Abstract
Background
In the era of anti-retroviral therapy (ART), depression and substance use predict hastened HIV disease progression but the underlying biological or behavioral mechanisms that explain these effects are not fully understood.
Methods
Using outcome data from 603 participants enrolled in a randomized controlled trial of a behavioral intervention, binary logistic and linear regression were employed to examine whether inconsistent patterns of ART utilization partially mediated the effects of depression and substance use on higher HIV viral load over a 25-month follow-up.
Results
Elevated affective symptoms of depression independently predicted ART discontinuation (Adjusted OR [AOR] = 1.39, 95% CI = 1.08 – 1.78), and use of stimulants at least weekly independently predicted intermittent ART utilization (AOR = 2.62, 95% CI = 1.45 – 4.73). After controlling for the average self-reported percentage of ART doses taken and baseline T-helper (CD4+) count, elevated depressive symptoms predicted a 50% higher mean viral load, and weekly stimulant use predicted a 137% higher mean viral load. These effects became non-significant after accounting for inconsistent patterns of ART utilization, providing evidence of partial mediation.
Conclusions
Inconsistent patterns of ART utilization may partially explain the effects of depression and stimulant use on hastened HIV disease progression.
Keywords: Access, Adherence, Antiretroviral, Cocaine, Depression, Disease Progression, Highly Active, HIV/AIDS, HIV Viral Load, Methamphetamine, Substance Use, Utilization
Introduction
In the era of anti-retroviral therapy (ART), depression predicts T-helper (CD4+) count decline, increases in HIV viral load, impaired responses to ART, faster development of an AIDS-defining illness, and hastened AIDS-related mortality.1 Although depression is associated with non-adherence to medical treatment, the effects of depression on HIV disease markers, development of an AIDS-defining illness, and mortality remain after accounting for the self-reported percentage of ART medication doses taken.2, 3 Similarly, the use of stimulants (i.e., cocaine, crack, and methamphetamine) or heroin independently predicts more rapid CD4+ count decline and elevated HIV viral load, faster development of an opportunistic infection, and hastened AIDS-related or all-cause mortality 4-7 Stimulant use also predicts more rapid HIV disease progression after controlling for the percentage of ART medication doses taken,4, 7 which is interesting given that stimulant users are substantially less likely to achieve adequate levels of ART adherence.8 Inconsistent patterns of ART utilization, another important marker of non-adherence, may partially account for these effects of depression and substance use on hastened HIV disease progression. Depression predicts inconsistent ART utilization as well as increased odds of ART discontinuation,9, 10 and one recent investigation observed that the effect of depression on hastened all cause mortality is most pronounced among those who inconsistently utilize ART.11 On the other hand, substance users are more likely to receive intermittent or no HIV medical care, 12 and this may explain lower observed rates of ART utilization.7 The overarching goal of the present investigation was to examine whether inconsistent ART utilization is on the causal pathway linking psychiatric co-morbidities to more rapid HIV disease progression. Specifically, we investigated whether inconsistent patterns of ART utilization mediated the effects of depression and substance use on higher HIV viral load.
Methods
The NIMH Healthy Living Project was multi-site randomized controlled trial of a behavioral intervention designed to reduce HIV transmission risk behavior. Participants completed follow-up assessments every 5 months for 25 months. Peripheral venous blood samples were obtained at baseline as well as at the 10, 15, and 25 month follow-up visits. Detailed information regarding the eligibility criteria, participant characteristics, and intervention effects on the primary outcome measure (HIV transmission risk) has been published elsewhere.13
Measures
Demographics
Age, ethnicity, gender, education, and sexual orientation were assessed by questionnaire.
Depressive Symptoms
The 21-item Beck Depression Inventory I (BDI) assessed the severity depressive symptoms during the past week.14 Because somatic depressive symptoms and HIV symptoms are confounded, a modified 12-item BDI-Affective (i.e., sadness, pessimism, failure, decreased satisfaction, guilt, punishment, disappointment, self-blame, suicide, crying, irritation, and decreased interest) subscale was computed (Cronbach’s α = .85).
Substance Use
Participants rated their use of various substances during the past 3 months from 0 (never) to 7 (daily). Those who reported using stimulants (cocaine, crack, or methamphetamine) at least weekly were compared to participants who reported using 2-3 times a month or less. Rates of heroin use were low in this sample, and participants reporting any heroin use were compared to those who reported none.
Percentage of ART Doses Taken
Self-reported percentage of ART doses taken during the past three days was measured at each assessment visit.15 Using all available data provided by participants in 6 assessments over 25 months, the average self-reported percentage of pills taken was calculated.
ART Utilization Patterns
At each assessment, participants reported whether they were currently taking ART. Individuals were classified as engaging in 3 distinct patterns of ART utilization:
continuous ART utilization - being on ART at baseline and remaining on ART;
ART discontinuation - stopping ART and remaining off during any subsequent follow-up assessments; and 3) intermittent ART utilization - stopping and restarting ART at least once.
HIV Disease Markers
HIV-1 viral load was determined using the AMPLICOR ultrasensitive method for the in vitro reverse transcriptase polymerase chain reaction assay (Roche Laboratories, US # 83088), which has a valid range of 50 to 750,000 copies/ml. CD4+ count was determined using direct immunoflourescence.
Statistical Analyses
In order to have sufficient observed data to characterize patterns of ART utilization, only participants who completed at least 3 of the 6 assessments (85% of the total sample) were examined to determine eligibility for the present study. Participants who reported being continuously off ART (n = 191) were excluded. In total, 603 participants who reported ART discontinuation (n = 120), intermittent ART utilization (n =142), or continuous ART utilization (n = 341) were included in the present analyses. Those who reported ART discontinuation and intermittent ART utilization were compared in separate multiple logistic regression analyses to the reference group of individuals who were continuously on ART. The composite score for affective symptoms of depression was transformed into a z-score (M = 0, SD = ± 1), so that the odds ratio reflects the increased odds of each pattern of inconsistent ART utilization per 1 standard deviation increase. Finally, using hierarchical linear regression, inconsistent patterns of ART utilization were examined as mediators of the effects of depressive symptoms and weekly stimulant use on mean log10 HIV viral load in the 25 months after baseline (i.e., average of the 10, 15, and 25 month follow-up assessments). Using a simple formula [100(10Beta − 1)], unstandardized parameter estimates were converted to determine the percent increase in mean HIV viral load.
Results
Participant Demographics
The mean age of the 603 participants included in these analyses was 40.6 (range 19–66) years. Most participants were male (80%) and 70% identified as lesbian, gay, bisexual, or questioning (LGBQ). Fifty-four percent of participants were African American, 25% were Caucasian, and 14% were Hispanic/Latino. Fifty-eight percent reported attending at least some college and 11% reported being homeless in the past year. At baseline, 94% of participants were on ART, 33% had an undetectable HIV viral load, and the mean CD4+ count was 415 (SD = 271) cells/μl. On average, participants reported taking 88% (SD = 16) of prescribed ART doses using all available data from the six assessments across the 25-month investigation period. At baseline, approximately one-fifth (18%) reported at least weekly stimulant use, 5% reported any heroin use, and 12% reported any injection drug use in the past year.
Predictors of Inconsistent Patterns of ART Utilization
Elevated affective symptoms of depression at baseline independently predicted a 39% increase in the odds of ART discontinuation (See Table 1). As shown in Table 2, weekly stimulant use at baseline independently predicted more than a 2.5-fold increase in the odds of intermittent ART utilization (51% vs. 25%). There were no effects of the Healthy Living Project intervention on ART discontinuation (OR = 1.12, 95% CI = 0.74 – 1.70) or intermittent ART utilization (OR = 1.09, 95% CI = 0.74 – 1.61).
Table 1.
Baseline Predictors of ART Discontinuation (n = 461)
| OR | 95% CI | AOR | 95% CI | |
|---|---|---|---|---|
| Caucasian | Reference | Reference | ||
| African American | 2.00** | 1.20 – 3.31 | 1.37 | 0.74 – 2.52 |
| Hispanic/Latino | 1.74 | 0.89 – 3.39 | 1.98 | 0.92 – 4.27 |
| Other Ethnic Minority | 2.51* | 1.08 – 5.83 | 3.10* | 1.17 – 8.23 |
| LGBQ | 0.68 | 0.43 – 1.07 | ||
| Male | 0.61 | 0.36 – 1.03 | ||
| Age (decade) | 0.64** | 0.48 – 0.86 | 0.65* | 0.46 – 0.94 |
| Did not Graduate High School | Reference | Reference | ||
| High School Graduate | 0.85 | 0.46 – 1.57 | 1.06 | 0.51 – 2.20 |
| At Least Some College | 0.49** | 0.29 – 0.84 | 0.84 | 0.43 – 1.64 |
| HIV Viral Load (log10) | 1.58** | 1.33 – 1.87 | 1.62** | 1.36 – 1.94 |
| CD4+ < 200 cells/μl | 1.19 | 0.68 – 2.08 | ||
| Depressive Symptoms | 1.29* | 1.05 – 1.59 | 1.39** | 1.08 – 1.78 |
| Weekly Stimulant Use | 1.55 | 0.88 – 2.72 | ||
| Any Heroin Use | 1.86 | 0.70 – 4.91 |
p > .05;
p ≤ .01;
OR = Odds Ratio; AOR = Adjusted Odds Ratio; CI = Confidence Interval; LGBQ = Lesbian, Gay, Bisexual, or Questioning
Table 2.
Baseline Predictors of Intermittent ART Utilization (n = 483)
| OR | 95% CI | AOR | 95% CI | |
|---|---|---|---|---|
| Caucasian | Reference | |||
| African American | 1.53 | 0.98 – 2.39 | ||
| Hispanic/Latino | 0.95 | 0.49 – 1.84 | ||
| Other Ethnic Minority | 1.49 | 0.65 – 3.43 | ||
| LGBQ | 0.50** | 0.33 – 0.76 | 0.65 | 0.35 – 1.23 |
| Male | 0.39** | 0.24 – 0.62 | 0.57 | 0.28 – 1.15 |
| Age (decade) | 0.71* | 0.54 – 0.94 | 0.70* | 0.50 – 0.99 |
| Did not Graduate High School | Reference | |||
| High School Graduate | 0.90 | 0.49 – 1.63 | ||
| At Least Some College | 0.62 | 0.37 – 1.04 | ||
| HIV Viral Load (log10) | 1.68** | 1.43 – 1.97 | 1.68** | 1.40 – 2.02 |
| CD4+ < 200 cells/μl | 2.13** | 1.32 – 3.44 | 1.08 | 0.60 – 1.92 |
| Depressive Symptoms | 1.18 | 0.97 – 1.43 | ||
| Weekly Stimulant Use | 3.10** | 1.92 – 5.00 | 2.62** | 1.45 – 4.73 |
| Any Heroin Use | 2.77* | 1.19 – 6.43 | 1.34 | 0.44 – 4.12 |
p > .05;
p < .01;
OR = Odds Ratio; AOR = Adjusted Odds Ratio; CI = Confidence Interval; LGBQ = Lesbian, Gay, Bisexual, or Questioning
ART Utilization Patterns Mediate the Effects of Depression and Stimulant Use on Viral Load
There were no effects of the Healthy Living Project intervention on mean HIV viral load over follow-up (t (538) = -0.21, p > .10). Consequently, intervention assignment was not included in subsequent analyses. As shown in Figure 1, elevated affective symptoms of depression at baseline predicted a 50% higher mean HIV viral load in the 25 months following baseline (β = .13, p < .01) after controlling for the effects of baseline CD4+ count (β = -.19, p < .001) and average self-reported percentage of ART doses taken (β = -.20, p < .001). After accounting for the increased odds of ART discontinuation among individuals with elevated affective symptoms of depression, the effect of depression on higher mean viral load was no longer significant (21% higher viral load; β = .06, p > .10). Similarly, weekly stimulant use at baseline predicted a 137% higher mean viral load (β = .12, p < .05) after controlling for the effects of baseline CD4+ count (β = -.21, p < .001) and average self-reported percentage of ART doses taken (β = -.30, p < .001). After accounting for the increased odds of intermittent ART utilization among weekly stimulant users, the effect of weekly stimulant use on higher mean viral load was no longer significant (59% higher viral load; β = .06, p > .10). Taken together, these results are indicative of partial mediation.
Figure 1.
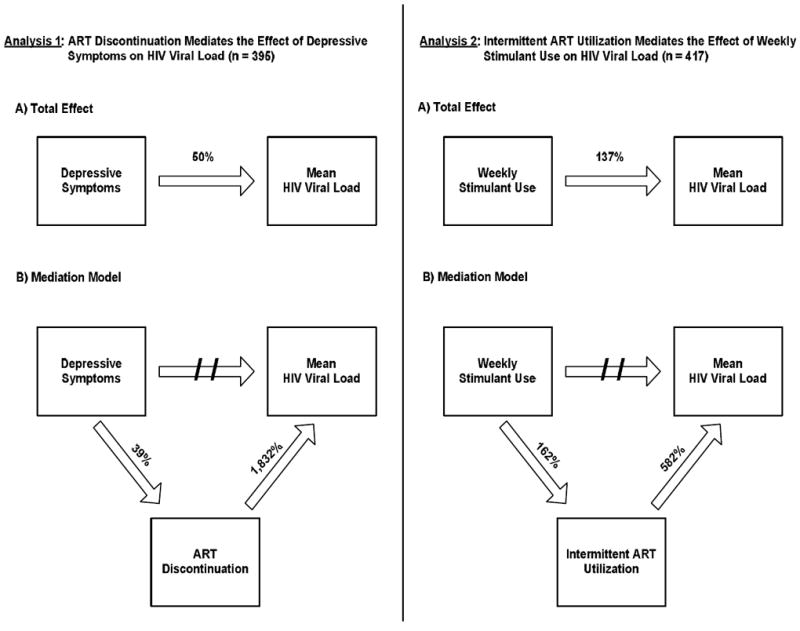
Inconsistent ART utilization patterns explain the effects of depressive symptoms and weekly stimulant use on mean HIV viral load.
Total Effect = Percent increase in HIV viral load after controlling for average self-reported percentage of ART doses taken and baseline CD4+ count; Mediation Model = Inconsistent patterns of ART utilization act as a mechanisms for the effects of depressive symptoms and weekly stimulant use on higher mean HIV viral load; Mean HIV Viral Load = Average HIV viral load in the 25 months following baseline; Percentages = reflect the percent increase in the odds of inconsistent ART utilization patterns or the percent increase in mean log10 HIV viral load
Discussion
The present study observed that inconsistent patterns of ART utilization account for the effects of depression and stimulant use on higher HIV viral load. There is increasing interest in promoting universal voluntary counseling and testing for HIV followed by immediate initiation of ART to reduce HIV transmission rates by lowering community viral load.16 Findings from the present study indicate that adjuvant mental health and substance abuse treatment will be needed to promote sustained ART utilization, achieve viral suppression, and address HIV transmission risk behavior among individuals with psychiatric co-morbidities. In the context of HIV medical care, this will require implementation of rapid screening tools for depression and substance abuse, as well as efficient methods for linkage to mental health and/or substance abuse treatment. Although findings from the present study indicate that inconsistent ART utilization partially explains the effects of depression and stimulant use on higher HIV viral load, this does not rule out other plausible biological or behavioral pathways. It is noteworthy that some investigations conducted in the era prior to ART observed that depression and substance use predicted more rapid HIV disease progression.1, 17 Psychological stress and stimulant use activate the hypothalamic-pituitary-adrenal (HPA) axis as well as the autonomic nervous system, leading to enhanced secretion of immunomodulatory hormones (e.g., cortisol and norepinephrine). In addition, other behavioral factors such as sleep dysregulation and poor nutrition could partially explain the effects of depression and stimulant use on more rapid HIV disease progression. Future research should examine other plausible bio-behavioral pathways that may partially account for the effects of these psychiatric risk factors for HIV disease progression in order to inform the development of more comprehensive intervention efforts aimed at optimizing health outcomes among HIV-positive persons.
This investigation also observed that greater depressive symptom severity and at least weekly stimulant use were linked to higher viral load via specific patterns of inconsistent ART utilization. Those with elevated depressive symptom severity may be more likely to discontinue ART regimens due to the pervasive sense of hopelessness and pessimism that are common features of depression. In fact, discontinuation of ART could be a para-suicidal behavior and a thorough assessment of suicidality may be warrented.18 Intermittent ART utilization may be more common among stimulant users because stochastic periods of binge use are common in this population.19 Individuals may be more likely to stop taking ART regimens during periods of binge stimulant use but then re-initiate ART during periods of less frequent stimulant use or abstinence. Further research is needed to elucidate the underlying psychological and/or behavioral mechanisms whereby depression and stimulant use are linked to inconsistent patterns of ART utilization.
The Healthy Living Project was a randomized controlled trial of a behavioral intervention designed to reduce HIV transmission risk, and only individuals who reported engaging in HIV transmission risk behavior or unprotected intercourse with a non-primary HIV-positive partner were enrolled.13 Because individuals in this trial reported engaging in sexual risk taking, this may have selected for a cohort that was more vulnerable to engaging in other health risk behaviors such as inconsistent ART utilization. Further research with more representative cohorts of HIV-positive persons should determine if inconsistent patterns of ART utilization explain the effects of depression and stimulant use on HIV viral load, progression to AIDS, and mortality. However, the fact that the majority of individuals enrolled in this trial reported engaging in HIV transmission risk underscores the potential public health significance of adjuvant psychological and behavioral interventions to lower HIV viral load. Achieving viral suppression among HIV-positive individuals who are engaging in transmission risk behavior is crucial if “Test and Treat” approaches to HIV prevention are to be effective.16 However, it is likely that adjuvant mental health and substance abuse treatment to address psychiatric co-morbidities as well as behavioral interventions to promote engagement in HIV medical care will only be partially effective in achieving viral suppression. Prevention counseling to address ongoing HIV transmission risk behavior remains an important component of multi-faceted HIV prevention efforts, particularly among high risk populations that do not achieve viral suppression despite our best efforts to promote sustained ART utilization and adherence.
Acknowledgments
This research was funded by National Institute of Mental Health grants U10-MH57636, U10- MH57631, U10-MH57616, and U10-MH57615; and NIMH center grants P30-MH058107 (Mary Jane Rotheram-Borus, Ph.D., PI), P30-MH57226 (Jeffrey A. Kelly, Ph.D., PI), P30-MH43520 (Anke A. Ehrhardt, Ph.D., PI), and P30-MH062246 (Thomas J. Coates, Ph.D., PI).
The authors thank those at NIMH: Ellen Stover, Ph.D, and Willo Pequegnat, Ph.D., for their technical assistance in developing the study, and Christopher M. Gordon, Ph.D., and Dianne Rausch, Ph.D., for their support of this research. Gratitude is also given to F. Lennie Wong, Ph.D., Susan Tross, Ph.D., and Gary Dowsett, Ph.D. for their methodological guidance as well as data management expertise, to the assessors in each city who conducted the interviews, to our clinic and community based organization collaborators, to all other support staff involved in the project, and to the men and women who participated in the interviews.
References
- 1.Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom Med. 2008 Jun;70(5):539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- 2.Anastos K, Schneider MF, Gange SJ, et al. The association of race, sociodemographic, and behavioral characteristics with response to highly active antiretroviral therapy in women. J Acquir Immune Defic Syndr. 2005 Aug 15;39(5):537–544. [PubMed] [Google Scholar]
- 3.Antoni MH, Carrico AW, Duran RE, et al. Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosom Med. 2006 Jan-Feb;68(1):143–151. doi: 10.1097/01.psy.0000195749.60049.63. [DOI] [PubMed] [Google Scholar]
- 4.Cook JA, Burke-Miller JK, Cohen MH, et al. Crack cocaine, disease progression, and mortality in a multicenter cohort of HIV-1 positive women. AIDS. 2008 Jul 11;22(11):1355–1363. doi: 10.1097/QAD.0b013e32830507f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lucas GM, Griswold M, Gebo KA, Keruly J, Chaisson RE, Moore RD. Illicit drug use and HIV-1 disease progression: a longitudinal study in the era of highly active antiretroviral therapy. Am J Epidemiol. 2006 Mar 1;163(5):412–420. doi: 10.1093/aje/kwj059. [DOI] [PubMed] [Google Scholar]
- 6.Kapadia F, Cook JA, Cohen MH, et al. The relationship between non-injection drug use behaviors on progression to AIDS and death in a cohort of HIV seropositive women in the era of highly active antiretroviral therapy use. Addiction. 2005 Jul;100(7):990–1002. doi: 10.1111/j.1360-0443.2005.01098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrico AW. Substance use and HIV disease progression in the HAART era: Implications for the primary prevention of HIV infection. Life Sci. doi: 10.1016/j.lfs.2010.10.002. in press. [DOI] [PubMed] [Google Scholar]
- 8.Carrico AW, Johnson MO, Moskowitz JT, et al. Affect regulation, stimulant use, and viral load among HIV-positive persons on anti-retroviral therapy. Psychosom Med. 2007 Nov 15;69(8):785–792. doi: 10.1097/PSY.0b013e318157b142. [DOI] [PubMed] [Google Scholar]
- 9.Li X, Margolick JB, Conover CS, et al. Interruption and discontinuation of highly active antiretroviral therapy in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2005 Mar 1;38(3):320–328. [PubMed] [Google Scholar]
- 10.Cook JA, Cohen MH, Burke J, et al. Effects of depressive symptoms and mental health quality of life on use of highly active antiretroviral therapy among HIV-seropositive women. J Acquir Immune Defic Syndr. 2002 Aug 1;30(4):401–409. doi: 10.1097/00042560-200208010-00005. [DOI] [PubMed] [Google Scholar]
- 11.Lima VD, Geller J, Bangsberg DR, et al. The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. AIDS. 2007 May 31;21(9):1175–1183. doi: 10.1097/QAD.0b013e32811ebf57. [DOI] [PubMed] [Google Scholar]
- 12.Giordano TP, Gifford AL, White AC, Jr, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007 Jun 1;44(11):1493–1499. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 13.Healthy Living Project Team. Effects of a behavioral intervention to reduce risk of transmission among people living with HIV: the healthy living project randomized controlled study. J Acquir Immune Defic Syndr. 2007 Feb 1;44(2):213–221. doi: 10.1097/QAI.0b013e31802c0cae. [DOI] [PubMed] [Google Scholar]
- 14.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996 Dec;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 15.Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000 Jun;12(3):255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 16.Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA. 2009 Jun 10;301(22):2380–2382. doi: 10.1001/jama.2009.828. [DOI] [PubMed] [Google Scholar]
- 17.Kapadia F, Vlahov D, Donahoe RM, et al. The role of substance abuse in HIV disease progression: reconciling differences from laboratory and epidemiologic investigations. Clin Infect Dis. 2005;41:1027–1034. doi: 10.1086/433175. [DOI] [PubMed] [Google Scholar]
- 18.Carrico AW. Elevated suicide rate among HIV-positive persons despite the benefits of antiretroviral therapy: Implications for a stress and coping model of suicide. Am J Psychiatry. 2010;167(2):117–119. doi: 10.1176/appi.ajp.2009.09111565. [DOI] [PubMed] [Google Scholar]
- 19.Cheng WS, Garfein RS, Semple SJ, et al. Binge use and drug use behaviors among HIV(-), heterosexual methamphetamine users in San Diego. Subst Use Misuse. 2010;45(1-2):116–133. doi: 10.3109/10826080902869620. [DOI] [PMC free article] [PubMed] [Google Scholar]


