Abstract
Background
An emergency department thoracotomy (EDT) or an emergency thoracotomy (ET) in the operating theater are both beneficial in selected patients following thoracic penetrating injuries. Since outcome-descriptive European studies are lacking, the aim of this retrospective study was to evaluate ten years of experience at a Dutch level I trauma center.
Method
Data on patients who underwent an immediate thoracotomy after sustaining a penetrating thoracic injury between October 2000 and January 2011 were collected from the trauma registry and hospital files. Descriptive and univariate analyses were performed.
Results
Among 56 patients, 12 underwent an EDT and 44 an ET. Forty-six patients sustained one or multiple stab wounds, versus ten with one or multiple gunshot wounds. Patients who had undergone an EDT had a lower GCS (p < 0.001), lower pre-hospital RTS and hospital triage RTS (p < 0.001 and p = 0.009, respectively), and a lower SBP (p = 0.038). A witnessed loss of signs of life generally occurred in EDT patients and was accompanied by 100 % mortality. Survival following EDT was 25 %, which was significantly lower than in the ET group (75 %; p = 0.002). Survivors had lower ISS (p = 0.011), lower rates of pre-hospital (p = 0.031) and hospital (p = 0.003) hemodynamic instability, and a lower prevalence of concomitant abdominal injury (p = 0.002).
Conclusion
The overall survival rate in our study was 64 %. The outcome of immediate thoracotomy performed in this level I trauma center was similar to those obtained in high-incidence regions like the US and South Africa. This suggests that trauma units where immediate thoracotomies are not part of the daily routine can achieve similar results, if properly trained.
Keyword: Thoracic trauma
Introduction
Thoracic injuries represent one of the leading causes of death in all age groups, and account for 25–50 % of all traumatic injuries [1]. Thoracic trauma ranks third, after head and extremity trauma, among major accidents in the United States (US), and is responsible for approximately half of all traumatic deaths [2]. Most penetrating injuries of the chest can be managed nonoperatively or with minimally invasive techniques. A small but significant group of 10–15 % of patients with penetrating thoracic injuries require an immediate thoracotomy as part of their initial resuscitation. An immediate thoracotomy can be performed in the operating theater, herein referred to as an “emergency thoracotomy” (ET), or at the emergency department (ED), herein referred to as an “emergency department thoracotomy” (EDT). Survival rates after an immediate thoracotomy following penetrating thoracic trauma are usually reported to be around 9–12 % [3], but have been reported to be as high as 38 % [4]. Much effort has been devoted to identifying patients who are likely to benefit from an immediate thoracotomy [5–9]. Most of the experience of performing immediate thoracotomies has been gained in high-incidence regions like the US and South Africa [7, 8]. Although penetrating trauma accounts for only 5–10 % of all trauma in Europe, compared with 40–50 % in the US, the incidence rates of patients presenting to an ED in the Netherlands with penetrating injury has gradually increased over the past few years, by up to 8 % annually [10]. Despite this rise in incidence in the Netherlands and other European countries, there is a paucity of studies from Europe regarding the use and outcome of an immediate thoracotomy following penetrating thoracic trauma. Moreover, outcome-related physiologic parameters have only been validated in three studies [11–13], which makes it even more difficult to interpret and use these data in the European emergency situation [3].
Ten years ago, immediate thoracotomy in the management of life-threatening thoracic penetrating injury was embedded in our level I trauma center. Since the experience of performing immediate thoracotomies in Europe is limited compared with the US and South Africa [14, 15], the aim of this study was to evaluate our ten years of experience with immediate thoracotomy and to describe the practices and outcomes of penetrating thoracic trauma.
Methods
Study setting
This study was performed at a level I trauma center in the southwestern part of the Netherlands. This 1300+ bed university medical center serves a population of 4.9 million. Patients who have sustained penetrating chest injuries in our adherence area are announced by pre-hospital care providers (either ambulance or helicopter emergency medical services), after which a trauma team is assembled (available 24/7). The team consists of a trauma surgeon (head of the trauma team), a surgical resident, an anesthesiologist, an emergency physician, two emergency nurses, and a radiologist. Blood products and surgical equipment for either thoracotomy or sternotomy are available in the resuscitation room. In case of a resuscitative EDT, both the thoracic surgeon and the operating theater facilities are notified for subsequent definitive care. In hemodynamically stable patients, computed tomographic angiography (CTA) is readily available opposite to the resuscitation room if required.
Patient selection
Patients who underwent an immediate thoracotomy after sustaining penetrating thoracic injury between October 2000 and January 2011 were selected from the trauma registry. An immediate thoracotomy was defined as a thoracotomy required as an integral part of the initial resuscitation of the trauma patient in the ED, or for imminent surgical repair of the injuries in the operating theater [16]. Both ET and EDT were included. An ET was performed in resuscitation-responsive patients (systolic blood pressure (SBP) ≥60 mmHg), versus an EDT in resuscitation-unresponsive or transient patients with a SBP <60 mmHg. Both thoracotomies allow the evacuation of pericardial tamponade, direct control of intrathoracic hemorrhage, control of massive air embolism, open cardiac massage, and cross-clamping of the descending aorta to redistribute blood flow and limit subdiaphragmatic hemorrhage [17, 18]. Patients who had only undergone an elective thoracotomy were excluded. An elective thoracotomy was defined as a procedure to correct nonacute life-threatening thoracic injury or postinjury complications such as empyema. Patients receiving a thoracotomy after blunt thoracic trauma or after a nontraumatic thoracic injury (indicated when massive intrathoracic or abdominal bleeding occurs) were also excluded.
Intervention
Advanced trauma life support (ATLS) guidelines were used for initial assessment and treatment [19]. Patients who sustained penetrating thoracic injuries were managed as shown in Fig. 1. Indications for an EDT and an ET are shown in Fig. 2. Indications for an EDT included (1) loss of signs of life (SOL) on arrival at the ED but presence of SOL at the scene of injury, and (2) failure to respond to resuscitation with a SBP <60 mmHg. Pericardial tamponade only represented an indication for an EDT when accompanied with an associated SBP <60 mmHg. ET indications included (1) a hemothorax on chest X-ray (CXR) with an initial chest tube output of >1,500 mL or an ongoining chest tube output of >200 mL/h for 2–4 h after insertion of the tube, (2) a hemothorax on CXR with a chest tube output of <1,500 mL, but with CTA of the chest findings prompting surgical intervention (e.g., gross contrast extravasation or air leakage), (3) signs of pericardial tamponade, or (4) a massive air embolism [19]. Operative maneuvers performed during a thoracotomy and/or a laparotomy are shown in Table 2. Table 2 shows the operative findings following a thoracotomy and/or an additional laparotomy.
Fig. 1.
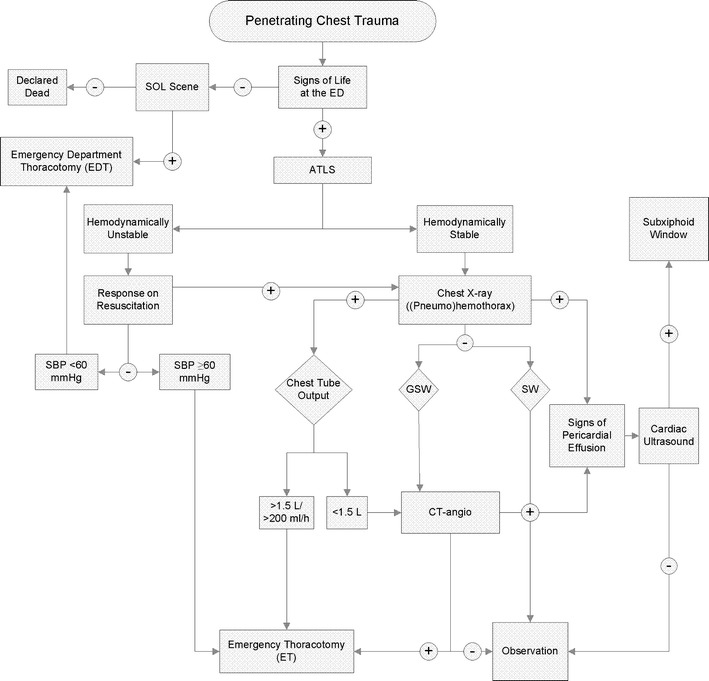
Flowchart with decision-making pathway for an immediate thoracotomy after penetrating chest trauma. ATLS advanced trauma life support, ED emergency department, SOL signs of life, SBP systolic blood pressure, GSW gunshot wound, SW stab wound, CT-angio computed tomography angiography. A hemodynamically unstable condition was defined as a SBP <100 mmHg with or without a response to resuscitation. A hemodynamically stable condition was defined as an SBP of ≥100 mmHg
Fig. 2.
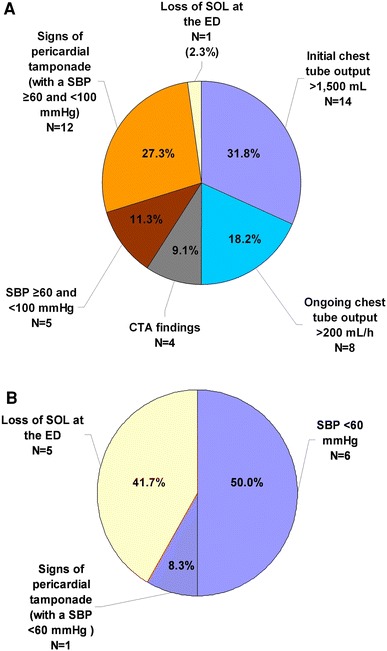
Indications for performing an ET (a) or an EDT (b). SOL signs of life, ED emergency department. Persisting shock was defined as a systolic blood pressure of ≥60 and <100 mmHg and no response to resuscitation or a transient response. Severe shock was defined as a systolic blood pressure of <60 mmHg and no response to resuscitation or a transient response. CTA findings included gross contrast extravasation, a hemothorax, or air leakage
Table 2.
Operative findings (A) and maneuvers (B) during EDT versus ET
| Overall (n = 56) | EDT (n = 12) | ET (n = 44) | p value | |
|---|---|---|---|---|
| (A) Operative findings (per patient) | ||||
| Hemothorax | 41 (73) | 6 (50) | 35 (80) | 0.039a |
| Lung injury | 27 (48) | 4 (33) | 23 (52) | 0.334b |
| Cardiac injury | 28 (50) | 7 (58) | 21 (48) | 0.746b |
| Diaphragm perforation | 6 (11) | 0 (0) | 6 (14) | 0.359a |
| Transection of intrathoracic vessels | 8 (14) | 4 (33) | 9 (20) | 0.055b |
| (B) Operative maneuvers (per patient) | ||||
| Control of intrathoracic hemorrhage | 47 (84) | 9 (75) | 38 (86) | 0.385b |
| Release of pericardial tamponade | 16 (29) | 4 (33) | 12 (27) | 0.726b |
| Internal cardiac massage | 13 (23) | 7 (58) | 6 (14) | <0.001b |
| Pneumectomy | 3 (5) | 0 (0) | 3 (7) | 0.512b |
| Pulmonary hilar twist or clamp | 2 (4) | 2 (17) | 0 (0) | 0.043b |
| Wedge resection | 2 (2) | 0 (0) | 2 (5) | N.S.b |
| Aortic cross-clamping | 1 (2) | 1 (8) | 0 (0) | 0.214b |
Data are shown as numbers with the corresponding percentages between parentheses, and were analyzed using the a Chi-squared test or b Fisher’s exact test
Data collection
Data on patient characteristics, injury characteristics, physiological parameters, and outcome were prospectively collected in and retrieved from our trauma registry and the patient hospital files. Data collected included age, gender, mechanism of injury, SOL, Glasgow coma scale (GCS score), injury severity score (ISS) [20], triage revised trauma score (triage RTS) [21], SBP, the need for cardiopulmonary resuscitation (CPR), transportation time, indications for thoracotomy, operative maneuvers, intraoperative findings, and complications. The length of hospital stay (H-LOS) was categorized as <24 or >24 h. Presence of SOL was defined by at the presence of at least one of the following: GCS >3, respiratory effort, cardiac activity on ECG or ultrasound (with or without a pulse), or evidence of pupillary reflexes. ISS was scored according to the abbreviated injury scale (AIS-90) [22]. CPR was performed according to the guidelines for resuscitation of the European Resuscitation Council (2005) [23].
Data analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) v.16.0 (SPSS, Chicago, IL, USA). Continuous data were tested for normality with the Shapiro–Wilk and Kolmogorov–Smirnov tests, and by inspecting the frequency distributions (histograms). Homogeneity of variance was checked for using Levene’s test. Since most of the continuous data were skewed, all data were analyzed using a nonparametric Mann–Whitney U test. Categorical data were compared using Fisher’s exact test or a chi-squared test: in small samples, or if the assumptions of the chi-squared test were not met, Fisher’s exact test was performed. P values of <0.05 were considered statistically significant.
Results
Over a ten-year period, a total of 416 patients with penetrating thoracic injury were referred to the ED; 72 presented with one or more gunshot wounds, and 344 with one or more stab wounds. Among all 416 patients, 346 patients presented only with thoracic trauma, while 70 patients presented with both thoracic and abdominal trauma. An intervention was indicated in 127 of 416 patients, including 39 thoracotomies, 32 laparotomies, and 17 patients who underwent both a thoracotomy and a laparotomy. The remaining 39 patients underwent other operative interventions. Among all 56 patients who underwent an immediate thoracotomy, 46 patients sustained a stab wound and 10 patients a gunshot wound. The male to female ratio was 6:1, and the median age was 32 years (P 25–P 75 25–41 years).
Among the 56 patients included in this study, 12 underwent an EDT and 44 an ET. Demographic and physiological data on these patients are shown in Table 1. In terms of the mechanism of injury, more gunshot wounds were found in the EDT group than in the ET group (p = 0.028). Overall, stab wounds dominated in both groups. Patients in the EDT group had a lower pre-hospital GCS (p < 0.001), lower pre-hospital RTS and hospital triage RTS (p < 0.001 and p = 0.009, respectively), and a lower hospital SBP (p = 0.038) than patients in the ET group. ISS, however, was similar in both groups.
Table 1.
Patient characteristics of the study population in whom immediate thoracotomy was performed in the ED (EDT) or in the operating theater (ET)
| Parameter | Overall (n = 56) | EDT (n = 12) | ET (n = 44) | p value |
|---|---|---|---|---|
| Pre-hospital | ||||
| Age (years)a | 32 (25–41) | 28 (24–41) | 33 (25–41) | 0.555c |
| Gender (men)b | 48 (86) | 10 (83) | 38 (86) | N.S.c |
| Stab woundsb | 46 (82) | 7 (58) | 39 (89) | 0.028d |
| Signs of lifeb | 55 (98) | 12 (100) | 43 (98) | N.S.c |
| Glasgow coma scorea | 14 (3–15) | 3 (3–10) | 14 (12–15) | <0.001c |
| Systolic blood pressure (mmHg)a | 98 (60–114) | 0 (0–110) | 100 (80–120) | 0.0140c |
| Revised trauma scorea | 11.00 (7.00–12.00) | 4.50 (4.00–7.00) | 12.00 (8.50–12.00) | <0.001c |
| Closed-chest cardiopulmonary resuscitationa | 6 (11) | 0 (0) | 6 (14) | N.S.e |
| In-hospital | ||||
| Time until ED arrival (min)a | 24 (15–32) | 13 (2–23) | 33 (18–35) | 0.006c |
| Time until thoracotomy (min)a | 68 (42–128) | 25 (15–107) | 79 (52–155) | 0.037c |
| Cardiopulmonary resuscitationb | 17 (30) | 9 (75) | 8 (18) | <0.001d |
| Signs of lifeb | 50 (89) | 7 (58) | 43 (98) | 0.001c |
| Systolic blood pressure (mmHg)a | 105 (69–120) | 0 (0–113) | 107 (80–126) | 0.038c |
| Injury severity scorea | 25 (16–34) | 34 (17–36) | 20 (15–34) | N.S.c |
| Triage-revised trauma scorea | 8 (4–8) | 4 (1–8) | 8 (5–8) | 0.009c |
| H-Los (days)a | 7 (0–12) | 0 (0–5) | 8 (5–14) | 0.005c |
| IC-LOS (days)a | 1 (0–3) | 0 (0–2) | 1 (1–3) | 0.012c |
a Data are displayed as the median, with the first and third quartiles given in parentheses
b Patient numbers are displayed, followed by the corresponding percentages in parentheses
c Mann–Whitney U test, d Fisher’s exact test, e Chi-squared test
H-LOS hospital length of stay, IC-LOS duration of stay at the intensive care unit
Cardiopulmonary resuscitation was performed in 19 patients, of which six received pre-hospital closed chest cardiopulmonary resuscitation (CC-CPR). All six patients who received pre-hospital CC-CPR, with or without additional in-hospital CPR, progressed to an ET. Of these six patients, five received an EDT before they were transported to the operation room for an EDT. The majority of the patients receiving in-hospital CPR underwent an EDT (p < 0.001). The median time interval from the arrival of emergency medical services at the scene of injury until admittance to the ED was shorter in the EDT group (13 min; P 25–P 75 2–23) than in the ET group (33 min; P 25–P 75 18–35; p = 0.006). The median time span from injury scene to thoracotomy was also shorter in the EDT group (25 min; P 25–P 75 15–107) than in the ET group (79 min; P 25–P 75 52–155; p = 0.037; Table 1).
Among all 56 immediate thoracotomies, ten were performed within 1 h after injury, 14 within 1–3 h, and six within 4–10 h. The transportation times of 26 patients could not be obtained. The indications for an ET are presented in Fig. 2a, and the indications for an EDT are shown in Fig. 2b. Indications are in agreement with the flowchart in Fig. 1.
A total of 64 incisions were performed: 22 midsternal incisions, 20 left anterolateral, ten right anterolateral, two left posterolateral, six right posterolateral, and four clamshell. Operative findings and maneuvers for EDT and ET are shown in Table 2. Hemothorax was found significantly more often in the ET group. Internal cardiac massage and pulmonary hilar twist were performed more frequently in the EDT group (p < 0.001 and p = 0.043, respectively). Abdominal trauma was found in ten of all 17 patients undergoing an additional laparotomy, and was not observed more often in either the ET or the EDT group (p = 0.433). The most common intra-abdominal findings were damage to the diaphragm and the liver.
In the survivors, postoperative complications occurred in 20 patients, of whom five experienced one or more complications (Table 3). Complications ranged from superficial wound infection to re-bleeding in six patients.
Table 3.
Complications following EDT and ET
| Complications | Overall (n = 56) | EDT (n = 12) | ET (n = 44) |
|---|---|---|---|
| Mortality | 20 (36) | 9 (75) | 11 (25) |
| Re-bleeding | 6 (11) | 1 (8) | 6 (14) |
| Acute respiratory distress syndrome | 2 (4) | 1 (8) | 1 (2) |
| Superficial wound infection | 1 (2) | 0 (0) | 1 (2) |
| Abscess | 2 (4) | 0 (0) | 2 (5) |
| Pneumonia | 3 (5) | 1 (8) | 2 (5) |
| Empyema | 2 (4) | 0 (0) | 2 (5) |
| Sepsis | 1 (2) | 0 (0) | 1 (2) |
| Rhabdomyolysis | 2 (4) | 1 (8) | 1 (2) |
| Neurological impairment | 2 (4) | 0 (0) | 2 (5) |
| Re-operation | 9 (16) | 1 (8) | 8 (18) |
Data are shown as numbers with the corresponding percentages between parentheses
Complications other than mortality are shown for survivors only
Re-operation was performed in nine patients and included two laparotomies and seven re-thoracotomies. Among this latter group, two patients underwent an elective thoracotomy and five a re-thoracotomy due to persistent thoracic blood loss. Operative findings following persistent thoracic blood loss included progressive rupture of the cardiac apex despite the placement of several cardiac sutures 2 h earlier, continuous bleeding of intercostal vessels, laceration of the aortic arch, bleeding of the subclavian artery, and a negative re-thoracotomy in one patient. The overall survival of patients was 64 %: 25 % in the EDT group and 75 % in the ET group (Table 4). In the EDT group, five out of 12 patients (42 %) advanced to definitive surgical care. The three patients who survived an EDT left the hospital without neurological impairment. Among all 44 patients in the ET group, 33 (75 %) survived until discharge, of whom 31 (94 %) were neurologically intact.
Table 4.
Factors associated with mortality after an immediate thoracotomy
| Factors | Total (n = 56) | Nonsurvivors (n = 20) | Survivors (n = 36) | p value |
|---|---|---|---|---|
| Pre-hospital | ||||
| Signs of lifeb | 55 (98) | 19 (95) | 36 (100) | 0.357d |
| Pupillary responseb | 45 (80) | 11 (55) | 34 (94) | 0.002e |
| Triage-revised trauma scorea | 11 (7–12) | 8 (4–11) | 12 (10–12) | 0.001c |
| Glasgow coma scalea | 14 (3–15) | 3 (3–13) | 15 (13–15) | <0.001c |
| Systolic blood pressure (mmHg)a | 98 (60–114) | 68 (0–109) | 101 (80–127) | 0.009c |
| Hemodynamic unstableb | 29 (52) | 15 (75) | 14 (39) | 0.031e |
| Gunshot woundb | 10 (17) | 6 (30) | 4 (11) | 0.142d |
| Abdominal injuryb | 10 (18) | 8 (40) | 2 (6) | 0.002d |
| In-hospital | ||||
| Injury severity scorea | 25 (16–34) | 34 (17–45) | 20 (12–30) | 0.011c |
| Triage-revised trauma scorea | 8 (4–8) | 4 (1–8) | 8 (6–8) | 0.008c |
| Systolic blood pressure (mmHg)a | 105 (69–120) | 70 (0–108) | 110 (91–130) | 0.003c |
| Signs of lifeb | 50 (89) | 14 (70) | 36 (100) | 0.001d |
| CPRb | 17 (30) | 15 (75) | 2 (6) | <0.001d |
| EDTb | 12 (21) | 9 (45) | 3 (8) | 0.002d |
| Transection of intrathoracic vesselsb | 8 (14) | 6 (30) | 2 (6) | 0.019d |
| Thoracotomy indications | 0.003e | |||
| Pericardial tamponadeb (with associated shock) | 13 (23) | 2 (10) | 11 (31) | |
| Ongoing chest tube production >200 mL/hb | 8 (14) | 1 (5) | 7 (19) | |
| Hemodynamically unstable conditionb | 11 (20) | 7 (35) | 4 (11) | |
| Absence of signs of lifeb | 5 (9) | 5 (25) | 0 (0) | |
aData are displayed as the median, with the first and third quartiles given within parentheses
bPatient numbers are displayed, with the percentages given within parentheses
Data were analyzed using c The Mann–Whitney U test, d Fisher’s exact test, e The chi-squared test
ED emergency department, CPR cardiopulmonary resuscitation, EDT emergency department thoracotomy. A pre-hospital hemodynamically unstable condition was defined as an SBP of <100 mmHg or no response to resuscitation. A hemodynamically unstable condition as an indication for thoracotomy was defined as an SBP of <60 mmHg or no response to resuscitation
The physiological conditions of the patients in relation to survival are shown in Table 4. Patients who survived had a lower ISS (p = 0.011) and lower rates of pre-hospital and hospital hemodynamic instability (p = 0.031 and p = 0.003, respectively). Fifty-five of the 56 patients who underwent an immediate thoracotomy had obtainable SOL after injury; 50 of the 55 still had SOL at the ED. One patient who lost SOL at the ED did not receive resuscitative interventions at the ED, but underwent an ET instead of an EDT. All six patients who lost SOL died. Patients who died had a higher prevalence of concomitant abdominal injury (Table 4). The finding of peritoneal and retroperitoneal fluid during the operation, suggesting the existence of additional abdominal trauma, also coincided with a higher mortality rate (p = 0.009 and p = 0.036, respectively). Conclusively, patients who died showed a higher rate of transected aorta or vena cava (p = 0.018). Suspected pericardial tamponade, on the other hand, had a more favorable outcome (p = 0.003).
Discussion
Nowadays, an EDT or an ET is performed in emergency situations following life-threatening thoracic—especially penetrating—trauma [8, 24, 25]. Guidelines for the treatment of thoracic injuries were established after World War II, and were derived originally from military experience [16]. In 2001, the National Association of Emergency Physicians and the American College of Surgeons composed a series of guidelines [3]. An EDT is recommended in patients who have sustained penetrating thoracic (cardiac) injuries and arrive at the trauma center after short on-scene and transportation times with witnessed or objectively measured SOL. However, physiological predictors of outcome, definitions of SOL, and the method used to identify patients in whom an immediate thoracotomy can be life-saving remain subjects for debate [3, 8, 14, 26–29]. Furthermore, outcome data from high-incidence regions like the US and South Africa may not be generalizable to the European population. Therefore, in this article, we have described our ten years of experience with immediate thoracotomies in a European level I trauma center.
The survival rate after an EDT published by the American College of Surgeons Committee on Trauma (ACSCOT) was only 11.2 %, among whom approximately 15 % survived with neurological impairment [3]. In our cohort, three out of 12 patients survived until discharge following an EDT; all were discharged without neurological impairment. Our survival rates compare favorably to other European studies in which mortality rates after EDT or ET of up to 100 % were found [15]. The most promising European experience so far has been the Glasgow series [30], with a 32 % survival rate (i.e., eight out of 25 patients survived) following immediate thoracotomy. Our overall survival rate of 64 % (36 out of 56 patients) is twice as high. The survival rate in the Glasgow series following an EDT was 6 %, which is much lower than the observed survival rate of 25 % in our level I trauma center. In order to determine if our favorable outcomes could be partly caused by overtreatment, preoperative indications were compared with the operative findings. When analyzing the EDTs, it seemed that the three patients who survived an EDT initially manifested with radiographic signs of a large hemothorax, shock, and signs of a pericardial-tamponade-like pericardial effusion on ultrasound or CTA. Consecutive operative findings were: laceration of the lung parenchyma, myocardial rupture, and laceration of the lung parenchyma. All patients were in severe shock (i.e., SBP <60 mmHg) and unresponsive to resuscitation. These patients could not have been transported to the OR for surgical treatment, and thus underwent an EDT. The abovementioned findings suggest that the decision to perform an EDT in these cases was adequate. Moreover, indications were in accordance with the ATLS and ERC guidelines [19, 31]. Based on our study findings, we are confident that the standard of care in combination with the developed treatment algorithm as shown in Fig. 1 allows us to achieve a relatively favorable outcome. Nevertheless, deciding on whether or not to perform an immediate thoracotomy remains a challenge.
Several indications, including specific physical parameters, were proven to be associated with a favorable outcome [3, 5, 14, 17, 19, 32, 33]. In our study, certain indications such as the presence of SOL, suspected traumatic pericardial tamponade, or the presence of concomitant abdominal injury were found to have a significant influence on the outcome after EDT or ET.
Loss of SOL is an important variable describing a patient’s physical condition that presented more often in the patients who died. Nevertheless, controversy exists over when and which SOL are related to a better outcome [34]. An immediate thoracotomy is believed to be beneficial in patients who arrive with vital signs at the ED or in those with a witnessed loss of SOL, not in those who are already showing no SOL before the (helicopter) emergency medical services have arrived at the scene of injury [3]. In our cohort, obtainable SOL were present in all 36 survivors. Survivors, however, did not show all possible SOL; two lost their pupillary response after injury, one suffered a prehospital asystole that persisted until arrival at the ED, and one showed a loss of SOL during the EDT. Seamon et al. reported similar findings and suggested that EDT can have a favorable outcome as long as one or more SOL are present at the scene of injury. Moreover, the moment in time when the SOL were observed seemed to affect the outcome [32]. All five patients who demonstrated recordable SOL at the incident scene but lost all SOL at or during transportation to the ED died in our study. Several authors support the theory that a witnessed loss of SOL is one of the indications to perform an immediate thoracotomy [3, 35]; however, our data proved that a poor outcome followed a witnessed loss of SOL. Considering this outcome, it was noted by Hall et al. that current recommendations to perform an immediate thoracotomy might be a little optimistic. They proposed that they are mainly based on the outcomes of the more specialized and experienced institutions, where immediate thoracotomies are performed more routinely [35]. Another option for improving the survival of patients with a witnessed loss of SOL might be a pre-hospital thoracotomy following the indications mentioned by Coats et al. [36]. Altogether, loss of SOL as an indication for an immediate thoracotomy deserves extra observation in the future, focusing in particular on low-incidence regions. Concomitant abdominal injury was found to be more prominent among the patients who died, which is in agreement with several studies from high-incidence regions [5, 6, 37, 38]. Mortality rates in our study were higher in patients receiving both a thoracotomy and a laparotomy. Negative laparotomy rates of up of 30 % were seen in cases with thoracoabdominal injuries [39, 40], with complication rates of 2.5–41 % [41]. Both findings reflect the importance of a reliable diagnostic approach for thoracoabdominal injuries. Further research in this area is desired, since most studies describe diagnostic imaging following blunt, not penetrating, trauma [42–45].
As for cardiac injury, the ACSCOT guidelines support the use of an EDT in hemodynamically unstable patients or patients with a witnessed loss of SOL in whom a pericardial tamponade is suspected. The ACSCOT guidelines also state that an EDT can be used as a diagnostic tool for discriminating cardiac from noncardiac thoracic injury [3]. In our center, clinical or CXR suspicion of pericardial tamponade (PT) is treated according to our algorithm (Fig. 1). Ultrasound-confirmed pericardial effusion (>8 mm) in patients with an SBP of <60 mmHg prompts immediate EDT. In patients with an SBP of >60 mmHg who undergo an ET for additional injuries, the pericardium is opened to assess the myocardium for injuries. In hemodynamically stable patients, the pericardium is inspected via the subxiphoid pericardial window (SPW) technique, as described by Arom et al. [46]. In cases with gross blood drainage from the pericardial sac, the procedure is converted into a sternotomy to treat the injuries to the heart. If only serosanguinolent fluid is encountered, a drain is placed in the pericardial sac until the output is less than 50 mL over 12 h, as advocated by Navsaria et al. [47]. In our cohort, patients with a suspected traumatic pericardial tamponade were more abundant among the survivors, suggesting a more favorable outcome [36, 48, 49]. Since outcome data from the high-incidence regions may not be generalizable to low-volume areas such as most European countries, further research from low-incidence regions is needed. Despite a lower occurrence of penetrating thoracic injuries, we were able to show that performing immediate thoracotomy in a level I trauma center in a lower-incidence region can produce similar outcomes to those seen in high-incidence regions. However, since immediate thoracotomies are not part of the daily routine of most trauma centers in these low-incidence regions, cooperation between different European hospitals could help to improve penetrating trauma research in the future. In addition, training programs in high-volume centers, in combination with recurrent surgical technique training on cadavers, may contribute to better outcomes.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Footnotes
O. J. F. Van Waes and P. A. Van Riet contributed equally to this work.
E. M. M. Van Lieshout and D. D. Hartog contributed equally to this work.
References
- 1.MacKenzie EJ. Epidemiology of injuries: current trends and future challenges. Epidemiol Rev. 2000;22(1):112–119. doi: 10.1093/oxfordjournals.epirev.a018006. [DOI] [PubMed] [Google Scholar]
- 2.LoCicero J, 3rd, Mattox KL. Epidemiology of chest trauma. Surg Clin North Am. 1989;69(1):15–19. doi: 10.1016/s0039-6109(16)44730-4. [DOI] [PubMed] [Google Scholar]
- 3.Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons Committee on Trauma. Practice management guidelines for emergency department thoracotomy. J Am Coll Surg. 2001;193(3):303–9. [DOI] [PubMed]
- 4.Baxter BT, Moore EE, Moore JB, Cleveland HC, McCroskey BL, Moore FA. Emergency department thoracotomy following injury: critical determinants for patient salvage. World J Surg. 1988;12(5):671–675. doi: 10.1007/BF01655882. [DOI] [PubMed] [Google Scholar]
- 5.Rhee PM, Acosta J, Bridgeman A, Wang D, Jordan M, Rich N. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190(3):288–298. doi: 10.1016/S1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 6.Karmy-Jones R, Nathens A, Jurkovich GJ, Shatz DV, Brundage S, Wall MJ, Jr, Engelhardt S, Hoyt DB, Holcroft J, Knudson MM, Michaels A, Long W. Urgent and emergent thoracotomy for penetrating chest trauma. J Trauma. 2004;56(3):664–668. doi: 10.1097/01.TA.0000068238.74552.4B. [DOI] [PubMed] [Google Scholar]
- 7.Miglietta MA, Robb TV, Eachempati SR, Porter BO, Cherry R, Brause J, Barie PS. Current opinion regarding indications for emergency department thoracotomy. J Trauma. 2001;51(4):670–676. doi: 10.1097/00005373-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Brown SE, Gomez GA, Jacobson LE, Scherer T 3rd, McMillan RA. Penetrating chest trauma: should indications for emergency room thoracotomy be limited? Am Surg. 1996;62(7):530–3. (discussion 533–534). [PubMed]
- 9.Durham LA, 3rd, Richardson RJ, Wall MJ, Jr, Pepe PE, Mattox KL. Emergency center thoracotomy: impact of prehospital resuscitation. J Trauma. 1992;32(6):775–779. doi: 10.1097/00005373-199206000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Bruinsma MY, Moors JA. Illegale vuurwapens. gebruik, bezit en handel in Nederland 2001–2003, IV A Beleidsonderzoek en advies & Ministerie van justitie/WODC, Tilburg en Den Haag; 2005.
- 11.Asensio JA, Hanpeter D, Demetriades D. The futility of the liberal utilization of emergency department thoracotomy. A prospective study. In: Proceedings of the american association for the surgery of trauma 58th annual meeting. Baltimore, Maryland; 1998.
- 12.Asensio JA, Murray J, Demetriades D, Berne J, Cornwell E, Velmahos G, Gomez H, Berne TV. Penetrating cardiac injuries: a prospective study of variables predicting outcomes. J Am Coll Surg. 1998;186(1):24–34. doi: 10.1016/S1072-7515(97)00144-0. [DOI] [PubMed] [Google Scholar]
- 13.Asensio JA, Berne JD, Demetriades D, Chan L, Murray J, Falabella A, Gomez H, Chahwan S, Velmahos G, Cornwell EE, Belzberg H, Shoemaker W, Berne TV. One hundred five penetrating cardiac injuries: a 2-year prospective evaluation. J Trauma. 1998;44(6):1073–1082. doi: 10.1097/00005373-199806000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Soreide K, Petrone P, Asensio JA. Emergency thoracotomy in trauma: rationale, risks, and realities. Scand J Surg. 2007;96(1):4–10. doi: 10.1177/145749690709600102. [DOI] [PubMed] [Google Scholar]
- 15.Soreide K, Soiland H, Lossius HM, Vetrhus M, Soreide JA, Soreide E. Resuscitative emergency thoracotomy in a Scandinavian trauma hospital—is it justified? Injury. 2007;38(1):34–42. doi: 10.1016/j.injury.2006.06.125. [DOI] [PubMed] [Google Scholar]
- 16.Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma—a review. Injury. 2006;37(1):1–19. [DOI] [PubMed]
- 17.Beall AC, Jr, Diethrich EB, Crawford HW, Cooley DA, De Bakey ME. Surgical management of penetrating cardiac injuries. Am J Surg. 1966;112(5):686–692. doi: 10.1016/0002-9610(66)90105-X. [DOI] [PubMed] [Google Scholar]
- 18.Grove CA, Lemmon G, Anderson G, McCarthy M. Emergency thoracotomy: appropriate use in the resuscitation of trauma patients. Am Surg. 2002;68(4):313–316. [PubMed] [Google Scholar]
- 19.Trauma ACoSCo. Advanced trauma life support for doctors. 8th ed. American College of Surgeons: Chicago; 2008.
- 20.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma. 1989;29(5):623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Garthe E, States JD, Mango NK. Abbreviated injury scale unification: the case for a unified injury system for global use. J Trauma. 1999;47(2):309–323. doi: 10.1097/00005373-199908000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005;67(Suppl 1):S7–S23. doi: 10.1016/j.resuscitation.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Gomez G, Fecher A, Joy T, Pardo I, Jacobson L, Kemp H. Optimizing outcomes in emergency room thoracotomy: a 20-year experience in an urban level I trauma center. Am Surg. 2010;76(4):406–10. [PubMed]
- 25.Brautigan MW. Patient selection in emergency thoracotomy. Resuscitation. 1991;22(1):103–108. doi: 10.1016/0300-9572(91)90069-B. [DOI] [PubMed] [Google Scholar]
- 26.Henderson VJ, Smith RS, Fry WR, Morabito D, Peskin GW, Barkan H, Organ CH., Jr Cardiac injuries: analysis of an unselected series of 251 cases. J Trauma. 1994;36(3):341–348. doi: 10.1097/00005373-199403000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Danne PD, Finelli F, Champion HR. Emergency bay thoracotomy. J Trauma. 1984;24(9):796–802. doi: 10.1097/00005373-198409000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Athanasiou T, Krasopoulos G, Nambiar P, Coats T, Petrou M, Magee P, Uppal R. Emergency thoracotomy in the pre-hospital setting: a procedure requiring clarification. Eur J Cardiothorac Surg. 2004;26(2):377–386. doi: 10.1016/j.ejcts.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 29.Cothren CC, Moore EE. Emergency department thoracotomy for the critically injured patient: objectives, indications, and outcomes. World J Emerg Surg. 2006;1:4. doi: 10.1186/1749-7922-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bleetman A, Kasem H, Crawford R. Review of emergency thoracotomy for chest injuries in patients attending a UK accident and emergency department. Injury. 1996;27(2):129–132. doi: 10.1016/0020-1383(95)00179-4. [DOI] [PubMed] [Google Scholar]
- 31.Onat S, Ulku R, Avci A, Ates G, Ozcelik C. Urgent thoracotomy for penetrating chest trauma: analysis of 158 patients of a single center. Injury. 2010;41(7):876–880. doi: 10.1016/j.injury.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Seamon MJ, Fisher CA, Gaughan JP, Kulp H, Dempsey DT, Goldberg AJ. Emergency department thoracotomy: survival of the least expected. World J Surg. 2008;32(4):604–612. doi: 10.1007/s00268-007-9392-9. [DOI] [PubMed] [Google Scholar]
- 33.Lorenz HP, Steinmetz B, Lieberman J, Schecoter WP, Macho JR. Emergency thoracotomy: survival correlates with physiologic status. J Trauma. 1992;32(6):780–785. doi: 10.1097/00005373-199206000-00020. [DOI] [PubMed] [Google Scholar]
- 34.Moore EE, Knudson MM, Burlew CC, Inaba K, Dicker RA, Biffl WL, Malhotra AK, Schreiber MA, Browder TD, Coimbra R, Gonzalez EA, Meredith JW, Livingston DH, Kaups KL. Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. J Trauma. 2011;70(2):334–9. [DOI] [PubMed]
- 35.Hall BL, Buchman TG. A visual, timeline-based display of evidence for emergency thoracotomy. J Trauma. 2005;59(3):773–777. [PubMed] [Google Scholar]
- 36.Coats TJ, Keogh S, Clark H, Neal M. Prehospital resuscitative thoracotomy for cardiac arrest after penetrating trauma: rationale and case series. J Trauma. 2001;50(4):670–673. doi: 10.1097/00005373-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 37.Mejia JC, Stewart RM, Cohn SM. Emergency department thoracotomy. Semin Thorac Cardiovasc Surg. 2008;20(1):13–18. doi: 10.1053/j.semtcvs.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 38.Morgan BS, Garner JP. Emergency thoracotomy—the indications, contraindications and evidence. J R Army Med Corps. 2009;155(2):87–93. doi: 10.1136/jramc-155-02-02. [DOI] [PubMed] [Google Scholar]
- 39.Soffer D, McKenney MG, Cohn S, Garcia-Roca R, Namias N, Schulman C, Lynn M, Lopez P. A prospective evaluation of ultrasonography for the diagnosis of penetrating torso injury. J Trauma. 2004;56(5):953–957. doi: 10.1097/01.TA.0000127806.39852.4E. [DOI] [PubMed] [Google Scholar]
- 40.van den Berg HR, Lere SG, Schipper IB, Patka P. Abdominal gunshot wounds: possibilities for selective conservative management. Ned Tijdschr Geneeskd. 2007;151(15):841–847. [PubMed] [Google Scholar]
- 41.de Vries CS, Africa M, Gebremariam FA, van Rensburg JJ, Otto SF, Potgieter HF. The imaging of stab injuries. Acta Radiol. 2010;51(1):92–106. doi: 10.3109/02841850903225198. [DOI] [PubMed] [Google Scholar]
- 42.Salera D, Argalia G, Giuseppetti GM. Screening US for blunt abdominal trauma: a retrospective study. Radiol Med. 2005;110(3):211–220. [PubMed] [Google Scholar]
- 43.Brown MA, Casola G, Sirlin CB, Patel NY, Hoyt DB. Blunt abdominal trauma: screening us in 2,693 patients. Radiology. 2001;218(2):352–358. doi: 10.1148/radiology.218.2.r01fe42352. [DOI] [PubMed] [Google Scholar]
- 44.Lingawi SS, Buckley AR. Focused abdominal US in patients with trauma. Radiology. 2000;217(2):426–429. doi: 10.1148/radiology.217.2.r00nv23426. [DOI] [PubMed] [Google Scholar]
- 45.Nural MS, Yardan T, Guven H, Baydin A, Bayrak IK, Kati C. Diagnostic value of ultrasonography in the evaluation of blunt abdominal trauma. Diagn Interv Radiol. 2005;11(1):41–44. [PubMed] [Google Scholar]
- 46.Arom KV, Richardson JD, Webb G, Grover FL, Trinkle JK. Subxiphoid pericardial window in patients with suspected traumatic pericardial tamponade. Ann Thorac Surg. 1977;23(6):545–549. doi: 10.1016/S0003-4975(10)63699-5. [DOI] [PubMed] [Google Scholar]
- 47.Navsaria PH, Nicol AJ. Haemopericardium in stable patients after penetrating injury: is subxiphoid pericardial window and drainage enough? A prospective study. Injury. 2005;36(6):745–750. doi: 10.1016/j.injury.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 48.Trunkey D. Initial treatment of patients with extensive trauma. N Engl J Med. 1991;324(18):1259–1263. doi: 10.1056/NEJM199105023241806. [DOI] [PubMed] [Google Scholar]
- 49.Molina EJ, Gaughan JP, Kulp H, McClurken JB, Goldberg AJ, Seamon MJ. Outcomes after emergency department thoracotomy for penetrating cardiac injuries: a new perspective. Interact Cardiovasc Thorac Surg. 2008;7(5):845–848. doi: 10.1510/icvts.2008.183293. [DOI] [PubMed] [Google Scholar]


