Abstract
Background:
Vagal reflex initiated by esophageal stimulation and microaspiration can cause chronic cough in patients with gastroesophageal reflux disease (GERD). By raising intraabdominal pressure, cough can, in turn, predispose to GERD. The role of the upper esophageal sphincter (UES) in preventing esophagopharyngeal reflux during coughing is not well known. The aim of this study was to evaluate the UES response during coughing.
Methods:
We studied 20 healthy young (10 women; age, 27 ± 5 years) and 15 healthy elderly (nine women; age, 73 ± 4 years) subjects. Hard and soft cough-induced pressure changes in the UES, distal esophagus, lower esophageal sphincter, and stomach were determined simultaneously using high-resolution manometry and concurrent acoustic cough recordings.
Results:
Resting UES pressure was significantly higher in the young compared with the elderly subjects (42 ± 14 mm Hg vs 24 ± 9 mm Hg; P < .001). Cough induced a UES contractile response in all subjects. Despite lower UES resting pressures in the elderly subjects, the maximum UES pressure during cough was similar between the young and the elderly subjects (hard cough, 230 ± 107 mm Hg vs 278 ± 125 mm Hg, respectively; soft cough, 156 ± 85 mm Hg vs 164 ± 119 mm Hg, respectively; P not significant for both). The UES pressure increase over baseline during cough was significantly higher than that in the esophagus, lower esophageal sphincter, and stomach for both groups (P < .001).
Conclusions:
Cough induces a rise in UES pressure, and this response is preserved in elderly people. A cough-induced rise in UES pressure is significantly higher than that in the esophagus and stomach, thereby providing a barrier against retrograde entry of gastric contents into the pharynx.
Cough is a complex reflex mechanism necessary to preserve life by mechanically clearing the airways of secretions, foreign bodies, and microorganisms.1 It is also the most common symptom for which patients seek medical attention.2 Several studies have shown that chronic cough can be associated with gastroesophageal reflux disease (GERD).3‐5 The abrupt rise of intraabdominal pressure during cough potentially can overcome the lower esophageal sphincter (LES) barrier, allowing gastric contents to enter the lower esophagus.6,7 In a study by Yapici et al,6 > 50% of the subjects had gastroesophageal reflux during voluntary coughing. Gastroesophageal reflux, on the other hand, can provoke cough either by vagal reflex initiated by distal esophageal stimulation or by microaspiration.7‐11 Hence, there appears to be a close association between cough and gastroesophageal reflux either as cough preceding reflux events or as reflux events preceding cough, as recently shown by simultaneous impedance and acoustic cough recordings in patients with chronic cough.12 Besides generating a pressure gradient between the stomach and the esophagus and, thus, predisposing to gastroesophageal reflux13,14 by abruptly raising intrathoracic pressure, cough can predispose to esophagopharyngeal reflux. Microaspiration of pharyngeal contents has been postulated as one of the mechanisms of chronic cough.7,10‐15 Besides microaspiration, refluxate-induced chronic inflammation and sensitization of peripheral nerves mediating cough in the larynx are also considered mechanisms by which refluxate crossing the upper esophageal sphincter (UES) can cause chronic cough.16
Although the UES has been proposed to protect against entry of esophageal contents into the pharynx, this protective role in preventing esophagopharyngeal reflux during coughing is not well known. The aim of this study was to evaluate the UES response during coughing.
Materials and Methods
This study was approved by the Institutional Review Board, Medical College of Wisconsin (PR000007125; Mechanisms for Prevention of Aspiration). All subjects provided informed and written consent to participate in the study.
Subjects
Twenty healthy young (10 women; age [mean ± SD], 27 ± 5 years) and 15 healthy elderly (nine women; age, 73 ± 4 years) subjects were studied. All subjects completed the Mayo GERD Questionnaire and underwent a medical interview and physical examination. Subjects with symptoms of GERD or upper aerodigestive symptoms (eg, globus, altered taste, change in voice, hoarse voice, cough, throat-clearing, sinus irritation, shortness of breath) were excluded. Only those who never smoked cigarettes or occasionally smoked but stopped > 5 years ago were enrolled. Our previous studies have shown that cigarette smoking can alter the elicitation of aerodigestive reflexes, including the UES response, to pharyngeal stimulation.17,18 We also excluded those who consumed alcohol because our previous study showed that alcohol can also alter UES response.19 Subjects with systemic disorders (diabetes; hypertension; Parkinsonism; neurologic disorders, including previous stroke; and otolaryngology disorders) were excluded. Except for those taking small doses of prophylactic aspirin (in the elderly subject group), subjects taking any other medications were excluded.
Through unsedated transnasal endoscopy screening, our previous study showed abnormal upper gastrointestinal findings in up to 20% of healthy, asymptomatic volunteers.20‐22 Hence, all present study subjects underwent unsedated transnasal endoscopy using the previously described techniques.21 During this examination, the larynx was also examined. The screening endoscopy was performed within 1 week prior to the study. Subjects with abnormal findings were excluded from the study.
Study Protocol
After a 6-h fasting period, subjects were studied in an upright sitting position in a quiet room. The nasal cavity was anesthetized with 2% lidocaine hydrochloride jelly (Akorn, Inc). A solid-state manometry catheter with a 4.2-mm outer diameter and 36 circumferential sensors spaced 1 cm apart (ManoScan 360; Sierra Scientific Instruments, LLC) was passed transnasally and positioned with the proximal manometric sensors lying in the pharynx and distal sensors in the stomach. Subjects were then given a 10-min period to adjust to the catheter before the study was started.
A microphone (Labtec AM-242; Labtec, Inc) was positioned in front of the subject 25 cm (10 in) away from the lower mandible. Each subject was instructed to generate hard-intensity (forceful) and soft-intensity (effortless) cough sounds. Each cough event was repeated three times.
Prior to each cough, subjects were asked to swallow to clear the pharynx of any saliva. During the recording period, they were instructed to refrain from swallowing. The manometric and sound recordings were synchronized, and cough was demarcated (Fig 1).
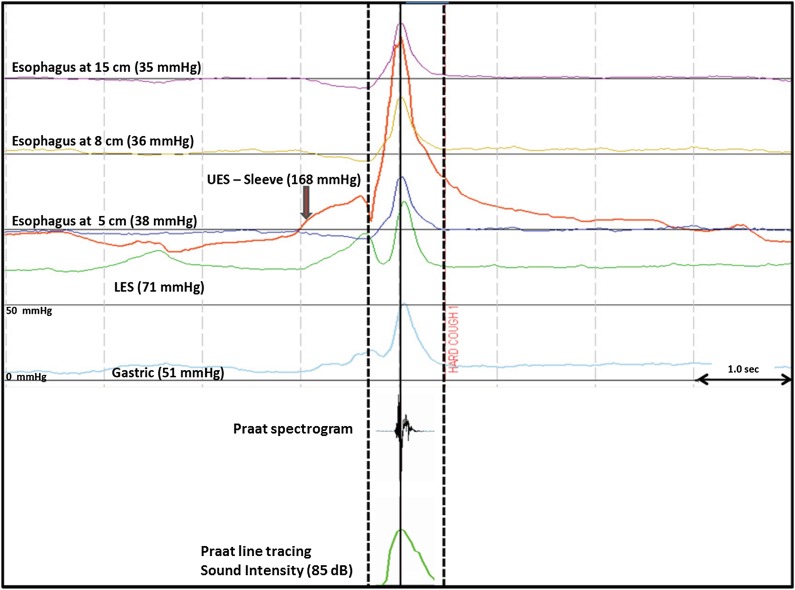
Figure 1.
Example of concurrent manometry line tracing during cough and Praat acoustic cough tracing. The solid-line frame represents the cough event. Intraluminal pressure measurements were noted at peak UES pressure (red line). Sound intensity was measured at the point of maximum intensity (Praat recordings). Each block on the y-axis has a pressure range of 0 to 50 mm Hg. LES = lower esophageal sphincter; UES = upper esophageal sphincter.
Pressure Recording and Measurement
Manometric data were recorded and analyzed using ManoView software (Sierra Scientific Instruments, LLC). All pressure measurements were referenced to atmospheric pressure. We determined the concurrent intraluminal pressures at baseline and during cough at the (1) UES, (2) esophagus, (3) LES, and (4) stomach. Both UES and LES pressures were measured by applying the e-Sleeve function of the ManoView software to obtain the highest pressure irrespective of the axial sphincter excursion during cough. The high-resolution catheter incorporated 36 channels spaced 1 cm apart. These channels record true circumferential pressure, with each channel having 12 pressure sensing points (432 data points). The e-Sleeve function involves placing spatial markers over a region (eg, upper and lower edge of the UES high-pressure zone), and the highest pressure measured from any set of sensors in this region is recorded. Hence, e-Sleeve measures the highest recorded sphincter barrier pressure and rejects artifacts in pressure recordings due to sphincter shortening and sphincter movement.
Baseline UES pressure was measured at the end-expiratory point. During cough, the time point at which the UES pressure reached its maximum value was recorded (Fig 1). At this point, pressure recordings at all other sites were noted.
Cough Sound Recording
Three hard (forceful) and soft (effortless) cough sounds each were recorded for each subject. Cough sound parameters were recorded in real time through a microphone using Audacity free software, version 1.2.6 (http://audacity.sourceforge.net/copyright). Cough sounds were recorded at 44 kHz and were saved in 32-bit (floating-point) samples. The files were exported in wave audio file format to Praat software, version 5.1.17 (Institute of Phonetic Sciences, University of Amsterdam) for intensity analysis. Praat cough sound files were opened as long sound files, and cough intensity was viewed as spectral and line plots. Intensity for each cough sound was measured at the point of maximum intensity for each cough event (Fig 1).
Videofluoroscopic Recordings
To evaluate whether the UES pressure increase was secondary to UES contraction or an artifact related to posterior movement of the larynx compressing the manometric catheter against the spine, we recorded the hyoid movement by videofluoroscopy in five additional healthy volunteers (Fig 2). Videofluoroscopic recordings were performed at 90 keV with 22 cm (9-in) image-intensifier fluoroscopic images at 30 video frames/s (or 60 fields/s) for subsequent analysis.
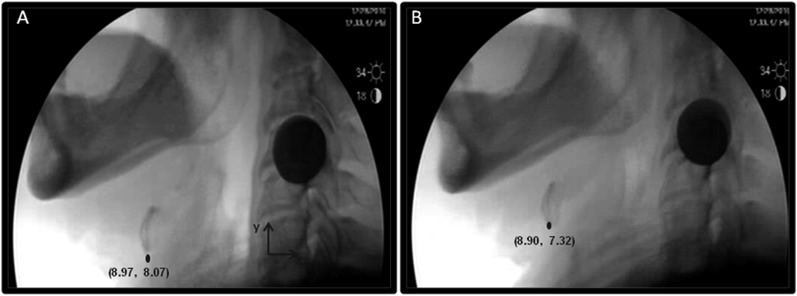
Figure 2.
A, Sagittal view of fluoroscopic images before cough. B, Sagittal view of fluoroscopic images during cough. The spatial location of the hyoid bone is noted with the circle and recorded as Cartesian coordinate pairs relative to a coordinate axis, where y is parallel to the spine. The hyoid bone moves slightly superior and anterior during cough compared with the resting position.
Statistical Analysis
Descriptive statistics are reported as mean ± SD for normally distributed data. When appropriate, logarithmic transformations were performed. The comparison of pressures at different measurement sites before and during cough within groups was done by repeated-measures analysis of variance. The comparison between groups (elderly vs young) was performed with Student t test. For all comparisons, a type I error P < .05 corrected for multiple comparisons when appropriate was considered significant. Two experienced physicians blinded to experimental conditions analyzed the data independently. Interobserver agreement was determined by applying κ statistics.
Results
All subjects completed the study without complications. Transnasal upper gastrointestinal endoscopic evaluation was normal in all. Both the young and the elderly subjects were successful in generating hard- and soft-intensity cough sounds with no discomfort.
The analysis between the young and the elderly groups showed no significant differences in cough intensity (hard cough, 77 ± 9 dB vs 76 ± 11 dB, respectively; soft cough, 67 ± 10 dB vs 65 ± 11 dB, respectively; P not significant). The cough intensity was significantly different between hard and soft cough for both groups (P < .02).
Resting Pressures
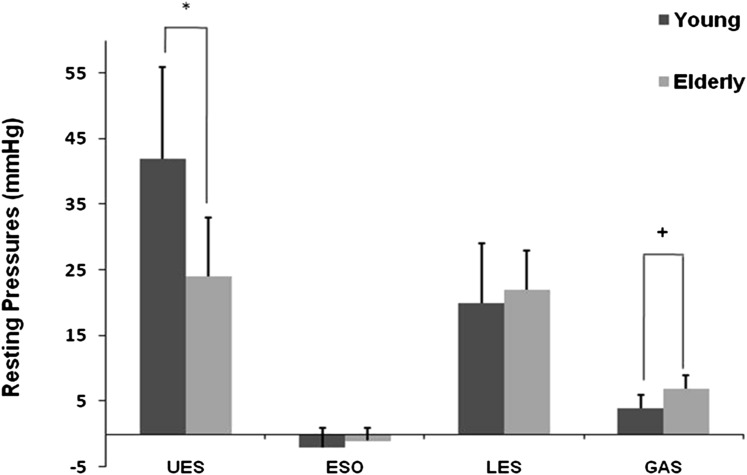
Resting UES pressure was significantly lower in the elderly group than in the young group (42 ± 14 mm Hg vs 24 ± 9 mm Hg, P < .001) (Fig 3). On the other hand, resting intragastric pressure was significantly higher in the elderly group than in the young group (4 ± 2 mm Hg vs 7 ± 2 mm Hg, P < .01) (Fig 3). There was no significant difference in the resting LES and esophageal pressures between the two groups.
Figure 3.
Baseline pressures at different intraluminal sites. Elderly subjects had significantly lower UES pressure and significantly higher gastric pressure. *P < .001; +P < .01 young vs elderly subjects. ESO = esophageal; GAS = gastric. See Figure 1 legend for expansion of other abbreviations.
Cough-Induced Pressure Changes
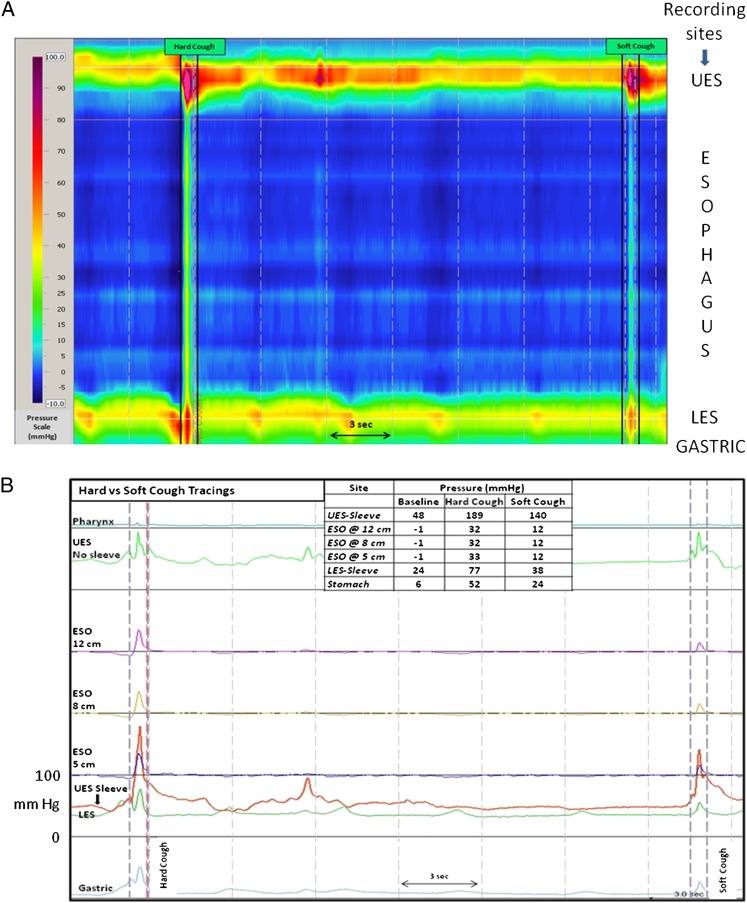
All cough events (hard and soft) in both subject groups resulted in a significant rise in pressure at all recorded sites (stomach, LES, esophagus, UES) compared with baseline values (Table 1). This rise in pressure at all sites in both groups was significantly higher during hard cough than during soft cough (Fig 4, Table 1).
Table 1.
—Pressure Values (mm Hg) at Various Sites During Hard and Soft Cough in the Young and the Elderly Subjects
| Pressure, mm Hg |
|||
| Cough Event | Baselinea,b | Hard Coughc | Soft Cough |
| Young | |||
| UES | 42 ± 14 | 230 ± 107 | 156 ± 85 |
| Esophagus | −2 ± 3 | 55 ± 28 | 26 ± 25 |
| LES | 20 ± 9 | 76 ± 26 | 48 ± 24 |
| Gastric | 4 ± 2 | 62 ± 26 | 34 ± 26 |
| Elderly | |||
| UES | 24 ± 9 | 278 ± 125 | 164 ± 119 |
| Esophagus | −1 ± 2 | 51 ± 24 | 18 ± 14 |
| LES | 22 ± 6 | 91 ± 37 | 44 ± 19 |
| Gastric | 7 ± 2 | 64 ± 25 | 26 ± 11 |
Data are presented as mean ± SD. P value is not significant for young vs elderly subjects. LES = lower esophageal sphincter; UES = upper esophageal sphincter.
P < .001 baseline vs hard cough.
P < .001 baseline vs soft cough.
P < .001 hard vs soft cough.
Figure 4.
Representative example of the effect of hard and soft cough on luminal pressures of the esophagus and its sphincters in a young subject. A, Contour plot. B, Line tracings (each block on the y-axis has a pressure range of 0-100 mm Hg). The dashed frame represents the cough event measured simultaneously at peak pressure in the UES, esophagus, LES, and stomach. See Figure 1 and 3 legends for expansion of abbreviations.
Pressure Increase Over Baseline
Gastric, LES, esophageal, and UES pressure increases above their respective baseline values (δ) were significantly higher during hard cough than during soft cough (Table 2). The δ for UES pressure was significantly higher than that of all other intraluminal sites in both group for both hard and soft cough (P < .001). The cough-induced gastric, LES, esophageal, and UES pressure increases above baseline were similar in young and elderly subjects.
Table 2.
—Rise in Pressure Over Baseline Values (mm Hg) at Various Sites During Hard and Soft Cough in the Young and the Elderly Subjects
| Δ Pressure, mm Hg |
||||||||
| UES |
Esophagus |
LES |
Gastric |
|||||
| Cough Event | Young | Elderly | Young | Elderly | Young | Elderly | Young | Elderly |
| Soft cough | 114 ± 84a,b | 138 ± 120a,c | 27 ± 27b | 19 ± 14b | 30 ± 26b | 22 ± 19c | 29 ± 26b | 19 ± 13b |
| Hard cough | 188 ± 102a | 255 ± 124a | 57 ± 28 | 52 ± 23 | 56 ± 26 | 68 ± 39 | 57 ± 26 | 57 ± 25 |
Data are presented as mean ± SD. P value is not significant for young vs elderly subjects. See Table 1 for expansion of abbreviations.
P < .001 UES vs esophagus, LES, and gastric.
P < .01 soft vs hard cough.
P < .001 soft vs hard cough.
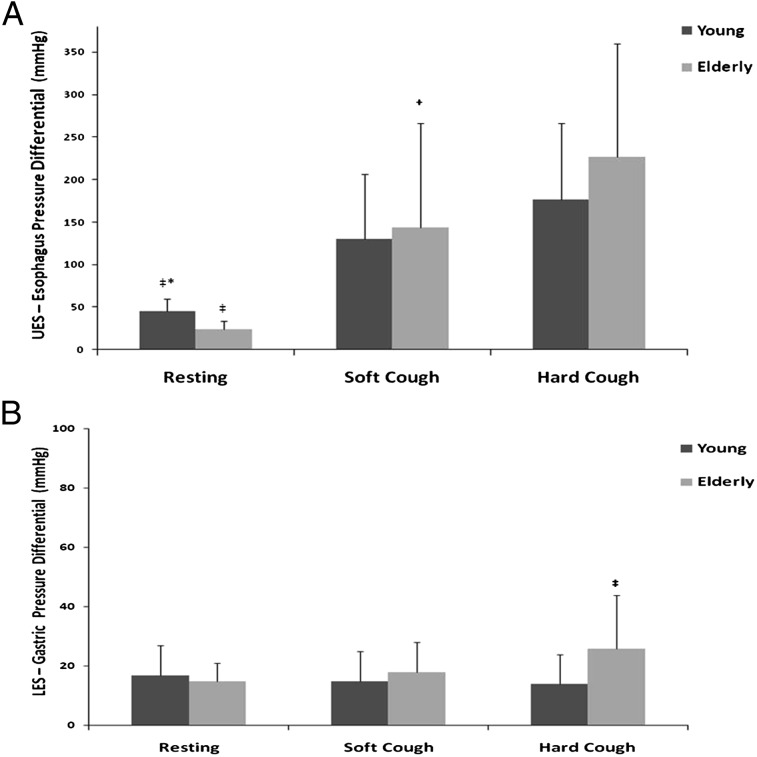
Cough-Induced Pressure Differentials
Because the LES acts like a mechanical barrier to prevent gastric contents from entering the esophagus and, similarly, the UES acts like a mechanical barrier preventing esophageal contents from reaching the pharynx, we calculated the LES to gastric and the UES to esophageal pressure differentials at baseline and during coughing episodes. As shown in Figure 5, similar to the baseline pattern, the UES pressure was always higher than the intraesophageal pressure during hard and soft coughs in both the young and the elderly subjects. A similar pattern was noted with the LES pressure always being higher than the intragastric pressure during cough events in both groups. During hard and soft coughs, the UES − intraesophageal pressure (measured at 8 cm above the LES) differential was significantly higher than that at baseline for both groups. Hard cough led to a significantly larger differential than did soft cough in the elderly subjects (Fig 5A). Compared with the UES, although the LES pressure was always higher than the intragastric pressure, this pressure differential did not significantly change with cough (hard or soft) and was unaffected by age, except for being higher in the elderly subjects compared with the young subjects during hard cough (Fig 5B).
Figure 5.
A, UES − esophagus pressure differential. ‡P < .001 resting vs soft cough and resting vs hard cough for both young and elderly subjects; *P < .001 young vs elderly resting pressures; +P < .05 soft vs hard cough in elderly subjects. B, LES − gastric pressure differential. ‡P < .01 hard cough in young vs elderly subjects; P value not significant for resting vs hard vs soft cough for both young and elderly subjects. See Figure 1 legend for expansion of abbreviations.
Laryngeal Movement During Cough
Five additional subjects were studied with only videofluoroscopy. These separate volunteers did not undergo esophageal manometry study. The sole purpose of this evaluation was to determine whether a rise in UES pressure was due to true UES contractions or secondary to the UES being pushed by laryngeal structures during cough. The hyoid movement during cough was 0.5 ± 0.4 mm in the anterior and 0.6 ± 0.3 mm in the superior directions. None of the cough events was associated with posterior or inferior movement of the hyoid bone (Fig 2).
Interobserver Agreement
Recordings were analyzed by two independent observers. There was a high degree of concordance between the two (κ = 0.9).
Discussion
Cough is needed to preserve life by expelling foreign bodies and microorganisms from the airways.1 It is the most common symptom for which patients seek medical attention.2 The association between cough and gastroesophageal reflux events has been well studied and documented either as cough-inducing reflux or as reflux-inducing cough.3‐16 During cough, contraction of the accessory respiratory muscles and the diaphragm, among other events, create an abrupt increase in intraabdominal and intrathoracic pressures.1 An abrupt rise of intraabdominal pressure can overcome the LES barrier, thereby allowing gastric contents to enter the esophagus.6,7 In one study using scintigraphy, > 50% of the subjects had gastroesophageal reflux during voluntary coughing.6 Gastroesophageal reflux, on the other hand, can provoke cough either by vagal reflex initiated by distal esophageal stimulation or by microaspiration.7‐11 Besides predisposing to gastroesophageal reflux13,14 by abruptly raising intrathoracic pressure, cough can predispose to esophagopharyngeal reflux. Microaspiration of pharyngeal contents has been postulated as one of the mechanisms of chronic cough.7,10‐15 Sensitization of peripheral nerves mediating cough in the larynx is also considered one of the mechanisms by which refluxate crossing the UES can cause chronic cough.16 Hence, cough-induced GERD and GERD-induced cough can potentially create a vicious cycle between GERD and cough. Because the UES high-pressure barrier protects against gastric refluxate entering the pharynx, we evaluated the UES response to cough.
In healthy subjects, gastric refluxate rarely reaches the upper esophagus. Previous studies have shown that only 11% of the gastroesophageal refluxate reaches the proximal esophagus,23 and only 8% enters the pharynx.24 The paucity of proximal reflux events and airway complications is proposed to be due to the presence of protective mechanisms that have been well characterized in the esophagus. Some of these include mechanisms resulting in esophageal acid clearance,25 secondary peristalsis,26 and esophagoglottal reflexes.23 In contrast, the protective role of the UES during coughing has not been systematically studied. To our knowledge, the present study is one of the first to characterize the UES response during various types of cough by using simultaneous manometry and acoustic cough recordings.
The results of the present study indicate that soft and hard cough induce a UES pressure increase that is significantly higher than other intraluminal pressure increases, including the esophagus, LES, and stomach. Hence, the UES functions as a mechanical barrier against entry of esophageal contents into the pharynx. Two mechanisms can explain the disproportionately higher UES pressure increases recorded during cough: (1) neuromuscular UES contractile reflex that could be part of the cough reflex and (2) mechanical compression of the UES by surrounding structures during cough. We excluded the second possibility by studying the laryngeal movements during cough using concurrent videofluoroscopy recordings and showed absence of posterior laryngeal movement during cough. In fact, the hyoid bone moved anteriorly and superiorly during cough, which could have resulted in lowering the UES pressure had it not been for an intrinsic UES contractile response with cough. This contractile response is most likely an integral part of the cough reflex. Similar to our previous reports in healthy young and elderly subjects during phonation events,27,28 this finding suggests the presence of a UES contractile response as part of the cough reflex. To further support this notion, there is electromyographic evidence of contraction of the cricopharyngeus muscle during cough in animal models.29 However, because intraluminal esophageal pressure increased with all cough events in the present study, the possibility of cough inducing an esophago-UES contractile reflex cannot be excluded.
As previously described,28 the baseline UES pressures were different between the young and the elderly subjects. The elderly subjects had significantly lower UES pressures and significantly higher gastric pressures at baseline. Although this could predispose the elderly subjects to gastroesophagopharyngeal reflux, their δ was significantly higher than that in the young subjects, and the absolute UES pressure recordings during soft and hard cough were similar between the groups. Moreover, the pressure gradients that prevent transit of gastric contents into the pharynx, namely the UES > esophagus and LES > gastric, were maintained in the elderly subjects and was similar to that in the young subjects. Hence, in contrast to aging-related deterioration of some other UES aerodigestive-protective mechanisms,30,31 the UES response to cough is preserved in elderly people despite a significantly lower resting UES pressure.
The magnitude of the pressure increase in the stomach, LES, esophagus, and UES was significantly higher for hard cough than for soft cough in both the young and the elderly subjects. This finding suggests that pressure responses in the upper GI tract during cough depend on the intensity of the cough efforts. However, except for the rise in UES pressure for reasons described previously, it is not clear whether the rise in pressures at other sites are related to intrinsic muscle contractile response, extrinsic factors (ie, abdominal muscles, intercostal muscles, diaphragm), or both.
In summary, cough elicits a UES contractile response that could be an integral part of the cough reflex. Rise in UES pressure is higher with hard cough than with soft cough. Despite significant increases in intragastric and intraesophageal pressures during coughing spells, the magnitude of rise in UES pressure is proportionally much higher than that in intragastric and intraesophageal pressures, thereby maintaining a strong pressure barrier to entry of gastric and esophageal contents into the pharynx and thus protecting the airways. Despite a significantly lower basal tone, the UES contractile response to cough is preserved in elderly people.
Acknowledgments
Author contributions: Dr Shaker had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Amaris: contributed to procedure performance, data collection, data analysis, and writing of the manuscript.
Dr Dua: contributed to the study concept and design, procedure performance, data collection, data analysis, and writing of the manuscript.
Dr Naini: contributed to procedure performance, data collection, data analysis, and writing of the manuscript.
Dr Samuel: contributed to reanalyzing the data to determine interobserver variability (κ value).
Dr Shaker: contributed to the study concept and design and writing of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsor: The sponsors had no role in the design of the study, the collection and analysis of the data, or in the preparation of the manuscript.
Abbreviations
- GERD
gastroesophageal reflux disease
- LES
lower esophageal sphincter
- UES
upper esophageal sphincter
Footnotes
Part of this work was presented at the 18th Annual Dysphagia Research Society Annual Meeting, held on March 3-6, 2010, in San Diego, CA.
Funding/Support: This work is supported in part by National Institutes of Health [Grants 1P01DK068051-01A1 and 5RO1DK025731].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.McCool FD. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):48S-53S [DOI] [PubMed] [Google Scholar]
- 2.Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001-02. Vital Health Stat. 2006;13(159):1-66 [PubMed] [Google Scholar]
- 3.Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54(4):449-454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irwin RS, Curley FJ, French CL. Chronic cough. The spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Am Rev Respir Dis. 1990;141(3):640-647 [DOI] [PubMed] [Google Scholar]
- 5.Palombini BC, Villanova CA, Araújo E, et al. A pathogenic triad in chronic cough: asthma, postnasal drip syndrome, and gastroesophageal reflux disease. Chest. 1999;116(2):279-284 [DOI] [PubMed] [Google Scholar]
- 6.Yapici O, Basoglu T, Canbaz F, Sever A. The role of coughing as a gastroesophageal-reflux provoking maneuver: the scintigraphical evaluation. Nucl Med Commun. 2009;30(6):440-444 [DOI] [PubMed] [Google Scholar]
- 7.Smith J, Woodcock A, Houghton L. New developments in reflux-associated cough. Lung. 2010;188(suppl 1):81-86 [DOI] [PubMed] [Google Scholar]
- 8.Kollarik M, Brozmanova M. Cough and gastroesophageal reflux: insights from animal models. Pulm Pharmacol Ther. 2009;22(2):130-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurski RR, da Rosa AR, do Valle E, de Borba MA, Valiati AA. Extraesophageal manifestations of gastroesophageal reflux disease. J Bras Pneumol. 2006;32(2):150-160 [DOI] [PubMed] [Google Scholar]
- 10.Paterson WG, Murat BW. Combined ambulatory esophageal manometry and dual-probe pH-metry in evaluation of patients with chronic unexplained cough. Dig Dis Sci. 1994;39(5):1117-1125 [DOI] [PubMed] [Google Scholar]
- 11.Wiener GJ, Tsukashima R, Kelly C, et al. Oropharyngeal pH monitoring for the detection of liquid and aerosolized supraesophageal gastric reflux. J Voice. 2009;23(4):498-504 [DOI] [PubMed] [Google Scholar]
- 12.Smith JA, Decalmer S, Kelsall A, et al. Acoustic cough-reflux associations in chronic cough: potential triggers and mechanisms. Gastroenterology. 2010;139(3):754-762 [DOI] [PubMed] [Google Scholar]
- 13.Dent J, Holloway RH, Toouli J, Dodds WJ. Mechanisms of lower oesophageal sphincter incompetence in patients with symptomatic gastrooesophageal reflux. Gut. 1988;29(8):1020-1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ing AJ, Ngu MC, Breslin AB. Pathogenesis of chronic persistent cough associated with gastroesophageal reflux. Am J Respir Crit Care Med. 1994;149(1):160-167 [DOI] [PubMed] [Google Scholar]
- 15.Pellegrini CA, DeMeester TR, Johnson LF, Skinner DB. Gastroesophageal reflux and pulmonary aspiration: incidence, functional abnormality, and results of surgical therapy. Surgery. 1979;86(1):110-119 [PubMed] [Google Scholar]
- 16.Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101(4 pt 2):(suppl 53):1-78 [DOI] [PubMed] [Google Scholar]
- 17.Dua K, Bardan E, Ren J, Sui Z, Shaker R. Effect of chronic and acute cigarette smoking on the pharyngo-upper oesophageal sphincter contractile reflex and reflexive pharyngeal swallow. Gut. 1998;43(4):537-541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dua K, Bardan E, Ren J, Sui Z, Shaker R. Effect of chronic and acute cigarette smoking on the pharyngoglottal closure reflex. Gut. 2002;51(6):771-775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dua KS, Surapaneni SN, Santharam R, Knuff D, Hofmann C, Shaker R. Effect of systemic alcohol and nicotine on airway protective reflexes. Am J Gastroenterol. 2009;104(10):2431-2438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dua KS, Surapaneni SN, Hafeezullah M, Reddy N, Tatro L, Shaker R. Prevalence of abnormal upper GI findings in apparently healthy volunteers enrolled for research studies. Gastrointest Endosc. 2009;69(5):B350-AB351 [Google Scholar]
- 21.Siwiec RM, Dua K, Surapaneni SN, Hafeezullah M, Massey BT, Shaker R. Unsedated transnasal endoscopy with ultrathin endoscope as a screening tool for research studies. Laryngoscope. 2012;122(8):1719-1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shaker R, Saeian K. Unsedated transnasal laryngo-esophagogastroduodenoscopy: an alternative to conventional endoscopy. Am J Med. 2001;111(8 suppl 1):153-156 [DOI] [PubMed] [Google Scholar]
- 23.Shaker R, Milbrath M, Ren J, et al. Esophagopharyngeal distribution of refluxed gastric acid in patients with reflux laryngitis. Gastroenterology. 1995;109(5):1575-1582 [DOI] [PubMed] [Google Scholar]
- 24.Emerenziani S, Cicala M, Zhang X, et al. Effect of oesophagitis on proximal extent of gastro-oesophageal reflux. Neurogastroenterol Motil. 2007;19(6):459-464 [DOI] [PubMed] [Google Scholar]
- 25.Ing AJ, Ngu MC, Breslin AB. Chronic persistent cough and clearance of esophageal acid. Chest. 1992;102(6):1668-1671 [DOI] [PubMed] [Google Scholar]
- 26.Shaker R. Airway protective mechanisms: current concepts. Dysphagia. 1995;10(4):216-227 [DOI] [PubMed] [Google Scholar]
- 27.Perera L, Kern M, Hofmann C, et al. Manometric evidence for a phonation-induced UES contractile reflex. Am J Physiol Gastrointest Liver Physiol. 2008;294(4):G885-G891 [DOI] [PubMed] [Google Scholar]
- 28.Schneeberger B, Perera L, Surapaneni SN, Kuribayashi S, Dua K, Shaker R. Phonation-induced UES Contractile Reflex is Preserved in the Elderly. Gastroenterology. 2009;136(5):(suppl 1):A-468 [Google Scholar]
- 29.Lang IM, Marvig J, Sarna SK. Electromyography (EMG) of the pharyngo-esophageal junction (PEJ) during various physiologic states. Gastroenterology. 1998;94:249A [Google Scholar]
- 30.Shaker R, Ren J, Bardan E, et al. Pharyngoglottal closure reflex: characterization in healthy young, elderly and dysphagic patients with predeglutitive aspiration. Gerontology. 2003;49(1):12-20 [DOI] [PubMed] [Google Scholar]
- 31.Shaker R, Ren J, Podvrsan B, et al. Effect of aging and bolus variables on pharyngeal and upper esophageal sphincter motor function. Am J Physiol. 1993;264(3 pt 1):G427-G432 [DOI] [PubMed] [Google Scholar]