Abstract
Background:
Protecting households against financial risks is one of objectives of any health system. In this regard, Iran’s fourth five year developmental plan act in its 90th article, articulated decreasing household’s exposure to catastrophic health expenditure to one percent. Hence, this study aimed to measure percentage of Iranian households exposed to catastrophic health expenditures and to explore its determinants.
Methods:
The present descriptive-analytical study was carried out retrospectively. Households whose financial contributions to the health system exceeded 40% of disposable income were considered as exposed to catastrophic healthcare expenditures. Influential factors on catastrophic healthcare expenditures were examined by logistic regression and chi-square test.
Results:
Of 39,088 households, 80 were excluded due to absence of food expenditures. 2.8% of households were exposed to catastrophic health expenditures. Influential factors on catastrophic healthcare were utilizing ambulatory, hospital, and drug addiction cessation services as well as consuming pharmaceuticals. Socioeconomics characteristics such as health insurance coverage, household size, and economic status were other determinants of exposure to catastrophic healthcare expenditures.
Conclusion:
Iranian health system has not achieved the objective of reducing catastrophic healthcare expenditure to one percent. Inefficient health insurance coverage, different fee schedules practiced by private and public providers, failure of referral system are considered as probable barriers toward decreasing households’ exposure to catastrophic healthcare expenditures.
Keywords: Catastrophic healthcare expenditures, Impoverishment, Financial protection, Iran
Introduction
Health expenditures are among issues which have always been discussed by researchers in the fields of economics and public health (1). Medical technology development, the indiscriminate growth of population, lifestyle changes as a result of industrialization, the emergence of new diseases, etc have caused increasing growth of health services expenditures in recent decades (2). Due to high health expenditures, each year nearly 44 million households (more than 150 million people) worldwide have to pay catastrophic healthcare expenditures. Almost 25 million of households or, in other words more than 100 million people, are pushed below the poverty line due to catastrophic expenditures (3).
People get sick all over the world and resources are used to cure them (4). The more, providing resources relies on public resources and prepayments, the more fair the health system is conversely, the more financial resources are provided from direct payments, the more unfair the health financing system is. The most important result of unfair participation of households in health financing is that the percentage of households exposed to catastrophic healthcare expenditures will increase (5).
In the study of national health accounts in the Ministry of Health in 2007, out of pocket payments were reported %52.6 (5). High share of out of pocket payments and the necessity of protection against financial risks, which is one of three goals of each health system (as well as Iran’s) and the impact that this objective has on other two objectives (health, responsiveness) shall be considered more (6).
Nowadays, lack of financial protection in health is recognized as the disease of health systems. The most obvious symptom of that is the households suffer from not only the illness but also the poverty and economic destruction; in other words they suffer facing catastrophic expenditures and poverty caused by health financing. Therefore, timely diagnosis of this disease by measuring and monitoring catastrophic health and identification of the factors that put household at risk of dealing with these expenditures will help policy makers in choosing precautionary policies and treatment methods for this disease (7).
Iran’s fourth five year developmental plan act in its 90th article, articulated decreasing household’s exposure to catastrophic health expenditure to one percent. We aimed to assess degree of success in achieving the mentioned objective at the end of forth five year developmental plan.
Methods and Materials
The current cross sectional study has been carried out retrospectively based on data obtained from the Iranian household survey, conducted by statistical centre of Iran (SCI). This study draws on micro-data sets of SCI House-hold Income and Expenditure Survey (HIES) for the year 2008. The HIES is a nationally and regionally representative household survey carried out by SCI through the sample observations. The ultimate sampling unit is a household. Information for the HIES is collected by personal interview with household heads over a 24 hour period for rural and 48 hour period for urban for food items and month by month for non-food items throughout the year. The sampling methodology can be described as multistage random sampling with geographical stratification and clustering. The sample size for present analysis is as follows: 39,088 households of which 19,707 households lived in rural areas and 19,381 households lived in urban areas.
The SCI uses a questionnaire for data collection which consists of four parts as follows:
Part I - The social characteristics of household members;
Part II - The profile of residence, living facilities and major appliances;
Part III - Food and non-food expenditures of the household;
Part IV - Household incomes;
For this study, we extracted required information from the raw data. Although the income and overall expenses of a household can be estimated through the questionnaire, for analysis, overall spending is preferred to the income of a household for two reasons; first, the variance of current expenditures is fewer than the current income. Income data are a reflection of random shocks while using expenditure data gives a better understanding of the income and effects of income random shocks are not considered in that. Secondly, in most households’ traversal, expenditure data are more valid than income data. For this reason, in calculations, household spending is considered better than the income reported by households.
Data analysis
Households with health expenditures more than 40% of their ability to pay have been categorized as households dealing with catastrophic expenditures. Household ability to pay means effective income minus subsistence expenditures of the household. However, for some households which had announced their food expenditures less than their subsistence expenditures, we calculated ability to pay of the household considering the effective income minus food expenditures. The effective income was calculated based on the total consumption expenditures of a household in a certain period of time. To calculate the subsistence expenditures of household, poverty line based on the food was used, i.e. part of the total expenditures of the household spent for food. Since the poorer households spend greater share of their consuming expenditures on food, per capita average of equivalent food expenditures of those households which are placed on the 45 to 55 percentile comparing to total expenditures of the household was considered as the poverty line. Food expenditures increase according to the number of household members but this increase is less than the increase ratio in household. So, the subsistence expenditure of each household is calculated based on the equivalent family size. The equivalent family size was calculated based on real size of the household raised to fixed β power (equivalent to 0.56). The subsistence expenditures minus the total expenditures are the household capacity to pay. Then, the ratio of each household health expenditure to its capacity to pay was calculated. If the number was over 40%, that household was categorized in the group of households exposed to catastrophic health expenditures (3, 8–11) (Formulas for calculation have been annexed to the article).
After calculating the catastrophic expenditures based on the household capacity to pay, in the second part of the study, the impact of several factors on the main outcome of study was assessed. Independent variables considered were family size, health insurance status of the household, household economic status, outpatient and inpatient services utilization, consumption of pharmaceutical and medical products. The main outcome of study was whether households facing with catastrophic health expenditures. Univariate analysis was done using the Chi-square test. In the Univariate analysis, association between each factor and outcome was assessed, irrespective of other variables. Then multifactorial model (also known as adjusted model) was fitted in which impact of variables was adjusted in presence of other variables being offered to the model. To do so, logistic regression model in conjunction with Backward Elimination (B.E.) variable selection method was fitted. In the B.E. method, full model was fitted. Then variable with the highest P-value was removed, and the model was re-fitted. The whole process continued until all variables retained significant. Results of Univariate and multifactorial models are presented in terms of Odds Ratio (OR), Confidence Interval (C.I), and P-value. A P-value less than 0.05 was considered as statistical significance. Data analysis was carried out in SPSS ver.16 and Excel.
Results
39,008 households out of 39,088 households were included in the final analysis) 80 were excluded due absence of food expenditures). Eleven percent of household heads were female. If we consider those head of households who are housekeeper as unemployed ones (with no income), nearly 3% of the households were unemployed (Table 1).
Table 1:
Demographics variables according to place of residence
| Place of residence | Urban (%) | Rural (%) | Total (%) | |
|---|---|---|---|---|
| Gender | Male | 89.71 | 88.09 | 88.9 |
| Female | 10.29 | 11.89 | 11.1 | |
| Occupation | Employed | 71.32 | 76.97 | 74.145 |
| Unemployed (searching for job) | 1.85 | 2.08 | 1.965 | |
| Having income (without job) | 24.47 | 18.64 | 21.555 | |
| Student | 0.29 | 0.05 | 0.17 | |
| Housewife | 0.87 | 1.08 | 0.975 | |
| Other | 1.20 | 1.18 | 1.19 | |
| Marital status | Married | 87.74 | 86.64 | 87.19 |
| Widow(er) | 9.42 | 11.5 | 10.46 | |
| Divorced | 0.87 | 0.56 | 0.715 | |
| Single | 1.96 | 1.3 | 1.63 |
Household’s expenditure data
The average of food expenditure for each household was 174.7 USD monthly (The first and third percentile were 90.8 and 220.4 USD respectively). The consumption expenditure average for each household was 606.4 USD monthly (The first and third percentile were 276.2 and 748.2 USD respectively). The share of food expenditure for each household was roughly 28.8% of the total consumption expenditure. Ability to pay for each household was estimated 471.7USD monthly.
In urban areas, the average of food expenditure for each household was 177.1USD monthly. The average of consumption expenditure for each urban household was estimated 752 USD monthly. The share of food expenditure of each household was roughly 23.5% of the total consumption expenditure. Ability to pay for each household was 617.7 USD monthly (The first and third percentile were 164.5 and 583USD respectively).
In rural areas, the average of food expenditure for each household was 172.3 USD monthly which is almost equal to food expenditure in urban areas. The average of consumption expenditure for each household is 460.7 USD monthly. Ability to pay for each household was estimated 328.1USD. The share of food expenditure for each household is roughly 37.4% of the total consumption expenditure. The average of food expenditure in rural and urban areas did not differ much (they were nearly equivalent), but the average of consumption expenditure in urban areas was nearly twice as the rural areas (1.88) and consequently the ability to pay in urban areas was twice as the rural areas. The average of consumption expenditure in urban areas was 4.24 times the average of their food expenditure. In urban areas, the share of food expenditure was 23.5% of the total consumption expenditure. The share of food expenditures was 27% of the ability to pay. In rural areas, the share of food expenditure was 37.4% of the total consumption expenditure and 52% of the ability to pay.
In this study, the households whose consumption expenditure was less than their subsistence expenditure were considered as poor households. The percentage of poverty in this study was 8.35% (2.8% in urban areas, 13.9% in rural areas). The number of rural poor households is five times of the number of urban poor households. The subsistence expenditure for each household was calculated based on adjusted family size so that living expenditure for each person (minimum survival rate) was calculated 80.6 USD monthly.
Health Expenditures
Mean health expenditures was 38.3 USD monthly (The first and third percentile were 0 and 25.6 USD respectively). The share of health expenditures was 6.3% of the total consumption expenditure and the share of these expenditures was 8.1% of the ability to pay for each household. The average of health expenditures was estimated 18.3 USD for each person monthly (urban areas: 23 USD and rural areas: 13.6 USD); in urban areas the share of health expenditures was 6.2% of the total consumption expenditure for each household and the share of health expenditures was 7.6% of the ability to pay for each household. In rural areas, the share of health expenditures was 6.4% of the total consumption expenditure for each household and the share of health expenditures was 8.9% of the ability to pay for each household. Meanwhile, average monthly health expenditures were estimated 18.4 USD for each person (23.1 and 13.7 USD for urban and rural areas respectively). Table 2 shows the percentage of households who have used all types of health services.
Table 2:
Health services utilization according to place of residence
| Health services\ Place of residence | Urban (%) | Rural (%) | Total (%) |
|---|---|---|---|
| Medicines | 65.5 | 63.3 | 64.6 |
| Inpatient services | 10.7 | 13.1 | 11.9 |
| Outpatient services | 55.7 | 53.4 | 54.55 |
| Drug addiction quit services | 0.09 | 0.07 | 0.08 |
| Health insurance | 62.7 | 86.7 | 74.4 |
Pharmaceutical products have the most and drug addiction cessation services have the least usage. More than half of the households have used outpatient services. Also, 74.4% of households used one of the health insurances.
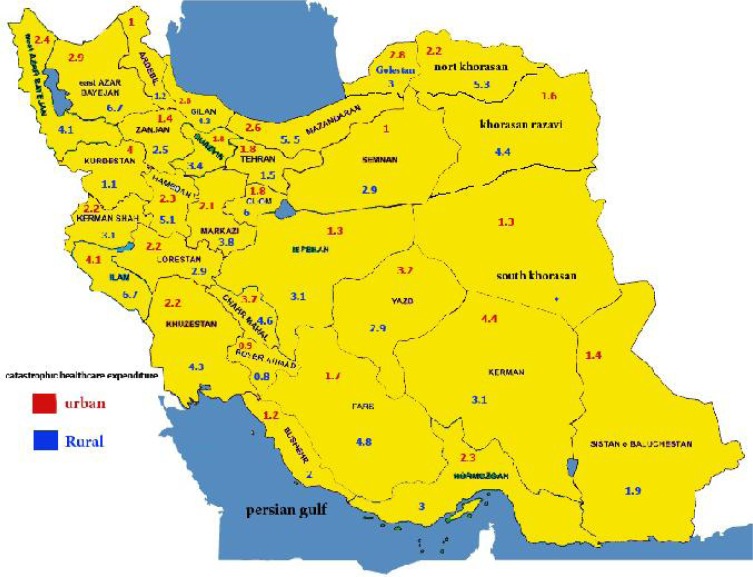
The percentage of households exposed to catastrophic health expenditures was estimated 2.8% with 2.1% for urban areas (CI: 1.9% – 2.4%) and 3.4 % for rural areas: (CI: 3.2% – 3.7%). In this study, the percentage of households faced with these expenditures was calculated separately in each province and the results are presented in Figure 1. To determine the factors affecting households’ exposure to catastrophic health expenditures, the Chi-square and logistic regression were used and the results are shown in Table 3.
Fig. 1:
Percentage of household exposed to catastrophic healthcare expenditure among Iran provinces-2008
Table 3:
Determinants of exposure to catastrophic health expenditures
| Variable |
Catastrophic expenditure
|
Univariate OR (CI) | Multifactorial OR (CI) | ||
|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||
| Insurance | No | 279 (25.6) | 9469 (25) | 0.97 (0.84–1.11) | 0.83 (0.72–0.96) |
| Yes | 810 (74.4) | 28450(75) | P = 0.626 | P = 0.016 | |
| Outpatient service expenses | No | 242 (22.2) | 17436 (46) | 2.98 (2.58–3.44) | 3.42 (2.88–4.05) |
| Yes | 847 (77.8) | 20482 (54) | P < 0.001 | P < 0.001 | |
| Inpatient service expenses | No | 466 (42.8) | 33862(89.3) | 11.16 (9.86–12.64) | 11.84 (10.33–13.57) |
| Yes | 623 (57.2) | 4057 (10.7) | P < 0.001 | P < 0.001 | |
| Pharmacetical expenses | No | 113 (10.4) | 13712 (36.2) | 4.89 (4.02–5.95) | 1.06 (0.84–1.35) |
| Yes | 976 (89.6) | 24204 (63.8) | P < 0.001 | P < 0.001 | |
| Drug addiction cessation services expenses | No | 1083 (99.4) | 37894 (99.9) | 3.40 (3.44–20.51) | 13.32 (5–35.47) |
| Yes | 6 (0.6) | 25 (0.1) | P < 0.001 | P < 0.001 | |
| Household size | 1≤x< 3 | 296 (27.2) | 6784 (17.9) | 0.57 (0.50–0.66) | 0.59 (0.5–0.69) |
| 3≤x< 6 | 596 (54.7) | 23811 (62.8) | P < 0.001 | P <0.001 | |
| 6≤x | 197 (18.1) | 7324 (19.3) | |||
| Economic status | Quintile 1 | 322 (29.6) | 7484 (19.7) | 0.77 (0.65–0.91) | |
| P < 0.001 | |||||
| Quintile 2 | 251 (23) | 7547 (19.9) | 0.57 (0.47–0.68) | ||
| P < 0.001 | |||||
| Quintile 3 | 187 (17.2) | 7614 (20.1) | 0.50 (0.41–0.60) | ||
| P < 0.001 | |||||
| Quintile 4 | 164 (15.1) | 7638 (20.1) | 0.50(0.42–0.61) | ||
| P < 0.001 | |||||
| Quintile 5 | 165 (15.2) | 7636 (20.1) | |||
Multifactorial logistic regression analysis showed that the expenditure of drug addiction cessation and inpatient services had the greatest impact on households’ exposure to catastrophic health expenditures. Households using drug addiction cessation services and those using inpatient services have been 13.33 and 11.84 times more subject to catastrophic health expenditures than households not using these services. Also, households using outpatient services faced with catastrophic expenditures 3.42 times more than those who did not use such services, which had a significant relationship in all cases except pharmaceutical services. Less populated households are less prone to catastrophic expenditures. Economic status was another effective factor in facing with catastrophic expenditures. The households ranked in higher quintiles (with better economic status) dealt with catastrophic expenditures 46% less than households with poor economic status. In addition, there was no significant relationship concerning health insurances.
Discussion
As per the article 90 of the fourth 5-year plan (2005–2009) the number of households facing with catastrophic health expenditures were reported 2.3% all over the country at the beginning of the plan and the aim of the plan was to decrease it to 1% (5). Our study which was carried out in final years of the fourth plan showed that exposure to catastrophic health expenditures in rural areas were 3.4% and in urban areas were 2.1%, i.e. not only the percentage of catastrophic expenditures has not decreased, but also it has increased comparing to beginning years of the plan. However, as long as the amount of out of pocket payments is high, we can’t achieve this goal. Also, there is a considerable inequality not only among provinces but also among rural and urban areas of a single province. The main reason for high number of households dealing with catastrophic expenditures was the high percentage of households in rural areas facing with catastrophic expenditures (more than 5%). These findings are consistent with previous Iranian study which estimated exposure of households with catastrophic health expenditures as 4% (10). Another Iranian study estimated this figure as 3.29% for rural areas all over the country and 1.87% for urban areas (12). On the other hand, other Iranian studies at regional level estimated this figure as 22.2% in province of Kermanshah (13) and 11.7% in District 17 of Tehran (6). Of course, these great divergences are because of the respective survey methods or data analysis, the possibility of high expenditures due to sophisticated access to health and treatment services and also better and easier access to these facilities in the capital comparing to other areas. According to a study in Georgia, 14.8% of households in the capital of the country faced with catastrophic expenditures, while it was 11.2% in east of the country and %10.%1 in western part of the country (14).
Based on the results of household’s economic status, households with better financial status, face with catastrophic health expenditures less than households with worse economic status. These findings are consistent with Kavousi et al (6) and results of other studies in this field, particularly with the studies carried out in developing countries (15–17). Conversely a study in 13 Asian countries showed that households with better economic status, particularly in countries with low and average income, spend higher proportion of their ability to pay for healthcare services and in some Asian countries such as Indonesia, in which the poor are exempted from payments purposely, households with better economic status shall pay catastrophic expenditures(11). A Thai study also showed that, after implementation of universal insurance coverage, the rich are subject to catastrophic health expenditures instead of poor households (18). This might be because of the fact that, the rich seek expensive services from private sector more or they unnecessarily use health services. The other reason which is more probable is that the poor overlook their demand for health services.
This study did not indicate any relation between the insurance status and confronting with catastrophic expenditures. However, these findings were contradictory to other studies (3, 6). The implementation of insurance policies to protect households against catastrophic expenditures has been suggested as a solution for health system financial protection deficiency (11, 18, 19). Yet a Study in China showed that health insurance increases the risk of dealing with catastrophic health expenditures for households by encouraging people to use services more and to use sophisticated services (20). These findings indicate that the insurance system of the country is inefficient concerning financial protection of households. In designing health insurance system, it is necessary to pay attention to benefit packages, payment methods and the behavior of insurers.
Based on this research, health services consumption is considered as another important determinant of household’s exposure to catastrophic health expenditures and there is a significant relation between facing with catastrophic health expenditures and variables such as outpatient and inpatient services utilization. A study in district 17 of Tehran showed that households using inpatient and dental services are more subject to catastrophic health expenditures (6). The Thai study concluded that hospitalization of a member of the household during the past 12 months in public or private hospital is a factor for dealing with catastrophic health expenditures. This relation was more remarkable concerning private hospital (18). A study conducted in Nepal showed that %20 of households, having hospitalized patients, has been pushed under poverty line and the rest have been driven close to it (21). Su in a study has endorsed the relationship between service consumption and confronting catastrophic health expenditures. In Thailand, after implementation of universal insurance coverage, using private hospital services or some non-covered medical procedures such as dialysis and chemotherapy caused people to deal with catastrophic expenditures (16). The relationship between health services consumption and exposure to catastrophic health expenditures was significant as well in a study conducted in Kermanshah province of Iran (13). This study showed that using drug addiction cessation services (13.5 times), inpatient services (12 times) and outpatient services (3.5 times) caused the households to face with catastrophic expenditures.
Based on findings of the study, there is a significant relationship between household size and confronting with catastrophic health expenditures. Households with 1 to 2 members have faced with catastrophic expenditures more than households with more than 6 members and households with 3 to 5 members. In this regard, a previous Iranian study showed that households with less than five people are facing catastrophic expenditures more likely, although this relationship was not significant (10). In Thailand, there was a very weak correlation found between household size and catastrophic expenditures (19). Yet, study conducted in district 17 of Tehran did not report any relation between household size and confronting catastrophic expenditures (6).
Study limitations
Although the applied technique to measure catastrophic expenditures in this study is one of the most common methods in calculating catastrophic expenditures throughout different countries, it should be considered that households who ignore using health services due to lack of financial ability, households who reduce their food expenses to provide health expenditures and also the opportunity costs (travel costs, the loss of income, etc) due to using health services, will be omitted in this manner. Although budget household survey is claimed to be a nationally and regionally representative survey, but one should be cautious when using the data at provincial level so this part is one of the limitations of the present study when it comes to interpreting the data at provincial level.
Conclusion
Exposure to catastrophic health expenditures in 2008 was 34 households per 1000 households in rural areas and 21 households in urban areas. Determinants of this exposure have been factors such as family size, economic status and health services consumption such as inpatient, outpatient and drug addiction cessation services.
Undoubtedly, it is necessary for planners and policy makers to use findings of such research to develop five-year plans and also for health managers to make developed plans and goals more realistic and more implementable. It seems that inter- and intra sectoral partnerships are required to promote equity in health, to promote economic status of families especially rural ones, to pay attention to social determinants affecting health, to strengthen supervision and fee setting duty of insurance organizations on service providers, and to set realistic and coordinated tariffs between public and private sectors.
Considering the epidemiologic transition and growing number of diseases such as cardiovascular, psychosomatic diseases and traumatic events, which are considered costly diseases, it is necessary to bring community, based medical services from slogan into operation.
Ethical Considerations
Considering that in this research, expenditure –income of households has been used and these data were provided for researchers anonymously, so no particular ethical issue was relevant in this research. Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
We sincerely thank everyone who contributed to our study. We appreciate the employees of Statistical Center of Iran, especially Mr Asmari Joghani and his colleagues in Management and Planning Deputy of General Governor of Kerman. It should be noted that this study has been carried out by sponsorship of Research and Technology Deputy of Kerman University of Medical Sciences. Also, the authors appreciate Farzan Institute for Research and Technology for their useful comments and technical assistance. This paper has been extracted from a BSc thesis in health services administration. The authors declare that there is no conflict of interest.
Annex
For calculating catastrophic expenditure the following formula was used:
Ability to pay of the household (household’s paying capacity) was calculated as follows:
Some households may report their food expenses less than subsistence expenditures and in this case the paying ability of the household is calculated as follows:
Subsistence expenditures are calculated as follows:
- The portion of food expenses of all household’s expenses:
- Modified dimension of household for each household:
- Food expenses of each household on its modified dimension:
Sample households were set based on “the portion of food from all household’s expenses” and then are divided into 100 equal groups. Each of these groups is called percentile. Percentiles 45 and 55 are selected and are called food 45 and food 55, respectively.
- Mean weigh of food expenses at percentile 45 to percentile 55 yields poverty line:
Living expense for each household is calculated as: Seh = pl eq sizeh (3, 12).
References
- 1.Mohesni M. Medical Sociology. 7th edition. Tahoori Library publication; Tehran: 2003. [Persian] [Google Scholar]
- 2.Asefzadeh S, Rezappor A. Health management. 2nd publication. Qazvin University of medical sciences and Hadith rooz Publication; 2008. [Persian] [Google Scholar]
- 3.Xu K, Evans DB, Kawabata K, et al. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–17. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 4.Witter S, Ensor T, Jowett M, Thompson R. Health Economics for Developing Countries: A Practical Guide. New York: Mcmillan education; 2002. p. 181. [Google Scholar]
- 5.Iran’s Ministry of Health Health financing of Islamic republic of Iran in fifth economic, social and cultural development plan. 2009. 8th revision.
- 6.Roberts M, Hsiao W, Berman P, Reich M. Getting Health Reform Right: A Guide to Improving Performance and Equity. 1 edition Oxford University Press; USA: 2003. [Google Scholar]
- 7.Kavosi Z, Rashidian A, Pourmalek F, et al. Measuring Household Exposure to Catastrophic Health Care Expenditures: a Longitudinal Study in Zone 17 of Tehran. Hakim Research Journal. 2009;12:38–47. [Google Scholar]
- 8.Naghavi M, et al. Health services Utilization in Iran, Ministry of health and medical education publication 2005.
- 9.Monograph on the Internet. Lee TJ. Paying out-of-pocket for health care in Korea: change in catastrophic and poverty impact over a decade. 2007. Available: http://www.hsph.harvard.edu/research/takemi/files/RP254_takemi_journal1_lee.pdf.
- 10.Mohammadalizadeh Hanjani H, Fazaeli AA. Equity status in Iran Health system financing. Social Welfare Journal. 2008;5:289–299. [Google Scholar]
- 11.O’Donnell O, van Doorslaer E, Rannan-Eliya RP, et al. Who pays for health care in Asia? J Health Econ. 2008;27(2):460–75. doi: 10.1016/j.jhealeco.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Fazaeli AA. Health financial equity indices trend. 2008. A report to ministry of health and medical education.
- 13.Karami M, Najafi F, Karami M. Catastrophic Health Expenditures in Kermanshah, West of Iran: Magnitude and Distribution. J Res Health Sci. 2009;9(2):36–40. [PubMed] [Google Scholar]
- 14.Got adze G, Zuidze A, Ruhhadze N. Household catastrophic Health expenditure: evidence from Georgia and its policy implications. BMC Health Services Research. 2009;9:69. doi: 10.1186/1472-6963-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun X, Jackson S, Carmichael G, Sleigh AC. Catastrophic medical payment and financial protection in rural China: evidence from the New Cooperative Medical Scheme in Shandong Province. Health Economic. 2009;18(1):103–19. doi: 10.1002/hec.1346. [DOI] [PubMed] [Google Scholar]
- 16.Tin su T, Kouyate B, Flessa S. Catastrophic household expenditure for health care in a low-income society: a study from Nouna district‚ Burkinafaso. Bulletin of the World Health Organization. 2006;84(1):21–27. doi: 10.2471/blt.05.023739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wyszewianski L. Families with catastrophic health care expenditures. Health Serv Res. 1986;21(5):617–34. [PMC free article] [PubMed] [Google Scholar]
- 18.Somkotra T, Lagrada LP. Which Households Are At Risk Of Catastrophic Health Spending: Experience In Thailand After Universal Coverage. Health Affairs. 2009;28:467–78. doi: 10.1377/hlthaff.28.3.w467. [DOI] [PubMed] [Google Scholar]
- 19.Limwattananon S, Tangcharoensathien V, Prakongsai P. Equity in financing healthcare: impact of universal access to healthcare in Thailand. 2005. Report No 16.
- 20.Wagstaff A, Lindelow M. Can insurance increase financial risk? The curious case of health insurance in China. Journal of Health Economics. 2008;27:990–1005. doi: 10.1016/j.jhealeco.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Adhikari SR, Maskay NM, Sharma BP. Paying for hospital based care of Kala-azar in Nepal: assessing catastrophic, impoverishment and economic consequences. Health Policy and Planning. 2009;2009;24:129–39. doi: 10.1093/heapol/czn052. [DOI] [PubMed] [Google Scholar]