Abstract
AIMS
Given the reported high rates of medication errors, especially in elderly patients, we hypothesized that current curricula do not devote enough time to the teaching of geriatric pharmacology. This review explores the quantity and nature of geriatric pharmacology education in undergraduate and postgraduate curricula for health professionals.
METHODS
Pubmed, Embase and PsycINFO databases were searched (from 1 January 2000 to 11 January 2011), using the terms ‘pharmacology’ and ‘education’ in combination. Articles describing content or evaluation of pharmacology education for health professionals were included. Education in general and geriatric pharmacology was compared.
RESULTS
Articles on general pharmacology education (252) and geriatric pharmacology education (39) were included. The number of publications on education in general pharmacology, but not geriatric pharmacology, has increased over the last 10 years. Articles on undergraduate and postgraduate education for 12 different health disciplines were identified. A median of 24 h (from 15 min to 4956 h) devoted to pharmacology education and 2 h (1–935 h) devoted to geriatric pharmacology were reported. Of the articles on education in geriatric pharmacology, 61.5% evaluated the teaching provided, mostly student satisfaction with the course. The strength of findings was low. Similar educational interventions were not identified, and evaluation studies were not replicated.
CONCLUSIONS
Recently, interest in pharmacology education has increased, possibly because of the high rate of medication errors and the recognized importance of evidence-based medical education. Nevertheless, courses on geriatric pharmacology have not been evaluated thoroughly and none can be recommended for use in training programmes. Suggestions for improvements in education in general and geriatric pharmacology are given.
Keywords: geriatrics, medical education, pharmacology, pharmacotherapy, postgraduate, undergraduate
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
The rate of medication errors is high, and these errors can cause adverse drug reactions. Elderly individuals are most vulnerable to adverse drug reactions.
One cause of medication errors is the lack of drug knowledge on the part of different health professionals.
Medical curricula have changed in recent years, resulting in less education in the basic sciences, such as pharmacology.
WHAT THIS STUDY ADDS
Our study shows that little curricular time is devoted to geriatric pharmacology and that educational programmes in geriatric pharmacology have not been thoroughly evaluated.
While interest in pharmacology education has increased recently, this is not the case for geriatric pharmacology education.
Education on geriatric pharmacology should have more attention in the curricula of health professionals, given the often complex pharmacotherapy in elderly patients.
Educational topics should be related to the known risk factors of medication errors, such as polypharmacy, dose adjustments in organ dysfunction and psychopharmacotherapeutics.
Introduction
Medication errors due to human mistakes have raised concerns about the pharmacological knowledge of different health professionals [1, 2]. Medication errors may lead to adverse drug reactions (ADRs) [3], which, in turn, are responsible for 3.0–6.5% of all hospital admissions [3–6]. The numbers are even higher for elderly individuals, ranging from 3.6 to 13.3% [4–6]. About 47–72% of ADRs are potentially preventable [3, 5]. The main cause of medication errors is insufficient knowledge of drug therapy on the part of doctors and other health professionals [1, 7]. Moreover, pharmacotherapy is becoming more complex, especially in older patients [7]. Worldwide, elderly people form the largest group of people admitted to hospital, and the elderly population is increasing rapidly [8, 9]. This means that most healthcare professionals will face the challenge of prescribing for elderly patients. In the last decade, medical and nursing curricula have changed, with less time being devoted to basic sciences, such as pharmacology [10, 11]. The focus of medical curricula has changed from basic science discipline-based to integrated organ- and disease-based approaches since the introduction of problem-based learning in the 1970–1980s in many places in the world [11–13], and in nursing curricula there has been a shift from a biomedical model focused on curing to a holistic model focused on caring [10]. This has frequently resulted in abandoning separate pharmacology courses and integrating pharmacology into problem-oriented courses. The lack of a thorough grounding in the medical sciences might contribute to insufficient knowledge of clinical pharmacology and drug therapy [14]. Moreover, there seem to be few effective programmes for teaching health professionals' prescribing skills. The systematic review of Ross et al. identified the ‘World Health Organization guide to good prescribing’ as the only effective programme for teaching medical students how to prescribe [15, 16]. Little is known about the education in pharmacology given to health professionals other than medical students, and even less is known about their education in geriatric pharmacology.
Given the high rates of medication errors worldwide, we hypothesized that health professionals receive insufficient education in pharmacology, and especially in geriatric pharmacology, during their training. We performed a systematic review to gain insight into education in geriatric pharmacology in terms of its volume and content in curricula and to establish what constitutes effective education in geriatric pharmacology.
Methods
The review was performed using the PRISMA guidelines for systematic reviews and meta-analysis and the Cochrane guidelines [17, 18].
Data sources and search strategy
To put education in geriatric pharmacology in the context of education in general pharmacology, we searched the literature for studies on education in pharmacology, focusing on the literature after 2000. The reason for limiting the search to the period between 2000 and 2011 is to minimize results from curricula that no longer exist. Medical curricula change regularly, and many have changed to problem-based formats. An 11 year period provides a reasonable chance to report on current practices.
The databases PubMed, Embase and PsycINFO were searched from 1 January 2000 to 11 January 2011 using the terms ‘pharmacology’ (in title/abstract) combined with ‘education’ (in title), and synonyms. Articles on education in geriatric pharmacology were manually selected from this broader search, because adding the term ‘geriatric’ and synonyms resulted in an improbably low number of articles. Limits other than time limits were not used in the searches. The search syntax used in Pubmed, Embase and PsycINFO is depicted in Figure 1.
Figure 1.
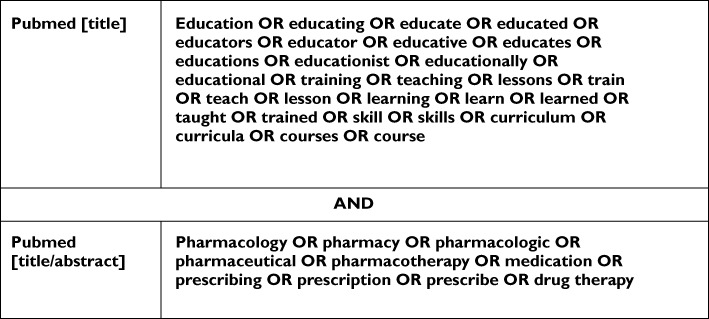
Search syntax in PubMed. Equal search strategy in Embase and PsycINFO (limit: 1 January 2000 to 11 January 2011)
All duplicate articles were excluded, and the remaining articles were screened on title, abstract and full text. If an abstract was not available, the full text of the article was screened. If the full-text article was not retrievable from the corresponding author or from national university libraries, the article was excluded. Articles cited by another article for the description of the education were included as related articles.
Study selection
First, all titles were screened for relevance using the following exclusion criteria: (i) animal studies or nonhuman pharmacology education; (ii) content not (pharmacology) education; (iii) education for patients or informal caregivers; and (iv) educational terminology used with a non-educational meaning, e.g. teaching hospital. Second, the abstracts were screened for relevance using the same exclusion criteria as above with the additional exclusion criterion of language different from English, German or Dutch. Third, all relevant full-text articles were screened using the following exclusion criteria: (i) language different from English, German or Dutch; (ii) education for patients or informal caregivers (not health professionals); (iii) does not contain description of pharmacology education in terms of content or quantity; (iv) only congress abstract available without a description of education; and (v) full text not available.
Study eligibility criteria
We considered all articles on education in geriatric pharmacology for health professionals. Education was defined as any structured educational activity. First, all articles describing pharmacology education for health professionals were selected. Articles were eligible if the education was described in terms of study load (study hours) or content; content was described in terms of educational topic and teaching method. Second, articles on education in geriatric pharmacology were selected from the articles on pharmacology education, namely, articles covering geriatrics, specific geriatric syndromes (e.g. Alzheimer's disease, delirium) or specific problems common in a geriatric population (e.g. polypharmacy, renal failure) as educational topic. There were no eligibility criteria for study design. All articles on education in geriatric pharmacology were independently assessed by three authors (C.J.P.W.K., L.vH. and L.J.) in terms of the educational content, study load and evaluation. The reviewers reached full consensus on eligibility of the studies after discussion.
Data extraction
To enable comparison of education in geriatric pharmacology and general pharmacology, we extracted information about the status of the education (mandatory or elective). If the education was given as part of a university or school curriculum, it was assumed to be mandatory if not mentioned otherwise. The study load was extracted and described in terms of study hours devoted to pharmacology education, and in proportion to the total study load, if this information was provided. Credit hours (CHs) were transformed to 40 study hours, ECTS (European Credit Transfer System) to 28 study hours, and 1 day to 8 study hours if not described otherwise in the article. Education was classified by health profession and by undergraduate or postgraduate level.
Qualitative grading
The methodology used to evaluate the education, summarized as strength of findings, and the impact of the studies were graded. The Best Evidence Medical Education (BEME) criteria were used to grade the methodology [19]. The BEME score is based on critical appraisal of the study and reflects the credibility of study results. Scores range from 1 to 5, as follows: level 1, no clear conclusions can be drawn, not significant; level 2, results ambiguous, but there appears to be a trend; level 3, conclusions can probably be based on the results; level 4, results are clear and very likely to be true; and level 5, results are unequivocal. The Kirkpatrick model of hierarchy of evaluation, modified by Freeth, was used to evaluate the impact of the education [20, 21]. Scores range from 1 to 4, as follows: level 1, learners reaction such as learners' views on the learning experience; level 2a, modified attitude; level 2b, acquisition of knowledge or skills; level 3, behavioural changes; level 4a, change in organization practice; and level 4b, benefits to patients.
Data synthesis
All descriptive analyses were performed in SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL, USA). The proportion of articles published in different years, in different continents and with regard to different health professions were calculated. When ranges of study hours were given in an article, these were not used to calculate median values.
Results
Search results
Figure 2 shows the flowchart of the review. Of 9819 articles retrieved, 252 concerned pharmacology education and were included. Of these 252 articles, 39 reported on education in geriatric pharmacology as defined in the eligibility criteria.
Figure 2.
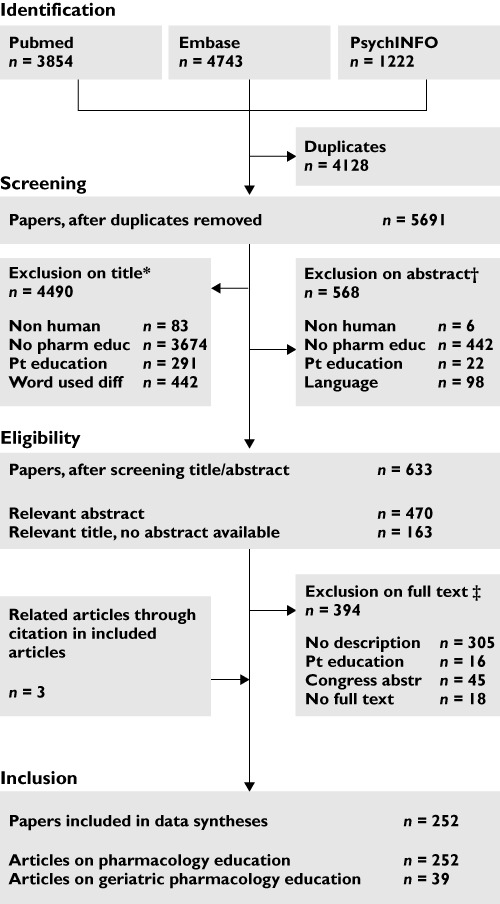
Search results with reasons for exclusion. *Exclusion criteria: Non human, animal studies or nonhuman pharmacology education; No pharm educ, content not (pharmacology) education; Pt educ, education for patients or informal caregivers (not health professionals); and Word used diff, the word education is used in a different way from education (e.g. teaching hospital, learning disabilities). † Exclusion criteria: Language, language other than English, German or Dutch. ‡ Exclusion criteria: No description, does not contain objective and quantitative description of pharmacology education; Congress abstr, only congress abstract available without a quantitative description of education; and No full text, not available in full text for screening, despite all efforts, and thus excluded
Study characteristics
The number of articles on pharmacology education appeared to have increased in the past decade, from six articles in 2000 to 45 articles in 2010. No such trend was seen for articles on education in geriatric pharmacology (Figure 3).
Figure 3.
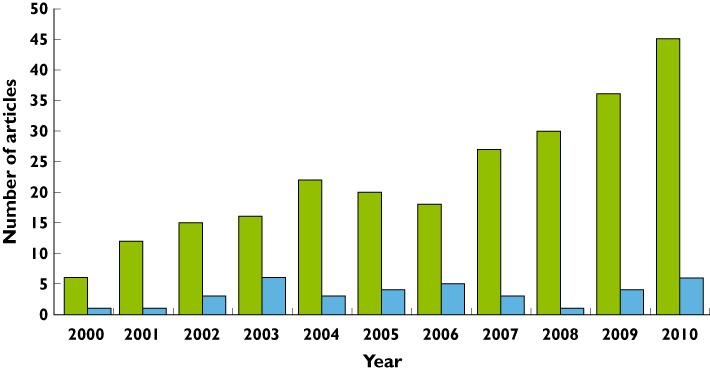
Relevant articles on pharmacology education and geriatric pharmacology education per year. The three related articles in Figure 2 were from the period before 2000 and are not included. General pharmacology education ( ); Geriatric pharmacology education (
); Geriatric pharmacology education ( )
)
Most articles came from North America and Europe, 106 (42.6%) and 82 (32.9%) respectively, and mainly from the USA (n = 90, 36.1%) and the UK (n = 37, 14.9%). However, all continents were represented in the literature on pharmacology education. The topics described in most articles on pharmacology education were clinical pharmacology and therapeutics (28.5%), different medication groups (9.2%), geriatrics (6.4%) and basic knowledge of pharmacology (6.0%). For twelve different health professionals and students education was identified.
Education in general and geriatric pharmacology
A median of 24 h (range 0.25–4965 h) was devoted to education in general pharmacology and a median of 2 h (range 1–935 h) to education in geriatric pharmacology (Table 1). The majority of studies did not provide information about the total study load; therefore, the proportion of the total study load could not be calculated for either general or geriatric pharmacology education.
Table 1.
Time spent on education in general pharmacology and geriatric pharmacology for different health professionals and students
| Articles (n) | General pharmacology education* | Geriatric pharmacology education* | ||
|---|---|---|---|---|
| Health professional | General pharm educ | Geriatric pharm educ | Education time median h (range) | Education time median h (range) |
| Undergraduate | ||||
| Medical student | 61 | 12 | 80 (1.5–4956) | 1.5 (1–23) |
| Pharmacy student | 85 | 13 | 20 (1–400) | 10 (1–160) |
| Nursing student | 16 | 2 | 13 (1.25–85) | NA |
| Paramedical student | 2 | NA | 20 | NA |
| Dental student | 1 | NA | 20 | NA |
| Nurse practitioner student | 1 | 1 | NA | NA |
| Postgraduate | ||||
| Physician | 47 | 11 | 8 (0.5–160) | 2 (1.25–23) |
| Pharmacist | 21 | 2 | 20 (0.25–935) | 471 (7–935) |
| Nurse | 25 | NA | 15 (0.25–304) | NA |
| Physician assistant | 1 | NA | 3 | NA |
| Nurse aractitioner | 1 | NA | 3 | NA |
| Other paramedical health professional | 2 | NA | 38 | NA |
| Total† | 263 | 41 | 24 (0.25–4965) | 2 (1–935) |
Eighty-nine articles lacked a description of the education time and were left out of the calculations.
Eleven articles had descriptions of education for more than one health professional. NA, data not available. The proportion to the total study load could not be calculated due to a lack of data on total study load in the majority of studies.
There were no studies reporting education in geriatric pharmacology for paramedical students, dental students, nurses, nurse practitioners, physician assistants and other paramedical health professionals. As shown in Table 1, the geriatric pharmacology study load was described for undergraduate and postgraduate medical and pharmacy courses only.
Table 2 describes the content, study load and evaluation of education in geriatric pharmacology in undergraduate (n = 18) and postgraduate curricula (n = 14). Twenty-four of the 32 articles (61.5%) presented data on the evaluation of education in geriatric pharmacology.
Table 2.
Pre- and postgraduate geriatric pharmacology education, sorted by health professional
| Study | Country | Health professional | Course description | Quantitative description | Type of teaching | In curriculum | Evaluation | Level of evaluation* | Strength of findings† | |
|---|---|---|---|---|---|---|---|---|---|---|
| Undergraduate | ||||||||||
| Estus et al. (2010) [52, 53] | USA | Pharm students (pharmD) | Geriatric pharmacotherapy | 120 h (3 CH) | Facebook, ‘adopt a patient’, patient cases, book and film clubs, lectures, scientific and reflective writing | Yes | Elective | Students' (n = 28) satisfaction on Facebook use: 93% valuable. Students' (n = 92) satisfaction on other teaching methods: 3.8–4.7 out of maximum 5 points | 1 | 1 |
| Jaedhe (2009) [54] | Germany | Pharm students | Individual pharmacotherapy, 1/6 topics geriatric patients | 5 h for 6 topics | Lectures | Yes | Both | ? | ||
| Divine & Cain (2009) [55] | USA | Pharm students | Polypharmacy adherence as part of geriatric course | Total course 120 h (3 CH) | Polypharmacy medication simulation project, reflective assignment | Yes | Elective | Qualitative research on students' satisfaction (n = 173, response rate 100%): 83% positive comments on education on open-ended questions | 1 | 1 |
| Ross et al. (2006) [56] | USA | Pharm students | Vertical integrated course. 68 topics of which Alzheimer's and Parkinson's disease | 80 h for 68 topics | Small groups | Yes | Mandatory | ? | ||
| Sauer (2006) [24] | USA | Pharm students | Pharmacy practice experience in ambulatory care, topic geriatrics | 6 weeks, half time | Rotations | Yes | Mandatory | Qualitative research using portfolio essays: 107 of 117 portfolios studied, essay pre-experience and postexperience. Students' attitudes towards elderly improved | 2a | 4 |
| Lam (2005) [57] | USA | Pharm students | Geriatric clerkship | 160 h | Clerkship | Yes | Elective | Students n = 24. 65% of written advices to prescribers was adopted by prescriber | 4b | 1 |
| Bratt (2003) [58] | UK | Pharm students | CNS pharmacology, 1 topic: Alzheimer's disease | 10 h | Integrated, hybrid lecture and PBL containing lectures, seminars and self study | Yes | Mandatory | Of 104 students, 51.4% preferred traditional lectures to the PBL; 54.2% PBL did aid knowledge retention. Mature students (44%) vs. younger students (25.8%) preferred PBL over traditional lectures (P < 0.01, Mann–Whitney U rank sum test) | 1 | 1 |
| Strohkirch & Jaehde (2003) [59] | Germany | Pharm students | clinical pharmacology. Topics: geriatrics, renal failure, medication review | ? | Lectures, workshops, bedside teaching, practice simulation | Yes | Elective | ? | ||
| George & Jacobs (2011) [60] | USA | Medical students, residents and fellows | Geriatric pharmacotherapy | 23 times, 1 h sessions | Seminars using the Medication Screening Questionnaire | Yes | ? | Qualitative evaluation of education. 163 of 241 participants. 99% (strongly) agreed that overall quality of the sessions was excellent. All (strongly) agreed on meeting learning goals | 1 | 1 |
| Naritoku & Faingold (2009) [61] | USA | Medical students | Pharmacotherapeutics, 1 topic, Alzheimer's disease | 1 h | (Interactive) lectures | Yes | Mandatory | n = 39, response rate 64%. Students' satisfaction on Alzheimer's topic: 4.7 ± 0.61 (out of 5) | 1 | 1 |
| Franson et al. (2008) [22] | Netherlands | Medical students | Pharmacology, 1 topic geriatrics | Average time 1–2 h | e-Learning | Yes | Mandatory | 1100 students, >175 000 hits. Time spent on the program was associated with grades on topic: regression equation grade = 5.02 + 0.034 × time spent on program | 2b | 3 |
| Dubois et al. (2007) [23] | Netherlands | Medical students | Geriatric pharmacotherapy | ? | Therapeutic plan writing and self-study computer materials | Yes | Both | Cohort 1999 vs. cohort 2000 with intervention: percentage of students with sufficient result on therapeutic plan writing in intervention cohort improved compared with pre-intervention cohort (31% vs 69% two-sample t-test, P < 0.05) | 2b | 4 |
| Smith et al. (2006) [62] | Australia | Medical students | Polypharmacy as part of rational prescribing course | 12 modules | e-Learning | Yes | ? | In total, 363 students on online survey (response rate 6–13% in different years): 91–92% content module appropriate, 78–86% felt equipped to prescribe | 1 | 1 |
| Eroglu & Uresin (2003) [63] | Turkey | Medical students | Pharmacology education, geriatrics 1 of 17 subjects | 24 h for all 17 subjects | PBL | Yes | Mandatory | ? | ||
| Herzig et al. (2003) [64]; Antepohl & Herzig (1999) [65] | Canada | Medical students | Pharmacology course, 1 topic Parkinson's disease | 3 h per topic | Problem based learning vs Lecture based learning | No | Pretest, post-test, post-test after 18 months showed no differences in the PBL group (n = 17/55, mean score on final test 20.1 ± 5.0) vs. the lecture-based learning group (n = 15/57, mean score on final test 19.0 ± 4.7) on pharmacology knowledge. 80 students were lost to follow-up for the final post-test | 2b | 1 | |
| Faingold & Dunaway (2002) [66] | USA | Medical students | CNS. Topics: Parkinson's disease, dementia | 1.5 h for both topics together | Integrated lectures, small groups | Yes | Mandatory | ? | ||
| Lathers & Smith (2002) [67] | USA | Medical students, residents | Geriatric clinical pharmacology | 2 h | ‘Clinical pharmacology problem-solving unit’. Case-based learning | Yes | ? | Of 455 students and residents, 40% (range in different years 25–65%) found it useful for learning | 1 | 1 |
| Lim & Honey (2006) [68] | New Zealand | Nursing students | Elderly pharmacokinetics | ? | Integrated, PBL | Yes | Mandatory | ? | ||
| Postgraduate | ||||||||||
| Leikola et al. (2009) [69] | Finland | Pharmacists | Comprehensive medication review, rational prescribing, clinical pharmacology | 935 h (35 ECTS) | Seminars, e-learning, learning in practice | Yes | Elective | Online evaluation (n = 38, response rate 90%): 92% met educational needs, 95% would recommend training to peers | 1 | 1 |
| Demirkan et al. (2004) [35] | Turkey | Pharmacists | Good practice pharmacists, 1 topic: group at risk (geriatric, renal and liver failure) | 7 h | Lectures, workshops | Yes | Elective | 95 pharmacists participated: score on pretest vs. post-test on all topics: 36.1 ± 7.9 vs. 56.6 ± 10.3 | 2b | 3 |
| Strohkirch & Jaehde (2003) [59] | Germany | Pharmacists | Clinical pharmacology | 1 year, 4 modules at university | Practice in own work environment, online support | Yes | Elective | ? | ||
| Warshaw et al. (2010) [70] | USA | GP | Medication management as part of geriatric education | 1.25 h medication management | Presentations | Yes | ? | 60 GPs: response rate 80–93% (over different years). Score 3.8 out of 4 on presentation content, quality and meeting educational needs | 1 | 1 |
| Midlöv et al. (2006) [31] | Sweden | GP | Psychoactive drugs | 2 visits | Outreach visits | No | Decrease in benzodiazepine prescribing after 9 months in intervention group (n = 23) compared with control group (n = 31) (P < 0.05). GP's satisfaction: median 8–10 out of 10 on 6 subjects | 1,4b | 4 | |
| Straand et al. (2006) [71] | Norway | GP | Pharmacotherapeutics | 2 visits, 8 h workshop | Outreach visits, workshops, feedback reports | No | ? | |||
| Pimlott et al. (2003) [32] | Canada | GP | Benzodiazepine use in elderly | 3 times in 6 months | Educational bulletins, feedback on prescriptions | No | Randomisation of physicians. Intervention (n = 168) vs. control group (n = 206): 0.7% decrease vs. 1.1% increase in long-acting benzodiazepine (P = 0.036, not clinically relevant), no other significant differences | 4b | 3 | |
| Lutters et al. (2004) [72] | Switzerland | Hospital physicians | Antibiotics prescriptions in elderly | Weekly ward rounds | Ward rounds with infectious disease specialist, lectures, individual counselling, pocket cards | Yes | Mandatory | Interventional cohort study (before, during and after intervention): 680 patients receiving antibiotics included: 15% reduction in proportion of patients receiving antibiotics (P = 0.08), 26% reduction in number of antibiotics administered (P < 0.001). In 83 of 110 patients, guidelines correctly implemented | 4b | 2 |
| George & Jacobs (2011) [60] | USA | Residents and fellows, medical students | Geriatric pharmacotherapy | 23 times, 1 h sessions | Seminars using the Medication Screening Questionnaire | Yes | ? | Qualitative evaluation of education. 163 of 241 participants. 99% (strongly) agreed that overall quality of the sessions was excellent. All (strongly) agreed on meeting learning goals | 1 | 1 |
| Naughton et al. (2010) [33] | USA | Internal medicine residents | Polypharmacy training as part of NSAID prescribing training | 7 monthly modules | Patient chart review, lectures | Yes | Mandatory | 35 postgraduate internal medicine residents. Pre-intervention vs. postintervention: reduction in NSAID prescribing after 1 year: 29 vs. 16% (P = 0.002) reduction in NSAID and 14 vs. 7% reduction in NSAID in conjunction with a diuretic (P = 0.024) | 4b | 3 |
| Baum & Harder (2010) [34] | Germany | Residents, senior physicians | Renal failure adjustments | 2 h | Lecture | Yes | ? | 8 physicians. 2 patient cohorts: pre-education (n = 85) vs. posteducation (n = 85). Cohort 1, 55 of 85 misdosing vs. cohort 2, 28 of 85 misdosing at day 2 of hospital admission (P = 0.05) | 4b | 3 |
| Montagnini et al. (2004) [73] | USA | Internal medicine residents | Geriatric and palliation rotation | One month rotation. Amount of hours on pharmacology education unclear. | Lectures, bedside teaching, conferences, practice-based learning | Yes | Mandatory | 28 residents completed the evaluation forms (prerotation and postrotation). On palliation topics (including delirium), residents self-assessments increased from 2.89–3.71 to 4.10–4.67 (out of 5). P < 0.00001 | 2b | 2 |
| Lathers & Smith (2002) [67] | USA | Residents (medical, psychiatry), medical studdents | Geriatric clinical psychopharmacology | 2 h | ‘Clinical pharmacology problem-solving unit’. Case-based learning | Yes | ? | Of 455 students and residents, 40% (range in different years 25–65%) found it useful for learning | 1 | 1 |
| Meagher (2010) [74] | UK | Healthcare workers | Pharmacotherapy in delirium | 2 h | Workshop | No | Congress workshop. n = 66 (response rate unknown). Pre-education vs. posteducation on rating adverse events: concerns regarding extrapyramidal side effects reduced (52 vs. 21%; P < 0.001). Posteducation survey on future pharmacotherapy: positive attitude regarding prophylaxis in high-risk patients: 56% respondents. | 2a | 1 | |
Abbreviations: CH, credit hour; CNS, central nervous system; ECTS, European Credit Transfer System; NSAID, nonsteroidal anti-inflammatory drug; GP, General Practitioner; PBL, problem-based learning; and Pharm students, pharmacy students.
Modified level of evaluation of Kirkpatrick.
Strength of findings after critical appraisal.
Undergraduate education in geriatric pharmacology
As shown in Table 2, there was no uniform course on geriatric pharmacology for medical, pharmacy or nursing students, with courses differing in terms of topics covered and/or teaching method. There was little evidence that the education in geriatric pharmacology was effective; 67% (12 of 18) of the educational programmes had methodological problems and/or low levels of impact, such as students' satisfaction. No evaluation studies were replicated. Of articles reporting on courses for medical students, Franson et al. described an effective e-learning programme for pharmacology, in which geriatrics was one of the topics covered [22]. Dubois et al. reported that a therapeutic plan-writing course improved the therapeutic plan-writing skills of students who completed the course [23]. With regard to pharmacy students, Sauer showed that an ambulatory care service rotation improved students' attitudes towards the elderly [24].
Seven survey studies have described education in geriatric pharmacology for different health professionals in general without a description of the precise content of the education or an evaluation of the education. Therefore, these studies were not included in Table 2. [10, 25–30]. Of these studies, five concerned surveys with large methodological differences of the American and Canadian schools and universities for pharmacy, showing large differences in the provision of courses on geriatric pharmacology. Taken together, these studies describe that 53–100% of the schools and colleges provided some education on the topic within separate non-integrated courses, during integrated education or during geriatric clerkships [25–29]. One study showed that all UK colleges of nursing provided some form of education in medicine and the elderly [10]. Another survey of the schools for nurse practitioners shows that 96% covered the topic ‘elderly individuals’ in the pharmacology and pharmacotherapy course [30].
Taken together, no single undergraduate course in geriatric pharmacology has been broadly implemented, i.e. no examples of geriatric pharmacology education were reported to be used inter-institutionally, and no studies evaluating educational interventions have been replicated.
Postgraduate geriatric pharmacology education
Again, there were no uniform postgraduate courses on geriatric pharmacology for physicians or pharmacists, with courses differing in their content and/or teaching methods. Twelve of the 14 articles (86%) evaluated courses, but there were methodological problems in most studies. In contrast to the undergraduate courses, the postgraduate courses were mostly evaluated in terms of improving patient care. Again, no educational programme was evaluated more than once. For general practitioners, Midlöv et al. showed that outreach visits could decrease benzodiazepine use in elderly patients [31]. Pimlot et al. showed that educational bulletins and feedback on prescriptions for general practitioners could cause a small, probably not relevant, decrease in the use of long-acting benzodiazepines [32]. For residents, Naughton et al. found a reduction in inappropriate nonsteroidal anti-inflammatory drug use after polypharmacy medication review and lectures [33]. Baum and Harder showed that a lecture for senior physicians and residents on renal failure adjustments led to a decrease in medication misdosing [34]. Demirkan et al. evaluated a course for pharmacists containing lectures and workshops about drug therapy for groups at risk [35].
Taken together, there was no broadly implemented course on geriatric pharmacology in postgraduate curricula for physicians or pharmacists, i.e. no examples of geriatric pharmacology education were reported to be used inter-institutionally, and no studies evaluating educational interventions have been replicated.
Discussion
The increasingly complex pharmacotherapy, especially in elderly patients, and medication errors due to health professionals' lack of knowledge of drug therapy, leads to an urgent need to improve health professionals' knowledge of geriatric pharmacology. This review shows that interest in education in general pharmacology is increasing, with undergraduate and postgraduate courses providing a median of 24 h of teaching in general pharmacology. In contrast, interest in education in geriatric pharmacology has not increased in the last decade, with undergraduate/postgraduate courses providing a median of 2 h of teaching in geriatric pharmacology per course. Taken together, we found that undergraduate and postgraduate curricula for different health professionals devote relatively little study time to general and geriatric pharmacology. We could not retrieve reliable information on the proportion of time spent on geriatric pharmacology education relative to general pharmacology or to the total study load in the described curricula. In addition, we could not find any information on the optimal or desirable study load on and content of geriatric pharmacology education. Educational programmes in geriatric pharmacology have not been broadly implemented in curricula and have hardly been proved to be effective in evaluation studies. We conclude that there is no inter-institutional consensus about a best approach to geriatric pharmacology education.
While one would expect more time to be devoted to geriatric pharmacology education research, given the increasing interest in evidence-based medical education [36] and the high rate of medication errors in the vulnerable elderly [1, 37], this would not appear to be the case, even though databases such as PubMed showed increased numbers of publications searching for geriatrics, pharmacology and education separately. This review shows that the interest in research in general pharmacology education has increased, in contrast to research in geriatric pharmacology education. In addition, the need for improvement in geriatric education seems to be a worldwide issue for different health professionals [38, 39]. Taken together, it remains unexpected and unclear why there is not an increasing interest specifically in education in geriatric pharmacology, as there seems to be in pharmacology and geriatric education. This may underline the need for improvement in geriatric pharmacology education and research on this topic.
In contrast to ideas about the content and study load of a core curriculum for medical students, no mention is made of how many hours should be devoted to teaching geriatric pharmacology [11]. Although a clear norm on study load is not available, given the problems of complex pharmacotherapy in elderly patients, the present study load is probably insufficient [1].
None of the courses in geriatric pharmacology has been thoroughly researched and been proved to be effective, and no studies reporting education in geriatric pharmacology for paramedical students, dental students, nurses, nurse practitioners, physician assistants and other health professionals were found. We did not find clear best practices, but many interventions concerned polypharmacy, dose adjustments in elderly patients and in renal failure, and psychopharmacotherapeutics. This seems to be a logical choice for the content of the education, because these are all known risk factors for medication errors [3, 40, 41]. Odegard et al. suggested teaching geriatric pharmacology to pharmacy students in terms of values, attitudes, knowledge and skills [42]. In contrast to education in geriatric pharmacology, there is an effective educational programme for general pharmacotherapy. Medical students and junior doctors can be taught how to prescribe with the World Health Organization ‘Guide to Good Prescribing’, or six-step method, a broadly evaluated educational intervention on prescribing [15, 16].
The need to improve the pharmacological training of different health professionals is clear because it may decrease harmful medication errors [1]. In general, training is most effective if it fulfils three criteria: it is offered throughout the study; it is integrated in the curriculum; and it is placed in the context of clinical cases. Studies have shown that knowledge is best acquired and retained if it is imparted regularly in small portions [43], and that integration in the curriculum can lead to a more contextualized approach to learning [44]. Integration can be horizontal, with a more-or-less interdisciplinary approach within study years, or vertical, with integration between theoretical knowledge and clinical practice throughout the study years [44, 45]. Moreover, education with a focus on contextualization of pharmacology problems has been shown to improve pharmacotherapeutics [46]. A longitudinal course on clinical pharmacology and pharmacotherapy, although not specifically on geriatric pharmacology education, is described by Richir et al. and fulfils these criteria [47].
This study had several limitations. It was based on the literature, and the literature might not accurately reflect the amount of teaching devoted to specific topics in existing curricula. A large publication bias is likely. Therefore, it is difficult to draw conclusions about how many hours are actually spent on the topic. In this review, we primarily focused on evidence-based education with proof of efficacy of the education. However, in medical education research this proof is difficult to acquire because it is methodologically difficult to tie curricular interventions to relevant long-term outcomes effectively. This is due to the large and partly unclear set of variables of the contextually rich environment of medical education. One way to improve education might be to focus on understanding collective theoretical problems in this contextually rich environment, e.g. students' motivation, instead of looking for proof of the efficacy of a specific intervention [48]. Related to this problem, it must be noted that the evidence for an improvement in pharmacotherapy education leading to a reduction in medication errors in clinical practice is still weak. However, it is a generally accepted focus for preventing medication errors [1, 49]. As mainly junior doctors are involved in medication errors, it can be assumed that considerable knowledge acquisition occurs, often implicitly, through experience in the workplace [50, 51]. Explicit learning, such as courses, might make this implicit learning more explicit. In this review, we only addressed explicit learning. Finally, as we concentrated on studies published after the major curricular innovations of the late 1990s and the shift to problem-based learning, we do not know how effective the ‘traditional’ curricula were in teaching general pharmacology and, in particular, geriatric pharmacology.
This review shows that there is a considerable need to improve education in geriatric pharmacology for health professionals at both undergraduate and postgraduate levels, and that in general the current curricula do not devote enough time to the teaching of pharmacology. Moreover, the best way to provide this education needs to be investigated. The content of geriatric pharmacology education should be related to known risk factors of medication errors in elderly patients and should focus especially on the appropriate prescribing in the case of polypharmacy and renal failure and on the prevention of inappropriate prescribing of psychotropic drugs. The literature suggests that training in pharmacology might be most effective if it is offered throughout the medical curriculum, is integrated in the different disciplines and is given clinical relevance in the form of case studies. More research in the field of geriatric pharmacology education may contribute to improving the care for older people.
Acknowledgments
Expertise Centre Pharmacotherapy in Old Persons (EPHOR) is funded by the Netherlands Organisation for Health Research and Development (ZonMw).
Competing Interests
There are no competing interests to declare.
REFERENCES
- 1.Likic R, Maxwell SR. Prevention of medication errors: teaching and training. Br J Clin Pharmacol. 2009;67:656–61. doi: 10.1111/j.1365-2125.2009.03423.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco HJ, Gallivan T, Hallisey R, Ives J, Laird N, Laffel G. Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA. 1995;274:35–43. [PubMed] [Google Scholar]
- 3.Krahenbuhl-Melcher A, Schlienger R, Lampert M, Haschke M, Drewe J, Krahenbuhl S. Drug-related problems in hospitals: a review of the recent literature. Drug Saf. 2007;30:379–407. doi: 10.2165/00002018-200730050-00003. [DOI] [PubMed] [Google Scholar]
- 4.Kongkaew C, Noyce PR, Ashcroft DM. Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother. 2008;42:1017–25. doi: 10.1345/aph.1L037. [DOI] [PubMed] [Google Scholar]
- 5.Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329:15–9. doi: 10.1136/bmj.329.7456.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leendertse AJ, Visser D, Egberts AC, van den Bemt PM. The relationship between study characteristics and the prevalence of medication-related hospitalizations: a literature review and novel analysis. Drug Saf. 2010;33:233–44. doi: 10.2165/11319030-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Aronson JK, Henderson G, Webb DJ, Rawlins MD. A prescription for better prescribing. BMJ. 2006;333:459–60. doi: 10.1136/bmj.38946.491829.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Agency for Healthcare Research and Quality, Agency for Healthcare Research and Quality., U.S. Department of Health & Human Services. Available at http://www.ahrq.gov/data/hcup/factbk6/fbk6fig3.htm (last accessed 26 July 2011)
- 9. Hospital Episode Statistics HES (admitted patient care) England 2009/10, The Health and Social Care Information Centre. Available at http://www.ic.nhs.uk/news-and-events/news/elderly-people-account-for-bigger-proportion-of-nhs-hospital-activity-every-year-report-shows (last accessed 28 March 2012)
- 10.Morrison-Griffiths S, Snowden MA, Pirmohamed M. Pre-registration nurse education in pharmacology: is it adequate for the roles that nurses are expected to fulfil? Nurse Educ Today. 2002;22:447–56. [PubMed] [Google Scholar]
- 11.Maxwell S, Walley T BPS Clinical Section Committee. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow's doctors. Br J Clin Pharmacol. 2003;55:496–503. doi: 10.1046/j.1365-2125.2003.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harden RM, Sowden S, Dunn WR. Educational strategies in curriculum development: the SPICES model. Med Educ. 1984;18:284–97. doi: 10.1111/j.1365-2923.1984.tb01024.x. [DOI] [PubMed] [Google Scholar]
- 13.Wood DF. Problem based learning. BMJ. 2008;336:971. doi: 10.1136/bmj.39546.716053.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boreham NC, Mawer GE, Foster RW. Medical students' errors in pharmacotherapeutics. Med Educ. 2000;34:188–93. doi: 10.1046/j.1365-2923.2000.00510.x. [DOI] [PubMed] [Google Scholar]
- 15.Ross S, Loke YK. Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol. 2009;67:662–70. doi: 10.1111/j.1365-2125.2009.03395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing, a practical manual. World Health Organization. Available at http://apps.who.int/medicinedocs/pdf/whozip23e/whozip23e.pdf (last accessed 1 December 2011)
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cochrane Handbook for Systematic Reviews of Interventions, Cochrane Collaboration. Available at http://www.cochrane-handbook.org/ (last accessed 26 July 2011)
- 19.BEME Collaboration. Best Evidence Medical Education, BEME Collaboration. Available at http://www2.warwick.ac.uk/fac/med/beme/writing/startingreview/ (last accessed 26 July 2011)
- 20.Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M, Prideaux D. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28:497–526. doi: 10.1080/01421590600902976. [DOI] [PubMed] [Google Scholar]
- 21.Freeth D, Hammick M, Koppel I, Reeves S, Barr H. A Critical Review of Evaluations of Interprofessional Education. Higher Education Academy Learning and Teaching Support Network. Available at http://repos.hsap.kcl.ac.uk/content/m10123/latest/occp2.pdf (last accessed 28 March 2012) [PubMed]
- 22.Franson KL, Dubois EA, de Kam ML, Cohen AF. Measuring learning from the TRC pharmacology E-Learning program. Br J Clin Pharmacol. 2008;66:135–41. doi: 10.1111/j.1365-2125.2008.03167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubois E, Franson K, Bolk J, Cohen A. The impact of pre-clinical pharmacology and pharmacotherapy training on students' abilities and perceptions during clinical rotations. Med Teach. 2007;29:981–3. doi: 10.1080/01421590701663303. [DOI] [PubMed] [Google Scholar]
- 24.Sauer BL. Student-directed learning in a community geriatrics advanced pharmacy practice experience. Am J Pharm Educ. 2006;70:54. doi: 10.5688/aj700354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Linnebur SA, O'Connell MB, Wessell AM, McCord AD, Kennedy DH, DeMaagd G, Dent LA, Splinter MY, Biery JC, Jr, Chang F, Jackson RC, Miller SL, Sterling T ACCP Task Force. Pharmacy practice, research, education, and advocacy for older adults. Pharmacotherapy. 2005;25:1396–430. doi: 10.1592/phco.2005.25.10.1396. [DOI] [PubMed] [Google Scholar]
- 26.Herndon CM, Jackson K, II, Fike DS, Woods T. End-of-life care education in United States pharmacy schools. Am J Hosp Palliat Care. 2003;20:340–4. doi: 10.1177/104990910302000507. [DOI] [PubMed] [Google Scholar]
- 27.Dutta AP, Daftary MN, Oke F, Mims B, Hailemeskel B, Sansgiry SS. Geriatric education in US schools of pharmacy: a snapshot. Consult Pharm. 2005;20:45–52. doi: 10.4140/tcp.n.2005.45. [DOI] [PubMed] [Google Scholar]
- 28.Bloom MZ. How teaching students about geriatric pharmacy can help patients – and you. Consult Pharm. 2005;20:16–21. doi: 10.4140/tcp.n.2005.16. 25–8. [DOI] [PubMed] [Google Scholar]
- 29.Dawson GD. Geriatric-care education and training: pharmacy education and state home care association surveys. Gerontol Geriatr Educ. 2000;20:51–71. [Google Scholar]
- 30.Morris NS, Possidente CJ, Muskus C. Implementation of curriculum guidelines for pharmacology and pharmacotherapeutics in FNP graduate programs: a national survey. Clin Excell Nurse Pract. 2001;5:37–43. [PubMed] [Google Scholar]
- 31.Midlöv P, Bondesson A, Eriksson T, Nerbrand C, Höglund P. Effects of educational outreach visits on prescribing of benzodiazepines and antipsychotic drugs to elderly patients in primary health care in southern Sweden. Fam Pract. 2006;23:60–4. doi: 10.1093/fampra/cmi105. [DOI] [PubMed] [Google Scholar]
- 32.Pimlott NJ, Hux JE, Wilson LM, Kahan M, Li C, Rosser WW. Educating physicians to reduce benzodiazepine use by elderly patients: a randomized controlled trial. CMAJ. 2003;168:835–9. [PMC free article] [PubMed] [Google Scholar]
- 33.Naughton BJ, Singh R, Wisniewski AM, Singh G, Anderson DR. Improving quality of NSAID prescribing by internal medicine trainees with an educational intervention. Teach Learn Med. 2010;22:287–92. doi: 10.1080/10401334.2010.512547. [DOI] [PubMed] [Google Scholar]
- 34.Baum S, Harder S. Appropriate dosing in patients with impaired renal function on medical wards before and after an educational intervention. Int J Clin Pharmacol Ther. 2010;48:29–35. doi: 10.5414/cpp48029. [DOI] [PubMed] [Google Scholar]
- 35.Demirkan K, Celiker A, Yilmaz D, Sancar M, Apikoglu Rabus S, Izzettin FV, Sahin F. Improvement in pharmacists' knowledge through professional inservice education programs. Fabad J Pharm Sci. 2004;29:117–20. [Google Scholar]
- 36.Harden RM, Grant J, Buckley G, Hart IR. Best Evidence Medical Education. Adv Health Sci Educ Theory Pract. 2000;5:71–90. doi: 10.1023/A:1009896431203. [DOI] [PubMed] [Google Scholar]
- 37.Ballentine NH. Polypharmacy in the elderly: maximizing benefit, minimizing harm. Crit Care Nurs Q. 2008;31:40–5. doi: 10.1097/01.CNQ.0000306395.86905.8b. [DOI] [PubMed] [Google Scholar]
- 38.Bednash G, Mezey M, Tagliareni E. The Hartford Geriatric Nursing Initiative experience in geriatric nursing education: looking back, looking forward. Nurs Outlook. 2011;59:228–35. doi: 10.1016/j.outlook.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 39.Keller I, Makipaa A, Kalenscher T, Kalache A. Global Survey on Geriatrics in the Medical Curriculum. World Health Organization. Available at http://www.who.int/ageing/publications/alc_tegeme_survey.pdf (last accessed 1 December 2011)
- 40.Zaal RJ, van Doormaal JE, Lenderink AW, Mol PG, Kosterink JG, Egberts TC, Haaijer-Ruskamp FM, van den Bemt PM. Comparison of potential risk factors for medication errors with and without patient harm. Pharmacoepidemiol Drug Saf. 2010;19:825–33. doi: 10.1002/pds.1977. [DOI] [PubMed] [Google Scholar]
- 41.van den Bemt PM, Egberts TC, de Jong-van den Berg LT, Brouwers JR. Drug-related problems in hospitalised patients. Drug Saf. 2000;22:321–33. doi: 10.2165/00002018-200022040-00005. [DOI] [PubMed] [Google Scholar]
- 42.Odegard PS, Breslow RM, Koronkowski MJ, Williams BR, Hudgins GA. Geriatric pharmacy education: a strategic plan for the future. Am J Pharm Educ. 2007;71:47. doi: 10.5688/aj710347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Raman M, McLaughlin K, Violato C, Rostom A, Allard JP, Coderre S. Teaching in small portions dispersed over time enhances long-term knowledge retention. Med Teach. 2010;32:250–5. doi: 10.3109/01421590903197019. [DOI] [PubMed] [Google Scholar]
- 44.Wijnen-Meijer M, ten Cate OT, van der Schaaf M, Borleffs JC. Vertical integration in medical school: effect on the transition to postgraduate training. Med Educ. 2010;44:272–9. doi: 10.1111/j.1365-2923.2009.03571.x. [DOI] [PubMed] [Google Scholar]
- 45.Harden RM, Davis MH, Crosby JR. The new Dundee medical curriculum: a whole that is greater than the sum of the parts. Med Educ. 1997;31:264–71. doi: 10.1111/j.1365-2923.1997.tb02923.x. [DOI] [PubMed] [Google Scholar]
- 46.Schwartz A, Weiner SJ, Harris IB, Binns-Calvey A. An educational intervention for contextualizing patient care and medical students' abilities to probe for contextual issues in simulated patients. JAMA. 2010;304:1191–7. doi: 10.1001/jama.2010.1297. [DOI] [PubMed] [Google Scholar]
- 47.Richir MC, Tichelaar J, Geijteman EC, de Vries TP. Teaching clinical pharmacology and therapeutics with an emphasis on the therapeutic reasoning of undergraduate medical students. Eur J Clin Pharmacol. 2008;64:217–24. doi: 10.1007/s00228-007-0432-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Regehr G. It's NOT rocket science: rethinking our metaphors for research in health professions education. Med Educ. 2010;44:31–9. doi: 10.1111/j.1365-2923.2009.03418.x. [DOI] [PubMed] [Google Scholar]
- 49.De Vries TP. Presenting clinical pharmacology and therapeutics: general introduction. Br J Clin Pharmacol. 1993;35:577–9. doi: 10.1111/j.1365-2125.1993.tb04184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tichelaar J, Richir MC, Avis HJ, Scholten HJ, Antonini NF, De Vries TP. Do medical students copy the drug treatment choices of their teachers or do they think for themselves? Eur J Clin Pharmacol. 2010;66:407–12. doi: 10.1007/s00228-009-0743-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dean B, Schachter M, Vincent C, Barber N. Prescribing errors in hospital inpatients: their incidence and clinical significance. Qual Saf Health Care. 2002;11:340–4. doi: 10.1136/qhc.11.4.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Estus EL, Hume AL, Owens NJ. An active-learning course model to teach pharmacotherapy in geriatrics. Am J Pharm Educ. 2010;74:38. doi: 10.5688/aj740338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Estus EL. Using facebook within a geriatric pharmacotherapy course. Am J Pharm Educ. 2010;74:145. doi: 10.5688/aj7408145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jaehde U. Training in clinical pharmacy at the Universitiy of Bonn – the first steps towards the patient. Krankenhauspharmazie. 2009;30:205–8. [Google Scholar]
- 55.Divine HS, Cain J. Assessing the effect of a polypharmacy medication adherence simulation project in a geriatrics course in a college of pharmacy. J Am Geriatr Soc. 2009;57:1487–91. doi: 10.1111/j.1532-5415.2009.02364.x. [DOI] [PubMed] [Google Scholar]
- 56.Ross LA, Crabtree BL, Theilman GD, Ross BS, Cleary JD, Byrd HJ. Implementation and refinement of a problem-based learning model: a ten-year experience. Am J Pharm Educ. 2007;71:17. doi: 10.5688/aj710117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lam A. Senior care clerkship: an innovative collaboration of pharmaceutical care and learning. Consult Pharm. 2005;20:55–60. doi: 10.4140/tcp.n.2005.55. [DOI] [PubMed] [Google Scholar]
- 58.Bratt AM. A large group hybrid lecture and problem-based learning approach to teach Central Nervous System Pharmacology within the third year of an integrated masters level pharmacy degree course. Pharm Educ. 2003;3:35–52. [Google Scholar]
- 59.Strohkirch AM, Jaehde U. The role of the teacher-practitioner in integrating pharmacy education and practice: a pilot project in Germany. Pharm Educ. 2003;3:67–71. [Google Scholar]
- 60.George CJ, Jacobs LG. Geriatrics medication management rounds: a novel approach to teaching rational prescribing with the use of the medication screening questionnaire. J Am Geriatr Soc. 2011;59:138–42. doi: 10.1111/j.1532-5415.2010.03231.x. [DOI] [PubMed] [Google Scholar]
- 61.Naritoku DK, Faingold CL. Development of a therapeutics curriculum to enhance knowledge of fourth-year medical students about clinical uses and adverse effects of drugs. Teach Learn Med. 2009;21:148–52. doi: 10.1080/10401330902791313. [DOI] [PubMed] [Google Scholar]
- 62.Smith A, Tasioulas T, Cockayne N, Misan G, Walker G, Quick G. Construction and evaluation of a web-based interactive prescribing curriculum for senior medical students. Br J Clin Pharmacol. 2006;62:653–9. doi: 10.1111/j.1365-2125.2006.02651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eroglu L, Uresin Y. A model of pharmacology education: the experience of Istanbul Medical Faculty. J Clin Pharmacol. 2003;43:237–42. doi: 10.1177/0091270003251116. [DOI] [PubMed] [Google Scholar]
- 64.Herzig S, Linke RM, Marxen B, Borner U, Antepohl W. Long-term follow up of factual knowledge after a single, randomised problem-based learning course. BMC Med Educ. 2003;3:3. doi: 10.1186/1472-6920-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Antepohl W, Herzig S. Problem-based learning versus lecture-based learning in a course of basic pharmacology: a controlled, randomized study. Med Educ. 1999;33:106–13. doi: 10.1046/j.1365-2923.1999.00289.x. [DOI] [PubMed] [Google Scholar]
- 66.Faingold CL, Dunaway GA. Teaching pharmacology within a multidisciplinary organ system-based medical curriculum. Naunyn Schmiedebergs Arch Pharmacol. 2002;366:18–25. doi: 10.1007/s00210-002-0565-7. [DOI] [PubMed] [Google Scholar]
- 67.Lathers CM, Smith CM. Development of innovative teaching materials: clinical pharmacology problem-solving (CPPS) units: comparison with patient-oriented problem-solving units and problem-based learning – a 10-year review. J Clin Pharmacol. 2002;42:477–91. doi: 10.1177/00912700222011535. [DOI] [PubMed] [Google Scholar]
- 68.Lim AG, Honey M. Integrated undergraduate nursing curriculum for pharmacology. Nurse Educ Pract. 2006;6:163–8. doi: 10.1016/j.nepr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 69.Leikola SN, Tuomainen L, Ovaskainen H, Peura S, Sevon-Vilkman N, Tanskanen P, Airaksinen MS. Continuing education course to attain collaborative comprehensive medication review competencies. Am J Pharm Educ. 2009;73:108. doi: 10.5688/aj7306108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Warshaw GA, Modawal A, Kues J, Moore I, Margolin G, Sehgal M, Mueller S, Cluxton R. Community physician education in geriatrics: applying the assessing care of vulnerable elders model with a multisite primary care group. J Am Geriatr Soc. 2010;58:1780–5. doi: 10.1111/j.1532-5415.2010.03029.x. [DOI] [PubMed] [Google Scholar]
- 71.Straand J, Fetveit A, Rognstad S, Gjelstad S, Brekke M, Dalen I. A cluster-randomized educational intervention to reduce inappropriate prescription patterns for elderly patients in general practice – the Prescription Peer Academic Detailing (Rx-PAD) study [ NCT00281450] BMC Health Serv Res. 2006;6:72. doi: 10.1186/1472-6963-6-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lutters M, Harbarth S, Janssens JP, Freudiger H, Herrmann F, Michel JP, Vogt N. Effect of a comprehensive, multidisciplinary, educational program on the use of antibiotics in a geriatric university hospital. J Am Geriatr Soc. 2004;52:112–6. doi: 10.1111/j.1532-5415.2004.52019.x. [DOI] [PubMed] [Google Scholar]
- 73.Montagnini M, Varkey B, Duthie E., Jr Palliative care education integrated into a geriatrics rotation for resident physicians. J Palliat Med. 2004;7:652–9. doi: 10.1089/jpm.2004.7.652. [DOI] [PubMed] [Google Scholar]
- 74.Meagher DJ. Impact of an educational workshop upon attitudes towards pharmacotherapy for delirium. Int Psychogeriatr. 2010;22:938–46. doi: 10.1017/S1041610210000475. [DOI] [PubMed] [Google Scholar]


