To the Editor
In a previous communication (1), we traced the history of spending on cardiovascular disease (CVD) treatment, prevention, and research since 1996. As we noted there, such spending estimates naturally lead to the question of whether the money has been well spent. To begin to address this question, we extend our previous results to provide a preliminary indication of the cost-effectiveness of these expenditures and to identify gaps in the cost-effectiveness literature.
To accomplish this, we link the previously-reported spending data with data from the Cost-Effectiveness Analysis (CEA) Registry maintained by Tufts Medical Center (www.cearegistry.org). The Registry is a nationally and internationally known and respected resource containing detailed, standardized information on more than 2,800 published cost-effectiveness analyses evaluating a wide range of medical and health interventions. Each paper catalogued in the Registry estimates the cost-effectiveness as an intervention’s incremental costs (expressed here in 2010 U.S. dollars) divided by its health benefits quantified in terms of quality-adjusted life-years (QALYs) (2). Low cost-effectiveness ratios are “favorable” because they indicate that incremental QALYs can be accrued inexpensively. An intervention is “cost-saving” if it reduces costs while improving health. Poorly performing interventions can both increase costs and make health worse. The combined dataset links expenditures associated with treatment or prevention of each type of CVD with cost-effectiveness information for many of the interventions for treating or preventing the condition. In an attempt to control for the variability in the quality of the cost data in the studies extracted from the Registry, we have included in the combined dataset only studies that treated the discounting of cost and effectiveness properly.
Table 1 summarizes the expenditure data previously presented in (1), including national expenditures for various years and compound annual growth rates for these expenditures from 1996 through 2008. To these data we have appended 1) the number of Registry-catalogued CEA studies published between 2000 and early 2011, 2) the number of studies per billion dollars of spending, and 3) the median cost per QALY calculated for interventions in each spending category. The first two of these statistics provide a rough indication of the resources devoted to studying the cost-effectiveness of interventions for each condition and how that sum compares to medical expenditures for that condition; the third statistic provides a rough indication of the cost-effectiveness of the medical spending.
Table 1.
CVD Expenditures and Cost-Effectiveness Findings by Spending Category
| Expenditures by Year ($ Billions)
|
Annual Growth | # of CEA Studies | Studies/$B Spending | Median $/QALY | |||
|---|---|---|---|---|---|---|---|
| 1996 | 2002 | 2008 | |||||
| Treatment | $ 133.6 | $ 166.6 | $ 234.4 | 4.8% | 262 | 1.12 | $ 22,625 |
| Heart conditions | $ 81.0 | $ 94.2 | $ 137.1 | 4.5% | 193 | 1.41 | $ 27,517 |
| Coronary Heart Disease | $ 53.5 | $ 55.2 | $ 82.6 | 3.7% | 88 | 1.06 | $ 22,113 |
| Congestive Heart Failure | $ 12.3 | $ 17.6 | $ 24.7 | 6.0% | 31 | 1.26 | $ 49,637 |
| Dysrhythmias | $ 12.6 | $ 16.4 | $ 24.4 | 5.6% | 30 | 1.23 | $ 48,183 |
| Cerebrovascular disease | $ 22.9 | $ 24.0 | $ 38.0 | 4.3% | 41 | 1.08 | $ 12,427 |
| Prevention | $ 22.1 | $ 43.3 | $ 68.3 | 9.9% | 97 | 1.42 | $ 16,866 |
| Hypertension | $ 13.3 | $ 24.0 | $ 30.5 | 7.2% | 25 | 0.82 | $ 5,754 |
| Hyperlipidemia | $ 4.0 | $ 11.5 | $ 26.9 | 17.1% | 9 | 0.33 | $ 31,614 |
| Total | $ 155.7 | $ 210.0 | $ 302.8 | 5.7% | 359 | 1.19 | $ 20,555 |
Figure 1 illustrates the distribution of cost-effectiveness ratios for CVD preventive interventions and for CVD treatments. The figure is similar to that presented by Cohen et al. for all conditions (3), but is updated and restricted to CVD interventions.
Figure 1. Distribution of Cost-Effectiveness Ratios for CVD Preventive Measures and Treatments.
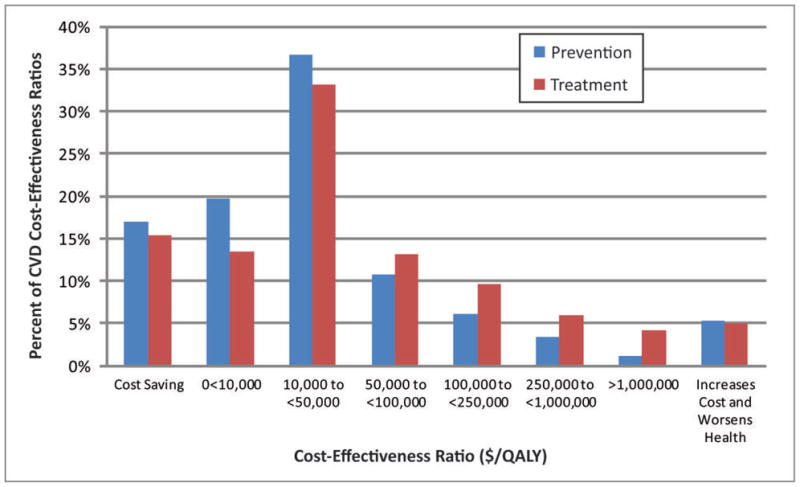
Data are from the Tufts-New England Medical Center Cost-Effectiveness Registry. QALY denotes quality-adjusted life-year. Percentages represent the proportion of ratios published in the registry for CVD preventive measures or CVD treatments that fall within each cost-effectiveness range.
We observe the following from these exhibits:
Median values in the far right column of Table 1 and the general shape of the bar chart in Figure 1 suggest that, in general, preventive measures are slightly more cost-effective than treatment interventions. For example, the table suggests that the median ratio across all treatment interventions is nearly $6,000 per QALY greater (less favourable) than the median ratio for prevention.
Most interventions, whether for prevention or treatment, do not save money: as the figure indicates, just over 15% of interventions in either class are cost saving. (This is also true of interventions addressing a broad range of conditions (3)).
On the other hand, all median ratios in the table are less than the $50,000 per QALY threshold sometimes suggested as a conservative basis for classifying interventions as cost-effective – i.e., providing good value (4).
However, the figure illustrates that 16% of preventive measures and 25% of treatments have cost-effectiveness values exceeding $100,000 per QALY, the threshold sometimes considered to be an upper bound on what is considered good value. These results suggest that there may be opportunities to improve the cost-effectiveness of both prevention and treatment of CVD by reallocating resources away from less efficient measures and towards more efficient measures.
The table suggests that hypertension prevention is highly cost-effective in general, with a median value of $5,754 per QALY.
Relative to the spending on prevention of hyperlipidemia, there are relatively few cost-effectiveness studies (0.33 studies per billion dollars of expenditures in this category), possibly suggesting a need for further analysis of hyperlipidemia measures.
With the exception of hyperlipidemia, the number of studies pertaining to each spending category is roughly proportional to spending levels, with values ranging from 0.82 to 1.42 studies per billion dollars of expenditures.
Linking category expenditures and cost-effectiveness information produces a rough indication of where CVD spending appears to be cost-effective and where additional study may be needed to better characterize cost-effectiveness. Our work continues toward refining these linkages.
Acknowledgments
This research was supported by Award Number R21HL098874 from the National Heart, Lung, and Blood Institute (NHLBI). The content is solely the responsibility of the author and does not necessarily represent the official views of the NHLBI or the National Institutes of Health.
List of Abbreviations
- CVD
cardiovascular disease
- CEA
cost-effectiveness analysis
- QALYs
quality-adjusted life years
Footnotes
None of the authors has any relationship with industry.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Miller G, Hughes-Cromwick P, Roehrig C. National spending on cardiovascular disease, 1996–2008. Journal of the American College of Cardiology. 2011;58(19):2017–2019. doi: 10.1016/j.jacc.2011.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neumann P, Greenberg D. Is the United States ready for QALYs? Health Affairs. 2009;28(5):1366–1371. doi: 10.1377/hlthaff.28.5.1366. [DOI] [PubMed] [Google Scholar]
- 3.Cohen J, Neumann P, Weinstein M. 2008 Does preventive care save money? Health economics and the presidential candidates. The New England Journal of Medicine. 2008;358(7):661–663. doi: 10.1056/NEJMp0708558. [DOI] [PubMed] [Google Scholar]
- 4.Evans C, Tavakoli M, Crawford B. Use of quality adjusted life years and life years gained as benchmarks in economic evaluations: a critical appraisal. Health Care Management Science. 2004;7:43–49. doi: 10.1023/b:hcms.0000005397.93173.bb. [DOI] [PubMed] [Google Scholar]


