Abstract
Wound care is constantly evolving with the advances in medicine. Search for the ideal dressing material still continues as wound care professionals are faced with several challenges. Due to the emergence of multi-resistant organisms and a decrease in newer antibiotics, wound care professionals have revisited the ancient healing methods by using traditional and alternative medicine in wound management. People's perception towards traditional medicine has also changed and is very encouraging. The concept of moist wound healing has been well accepted and traditional medicine has also incorporated this method to fasten the healing process. Several studies using herbal and traditional medicine from different continents have been documented in wound care management. Honey has been used extensively in wound care practice with excellent results. Recent scientific evidences and clinical trials conducted using traditional and alternative medicine in wound therapy holds good promise in the future.
KEY WORDS: Alternative medicine, complementary medicine, traditional medicine, wound healing, wound management
INTRODUCTION
Traditional medicine (also known as indigenous or folk medicine) comprises the knowledge that has been developed over generations within various societies before the era of modern medicine. Practices known as traditional medicines include Herbal, Ayurveda, Siddha, Unani, Iranian, Islamic, Vietnamese, Chinese, Acupuncture, Muti, Ifá, African and other pseudo-medical knowledge and practices all over the globe.
It may include formalized aspects of folk medicine, i.e. longstanding remedies passed on and practiced by lay people.
The World Health Organization (WHO) defines traditional medicine as ‘the health practices, approaches, knowledge and beliefs incorporating plant, animal and mineral-based medicines, spiritual therapies, manual techniques and exercises, applied singularly or in combination to treat, diagnose and prevent illnesses or maintain well-being’.[1]
In some Asian and African countries, up to 80% of the population rely on traditional medicine for their primary health-care needs. When adopted outside of its traditional culture, traditional medicine is often called complementary and alternative medicine (CAM).
Alternative medicine is any healing practice ‘that does not fall within the realm of conventional medicine’. It may be based on historical or cultural traditions, rather than on scientific evidence. The terms ‘complementary medicine’ or ‘alternative medicine’ is used inter-changeably with traditional medicine in some countries. They refer to a broad set of health-care practices that are not part of that country's own tradition and are not integrated into the dominant health-care system.
A wound can be defined as a disruption in the continuity of the epithelial lining of the skin or mucosa. Injury, due to surgery or accident, results in destruction of tissue, disruption of blood vessels and extravasations of blood constituents and hypoxia. Wound healing is a complex process that has three phases: inflammatory phase, proliferative phase and maturation phase.
Wound healing is the result of interactions among cytokines, growth factors, blood and cellular elements, and the extracellular matrix. The cytokines promote healing by various pathways, such as stimulating the production of components of the basement membrane, preventing dehydration, increasing inflammation and the formation of granulation tissue.
Wounds can be broadly classified into acute and chronic wounds depending on their aetiology. Acute wounds occur most commonly due to accidents such as trauma or burns. Acute wounds should normally heal in a short duration provided the right treatment is given. In wound healing, it is always pertinent to achieve rapid and complete wound healing since the resulting scar tissue will be more satisfactory. Hence, the goal of every medical practitioner treating wounds should be to achieve early wound healing. Chronic wounds take a longer time to heal or sometimes even recur due to the underlying pathology. Hence, the underlying problem should first be identified and treated accordingly. When treating chronic wounds, it is important to note that biofilms play an important role in the prevention of wound healing. These biofilms harbour various microorganisms which delay the wound healing process. Due to the rise in antibiotic resistance, alternative/traditional medicines are increasingly becoming popular to overcome these multi- resistant organisms. Patients with chronic wounds require prolonged periods of dressings and this can cause a significant financial burden to the health-care system. With the advent of alternative and traditional wound care products, the financial burden can be significantly reduced. The concept of moist wound healing has been generally well accepted and many practitioners are adopting this method.[2] Several traditional wound-care products are currently commercially available incorporating the concept of moist wound healing.
Generally, the importance and efficacy of traditional and complementary medicine have risen. Almost four billion people worldwide use plants as medicines as nothing else is affordable or available.[3] Patients who use alternative medicine are generally between the ages of 30 and 49 years.[4] Generally, women more commonly use CAM compared to men.[5–7]
PLANT EXTRACTS AND HERBAL MEDICINE FOR WOUND CARE
Herbal medicines include herbs, herbal materials, herbal preparations and finished herbal products that contain an active ingredient, parts of plants, or other plant materials, or combinations. Before the advent of modern medicine, people of all continents have used medicines from plant origins since pre-historic times.
Ancient Egyptian medicines of 1000 BC are known to have used garlic, opium, castor oil, coriander, mint, indigo and other herbs for medicine and the Old Testament also mentions herbal use and cultivation, including mandrake, vetch, caraway, wheat, barley and rye. In India, Ayurvedic medicine has used many herbs such as turmeric possibly as early as 1900 BC.[8]
The first Chinese herbal book, the Shennong Bencao Jing, compiled during the Han Dynasty but dating back to a much earlier date, possibly 2700 BC, lists 365 medicinal plants and their uses-including ma-Huang, the shrub that introduced the drug ephedrine to modern medicine. Succeeding generations augmented on the Shennong Bencao Jing, as in the Yaoxing Lun (Treatise on the Nature of Medicinal Herbs), a 7th century Tang Dynasty treatise on herbal medicine. A number of traditions came to dominate the practice of herbal medicine at the end of the 20th century: The ‘classical’ herbal medicine system is based on Greek and Roman sources, the Siddha and Ayurvedic medicine systems from various South Asian Countries, Chinese herbal medicine, Traditional African medicine, Unani-Tibb medicine, Shamanic herbalism and Native American medicine.
Aloe vera
Aloe vera is a cactus-like plant which readily grows in hot, arid conditions. Aloe vera gel is obtained from the mucilaginous part of the centre of the leaf. It has been used for many centuries and comprises the major ingredient in various commercial skin and wound-care products. It can be used orally and topically to treat a wide range of health-related disorders. The aloe vera gel contains vitamins A, B, C, E, enzymes, polysaccharides, amino acids, sugars and minerals.
In the management of acute and chronic wounds, several reports using aloe vera have demonstrated variable results.[9–13] Hence, it can be concluded that though there is supporting evidence that aloe vera can improve wound healing rates, further large randomized control trials are needed to substantiate this.
Traditional chinese medicine
Traditional Chinese Medicine (TCM) refers to a broad range of medicine practices sharing common theoretical concepts which have been developed in China and are based on a tradition of more than 2000 years, including various forms of herbal medicine, acupuncture, massage, exercise (qigong) and dietary therapy. Although these practices are considered alternative medicine in the Western world, they are a common part of medical care throughout East Asia, accounting for the estimated 40% of all health care delivered in China.
Several studies conducted in China using TCM have demonstrated positive outcome on acute and chronic wounds. Hence, TCM has a strong potential to be widely used in traditional wound care.[14–16]
Miscellaneous herbal medicine in wound care
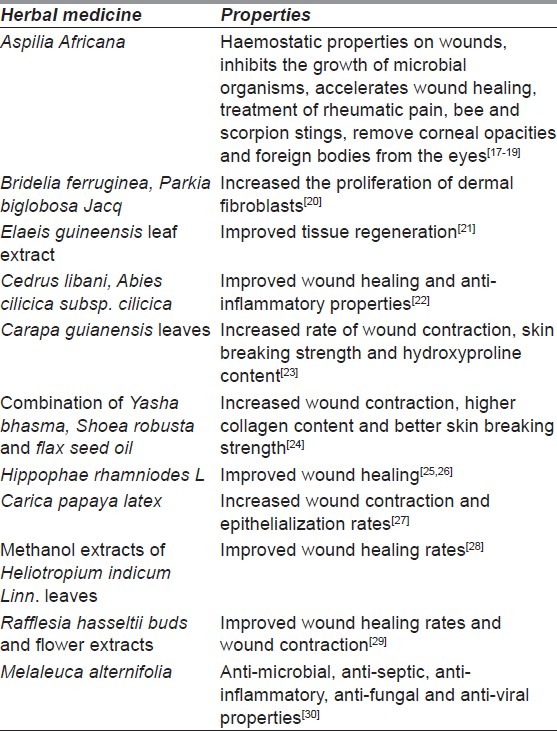
The use of herbal medicine in wound care has been very encouraging and several researchers around the globe have started to publish their results. Table 1 summarizes the use of miscellaneous herbal medicines in wound care.
Table 1.
Miscellaneous herbal medicine in wound care
Role of honey in wound management
Honey is a combination of various sugars producing a highly viscous sweet solution which is obtained from the nectar of flower or other plant secretions. The honey bee (Apis mellifera) is responsible for this mixture of sugars in addition to various other enzymes which originate from the bees.
The use of honey in wound management dates back to many centuries. Honey has been used to treat wounds, burns, cataracts, skin ulcers and diarrhoea.[31,32] The medicinal property of honey has been described in the Bible, the Quran and the Torah.[33,34] The first documentation of the use of honey in wound management was by the Egyptians in 2000 BC.[31] The Egyptians have used honey as a beauty cream and also for embalming the dead. In Ayurvedic medicine, honey has been described as the nectar of life. It has been used widely to treat various diseases.[32] In the early 20th century, various reports have documented the use of honey in burns and have confirmed the advantages of using this natural remedy for wounds.[35,36] However, with the advent of antibiotics and other surgical procedures, the Western medicine replaced the use of honey.[37] Due to the widespread use of antibiotics, resistance to various antibiotics has developed and many multi-resistant micro-organisms are present. As the introduction of newer antibiotics decreased, the emergence of alternative or traditional medicine was reborn. Hence, the interest of using honey for wound management was re-initiated.
Composition and properties of honey
Honey has approximately 40% fructose, 30% glucose, 5% sucrose and 20% water. It also contains several amino acids, antioxidants, vitamins, minerals, glucose oxidase, which produces hydrogen peroxide, and gluconic acid, which gives the honey an acidic pH of 3.2-4.5.[38] Since Clostridium botulinum is able to survive in honey, there is a risk of botulism or gangrene.[39] Hence, it is advocated to sterilize the honey using gamma irradiation at a dose of 25-50 kGy.[40]
Honey has a unique property of delivering a moist wound healing environment due to its highly viscous nature.[41] Due to the hyperosmolarity of honey, it is able to absorb the exudates from the wound and enable the wound to heal in a moist environment. Honey has anti-bacterial, anti- inflammatory and anti-fungal properties.[42–46] Honey has been documented to increase wound contraction and wound epithelialization in animal and human studies.[47,48] Honey has the inherent capability to increase the formation of granulation tissue, stimulate tissue growth, and reduce edema, inflammation and the synthesis of collagen.[41] Honey is able to reduce the incidence of post-operative adhesions in intra-abdominal tissues.[49] Honey has the potential to deodorize the wound and also reduce pain.[41]
The anti-bacterial properties are due to the complex interplay of the various components of honey, namely hydrogen peroxide, methylgyoxal and bee defensin-1.[50,51] From a recent study by Kwakman et al., it was concluded that the bactericidal activity of honey is highly complex and vary for individual bacterial species.[50] The concentration of honey has also an impact on the anti-bacterial activity; the higher the concentration of honey, the greater is its anti-bacterial action.[52]
Interestingly, different sources of honey have different bactericidal activity. Hence, it is imperative to delineate the exact spectrum of anti-bacterial activity for different sources of honey.[50] The major medical-grade honeys approved for clinical application are Manuka and Revamil®. Manuka honey which is produced from the manuka bush (Leptospermum scoparium) originates from New Zealand and Australia and has been widely tested worldwide. However, almost every sub continent has individual sources of honey and has reported successful results in wound therapy.
CURRENT SCIENTIFIC EVIDENCE ON THE USE OF HONEY IN WOUND MANAGEMENT
Numerous clinical trials have been conducted to test the efficacy of honey in wound management. The focus of this article will be on human trials. A total of 20 clinical trials have been conducted on acute and chronic wounds.
In acute wounds, a total of 15 clinical trials have been conducted using honey. Acute wounds can be subdivided into acute burn wounds and acute wounds not caused by burns.
Acute burn wounds
A total of 11 clinical trials have been conducted on acute burn wounds.
Subrahmanyam et al. conducted two trials (n = 154) on superficial burn wounds. In both the trials, the control group used silver sulfadiazine (SSD) and honey-treated wounds had better healing rates.[53,54] Gupta et al. conducted a trial (n = 108) on superficial and partial thickness burn wounds, comparing honey with SSD. They also noted better healing rates with the honey group (18.1 vs. 32.6 days).[55] Six trials (n = 1326) were conducted on partial thickness burn wounds. Five of the six trials were conducted by the same researcher. In all the six trials conducted on partial thickness burn wounds, honey showed better healing properties.[56–61] Subrahmanyam et al. conducted two trials on mixed partial thickness and full thickness burn wounds. In the first study (n = 50), they compared honey dressing with tangential excision and skin grafting. The skin grafting group showed better healing patterns compared to the honey-treated group (18.4 vs. 32 days).[62] In the second study, honey was compared with SSD in 100 patients with less than 40% total body surface area (TBSA) of burns. The healing rates were better with the honey-treated group (15.4 vs. 17.2 days).[63] From these selected clinical trials, there seems to be a trend in favour of honey in the management of superficial and partial thickness burn wounds, but strong evidence is lacking. In the management of full thickness burn wounds, honey does not seem to improve healing as only two studies have been conducted. Hence, more clinical trials are needed to substantiate the evidence of the use of honey in superficial and partial thickness burn wounds.
Non-burn acute wounds
Four clinical trials have been conducted for non-burn acute wounds.
Two studies were conducted on surgical wounds created following partial or total toe nail avulsions. In the first study (n = 51), Marshal et al. failed to report better healing rates with honey compared to iodine (33.4 vs. 25.4 days).[64] In the second study (n = 100), McIntosh et al. also did not achieve better healing rates with honey compared to paraffin gauze dressing (40.3 vs. 39.98 days).[65] There was only one trial (n = 87) conducted on laceration or shallow abrasion wounds in 2006 by Ingle et al. In this study, the authors compared honey with hydrogel dressing in abrasion wounds between 10 and 100 cm2. There was no difference in the healing rates (16.48 vs. 16.88 days).[66] From these selected clinical trials, there is insufficient evidence to support the use of honey in acute wounds such as abrasions, lacerations or toe nail avulsions. A trial (n = 75) was conducted by Farrah et al. on split skin graft donor sites using honey hydrogel and plain hydrogel. The honey hydrogel group showed better healing rates at days 10 and 15.[67]
In chronic wounds, a total of five clinical trials have been conducted using honey. Two trials were conducted for chronic leg ulcers.[68,69] Both these trials had no significant effect of honey on ulcer healing at 12 weeks. Jull et al. conducted a study (n = 368) on chronic leg ulcers comparing honey and usual care. The time to achieve complete healing was 12 weeks. Only 55.6% of the honey-treated wounds healed at 12 weeks in comparison with 49.7% for the control group.[68] Gethin et al. conducted another study (n = 108) on chronic leg ulcers comparing honey and hydrogel. The honey-treated group did not show better healing rates (44.4% vs. 33.3%).[69] Weheida et al. conducted a trial on pressure ulcers grade I or grade II. The honey group had better healing rates compared to the control group (8.20 vs. 9.93 days).[70] But strong evidence is lacking as more clinical studies are necessary. Al Waili conducted a study (n = 50) on infected post-operative wounds. Infected caesarean or hysterectomy wounds were tested with honey and povidone iodine with ethanol 70%. The results favoured the honey group (84.6% vs. 50%).[71] Subrahmanyam et al. conducted a study (n = 30) on patients with Fournier's gangrene. Honey was compared with EUSOL dressing and the wound healing rates significantly favoured the honey group (18.5 vs. 26.5 days).[72] Based on these limited studies, it is inappropriate to conclude that honey has a beneficial role in chronic wounds. However, larger randomized clinical trials are advocated to further substantiate the usefulness of honey.
In this review, it is clear that traditional medicine from plant and flower extracts can be used for wound management in certain conditions. Due to the escalating cost of health care especially in wound management, it is economical to use traditional medicine to treat wounds. However, large randomized clinical trials are necessary to give more concrete evidence supporting the use of traditional medicine in wound management. But this does not deter the promise that traditional medicine holds good for the management of wounds in future.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. Traditional medicine: Fact sheet N134. 2008. Dec, [Last accessed on 2012 Apr 15]. Available from: http://www.who.int/mediacentre/factsheets/fs134/en/
- 2.Lusby PE, Coombes AL, Wilkinson JM. Bacterial activity of different honeys against pathogenic bacteria. Arch Med Res. 2005;36:464–7. doi: 10.1016/j.arcmed.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 3.Chambliss LR. Alternative and Complementary Medicine: An Overview. Clin Obstet Gynaecol. 2001;44:640–52. doi: 10.1097/00003081-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Astin J, Marie A, Pelletier KR, Hansen E, Haskenn WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158:2303–10. doi: 10.1001/archinte.158.21.2303. [DOI] [PubMed] [Google Scholar]
- 5.Cassileth B, Lusk E, Strouse T, Bodenheimer BJ. Contemporary unorthodox treatments in cancer medicine: A study of patients, practices, and practitioners. Ann Intern Med. 1984;101:105–12. doi: 10.7326/0003-4819-101-1-105. [DOI] [PubMed] [Google Scholar]
- 6.Cook C, Baisden D. Ancillary use of folk medicine by patients in primary care clinics in southwestern West Virginia. South Med J. 1986;79:1098–101. doi: 10.1097/00007611-198609000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Millar W. Use of alternative health care by Canadians. Can J Public Health. 1997;88:154–8. doi: 10.1007/BF03403879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aggarwal BB, Sundaram C, Malani N, Ichikawa H. Curcumin: The Indian solid gold. Adv Exp Med Biol. 2007;595:1–75. doi: 10.1007/978-0-387-46401-5_1. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Bigas M, Cruz NI, Suarez A. Comparative evaluation of Aloe vera in the management of burn wounds in guinea pigs. Plast Reconstr Surg. 1988;81:386–9. doi: 10.1097/00006534-198803000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman T, Kalderon N, Ullmann Y, Berger J. Aloe vera gel hindered wound healing of experimental second-degree burns: A quantitative controlled study. J Burn Care Rehabil. 1988;9:156–9. doi: 10.1097/00004630-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Visuthikosol V, Chowchuen B, Sukwanarat Y, Sriurairatana S, Boonpucknavig V. Effect of Aloe vera gel to healing of burn wound a clinical and histologic study. J Med Assoc Thai. 1995;78:403–9. [PubMed] [Google Scholar]
- 12.Khorasani G, Hosseinimehr SH, Azadbakht M, Zamani A, Mahdavi MR. Aloe vs silver sulfadiazine creams for second degree burns: A randomized controlled study. Surg Today. 2009;39:587–91. doi: 10.1007/s00595-008-3944-y. [DOI] [PubMed] [Google Scholar]
- 13.Avijgan M. Phytotherapy: An alternative treatment for nonhealing ulcers. J Wound Care. 2004;13:157–8. doi: 10.12968/jowc.2004.13.4.26599. [DOI] [PubMed] [Google Scholar]
- 14.Lv G, Cai L, Yu J. Effectiveness of traditional Chinese medicine and Western medicine in treating residual deep burn wound. [Article in Chinese] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24:937–9. [PubMed] [Google Scholar]
- 15.Li FL, Deng H, Wang HW, Xu R, Chen J, Wang YF, et al. Effects of external application of Chinese medicine on diabetic ulcers and the expressions of â-catenin, c-myc and K6. Chin J Integr Med. 2011;17:261–6. doi: 10.1007/s11655-011-0703-5. [DOI] [PubMed] [Google Scholar]
- 16.Lau KM, Lai KK, Liu CL, Tam JC, To MH, Kwok HF, et al. Synergistic interaction between astragali radix and rehmanniae radix in a Chinese herbal formula to promote diabetic wound healing. J Ethnopharmacol. 2012;141:250–6. doi: 10.1016/j.jep.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 17.Macfoy CA, Cline EI. In vitro antibacterial activities of three plants used in traditional medicine in Sierra Leone. J Ethnopharmacol. 1990;28:323–7. doi: 10.1016/0378-8741(90)90083-6. [DOI] [PubMed] [Google Scholar]
- 18.Oyedepo OO, Akindele VR, Okunfolami OK. Effect of extracts of Olax subscorpioides and Aspilia africana on bovine red blood cells. Phytother Res. 1997;11:305–6. [Google Scholar]
- 19.Okoli CO, Akah PA, Nwafor SV, Anisiobi AI, Ibegbunam IN, Erojikwe O. Anti-inflammatory activity of hexane leaf extract of Aspilia africana C.D. Adams. J Ethnopharmacol. 2007;109:219–25. doi: 10.1016/j.jep.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 20.Adetutu A, Morgan WA, Corcoran O. Ethnopharmacological survey and in vitro evaluation of wound-healing plants used in South-western Nigeria. J Ethnopharmacol. 2011;137:50–6. doi: 10.1016/j.jep.2011.03.073. [DOI] [PubMed] [Google Scholar]
- 21.Sasidharan S, Logesvarasoo S, Latha LY. Wound healing activity of Elaeis Guineensis leaf extract ointment. Int J Mol Sci. 2011;13:336–47. doi: 10.3390/ijms13010336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tumen I, Akkol EK, Süntar I, Keleş H. Wound repair and anti-inflammatory potential of essential oils from cones of Pinaceae: Preclinical experimental research in animal models. Ethnopharmacol. 2011;137:1215–20. doi: 10.1016/j.jep.2011.07.046. [DOI] [PubMed] [Google Scholar]
- 23.Nayak BS, Kanhai J, Milne DM, Pereira LP, Swanston WH. Experimental evaluation of ethanolic extracts of carapa guianensis l.leaf for its wound healing activity using three wound models. Evid Based Complement Alternat Med. 2011;2011:419612. doi: 10.1093/ecam/nep160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Datta HS, Mitra SK, Patwardhan B. wound healing activity of topical forms based on ayurveda. Evid Based Complement Alternat Med. 2011;2011:134378. doi: 10.1093/ecam/nep015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta A, Kumar R, Pal K, Banerjee PK, Sawhney RC. A preclinical study of the effects of seabuckthorn (Hippophae rhamnoides L.) leaf extract on cutaneous wound healing in albino rats. Int J Low Extrem Wounds. 2005;4:88–92. doi: 10.1177/1534734605277401. [DOI] [PubMed] [Google Scholar]
- 26.Upadhyay NK, Kumar R, Siddiqui MS, Gupta A. Mechanism of wound-healing activity of hippophae rhamnoides l.leaf extract in experimental burns. Evid Based Complement Alternat Med. 2011;2011:659705. doi: 10.1093/ecam/nep189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gurung S, Skalko-Basnet N. Wound healing properties of Carica papaya latex: In vivo evaluation in mice burn model. J Ethnopharmacol. 2009;121:338–41. doi: 10.1016/j.jep.2008.10.030. [DOI] [PubMed] [Google Scholar]
- 28.Dash GK, Murthy PN. Studies on wound healing activity of heliotropium indicum linn.leaves on rats. ISRN Pharmacol. 2011;2011:847980. doi: 10.5402/2011/847980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdulla MA, Ahmed KA, Ali HM, Noor SM, Ismail S. Wound Healing Activities of Rafflesia Hasseltii Extract in Rats. J Clin Biochem Nutr. 2009;45:304–8. doi: 10.3164/jcbn.09-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (tea tree) oil: A review of antimicrobial and other medicinal properties. Clin Microbiol Rev. 2006;19:50–62. doi: 10.1128/CMR.19.1.50-62.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunford C, Cooper R, Molan P, White R. The use of honey in wound management. Nurs Stand. 2000;15:63–68. doi: 10.7748/ns2000.11.15.11.63.c2952. [DOI] [PubMed] [Google Scholar]
- 32.Grover SK, Prasad GC. Uses of Madhu in ayurveda. J NIMA. 1985;10:7–10. [Google Scholar]
- 33.Lusby PE, Coombes A, Wilkinson JM. Honey: A potent agent for wound healing? J Wound Ostomy Continence Nurs. 2002;29:295–300. doi: 10.1067/mjw.2002.129073. [DOI] [PubMed] [Google Scholar]
- 34.Namias N. Honey in the management of infections. Surg Infect (Larchmt) 2003;4:219–26. doi: 10.1089/109629603766957022. [DOI] [PubMed] [Google Scholar]
- 35.Philips CE. Honey for burns. Glean. Bee Cult. 1933;61:284. [Google Scholar]
- 36.Voigtlander N. Honey for burns and scalds. Bee World. 1937;18:128. [Google Scholar]
- 37.Cutting K. Honey and contemporary wound care: An overview. Ostomy Wound Manage. 2007;53:49–54. [PubMed] [Google Scholar]
- 38.Sato T, Miyata G. The nutraceutical benefit, part III: Honey. Nutrition. 2000;16:468–9. doi: 10.1016/s0899-9007(00)00271-9. [DOI] [PubMed] [Google Scholar]
- 39.Snowdon JA, Cliver DO. Microorganisms in honey, review article. Int J Food Microbiol. 1996;31:1–26. doi: 10.1016/0168-1605(96)00970-1. [DOI] [PubMed] [Google Scholar]
- 40.Yusof N, Ainul Hafiza AH, Rozaini MZ, Zuki AB. Development of honey hydrogel dressing for enhanced wound healing. Rad Phys Chem. 2007;76:1767–70. [Google Scholar]
- 41.Bittmann S, Luchter E, Thiel M, Kameda G, Hanano R, Längler A. Does honey have a role in paediatric wound management? Br J Nurs. 2010;19:19–24. doi: 10.12968/bjon.2010.19.Sup5.77704. [DOI] [PubMed] [Google Scholar]
- 42.Adams CJ, Boult CH, Deadman BJ, Farr JM, Grainger MN, Manley-Harris M, et al. Isolation by HPLC and characterisation of the bioactive fraction of New Zealand manuka (Leptospermum scoparium) honey. Carbohydr Res. 2008;343:651–9. doi: 10.1016/j.carres.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 43.Mavric E, Wittmann S, Barth G, Henle T. Identification and quantification of methylglyoxal as the dominant antibacterial constituent of Manuka (Leptospermum scoparium) honeys from New Zealand. Mol Nutr Food Res. 2008;52:483–9. doi: 10.1002/mnfr.200700282. [DOI] [PubMed] [Google Scholar]
- 44.Kwakman PH, Te Velde AA, de Boer L, Speijer D, Vandenbroucke- Grauls CM, Zaat SA. How honey kills bacteria. FASEB J. 2010;24:2576–82. doi: 10.1096/fj.09-150789. [DOI] [PubMed] [Google Scholar]
- 45.Molan PC. Potential of honey in the treatment of wounds and burns. Am J Clin Dermatol. 2001;2:13–9. doi: 10.2165/00128071-200102010-00003. [DOI] [PubMed] [Google Scholar]
- 46.Molan PC. Re-introducing honey in the management of wounds and ulcers–Theory and practice. Ostomy Wound Manage. 2002;48:28–40. [PubMed] [Google Scholar]
- 47.Hejase M, Bihrle R, Coogan CL. Genital Fournier's gangrene: Experience with 38 patients. Urology. 1996;47:734–9. doi: 10.1016/s0090-4295(96)80017-3. [DOI] [PubMed] [Google Scholar]
- 48.Iftikhar F, Arshad M, Rasheed F, Amraiz D, Anwar P, Gulfraz M. Effects of acacia honey on wound healing in various rat models. Phytother Res. 2010;24:583–6. doi: 10.1002/ptr.2990. [DOI] [PubMed] [Google Scholar]
- 49.Aysan E, Ayar E, Aren A, Cifter C. The role of intra-peritoneal honey administration in preventing post-operative peritoneal adhesion. Eur J Obstet Gynecol Reprod Biol. 2002;104:152–5. doi: 10.1016/s0301-2115(02)00070-2. [DOI] [PubMed] [Google Scholar]
- 50.Kwakman PH, Zaat SA. Antibacterial components of honey. IUBMB Life. 2012;64:48–55. doi: 10.1002/iub.578. [DOI] [PubMed] [Google Scholar]
- 51.Mandal MD, Mandal S. Honey: Its medicinal property and antibacterial activity. Asian Pac J Trop Med. 2011:154–60. doi: 10.1016/S2221-1691(11)60016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Badawy OF, Shafii SS, Tharwat EE, Kamal AM. Antibacterial activity of bee honey and its therapeutic usefulness against Escherichia coli O157:H7 and Salmonella typhimurium infection. Rev Sci Tech. 2004;23:1011–22. doi: 10.20506/rst.23.3.1543. [DOI] [PubMed] [Google Scholar]
- 53.Subrahmanyam M. Topical application of honey in treatment of burns. Br J Surg. 1991;78:497–8. doi: 10.1002/bjs.1800780435. [DOI] [PubMed] [Google Scholar]
- 54.Subrahmanyam M. A prospective randomised clinical and histological study of superficial burn wound healing with honey and silver sulfadiazine. Burns. 1998;24:157–61. doi: 10.1016/s0305-4179(97)00113-7. [DOI] [PubMed] [Google Scholar]
- 55.Gupta SS, Singh O, Bhagel PS, Moses S, Shukla S, Mathur RK. Honey dressing versus silver sulfadiazene dressing for wound healing in burn patients: A retrospective study. J Cutan Aesthet Surg. 2011;4:183–7. doi: 10.4103/0974-2077.91249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Subrahmanyam M. Honey impregnated gauze versus polyurethane film (OpSite) in the treatment of burns-a prospective randomised study. Br J Plast Surg. 1993;46:322–3. doi: 10.1016/0007-1226(93)90012-z. [DOI] [PubMed] [Google Scholar]
- 57.Subrahmanyam M. Honey-impregnated gauze versus amniotic membrane in the treatment of burns. Burns. 1994;20:331–3. doi: 10.1016/0305-4179(94)90061-2. [DOI] [PubMed] [Google Scholar]
- 58.Subrahmanyam M. Honey dressing for burns - an appraisal. Ann Burns Fire Disasters. 1996;9:33–5. [Google Scholar]
- 59.Subrahmanyam M. Honey dressing versus boiled potato peel in the treatment of burns: A prospective randomized study. Burns. 1996;22:491–3. doi: 10.1016/0305-4179(96)00007-1. [DOI] [PubMed] [Google Scholar]
- 60.Subrahmanyam M. Addition of antioxidants and polyethylene glycol 4000 enhances the healing property of honey in burns. Ann Burns Fire Disasters. 1996;9:93–5. [Google Scholar]
- 61.Rodzaian WS, Dorai AA, Halim AS. Treatment of partial thickness burn wounds using tualang honey, hydrofibre and silver dressings: A pilot study. JAAS. 2011;3:54–8. [Google Scholar]
- 62.Subrahmanyam M. Early tangential excision and skin grafting of moderate burns is superior to honey dressing: A prospective randomised trial. Burns. 1999;25:729–31. doi: 10.1016/s0305-4179(99)00063-7. [DOI] [PubMed] [Google Scholar]
- 63.Subrahmanyam M, Sahapure AG, Nagane NS, Bhagwat VR, Ganu JV. Effects of topical application of honey on burn wound healing. Ann Burns Fire Disasters. 2001;14:143–5. [Google Scholar]
- 64.Marshall C, Queen J, Manjooran J. Honey vs povidine iodine following toenail surgery. Wound UK. 2005;1:10–18. [Google Scholar]
- 65.McIntosh CD, Thomson CE. Honey dressing versus paraffin tulle gras following toenail surgery. J Wound Care. 2006;15:133–6. doi: 10.12968/jowc.2006.15.3.26877. [DOI] [PubMed] [Google Scholar]
- 66.Ingle R, Levin J, Polinder K. Wound healing with honey-a randomised controlled trial. S Afr Med J. 2006;96:831–5. [PubMed] [Google Scholar]
- 67.Imran FH, Dorai AA, Halim AS, Sulaiman WA. Tualang Honey Hydrogel in the treatment of Split-Skin Graft Donor Sites. JAAS. 2011;3:33–7. [Google Scholar]
- 68.Jull A, Walker N, Parag V, Molan P, Rodgers A. Honey as Adjuvant Leg Ulcer Therapy trial collaborators. Randomized clinical trial of honey impregnated dressings for venous leg ulcers. Br J Surg. 2008;95:175–82. doi: 10.1002/bjs.6059. [DOI] [PubMed] [Google Scholar]
- 69.Gethin G, Cowman S. Bacteriological changes in sloughly venous leg ulcers treated with manuka honey or hydrogel: An RCT. J Wound Care. 2008;17:241–7. doi: 10.12968/jowc.2008.17.6.29583. [DOI] [PubMed] [Google Scholar]
- 70.Weheida SM, Nagubib HH, El-Banna HM, Marzouk S. Comparing the effects of two dressing techniques on healing of low grade pressure ulcers. J Med Res Inst. 1991;12:259–78. [Google Scholar]
- 71.Al-Waili NS, Saloom KY. Effects of topical honey on postoperative wounds infections due to gram positive and gram negative bacteria following caesarean sections and hysterectomies. Eur J Med Res. 1999;4:126–30. [PubMed] [Google Scholar]
- 72.Subrahmanyam M, Ugane SP. Honey dressing beneficial in treatment of Fournier's gangrene. Indian J Surg. 2004;66:75–7. [Google Scholar]


