Abstract
A cluster randomized controlled trial was initiated in Kenya to determine if full integration (FI) of HIV care, including HAART, into antenatal care (ANC) clinics improves health outcomes among HIV-infected women and exposed infants, compared to a non-integrated (NI) model. This paper examines ANC clients’ satisfaction with and preferences regarding HIV-integrated services. In this cross-sectional study, pregnant women attending five FI clinics (n=185) and four NI clinics (n=141) completed an interviewer-administered questionnaire following an ANC visit. By self-report, 55 women (17%) were HIV(+), 230 (71%) were HIV(−) and 40 (12%) did not know their HIV status. Among HIV-infected women, 79% attending FI clinics were very satisfied with their clinic visit compared to 54% of women attending NI clinics (P=0.044); no such difference was found among HIV-uninfected women. In multivariate analysis, overall satisfaction was also independently associated with satisfaction with administrative staff, satisfaction with health care providers, positive evaluation of wait time, and having encountered a receptionist. Full integration of HIV care into antenatal clinics can significantly increase overall satisfaction with care for HIV-infected women, with no significant decrease in satisfaction for HIV-uninfected women served in the same clinics.
Keywords: patient satisfaction, HIV, antenatal care, service integration, Kenya
Introduction
Antenatal clinics in Kenya have reported high HIV prevalence rates, up to 31% in some parts of the country (NASCOP, 2005; WHO, UNAIDS, & UNICEF, 2009; Gray et al., 2005) with 70% of infected adults living in rural areas (NASCOP 2008). However, it is estimated that only 56% of HIV-infected pregnant women in Kenya access basic services for the prevention of mother-to-child transmission (PMTCT) (WHO, UNAIDS, and UNICEF, 2009).
Prior studies indicate that integrating HIV and antenatal care (ANC) services may have positive effects on uptake of HIV services (Van Der Merwe, et al., 2006; Welty et al., 2005; Killam et al., 2010). However, studies have not assessed patients’ perspectives, despite the importance of patient satisfaction for program success. Low patient satisfaction has been shown to be associated with poorer HAART treatment outcomes (Gellaitry et al., 2005; Barfod et al., 2005) and lower treatment adherence (Heckman et al., 2004). To date no patient satisfaction studies have been reported in the context of programs offering of integrated HIV and ANC services in sub-Saharan Africa.
Family AIDS Care and Education Services (FACES) is a PEPFAR-funded program run through a collaboration of the Kenya Medical Research Institute (KEMRI) and the University of California, San Francisco (UCSF). Investigators from KEMRI and UCSF initiated a cluster randomized controlled trial; the Study of HIV and Antenatal care Integration in Pregnancy (SHAIP), in two rural districts of Nyanza Province, Kenya. The study is assessing the effects of full integration of HIV care and Antenatal Care (ANC) on service uptake, adherence to treatment, and health outcomes of HIV-infected pregnant women and their infants. For SHAIP, all of the government health facilities in the two districts that were providing HAART by June 2009 (12 facilities) were randomized to provide either fully integrated (FI) HIV and ANC services (intervention arm) or non-integrated (NI) services (control arm). This Cluster RCT gave us the opportunity to evaluate patient satisfaction at five FI and four NI clinics.
Methods
This was a cross-sectional observational sub-study nested in a cluster randomized trial. At the time this study was conducted in February-April 2009, 9 out of 12 study sites had been randomized, trained, and were providing services in their randomized service delivery model. In fully integrated (FI) clinics, ANC, PMTCT, HIV care and treatment (including HAART) are provided in the same visit. In the control (NI) clinics ANC and basic PMTCT services (single dose nevirapine and short course AZT) were provided in one visit, with referral to a separate clinic in the same health facility for HIV care and treatment (including HAART if indicated, opportunistic infection prophylaxis, education, and adherence counseling). Providers from both FI and NI arms received the same five-day training package on clinical HIV/AIDS care, PMTCT, and high quality ANC care; and equivalent instructions on roles, responsibilities, and expectations, as well as study and clinic flow logistics for FI or NI services.
For the current study, eligible participants were pregnant women, at least 18 years of age, who had completed at least one ANC visit at one of these clinics. Independent interviewers verbally administered a one-time questionnaire to clients after an ANC visit in the participant’s preferred language (English, Kiswahili, or Dholuo). This study’s questionnaire items were adapted from the AIDS Clinical Trial Group Health and Options Questionnaire, and similar adaptations have been previously validated and implemented by the FACES program to improve quality of care at the sites. The questionnaire also included additional items based on review of prior patient satisfaction studies in the literature (Weston et al., 2009). Demographic characteristics, wait time measures, perceptions of care received, self-reported HIV status, and personal preferences for integration or non-integration of services were collected.
The question “How satisfied were you with the services you received today from each of the following departments” was used to assess pregnant women’s level of satisfaction with the receptionist, the clinic and community health assistant (CCHA), the nurse or doctor, and her overall clinic experience, with possible answers ranging from “very satisfied (VS)” (4), “satisfied (S)” (3), “unsatisfied (US)” (2), and “very unsatisfied (VUS)” (1). CCHAs are lay health workers within the FACES program who assist the nurses and doctors in taking care of patients as well as assisting in FACES program research through recruitment and data gathering (Agengo et al., 2009).
We also assessed satisfaction with different aspects of care including enough time spent, respect , careful listening, courtesy, being helpful, and privacy and confidentiality, with possible responses being “all of the time” (4), “most of the time” (3), “some of the time” (2), and “none of the time” (1). Time spent waiting for the clinic visit was rated as “just right” (3), “a bit long” (2), or “much too long” (1). In addition, composite variables were created to capture satisfaction with administrative staff (receptionist and/or CCHA) and satisfaction with health professionals (nurses and/or doctors).
Participants were also asked directly: “If you could choose, would you rather receive your HIV and antenatal care (a) in one setting, for example in the antenatal department, or (b) in separate departments, for example HIV care at Patient Support Center (PSC) and antenatal care at the antenatal department.” PSCs are specialized HIV clinics within Kenyan government health facilities providing counseling and support with HIV diagnosis and treatment.
Statistical analyses were conducted using the chi-square test, the weighted t-test, and linear and logistic regression using STATA (Statacorp, College Station, Texas) version 10.0 (Statacorp, 2005). A multilevel random effects logistic regression model, including statistically significant predictors from bivariate analyses (p<.05) and theoretically important variables, was used in the analyses of the predictors of overall satisfaction, in order to account for clustering by site (Vittinghoff, 2005).
Stratified analyses were conducted by HIV status [dichotomized into HIV-infected vs. others (including HIV-uninfected women and those with unknown HIV status)] and by integration status of the clinic (FI vs. NI). Satisfaction variables were dichotomized as “very satisfied” vs. “less than very satisfied,” for questions regarding overall satisfaction with staff, “all of the time” vs. “not all of the time“ for questions on staff attitudes and behaviors, and “just right” vs. “less than just right” for wait time questions.
Results
We recruited 334 women; none refused, while 8 women were later withdrawn from the study by investigators for not meeting eligibility criteria. Thus 326 women were included in the analyses: 185 from five FI sites and 141 from four NI sites. Background characteristics of the participants were comparable between the FI and NI sites with regards to age, marital status, gestational age, gravida, familiarity with clinic, and HIV status (Table 1). The average number of clients per day during the February to mid April 2009 study period ranged from 4-28 at the 5 FI sites and from 7-19 at the 4 NI sites. By self-report, 55 (17%) women were HIV-positive; 230 (71%) HIV-negative; and 40 (12%) had unknown HIV serostatus.
Table 1.
Characteristics of Pregnant Women attending ANC clinics in Migori & Rongo Districts, Kenya
| Participant characteristics | overall n=326 |
Integrated group (intervention), n= 185 |
Nonintegrated group (control), n = 141 |
p |
|---|---|---|---|---|
| Age, mean yrs (±SD) | 24.3 (±5.4) | 23.9 (±5.3) | 24.9 (±5.5) | 0.13§ |
| Married, n(%) | 302 (92.6) | 169 (91.4) | 133 (94.3) | 0.308 |
| Gestation, mean months (SD) | 6.7 (1.7) | 6.6 (1.7) | 6.7 (1.6) | 0.59§ |
| First ANC for this pregnancy, n(%) | 136 (41.7) | 78 (42.2) | 58 (41.1) | 0.85 |
| Positive Self-rated health (score ≥ 3/5)¥ | 187 (57.4) | 114 (61.0) | 73 (39.0) | 0.075 |
| Previously pregnant, n(%) | 268 (82.2) | 148 (80.0) | 120 (85.1) | 0.23 |
| gravida, mean(SD) | 3.52 (2.0) | 3.47 (2.0) | 3.57 (2.0) | 0.64§ |
| received ANC in prior pregnancy, n(%) | 251 (93.3) | 138 (92.0) | 113 (95.0) | 0.34 |
| self-reported HIV (+), n(%) | 55 (16.9) | 29 (15.7) | 26 (18.6) | 0.44 |
| HIV (−) | 230 (70.8) | 136 (73.5) | 94 (67.1) | |
| HIV status unknown | 40 (12.3) | 20 (10.8) | 20 (14.3) |
p from chi2 test unless § t-test. ¥ excellent(5), very good(4), good(3), or fair (2), poor (1)
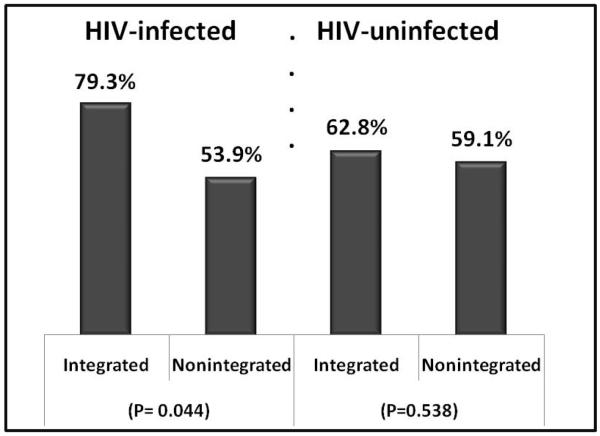
Overall satisfaction with the clinic visit was high: 96% of women who attended FI ANC clinics and 97% who attended NI ANC clinics were either “satisfied” or “very satisfied” with their clinic visit. When stratified by HIV status, 79% of HIV-infected women attending FI clinics were “very satisfied” with their clinic visit compared to only 54% of such women attending NI clinics (P=0.044). This difference was not significant for HIV-uninfected women attending FI (63%) and NI (59%) clinics (p=0.500) (Figure 1).
Figure 1.
Percent “Very Satisfied” with Overall Clinic Visit, Stratified by HIV Status, Compared between Integrated and Non-integrated Study Arms
Women at FI clinics reported an average wait time of 92.6 minutes [95%CI 79-106] vs. 63.3 minutes [95%CI 52-74] at the NI clinics, an average difference of 29.3 minutes (p=0.002). Even after controlling for average daily patient volume at each site in a linear regression analysis, women at FI sites still waited an average of 26.6 minutes longer than those at NI sites (p=0.009). However, actual wait time was not associated with the women’s overall clinic visit satisfaction score (p=0.388). Instead, the women’s evaluation of her wait time was associated with overall clinic satisfaction: 68% of women who thought their wait time were “just right” were very satisfied with their overall clinic visit vs. 56% who felt their wait time was “a bit too long” and 50% of those who felt it was “much too long” (p=0.031).
When asked for their preference, 82% of HIV-infected women preferred integration vs. 68% of HIV-uninfected women (p=0.038). Unadjusted random effects logistic regression analyses (bivariate associations accounting for clustering by site) revealed that encountering a receptionist (OR = 2.26, 95%CI 1.40-3.64), being satisfied with waiting time (OR = 1.82, 95%CI 1.15-2.88), as well as being very satisfied with the doctor/nurse or administrative staff or with any of the six aspects of care (i. time spent, ii. respect, iii. listening, iv. courtesy and respect, v. helpfulness, and vi. privacy & confidentiality) were also significantly associated with being “very satisfied” with the clinic visit.
Multivariate analysis, using random effects logistic regression to account for clustering by site, was performed to examine the relative importance of different aspects of care in understanding women’s overall satisfaction. We found significant independent associations with overall satisfaction while including the following variables in the model: being “very satisfied” with the health professionals (OR = 4.09, 95% CI 2.06-8.11), being “very satisfied” with the administrative staff (OR = 3.34, 95% CI 1.49-7.47), having encountered a receptionist (OR = 2.10, 95% CI 1.02-4.33), feeling that wait time was “just right” (OR = 2.3, 95% CI 1.22-4.09), a preference for integrated services (OR = 2.03, 95% CI 1.07-3.85), and attending an integrated clinic (OR = 10.34, 95% CI 2.08-51.3) (Table 2).
Table 2.
Logistic Regression of Satisfaction Measures and Other Significant Predictor Variables on Overall Satisfaction (n=276)®
| n/total | Unadjusted (univariate) |
n/276 | Adjusted (multivariate) | |||
|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | OR | 95% CI | ||
| Very satisfied with docs and/or nurses | 172/319 | 8.12*** | 4.80-13.76 | 150 | 4.09*** | 2.06-8.11 |
| Very satisfied with administrative staff | 104/284 | 6.60*** | 3.49-12.48 | 103 | 3.34** | 1.49-7.47 |
| Encountered a receptionist | 222/326 | 2.26*** | 1.40-3.64 | 215 | 2.10* | 1.02-4.33 |
| Felt that waiting time was just right | 197/325 | 1.82* | 1.15-2.88 | 164 | 2.23* | 1.22-4.09 |
| Prefers integration | 228/326 | 2.57*** | 1.55-4.25 | 192 | 2.03* | 1.07-3.85 |
| HIV-positive | 55/325 | 1.32 | 0.71-2.44 | 45 | 0.31 | 0.09 -1.04 |
| Integrated (FI) clinic (intervention arm) | 185/326 | 1.36 | 0.87-2.14 | 154 | 10.34** | 2.08-51.3 |
| Interaction: integration & HIV status | --- | 8.78* | 1.56-47.8 | |||
p<0.05
p≤0.005
p≤0.001
All estimates account for clustering by site (health facility) using Random Effects Logistic Regression. Multivariate analysis has a total n value of 276 because it excludes any entry that has a missing value for any of the listed variables. There are only 284 responses for “satisfaction with administrative staff (CCHA and receptionist)” and only 319 entries for “satisfaction with doctor and/or nurse.”
As expected from the bivariate results, there was a significant interaction between study arm (FI vs. NI) and HIV status (HIV-infected vs. others) in the multivariate model, reflecting the fact that integration made a significant positive difference in satisfaction for HIV-infected women, but not for HIV-uninfected women (Table 2).
Discussion
Recent efforts have suggested that there are significant benefits of integration of HIV care into antenatal care services (Van Der Merwe et al., 2006; Welty et al., 2005; Killam et al., 2010) or into existing primary health care systems (Pfeiffer et al., 2010), through markers such as shorter time to ART initiation, higher rate of treatment adherence, and decline in loss-to-follow-up rates.
This study adds patients’ perspectives to existing clinical data and providers’ perspectives on integration (Winestone 2010). Our findings suggest that integration of HIV care and antenatal care is highly desired by HIV-infected women, while also being acceptable to most HIV-uninfected women. In our population, integration improved HIV-infected women’s satisfaction with their overall clinic experience, while it appeared to have no detrimental effect on the HIV-uninfected women’s experience. This is possibly due to the ease of receiving care for both services in one single visit, removing the logistical difficulties of standing in line for services at two different clinics. It could also be due to decreased stigma associated with the FI service model, in which HIV-positive women appear to simply be receiving ANC care just like HIV-negative women.
In antenatal clinics caring for many HIV-infected women, improving HIV and antenatal care to this population is critical. To our knowledge, no previous studies have looked at how patient satisfaction is affected by integration of ANC and HIV services. Even with the high HIV prevalence in this rural Kenyan setting, the majority of ANC clients are HIV-uninfected and it is important to assess any potential advantages and disadvantages to this model of care from their perspectives as well. Although full integration appears to have increased average wait time for ANC services irrespective of HIV status and clinic volume, this was not associated with a decrease in women’s satisfaction with services.
It was interesting to find that 68% of HIV-uninfected women also stated a preference for the integrated service model. We hypothesize that this is due in part to women understanding and appreciating the integration benefit for others. It is also possible that such a high prevalence of HIV infection in the community(NASCOP, 2005; WHO, UNAIDS, & UNICEF, 2009; Gray et al., 2005; NASCOP, 2008) leads to a high perception of sero-conversion risk (Charles, 2009; Do, 2009), resulting in a fear by the HIV-uninfected women of one day sero-converting and requiring HIV services in the future. Of note, there was no difference in the cost to women for fully integrated vs. non integrated services.
The study had a number of limitations. It has been observed in several settings in Africa that people are often reluctant to voice negative opinions of the health services they receive (Nordberg & Holmberg, 1996; Fawole et al., 2008; Reshef & Reshef, 1997). In our study we found very high overall satisfaction rates and thus we dichotomized variables as “very satisfied” versus being “less than ‘very satisfied’”. Furthermore, as previously reported, people often report higher rates of overall satisfaction with care, while being more willing to point out dissatisfaction with specific aspects of services (Agha & Do, (2009). Another possible explanation for the relatively high satisfaction levels found in this study could be the fact that patients were interviewed immediately following the clinic visit—there is evidence that people report much higher satisfaction just after a health care visit than after a period of time has passed (Jensen, Ammentorp, & Kofoed, 2010). There is also a possibility that interviewing only clinic clients may decrease generalizability, by including only self-selected patients who already favor such clinics. However, the patients in these rural locations tend to attend the only facility within walking or bicycling distance from their homes. Furthermore, the SHAIP trial includes all of the qualifying health facilities in these districts, which improves generalizability.
HIV status was also based on self-report, making it subject to under-reporting, given the HIV/AIDS stigma still prevalent in Kenya (Yebei, Fortenberry, & Ayuku, 2008).25 Finally, inclusion of only nine sites from the larger Cluster RCT meant that there was a risk of imbalances in site characteristics that might have affected the study outcomes.
This study’s findings will be combined with other findings from SHAIP to evaluate the evidence for this experimental service delivery model in order to inform clinical care models in Kenya and other countries in sub-Saharan Africa. SHAIP is collecting data on the effects of integration on maternal uptake of HIV services, adherence to care, maternal immunoligic outcomes, vertical transmission, infant health outcomes, and health care provider perspectives. We expect that these results together will provide strong scientific evidence for decision-making regarding continuation of the traditional referral model for HIV care and treatment or for switching to the fully integrated care model.
ACKNOWLEDGEMENTS
We would like to thank the Kenyan women who participated in the study and shared their experiences with us. We acknowledge the support of Family AIDS Care and Education Services (FACES) and Research, Care and Training Program at Kenya Medical Research Institute (KEMRI). We thank the trilingual research assistants Salome Ogola Amuom and Samuel Otieno for their diligent work in collecting the data. We gratefully acknowledge the Director KEMRI and the Director of KEMRI’s Centre for Microbiology Research for their support in conducting this research. We also thank Janet Myers, PhD, MPH and David Glidden, PhD for study design and analysis advice. The project received IRB approval from both UCSF and KEMRI.
This publication was supported by NIH/NCRR/OD UCSF-CTSI Grant Number TL1 RR024129, UCSF Quarterly Research Fellowship, UCSF SBS/PTD Student Research Fund, and UCSF Pathway Project Fund. Janet Turan’s work on this study was supported by grant #5K01MH81777 from the U.S. National Institute of Mental Health (NIMH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or NIMH.
Footnotes
e) Meetings: Preliminary findings were presented at the 7th annual Global Health and Innovations Conference, Connecticut, USA on April 17-18, 2010.
REFERENCES
- Agengo G, Lewis-Kulzer J, Nyabiage L, et al. Maximizing Human Resources by Involving Lay Health Care Workers in HIV Service Delivery in Kenya. Poster session presented at the annual IAS Conf 2009; Cape Town, South Africa. [Retrieved online August 14, 2011]. 2009. http://www.faces-kenya.org/publications/LHCW%20IAS%2009.pdf. [Google Scholar]
- Agha S, Do M. [Retrieved online on August 18, 2011];The quality of family planning sercives and client satisfaction in the public and private sectors in Kenya. Int J Qual Health Care. 2009 21(2):87–96. doi: 10.1093/intqhc/mzp002. from http://intqhc.oxfordjournals.org/content/early/2009/02/03/intqhc.mzp002.full.pdf+html. [DOI] [PubMed] [Google Scholar]
- Barfod TS, Gerstoft J, Rodkjaer L, et al. Patients’ answers to simple questions about treatment satisfaction and adherence and depression are associated with failure of HAART: a cross-sectional survey. AIDS Patient Care STDS. 2005;19(5):317–325. doi: 10.1089/apc.2005.19.317. doi:10.1089/apc.2005.19.317. [DOI] [PubMed] [Google Scholar]
- Charles MP, Kweka EJ, Mahande AM. Evaluation of uptake and attitude to voluntary counseling and testing among health care professional students in Kilimanjaro region, Tanzania. BMC Public Health. 2009;9(9):128. doi: 10.1186/1471-2458-9-128. doi:10.1186/1471-2458-9-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do M, Meekers D. Multiple sex partners and perceived risk of HIV infection in Zambia: attitudinal determinants and gender differences. AIDS Care. 2009;21(10):1211–1221. doi: 10.1080/09540120902730047. doi:10.1080/09540120902730047. [DOI] [PubMed] [Google Scholar]
- Fawole A, Okunlola MA, Adekunle AO. Clients’ perceptions of the quality of antenatal care. J natl Med Assoc. 2008;100(9):1052–1058. doi: 10.1016/s0027-9684(15)31443-7. [DOI] [PubMed] [Google Scholar]
- Gellaitry G, Cooper V, Davis C, et al. Patients’ perception of information about HAART: impact on treatment decisions. AIDS Care. 2005;17(3):367–376. doi: 10.1080/09540120512331314367. doi:10.1080/09540120512331314367. [DOI] [PubMed] [Google Scholar]
- Gray RHRH, Li XX, Kigozi GG, et al. Increased risk of incident HIV during pregnancy in Rakai, Uganda: a prospective study. Lancet. 2005;366(9492):1182–1188. doi: 10.1016/S0140-6736(05)67481-8. doi:10.1016/S0140-6736(05)67481-8. [DOI] [PubMed] [Google Scholar]
- Heckman BD, Catz SL, Heckman TG, et al. Adherence to antiretroviral therapy in rural persons living with HIV disease in the United States. AIDS Care. 2004;16(2):219–230. doi: 10.1080/09540120410001641066. doi:10.1080/09540120410001641066. [DOI] [PubMed] [Google Scholar]
- Jensen HI, Ammentorp J, Kofoed PE. User satisfaction is influenced by the interval between a health care service and the assessment of the service. Soc Sci Med. 2010;70(12):1882–1887. doi: 10.1016/j.socscimed.2010.02.035. doi:10.1016/j.socscimed.2010.02.035. [DOI] [PubMed] [Google Scholar]
- Killam WP, Tambatamba BC, Chintu N, et al. Antiretrovial therapy in antenatal care to increase treatment initiation in HIV-infected pregnant women: a stepped-wedge evaluation. AIDS. 2010;24(1):85–91. doi: 10.1097/QAD.0b013e32833298be. doi:10.1097/QAD.0b013e32833298be. [DOI] [PubMed] [Google Scholar]
- National AIDS and STI Control Programme . Kenya AIDS Indicator Survey, KAIS 2007, Preliminary Report. Ministry of Health, Kenya; Nairobi, Kenya: [Retrieved online August 14, 2011]. 2008. from http://www.wofak.or.ke/Publications/kais__preliminary_report_july_29.pdf. [Google Scholar]
- National AIDS and STI Control Programme (NASCOP) Ministry of Health, Kenya . AIDS in Kenya. 7th ed. NASCOP; Nairobi: [Retrieved August 14, 2011]. 2005. from http://www.policyproject.com/pubs/countryreports/KEN_AIDS_7thEd.pdf. [Google Scholar]
- Nordberg E, Holmberg S. Patient attitudes to major surgery in rural Kenya. Int J Qual health Care. 1996;8(3):265–269. doi: 10.1093/intqhc/8.3.265. doi:10.1093/intqhc/8.3.265. [DOI] [PubMed] [Google Scholar]
- Pfeiffer J, Montoya P, Baptista AJ, et al. Integration of HIV/AIDS services into African primary health care: lessons learned for health system strengthening in Mozambique - a case study. J Int AIDS Soc. 2010;13(1):3. doi: 10.1186/1758-2652-13-3. doi:10.1186/1758-2652-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reshef DS, Reshef SH. Postoperative cataract surgery satisfaction in a rural Kenyan clinic. J Cataract Refract Surg. 1997;23(4):575–580. doi: 10.1016/s0886-3350(97)80217-9. [DOI] [PubMed] [Google Scholar]
- Statacorp . Stata Statistical Software: Release 10. 2005. Statacorp, LP; College Station, Texas: 2005. [Google Scholar]
- Van Der Merwe K, Chersich MF, Technau K, et al. Integration of antiretroviral treatment within antenatal care in Gauteng Province, South Africa. J Acquir Immune Defic Syndr. 2006;43(5):577–581. doi: 10.1097/01.qai.0000243099.72770.d2. doi:10.1097/01.qai.0000243099.72770.d2. [DOI] [PubMed] [Google Scholar]
- Vittinghoff E, Shiboski SC, Glidden DV, et al. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. Springer; New York: 2005. [Google Scholar]
- Welty TK, Bulterys M, Welty ER, et al. Integrating prevention of mother-to-child HIV transmission into routine antenatal care: the key to program expansion in Cameroon. J Acquir Immune Defic Syndr. 2005;40(4):486–493. doi: 10.1097/01.qai.0000163196.36199.89. doi:10.1097/01.qai.0000163196.36199.89. [DOI] [PubMed] [Google Scholar]
- Weston R, Dabis R, Ross JDC. Measuring patient satisfaction in sexually transmitted infection clinics: a systemic review. Sex Transm Infect. 2009;85(6):459–467. doi: 10.1136/sti.2009.037358. doi:10.1136/sti.2009.037358. [DOI] [PubMed] [Google Scholar]
- Winestone LE, Bukusi EA, Cohen CR, et al. Provider Perspectives on Integration of HIV Care and Treatment into Antenatal Care in Rural Kenya: A Qualitative Interview Study. Poster session presented at the International AIDS Conference; Vienna, Austria. Jul, 2010. [Google Scholar]
- World Health Organization. UNAIDS. UNICEF [Retrieved online August 14, 2011];Progress Report, 2009. 2009 from http://www.who.int/hiv/amds/who_introduction_universal_access_souteyrand.pdf.
- World Health Organization. UNAIDS. UNICEF . Towards Universal Access : Scaling up priority HIV/AIDS interventions in the health sector : Progress report 2009. World Health Organization; Geneva, Switzerland: 2009. [Google Scholar]
- Yebei VN, Fortenberry JD, Ayuku DO. [Retrieved online on August 18, 2011];Felt stigma among people living with HIV/AIDS in rural and urban Kenya. Afr Health Sci. 2008 8(2):97–102. from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2584319/?tool=pubmed. [PMC free article] [PubMed] [Google Scholar]