Abstract
Background
Prior research established that psychological factors are associated with the frequency of stimulant (i.e., cocaine, crack, and methamphetamine) use among substance-using men who have sex with men (MSM). The present investigation examined whether and how psychological factors are associated with engagement in any stimulant use in the broader population of MSM.
Methods
A probability sample of 879 MSM residing in San Francisco was obtained using random digit dialing from May of 2002 through January of 2003. Of these, 711 participants (81%) completed a mail-in questionnaire that assessed psychological factors and substance use. After accounting for demographic factors, a multiple logistic regression analysis examined correlates of any self-reported stimulant use during the past 6 months. Path analyses examined if the use of alcohol or other substances to avoid negative mood states (i.e., substance use coping) mediated the associations of sexual compulsivity and depressed mood with stimulant use.
Results
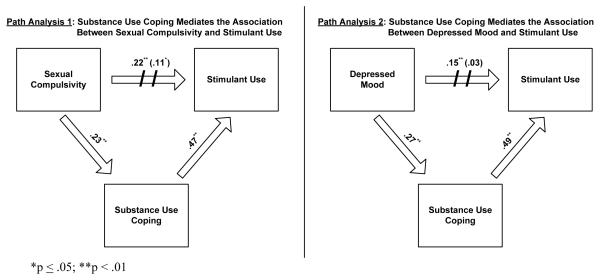
Younger age (adjusted OR [AOR] = 0.58; 95% CI = 0.47 – 0.70), HIV-positive serostatus (AOR = 2.55; 95% CI = 1.61 – 4.04), greater depressed mood (AOR = 1.26; 95% CI = 1.05 – 1.52) and higher sexual compulsivity (AOR = 1.46; 95% CI = 1.18 – 1.80) were independently associated with increased odds of stimulant use. Substance use coping partially mediated the associations of sexual compulsivity (βindirect = 0.11, p < .001) and depressed mood (βindirect = 0.13, p < .001) with stimulant use.
Conclusions
Clinical research is needed to examine if interventions targeting sexual compulsivity and emotion regulation reduce stimulant use among MSM.
Keywords: Cocaine, Crack, Depression, Men who have Sex with Men, Methamphetamine, Sexual Compulsivity
1. Introduction
Over a decade of research provides compelling evidence that stimulant (i.e., cocaine, crack, and methamphetamine) use and HIV/AIDS are intertwined epidemics (Colfax et al., 2010; Halkitis et al., 2001; Shoptaw, 2000), particularly among men who have sex with men (MSM). HIV-negative individuals who use stimulants report higher rates of sexual risk taking behavior and are at increased risk for contracting HIV as well as other sexually transmitted infections (Colfax et al., 2005; Koblin et al., 2006; Ostrow et al., 2009; Parsons and Bimbi, 2007; Shoptaw and Reback, 2007). Among HIV-positive persons, the use of stimulants has been associated with greater odds of engaging in HIV transmission risk behavior (Johnson et al., 2008; Morin et al., 2007), impaired HIV disease management (Carrico et al., 2011a; Carrico et al., 2007b; Carrico et al., 2011b; Ellis et al., 2003; Hinkin et al., 2007), and hastened HIV disease progression (Carrico, 2011; Cook et al., 2008). The co-occurrence of HIV transmission risk behavior and non-adherence to anti-retroviral therapy among HIV-positive stimulant users may also substantially contribute to the transmission of medication-resistant strains of the virus (Colfax et al., 2007; Gorbach et al., 2008; Kalichman, 2008). Taken together, these data indicate that stimulant use and its behavioral sequelae are important targets for interventions across the spectrum of HIV prevention and care.
Prior research has focused extensively on examining the psychological correlates of stimulant use among MSM with the goal of informing the development of innovative interventions. Findings from convenience samples of substance-using MSM indicate that greater avoidant-oriented coping, motivations to use substances to avoid negative emotions as well as enhance positive emotions, and higher drug-related sensation seeking are associated with more frequent stimulant use (Halkitis et al., 2005; Halkitis et al., 2007; Halkitis and Shrem, 2006; Palamar et al., 2008). There is also increasing recognition that sexual compulsivity may be an important determinant of sexual risk taking behavior and concomitant stimulant use (Parsons et al., 2008; Parsons et al., 2007). Consistent with the proposed criteria for Hypersexual Disorder in the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (APA, 2011), sexual compulsivity is characterized by difficulties with managing frequent sexual fantasies, urges, or behaviors. Although previous research with MSM observed that sexual compulsivity is associated with sex under the influence of stimulants (Grov et al., 2010; Semple et al., 2006), relatively little is known about the underlying mechanism(s) that account for this relationship. Difficulties with emotion regulation are thought to be one important feature of sexual compulsivity such that sexual fantasies, urges, or behaviors are emitted in response to negative emotions (Bancroft, 2008; Bancroft et al., 2003). However, various forms of negative affect (e.g., depression and anxiety) have not been reliably associated with stimulant use in prior studies with MSM (Halkitis et al., 2005; Halkitis et al., 2007; Halkitis and Shrem, 2006; Palamar et al., 2008). Further research with more representative samples is needed to examine if sexual compulsivity and depressed mood are associated with engagement in stimulant use among the broader population of MSM.
Two distinct theoretical frameworks may assist with elucidating the underlying pathway(s) whereby sexual compulsivity and depressed mood are associated with engagement in stimulant use among MSM. The Self-Control Strength Model proposes that the capacity for effortful self-regulation of behavior is a limited resource that is depleted more rapidly when individuals are experiencing negative emotions such as depressed mood (Baumeister et al., 2007; Gailliot et al., 2007; Muraven and Baumeister, 2000). Because the experience of depressed mood depletes resources that are crucial to self-control (Hagger et al., 2010), it can increase vulnerability for engagement in a variety of health risk taking behaviors such as substance use. Thus, we hypothesize that increased depressed mood will facilitate engagement in stimulant use among those who are more predisposed to the cognitive-behavioral responses that characterize sexual compulsivity. It is also plausible that substance use stems from an over-learned pattern of avoidance in response to stressful life circumstances. Drawing upon Stress and Coping Theory (Carrico et al., 2007a; Folkman, 1997; Gifford et al., 2006; Moggi et al., 1999), substance use can be conceptualized as a form of coping which allows one to temporarily escape negative mood states. Those with elevated sexual compulsivity and depressed mood may be more predisposed to use alcohol or other substances as a means of temporarily avoiding stressful life circumstances. This substance use coping could, in turn, promote engagement in stimulant use. To our knowledge, no investigation to date has explicitly tested theory-based pathways that could explain the associations of sexual compulsivity and depressed mood with stimulant use among MSM.
The goal of the present investigation was to examine whether and how psychological factors are associated with stimulant use in a probability sample of MSM. We hypothesized that elevated depressed mood and greater sexual compulsivity would be independently associated with increased odds of reporting any stimulant use in the past 6 months. In order test the Self-Control Strength Model, we examined whether depressed mood moderated the association between sexual compulsivity and stimulant use. Informed by Stress and Coping Theory, we also examined whether a tendency to use alcohol or other substances to avoid stressful life circumstances (i.e., substance use coping) mediated the associations of sexual compulsivity and depressed mood with stimulant use.
2. Methods
2.1. Data Collection
Data for the Urban Men’s Health Study 2002 (UMHS-2002) were collected in San Francisco from May 24, 2002 to January 19, 2003 using random digit dialing. Details of the sampling methodology are described elsewhere (Catania et al., 2001). Westat Corporation constructed the sampling frame and participated in data collection. MSM were defined as those who reported same gender sex (of any kind) since age 14 and/or self-identified as gay or bisexual. Respondents participated in an initial telephone interview (response rate = 74%) followed by a self-administered mail-in questionnaire (received within 1–2 weeks of completing the telephone interview; response rate = 81%). Self-reported substance use and selected psychological measures were included in the self-administered mail-in questionnaire. Participants provided informed consent with procedures approved by the University of California, San Francisco Committee on Human Research and the Westat IRB.
2.2. Measures
2.2.1. Demographics
Age, education, income, ethnicity, and HIV status were assessed during the initial telephone interview.
2.2.2. Depressed Mood
During the telephone interview, participants completed 8 items assessing depressed mood during the past 6 months (Radloff, 1977). This modified depressed mood sub-scale for the Centers for the Epidemiologic Study of Depression measure had adequate internal consistency (Cronbach’s α = .86; M = 11.6, SD = 6.6).
2.2.3. Sexual Compulsivity
The 6-item Sexual Preoccupation Scale was completed in the mail-in questionnaire to assess cognitive dimensions of sexual compulsivity (Snell and Papini, 1989). Participants rated items (e.g., “I’m constantly thinking about having sex.”) on a 4-point, Likert-type scale from “I agree a lot” to “I disagree a lot”. Higher scores reflect greater sexual compulsivity (Cronbach’s α = .77; M = 15.6, SD = 3.5).
2.2.4. Substance Use Coping
In the mail-in questionnaire, participants were asked to rate how they typically responded when they experienced stressful events in the past 12 months. Using the 4-item Substance Use Coping sub-scale of the COPE (Carver et al., 1989), participants rated items (e.g., “I try to lose myself for awhile by drinking alcohol or taking drugs.”) on a 4-point, Likert-type scale from “Never” to “Often” (Cronbach’s α = .94; M = 7.3, SD = 3.4).
2.2.5. Stimulant Use
In the mail-in questionnaire, participants indicated the number of times they used powder cocaine, crack, methamphetamine, and other amphetamines during the past 6 months. These data were summed and dichotomized to compare those who reported any stimulant use during the past 6 months to participants who did not report stimulant use. In addition, 8 participants who reported stimulant use during a sexual event in the past 3 months in the initial telephone interview did not report stimulant use in the mail-in questionnaire. These participants were re-categorized as engaging in stimulant use during the past 6 months.
2.3. Statistical Analyses
The present investigation utilized multiple logistic regression to examine correlates of stimulant use. Because previous investigations have observed that background characteristics such as age and ethnicity may be important correlates of stimulant use, we included demographic factors in the regression model. Sexual compulsivity and depressed mood were transformed into z-scores (M = 0, SD = ±1) to facilitate interpretation of the adjusted odds ratio (AOR). The AOR reflects the independent association of each variable with stimulant use in the multivariate model. Given prior research demonstrating that the prevalence of stimulant use is elevated among HIV positive persons, we examined whether the associations of depressed mood and sexual compulsivity with stimulant use were moderated by HIV status. Consistent with the Self-Control Strength Model, we also examined if the association of sexual compulsivity with stimulant use was moderated by depressed mood. Maximum likelihood estimation procedures with Monte Carlo integration in Mplus 6.0 were employed to obtain parameter estimates that utilize all available data from the 711 participants that completed the mail-in questionnaire.
Informed by Stress and Coping Theory, we conducted path analyses in Mplus 6.0 to examine whether substance use coping mediated the associations sexual compulsivity and depressed mood with stimulant use. We utilized multiple descriptive indices of model fit: comparative fit index (CFI) values greater than .95, root mean square error of approximation (RMSEA) values less than .06, and weighted root-mean-square residual (WRMR) values less than .90 (Hu and Bentler, 1998). Although a non-significant chi-square (χ2) is also generally indicative of better model fit, this statistic may detect trivial model misfit to the data given the relatively large sample size for the present investigation. The categorical outcome variable (i.e., stimulant use) required the use of the weighted least squares-mean and variance-adjusted estimator with delta parameterization (Muthén and Muthén, 2004). In order to test for mediation, we examined the significance of the indirect effects of sexual compulsivity and depressed mood on stimulant use via substance use coping. After obtaining satisfactory global model fit, we refitted the model using a maximum likelihood logit link function to obtain OR’s and their 95% confidence intervals for the associations of sexual compulsivity, depressed mood, and substance use coping with stimulant use.
3. Results
3.1. Adjusted Sampling Weights
Weights for the household probability sample of adult MSM living in San Francisco were adjusted to account for predictors of response to the mail-in questionnaire (n = 711; 81%). In total, we examined the univariate associations of 38 potential predictor variables from the telephone survey with response to the mail-in questionnaire. The potential predictors included: demographic characteristics, health-related variables (i.e., self-rated health, HIV serostatus, sexually transmitted infection history, and history of intravenous drug use), attendance at venues where MSM socialize, same-gender sexual behavior in the past 12 months, attitudes toward sex, sexual history (i.e., age at same-gender sexual debut and history of sexual abuse), psychological adjustment (i.e., depressed mood), and migration history. Where the univariate p-value was ≤ .25, variables were considered for inclusion in the multiple logistic regression model predicting response to the mail-in questionnaire. Maximum likelihood estimation procedures with Monte Carlo integration in Mplus 6.0 were utilized to enhance the precision of this predictive model, which contained 11 variables. As shown in Table 1, a greater number of years as a resident of San Francisco, better self-rated health, more frequent cruising for sex, engaging in insertive anal sex without a condom in the past 12 months, and more moves since age 18 were associated with significantly greater odds of responding to the mail-in questionnaire. Using the unstandardized parameter estimates from the final predictive model, we calculated the predicted probability of response to the mail-in questionnaire. Adjusted sampling weights are the product of the sampling weight from the household probability sample and the reciprocal of the probability of response to the mail-in questionnaire. The resulting adjusted sampling weights were then scaled so that they sum to the number of men who responded to the mail-in questionnaire. Adjusting sampling weights for the probability of response substantially attenuates possible bias in the prevalence estimates for stimulant use arising from attrition due to non-participation in the mail-in questionnaire (Kalton, 1983).
Table 1.
Correlates of response to the mail-in questionnaire (N = 879).
| AOR (95% CI) | |
|---|---|
| Income | 0.93 (0.81 – 1.07) |
| Current Primary Partner | 0.87 (0.61 – 1.24) |
| Employed | 0.98 (0.61 – 1.58) |
| Number of Years Lived in San Francisco | 1.03 (1.01 – 1.05)** |
| Self-Rated Health | 1.24 (1.01 – 1.53)* |
| HIV-Positive | 1.35 (0.85 – 2.13) |
| Number of Visits to a Gay Bar (Past 12 Months) | 0.99 (0.99 – 1.00) |
| Number of Times Cruising for Sex (Past 12 Months) | 1.03 (1.01 – 1.06)* |
| Insertive Anal Sex Without a Condom (Past 12 Months) | 1.03 (1.01 – 1.06)* |
| Sexual Assertiveness | 1.07 (0.98 – 1.18) |
| Number of Moves Since Age | 18 1.11 (1.02 – 1.21)* |
p < .05
p < .01
3.2. Participant Demographics
The majority of the 711 participants who responded to the mail-in survey were Caucasian (81%) and HIV-negative (73%). Most participants were 40 years of age or older (63%), currently employed (71%), had at a least an undergraduate degree (69%), and made less than $60,000 per year (62%). The prevalence of any stimulant use in the past 6 months was 23% (95% CI = 20% - 27%). For each stimulant, the prevalence of any use during the past 6 months was: 17% (95% CI = 14% - 20%) for methamphetamine, 10% (95% CI = 8% - 12%) for powder cocaine, 2% (95% CI = 1% - 4%) for crack, and 1% (95% CI = 1% - 2%) for other amphetamines. Among those who reported using any stimulants in the past 6 months, 28% reported using more than one stimulant during this period and 42% had not utilized any HIV prevention services or substance abuse treatment in the past year.
3.3. Psychological Correlates of Stimulant Use
Table 2 summarizes the results of the multiple logistic regression model examining correlates of stimulant use. Results indicated that each decade increase in age was associated with a 42% decrease in the odds of reporting stimulant use. HIV-positive persons had 2.5-fold greater adjusted odds of reporting stimulant use (33% vs. 21%). Finally, each standard deviation increase in depressed mood and sexual compulsivity was associated with a 26% and 46% increase in the odds of reporting stimulant use, respectively. HIV-positive serostatus did not moderate the associations of depressed mood (AOR = 0.87; 95% CI = 0.60 – 1.27) and sexual compulsivity (AOR = 1.23; 95% CI = 0.78 – 1.93) with stimulant use. Similarly, depressed mood did not moderate the association of sexual compulsivity with stimulant use (AOR = 1.00; 95% CI = 0.82 – 1.21). These interaction terms were excluded from the final multivariate model.
Table 2.
Correlates of stimulant use among MSM recruited via probability-based sampling (n = 711)
| OR (95% CI) | AOR (95% CI) | |
|---|---|---|
| Age (decade) | 0.65 (0.54 – 0.78)** | 0.58 (0.47 – 0.70)** |
| High School or Less | Reference | Reference |
| Some College | 0.72 (0.37 – 1.41) | 0.64 (0.31 – 1.30) |
| College Graduate | 0.81 (0.44 – 1.48) | 0.74 (0.39 – 1.42) |
| Graduate Degree | 0.59 (0.30 – 1.14) | 0.61 (0.29 – 1.25) |
| Income | 1.03 (0.93 – 1.15) | 1.10 (0.97 – 1.25) |
| Ethnic Minority | Reference | Reference |
| Caucasian | 1.14 (0.66 – 1.94) | 1.41 (0.78 – 2.55) |
| HIV-negative or Unknown | Reference | Reference |
| HIV-Positive | 1.77 (1.20 – 2.62)** | 2.55 (1.61 – 4.04)** |
| Depressed Mood | 1.30 (1.09 – 1.54)** | 1.26 (1.05 – 1.52)* |
| Sexual Compulsivity | 1.46 (1.20 – 1.79)** | 1.46 (1.18 – 1.80)** |
p < .05
p < .01
3.4. Path Analyses Examining Substance Use Coping as a Mediator
For the path analyses, demographic factors from the multiple logistic regression model were included as predictors of stimulant use. The first path analysis examining whether substance use coping mediated the association between sexual compulsivity and stimulant use appeared to be an adequate fit for the data [χ2 (14) = 32.932, p = .0029; CFI = .99; RMSEA = .04; WRMR = .75]. As shown in Figure 1, greater sexual compulsivity was significantly associated with increased substance use coping (β = .23, p < .01). Greater substance use coping was, in turn, associated with increased odds of stimulant use (β = .47, p < .01; OR = 1.31, 95% CI = 1.23 – 1.39). The indirect effect of sexual compulsivity on stimulant use via substance use coping was also significant (β = .11, p < .01). After accounting for this indirect effect, sexual compulsivity was associated with increased odds of stimulant use (β = .11, p = .05; OR = 1.27, 95% CI = 1.01 – 1.60). The second path analysis examining whether substance use coping mediated the association between depressed mood and stimulant use also appeared to be an adequate fit for the data [χ2 (14) = 48.577, p < .0001; CFI = .99; RMSEA = .059; WRMR = .92]. As shown in Figure 1, greater depressed mood was significantly associated with increased substance use coping (β = .27, p < .01). Greater substance use coping was, in turn, associated with increased odds of stimulant use (β = .49, p < .01; OR = 1.32, 95% CI = 1.24 – 1.40). The indirect effect of depressed mood on stimulant use via substance use coping was also significant (β = .13, p < .01). After accounting for this indirect effect, depressed mood was not significantly associated with stimulant use (β = .03, p > .05; OR = 1.04, 95% CI = 0.85 – 1.29). Taken together, this pattern of results is indicative of partial mediation.
Figure 1.
Mediation analyses (n = 711).
4. Discussion
Prior research has focused extensively on examining psychological correlates of more frequent stimulant use in convenience samples of substance-using MSM (Halkitis et al., 2005; Halkitis et al., 2007; Halkitis and Shrem, 2006; Palamar et al., 2008; Semple et al., 2006). To our knowledge, the present study is the first to examine psychological correlates of engaging in any stimulant use with probability-based sample of MSM. Greater depressed mood and sexual compulsivity were independently associated with increased odds of reporting any stimulant use in the past 6 months, after accounting for demographic characteristics. Findings did not provide support for the Self-Control Strength Model in that the association between sexual compulsivity and stimulant use was not moderated by depressed mood. However, results of path analyses provide support for Stress and Coping Theory because substance use coping partially mediated the associations of depressed mood and sexual compulsivity with stimulant use. Consistent with negative reinforcement models of addiction (Baker et al., 2004), findings indicate that a desire to escape or avoid negative emotions may partially explain why these psychological factors are associated with engagement in stimulant use in the broader population of MSM.
Although findings from the present study provide some insight into psychological risk factors for stimulant use, one cannot conclude from this cross-sectional study that sexual compulsivity, depressed mood, and substance use coping are causally related to engagement in stimulant use. In fact, it is possible that stimulant use leads to increases in sexual compulsivity and difficulties with emotion regulation. Longitudinal research that includes multi-method assessment of emotion regulation as well as toxicology screening for stimulant use is needed to determine whether and how psychological factors predict changes in stimulant use among MSM. Identifying the specific difficulties with emotion regulation (e.g., decreased emotional awareness, poor negative emotion regulation, or blunted positive emotion regulation) that explain the effects of sexual compulsivity and depressed mood on stimulant use could further inform the development of innovative interventions for this population. Future longitudinal research should also examine the differential effects of psychological factors on specific patterns (e.g., binge vs. chronic) and types (e.g., cocaine vs. methamphetamine) of stimulant use. Another important limitation of the present study is that the probability-based sampling methodology did not recruit large numbers of ethnic minority MSM. Studies are needed to examine the context and correlates of stimulant use among African American and Hispanic/Latino MSM. Finally, it is noteworthy that data for this study were collected approximately 8 years ago and the prevalence of methamphetamine use declined dramatically during this period, particularly among HIV-negative MSM (Pantalone et al., 2010; Vaudrey et al., 2007). Although reductions in the prevalence of methamphetamine use are unlikely to alter the psychological processes that contribute to vulnerability for engagement in stimulant use, further research is needed to examine the interaction of social and psychological factors on stimulant use among MSM.
In conclusion, the findings from the present investigation highlight that difficulties with emotion regulation represent a key, underlying pathway that may explain the effects of sexual compulsivity and depressed mood on engagement in stimulant use among MSM. These results have important implications for the development of more effective interventions aimed at stimulant-using MSM. A recent multi-site, randomized controlled trial that enrolled substance-using MSM who were non-treatment-seeking (i.e., Project MIX) observed that a cognitive-behavioral intervention did not achieve greater reductions in sexual risk taking and concomitant substance use compared to an attention-control condition (Mansergh et al., 2010). Clinical research is needed to examine the efficacy of innovative interventions targeting sexual compulsivity and emotion regulation with stimulant-using MSM, many of whom are not engaged in HIV prevention services or substance abuse treatment.
Acknowledgments
Role of Funding Source: This research was supported by funding from the National Institute of Mental Health (R01-MH054320; Catania, PI) and National Institute on Drug Abuse (R03-DA030124; Carrico, PI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors: AWC and JTM developed study hypotheses. AWC, LMP, SBS, and TBN were the primary individuals responsible for data analysis. Interpretation of findings was coordinated by AWC and JTM with feedback from the entire team. Detailed comments on draft manuscripts prepared by AWC were provided by JTM, RDS, TMR, and WJW.
Conflict of Interest: No conflict declared
References
- American Psychiatric Association (APA) Sexual and Gender Identity Disorders Work Group [accessed on 9/30/11];Hypersexual Disorder. 2011 http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=415.
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol. Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bancroft J. Sexual behavior that is “out of control”: a theoretical conceptual approach. Psychiatr. Clin. North Am. 2008;31:593–601. doi: 10.1016/j.psc.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Bancroft J, Janssen E, Strong D, Vukadinovic Z. The relation between mood and sexuality in gay men. Arch. Sex. Behav. 2003;32:231–242. doi: 10.1023/a:1023461500810. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Vohs KD, Tice DM. The strength model of self-control. Curr. Dir. Psychol. Sci. 2007;16:351–355. [Google Scholar]
- Carrico AW. Substance use and HIV disease progression in the HAART era: implications for the primary prevention of HIV. Life Sci. 2011;88:940–947. doi: 10.1016/j.lfs.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Bangsberg DR, Weiser SD, Chartier M, Dilworth SE, Riley ED. Psychiatric correlates of HAART utilization and viral load among HIV-positive impoverished persons. AIDS. 2011a;25:1113–1118. doi: 10.1097/QAD.0b013e3283463f09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, Gifford EV, Moos RH. Spirituality/religiosity promotes acceptance-based responding and 12-step involvement. Drug Alcohol Depend. 2007a;89:66–73. doi: 10.1016/j.drugalcdep.2006.12.004. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Johnson MO, Moskowitz JT, Neilands TB, Morin SF, Charlebois ED, Steward WT, Remien RH, Wong FL, Rotheram-Borus MJ, Lightfoot MA, Chesney MA. Affect regulation, stimulant use, and viral load among HIV-positive persons on anti-retroviral therapy. Psychosom. Med. 2007b;69:785–792. doi: 10.1097/PSY.0b013e318157b142. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Riley ED, Johnson MO, Charlebois ED, Neilands TB, Remien RH, Lightfoot MA, Steward WT, Weinhardt LS, Kelly JA, Rotheram-Borus MJ, Morin SF, Chesney MA. Psychiatric risk factors for HIV disease progression: the role of inconsistent patterns of antiretroviral therapy utilization. J. Aquir. Immune Defic. Syndr. 2011b;56:146–150. doi: 10.1097/QAI.0b013e318201df63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J. Pers. Soc. Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Catania JA, Osmond D, Stall RD, Pollack L, Paul JP, Blower S, Binson D, Canchola JA, Mills TC, Fisher L, Choi KH, Porco T, Turner C, Blair J, Henne J, Bye LL, Coates TJ. The continuing HIV epidemic among men who have sex with men. Am. J. Public Health. 2001;91:907–914. doi: 10.2105/ajph.91.6.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, Chesney M, Vittinghoff E. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J. Urban Health. 2005;82:i62–70. doi: 10.1093/jurban/jti025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Santos GM, Chu P, Vittinghoff E, Pluddemann A, Kumar S, Hart C. Amphetamine-group substances and HIV. Lancet. 2010;376:458–474. doi: 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- Colfax GN, Vittinghoff E, Grant R, Lum P, Spotts G, Hecht FM. Frequent methamphetamine use is associated with primary non-nucleoside reverse transcriptase inhibitor resistance. AIDS. 2007;21:239–241. doi: 10.1097/QAD.0b013e3280114a29. [DOI] [PubMed] [Google Scholar]
- Cook JA, Burke-Miller JK, Cohen MH, Cook RL, Vlahov D, Wilson TE, Golub ET, Schwartz RM, Howard AA, Ponath C, Plankey MW, Levine AM, Grey DD. Crack cocaine, disease progression, and mortality in a multicenter cohort of HIV-1 positive women. AIDS. 2008;22:1355–1363. doi: 10.1097/QAD.0b013e32830507f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis RJ, Childers ME, Cherner M, Lazzaretto D, Letendre S, Grant I. Increased human immunodeficiency virus loads in active methamphetamine users are explained by reduced effectiveness of antiretroviral therapy. J. Infect. Dis. 2003;188:1820–1826. doi: 10.1086/379894. [DOI] [PubMed] [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Soc. Sci. Med. 1997;45:1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Gailliot MT, Baumeister RF, DeWall CN, Maner JK, Plant EA, Tice DM, Brewer LE, Schmeicel BJ. Self-control relies on glucose as a limited energy source: willpower is more than a metaphor. J. Pers. Soc. Psychol. 2007;92:325–336. doi: 10.1037/0022-3514.92.2.325. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Ritsher JB, McKellar JD, Moos RH. Acceptance and relationship context: a model of substance use disorder treatment outcome. Addiction. 2006;101:1167–1177. doi: 10.1111/j.1360-0443.2006.01506.x. [DOI] [PubMed] [Google Scholar]
- Gorbach PM, Drumright LN, Javanbakht M, Pond SL, Woelk CH, Daar ES, Little SJ. Antiretroviral drug resistance and risk behavior among recently HIV-infected men who have sex with men. J. Acquir. Immune. Defic. Syndr. 2008;47:639–643. doi: 10.1097/QAI.0b013e3181684c3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Arch. Sex. Behav. 2010;39:340–349. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger MS, Wood C, Stiff C, Chatzisarantis NL. Ego depletion and the strength model of self-control: a meta-analysis. Psychol. Bull. 2010;136:495–525. doi: 10.1037/a0019486. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Green KA, Mourgues P. Longitudinal investigation of methamphetamine use among gay and bisexual men in New York City: findings from Project BUMPS. J. Urban Health. 2005;82:i18–25. doi: 10.1093/jurban/jti020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Mukherjee PP, Palamar JJ. Multi-level modeling to explain methamphetamine use among gay and bisexual men. Addiction. 2007;102(Suppl. 1):76–83. doi: 10.1111/j.1360-0443.2007.01769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: crystal methamphetamine drug use in relation to HIV transmission among gay men. J. Homosex. 2001;41:17–35. doi: 10.1300/J082v41n02_02. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Shrem MT. Psychological differences between binge and chronic methamphetamine using gay and bisexual men. Addict. Behav. 2006;31:549–552. doi: 10.1016/j.addbeh.2005.05.040. [DOI] [PubMed] [Google Scholar]
- Hinkin CH, Barclay TR, Castellon SA, Levine AJ, Durvasula RS, Marion SD, Myers HF, Longshore D. Drug use and medication adherence among HIV-1 infected individuals. AIDS Behav. 2007;11:185–194. doi: 10.1007/s10461-006-9152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol. Methods. 1998:424–453. [Google Scholar]
- Johnson MO, Carrico AW, Chesney MA, Morin SF. Internalized heterosexism among HIV-positive, gay-identified men: implications for HIV prevention and care. J. Consult. Clin. Psychol. 2008;76:829–839. doi: 10.1037/0022-006X.76.5.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC. Co-occurrence of treatment nonadherence and continued HIV transmission risk behaviors: implications for positive pervention interventions. Psychosom. Med. 2008;70:593–597. doi: 10.1097/PSY.0b013e3181773bce. [DOI] [PubMed] [Google Scholar]
- Kalton G. Introduction to Survey Sampling. Sage Publications, Inc.; London, UK: 1983. [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Barresi PJ, Coates TJ, Chesney MA, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Mansergh G, Koblin BA, McKirnan DJ, Hudson SM, Flores SA, Wiegand RE, Purcell DW, Colfax GN. An intervention to reduce HIV risk behavior of substance-using men who have sex with men: a two-group randomized trial with a nonrandomized third group. PLoS. Med. 2010;7:e1000329. doi: 10.1371/journal.pmed.1000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moggi F, Ouimette PC, Moos RH, Finney JW. Dual diagnosis patients in substance abuse treatment: relationship of general coping and substance-specific coping to 1-year outcomes. Addiction. 1999;94:1805–1816. doi: 10.1046/j.1360-0443.1999.941218056.x. [DOI] [PubMed] [Google Scholar]
- Morin SF, Myers JJ, Shade SB, Koester K, Maiorana A, Rose CD. Predicting HIV transmission risk among HIV-infected patients seen in clinical settings. AIDS Behav. 2007;11:S6–16. doi: 10.1007/s10461-007-9253-4. [DOI] [PubMed] [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychol. Bull. 2000;126:247–259. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén B. How to use a Monte Carlo Study to decide on sample size and determine power. Struct. Equ. Modeling. 2004;4:599–620. [Google Scholar]
- Ostrow DG, Plankey MW, Cox C, Li X, Shoptaw S, Jacobson LP, Stall RC. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J. Aquir. Immune Defic. Syndr. 2009;51:349–355. doi: 10.1097/QAI.0b013e3181a24b20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Mukherjee PP, Halkitis PN. A longitudinal investigation of powder cocaine use among club-drug using gay and bisexual men. J. Stud. Alcohol Drugs. 2008;69:806–813. doi: 10.15288/jsad.2008.69.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantalone DW, Bimbi DS, Holder CA, Golub SA, Parsons JT. Consistency and change in club drug use by sexual minority men in New York City, 2002 to 2007. Am. J. Public Health. 2010;100:1892–1895. doi: 10.2105/AJPH.2009.175232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Bimbi DS. Intentional unprotected anal intercourse among sex who have sex with men: barebacking - from behavior to identity. AIDS Behav. 2007;11:277–287. doi: 10.1007/s10461-006-9135-1. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Arch. Sex. Behav. 2008;37:817–826. doi: 10.1007/s10508-007-9218-8. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Kelly BC, Bimbi DS, Muench F, Morgenstern J. Accounting for the social triggers of sexual compulsivity. J. Addict. Dis. 2007;26:5–16. doi: 10.1300/J069v26n03_02. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. J. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Semple SJ, Zians J, Grant I, Patterson TL. Sexual compulsivity in a sample of HIV-positive methamphetamine-using gay and bisexual men. AIDS Behav. 2006;10:587–598. doi: 10.1007/s10461-006-9127-1. [DOI] [PubMed] [Google Scholar]
- Shoptaw S. Substance abuse treatment as HIV prevention for men who have sex with men. AIDS Behav. 2000;4:193–203. [Google Scholar]
- Shoptaw S, Reback CJ. Methamphetamine use and infectious disease-related behaviors in men who have sex with men: implications for interventions. Addiction. 2007;102(Suppl. 1):130–135. doi: 10.1111/j.1360-0443.2006.01775.x. [DOI] [PubMed] [Google Scholar]
- Snell WE, Papini DR. The sexuality scales: an instrument to measure sexual-esteem, sexual-depression, and sexual-preoccupation. J. Sex. Res. 1989;26:256–263. [Google Scholar]
- Vaudrey J, Raymond HF, Chen S, Hecht J, Ahrens K, McFarland W. Indicators of use of methamphetamine and other substances among men who have sex with men, San Francisco, 2003-2006. Drug Alcohol Depend. 2007;90:97–100. doi: 10.1016/j.drugalcdep.2007.02.020. [DOI] [PubMed] [Google Scholar]