Abstract
Lymphoedema is a progressive condition that can have a marked physical and psychological impact on affected patients and significantly reduce the quality of life. The ulcers on chronic lymphoedema patient, which often also makes it impossible for them to work. If left untreated, tends to progress or worsen. Ulcers in lymphoedema patients, therefore, represent not only a medical but also a psychological problem. The treatment is often regarded as being worse than it actually is. In our study of more than 25 years shows around 10% cases are due to chronic lymphodema. Ulcers of chronic lymphoedema are classified into four stages according to their presentation. Their management depends upon their stage of presentation. Patients with chronic lymphoedema and ulceration require a different approach to treatment. The specific issues associated with managing the patient with lymphoedematous ulceration include, limb shape distortion i.e., elephantiasis, care of the skin creases and folds, and swelling of the toes and fore foot. Stage I ulcers will heal with conservative treatment without any surgical intervention. Stage II ulcers needs debridement of the wound and split-thickness skin grafting. The most difficult to treat are the stage III and IV ulcers, due to associated skin changes and reduced vascularity. These cases need debulking along with excision of the ulcer. In order to prevent recurrence of the ulcer in all the four stages needs prolonged follow-up and limb care.
KEY WORDS: Lymphoedema, nodo-venous shunt, omentum, ulcer leg
INTRODUCTION
Approximately 70% of the limb ulcers are caused by venous diseases. Rest 30% are due to vascular diseases including, diabetic, malignant ulcers, traumatic ulcers, chronic lymphoedema and a few medical conditions. According to World Health Organisation (WHO) there are 120 million filarial lymphoedema cases distributed widely in 81 countries mostly in tropical and subtropical regions. Out of these 120 million, 41% of filarial lymphoedema cases are reported from India. In tropical and subtropical countries lymphoedema and its related complications are an underestimated health problem.[1]
Ulcer development in chronic lymphoedema even though less frequent than venous ulcers of the leg, is a very serious complication.[2] The main reasons for ulceration were found to be ulcerated lymphangiectasia, lymphorrhorea, inflammation and pustule formation, skin maceration, infection, papillomatosis and hyperkeratosis. These sequential changes give rise to ulcers in the overlying skin because adequate perfusion is impaired.
Aetopathogenesis
The most common aetiological agents are the group A β-hemolytic Streptococcus and Staphylococcus aureus.[3] The affected lymphatics are dilated and filled with exudates, chiefly of neutrophils and monocytes.[4] This leads to occlusion of lymphatic drainage and the abnormal accumulation of interstitional fluid, proteins, growth factors and other active peptide moieties, glycosaminoglycans and particulate matter including bacteria. As a result there is increase collagen production by fibroblasts, accumulation of inflammatory cells predominately macrophages and lymphocytes and activation of keratinocytes. The end result protein-rich oedema fluid increases deposition of ground substance, subdermal fibrosis and dermal thickening and proliferation, severe cases cellulitis or focal abscess formation. Chronic lymphoedema gives rise to ulcers in the overlying skin, because adequate perfusion is impaired.
MATERIALS AND METHODS
Seven thousand and two hundred and fifty chronic lymphoedema cases are studied since 1986. Out of these 4450 cases are male and 2800 cases are female with the age group ranging from 10 years to 90 years. Of these 74% of the cases are in the age group of 30-50 years. Stage III and stage IV are 92%, which means, bulk of the cases that come to us are in advanced stage of the disease. In my series almost all cases are secondary lymphoedema cases. There are only nine cases which are due to primary lymphoedema, in the age group of 10-25 years. The skin changes i.e., nodule formation, lymphorrhoea with maceration and ulceration cases are 22%
Chronic lymphoedema leg ulcer patients are divided in to 4 stages.
Stage 1 Lymphorrhoea with eczematous ulcerated lesion-, 2% of cases
Stage 2 Established ulcerated lesions- 4% of cases
Stage 3 Ulceration with deep sinus tract in elephantiasis legs- 3% of cases
Stage 4 Ulcers developed after excision procedures-1% of cases
In our study 10% of chronic lymphoedema patients present with leg ulcers. Few stage 1 cases come with Acute Dermato- Lymphangio-Adenitis (ADLA). These cases are frequently seen in rainy seasons due to fungal and bacterial infections in the webs of the toes. Some of these cases land with septicaemia with high mortality especially in elderly age group patients with metabolic diseases. Prevention of ADLA attacks in these patients is important since the occurrence of lymphoedema and its progress are related to these repeated infections. Long-term antibiotic therapy using long-acting parenteral benzathine penicillin is indicated to prevent recurrent ADLA attacks and its complications.[5] Stage 3 neglected cases come with deep sinus tract with foul-smelling discharge and some cases with maggot formation. The most difficult to treat cases are of the stage 4 after excision procedures like Kondoleon and Charles. The ulcers develop after these procedures are due to lymphorrhoea and its complications.
MANAGEMENT
Interestingly, in most endemic areas over 95% of cases of lymphoedema are amicrofilaraemic even by membrane filtration technique. ICT (immunochromatographic test) - Card test is useful for Wuchereria bancrofti circulating filarial antigen detection.
Isotope lymphoscintigraphy is useful to identify the lymphatic obstruction by RISHA or by technicium 99 - 0.5 to 1 ml is injected into the web space intradermally and lymphatics are traced by gamma camera.[6]
Stage 1
Leg ulcers are managed with conservative management. These ulcers will heal completely after bed rest, elevation of limb, wound dressing, antibiotics along with Diethyl carbamazine citrate (DEC) within a week.[7] Local antibiotic ointment or VAC is also useful in some cases [Figures 1 and 2].[8]
Figure 1.

Stage 1 ulcer with lymphorrhoea
Figure 2.

Stage 1 healed ulcer
Skin care is a major concern when managing patients with ulceration and oedema. Moisturization of the skin is essential to maintain its hydration. An appropriate dressing should be used to protect the skin around the wound from maceration.
Stage 2
Ulcers need surgical intervention along with conservative measures. Debridement of the ulcer and split-thickness skin grafting is necessary in these cases. Mean hospital stay in these cases is about 3-4 weeks. Postoperative limb care is utmost important to prevent recurrent ulcers formation in these patients [Figures 3 and 4].
Figure 3.

Stage 2 chronic ulcers
Figure 4.
Stage 2 chronic ulcers
Stage 3
Ulcers of the chronic Lymphoedema leg are the complicated cases. Even though surface ulcers look small, the sinus tract extends deep with lot of necrosed tissue inside. In the deep cavity maggots will form. All these cases need excision of the ulcer along with sinus tract as a combined debulking procedure. The obstructed lymphatics are first bypassed by doing nodovenous shunt or omfentum transposition depending on secondary or primary lymphoedema leg ulcers, respectively [Figures 5 and 6].
Figure 5.

Stage 3 ulcer with sinus tract
Figure 6.

After N-V Shunt and debulking - patient in Figure
Stage 4
Ulcers are the one following excision procedures in stage IV lymphoedema cases after Kondoleon and Charles. These ulcers are not going to heal with traditional methods of ulcer healing. After prolonged conservative measures followed by split-thickness skin grafting, some of these cases may heal but, they will recur in due course of time. Continuous lymphorrhoea lead to maceration of the skin and ulcer formation. A graduated, sustained compression therapy is traditionally used in the management of this type of leg ulcers. The multilayer lymphoedema bandaging (MLLB) such as padding, toe bandaging and full leg bandaging may be incur-porated into venous bandaging systems, as they help to reduce the oedema thereby enhancing healing.[9] Multilayered bandaging system is used and is said to be more effective than single layer system.[10] Mobility and exercise play an important role in the management of patients with lymphoedema and ulceration, especially if the patient is undergoing MLLB. Movement can improve lymph flow by enhancing the muscle pump action which has an effect on lymphatic and venous flow.[11] Healing of the ulcer after these measures and skin grafting needs prolonged follow-up to prevent recurrence [Figures 7 and 8].
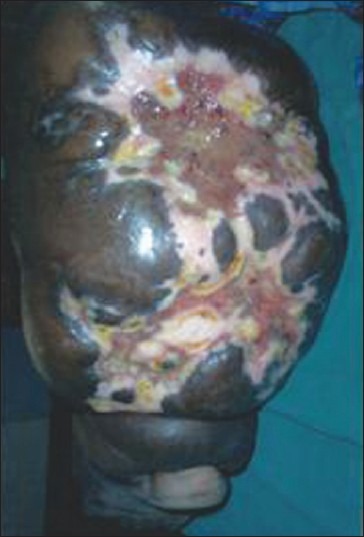
Figure 7.

Stage 4 ulcers after excisional procedure
Figure 8.

Stage 4 ulcers after excisional procedure
RESULT
Ulcer development in lymphoedema is rare and a very serious complication. The main reasons for ulceration were found to be ulcerated lymphangiectasia, lymph trickling, inflammation and pustule formation, skin maceration, infection, papillomatosis and hyperkeratosis. The small arteries are damaged in lymphoedema. The treatment does not end after healing of the ulcer, in whatever stage it may be presented. Postoperative skin care of the limb, compression bandage, limb exercises to promote lymph drainage are absolutely necessary. A course of antibiotics and diethyl carbamazine citrate are necessary to treat reinfection and prevent recurrence of the leg ulcer. These patients lead comfortable life as long as they follow the postoperative care.[12] In my observation those patients who are for long-term follow-up, are free from any complications for years together. In my observation all the stage 1 ulcers will heal in a week to 10 days time, whereas in stage 4 ulcers remain as chronic nonhealing in 10-20% of our cases. State 2 and 3 ulcers will heal in 3-4 weeks time after surgical procedures described earlier.
DISCUSSIONS AND CONCLUSIONS
Recognition of chronic oedema in patients with ulceration is essential if treatment is to be managed effectively. A combined approach to management is essential to facilitate successful outcomes for this client group. Assessment and correct diagnosis is crucial to the recognition of chronic lymphoedema leg ulcer. Complex physiotherapy of lymphoedema is necessary to prevent ulceration. Those patients who are not in follow-up are coming with recurrence of the ulcers. The staging of the filarial lymphodema leg ulcers are conveniently divided in to four stages in my cases according to the clinical presentation and response to the treatment. Meticulous care of the lymphoedema leg and treatment for reinfection prevent ulcer formation in lymphoedema. Judit Daroczy in his study in ulcers in lymphoedema stated that inflammatory cell markers (CD68-positive macrophages) were found in higher number in lymphoedema ulcers than in diabetic ulcers. Biopsy of chronic lymphoedema ulcers in our series showed only inflammatory cells. None of these cases turned into malignant ulcers even in very long-standing nonhealing ulcers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Moffatt CJ, Franks PJ, Doherty DC, Williams AF, Badger C, Jeffs E, et al. Lymphoedema: An underestimated health problem. QJM. 2003;96:731–8. doi: 10.1093/qjmed/hcg126. [DOI] [PubMed] [Google Scholar]
- 2.Moffatt CJ, Franks PJ, Doherty DC, Martin R, Blewett R, Ross F. Prevalence of leg ulceration in a London population. QJM. 2004;97:431–7. doi: 10.1093/qjmed/hch075. [DOI] [PubMed] [Google Scholar]
- 3.Suma TK, Shenoy RK, Varghese J, Kuttikkal VV, Kumaraswami V. Estimation of ASO titer as an indicator of streptococcal infection precipitating acute adenolymphangitis in lymphoedema caused by brugian filariasis. Southeast Asian J Trop Med Public Health. 1997;28:826–30. [PubMed] [Google Scholar]
- 4.Vaqas B, Ryan TJ. Lymphoedema: Pathophysiology and management in resource-poor setting- relevance for lymphatic filariasis control programmes. Filaria J. 2003;2:4. doi: 10.1186/1475-2883-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shenoy RK, Sandhya K, Suma TK, Kumaraswami V. A preliminary study of filariasis related acute adenolymphangitis with special reference to precipitating factors and treatment modalities. Southeast Asian J Trop Med Public Health. 1995;26:301–5. [PubMed] [Google Scholar]
- 6.Tiwari A, Cheng KS, Button M, Myint F, Hamilton G. Differential diagnosis, investigation and current treatment of lower limb lymphoedema. Arch Surg. 2003;138:152–61. doi: 10.1001/archsurg.138.2.152. [DOI] [PubMed] [Google Scholar]
- 7.Shenoy RK, Kumaraswami V, Suma TK, Rajan K, Radhakuttyamma G. A double blind placebo -controlled study of the efficacy of oral penicillin, diethylcarbamazine or local treatment of the affected limb in preventing acute adenolymphangitis in lymphoedema caused by brugian filariasis. Ann Trop Med Parasitol. 1999;93:367–77. doi: 10.1080/00034989958366. [DOI] [PubMed] [Google Scholar]
- 8.Wollina U, Hansel G, Krönert C, Heinig B. Using VAC to facilitate healing of traumatic wounds in patients with cronic lymphoedema. J Wound Care. 2010;19:15–7. doi: 10.12968/jowc.2010.19.1.46094. [DOI] [PubMed] [Google Scholar]
- 9.McCann M. Toe bandaging for lymphoedema and venous ulceration. (430-3).Br J Nurs. 2008;17:428. doi: 10.12968/bjon.2008.17.7.29061. [DOI] [PubMed] [Google Scholar]
- 10.Flecher A, Cullum N, Sheldon TA. A systematic review of compression treatment for venous leg ulcers. BMJ. 1997;315:576–80. doi: 10.1136/bmj.315.7108.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mortimer PS, Simmonds R, Rezvani M, Robbins M, Hopewell JW, Ryan TJ. The measurement of skin lymph flow by isotope clearance-reliability, reproducibility injection dynamics and effect of massage. J Invest Dermatol. 1990;95:677–82. doi: 10.1111/1523-1747.ep12514347. [DOI] [PubMed] [Google Scholar]
- 12.Franks PJ, Moffatt CJ, Doherty DC, Williams AF, Jeffs E, Mortimer PS. Assessment of health-related quality of life in patients withlymphedema of the lower limb. Wound Repair Regen. 2006;14:110–8. doi: 10.1111/j.1743-6109.2006.00099.x. [DOI] [PubMed] [Google Scholar]


