |
Not recorded for six children.
Not recorded for 30 children.
Table 2.
Paediatric visits managed by cadre and site (n=704 visits)
| Characteristic | Martin Preuss Centre (n=383) | Lighthouse clinic (n=321) |
|---|---|---|
| Visits per nurse (n=8) | ||
| N1 | 96 | 0 |
| N2 | 23 | 0 |
| N3 | 0 | 76 |
| N4 | 245 | 1 |
| N5 | 2 | 68 |
| N6 | 3 | 54 |
| N7 | 0 | 122 |
| N8 | 14 | 0 |
| Visits per clinical officer (n=18) | ||
| C1–3 | 0 | 7 |
| C4 | 102 | 0 |
| C5 | 2 | 2 |
| C6–7 | 0 | 3 |
| C8 | 8 | 141 |
| C9–10 | 0 | 49 |
| C11 | 124 | 0 |
| C12 | 123 | 2 |
| C13 | 24 | 0 |
| C14 | 0 | 100 |
| C15–18 | 0 | 17 |
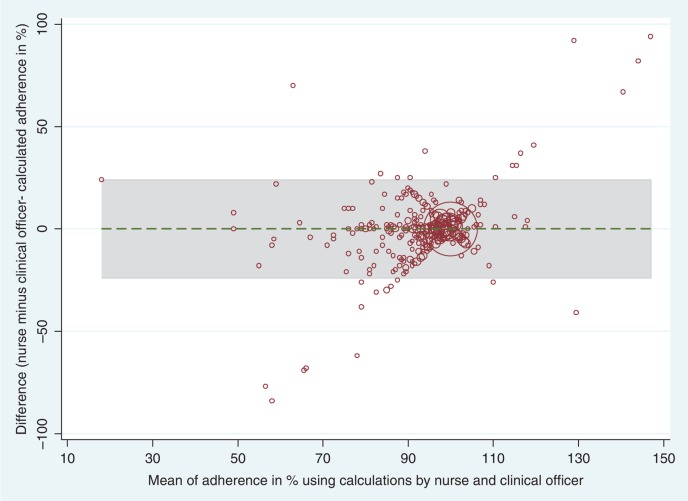
Overall, there was a good agreement in the responses of nurses and clinical officers to the questions in Box 1 with narrow LoA indicating small differences in the paired responses of the two cadres. The mean differences were generally close to zero, indicating that no cadre systematically calculated higher or lower values than the other. Of note, the two cadres’ calculations related to key aspects of paediatric ART management showed excellent agreement, as shown in the example of adherence (Q8, Figure 2). The differences for adherence showed a variation of 48% (LoA:−24% to +24%). These lower and upper boundaries include 95% of the differences of the reviews when nurses and clinical officers calculated adherence. The mean difference of 0.003 (95% CI:−0.9 to 0.9) shows only a very small bias towards nurses, who, on average, calculated slightly better adherence than clinical officers. Two diagonal linear trends left from the centre area of mean 98% adherence are apparent in Figure 2: agreement in adherence calculations is better when patients adhere better and differences increase as the mean adherence decreases.
Figure 2.
Bland- Altman graph plotting differences in adherence assessment between nurses and clinical officers against the mean adherence for each visit. The grey area covers 95% of the differences.
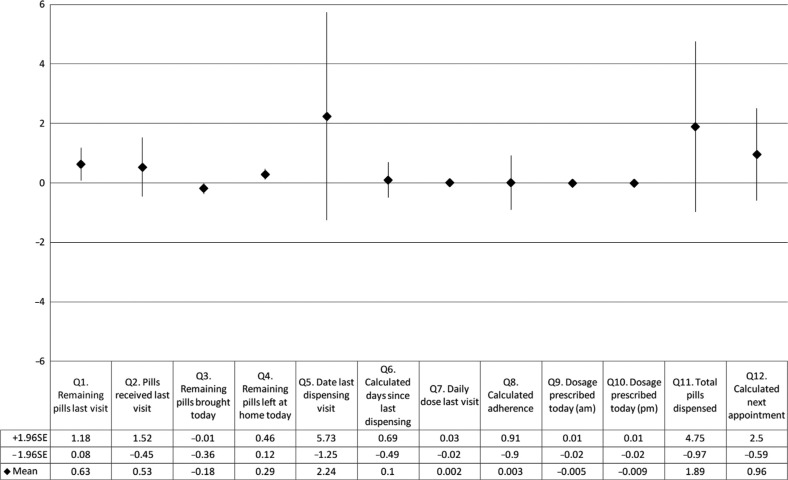
Responses to nine out of 12 questions showed a similar high agreement with narrow LoA, including the questions about morning and evening ART dosages (Q9 and 10) with LoA of−0.4 to 0.4 and −0.41 to 0.4, respectively. Mean differences close to zero demonstrate good agreement between cadres and little bias towards one cadre (Figure 3). Furthermore, there was very good agreement in the ART formulation prescribed (either split adult tablets or paediatric FDC) by nurses and clinical officers (kappa 0.93). However, in 13 out of 704 visits (0.02%) the ART formulation prescribed by nurses and clinical officers differed. Stronger bias was evident in responses to questions on remaining pills at the last visit (Q1), remaining pills brought today (Q3) and remaining pills left at home today (Q4), with mean differences of 0.63 (95% CI: 0.08 to 1.18), −0.18 (95% CI: −0.36 to −0.01) and 0.29 (95% CI: 0.12 to 0.46), respectively (Figure 3).
Figure 3.
Mean differences with 95% confidence intervals between assessments of nurses and clinical officers using an electronic system, derived from Bland- Altman plots.
Responses to questions with mean differences furthest from zero, indicating larger bias towards one cadre, were related to the date of the last dispensing visit (mean difference Q5: 2.24 days), the calculation of the number of pills to be dispensed today (mean difference Q11: 1.89 pills) and the date of next visit (mean difference Q12: 0.96 days) where nurses, on average, recorded the previous visit closer to the current visit, prescribed more pills and gave later appointment dates than clinical officers (Figure 3). Differences in the responses to the questions 5, 11 and 12 were also most widely spread with LoA of 82 days, 152 tablets and 83 days, respectively (additional file 3: Bland Altman graphs for Questions 5, 11 and 12). In addition, differences in the responses to questions 5 and 12 remained unchanged over the study period as evidenced by a largely equal distribution of the scatter points from the left to the right side of the graphs. The mean number of pills prescribed (Q11) cluster around standard monthly or 2-month supplies according to different body weight bands.
Discussion
Our study shows that nurses’ ART prescription practices for children on first line split adult or paediatric FDC, calculations of patient adherence and next appointment date setting are similar to those practices among clinical officers supported by an automated electronic system. The formulas and dosage charts provided to both nurses and clinical officers appear user-friendly and arithmetic skills of involved nurses are sufficient. Interestingly, the time required to visit each cadre was similar. Our findings highlight several aspects of paediatric ART management that have clinical and programmatic implications.
First, nurses correctly calculate – with pen and paper – medication adherence since the last visit using pill counts. Paediatric ART in FDC tablet formulation is more practical than syrups [11,17], and allow nurses to transfer the skills learned in adult pill count measurements to paediatric care. Though incorporating fractions of tablets and differing doses based on body weight from remaining supplies of prior and current visits make calculations difficult, our study shows that nurses, using this information and following a formula, can correctly calculate adherence based on pill counts. The process of conducting an accurate pill count and carefully calculating adherence in the presence of child and caregiver may, in itself, reinforce and promote adherence. However, it is unknown why differences between nurses’ and clinical officers’ calculations increase in regions of lower adherence.
Second, nurses were able to choose the correct formulation and prescribe the correct dosage for AM and PM dosing. Despite using FDC tablets, the regimens used in the study were still complex: in some weight bands AM and PM dosages differed for split adult tablets and two different paediatric formulations were in use. Although only a small proportion of visits required changes in regimens or dosing bands our finding of correct AM and PM dosing is important – errors during these critical events may result in over- or under-dosing, potentially with severe consequences for the child. If regimens and dosages remain unchecked, errors are carried forward. Nurses are often “the last line of defence” to administer prescribed medications correctly [5]; in the context of a public health sector ART clinic in Malawi and other countries in sub-Saharan Africa, they are often the only ones providing care. However, our study also highlights a limitation of task shifting: the study was interrupted for three weeks during which 233 paediatric visits at MPC were managed only by clinical officers because the two available nurses were required to conduct routine reviews for stable adult patients. Although there is some risk that continued task shifting to nurses may stretch human resources or exceed nurse capacity resulting in lower quality of services [32], our findings show that paediatric ART can be prescribed safely by nurses in these settings and adds further support to nurse-led, high quality care.
Third, based on standard 1- or 2-month supplies according to weight bands, nurses were able to calculate next appointment dates correctly. Knowing when patients are expected to return has three major implications for clinic organization and patient management. First, it allows daily planning and staffing of the clinic due to a foreseeable workload. This is particularly important when the demand for services outweighs the capacity of providers. At the same time, patients are re-assured that they receive services that day, reducing anxiety, transportation and time costs. Second, it facilitates identification of patients that miss appointments, helping launch tracing efforts at an early stage of lost to follow up (LTFU). Early tracing helps to identify true outcomes and return patients back to care [26]. This, in turn, improves the quality of routine monitoring and evaluation of the entire programme by reducing LTFU and presenting realistic outcomes [26]. Lastly, calculating appointments correctly enables nurses to adjust appointments between child and caregiver, should he/she also be on ART. Synchronized appointments of the family members may have a positive effect on adherence by reducing the number of clinic visits per family and improving patient satisfaction especially in health facilities where adults and children are frequently seen in the same queue. Care provided to the family unit may also reduce stigma and have other positive effects, for example allowing a discussion of family planning, HIV counselling and testing or control of STDs [33].
Lastly, the dramatic differences in workload between individuals of the same cadre and between cadres merit attention as the division of labour may affect the quality of care, including the fundamental paediatric management skills assessed in this study. From the results of the study, it appears that a few nurses and clinical officers completed a disproportionate amount of the patient assessments and reviews. Several factors likely contributed to this finding. First, some clinical officers work at Lighthouse on a rotation, contributing only few study reviews. Second, staff have other responsibilities, by choice or by requirement, outside of patient care. Clinical officers often have management responsibilities including clinic coordination, mentoring duties, and supervision, both within and outside the clinic. In addition to providing care for the vast majority of stable adult patients, nurses also rotate to manage the pharmacy and provide counselling sessions. The differences in work load revealed by these findings require further elucidation and follow-up to better distribute the burden among all staff members.
Our study has a number of limitations. First, as Lighthouse Trust provides services only to HIV-infected individuals, the study nurses already routinely managed adult patients and were used to both pill-count measurement and calculation of next appointments. However, many factors are the same between Lighthouse and other clinics. Dosage guidelines, 1- or 2-month supplies of pills, and formulas for measurement of adherence are standardized in the national ART guidelines, and all staff, nationwide, undergoes standard National ART training based on these guidelines; therefore, our results may be reproducible in other facilities in Malawi. Second, as discussed above, relatively few nurses and clinical officers managed the majority of visits, which may reflect preferences for paediatric management by a few better-qualified, more motivated nurses and clinical officers and result in higher than average care quality. Moreover, some caregivers and children may prefer a specific nurse or clinical officer, accepting a longer waiting time or re-arranging their place in the patient queue to be seen by their preferred provider. However, in post hoc analysis limited to the five nurses and five clinical officers that contributed 50 or more visits (results not shown), the findings were similar to our original analysis. Third, we only examined FDC tablet formulations. Results are likely to be different if different formulations (e.g. tablets and syrups) are used or combinations of different tablets containing single drugs or dual formulations, as it is the case for alternative first- or second-line regimens, where complexity is higher. Lastly, the design did not allow comparison of patients’ clinical or virological outcomes, and we did not assess or compare the clinical skills of nurses and clinical officers, two aspects that would add to the discussion of service quality. However, we believe that the aspects of paediatric patient management included in our study are demonstrative of quality care and suggest that paediatric patient outcomes would be favourable whether managed by nurses or clinical officers.
Conclusions
Nurses, similar to their clinical officer peers, prove capable and motivated to provide quality ART care for paediatric patients as measured by accurate dosing, formulation, adherence calculation and determination of next visit date. These results support previous task shifting of adult ART patient management and encourage further research in this human resource strategy for care of children as well. Our findings also support policy decisions for standardized, tablet based FDC for use in children, enabling easier and less error prone calculation of dosages. Although challenges in both supplies and funding for paediatric ART are formidable [34,35], it appears clear that nurse management of paediatric ART patients may help to achieve Malawi's paediatric targets in universal access to ART [36].
Acknowledgements
We are thankful to patients at Lighthouse clinic and MPC and Brian Faragher for providing statistical advice.
To access the supplementary material to this article please see Supplementary Files under Article Tools online.
Competing interests
Authors have no competing interests.
Authors' contributions
RW designed the study and wrote the first draft. RW and CF analyzed the data and CF made a substantial contribution to the writing of subsequent drafts of the manuscript. HT and CG were responsible for data management. RW, CH, JG and MK collected the data. SP contributed to design and study implementation. All authors reviewed and approved the final manuscript.
Abbreviations
ART, antiretroviral treatment; EDS, electronic data system; FDC, fixed dose combination; LoA, limits of agreement; LTFU, lost to follow up; MPC, Martin Preuss Centre.
References
- 1.Miller MR, Robinson KA, Lubomski LH, Rinke ML, Pronovost PJ. Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;16:116–26. doi: 10.1136/qshc.2006.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McPhillips HA, Stille CJ, Smith D, Hecht J, Pearson J, Stull J, et al. Potential medication dosing errors in outpatient pediatrics. J Pediatr. 2005;147:761–7. doi: 10.1016/j.jpeds.2005.07.043. [DOI] [PubMed] [Google Scholar]
- 3.Ghaleb MA, Barber N, Franklin BD, Yeung VW, Khaki ZF, Wong IC. Systematic review of medication errors in pediatric patients. Ann Pharmacother. 2006;40:1766–76. doi: 10.1345/aph.1G717. [DOI] [PubMed] [Google Scholar]
- 4.Ghaleb MA, Barber N, Franklin BD, Wong IC. The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child. 2010;95:113–8. doi: 10.1136/adc.2009.158485. [DOI] [PubMed] [Google Scholar]
- 5.Gonzales K. Medication administration errors and the pediatric population: a systematic search of the literature. J Pediatr Nurs. 2010;25:555–65. doi: 10.1016/j.pedn.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Santell JP, Hicks R. Medication errors involving pediatric patients. Jt Comm J Qual Patient Saf. 2005;31:348–53. doi: 10.1016/s1553-7250(05)31046-4. [DOI] [PubMed] [Google Scholar]
- 7.Caldwell NA, Power B. The pros and cons of electronic prescribing for children. Arch Dis Child. 2012 Feb;97(2):124–8. doi: 10.1136/adc.2010.204446. Epub 2011/06/18. [DOI] [PubMed] [Google Scholar]
- 8.Davey AL, Britland A, Naylor RJ. Decreasing paediatric prescribing errors in a district general hospital. Qual Saf Health Care. 2008;17:146–9. doi: 10.1136/qshc.2006.021212. [DOI] [PubMed] [Google Scholar]
- 9.Jani YH, Ghaleb MA, Marks SD, Cope J, Barber N, Wong IC. Electronic prescribing reduced prescribing errors in a pediatric renal outpatient clinic. J Pediatr. 2008;152:214–8. doi: 10.1016/j.jpeds.2007.09.046. [DOI] [PubMed] [Google Scholar]
- 10.Santell JP, Kowiatek JG, Weber RJ, Hicks RW, Sirio CA. Medication errors resulting from computer entry by nonprescribers. Am J Health Syst Pharm. 2009;66:843–53. doi: 10.2146/ajhp080208. [DOI] [PubMed] [Google Scholar]
- 11.Hoppu K, Sri RS, Dodoo AN. Realities of paediatric pharmacotherapy in the developing world. Arch Dis Child. 2011;96:764–8. doi: 10.1136/adc.2009.180000. [DOI] [PubMed] [Google Scholar]
- 12.Sigaloff KC, Calis JC, Geelen SP, van VM, de Wit TF. HIV-1-resistance-associated mutations after failure of first-line antiretroviral treatment among children in resource-poor regions: a systematic review. Lancet Infect Dis. 2011 Oct;11(10):769–79. doi: 10.1016/S1473-3099(11)70141-4. Epub 2011/08/25. [DOI] [PubMed] [Google Scholar]
- 13.Weidle PJ, Abrams EJ, Gvetadze R, Rivadeneira E, Kline MW. A simplified weight-based method for pediatric drug dosing for zidovudine and didanosine in resource-limited settings. Pediatr Infect Dis J. 2006;25:59–64. doi: 10.1097/01.inf.0000195619.76277.3f. [DOI] [PubMed] [Google Scholar]
- 14.Ponnet M, Frederix K, Petdachai W, Wilson D, Eksaengsri A, Zachariah R. A drug dosage table is a useful tool to facilitate prescriptions of antiretroviral drugs for children in Thailand. Int J STD AIDS. 2005;16:420–6. doi: 10.1258/0956462054094114. [DOI] [PubMed] [Google Scholar]
- 15.Weigel R, Makwiza I, Nyirenda J, Chiunguzeni D, Phiri S, Theobald S. Supporting children to adhere to anti-retroviral therapy in urban Malawi: multi method insights. BMC Pediatr. 2009;9:45. doi: 10.1186/1471-2431-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.HIV unit. Guidelines for the use of antiretroviral therapy in Malawi. 3rd ed. Malawi: Ministry of Health; 2008. Apr, Treatment of AIDS. [Cited 2011 Nov 22]. Available from: http://www.hivunitmohmw.org/uploads/Main/Malawi%20ART%20Guidelines%203rd%20Edition. [Google Scholar]
- 17.WHO Paediatric Antiretroviral Working Group. Geneva: 2007. Preferred antiretroviral medicines for treating and preventing HIV infection in younger children. [Cited 2011 Nov 22]. Available from: http://www.who.int/hiv/events/paediatricmeetingreport.pdf. [Google Scholar]
- 18.WHO. WHO generic tool for assessing paediatric ARV dosing. 2011. [Cited 2011 Nov 22]. Available from: http://www.who.int/hiv/paediatric/generictool/en/
- 19.Vanprapar N, Cressey TR, Chokephaibulkit K, Muresan P, Plipat N, Sirisanthana V, et al. A chewable pediatric fixed-dose combination tablet of stavudine, lamivudine, and nevirapine: pharmacokinetics and safety compared with the individual liquid formulations in human immunodeficiency virus-infected children in Thailand. Pediatr Infect Dis J. 2010;29:940–4. doi: 10.1097/INF.0b013e3181e2189d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Musiime V, Kendall L, Bakeera-Kitaka S, Snowden WB, Odongo F, Thomason M, et al. Pharmacokinetics and acceptability of once- versus twice-daily lamivudine and abacavir in HIV type-1-infected Ugandan children in the ARROW Trial. Antivir Ther. 2010;15:1115–24. doi: 10.3851/IMP1695. [DOI] [PubMed] [Google Scholar]
- 21.Mulenga V, Cook A, Walker AS, Kabamba D, Chijoka C, Ferrier A, et al. Strategies for nevirapine initiation in HIV-infected children taking pediatric fixed-dose combination “baby pills” in Zambia: a randomized controlled trial. Clin Infect Dis. 2010;51:1081–9. doi: 10.1086/656628. [DOI] [PubMed] [Google Scholar]
- 22.WHO. Task shifting to tackle health worker shortages. 2007. [Cited 2011 Nov 22]. Available from: http://www.who.int/healthsystems/task_shifting_booklet.pdf.
- 23.Sanne I, Orrell C, Fox MP, Conradie F, Ive P, Zeinecker J, et al. Nurse versus doctor management of HIV-infected patients receiving antiretroviral therapy (CIPRA-SA): a randomised non-inferiority trial. Lancet. 2010;376:33–40. doi: 10.1016/S0140-6736(10)60894-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCollum ED, Preidis GA, Kabue MM, Singogo EB, Mwansambo C, Kazembe PN, et al. Task shifting routine inpatient pediatric HIV testing improves program outcomes in urban Malawi: a retrospective observational study. PLoS One. 2010;5:e9626. doi: 10.1371/journal.pone.0009626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Griensven J, De Naeyer L, Uwera J, Asiimwe A, Gazille C, Reid T. Success with antiretroviral treatment for children in Kigali, Rwanda: experience with health center/nurse-based care. BMC Pediatr. 2008;8:39. doi: 10.1186/1471-2431-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tweya H, Gareta D, Chagwera F, Ben-Smith A, Mwenyemasi J, Chiputula F, et al. Early active follow-up of patients on antiretroviral therapy (ART) who are lost to follow-up: the ‘Back-to-Care’ project in Lilongwe, Malawi. Trop Med Int Health. 2010;15(Suppl 1):82–9. doi: 10.1111/j.1365-3156.2010.02509.x. [DOI] [PubMed] [Google Scholar]
- 27.Weigel R, Hochgesang M, Brinkhof MW, Hosseinipour MC, Boxshall M, Mhango E, et al. Outcomes and associated risk factors of patients traced after being lost to follow-up from antiretroviral treatment in Lilongwe, Malawi. BMC Infect Dis. 2011;11:31. doi: 10.1186/1471-2334-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Douglas GP, Gadabu OJ, Joukes S, Mumba S, McKay MV, Ben-Smith A, et al. Using touchscreen electronic medical record systems to support and monitor national scale-up of antiretroviral therapy in Malawi. PLoS Med. 2010 Aug 10;7(8) doi: 10.1371/journal.pmed.1000319.e1000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ministry of Health M. Clinical management of HIV in children and adults. Malawi integrated guidelines for providing HIV services in antenatal care, maternity care under 5 clinics, family planning clinics, exposed infant/pre-ART clinics, ART clinics; 2011. [Cited 2011 Nov 22]. Available from: http://www.hivunitmohmw.org/Main/AntiretroviralTherapy. [Google Scholar]
- 30.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 31.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 32.Fairall L. The effect of task-shifting antiretroviral care in South Africa: a pragmatic cluster randomized trial. Sixth International AIDS Society Conference on HIV pathogenesis, Treatment and Prevention; 17–20; Rome. Abstract MOPDD0105; 2011. Jul, [Google Scholar]
- 33.Betancourt TS, Abrams EJ, McBain R, Fawzi MC. Family-centred approaches to the prevention of mother to child transmission of HIV. J Int AIDS Soc. 2010;13(Suppl 2):S2. doi: 10.1186/1758-2652-13-S2-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schouten EJ, Jahn A, Ben-Smith A, Makombe SD, Harries AD, Aboagye-Nyame F, et al. Antiretroviral drug supply challenges in the era of scaling up ART in Malawi. J Int AIDS Soc. 2011;14(Suppl 1):S4. doi: 10.1186/1758-2652-14-S1-S4. accessed 2012 Aug 4. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3194149/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Medecins sans frontiers. No time to quit: HIV/AIDS treatment gap widening in Africa. MSF analysis of teh widening funding gap for HIV/AIDS treatment in sub-Saharan Africa. 2010. [Cited 2011 Nov 22]. Available from: http://www.doctorswithoutborders.org/publications/reports/2010/MSF-No-Time-to-Quit-HIV-AIDS.pdf.
- 36.National AIDS Commission. Universal access indicators and targets for Malawi. 2006. accessed 2012 Aug 4. Available from: http://www.docstoc.com/docs/90196888/Universal-Access-Targets-Final-Report-Jan-2007.