Abstract
Pressure ulcer in an otherwise sick patient is a matter of concern for the care givers as well as the medical personnel. A lot has been done to understand the disease process. So much so that USA and European countries have established advisory panels in their respective continents. Since the establishment of these organizations, the understanding of the pressure ulcer has improved significantly. The authors feel that the well documented and well publicized definition of pressure ulcer is somewhat lacking in the correct description of the disease process. Hence, a modified definition has been presented. This disease is here to stay. In the process of managing these ulcers the basic pathology needs to be understood well. Pressure ischemia is the main reason behind the occurrence of ulceration. Different extrinsic and intrinsic factors have been described in detail with review of literature. There are a large number of risk factors causing ulceration. The risk assessment scales have eluded the surgical literature and mostly remained in nursing books and websites. These scales have been reproduced for completion of the basics on decubitus ulcer. The classification of the pressure sores has been given in a comparative form to elucidate that most of the classifications are the same except for minor variations. The management of these ulcers is ever evolving but the age old saying of “prevention is better than cure” suits this condition the most.
KEY WORDS: Bed sore, decubitus ulcer, pressure ulcer, prevention, risk factors, ulcer
HISTORY
Pressure ulcers have been recognized as a disease entity since ages. Pressure sores have been found in Egyptian mummies, some of which are more than 5,000 years old. Egyptians used honey for the treatment of such ulcers and wounds.
In Persia, Avicenna used a variety of topical applicants on wounds. In Arabia, Maimonides recommended nutritional support to promote ulcer healing. A wide variety of topical remedies like honey, moldy bread, meat, animal and plant extracts, copper sulfate, zinc oxide and alum have been used in the past.[1]
Hippocrates (460-370 B.C) had described pressure ulcer in association with paraplegia with bladder and bowel dysfunction.[2] During the renaissance, Ambrose Paré, a 16th century French army barber-surgeon and founding father of medical surgical practice, wrote in his autobiography about a wounded French aristocrat developing a pressure ulcer. He mentioned cure with good nutrition, pain relief and debridement; which is no different than the present modality to some extent.[3]
In 19th century, Jean-Martin Charcot studied decubitus ulcers and subscribed to the “neurotrophic theory” for the causation of ulcer rather than the “pressure” as we believe today. Charcot directly related the occurrence of ulcer to the damage to central nervous system. ‘Decubitus ominosus’ was the term given to ulcer covered with eschar as it caused high mortality. Charcot described the decubitus ulcer in detail with its complications like ‘gangrenous pulmonary metastasis (infiltration)’ and spinal cord invasion. However, Brown-Sequard opposed this theory and proved that if the pressure is avoided in guinea pigs with spinal cord injury, the ulcer does not develop and the existing ulcer heals on relieving the pressure.[4] According to Ayurveda bed-sore is termed as “SayyajVrava”; ‘Sayyaj’ meaning bed and ‘vrava’ is ulcer or wound. Due to pressure ‘mamsadhatu’ (circulation) is affected and results in bedsore.
During the nineteenth century, discovery of bacteria by Pasteur, antisepsis by Lister and X-ray by Roentgen changed the understanding of these ulcers in general. The twentieth century brought in antibiotics which changed the scenario further. The later part of twentieth century witnessed studies on nutrition, trace elements, biomechanics and newer methods of management of these ulcers.
DEFINITIONS
Pressure ulcer is commonly termed as bed-sore, decubitus ulcer or pressure sore and sometimes as pressure necrosis or ischemic ulcer. The term pressure ulcer was popularized by the Agency for Healthcare Research and Quality. Pressure ulcer has been defined as “an area of unrelieved pressure usually over a bony prominence leading to ischemia, cell death and tissue necrosis”. This definition has been further refined by the National Pressure Ulcer Advisory Panel (NPUAP) and European Pressure Ulcer Advisory Panel (EPUAP) as “localized injury to the skin and/or underlying tissue usually over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction”.[5]
Both these definitions fall short of the complete description of pressure ulcer. So, we have proposed a modification of this definition. We define pressure ulcer as “an area of localized soft tissue ischemic necrosis caused by prolonged pressure higher than the capillary pressure with or without shear, related to posture which usually occurs over a bony prominence”.
PRESSURE ULCER ADVISORY PANELS
The National Pressure Ulcer Advisory Panel (NPUAP) is an independent American organization established in 1987. This non-profit organization deals with prevention, management and research on pressure ulcers. Similarly EPUAP was formed in December 1996 in London to support prevention and prepare guidelines for the management of pressure ulcer in all the European countries. Their mission statement reads as “to provide for the relief of persons suffering from or at risk of pressure ulcers, in particular through research and the education of the public.”
EPIDEMIOLOGY
Pressure ulcers have been described as one of the most costly and physically debilitating complications in the 20th century.[6] Pressure ulcers are the third most expensive disorder after cancer and cardiovascular diseases.
In Japanese Geriatric Health Services facility, the immobile geriatric patients represent 91% of total population with pressure ulcer in the Geriatric Health Service facility.[7]
The incidence of pressure ulcers is different in each clinical setting. Incidence rates of as low as 0.4% to as high as 38% have been reported in the inpatient department while prevalence has been reported as 3.5% to 69%.[8–11] In long term care facilities, the reported incidence is between 2.2% to 23.9% while in home care setting the incidence varies from 0 to 17%.[8] In a study from Ankara, Turkey it was found that 59.2% of these ulcers occur in patients admitted to the intensive care unit. The acceptable incidence rates for all settings should ideally be less than 2%. Two thirds of pressure sores occur in the elderly above 70 years of age. They are also common in young patients with neurological impairment. In Indian setting, the prevalence of pressure ulcers in hospitalized patients has been reported to be 4.94% in a study conducted by Chauhan et al.[12]
There are many studies on the incidence of pressure ulcer. In spinal cord injury patients, pressure ulcer occurs in 30-85% of patients during the first month of injury.[13–16] Also, paraplegics and quadriplegics are likely to have multiple ulcers.[17,18]
Patients with pressure ulcers have high mortality rates. Ueda et al, 1990 have reported 22% mortality over 6 years follow up of 23 patients with pressure ulcers.[19] Kuwahara et al. 2005 reported 68.8% mortality amongst elderly patients with NPUAP stage 3 and 4 pressure ulcers, because of secondary systemic complications.[20]
These data indicate that presence of pressure ulcer hampers quality of life and prevention of pressure ulcer is an important goal. Not surprisingly the hospital stay is longer in these patients with increased risk of nosocomial and renal infections. The hospital re-admission rate is also very high. Pressure ulcers result in an exponential increase in the healthcare burden and financial requirement for these patients. This brings us to the information on etiology and risk factors so that one can work on these factors for the prevention of pressure ulcers in susceptible patients.
ETIOPATHOGENESIS
Pressure between the bony prominence and external surface occludes the capillaries. The normal capillary pressure ranges from 16 to 33 mm Hg in different segments. External pressure of more than 33 mm Hg occludes the blood vessel so that the underlying and surrounding tissues become anoxic and if the pressure continues for a critical duration, cell death will occur, resulting in soft tissue necrosis and eventual ulceration.
As the new definition suggests, prolonged pressure is the leading contributing factor. It has been proven that there is an inverse relationship between the degree of pressure and the duration of pressure. Uninterrupted higher pressure requires shorter time while continuous lower pressure will require longer time to cause tissue necrosis and pressure ulceration.
Application of high pressure for shorter duration not only causes tissue necrosis due to blockage of capillaries but also produces pressure effect on the larger vessels causing thrombosis, more often venous thrombosis. Hence, the deleterious effect of high pressure for short duration is much more than that of low pressure for a longer duration. This has been proven by the observation that when the high pressure is relieved, ischemia persists because of effects on the adjacent larger vessels; while on relief from low pressure, the normal hyperemic response compensates for the temporary ischemia and the tissue does not undergo degeneration.
Due to the effect of pressure, the ischemic degenerative changes occur at all the levels simultaneously affecting the skin, subcutaneous fat, muscle and fascia if any between the bony prominence and the pressure causing surface. If subcutaneous necrosis occurs, ulceration will be clinically seen when the necrotic skin gives way. Hussain reported that for a specific pressure the obliteration of skin and subcutaneous vessels is more as compared to those of the underlying muscle.[21] But the tissue damage is more in the muscle after mechanical loading than in the skin.[22,23] Because of this the existing staging of pressure sores may not be justifiable. This needs to be studied further before any change in the prevailing staging is recommended.
One may question why different points in the body have different prevalence of ulceration. The variation in the pressure at different points during common postures is one explanation. The average pressure over the ischial tuberosity and the surrounding area exceeds 100 mm Hg during sitting,[24] at the sacral region it is 40-60 mm Hg in the supine position, while it is 70-80 mm Hg over the trochanteric region in the lateral lying down position.
Another reason for the differential incidence is the difference in the amount of soft tissue between the skin and the bony prominences. Sacrum and trochanters are devoid of much soft tissue covering. Effectively the skin directly covers these pressure points with very little interposition of soft tissue cushion, thus increasing the risk of ulceration as compared to the rest of the body [Figures 1–3].
Figure 1.
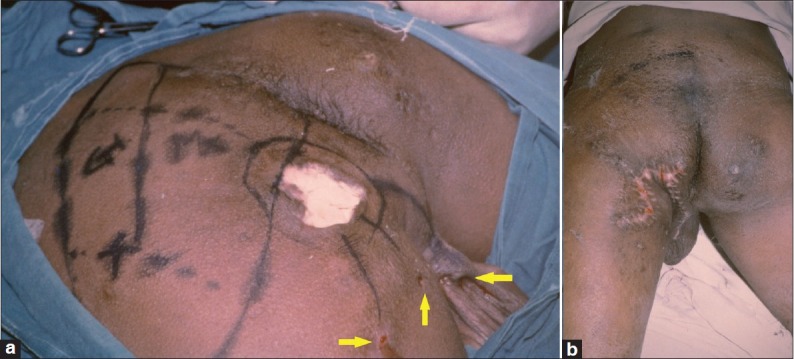
(a) Left sided ischial pressure ulcer with multiple sinuses in a paraplegic patient. Sinuses are highlighted with arrows. Gluteus maximus muscle has been marked for raising as a muscle flap (b) Complete excision of the ulcer with excision of sinuses has been done. The gluteus maximus muscle flap has been used to cover the ischial tuberosity and for filling the cavity
Figure 3.
(a) Left trochanteric pressure ulcer with a small external wound (b) The ulcer after debridement of the ulcer edge and the underlying bursa. One can notice the large wound under a small and deceptive pressure ulcer (c) Bilateral Trochanteric pressure ulcers have been resurfaced with bilateral tensor fascia lata myocutaneous flaps
Figure 2.

(a) A large sacral ulcer(b) Sacral ulcer has been managed with transverse back flap
The “sling effect” of the skin and subcutaneous tissue over the bony prominence is another interesting explanation. This sling effect prevents transmission of full pressure at deeper level, hence the impact of body pressure on the subcutaneous tissue is reduced to some extent.[25]
PATHOPHYSIOLOGY
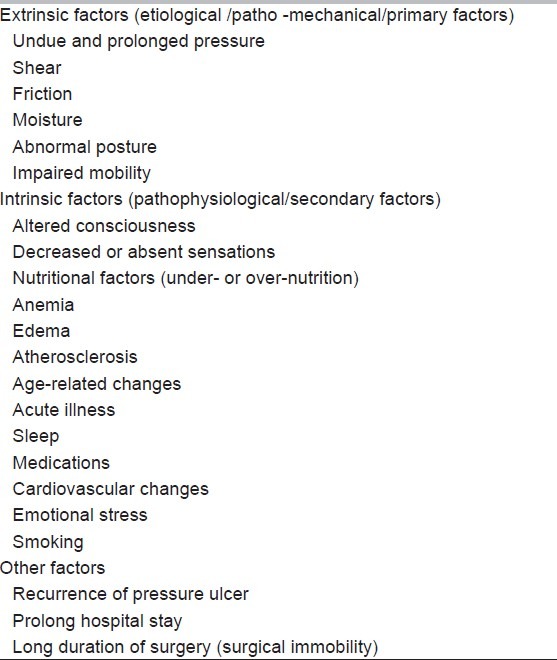
A lot of research has been undertaken to study the mechanism of tissue necrosis. It has been found that many intrinsic and extrinsic factors have an impact on the level and extent of tissue trauma. Extrinsic factors remain the main causative factors or the primary factors with “pressure” heading the list while intrinsic factors also called secondary factors contribute to it. The factors contributing to the formation of pressure ulcers are enlisted in Table 1.
Table 1.
Factors contributing to the formation of pressure ulcers
The dermal collagen fibers are also likely to protect against external pressure. Similarly the interstitial fluid acts as buffer and maintains the tissue hydrostatic pressure.[26–35]
Pressure
Pressure is the perpendicular load or force exerted on a unit area of the body.
Pressure = body weight/skin contact surface area.
Pressure effect is directly proportional to the body weight and the duration for which it is applied and is inversely proportional to the surface area of the skin in contact. The unit pressure is determined not only by the body weight but by the stiffness and composition of the tissues too. What is the resultant critical capillary pressure below which ischemia occurs is still questionable. Constant pressure for long period induces ischemia and causes reactive hyperemia. Muscles and subcutaneous tissues are more susceptible to pressure induced injury than the skin, therefore pressure ulcers are generally worse than what they appear on the skin surface. It has been rightly said that the wound that is seen on the surface is just the tip of the iceberg and the major injury lies under the skin defect.[24]
Apart from the direct effect of pressure causing ischemic tissue necrosis, the reperfusion after relieving the pressure leading to inflammatory tissue destruction by macrophages also participates in the causation of ulceration.[36]
Shearing
When the body tends to glide with gravity over a surface, the skin and the subcutaneous tissue remain stationary and there is a differential movement of the underlying soft-tissue like muscle and fascia. This shearing is an important patho- mechanical factor. This forceful inter-tissue plane movement causes stretching and tearing of blood vessels, reduced blood flow, stasis and ischemic tissue necrosis. This shearing may not directly cause any trauma to the skin surface. This usually occurs when a semi-reclining patient glides on the bed or on the operation table because of gravity or when the patient is turned and pushed on the bed without lifting him/her off the surface.
So, shear causes tissue damage differently, however, the damage is produced concomitant with pressure. It is difficult to create pressure without shear and shear without compression.[37]
Friction
Friction between the skin and the stationary, surfaces, such as bed clothes results in the loss of stratum corneum. This seems to be a trivial factor. However, this may initiate the breach in the epidermis. Repeated friction may lead to deeper injury. When there is loss of the stratum corneum, there is a breach in the barrier against infection. If the underlying tissue is relatively ischemic, it will get infected and result in deeper ulceration.
Moisture
This is an important extrinsic factor. The extrinsic moisture from perspiration, urine, feces and discharge causes maceration of the skin surface. The macerated skin forms blisters and is susceptible to breakdown. Excessive moisture on the skin surface also weakens the skin barrier and makes it more susceptible to pressure, shear and friction. This promotes the occurrence of ulceration.
Position of the patient
This is an extrinsic factor which determines the pressure points which are likely to cause pressure ulceration. Changes in body posture generates pressure at different anatomical points in the body making them susceptible to pressure ulceration [Figures 4a–d].
Figure 4.
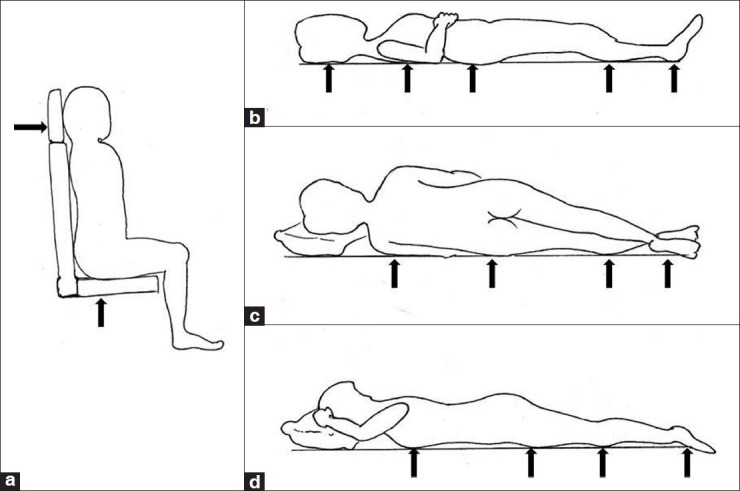
(a-d) Pressure points in sitting, supine, lateral and prone postures
These bony points transmit the body weight and hence, bear the brunt of pressure [Figures 5, 6]. In one of the studies ischial ulcer was the most common as the wheel chair bound patients spend long hours sitting, thus causing pressure on the ischial region. Trochanteric and sacral ulcers were the next common.[38]
Figure 5.

Pressure ulcer over the lateral border of heal, lateral malleolus and lateral border of fibula due to pressure in lateral posture
Figure 6.

Pressure ulcer over the knee and thigh because of the pressure in prone position
Studies have measured the transcutaneous oxygen tension at specific high risk pressure points during various postures on conventional as well as specialized beds. It has been proved that specialized beds maintain better tissue oxygen tension in weight bearing tissues.[39]
Immobility
This is inter-related with posture/position of the patient. Normal individual changes the posture frequently. Even during sleep, due to sensorimotor feedback system, a normal person periodically changes the posture in bed. This results in intermittent relief from pressure effect. This feedback system is impaired in neurologically compromised patients and in those who have received prolonged anesthesia or in sedated patients. The body fails to make postural adjustments in response to prolonged pressure and ischemia. The patients undergoing prolonged surgery of more than 4 hours are at a higher risk of developing pressure ulcer as they tend to stay immobile for a much longer period during the perioperative period.[40]
Neurological factors
The loss of sensory perception or impaired level of consciousness prevents the patient from perceiving the pain of pressure and the need to relieve it. Similarly neurological conditions causing paralysis or motor weakness prevents change of posture when pressure is exerted. Surprisingly poliomyelitis affected patients are less prone to pressure ulceration indicating that sensory loss is a more important factor. The sensation of pain and pressure prevents prolonged pressure and hence, the ischemia.
Metabolic and nutritional factors
Adequate nutrition, positive nitrogen balance, hydration, vitamins and trace elements are critical factors in the prevention of pressure ulceration. The patients with negative nitrogen balance are at a high risk of tissue breakdown and delayed healing [Figure 7]. A patient with rapid weight loss needs close observation. Patients with pressure ulceration or those prone to it should have an intake of 30-35 kcal/kg/day with 1.25-1.5 gram of protein/ kg/day. Specific supplementation with vitamin C, zinc and other trace elements needs to be assessed periodically in high risk patients.
Figure 7.

Sacral pressure ulcer in a patient with 60% total body surface burn
Hemoglobin is a good indicator of the patient's nutritional status. Good hemoglobin is required for tissue oxygenation. In anemic patients, oxygen carrying capacity of blood is reduced and hence, there is decreased supply of oxygen to the tissues. This will precipitate tissue necrosis in ischemic tissue because of mechanical pressure. Hence, well-nourished patients with good hemoglobin will be able to tolerate the deleterious effects of pressure better as compared to emaciated and anemic patients.
Edema
An edematous tissue has a compromised circulation and it is poor in nutrition. Increased tissue fluid also decreases the tissue oxygenation and is more prone to ulceration.One may think that edema fluid should have a cushioning effect and decrease the unit pressure over the pressure point. However, increased interstitial tissue fluid causes increased pressure over the blood vessels, decreases the pressure difference between the capillary blood and the tissue fluid and hence, decreases blood flow and oxygenation to the tissues. Hence, edema does not prevent rather enhances the deleterious effect of pressure.
RISK FACTORS AND PRESSURE ULCER RISK ASSESSMENT SCALES
This aspect of pressure ulcer is not discussed adequately amongst surgeons. These are more often deliberated upon in nursing literature. However, the treating surgeons should also be well aware of the various risk factors and the Risk Assessment Scales.
The extrinsic and intrinsic factors discussed above are the causative factors. There are a large number of other factors which are called risk factors. These factors should be looked for during the pre-ulcer period for a proper assessment of the risk of development of a pressure ulcer in a given patient. This is usually done by the nursing group in the unit. There are three scales in vogue. They are Norton, Braden and Waterlow scales. These scales are being reproduced from the original description.
An ideal risk assessment scale should have a high sensitivity and specificity for being able to correctly predict the risk of ulcer development. It should be easy to use and the criteria should be clear and definitive and applicable to different healthcare settings.[41]
Norton scale
Norton scale was developed by Doreen Norton et al. in 1962 [Table 2].[42]
Table 2.
Norton pressure ulcer risk assessment scale
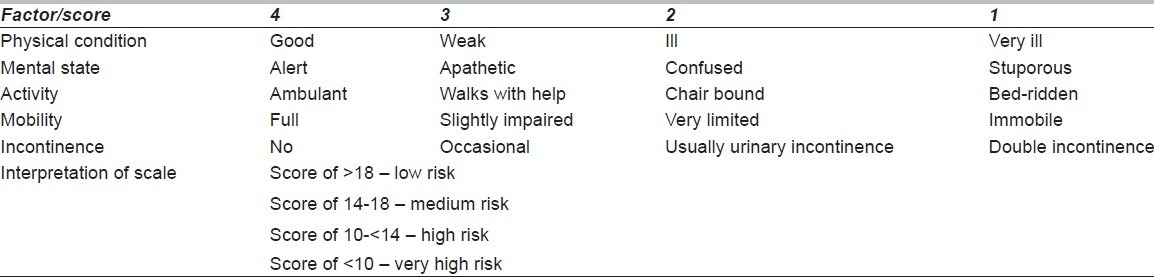
The Norton scale does not consider nutritional factors, shearing forces and does not have a functional definition of the applied parameters.
‘Norton plus scale’ is a modified scale in which the presence of the following are noted.[29,43]
Diabetes
Hypertension
Hematocrit – in males < 41%, in females < 36%
Hemoglobin – in males <14gm %; in females < 12gm %
Serum albumin level < 3.3 gm%
Fever - temperature >99.6°F
Prescription of ≥ 5 medications
Changes in mental state within 24 hours to confused, lethargic.
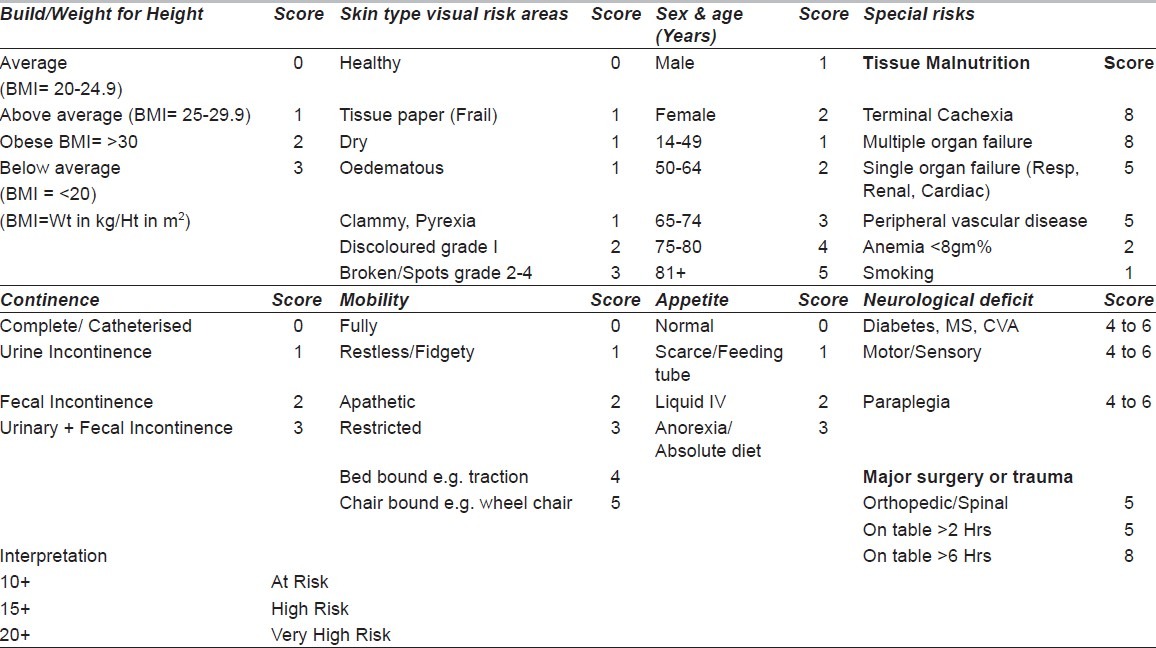
Waterlow scale
Waterlow scale was devised by Judy Waterlow et al. in 1987.[31,44,45] This is an incremental positive scoring system. [Table 3] Waterlow scale has the risk of over assessment. There are a large number of parameters making it complex. It states that women are at a higher risk of developing pressure ulcer than men.
Table 3.
Waterlow pressure ulcer risk assessment scale
Braden scale
This risk assessment scale has been devised by Bergstrom et al. in 1987 [Table 4]. It is an inverse scoring tool implying that the lower the score, the greater is the risk of developing ulcer. Score 1 is poor and 4 is normal.
Table 4.
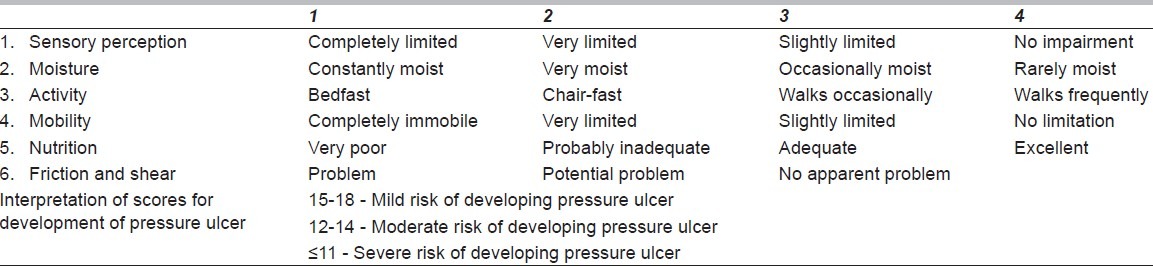
The same scale has been modified for predicting pressure ulcer risk in pediatric patients of ≥ 9 years of age, which is popularized as Modified Braden scale. In this scale only the interpretation score differs from the original Braden scale.
22-25 – mild risk
17-21 – moderate risk
≤ 16 – high risk
This scale is rated in scientific journals as having the best sensitivity and specificity. This scoring system is technically demanding and requires some training to use it properly.
CLASSIFICATION OF PRESSURE ULCER
The first well described classification of pressure sores was given by an orthopedic surgeon, Darrell Shea in 1975. It was a landmark paper in which Shea classified these ulcers into five categories defined by the anatomic depth of the soft tissue damage.[48] After Shea, the literature has been flooded with classifications. Amongst several, only a few classifications became popular. The most commonly used is the one presented by NPUAP. For the interest of readers the important classifications are reproduced along with a comparative table for easy understanding. [Table 5]
Table 5.
Comparative table of common classifications of pressure ulcers
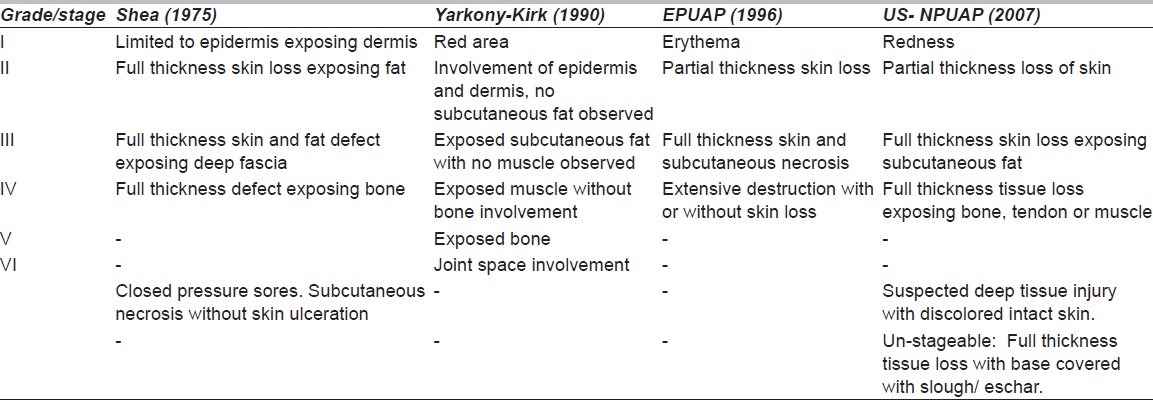
Popular classifications of pressure ulcer and comparison of various stages and grades [Table 2].
International classification of diseases (ICD-10) codes
ICD-10-AM codes are categorized into four stages as defined in the Australian Wound Management Guidelines but analysis is limited as there is no mechanism to identify the origin of the ulcer.
MANAGEMENT
Detailed management of pressure ulcer is beyond the scope of this article. “Prevention is better than cure” is best emphasized in the case of pressure ulcer. This condition is cent percent preventable with care, compassion and dedication towards the care of patients. Prevention is directed towards taking care of the extrinsic and intrinsic factors. There are innumerable methods of management of pressure ulcer as a wound. Many agents and methods have been used to take care of these wounds. The list is never-ending. Broadly these therapies can be enlisted under topical agents for debridement, topical therapeutic agents for infection control, therapeutic agents for wound healing, nutritional support, 2-hourly change of posture, avoidance/reduction of pressure with the use of special mattress and cushion, surgical management and education to patients and care givers.
CONCLUSIONS
Pressure ulcers are here to stay despite all the advances in prevention and management. One has to keep abreast with the etio-pathogenesis, risk factors and staging in detail so as to improve upon the understanding of this preventable condition. A more precise and wholesome definition has been suggested as the existing definition falls short of the true description of the disease process.
ACKNOWLEDGEMENT
The authors thank Dr. Aparna Agrawal, MD, Director Professor LHMC and Associated Hospitals, New Delhi for her suggestions, editing and correction of English transcript. We acknowledge the contribution of Ms. Shrreya Agrawal for preparing the line diagram.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Eltorai IM. History of spinal cord medicine. In: Lin VW, Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB, et al., editors. Spinal cord medicine: Principles and Practice. New York: Demos Medical Publishing; 2003. [Google Scholar]
- 2.Adams F. The genuine works of Hippocrates [translated from the Greek] Baltimore: Williams and Wilkins; 1939. pp. 231–42. [Google Scholar]
- 3.Levine JM. Historical notes on pressure ulcers: The cure of Ambrose Paré. Decubitus. 1992;5:23–4. [PubMed] [Google Scholar]
- 4.Levine JM. Historical perspective on pressure ulcer: The decubitus ominosus of Jean-Martin Charcot. J Am Geriatr Soc. 2005;53:1248–51. doi: 10.1111/j.1532-5415.2005.53358.x. [DOI] [PubMed] [Google Scholar]
- 5.Cosensus development conference statement. West Dundee, III: S N publications; 1989. [Last accessed on 2012 Jul 30]. National Pressure Ulcer Advisory Panel. Pressure Ulcers: Incidence, economics, risk assessment. Available from: http://www.npuap.org/pr2/htm . [Google Scholar]
- 6.Burdette-Taylor SR, Kass J. Heel ulcers in critical care unit: A major pressure problem. Crit Care Nurs. 2002;25:41–53. doi: 10.1097/00002727-200208000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Ozaka K, Watanabe Y. Epidemiology of vascular dementia. Nihon Rinsho. 2004;62S:13–7. [PubMed] [Google Scholar]
- 8.Cuddigan J, Ayello EA, Sussman C, Baranoski S. Pressure ulcers in America: Prevalence, incidence, and implications for the future. An executive summary of the National Pressure Ulcer Advisory Panel. 2001:153. doi: 10.1097/00129334-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Meehan M. Multi-site pressure ulcer prevalence survey. Decubitus. 1990;3:14–7. doi: 10.1097/00129334-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Shahin ES, Dassen T, Halfens RJ. Incidence, prevention and treatment of pressure ulcers in intensive care patients: A longitudinal study. Int J Nurs Stud. 2009;46:413–21. doi: 10.1016/j.ijnurstu.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 11.Leblebici B, Turhan N, Adam M, Akman MN. Clinical and epidemiologic evaluation of pressure ulcers in patients at a university hospital in Turkey. J Wound Ostomy Continence Nurs. 2007;34:407–11. doi: 10.1097/01.WON.0000281657.63449.1c. [DOI] [PubMed] [Google Scholar]
- 12.Chauhan VS, Goel S, Kumar P, Srivastava S, Shukla VK. The prevalence of pressure ulcers in hospitalized patients in a university hospital in India. J Wound Care. 2005;14:36–7. doi: 10.12968/jowc.2005.14.1.26724. [DOI] [PubMed] [Google Scholar]
- 13.Bliss MR. Acute pressure area care: Sir James Paget's legacy. Lancet. 1992;339:221–3. doi: 10.1016/0140-6736(92)90016-v. [DOI] [PubMed] [Google Scholar]
- 14.Curry K, Casady L. The relationship between extended periods of immobility and decubitus ulcer formation in acutely spinal-cord injured individuals. J Neurosci Nurs. 1992;24:185–9. doi: 10.1097/01376517-199208000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Linares HA, Mawson AR, Saurez E, Biundo JJ. Association between pressure sores and immobilization in the immediate post-injury period. Orthopedics. 1987;10:571–3. doi: 10.3928/0147-7447-19870401-07. [DOI] [PubMed] [Google Scholar]
- 16.Mawsun AR, Biundo JJ Jr, Neville P, Linares HA, Winchester Y, Lopez A. Risk factors for early occurring pressure ulcers following spinal cord injury. Am J Phys Med Rehabil. 1988;67:123–7. doi: 10.1097/00002060-198806000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Colen SR. Pressure sores. In: McCarthy JG, May JW, Littler JW, editors. Plastic surgery. Philadelphia: WB Saunders; 1990. pp. 3797–898. [Google Scholar]
- 18.Leigh IH, Bennet G. Pressure ulcers: Prevalence, etiology and treatment modalities. A review. Am J Surg. 1994;167:25S–30. doi: 10.1016/0002-9610(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 19.Ueda K, Tajima S, Sano S, et al. Mortality and recurrence rate after pressure ulcer operation for elderly long-term bedridden patients. J Osaka Med Coll. 1990;49:58–63. [Google Scholar]
- 20.Kuwahara M, Tada H, Mashiba K, Yurugi S, Iioka H, Niitsuma K, et al. Mortality and recurrence rate after pressure ulcer operation for elderly long-term bedridden patients. Ann Plast Surg. 2005;54:629–32. doi: 10.1097/01.sap.0000164465.40841.0b. [DOI] [PubMed] [Google Scholar]
- 21.Husain T. An experimental study of some pressure effects on tissues, with reference to the bedsore problem. J Pathol Bacteriol. 1953;66:347–58. doi: 10.1002/path.1700660203. [DOI] [PubMed] [Google Scholar]
- 22.Daniel RK, Priest DL, Wheatley DC. Etiologic factors in pressure sores: An experimental model. Arch Phys Med Rehabil. 1982;62:492–8. [PubMed] [Google Scholar]
- 23.Nola GT, Vistnes LM. Differential response of skin and muscle in the experimental production of pressure sores. Plast Reconstr Surg. 1980;66:728–33. doi: 10.1097/00006534-198011000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Kosaik M. Etiology and pathology of decubitus ulcers. Arch Phys Med Rehabil. 1959;40:62–8. [PubMed] [Google Scholar]
- 25.Romaneki M. Science and practice of pressure ulcer management. London: Springer-Verlay London Ltd; 2006. [Google Scholar]
- 26.Sangeorzan BJ, Harrington RM, Wyss CR, Czerniecki JM, Matsen FA., 3rd Circulatory response of skin to loading. J Orthop Res. 1989;7:425–31. doi: 10.1002/jor.1100070315. [DOI] [PubMed] [Google Scholar]
- 27.Collier M. Blanching and non-blanching hyperaemia. J Wound Care. 1999;8:63–4. doi: 10.12968/jowc.1999.8.2.26350. [DOI] [PubMed] [Google Scholar]
- 28.Deeks J, Higgins J, Riis J, Silagy C. Module 11: Summary statistics for dichotomous outcomes data. In: Alderson P, Green S, editors. Cochrane collaboration open learning material for reviewers. Version 1.1. Chichester: John Wiley; 2002. pp. 87–102. [Google Scholar]
- 29.Gosnell DJ. An assessment tool to identify pressure sores. Nurs Res. 1973;22:55–9. [PubMed] [Google Scholar]
- 30.Lowthian P. Pressure sore prevalence: A survey of sores in orthopedic patients. Nurs Times. 1979;75:358–60. [PubMed] [Google Scholar]
- 31.Waterlow J. Pressure sores: A risk assessment card. Nurs Times. 1985;81:49–55. [PubMed] [Google Scholar]
- 32.Braden B, Bergstrom N. A conceptual schema for the study of the etiology of pressure sores. Rehabil Nurs. 1987;12:8–12. doi: 10.1002/j.2048-7940.1987.tb00541.x. [DOI] [PubMed] [Google Scholar]
- 33.Gosnell DJ. Pressure sore risk assessment. Part II. Analysis of risk factors. Decubitus. 1989;2:40–3. [PubMed] [Google Scholar]
- 34.Defloor T. The risk of pressure sore: A conceptual scheme. J Clin Nurs. 1999;8:206–16. doi: 10.1046/j.1365-2702.1999.00254.x. [DOI] [PubMed] [Google Scholar]
- 35.Pressure ulcer prevention: Clinical guideline No. 7. London: NICE; 2003. National Institute for Clinical Excellence. [Google Scholar]
- 36.Salcido R, Fisher SB, Donofrio JC, Bieschke M, Knapp C, Liang R, et al. An animal model and computer-controlled surface pressure delivery system for the production of pressure ulcers. J Rehabil Res Dev. 1995;32:149–61. [PubMed] [Google Scholar]
- 37.Bridel J. The etiology of pressure sores. J Wound Care. 1993;2:230–8. doi: 10.12968/jowc.1993.2.4.230. [DOI] [PubMed] [Google Scholar]
- 38.Dansereau JG, Conway H. Closure of decubiti in paraplegics. Report of 2000 cases. Plast Reconstr Surg. 1964;33:474–80. [PubMed] [Google Scholar]
- 39.Feldman DL, Sepka RS, Kittzman B. Tissue oxygenation and blood flow on specialized and conventional hospital beds. Ann PlastSurg. 1993;30:441–4. doi: 10.1097/00000637-199305000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Walton-Geer PS. Prevention of pressure ulcer in the surgical patient. AORN J. 2009;89:538–48. doi: 10.1016/j.aorn.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 41.Torra i Bou JE. Valorar el riesgo de presentation presentar úlceras por presión. Escala de Braden. Rev Enferm. 1997;224:22–30. [PubMed] [Google Scholar]
- 42.Norton D, Exton-Smith AN, McLaren R. An Investigation of Geriatric Nursing Problems in Hospital. London: National Corporation for the Care of Old People; 1962. [Google Scholar]
- 43.Berglund B, Nordström G. The use of the modified Norton scale in nursing-home patients. Scand J Caring Sci. 1995;9:165–9. doi: 10.1111/j.1471-6712.1995.tb00407.x. [DOI] [PubMed] [Google Scholar]
- 44.Edwards M. The levels of reliability and validity of the Waterlow pressure sore risk calculator. J Wound Care. 1995;4:373–8. doi: 10.12968/jowc.1995.4.8.373. [DOI] [PubMed] [Google Scholar]
- 45.Weststrate JT, Hop WC, Aalbers AG, Vreeling AW, Bruining HA. The clinical relevance of the Waterlow pressure sore risk scale in the ICU. Intensive Care Med. 1998;24:815–20. doi: 10.1007/s001340050671. [DOI] [PubMed] [Google Scholar]
- 46.Bergstrom N, Braden B, Laguzza A, Holman V. The Braden Scale for predicting pressure sore risk: Reliability studies. Nurs Res. 1987;36:205–10. [PubMed] [Google Scholar]
- 47.Bergstrom N, Demuth PJ, Braden BJ. A clinical trial of the Braden scale for predicting pressure sore risk. Nurs Clin North Am. 1987;22:417–28. [PubMed] [Google Scholar]
- 48.Shea JD. Pressure sores: Classification and management. Clin Orthop Relat Res. 1975;112:89–100. [PubMed] [Google Scholar]



