Abstract
Anxiety is common among adolescents with autism spectrum disorders (ASD) and may amplify the core social disability, thus necessitating combined treatment approaches. This pilot, randomized controlled trial (RCT) evaluated the feasibility and preliminary outcomes of the Multimodal Anxiety and Social Skills Intervention (MASSI) program in a sample of 30 adolescents with ASD and anxiety symptoms of moderate or greater severity. The treatment was acceptable to families, subject adherence was high, and therapist fidelity was high. A 16% improvement in ASD social impairment (within-group effect size = 1.18) was observed on a parent-reported scale. Although anxiety symptoms declined by 26%, the change was not statistically significant. These findings suggest MASSI is a feasible treatment program and further evaluation is warranted.
Keywords: autism, anxiety, adolescence, treatment
Autism Spectrum Disorder (ASD) is a group of heterogeneous conditions with social disability as the core feature. These conditions are now recognized as more common than previously believed, and the rise in detected prevalence of ASD has been most pronounced among those without intellectual disability (Honda, Shimizu, Imai, & Nitto, 2005; Kim et al., 2011; US CDC, 2012). There is growing appreciation for the co-occurrence of other psychiatric conditions (Witwer & Lecavalier, 2010), especially the anxiety disorders, in cognitively higher functioning youth with ASD (deBruin et al., 2007; Joshi et al., 2010). The prevalence of anxiety problems in school-age children and adolescents with ASD is in the range of 40% to 45% (White, Oswald, Ollendick, & Scahill, 2009), considerably higher than prevalence of anxiety disorders in epidemiological studies of children and adolescents in the general population (5 – 10%, see Costello, Egger, & Angold, 2004; 31.9%, see also Merikangas et al., 2010).
Historically, the social disability in ASD has been presumed to be due to indifference or lack of social motivation. However, emerging evidence from neuroimaging, psychophysiological, and behavioral studies suggests that social disability is associated with heightened arousal and avoidance of social stimuli at least for some youth with ASD (Dalton, Nacewicz, Alexander, & Davidson, 2007; Joseph, Ehrman, McNallly, & Keehn, 2008). Heightened arousal, especially in response to social-emotional information (Joseph et al., 2008, Kyllianinen & Hietanen, 2006), may impede accurate interpretation of social cues and appropriate responses to others. These observations suggest that the presence of anxiety contributes to social disability (e.g., Kleinhans et al., 2010; Myles, Barnhill, Hagiwara, Griswold, & Simpson, 2001) and social disability (awkward, unsuccessful or negative interactions with others) contributes to heightened anxiety (e.g., Bellini, 2006). This bi-directional model is at the crux of the treatment program we developed and evaluated in the present trial, the Multimodal Anxiety and Social Skills Intervention (MASSI) program.
Whatever the reason for the common co-occurrence of ASD and anxiety disorders, determining anxiety disorder diagnoses for children with ASD is complicated by language and cognitive delays present in many of these youth. Even those with language may struggle to describe their internal experiences in a manner that contributes to the clear diagnosis of anxiety disorders (Joshi et al., 2010; Leyfer et al., 2006). Further complicating differential diagnosis is the overlap among anxiety disorders in typically developing children and adolescents (Leyfer et al., 2006; Walkup et al., 2008). Evidence from treatment studies of youth with anxiety disorders uncomplicated by ASD suggests that primary diagnosis does not moderate outcomes. Specifically, cognitive-behavioral therapy (CBT) programs are effective across Social Phobia (SoP), Specific Phobia (SP), Separation Anxiety Disorder (SAD), and Generalized Anxiety Disorder (GAD) (e.g., Barrett et al., 1996; Kendall et al., 1997; Kendall et al., 2008; Ollendick et al., 2009; Silverman et al., 1999; Walkup et al., 2008). Accordingly, MASSI targets anxiety broadly and measures outcomes dimensionally.
MASSI, described in detail elsewhere (omitted for masked review), is a CBT program that targets concurrent anxiety and social disability in adolescents with ASD via individual therapy, group social skills training, and parent coaching. It was developed specifically for adolescents with high functioning autism spectrum disorders (HFASD) accompanied by moderate or greater anxiety problems. The ‘dual focus’ in treatment is based on the notion that unaddressed anxiety problems can undermine the benefits that might otherwise be realized with a ‘pure’ social skills intervention (White, Koenig, & Scahill, 2010). Adolescents with high levels of anxiety may be less able to make use of the social skills training, avoid opportunities to practice newly learned social skills, or both. Likewise, if the social disability is due to a skill deficit, addressing only anxiety may not lead to improved social competence. In the absence of age-appropriate social skills and sufficient practice opportunities to achieve fluency, the young person might continue to behave in ways that draw unwanted attention and lead to negative reactions from others, thereby potentially increasing anxiety. Unfortunately, as the child with ASD and his peer group age, behavioral oddities and social awkwardness may become more obvious and less tolerated. The adolescent’s behavior may contribute to negative attitudes and even ridicule from peers (Campbell, Ferguson, Herzinger, Jackson, & Marino, 2004; Harnum, Duffy, & Ferguson, 2007; Ochs, Kremer-Sadlik, Solomon, & Sirota, 2001; Shtayermman, 2007; Swaim & Morgan, 2001).
This picture may be especially true for social anxiety, in which anxiety may be heightened by the adolescents’ self-perceived difference between themselves and typically developing age-mates. Heightened anxiety in the social domain may contribute to avoidance and additional social delay. Falling behind age mates in social development in the social domain may perpetuate the adverse interaction between anxiety and social disability in ASD due to reduced opportunities to acquire social skills. Finally, although social disability is present across the full range of youth with ASD, higher functioning adolescents (typically defined based on assessed IQ above 70 and verbal fluency) with ASD are often aware of their deficits, which may amplify their anxiety (Klin & Volkmar, 2000; Tse, Strulovich, Tagalakis, Meng, & Fombonne, 2007; Witwer & Lecavalier, 2010; White et al., 2009).
No other treatment program, to our knowledge, has been designed to target anxiety and the social deficits of ASD concurrently in adolescents who are higher functioning. Although some studies have included elements of social skills training in anxiety CBT protocols for ASD (social coaching; Wood et al., 2009), most CBT programs have focused on anxiety reduction and have not measured social disability as an outcome (Chalfant, Rapee, & Carroll, 2007; Reaven et al., 2009; Sofronoff, Attwood, & Hinton, 2005; Wood, Drahota, Sze, Chiu, & Langer, 2009). Similarly, a study involving intensive social skills training in children (age 7 – 11) with ASD found improved knowledge of anxiety- and anger-management strategies, but the study did not target or directly assess symptoms of anxiety (Beaumont & Sofronoff, 2008). In addition, despite evidence that anxiety may be especially prominent during adolescence (Tse, Strulovich, Tagalakis, Meng, & Fombonne, 2007; White et al., 2009; Witwer & Lecavalier, 2010), intervention research in this area has not specifically focused on adolescents.
The initial iteration of the MASSI program was delivered to four adolescents with HFASD and at least moderate levels of anxiety. Three of the four youth showed reduced anxiety and all four demonstrated significant improvements in social functioning (omitted for masked review). Changes were made to the content and delivery of the program following this case series based on therapist input and feedback from the participants and their families. The purpose of the current pilot RCT was to determine if future study is warranted (cf., Leon, Davis, & Kraemer, 2011) by examining the feasibility of the program and preliminary results related to its efficacy. The focus on feasibility, rather than efficacy, is consistent with the step-wise approach to treatment development and recommendations about the role of pilot RCTs (Kraemer, Minitz, Noda, Tinklenberg, & Yesavage, 2006; Leon et al., 2011; Smith et al., 2007). We define feasibility as evidence that the treatment is acceptable to the patient population and that it can be reliably delivered. This is distinct from efficacy, which entails formal statistical comparison of outcomes across two or more treatments (cf., Chambless & Hollon, 1998).
Methods
Design
The study was approved by the institutional review board at the first author’s institution. Participants were recruited primarily through a university-affiliated clinic specializing in the treatment of ASD. In addition, area clinicians, clinics, schools, and media advertisements were used as referral sources. After determining eligibility (see later), participants were randomly assigned to receive the 14-week intervention immediately or to a Wait-List (WL) control condition of equal length, after which time they were offered the intervention. Enrollment into the study took place over a two-year period, from October 2008 through October 2010.
All families contacting the clinic with interest in the study were screened via a brief telephone interview. Subjects who appeared eligible for the study were invited for in-person assessment. During the clinic visit, consent was obtained and subjects were evaluated for eligibility.
Because MASSI includes simultaneous delivery of individual and group treatment, randomization occurred within groups of six participants (i.e., 3 subjects randomly assigned to active treatment and 3 to waitlist). To accumulate the study sample of 30, we enrolled five waves of six adolescents. Once a group of six participants meeting inclusion criteria was assembled, they were asked to return to the clinic for baseline assessment and random assignment. Random assignment was done by a person unaffiliated with the study who drew the names from a box. Once all study measures were completed at the baseline visit, the subject and family were informed about their treatment assignment (MASSI or WL). For each wave of 6 subjects, baseline measures were collected over a one-week period. Similarly, outcome measures were collected within five days of the treatment (or waitlist) endpoint. These groups were created sequentially, with no attempt made to affect group composition. As such, each treatment group of four (three with ASD and one non-ASD peer tutor) was fairly heterogeneous (e.g., participants of different ages and gender).
Participants
Inclusion and exclusion criteria
To be eligible for the study, participants had to be between the ages of 12 and 17 years, have an ASD diagnosis supported by the ADOS (Lord et al., 2002) and ADI-R (Lord et al., 1994), and meet diagnostic criteria for at least one of four anxiety disorders, SoP, GAD, SP, or SAD, as determined by the ADIS-C/P (Table 1). Youth also had to have a current verbal IQ of 70 or above and no previous diagnosis of intellectual disability. Concomitant psychiatric medication was permitted if the dose was stable for at least four weeks with no planned changes for the duration of the randomized trial.
Table 1.
Demographic and diagnostic information by group
| MASSI | WL | Full | χ2 / t | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Sex (male) | 11 (73%) | 12 (80%) | 23 (77%) | .19 |
| Latino/Hispanic | 0 | 1 | 1.03 | |
| Race | 2.15 | |||
| Caucasian | 12 (80%) | 14 (93%) | 26 (87%) | |
| Asian/Pacific Islander | 1 (7%) | 0 (0%) | 1 (.03%) | |
| African American | 1 (7%) | 1 (7%) | 2 (.07%) | |
| Pacific Islander | 1 (7%) | 0 (0%) | 1(.03%) | |
| Multiracial | 0 (0%) | 0 (0%) | 0 (0%) | |
| ASD diagnosis | 4.85 | |||
| Autism | 3 (20%) | 7 (47%) | 10 (33%) | |
| Aspergers | 11 (73%) | 5 (33%) | 16 (53%) | |
| PDD-NOS | 1 (7%) | 3 (20%) | 4 (13%) | |
| Baseline anxiety disordera | ||||
| SoP | 11 (73%) | 12 (80%) | 23 (77%) | .19 |
| GAD | 10 (67%) | 9 (60%) | 19 (63%) | .14 |
| SP | 9 (60%) | 7 (47%) | 16 (53%) | .54 |
| SAD | 0 (0%) | 1 (7%) | 1(.03%) | 1.03 |
| OCD | 3 (20%) | 1 (7%) | 4(13%) | 1.15 |
| PD/Agor | 0 (0%) | 1 (7%) | 1(.03%) | 1.03 |
| PTSD | 0 (0%) | 1 (7%) | 1(.03%) | 1.03 |
| M(SD) | M(SD) | M(SD) | ||
| Age (in months) | 170 (14 yrs) | 180 (15 yrs) | 175 (15 yrs) | 1.49 |
| Verbal IQ | 100.07(16.49) | 94.07(11.92) | 97.07(14.46) | 1.14 |
| Vineland | ||||
| Communication | 75.00(8.23) | 75.87(17.44) | 75.43(13.30 | .17 |
| Daily living skills | 75.87(18.04) | 80.93(14.01) | 78.40(16.08) | .86 |
| Socialization | 68.60(11.95) | 65.80(9.33) | 67.20(10.63) | .72 |
| Adaptive behavior composite | 71.40(10.52) | 72.27(11.02) | 71.83(10.60) | .22 |
Note. χ2 / t: between-group (MASSI and WL) comparison at baseline.
SoP: Social Phobia; GAD: Generalized Anxiety Disorder; SAD: Separation Anxiety Disorder; OCD: Obsessive-Compulsive Disorder; SP: Specific Phobia; PD/Agor: Panic Disorder with Agoraphobia; PTSD: Post-Traumatic Stress Disorder.
Baseline anxiety disorder: based on ADIS-C/P CSR of 4 or higher; no participants met criteria for PD without Agoraphobia or Agoraphobia without panic.
Adolescents with a primary (i.e., most severe or impairing) diagnosis of Obsessive-Compulsive Disorder (OCD), Panic Disorder (PD), Panic Disorder with Agoraphobia (PD/Ag), or Agoraphobia without Panic Disorder (Ag-PD) were excluded. Some of these disorders require more specialized types of CBT (e.g., exposure with response prevention for OCD), and little is known about the presentation or treatment of others (e.g., Ag-PD) in ASD. However, several participants had multiple anxiety disorders (e.g., SoP and OCD) (Table 1). Adolescents with serious behavioral problems (e.g., frequent tantrums or aggression) were also excluded. All potential participants who were excluded were provided with referrals.
Intervention Program and Implementation
Therapists
The principal investigator (XX) and four doctoral students in a clinical psychology program served as MASSI therapists. All student therapists were trained and supervised by the principal investigator, a licensed clinical psychologist. Prior to delivering the study treatment, therapists read study-related materials including relevant research and clinical articles and the MASSI manual, and watched every MASSI module (recorded sessions from previous participants treated by the principal investigator) - individual as well as group sessions. The content and recorded sessions were discussed in supervision before the therapist was considered ready to deliver the session. In addition, video recordings for each therapist’s first MASSI case were reviewed and the therapist received written and oral feedback on implementation and fidelity of individual sessions before delivering the next session. This approach ensured that identified problems could be corrected in a timely manner.
Intervention
MASSI (see [omitted for masked review], for fuller description) is a manual-based modular treatment program delivered via three modalities – individual therapy (up to 13 sessions), group therapy (skills practice, 7 sessions), and parent education and coaching (after each individual therapy session). Individual therapy sessions were approximately 60 – 70 minutes in length, with the inclusion of parents toward the end of each session for approximately 15 minutes. The group meetings each lasted 75 minutes. Each participant had his or her own identified clinician for individual therapy sessions; this therapist also co-led the participant’s group sessions. Thus, for each cohort of three MASSI participants, there were two therapists.
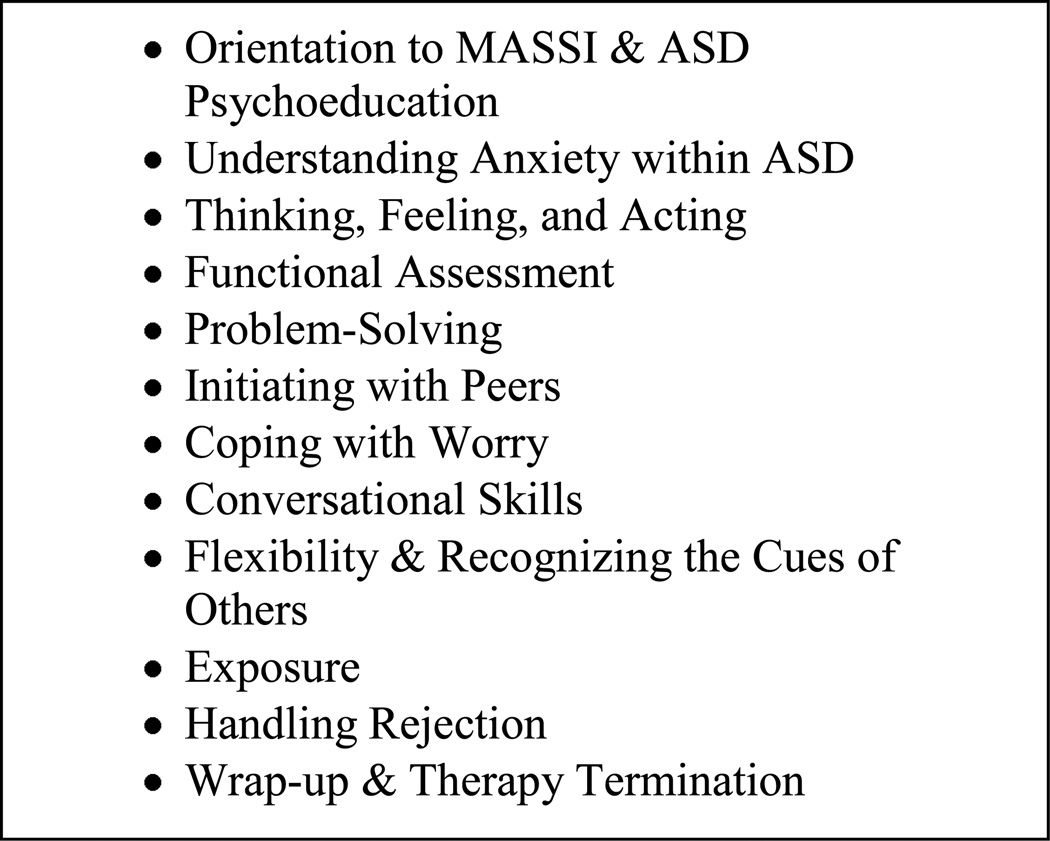
A treatment specific case conceptualization was developed after the third individual session and treatment proceeded to address the subject-specific anxiety symptoms and social skill deficits. To maximize flexibility, therapists selected appropriate treatment modules for the individual sessions from the MASSI manual based on the subject’s anxiety symptoms and the most impairing social difficulties (similar to the approach recommended by Chorpita, 2007). Modules could be repeated as needed for any given participant (see Figure 2 for listing of individual treatment modules).
Figure 2.
MASSI Individual therapy modules
The content of the seven group sessions was the same for all participants, as the skills covered (e.g., how to join into peer groups) have broad applicability for adolescents with ASD. In each group of three subjects with an ASD, there was one unaffected peer tutor (volunteer of similar age from the community), who offered age-appropriate modeling and feedback to the MASSI participants. The MASSI individual sessions also promoted social skills development. The decision to build an integrated intervention (i.e., group sessions delivered along with individual sessions) was based on the assumption that combined treatment would protect against attrition and promote more rapid improvement than sequential treatment. Although a full description of the treatment manual is beyond the scope of this paper (for fuller description, see XX), the content was based on the principles of CBT and applied behavior analysis.
Subject involvement
Therapists recorded attendance, and rated the subjects’ in-session participation (1 = uninvolved in session, 2 = minimally involved, 3 = moderately involved, 4 = actively involved) and homework completion after each individual session.
Subject satisfaction
At the final individual treatment session, parents and adolescents were asked to rate their satisfaction with the program as a whole (i.e., all components together) on a Likert scale ranging from 1 (not at all helpful) to 10 (very helpful). All ratings were completed in private without the therapist in the room and, once completed, were placed in an envelope sealed by the parent. They were also asked to rank order the individual components (i.e., individual sessions, group meetings, between-session assignments, psychoeducation) based on how helpful each aspect was to them.
Fidelity
At the conclusion of each individual and group therapy session, therapists rated their fidelity to the manual on a checklist reflecting key elements for that session. Therapists were also asked to indicate if homework from the previous session was reviewed and whether it was completed as planned. All therapy sessions were video-recorded, and 40% (14 of 35) of group and 14% (25 of 180) of individual therapy sessions were reviewed and independently coded for fidelity by trained coders. Video-recorded sessions for reliability were selected to ensure that every group therapy module and individual therapy module was reviewed at least once, and that each therapist was reviewed on at least two different individual modules. Coders made their ratings blind to the therapists’ ratings of fidelity. Adverse events spontaneously reported by parents, adolescent participants, or therapists were logged and reviewed by the first author.
Measures
Subject Characterization
Autism Diagnostic Interview-Revised (ADI-R; Lord et al., 1994)
The ADI-R is a structured parent interview used to support a clinical impression of autism. The ADI-R has excellent reliability and validity for the diagnosis of autism (Rutter, Le Couteur, & Lord, 2003), but the algorithm does not extend to other types of ASD such as Asperger’s disorder and pervasive developmental disorder-not otherwise specified. The interviewers in this trial were trained to reliability (i.e., >80% agreement with a reliable coder).
Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2002)
The ADOS is a semi-structured, observational assessment of communication, social interaction, and imaginative play. The ADOS is conducted with the adolescent and maps directly onto diagnostic criteria for ASD. Algorithm scores for communication and socialization are calculated to support an ASD diagnosis. All examiners were trained to reliability standards for administration and scoring (i.e., >80% agreement with a reliable coder).
Anxiety Disorders Interview Schedule for Children/Parents (ADIS-C/P; Silverman & Albano, 1996)
The ADIS-C/P is a semi-structured clinician-rating of DSM-IV anxiety disorders in childhood and adolescence. Based on an interview of the parent and adolescent, the clinician assigns an anxiety disorder diagnosis and an overall rating of severity (the Clinician Severity Rating; CSR) on a 9-point scale. CSRs of four or higher exceed the diagnostic threshold. Psychometric properties such as test-retest reliablity (Silverman, Saavedra, & Pina, 2001) and concurrent validity (Wood, Piacentini, Bergman, McCracken, & Barrios, 2002) of the ADIS-C/P are well established in samples of typically developing children. Similar to modifications made by Leyfer et al. (2006), clinicians administering the ADIS-C/P were mindful of the symptom overlap between ASD and anxiety disorders For instance, avoidance of social situations was coded as an anxiety symptom only if it was related to fear of evaluation rather than disinterest in social situations. All interviewers were trained to reliability, which included observation and administration alongside a reliable administrator of at least four ADIS interviews, to reach agreement (i.e., within one point) on assigned CSRs; under the direction of one of the ADIS developers. Given the questionable validity of self-reports in determining concurrent psychiatric symptoms in youth with an ASD, even among higher functioning adolescents (Mazefsky, Kao, & Oswald, 2011; White, Schry, & Maddox, 2012), the parent and adolescent were interviewed jointly for the ADIS, in keeping with the recommendation of Mazefsky and colleagues (2012).
Vineland Adaptive Behavior Scales-Second Edition (Sparrow, Cicchetti, & Balla, 2005)
The Vineland is a parent-report measure designed to measure the child’s competence in communication, daily living skills, and socialization. Used extensively in studies of children with developmental disabilities, the Vineland has excellent reliability and validity (Sparrow et al., 2005).
Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999)
The WASI is a reliable and valid measure of intelligence. Only the two verbal subtests (Vocabulary and Similarities) were administered to ensure that participants had adequate verbal ability to participate in the CBT program and understand questionnaire instructions.
Outcome Measures
Social Responsiveness Scale (SRS; Constantino & Gruber, 2005)
Given the dual treatment focus of MASSI, two primary outcome measures were used to measure change in social skill and anxiety domains. Completed by the parent or caregiver, the 65-item SRS is scored from 1 (not true) to 4 (almost always true). Higher scores on the SRS Total score reflect greater severity of social disability. Internal consistency on the Total score is excellent (.97, Constantino & Gruber, 2005). The SRS was selected as the primary measure of change because of its well established validity as a dimensional measure of severity of core ASD-related problems (i.e., in the domains of social behavior, social communication, restricted interests and unusual behaviors). Although it has not been widely used as an outcome measure, there is emerging evidence that it is sensitive to change with treatment of people with ASD (Bass, Duchowny, & Llabre, 2009; Lopata et al., 2010; White et al., 2010).
Child and Adolescent Symptom Inventory-4 ASD Anxiety Scale (CASI-Anx; Sukhodolsky et al., 2008)
As in typically developing children with anxiety disorders, we predicted that our adolescents would have more than one anxiety disorder (see Walkup et al., 2008). Thus, change in anxiety symptoms was approached dimensionally and not linked to a specific disorder. The primary outcome measure of anxiety symptoms was the 20-item CASI-Anxiety scale. These items were drawn from a larger pool of anxiety items in the Child and Adolescent Symptom Inventory-4 (Gadow & Sprafkin, 1997, 1998). The full CASI asks the parent (primary caregiver) to rate 132 DSM-IV based items on a 0 to 3 scale (0 = never, 1 = sometimes, 2 = often, and 3 = very often). The CASI-Anxiety scale has internal consistency of 0.85 and little or no overlap with symptoms of ASD (Sukhodolsky et al., 2008). Although it has not been used previously as an outcome measure, it contains DSM-IV based items across a range of anxiety disorders, which conceivably would change with effective treatment.
Pediatric Anxiety Rating Scale (PARS; Research Units on Pediatric Psychopharmacology; Anxiety Study Group, RUPP, 2002)
The PARS is a dimensional rating designed to assess symptoms across SAD, SoP, and GAD (RUPP, 2002). The first section includes 50 specific anxiety symptoms rated as present or absent over the previous week. In the second section, the clinician rates symptom severity for the past week on a six-point scale (0 = none, 5 = extreme) across seven different dimensions (number of endorsed symptoms, frequency, severity of distress, severity of physical symptoms, avoidance, interference at home, and interference out of home). In the original study (RUPP Anxiety Group, 2002) scores from five of the seven severity domains were summed to derive the total score. The number of symptoms domain was not included, because the developers of the scale surmised that this dimension was not related to anxiety severity. There was additional concern that side effects from the study drug (fluvoxamine) could confound the rating of physical symptoms such as insomnia and restlessness (RUPP Anxiety Group, 2002). For the present study, we did not include the number of symptoms in the total score, but we included physical symptoms because the study did not involve the use of medication. Thus, total scores (sum of six domains) were used and could range from 0 to 30, with higher scores indicative of greater severity. The PARS was conducted and scored by a trained rater who was blind to treatment assignment.
Clinical Global Impressions-Improvement scale (CGI-I; Guy, 1976)
The CGI-I is a 7-point scale designed to measure overall symptomatic change compared to baseline. Scores range from 1 (Very Much Improved) to 4 (Unchanged) to 7 (Very Much Worse). The CGI-I has been used in many clinical trials for over four decades, including treatment studies in children with ASD. In this study, the CGI-I was used as a categorical (responder vs. non-responder) outcome measure to assess global functioning (including functioning in school, activities of daily living, social activities, and home). The blinded independent evaluators (IEs) interviewed the parent and adolescent together at baseline to assess severity and again at the endpoint (immediately post-treatment) to assess improvement. All IEs were trained to reliability using a series of case vignettes. Reliability was demonstrated when the IE assigned the same severity and improvement ratings as the ‘gold standard’ rater on at least three training vignettes.
Developmental Disabled Children's Global Assessment Scale (DD-CGAS; Wagner et al., 2007)
The DD-CGAS is a reliable measure for global functioning in children with developmental disabilities. Scores on this measure range from 0 to 100 with higher scores indicating better overall functioning. The score on the DD-CGAS is based on clinician-review of all available information. In this trial, the DD-CGAS was completed by IEs blind to treatment condition. As described by Wagner and colleagues (2007), IEs were trained with a set of case vignettes and were required to achieve reliability (i.e., scoring within 10 points of gold standard ratings).
Analyses
In this study, feasibility included three related components: (a) treatment adherence (i.e., attendance, attrition, and compliance with prescribed assignments), (b) treatment integrity/fidelity (i.e., degree to which therapists delivered the program as intended), and (c) consumer satisfaction (i.e., degree to which participants perceived the intervention as helpful). Fidelity was computed as the percentage of treatment objectives delivered in each of the 12 therapy sessions (Pavuluri et al., 2004; RUPP Autism Network, 2007). The demonstration of feasibility, rather than efficacy, is a necessary prerequisite to justify further study of a new treatment (Leon et al., 2011). Moreover, because efficacy analyses in pilot trials are vulnerable to false negative and false positive findings, the results are potentially misleading (Kraemer & Kupfer, 2006). Therefore, we present preliminary efficacy analysis as a secondary aim. With a sample of 15 in the treatment group, we had 80% power to detect a large within-group effect (1.00; Pocock, 1983). A benchmark of .70 was set as our within-group effect size of clinical significance for the SRS. This benchmark is based on the chronic nature of ASD-related social disability in particular, and within-group effect sizes reported in other recent group-based social skills interventions for young people with ASD (e.g., Lopata et al., 2010).
To evaluate change in anxiety symptom severity, social competence, and global functioning, we calculated change within each group (MASSI and WL) and did between-group, intent-to-treat (ITT) analyses using all participants randomized (15 per group). Because the continuous outcome variables were not normally distributed, non-parametric tests were used. We used Wilcoxon rank sum tests to determine if observed changes in the treatment group on outcome measures were significant, and permutation to determine statistical significance of between-group differences. Permutation testing is a re-sampling based approach, in that the distribution of the test statistic under the null hypothesis is obtained by calculating all possible values through re-arranging the observed data points. This approach was selected over other non-parametric tests, such as the sign rank test, so that baseline scores could be included as a covariate. Permutation testing uses the same test statistic (e.g., t) but p-values are based on a sample-specific permutation distribution rather than from the theoretical distribution. This approach is especially useful in analyses with small samples. We performed 10,000 permutations for each test. The one-sided p value is calculated as the proportion of permutations in which the group mean differences were greater than or equal to the initially derived test statistic (Pitman, 1937). For the SRS, CASI-Anx, PARS, and DD-CGAS, permutation ANCOVA with baseline scores as the covariate and endpoint scores as the dependent variable was used. Pearson chi-square tests were used to compare the MASSI and WL groups on the CGI-I, with scores of 1 and 2 (very much or much improved, respectively) defined as ‘responder’ status and all other scores defined as ‘non-responder’. Participants who withdrew from the study early (two from MASSI and three from WL) were invited to participate in an early endpoint assessment (at the time of withdrawal) to obtain outcome measurements. Between- and within-group effect sizes (Cohen’s d) were calculated. Clinical significance, or magnitude of each subject’s change, was determined by computing reliable change indices (RCI; Jacobson & Truax, 1991). Based on this model, change scores greater than 1.96 were considered statistically significant and clinically meaningful.
Results
Preliminary analyses
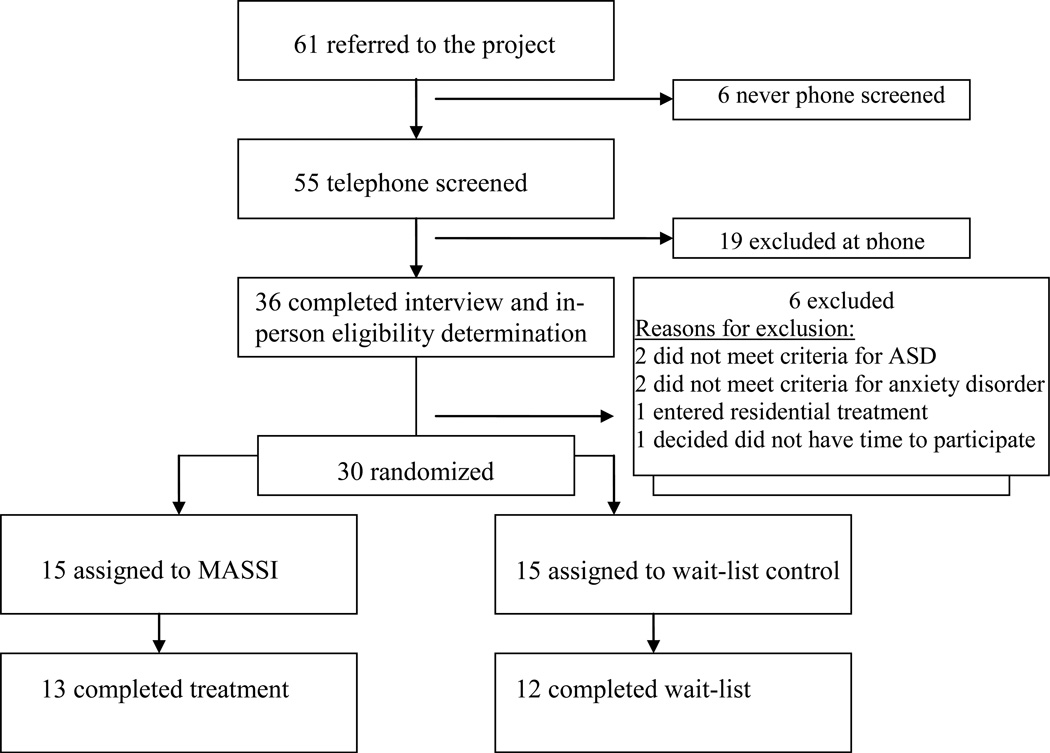
A total of 61 parents of potential participants were screened by telephone. Of these, 30 (49%) met inclusion criteria, and were assessed in the clinic, found eligible, and enrolled in the trial (see Figure 1). Demographic and clinical characteristics are presented in Table 1. Of the 30 participants enrolled in the trial, 23 (77% of sample) were male. As shown in Table 1, mean adaptive behavior scores were considerably lower than IQ scores. Twenty (67%; nine in the MASSI group and 11 in WL) were on psychotropic medication upon study entry, with psychostimulants, selective serotonin reuptake inhibitors, and atypical antipsychotics being most common for single drug treatment or combined drug treatment. Eleven subjects (37%; seven in MASSI and four in WL) were on two or more medications. 1
Figure 1.
CONSORT Flow chart of participants
Derived internal consistency estimates of the outcome measures were all acceptable - alpha of the SRS was .93, the CASI-Anx = .85, and the PARS = .77. There were no statistically significant differences between groups on any demographic or clinical variables at baseline (see Tables 1 and 2).
Table 2.
Baseline, Endpoint, Effect Size on Key Outcome Measures (LOCF)
| MASSI | WL | Effect Size (between-group) |
||
|---|---|---|---|---|
| (n = 15) | (n = 15) | |||
| SRS | 1.03 | |||
| BL | 88.87±12.32 | 85.73±14.14 | ||
| EP | 74.33±12.63 | 84.80±12.18 | ||
| effect size | 1.18 | 0.07 | ||
| PARS | 0.32 | |||
| BL | 14.80±3.67 | 14.53±6.66 | ||
| EP | 14.00±3.44 | 15.47±5.26 | ||
| effect size | 0.19 | -0.12 | ||
| CASI-Anx | 0.30 | |||
| BL | 18.47±9.04 | 18.53±9.47 | ||
| EP | 13.60±5.67 | 16.40±8.87 | ||
| effect size | 0.55 | 0.23 | ||
| DD-CGAS | .52 | |||
| BL | 56.93±11.44 | 60.87±9.03 | ||
| EP | 62.93±9.09 | 61.47±7.77 | ||
| effect size | 0.81 | 0.10 | ||
Effect size (between-group) calculation: change in MASSI (endpoint – baseline) – change in WL (endpoint-baseline)/pooled SD for full sample at baseline
Effect size (within-group) calculation: change score/SD for group at baseline, corrected for correlation between pre- and post-scores for full sample (Morris & DeShon, 2002)
SRS: Social Responsiveness Scale (Constantino & Gruber, 2005); PARS: Pediatric Anxiety Rating Scale (Anxiety Study Group, RUPP, 2002); CASI-Anx: Child and Adolescent Symptom Inventory-4 ASD Anxiety Scale (CASI-Anx; Sukhodolsky et al., 2008); DD-CGAS: Developmental Disabled Children's Global Assessment Scale (DD-CGAS; Wagner et al., 2007). BL: baseline; EP: endpoint
Feasibility-related outcomes
Attrition
Overall, 25 of 30 subjects (83.3%) completed the randomized trial: 13 of 15 (87%) in MASSI and 12 of 15 (80%) in WL (difference not significant). All drop-outs were male. One subject, who dropped out of MASSI after seven individual therapy sessions, cited decreases in teasing by his peers and decreased social anxiety after changing schools as the reasons for early withdrawal. The second participant left the study after five treatment sessions due to worsening self-harm, recurring suicidal ideation and suicide attempts requiring multiple emergency room visits. These serious adverse events were reviewed by the university’s institutional review board and an independent safety monitoring panel and were judged as unrelated to the study treatment. Of the three participants who dropped out during the WL period, one entered residential care for severe aggression and another withdrew due to worsening of his mother’s health condition, which prevented her from transporting her son to the clinic. The third WL dropout was due to the family’s inability to manage work and other time constraints along with planned treatment sessions. Three of the five participants who dropped out of the study early completed early endpoint assessments (both of the MASSI treatment dropouts, and one of the three from WL). For the two WL participants without early endpoint data, their prior assessment scores (from baseline) were carried forward for analysis (Last Observation Carried Forward: LOCF; e.g., Fidler, Faulkner, & Cumming, 2008).
Treatment dose
Per the treatment protocol, the ‘minimum full dose’ of MASSI requires 12 individual therapy sessions, but participants could receive one additional session (if needed) for a total of 13 individual sessions. In addition, seven group sessions for social skills training were planned for each subject in MASSI. Of the 180 required individual therapy sessions (12 sessions × 15 subjects), 168 were attended. Ten of the fifteen MASSI participants received 13 individual sessions. The mean number of individual sessions received across participants was 11.20 (range: 5 – 13). There were 35 planned group sessions for the 15 subjects assigned to MASSI (7 sessions × 5 group cohorts). Seven participants (47%) attended all group sessions; four missed one session, and four missed more than one session.
Homework compliance and subject involvement
Participant compliance with homework assignments, defined as at least partially completed between-session assignments, ranged from 0% to 100% across modules (mean compliance = 58%). The lowest rate of homework completion was for the module on functional assessment, which required the greatest time investment by parents, with daily recordings of antecedents and consequences related to problematic behaviors. Therapist-rated in session client participation showed a per session average of 3.51 ± 0.66 (range = 1 to 4), on a four-point scale with 1 = uninvolved and 4 = actively involved.
Satisfaction
Parents’ scores ranged from 2 to 10, on a 1 (not at all helpful) to 10 (very helpful) scale, with a mean of 8.21 (±2.49). Adolescent ratings of program satisfaction were somewhat lower (M = 7.47; SD = 3.11; range 1 – 10). Of the different components in MASSI (i.e., individual therapy, group therapy, between-session assignments, learning about anxiety and ASD, or other aspects), individual therapy was rated as the most helpful by the parents, M = 4.00, SD = 1.52, on a 1 (least helpful) to 5 (most helpful) scale. The most helpful component, according to the adolescents, was group therapy (3.50 ± 1.40), followed closely by individual therapy (3.36 ± 1.34).
Therapist fidelity
Fidelity to the stated treatment objectives for each module ranged from 87.50% to 100%. Three of the 15 subjects in MASSI accounted for 65% of the modules with less than perfect (i.e., under 100%) fidelity. This suggests that difficulty in delivering the treatment sessions as intended by the manual may have been due to subject characteristics rather than therapist ability or protocol structure. All group therapy sessions had 100% fidelity, indicating that the stated objectives were consistently incorporated across all group modules. Compared to the therapists’ fidelity rating, there was 100% agreement with the randomly selected, independent ratings of the 25 individual therapy and 14 group sessions.
Clinical outcomes
Anxiety and social measures
The within-group effect size of change on the SRS total score for MASSI participants was d = 1.18, and the Wilcoxon rank sum test (Z = −2.76, p < .01) indicated significant improvement from pre- to post-treatment. On the CASI-Anx, the within-group effect size was .55; however, the degree of change was not statistically significant (Z = −1.71, ns). The within-group change on the PARS was also not statistically significant, Z = −.71, ns (d = .19). There was a significant between-group difference, favoring those in MASSI, on the SRS Total T score (average t-statistic = 3.433, p = .007). However, there was no difference between groups on the CASI-Anx (average t-statistic = 1.186, p = .22), or the PARS (average t-statistic = 0.997, p = .31).
Clinical significance analyses
Nine of the 15 MASSI participants demonstrated reliable improvement (i.e., RCI > 1.96) on the SRS whereas none of the 15 WL participants had significant change from pre- to post-treatment on the SRS Total Score, chi square = 12.86, p < .001. On the CASI-Anx, four MASSI participants showed clinically significant and reliable change (i.e., RCI > 1.96), compared to two of 15 WL participants, chi square = .83, ns. In the treatment group, there was a 16% improvement in SRS scores, compared to a 1% improvement in the WL group. The four MASSI participants who had significant improvement on the CASI-Anx also made significant improvement on the SRS.
Overall Functioning
On the DD-CGAS, the MASSI participants had significant improvement from pre- to pos-treatment, Z = −2.74, p < .01; d = .81. There was also a significant group difference on the DD-CGAS (average value of t-statistics = 2.280, p = .029). The treatment group participants had an average six-point increase whereas the WL participants showed an average increase of approximately one-half point. On the CGI-I, 6 of 15 (40%) MASSI participants were rated as responders compared to 3 of 15 (20%) of WL participants, chi square = 1.43, ns. Participants with missing data on the CGI-I (i.e., no endpoint assessment) were considered non-responders.
Discussion
This study is the first randomized controlled trial of a psychosocial intervention concurrently targeting social deficits and anxiety in more able adolescents with ASD. The results of this pilot investigation support the feasibility of a relatively brief, structured, multi-component cognitive-behavioral treatment for social deficits and anxiety in adolescents with ASD. Therapists delivered the program with a high degree of integrity to the protocol, and consumers (participants and parents) reported high satisfaction with the treatment content and delivery. The average homework completion rate by the adolescents in this trial was consistent with compliance reported in previous CBT trials with adolescents, which have indicated that participants complete only approximately half of assigned between-session tasks (Clarke et al., 1992; Gaynor, Lawrence, & Nelson-Gray, 2006). Attendance at group and individual therapy sessions was quite good, and the attrition rate was comparable to other clinical trials with adolescents (e.g., TADS, 2012; Walkup et al., 2008). Given previous research (e.g., Hudson et al., 2009) indicating that treatment drop-out tends to be higher among older children and adolescents, and the clinical complexity1 of this adolescent sample (e.g., Stattin & Kerr, 2009), the degree of participant involvement and adherence in this trial are deemed acceptable.
These findings extend previous research and support the continued adaptation of CBT approaches in higher functioning adolescents with ASD. Furthermore, the evidence of feasibility indicates that further study and refinement of this intervention is warranted. As a pilot trial, this study did test the efficacy of MASSI compared to waitlist. The preliminary analyses of clinical outcome are presented to permit comparison with other trials of similar sample size focused on social skills or anxiety. The large within-group effect size on the parent-rated SRS in this trial (1.18) is similar to results of an open 16-session group-delivered social skills program for adolescents (White et al., 2010; ES = .91, n = 15) and higher than an intensive, five-week program for children (Lopata et al., 2010; ES = .56, n = 36). The between-group effect size of the SRS Total score change in this trial (d = 1.03) is somewhat higher than that obtained in the Lopata et al. (2011) RCT (d = .62).
The between-group effect size on the CASI-Anx of .30 in this trial falls within the range reported by previous trials of anxiety-focused interventions in ASD. In an RCT with an intervention targeting anxiety in children with ASD,Sofronoff et al. (2005) reported an ES of .16. More recent trials of anxiety-focused CBT programs for children with ASD (Reaven et al., 2009; Wood et al., 2009) have reported stronger effects, of .97 and .92 respectively. The Reaven et al. (2009) and Wood et al. (2009) trials both included younger children and had more intensive parent involvement in the treatment than the current study. There are several possible reason(s) for these differing effect sizes. The most likely explanation is that the sample sizes in these trials were small and estimates of effect size are therefore unstable (Leon et al., 2011). Other possible reasons include sample characteristics (e.g., school-age children versus adolescents) or dosage of intervention (e.g., perhaps more anxiety-targeted CBT is necessary within a dual-focus treatment).
Nonetheless, given the severe social deficits and additional impairment conferred by anxiety symptoms in adolescents with ASD, even small treatment effects may be clinically meaningful (White et al., 2010). Future trials might set a specific severity threshold on measures such as the CASI or PARS for entry and consider the minimum effect size that would be clinically meaningful (Kraemer, Minitz, Noda, Tinklenberg, & Yesavage, 2006). Because MASSI is directed at two important domains (social disability and anxiety), the clinically meaningful outcomes may not be the same. For adolescents with ASD accompanied by high anxiety, the anxiety may be considered the more acute problem and proposed as the primary endpoint. In this model, the more chronic problem, social disability, could be analyzed in a hierarchical fashion (no reduction in p value if the primary endpoint is positive).
There are several limitations that warrant consideration. First, the sample size was small and did not provide sufficient power to detect small to medium, but potentially clinically meaningful, effects. In addition, the measures chosen to assess treatment response in this trial were selected from a very short list of measures deemed to be suitable for social disability and anxiety in adolescents with ASD. Moreover, only a few of these measures (e.g., SRS, CGI-I) have been previously used in clinical trials with ASD. This reflects the early stage of treatment research on interventions designed to evaluate social disability and anxiety in youth with ASD. Third, given the non-normal distribution of outcome variable data, caution should be taken in comparing these effect sizes directly to effect sizes from other samples. Finally, although these results indicate that the program is feasible to implement and acceptable to consumers, its transportability to other clinical or educational settings was not evaluated. Coordinating combined group and individual therapy poses unique logistical and staffing challenges, and the length of sessions (along with twice-weekly sessions) may limit exportability. These challenges must be considered to improve likelihood of program adoption. It is possible that the group component, for instance, would be best-delivered in the school setting whilst the individual component is done in the clinic. It is also possible that MASSI can be adapted to be delivered solely in a group context.
In conclusion, anxiety is common among higher functioning adolescents with ASD. However, without an operational definition of ‘anxiety’ in youth with ASD and validated tools for its assessment, our ability to determine if the manifestations of anxiety are similar or distinct from anxiety in typically developing samples is limited. For instance, children with high temperamental negative affect are at high risk for anxiety and mood disorders (Clark & Watson, 1991; Trosper, Whitton, Brown, & Pincus, 2012) and heightened autonomic arousal, a feature often discussed in relation to ASD, is associated with only certain subtypes of anxiety (Brown & McNiff, 2009). Nevertheless, results of this trial support the feasibility of this novel intervention and suggest that further study of MASSI is warranted. Further research on the measurement of anxiety symptoms in children and adolescents with ASD as well as the interaction of anxiety and social disability in this population is needed.
Acknowledgments
This project was supported by a grant from the National Institute of Mental Health [1K01MH079945-01; PI: S. W. White]. We thank the participants in this study, their parents, and their teachers.
Footnotes
Participants in both groups (treatment and wait-list) had medication changes during the trial, despite being requested at baseline to delay or minimize medication regimen changes. During the trial, seven of the 15 participants in the MASSI group and nine of the 15 WL participants had medication dosage changes.
References
- Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology. 1996;64:333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- Bass MM, Duchowny CA, Llabre MM. The effect of therapeutic horseback riding on social functioning in children with autism. Journal of Autism and Developmental Disorders. 2009;39(9):1261–1267. doi: 10.1007/s10803-009-0734-3. [DOI] [PubMed] [Google Scholar]
- Beaumont R, Sofronoff K. A multi-component social skills intervention for children with asperger syndrome: The Junior Detective Training Program. Journal of Child Psychology and Psychiatry. 2008;49(7):743–753. doi: 10.1111/j.1469-7610.2008.01920.x. [DOI] [PubMed] [Google Scholar]
- Bellini S. The development of social anxiety in adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2006;21:138–145. [Google Scholar]
- Brown TA, McNiff J. Specificity of autonomic arousal to DSM-IV panic disorder and posttraumatic stress disorder. Behaviour Research and Therapy. 2009;47:487–493. doi: 10.1016/j.brat.2009.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JM, Ferguson JE, Herzinger CV, Jackson JN, Marino CA. Combined descriptive and explanatory information improves peers’ perceptions of autism. Research in Developmental Disabilities. 2004;25:321–339. doi: 10.1016/j.ridd.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Chalfant A, Rapee R, Carroll L. Treating anxiety disorders in children with high functioning autism spectrum disorders: A controlled trial. Journal of Autism and Developmental Disorders. 2007;37:1842–1857. doi: 10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Chorpita BF. In: Modular cognitive-behavioral therapy for childhood anxiety disorders. Guides to Individualized Evidence-Based Treatment. Persons JB, editor. New York: Guilford; 2007. [Google Scholar]
- Clarke G, Hops H, Lewinsohn PM, Andrews J, Seeley JR, Williams J. Cognitive-behavioral group treatment of adolescent depression: Prediction of outcome. Behavior Therapy. 1992;23:341–354. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale (SRS) Los Angeles, CA: Western Psychological Services; 2005. [Google Scholar]
- Costello EJ, Egger HL, Angold A. Developmental epidemiology of anxiety disorders. In: Ollendick TH, March JS, editors. Phobic and Anxiety Disorders in Children and Adolescent. New York: Oxford University Press; 2004. [Google Scholar]
- Dalton KD, Nacewicz BM, Alexander AL, Davidson RJ. Gaze-fixation, brain activation, and amygdala volume in unaffected siblings of individuals with autism. Biological Psychiatry. 2007;61:512–520. doi: 10.1016/j.biopsych.2006.05.019. [DOI] [PubMed] [Google Scholar]
- deBruin EI, Ferdinand RF, Meester S, De Nijs FA, Verheij F. High rates of psychiatric co-morbidty in PDD-NOS. Journal of Autism and Developmental Disorders. 2007;37:877–886. doi: 10.1007/s10803-006-0215-x. [DOI] [PubMed] [Google Scholar]
- Fidler F, Faulkner C, Cumming G. Analyzing and presenting results. In: Nezu AM, Nezu CM, editors. Evidence-based outcome research: A practical guide to conducting randomized trials for psychosocial interventions. New York: Oxford University Press; 2008. pp. 315–334. [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent symptom inventory-4 screening manual. Stony Brook, NY: Checkmate Plus; 1997. [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent symptom inventory-4 norms manual. Stony Brook, NY: Checkmate Plus; 1998. [Google Scholar]
- Gaynor ST, Lawrence PS, Nelson-Gray RO. Cognitive-behavioral therapy for adolescent depression: Review, preliminary findings, and implications for theory and practice. Behavior Modification. 2006;30:647–672. doi: 10.1177/0145445504272979. [DOI] [PubMed] [Google Scholar]
- Guy W. US Dept Health, Education, and Welfare publication; ADM No. 76-338. Rockville, MD: National Institute of Mental Health; 1976. ECDEU Assessment Manual for Psychopharmacology; pp. 218–222. [Google Scholar]
- Harnum M, Duffy J, Ferguson DA. Adults’ versus children’s percentions of a child with autism or atention deficit hyperactivity disorder. Journal of Autism and Developmental Disorders. 2007;37:1337–1343. doi: 10.1007/s10803-006-0273-0. [DOI] [PubMed] [Google Scholar]
- Honda H, Shimizu Y, Imai M, Nitto Y. Cumulative incidence of childhood autism: A total population study of better accuracy and precision. Developmental Medicine & Child Neurology. 2005;47:10–18. doi: 10.1017/s0012162205000034. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:533–544. doi: 10.1097/CHI.0b013e31819c2401. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Joseph RM, Ehrman K, McNallly R, Keehn B. Affective response to eye contact and face recognition ability in children with ASD. Journal of the International Neuropsychological Society. 2008;14:947–955. doi: 10.1017/S1355617708081344. [DOI] [PubMed] [Google Scholar]
- Joshi G, Petty C, Wozniak J, Henin A, Fried R, Galdo M, et al. The heavy burden of psychiatric comorbidity in youth with Autism Spectrum Disorders: A large comparative study of a psychiatrically referred population. Journal of Autism & Developmental Disorders. Advance online publication. 2010 doi: 10.1007/s10803-010-0996-9. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clincal trial. Journal of Consulting and Clinical Psychology. 1997;65(3):366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E. Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kim YS, Bennett LL, Koh YJ, Fombonne E, Laska E, Lim EC, Grinker RR. Prevalence of autism spectrum disorders in a total population sample. American Journal of Psychiatry. 2011;168:904–912. doi: 10.1176/appi.ajp.2011.10101532. [DOI] [PubMed] [Google Scholar]
- Kleinhans NM, Richards T, Weaver K, Johnson lC, Greenson J, Dawson G, Aylward E. Association between amygdala response to emotional faces and social anxiety in autism spectrum disorders. Neuropsychologia. 2010;48(12):3665–3670. doi: 10.1016/j.neuropsychologia.2010.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klin A, Volkmar FR. Treatment and intervention guidelines for individuals with asperger syndrome. In: Klin A, Volkmar FR, Sparrow SS, editors. Asperger Syndrome. New York: Guilford Press; 2000. pp. 340–366. [Google Scholar]
- Kyllianinen A, Hietanen J. Skin conductance responses to another person’s gaze in children with autism. Journal of Autism and Developmental Disorders. 2006;36(4):517–525. doi: 10.1007/s10803-006-0091-4. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biological Psychiatry. 2006;59:990–996. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- Kraemer H, Minitz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, Lainhart JE. Comorbid psychiatric disorders in children with autism; Interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lopata C, Thomeer ML, Volker MA, Nida RE, Lee GK, Toomey JA, Rodgers JD. RCT of a manualized social treatment for high-functioning Autism Spectrum Disorders. Journal of Autism and Developmental Disorders. 2010;40:1297–1310. doi: 10.1007/s10803-010-0989-8. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview—Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Hughes AJ, Oswald DP, Lainhart JE. Lack of correspondence between self- and parent-report on structured psychiatric interview of adolescents with high-functioning autism spectrum disorders; Oral presentation at the International Meeting for Autism Research; Toronto, Canada. 2012. May, [Google Scholar]
- Mazefsky CA, Kao J, Oswald DP. Preliminary evidence suggesting caution in the use of psychiatric self-report measures with adolescents with high-functioning autism spectrum disorders. Research in Autism Spectrum Disorders. 2011;5:164–174. doi: 10.1016/j.rasd.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-group designs. Psychological Methods. 2002;7(1):105–125. doi: 10.1037/1082-989x.7.1.105. [DOI] [PubMed] [Google Scholar]
- Myles B, Barnhill G, Hagiwara T, Griswold D, Simpson R. A synthesis of studies on the intellectual, academic, social/emotional and sensory characteristics of children with asperger syndrome. Education and Training in Mental Retardation and Developmental Disabilities. 2001;36:304–311. [Google Scholar]
- Ochs E, Kremer-Sadlik T, Solomon O, Gainer Sirota K. Inclusion as social practice: Views of children with autism. Social Development. 2001;10:399–419. [Google Scholar]
- Ollendick TH, Ost L-G, Reuterskiold L, Costa N, Cederlund R, Sirbu C, Thompson TE, III, Jarrett MA. One-session treatment of specific phobias in youth: A radomized clinical trial in the United States and Sweden. Journal of Consulting and Clinical Psychology. 2009;77:504–516. doi: 10.1037/a0015158. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Graczyk PA, Henry DB, Carbrat JA, Heidenreich J, Miklowitz DJ. Child- and family-focused cognitive-behavioral therapy for pediatric bipolar disorder: Development and preliminary results. Journal of the American Academy of Child Psychiatry. 2004;2004:43,528–43,537. doi: 10.1097/00004583-200405000-00006. [DOI] [PubMed] [Google Scholar]
- Pitman EJG. Significance tests which may be applied to samples from any population. Royal Statistical Society Supplement. 1937;4:119–130. 225–232. [Google Scholar]
- Pocock SJ. Clinical Trials: A Practical Approach. Chichester: John Wiley and Sons; 1983. [Google Scholar]
- Reaven JA, Blakeley-Smith A, Nichols S, Dasari M, Flanigan E, Hepburn S. Cognitive-behavioral group treatment for anxiety symptoms in children with highfunctioning autism spectrum disorders: A pilot study. Focus on Autism and Other Developmental Disabilities. 2009;24(1):27–37. [Google Scholar]
- Research Units on Pediatric Psychopharmacology Anxiety Study Group. The Pediatric Anxiety Rating Scale (PARS): Development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology [RUPP] Autism Network. Parent training for children with pervasive developmental disorders: A multi-site feasibility trial. Behavioral Interventions. 2007;22:179–199. [Google Scholar]
- Rutter M, Lord C, Le Couteur A. Autism Diagnostic Interview Revised Manual. Torrance, California, USA: Wester Psychological Services; 2003. [Google Scholar]
- Shatayermann O. Peer victimization in adolescents and young adults diagnosed with asperger’s syndrome: A link to depressive symptomatology, anxiety symptomatology, and suicidal ideation. Issues in Comprehensive Pediatric Nursing. 2007;30:87–107. doi: 10.1080/01460860701525089. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSMIV. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Silverman W, Kurtines W, Ginsburg G, Weems C, Rabian B, Serafini L. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67:675–687. doi: 10.1037//0022-006x.67.5.675. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with anxiety disorders interview schedule for DSM-IV : Child and parent versions. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Smith T, Scahill L, Dawson G, Guthrie D, Lord C, Odom S, Wagner A. Designing research studies on psychosocial interventions in autism. Journal of Autism and Developmental Disorders. 2007;37:354–366. doi: 10.1007/s10803-006-0173-3. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. A randomised controlled trial of a CBT intervention for anxiety in children with asperger syndrome. Journal of Child Psychology and Psychiatry. 2005;46(11):1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, Balla DA. Vineland-II Adaptive Behavior Scales. 2nd Edition. Circle Pines, MN: AGS Publishing; 2005. [Google Scholar]
- Stattin H, Kerr M. Challenges in intervention research on adolescent development. Journal of Adolescence. 2009;32:1437–1442. doi: 10.1016/j.adolescence.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold E, Aman MG, McDougle CJ, Vitiello B. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology. 2008;36:117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- Swaim KF, Morgan SB. Children’s attitudes and behavioral intentions toward a peer with autistic behaviors: Does a brief educational intervention have an effect? Journal of Autism and Developmental Disorders. 2001;31:195–205. doi: 10.1023/a:1010703316365. [DOI] [PubMed] [Google Scholar]
- TADS Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. Journal of the American Medical Association. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- Trosper SE, Whitton SW, Brown TA, Pincus DB. Understanding the latent structure of the emotional disorders in children and adolescents. Journal of Abnormal Child Psychology. 2012;40:621–632. doi: 10.1007/s10802-011-9582-7. [DOI] [PubMed] [Google Scholar]
- Tse J, Strulovich J, Tagalakis V, Meng L, Fombonne E. Social skills training for adolescents with asperger syndrome and high-functioning autism. Journal of Autism and Developmental Disorders. 2007;37:1960–1968. doi: 10.1007/s10803-006-0343-3. [DOI] [PubMed] [Google Scholar]
- United States Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders-autism and developmental Disabilities Monitoring Network, United States, 2008. MMWR Surveill Summ. 2012;61 (No. SS-3) [PubMed] [Google Scholar]
- Wagner A, Lecavalier L, Arnold LE, Aman MG, Scahill L, Stigler KA, Vitiello B. Developmental Disabilities Modification of Children’s Global Assessment Scale (DD-CGAS) Biological Psychiatry. 2007;61:504–511. doi: 10.1016/j.biopsych.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini JC, Birmaher B, Compton SN, Sherrill JT, Kendall PC. Cognitive behavioral therapy, Sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) San Antonio, TX: Harcourt Assessment; 1999. [Google Scholar]
- White SW, Koenig K, Scahill L. Group therapy to improve social skills in adolescents with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2010;25(4):209–219. [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Schry AR, Maddox BM. Brief report: The assessment of anxiety in high-functioning adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. Advance online publication. 2012 doi: 10.1007/s10803-011-1353-3. [DOI] [PubMed] [Google Scholar]
- Witwer AN, Lecavalier L. Validity of comorbid psychiatric disorders in youngsters with autism spectrum disorders. Journal of Developmental and Physical Disabilities. 2010;22:367–380. [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of Clinical Child and Adolescent Psychology. 2002;31(3):335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]