Abstract
BACKGROUND
Consumption of sugar-sweetened beverages may cause excessive weight gain. We aimed to assess the effect on weight gain of an intervention that included the provision of noncaloric beverages at home for overweight and obese adolescents.
METHODS
We randomly assigned 224 overweight and obese adolescents who regularly consumed sugar-sweetened beverages to experimental and control groups. The experimental group received a 1-year intervention designed to decrease consumption of sugar-sweetened beverages, with follow-up for an additional year without intervention. We hypothesized that the experimental group would gain weight at a slower rate than the control group.
RESULTS
Retention rates were 97% at 1 year and 93% at 2 years. Reported consumption of sugar-sweetened beverages was similar at baseline in the experimental and control groups (1.7 servings per day), declined to nearly 0 in the experimental group at 1 year, and remained lower in the experimental group than in the control group at 2 years. The primary outcome, the change in mean body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) at 2 years, did not differ significantly between the two groups (change in experimental group minus change in control group, −0.3; P = 0.46). At 1 year, however, there were significant between-group differences for changes in BMI (−0.57, P = 0.045) and weight (−1.9 kg, P = 0.04). We found evidence of effect modification according to ethnic group at 1 year (P = 0.04) and 2 years (P = 0.01). In a prespecified analysis according to ethnic group, among Hispanic participants (27 in the experimental group and 19 in the control group), there was a significant between-group difference in the change in BMI at 1 year (−1.79, P = 0.007) and 2 years (−2.35, P = 0.01), but not among non-Hispanic participants (P>0.35 at years 1 and 2). The change in body fat as a percentage of total weight did not differ significantly between groups at 2 years (−0.5%, P = 0.40). There were no adverse events related to study participation.
CONCLUSIONS
Among overweight and obese adolescents, the increase in BMI was smaller in the experimental group than in the control group after a 1-year intervention designed to reduce consumption of sugar-sweetened beverages, but not at the 2-year follow-up (the prespecified primary outcome). (Funded by the National Institute of Diabetes and Digestive and Kidney Diseases and others; ClinicalTrials.gov number, NCT00381160.)
The consumption of sugar-sweetened beverages among adolescents1 has increased in tandem with the prevalence of pediatric obesity in the United States,2 suggesting a causal relationship. At present, a substantial proportion of high-school students habitually consume sugar-sweetened beverages, including carbonated soda, sports drinks, energy drinks, and highly sweetened coffees and teas.3 Sugar-sweetened beverages are the leading source of added sugar in the diet of a wide range of racial and ethnic groups.4 According to nationally representative data, overweight and obese adolescents obtain more than 300 kcal per day from these products, amounting to an average of 15% of their total daily energy intake.5
Short-term feeding studies show greater energy intake and weight gain with the consumption of sugar-sweetened beverages than with beverages containing artificial sweeteners,6 and prospective observational studies show positive associations with the risk of obesity and related complications.7 However, the findings from the relatively few randomized, controlled trials designed to examine the effects of sugar-sweetened beverages on body weight have not been conclusive,8–10 and the use of public health measures to reduce the consumption of sugar-sweetened beverages remains controversial.11,12
We previously conducted a 6-month pilot study10 involving normal-weight, overweight, and obese adolescents who consumed sugar-sweetened beverages habitually. The experimental group received home delivery of noncaloric beverages, and the control group did not. The mean body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) decreased significantly in the experimental group, as compared with the control group, only among the overweight and obese adolescents. The current study, which is a follow-up to the pilot study,10 was designed to test the hypothesis that overweight and obese adolescents who received an intervention to reduce the consumption of sugar-sweetened beverages would gain weight at a slower rate than those who did not receive the intervention. We examined prespecified covariates as potential effect modifiers and mediators. In addition, we reanalyzed data from an observational study13 involving 548 middle-school students to corroborate the findings of the current study.
METHODS
STUDY DESIGN
We randomly assigned participants to an experimental group or a control group for 2 years. The study included a 1-year intervention and a 1-year follow-up, with assessment of study outcomes at the end of each period. The institutional review board at Boston Children’s Hospital approved the study protocol (available with the full text of this article at NEJM.org). Parents provided written informed consent, and participants provided written assent. Beverages for the intervention group were purchased from an online delivery service (Peapod) affiliated with a supermarket chain. The study was conducted between October 2007 and December 2011. The first two authors and the last author vouch for the accuracy and completeness of the data and analysis and the fidelity of the study to the protocol.
PARTICIPANTS
We enrolled 224 adolescents (124 boys and 100 girls) who reported consuming at least one serving (12 oz) per day of sugar-sweetened beverages or 100% fruit juice. Additional inclusion criteria were enrollment in grade 9 or 10 and a BMI at or above the 85th percentile for sex and age.14 During telephone conversations with parents, we collected demographic information, including sex, date of birth, race (white, black, Asian, multiple, or other), ethnic group (Hispanic or non-Hispanic), parents’ level of education, and total annual household income.
INTERVENTION
We used a multicomponent intervention designed to reduce the consumption of sugar-sweetened beverages in the experimental group. The emphasis was on displacing sugar-sweetened beverages with noncaloric beverages in the home as a strategy to decrease consumption.5 The 1-year intervention consisted of home delivery of noncaloric beverages (e.g., bottled water and “diet” beverages) every 2 weeks, monthly motivational telephone calls with parents (30 minutes per call), and three check-in visits with participants (20 minutes per visit). Written intervention messages with instructions to drink the delivered beverages and not to buy or drink sugar-sweetened beverages were mailed to participants. Unsweetened water was recommended over artificially sweetened beverages. Discussions during telephone calls and check-in visits focused exclusively on beverage consumption, with no attention to other dietary behaviors or to physical activity. We mailed $50 supermarket gift cards to participants in the control group at 4 and 8 months as a retention strategy but did not provide instructions on what to purchase with the cards.
OUTCOMES
All personnel who assessed study outcomes were unaware of the group assignments. The primary outcome was the change in BMI at 2 years. To calculate BMI, trained personnel measured weight and height using calibrated scales and stadiometers, respectively. We used data from bioelectrical impedance analysis (BIA) and the equation of Sun et al.15 to calculate body fat as a percentage of total body weight. In three telephone interviews conducted at each assessment (baseline, 1 year, and 2 years), participants were asked to recall their dietary intake and physical activity during the preceding 24 hours. Dietary intake data were collected with Nutrition Data System for Research (NDSR) software, versions 2006 through 2011, developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis. Final calculations were completed with NDSR, version 2011. Variables used to assess dietary quality included reported daily servings of sugar-sweetened, artificially sweetened, and unsweetened beverages; servings of 100% fruit juices; total energy and sugar intakes; and energy intake from sugar-sweetened beverages and 100% fruit juices. The interviewer also asked each participant to recall the activity performed most often during each 15-minute block throughout the previous day.16,17 We calculated a daily physical-activity factor, using metabolic equivalent (MET) levels for each reported activity,18 and hours of television viewing.
ADVERSE EVENTS
An adverse event was defined as any symptom or safety concern requiring medical attention that was reported by an adolescent or a parent during participation in the study.
STATISTICAL ANALYSIS
The trial was designed to have 80% power at a type I error rate of 5% to detect a net intervention effect with respect to the primary outcome BMI of 0.49, as attained with a shorter intervention in our pilot study.10 All analyses followed the intention-to-treat principle. Baseline demographic characteristics, dietary intake, and obesity-related behavioral variables were compared between the experimental and control groups with the use of Student’s t-test and Fisher’s exact test for continuous and categorical variables, respectively. Changes in BMI and other anthropometric outcomes were compared between groups with a general linear model, adjusted for baseline covariates that could affect body weight. We performed identical but separate analyses for the change from baseline after 1 year (intervention period) and the change from baseline after 2 years (follow-up period without further intervention). Dietary intakes and obesity-related behavioral outcomes were analyzed similarly, without adjustment for covariates. Residual analysis confirmed that the assumption of normal error was satisfied. The net intervention effect (the mean change in the experimental group minus the mean change in the control group) was calculated from the parameters of the fitted model.
We tested each covariate for interaction and, finding Hispanic ethnic group to be the sole significant effect modifier for between-group differences in the change in BMI, we constructed additional ethnicity-specific summary statistics for the anthropometric and behavioral outcomes from a model that included an interaction term for study group and ethnic group. Testing 14 covariates for effect modification with a critical value of P<0.05 gave us an expected number of 0.7, or less than 1, type I error for each time point. Missing values for BMI were conservatively imputed by assuming that the participant’s BMI z score was unchanged from baseline and calculating BMI at the appropriate later age from national norms.14 Other methods for treating missing data, including use of the immediately preceding BMI z score, produced similar results.
We also reanalyzed data from a 19-month prospective observational study of 548 ethnically diverse middle-school students13 to test for effect modification by ethnic group in the association of a change in the consumption of sugar-sweetened beverages with a change in BMI. We added an interaction term for ethnic group and change in consumption of sugar-sweetened beverages to the fully adjusted model. This regression included covariates related to diet (change in consumption of sugar-sweetened beverages, adjusted for total energy intake and controlled for baseline consumption; baseline fat and change in fat, expressed as a percentage of total energy intake; and baseline energy-adjusted intake of fruit juice and change in fruit-juice intake), demographic characteristics (age, sex, ethnic group, and race, with indicator variables for schools), anthropometric variables (BMI and triceps skin-fold thickness), physical activity (exercising to lose weight at baseline [yes or no], number of physical-education classes per week at baseline, and baseline physical activity [<3 METs vs. ≥3.5 METs] and change in physical activity), and hours of daily television viewing (baseline and change).
SAS software (version 9.2) was used for all computations. A two-sided P value of 0.05 or less was interpreted as a statistically significant result.
RESULTS
STUDY POPULATION
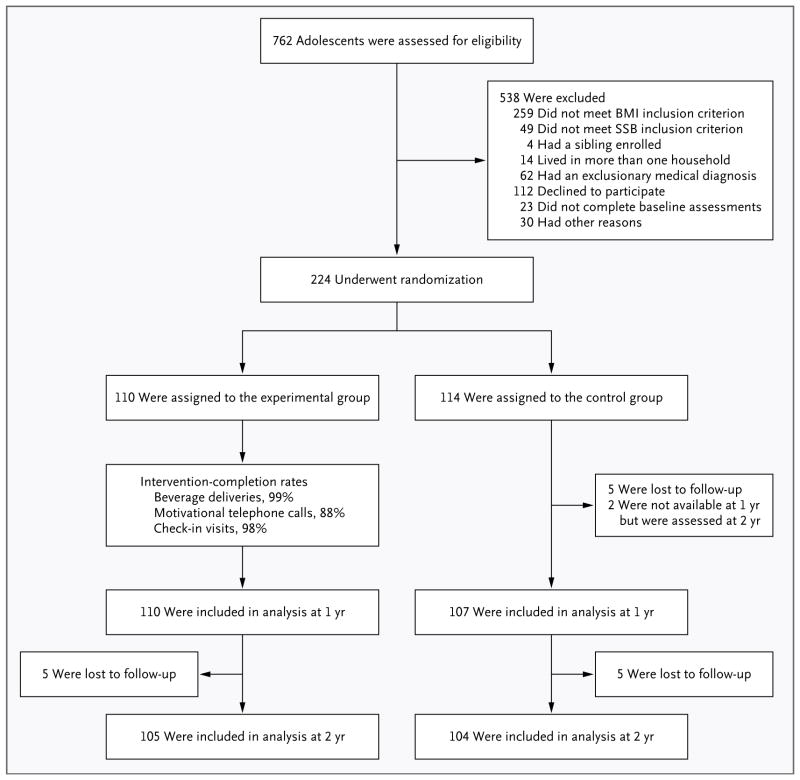
At baseline, there were no significant differences between the experimental and control groups with regard to demographic characteristics (Table 1) or other variables (Tables 2 and 3). The retention rate for study participants was 97% at 1 year and 93% at 2 years (Fig. 1), with no significant difference between groups in the percentage of participants available at 2 years for assessment of the primary outcome (P = 0.29).
Table 1.
Baseline Characteristics of the Study Participants.*
| Characteristic | Experimental Group (N = 110) | Control Group (N = 114) | P Value |
|---|---|---|---|
| Sex — no. (%) | |||
| Male | 58 (53) | 66 (58) | 0.50 |
| Female | 52 (47) | 48 (42) | |
| Race or ethnic group — no. (%)† | |||
| Race | |||
| White | 60 (55) | 64 (56) | 0.99 |
| Black | 26 (24) | 27 (24) | |
| Asian | 4 (4) | 4 (4) | |
| Multiple or other | 20 (18) | 19 (17) | |
| Ethnic group | |||
| Hispanic | 27 (25) | 19 (17) | 0.19 |
| Non-Hispanic | 83 (75) | 95 (83) | |
| Age — yr | 15.3±0.7 | 15.2±0.7 | 0.50 |
| Weight — kg | 85.2±16.8 | 86.1±17.0 | 0.70 |
| Height — cm | 167.4±8.8 | 168.9±9.1 | 0.21 |
| BMI | 30.4±5.2 | 30.1±4.7 | 0.64 |
| Weight status‡ | |||
| Overweight | 40 (36) | 44 (39) | 0.78 |
| Obese | 70 (64) | 70 (61) | |
| Body fat — % of total weight | 31.9±8.3 | 31.2±8.2 | 0.55 |
| Annual household income — no. (%) | |||
| <$30,000 | 30 (27) | 31 (27) | 0.71 |
| $30,000–$59,999 | 38 (35) | 34 (30) | |
| ≥$60,000 | 42 (38) | 49 (43) | |
| Parental educational level — no. (%)§ | |||
| Some high school | 2 (2) | 5 (4) | 0.56 |
| High-school diploma or GED certificate | 23 (21) | 20 (18) | |
| Some college or vocational school | 28 (25) | 24 (21) | |
| Associate’s degree | 7 (6) | 14 (12) | |
| Bachelor’s degree | 33 (30) | 33 (29) | |
| Some graduate school or graduate degree | 17 (15) | 18 (16) | |
| Daily physical activity level — MET | 1.53±0.18 | 1.54±0.18 | 0.85 |
| Television viewing — hr/day | 3.0±1.8 | 2.8±1.4 | 0.46 |
Plus–minus values are means ±SD. Means were compared with the use of the Student’s t-test and proportions compared with the use of Fisher’s exact test. Percentages may not sum to 100 owing to rounding. GED denotes General Educational Development, and MET metabolic equivalent.
Race and ethnic group were reported by the parents of the participants. “Multiple” included white–black (8 participants), white–Asian (3), white–black–Asian (1), and white–Arabic (1). “Other” included Latino or Latina (8 participants), Hispanic (7), Brazilian (2), Cape Verdean (2), Puerto Rican (4), Latino or Latina–Brazilian (1), Spanish (1), and American (1). Comparisons of baseline characteristics according to ethnic group are provided in Table S1 in the Supplementary Appendix.
Participants at or above the 85th percentile for BMI but below the 95th percentile were classified as overweight, and participants at or above the 95th percentile were classified as obese. The BMI range was 23.2 to 28.8 for overweight participants and 26.7 to 50.7 for obese participants.
The educational level listed is for the father or mother, depending on which parent had the higher level of education.
Table 2.
Dietary Intake.*
| Intake | Unadjusted Data | Change from Baseline | |||||
|---|---|---|---|---|---|---|---|
| Baseline | 1 Yr | 2 Yr | 1 Yr | P Value† | 2 Yr | P Value‡ | |
| Beverages (servings/day) | |||||||
|
| |||||||
| Sugar-sweetened | |||||||
|
| |||||||
| Experimental group | 1.7±0.9 | 0.2±0.4 | 0.4±0.5 | −1.5±0.1 | <0.001 | −1.3±0.1 | <0.001 |
|
| |||||||
| Control group | 1.7±1.1 | 0.9±1.1 | 0.8±0.8 | −0.8±0.1 | <0.001 | −0.9±0.1 | <0.001 |
|
| |||||||
| Difference | −0.7±0.1 | <0.001 | −0.4±0.1 | 0.005 | |||
|
| |||||||
| Fruit juices | |||||||
|
| |||||||
| Experimental group | 0.4±0.5 | 0.1±0.2 | 0.2±0.3 | −0.3±0.0 | <0.001 | −0.2±0.1 | 0.002 |
|
| |||||||
| Control group | 0.3±0.4 | 0.2±0.3 | 0.2±0.3 | −0.1±0.0 | 0.02 | −0.1±0.1 | 0.03 |
|
| |||||||
| Difference | −0.2±0.1 | 0.01 | −0.1±0.1 | 0.48 | |||
|
| |||||||
| Artificially sweetened | |||||||
|
| |||||||
| Experimental group | 0.1±0.3 | 0.9±1.0 | 0.4±0.8 | 0.8±0.1 | <0.001 | 0.3±0.1 | <0.001 |
|
| |||||||
| Control group | 0.1±0.2 | 0.3±0.5 | 0.3±0.6 | 0.2±0.1 | 0.01 | 0.2±0.1 | <0.001 |
|
| |||||||
| Difference | 0.6±0.1 | <0.001 | 0.1±0.1 | 0.32 | |||
|
| |||||||
| Unsweetened | |||||||
|
| |||||||
| Experimental group | 0.9±1.0 | 1.9±1.5 | 1.8±1.4 | 1.0±0.1 | <0.001 | 0.9±0.1 | <0.001 |
|
| |||||||
| Control group | 1.1±1.0 | 1.2±1.1 | 1.4±1.2 | 0.2±0.1 | 0.18 | 0.2±0.1 | 0.04 |
|
| |||||||
| Difference | 0.8±0.2 | <0.001 | 0.6±0.2 | <0.001 | |||
|
| |||||||
| Energy intake (kcal/day) | |||||||
|
| |||||||
| Total | |||||||
|
| |||||||
| Experimental group | 1967±553 | 1513±509 | 1619±444 | −454±48 | <0.001 | −361±54 | <0.001 |
|
| |||||||
| Control group | 1901±510 | 1720±420 | 1726±467 | −176±48 | <0.001 | −178±54 | 0.001 |
|
| |||||||
| Difference | −278±69 | <0.001 | −183±76 | 0.02 | |||
|
| |||||||
| Sugar-sweetened beverages | |||||||
|
| |||||||
| Experimental group | 242±140 | 29±58 | 52±70 | −213±14 | <0.001 | −188±15 | <0.001 |
|
| |||||||
| Control group | 242±155 | 134±159 | 109±112 | −108±14 | <0.001 | −130±15 | <0.001 |
|
| |||||||
| Difference | −105±20 | <0.001 | −58±21 | 0.007 | |||
|
| |||||||
| Fruit juices | |||||||
|
| |||||||
| Experimental group | 94±112 | 30±44 | 59±84 | −63±11 | <0.001 | −37±12 | 0.003 |
|
| |||||||
| Control group | 82±92 | 65±86 | 58±76 | −18±11 | 0.12 | −23±12 | 0.05 |
|
| |||||||
| Difference | −45±16 | 0.005 | −13±17 | 0.44 | |||
|
| |||||||
| Sugar (g/day) | |||||||
|
| |||||||
| Experimental group | 133±42 | 57±34 | 71±32 | −76±4 | <0.001 | −63±5 | <0.001 |
|
| |||||||
| Control group | 132±48 | 96±49 | 89±36 | −37±4 | <0.001 | −44±5 | <0.001 |
|
| |||||||
| Difference | −39±6 | <0.001 | −19±7 | 0.005 | |||
Plus–minus values for unadjusted data are means ±SD, and plus–minus values for changes from baseline are means ±SE. Changes were calculated at 1 year and 2 years from the general linear model, without adjustment for covariates.
The P values for changes from baseline in each study group are based on tests of the hypothesis that the mean change was zero.
The P values for the between-group differences in changes from baseline are based on tests of the hypothesis that the mean change was the same in the two groups. There were no significant ethnic group–study group interactions for any of the dietary variables.
Table 3.
Study Outcomes.*
| Variable | Unadjusted Data | Change from Baseline | |||||
|---|---|---|---|---|---|---|---|
| Baseline | 1 Yr | 2 Yr | 1 Yr | P Value† | 2 Yr | P Value‡ | |
| BMI | |||||||
|
| |||||||
| All participants | |||||||
|
| |||||||
| Experimental group | 30.36±5.24 | 30.50±5.55 | 31.10±5.94 | 0.06±0.20 | 0.75 | 0.71±0.28 | 0.01 |
|
| |||||||
| Control group | 30.05±4.66 | 30.61±5.37 | 31.03±5.51 | 0.63±0.20 | 0.001 | 1.00±0.28 | <0.001 |
|
| |||||||
| Difference | −0.57±0.28 | 0.045 | −0.30±0.40 | 0.46 | |||
|
| |||||||
| Non-Hispanic participants | |||||||
|
| |||||||
| Experimental group | 30.14±5.20 | 30.41±5.49 | 31.16±5.81 | 0.19±0.23 | 0.41 | 0.95±0.33 | 0.005 |
|
| |||||||
| Control group | 29.96±4.63 | 30.41±5.25 | 30.78±5.38 | 0.48±0.22 | 0.03 | 0.77±0.30 | 0.01 |
|
| |||||||
| Difference | −0.29±0.31 | 0.36 | 0.18±0.44 | 0.68 | |||
|
| |||||||
| Hispanic participants | |||||||
|
| |||||||
| Experimental group | 31.06±5.39 | 30.79±5.82 | 30.90±6.41 | −0.36±0.45 | 0.42 | −0.08±0.64 | 0.89 |
|
| |||||||
| Control group | 30.52±4.90 | 31.60±6.01 | 32.29±6.14 | 1.43±0.52 | 0.006 | 2.27±0.73 | 0.002 |
|
| |||||||
| Difference | −1.79±0.65 | 0.007 | −2.35±0.92 | 0.01 | |||
|
| |||||||
| Weight (kg) | |||||||
|
| |||||||
| All participants | |||||||
|
| |||||||
| Experimental group | 85.2±16.8 | 87.0±18.0 | 90.1±19.4 | 1.6±0.6 | 0.01 | 4.3±1.0 | <0.001 |
|
| |||||||
| Control group | 86.1±17.0 | 90.2±19.8 | 92.3±20.7 | 3.5±0.6 | <0.001 | 5.1±1.0 | <0.001 |
|
| |||||||
| Difference | −1.9±0.9 | 0.04 | −0.8±1.4 | 0.55 | |||
|
| |||||||
| Non-Hispanic participants | |||||||
|
| |||||||
| Experimental group | 86.1±17.4 | 88.5±18.6 | 92.5±20.0 | 2.2±0.7 | 0.003 | 5.5±1.1 | <0.001 |
|
| |||||||
| Control group | 85.8±16.9 | 89.3±19.1 | 91.3±19.9 | 3.0±0.7 | <0.001 | 4.4±1.0 | <0.001 |
|
| |||||||
| Difference | −0.8±1.0 | 0.42 | 1.1±1.5 | 0.48 | |||
|
| |||||||
| Hispanic participants | |||||||
|
| |||||||
| Experimental group | 82.7±15.1 | 82.6±15.6 | 83.2±16.2 | −0.5±1.4 | 0.74 | 0.3±2.1 | 0.88 |
|
| |||||||
| Control group | 87.8±18.2 | 95.4±23.4 | 98.2±24.6 | 6.0±1.7 | <0.001 | 9.2±2.5 | <0.001 |
|
| |||||||
| Difference | −6.4±2.1 | 0.003 | −8.8±3.1 | 0.005 | |||
|
| |||||||
| Height (cm) | |||||||
|
| |||||||
| All participants | |||||||
|
| |||||||
| Experimental group | 167.4±8.8 | 168.8±9.2 | 169.7±9.4 | 1.4±0.2 | <0.001 | 2.3±0.2 | <0.001 |
|
| |||||||
| Control group | 168.9±9.1 | 170.7±9.8 | 171.5±10.0 | 1.6±0.2 | <0.001 | 2.1±0.3 | <0.001 |
|
| |||||||
| Difference | −0.2±0.2 | 0.49 | 0.2±0.4 | 0.67 | |||
|
| |||||||
| Non-Hispanic participants | |||||||
|
| |||||||
| Experimental group | 168.8±8.4 | 170.3±8.6 | 171.5±8.7 | 1.6±0.2 | <0.001 | 2.6±0.3 | <0.001 |
|
| |||||||
| Control group | 168.8±9.0 | 170.5±9.6 | 171.3±9.8 | 1.7±0.2 | <0.001 | 2.2±0.3 | <0.001 |
|
| |||||||
| Difference | −0.1±0.3 | 0.80 | 0.4±0.4 | 0.29 | |||
|
| |||||||
| Hispanic participants | |||||||
|
| |||||||
| Experimental group | 163.2±8.6 | 164.0±9.3 | 164.4±9.8 | 0.8±0.4 | 0.05 | 1.1±0.6 | 0.05 |
|
| |||||||
| Control group | 169.4±10.0 | 171.7±11.1 | 172.4±11.6 | 1.4±0.5 | 0.004 | 2.1±0.7 | 0.002 |
|
| |||||||
| Difference | −0.6±0.6 | 0.30 | −1.0±0.8 | 0.24 | |||
Plus–minus values for unadjusted data are means ±SD, and plus–minus values for changes from baseline are means ±SE. Changes were calculated at 1 year and 2 years from the general linear model, and were adjusted for sex, race, ethnic group, household income, parental education, baseline BMI, baseline beverage consumption (energy from sugar-sweetened beverages and fruit juices and servings of artificially sweetened beverages and unsweetened beverages), baseline total energy intake, baseline sugar intake, and baseline obesity-related behavioral measures (physical activity and hours of television viewing). Results specific to ethnic group are from a model that included an interaction term for study group and ethnic group. For the change during the 2 years, before imputation, BMI data were available for 166 non-Hispanic participants (78 in the experimental group and 88 in the control group) and 43 Hispanic participants (27 in the experimental group and 16 in the control group).
The P values for changes from baseline in each study group are based on tests of the hypothesis that the mean change was zero.
The P values for the between-group differences in changes from baseline are based on tests of the hypothesis that the mean change was the same in the two groups.
Figure 1. Screening, Randomization, and Follow-up of the Study Participants.
Among the 538 adolescents who were excluded, 15 of the 49 who did not meet the sugar-sweetened–beverage (SSB) criterion also had other reasons and are included in the counts for those reasons. The weight and height of all available participants were measured at each time point in order to calculate BMI.
CHANGES IN DIETARY INTAKE
Changes in reported dietary intake are shown in Table 2. At 1 year, the change in consumption of sugar-sweetened beverages was significantly different between the groups (P<0.001), declining almost to 0 in the experimental group. Concomitantly, consumption of artificially sweetened and unsweetened beverages increased significantly in the experimental group as compared with the control group (P<0.001). At 2 years, the consumption of sugar-sweetened beverages remained lower and the consumption of unsweetened beverages remained higher in the experimental group (P = 0.005 and P<0.001, respectively), whereas the consumption of artificially sweetened beverages did not differ significantly between the groups (P = 0.32). Total energy intake and sugar intake decreased in the experimental group as compared with the control group at 1 year (P<0.001 for both comparisons), with group differences persisting at 2 years (P = 0.02 for total energy intake and P = 0.005 for sugar intake).
OUTCOMES
Study outcomes are presented in Table 3 and in the Supplementary Appendix (available at NEJM.org). The prespecified primary outcome, the net intervention effect on BMI at 2 years (the change in the experimental group minus the change in the control group), was not significant (−0.30, P = 0.46). However, the effect on BMI at the end of the 1-year intervention was significant (−0.57, P = 0.045). When sugar intake was added to the model, the intervention effect on BMI was strongly attenuated and no longer significant (−0.39, P = 0.24). The change in the mean (±SE) percentage of body fat in the experimental group as compared with the change in the control group was not significant (−0.5%±0.6, P = 0.40). Although there was no significant intervention effect for the change in overall reported physical activity (0.01±0.04 METs, P = 0.86), the experimental group had significant decreases in reported time spent watching television at 1 year (−0.6±0.2 hours per day, P = 0.002) and at 2 years (−0.7±0.2 hours per day, P = 0.001), whereas the control group had no significant change. The difference between the two groups (change in experimental group minus change in control group) was significant at 1 year (−0.7±0.3 hours per day, P = 0.01) and at 2 years (−0.6±0.3 hours per day, P = 0.04). Neither the change in television viewing (P = 0.03 for intervention effect on change in BMI at 1 year with change in television viewing added to the model) nor the change in any covariate other than sugar intake mediated the intervention effect on the change in BMI at 1 year.
EFFECTS OF ETHNIC GROUP
In prespecified tests of covariates for interaction with group assignment, we found significant effect modification according to ethnic group for changes in BMI (P = 0.04 at 1 year and P = 0.01 at 2 years) and body weight (P = 0.02 at 1 year and P = 0.005 at 2 years). Among Hispanics, there were significant intervention effects on the change in BMI at 1 year (−1.79, P = 0.007) and at 2 years (−2.35, P = 0.01) and on the change in body weight at 1 year (−6.4 kg, P = 0.003) and at 2 years (−8.8 kg, P = 0.005) (Table 3). Other covariates were not significant effect modifiers.
Given these results, we reanalyzed data from a 19-month prospective observational study that showed an overall positive association between change in consumption of sugar-sweetened beverages and change in BMI (β = 0.24, P = 0.03).13 Here, too, we found effect modification according to ethnic group (P = 0.007). The association for the 84 Hispanic youths in the study was strong (β = 0.63, P = 0.007), whereas that for the 464 non-Hispanics (predominantly non-Hispanic whites but also non-Hispanic blacks, Asian Americans, American Indians, and others) was not significant (β = 0.164, P = 0.11).
ADVERSE EVENTS
A total of seven events were reported by the parents of participants in the experimental group during motivational telephone calls (diagnosis of Graves’ disease, diagnosis of polycystic ovary syndrome, an infected finger, an asthma attack, a mild head injury due to a car accident, the development of a blood clot after knee surgery, and temporary hearing loss due to the buildup of fluid and wax in the ears).
DISCUSSION
The provision of noncaloric beverages virtually eliminated reported consumption of sugar-sweetened beverages and reduced total reported energy intake among overweight and obese adolescents after a 1-year intervention, and there were persistent effects on diet through follow-up at 2 years. The change in BMI differed significantly between the experimental and control groups at 1 year but not at 2 years. We also found evidence of effect modification according to ethnic group, with the change in BMI differing between groups in a small sample of Hispanics but not among non-Hispanic participants.
Multicomponent interventions, targeting several aspects of diet and physical activity to promote negative energy balance, constitute a common strategy for treating adolescent obesity.19,20 However, most intensive interventions have yielded disappointing results. In the present study, education and behavioral counseling focused specifically on decreasing consumption of sugar-sweetened beverages, a single dietary behavior that may be particularly important for controlling body weight. The significant intervention effect for the change in BMI observed at 1 year, together with the findings of de Ruyter et al. involving children 5 to 12 years of age (reported elsewhere in the Journal),21 provides support for public health guidelines that recommend limiting consumption of sugar-sweetened beverages.22 The lack of effect at 2 years could reflect increasing energy intake from sugar-sweetened beverages or fruit juices in the experimental group on discontinuation of the intervention; decreasing intake of sugar-sweetened beverages or fruit juices in the control group, possibly due to a secular trend resulting from efforts to eliminate these beverages from schools23; or both.
We examined several variables that could confound or mediate the effect of the intervention on BMI. We observed a difference in television viewing between the groups, but in our statistical models, this difference did not account for the difference in the change in BMI at 1 year. Similarly, no covariate other than sugar intake attenuated the intervention effect, suggesting that sugar intake had a mediating influence. However, we recognize that the intensity of the intervention, rather than provision of non-caloric beverages per se, may have led to salutary changes in other behaviors, such as decreased television viewing, and that these changes may affect body weight.
We conducted a subgroup analysis after a prespecified test revealed significant effect modification according to ethnic group, and reanalysis of data from a prospective observational study13 provided corroborative evidence. However, these data must be interpreted cautiously in view of the small size of the Hispanic subgroup. The reason for effect modification according to ethnic group remains speculative but may involve differences in physiology (e.g., involving insulin secretion in response to the ingestion of sugar24–26) or in genetic susceptibility (as reported elsewhere in the Journal27). Still, even though our statistical models controlled for baseline covariates and no effect modification was detected in our measures of household income and education, we cannot exclude the possibility that effect modification according to ethnic group arose from socioeconomic or behavioral differences between ethnic groups rather than from inherent physiological differences. Additional study is needed to determine whether ethnic group influences the effect of consuming sugar-sweetened beverages on body weight.
The strengths of our trial include a focus on a single dietary behavior in the home environment, a diverse sample, excellent participant-retention rates, collection of data on dietary process measures, and assessment of physical activity and television viewing. The limitations include a small sample as compared with samples in multisite studies, reliance on self-reporting of dietary intake (with the likelihood of underreporting)28 and physical activity, use of the BIA (a relatively inaccurate method)29 to estimate body fat, and lack of data on obesity-related risk factors, such as biomarkers of lipid and glucose metabolism.
In conclusion, replacement of sugar-sweetened beverages with noncaloric beverages did not improve body weight over a 2-year period, but group differences in dietary quality and body weight were observed at the end of the 1-year intervention period.
Supplementary Material
Acknowledgments
Supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK073025 and K24DK082730, to Dr. Ludwig) and from the National Center for Research Resources to the Boston Children’s Hospital General Clinical Research Center (M01RR02172), the Harvard Catalyst Clinical and Translational Science Center (UL1RR025758), and the New Balance Foundation. The observational study was supported by grants from the National Institute of Child Health and Human Development (HD30780), the Centers for Disease Control and Prevention (1U48DP001946), and the Robert Wood Johnson Foundation (66284).
We thank Margaret Apura for organizing daily study operations and overseeing the motivational telephone calls and check-in visits; Linda Seger-Shippee for conducting the 24-hour dietary and physical-activity recall interviews; Meredith Beard for administrative contributions; Hope Forbes, Sarah Kalil, Melissa Gallagher, Catherine Matero, Elizabeth Scarola, Abigail Lukens, Katherine Wargo, and Gayathry Sooriyakumar for assistance with data collection and management; Corrine Fischer for assistance with motivational telephone calls; administrators, nurses, and teachers at the participating schools for assistance with recruitment and retention; Drs. Isabelle Chase and Zameera Fida for facilitating recruitment in the dental clinic; Mohamad Daniar for maintaining the data-management system; and Drs. Joseph Majzoub and Walter Willett for their thoughtful review of a previous draft of this article.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Research Resources, the National Institute of Child Health and Human Development, the National Institutes of Health, or the Centers for Disease Control and Prevention.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Bremer AA, Byrd RS, Auinger P. Racial trends in sugar-sweetened beverage consumption among US adolescents: 1988–2004. Int J Adolesc Med Health. 2011;23:279–86. doi: 10.1515/ijamh.2011.056. [DOI] [PubMed] [Google Scholar]
- 2.Lee JM, Pilli S, Gebremariam A, et al. Getting heavier, younger: trajectories of obesity over the life course. Int J Obes (Lond) 2010;34:614–23. doi: 10.1038/ijo.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beverage consumption among high school students — United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:778–80. [PubMed] [Google Scholar]
- 4.Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. J Am Diet Assoc. 2010;110:1477–84. doi: 10.1016/j.jada.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 6.Tordoff MG, Alleva AM. Effect of drinking soda sweetened with aspartame or high-fructose corn syrup on food intake and body weight. Am J Clin Nutr. 1990;51:963–9. doi: 10.1093/ajcn/51.6.963. [DOI] [PubMed] [Google Scholar]
- 7.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–64. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ. 2004;328:1237. doi: 10.1136/bmj.38077.458438.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12:197–202. doi: 10.1017/S1368980008002644. [DOI] [PubMed] [Google Scholar]
- 10.Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics. 2006;117:673–80. doi: 10.1542/peds.2005-0983. [DOI] [PubMed] [Google Scholar]
- 11.Johnson RK, Appel LJ, Brands M, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120:1011–20. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 12.Allison DB, Mattes RD. Nutritively sweetened beverage consumption and obesity: the need for solid evidence on a fluid issue. JAMA. 2009;301:318–20. doi: 10.1001/jama.2008.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–8. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 15.Sun SS, Chumlea WC, Heymsfield SB, et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr. 2003;77:331–40. doi: 10.1093/ajcn/77.2.331. [DOI] [PubMed] [Google Scholar]
- 16.Bouchard C, Tremblay A, Leblanc C, Lortie G, Savard R, Thériault G. A method to assess energy expenditure in children and adults. Am J Clin Nutr. 1983;37:461–7. doi: 10.1093/ajcn/37.3.461. [DOI] [PubMed] [Google Scholar]
- 17.Weston AT, Petosa R, Pate RR. Validation of an instrument for measurement of physical activity in youth. Med Sci Sports Exerc. 1997;29:138–43. doi: 10.1097/00005768-199701000-00020. [DOI] [PubMed] [Google Scholar]
- 18.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 19.McGovern L, Johnson JN, Paulo R, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93:4600–5. doi: 10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- 20.Kamath CC, Vickers KS, Ehrlich A, et al. Clinical review: behavioral interventions to prevent childhood obesity: a systematic review and metaanalyses of randomized trials. J Clin Endocrinol Metab. 2008;93:4606–15. doi: 10.1210/jc.2006-2411. [DOI] [PubMed] [Google Scholar]
- 21.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367:1397–406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 22.Department of Agriculture, Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7. Washington, DC: Government Printing Office; Dec, 2010. [Google Scholar]
- 23.Cradock AL, McHugh A, Mont-Ferguson H, et al. Effect of school district policy change on consumption of sugar-sweetened beverages among high school students, Boston, Massachusetts, 2004–2006. Prev Chronic Dis. 2011;8:A74. [PMC free article] [PubMed] [Google Scholar]
- 24.Goran MI, Bergman RN, Cruz ML, Watanabe R. Insulin resistance and associated compensatory responses in African-American and Hispanic children. Diabetes Care. 2002;25:2184–90. doi: 10.2337/diacare.25.12.2184. [DOI] [PubMed] [Google Scholar]
- 25.Haffner SM, D’Agostino R, Saad MF, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites: the Insulin Resistance Atherosclerosis Study. Diabetes. 1996;45:742–8. doi: 10.2337/diab.45.6.742. [DOI] [PubMed] [Google Scholar]
- 26.Haffner SM, Miettinen H, Stern MP. Nondiabetic Mexican-Americans do not have reduced insulin responses relative to nondiabetic non-Hispanic whites. Diabetes Care. 1996;19:67–9. doi: 10.2337/diacare.19.1.67. [DOI] [PubMed] [Google Scholar]
- 27.Qi Q, Chu AY, Kang JH, et al. Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med. 2012;367:1387–96. doi: 10.1056/NEJMoa1203039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh R, Martin BR, Hickey Y, et al. Comparison of self-reported, measured, metabolizable energy intake with total energy expenditure in overweight teens. Am J Clin Nutr. 2009;89:1744–50. doi: 10.3945/ajcn.2008.26752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee SY, Gallagher D. Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care. 2008;11:566–72. doi: 10.1097/MCO.0b013e32830b5f23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.