Abstract
Context:
Wound measurement is an important aspect of wound management. Though there are many techniques to measure wounds, most of them are either cumbersome or too expensive.
Aims:
To introduce a simple and accurate technique by which wounds can be accurately measured.
Settings and Design:
This is a comparative study of 10 patients whose wounds were measured by three techniques, i.e. ruler, graph and our technique.
Materials and Methods:
The graph method was taken as the control measurement. The extent of deviation in wound measurements with our method was compared with the standard technique. The statistical analysis used was ANOVA.
Results:
The ruler method was highly inaccurate and overestimated the wound size by nearly 50%. Our technique remained consistent and accurate with the percentage of over or underestimation being 2-4% in comparison with the graph method.
Conclusions:
This technique is simple and accurate and is an inexpensive and non-invasive method to accurately measure wounds.
KEY WORDS: Digital planimetry, photography, wound measurement
You can’t manage what you can’t measure
W. Edwards Deming
INTRODUCTION
Measurement of a wound size gives the clinician an assessment of the amount of tissue damage, helps to track the healing process and enables him to take appropriate action. It provides baseline information and helps in tracking the progress with treatment, thus helping in auditing and predicting treatment efficacy. This evaluation has further implications in terms of cost-benefit analysis. Tallman et al. proposed that pilot studies have the potential to be shortened and larger trials could use the shorter end-point of early positive healing rates as a substitute and accurate surrogate for complete healing.[1]
The wound measurement techniques available today can be divided into contact and non-contact methods. Some commonly used techniques are the Ruler method, the Graph method or planimetry,[2] Computrized planimetry,[3] Digital planimetry,[4,5] Acetate method and Sterophotogrammetry.[6] Though a variety of techniques have been described, either they are inaccurate (ruler) or too cumbersome (graph). Some like digital planimetry may be too expensive. Here we describe a simple method of measuring wounds using a clinical photo and an open source software.
MATERIALS AND METHODS
This was an evaluative comparative pilot study and included 10 patients with wounds. At first visit, an accurate measurement of the wound size was made using the graph technique as this is the current gold standard. This data served as control measurements. The measurements were done by three clinicians. They were also asked to measure the wounds using the ruler technique (maximum length and width of wound) and our technique. The tools used were a square adhesive 4 × 4 cm2 in size with 16 square grids of 1 cm2 each, an ordinary digital camera and Image J™ free open source software.
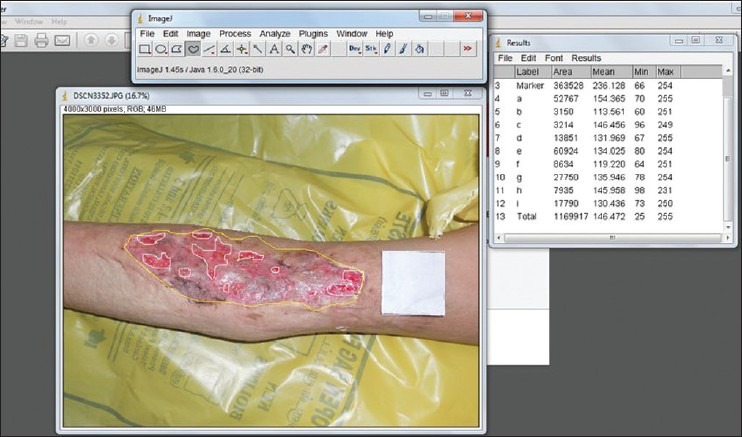
Wounds were photographed after placing the adhesive next to the wound [Figure 1]. This picture was then analysed using Image J™ as shown in Figure 2. The edges of the wound were marked and the number of pixels falling under the square adhesive marker and the marked wound were calculated. Since the dimensions of the square are known (16 cm2), it was possible to derive the exact size of the marked area of the wound [Figures 3 and 4].
Figure 1.
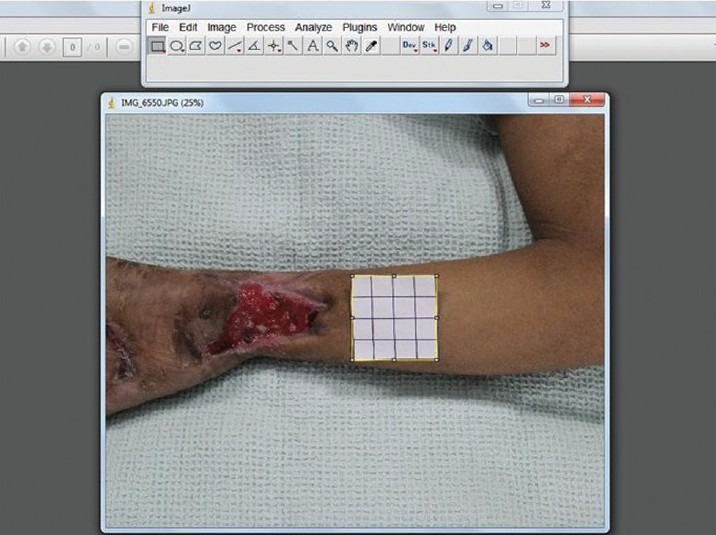
Photograph of the ulcer taken along with a 4 × 4 cm2 marker label
Figure 2.
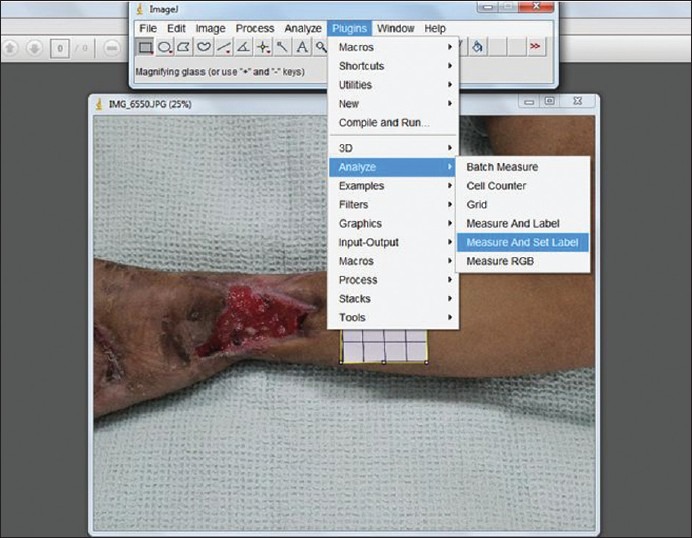
The dimensions and pixels of the marker measured with the rectangle selection, analysed and labelled
Figure 3.
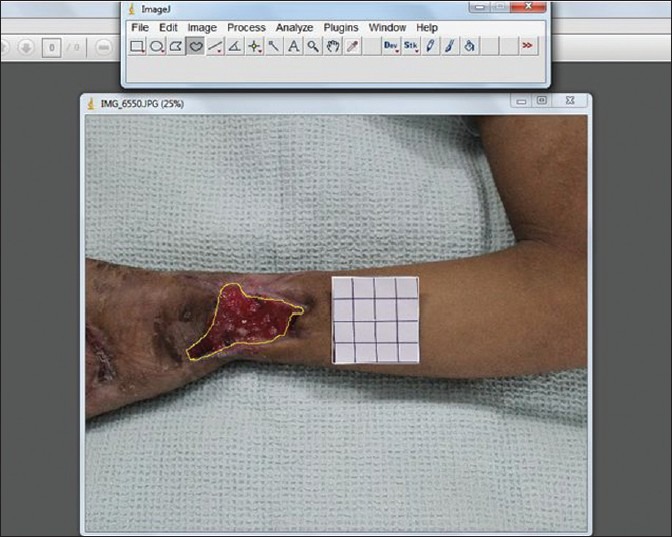
The wound edges marked with the freehand selection, analysed and labelled in a similar manner
Figure 4.
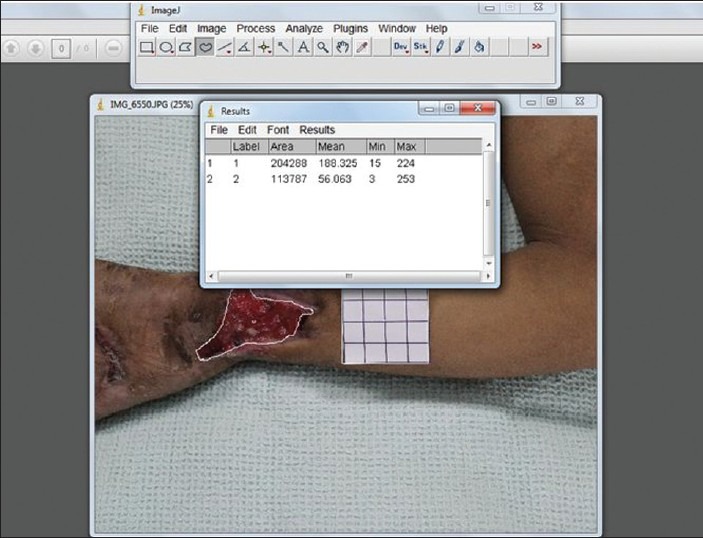
The ratio of the marker label and wound measurements give an accurate estimate of the wound size
In the case of curved wounds two parallel lines were drawn along the edge of a wound. Three photographs were then taken focusing on each of the three segments. The areas of each of the segments were then calculated as described above and then added up to give the total size of a curved wound.
A mean of the three raters’ wound surface area by the ruler and our technique was calculated. As wound surface area was calculated earlier by the graph method, the degree of overestimation or underestimation was then derived for each of the methods.
RESULTS
Of the 10 patients included in the study, nine were male. Eight of the wounds measured were on the lower limbs and one each on the upper limb and chest. All the wounds were measured initially by the graph method and compared with the ruler method and our technique. The mean of the measurements obtained from the three evaluators was used for data evaluation. The results obtained by the three techniques were tabulated and compared.
The mean area of wound as measured by the graph method was 48.92 cm2 (standard deviation 29.9342). The mean measurements with the ruler method and our technique were 48.94 cm2 (SD 29.9204) and 59.92 cm2 (SD 34.629), respectively [Figure 6]. The mean over-/under-estimation ranged from 28.9% to 42.9% with the ruler method and 1.6% to 2.4% with our technique. Statistical analysis with ANOVA showed that the difference between the three methods was not significant (P > 0.001). But there was a strong correlation between the graph method and our technique.
Figure 6.
Exact estimation of graft loss in a wound can be done by marking the wound margin and the islands of graft loss. The area of islands is then added and percentage graft loss derived
Figure 5.
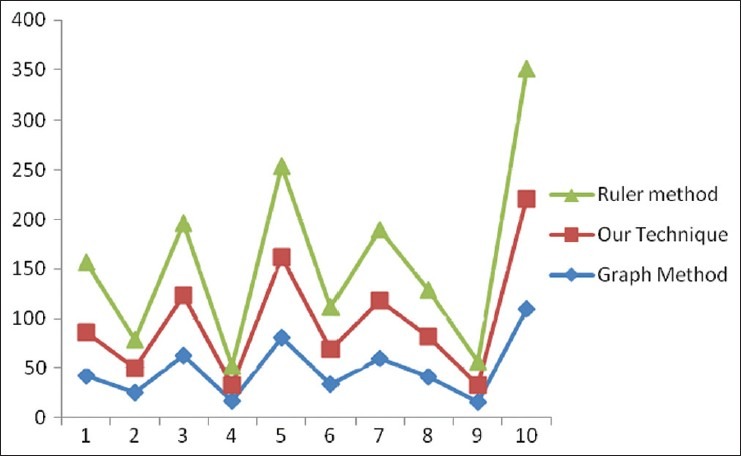
Comparison of wound measurements by the three methods
There were three wounds which had a curved surface. It was seen that results of our technique were as accurate as the graph method even on curved surfaces. The raters were not given any fixed distance to shoot the photos. Hence, there was variable distance from which the photographs were taken but the results continued to be consistent with our technique.
DISCUSSION
Wound assessment is essential to effective wound management, and wounds should be measured each time wounds are assessed.[7–9] Recording wound area and volume is considered a routine part of patient assessment and provides information on the progress of healing. It has been proposed in some studies that percentage change in wound area over a 4-week period of 30% or more is a good predictor of healing.[10,11]
Being able to predict whether wounds will heal readily with conventional treatment and deciding which patients are candidates for more radical treatment is important.[3] Continuous monitoring of changes in wound size is the key to such decision making. When wound is healing at a slower rate, it means that current wound healing strategy should be re-evaluated and adjunctive wound healing modalities should be considered. Knowing which ulcer will probably fail to heal within a 2- to 4-week period allows the clinician to consider alternative and perhaps more aggressive treatment strategies.[8] In our study, seven (70%) of the wounds were primarily skin grafted after healthy granulation tissue appeared, one (10%) had to be debrided and undergo negative pressure therapy before being grafted, and two wounds (20%) healed secondarily without surgery. Though it may not be possible to accurately predict which wounds will need grafting and which may heal secondarily, measuring the wound at regular intervals will give the clinician the percentage of decrease in wound size and with it gives him an idea as to whether the wound will heal without grafting within 2-3 weeks.
The most common method currently used to measure a wound is by a ruler.[3,12] Results of this study, and some previous studies,[3,7] demonstrate that using a ruler to measure the length and width of a wound and multiplying the two measurements together results in a wound area measurement much greater than the actual area especially for large irregular wounds. The graph method of measuring wounds is accurate but is cumbersome, labour intensive and is not feasible on an everyday basis. As with most contact techniques of wound measurement, there is also a chance of wound contamination. Both the graph method and ruler method have an additional disadvantage in which islands of epithelium may develop within a wound and this cannot be recorded in a simple measure of linear dimensions. Since the practice of taking clinical photography is high among plastic surgeons, measuring size of wounds using the clinical photography would be simple and easy.
Measuring wound size using clinical photographs is not practised routinely due to many reasons. The photographs need to be taken from a fixed distance each time to maintain uniformity and hence comparability. This method again required a tripod and can be cumbersome and time consuming. Another great disadvantage of the photographic measurement of wounds is its unreliability in the cases of wounds on curved surfaces like the limbs where it has been shown to considerably underestimate the size of the wounds. Also getting the true life size of wounds is not possible.
There have been a few studies where Image J has been used to measure wounds.[5,13,14] But they had many limitations, some of them were carried out on animal models, the calibrations were linearly done using a ‘ruler’ and calculations used were complex to name a few. These studies were also unable to find a solution for measuring a wound on a curved surface.
Some other uses of this technique maybe in estimating the amount of graft loss. Usually graft loss is measured by cursory inspection. Using our technique, we calculated the areas where there was patchy graft loss in a wound measuring approximately 6 × 7 cm2 which had been recently grafted [Figure 6]. We found the size estimation more accurate, though this technique needs further evaluation. This technique may also be used to evaluate images in a true life size. For example when an image of the face is taken, it can be enlarged based on the size of the square in the frame till a corresponding real life size image is achieved. This can be useful for facial analysis prior to surgery.
One disadvantage of our technique is its inability to give a three-dimensional volume measurement especially in cavity wounds. The measurement of cavity wounds is difficult. Cavity wounds can have a variable degree of undermining, making visualization of the area problematic. Some studies suggest that circumference measurement alone is sufficient to monitor changes in the size of cavity wounds.[10] Flanagan proposes that the healing of cavity wounds can be monitored by measuring the circumference of the wound, as this is related directly to both volume and area.[11] A study by Melhuish et al. measured area, volume and circumference of cavity wounds for a 10-week period or until the wounds had healed. In this study, the circumference of the wound was related to both the volume and area and it was concluded that a direct correlation existed between wound area and circumference and wound volume and circumference. This finding is supported by Gilman who provides evidence that it is possible to monitor wound healing accurately by measuring circumference alone.[10]
CONCLUSION
To promote high standards and evidence-based practice in wound management, the use of assessment parameters that are known to be reliable, such as wound measurement, is encouraged. Accurate wound measurement is an invaluable component for objective wound assessment. This technique is simple, non-invasive, inexpensive and is easily reproducible and assist clinicians in the treatment of wounds.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sheehan P, Jones P, Caselli A, Giurini J, Veves A. Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Diabetes Care. 2003;26:1879–82. doi: 10.2337/diacare.26.6.1879. [DOI] [PubMed] [Google Scholar]
- 2.Thomas AC, Wysocki AB. The healing wound: a comparison of three clinically useful methods of measurement. Decubitus. 1990;3:18–20. 24-25. [PubMed] [Google Scholar]
- 3.Haghpanah S, Bogie K, Wang X, Banks P, Ho CH. Reliability of electronic versus manual measurement techniques. Arch Phys Med Rehabil. 2006;87:1396–402. doi: 10.1016/j.apmr.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 4.McConnell EA. Do's and don’ts: measuring a wound. Nursing. 2000;30:12. doi: 10.1097/00152193-200030120-00004. 17. [DOI] [PubMed] [Google Scholar]
- 5.Chang AC, Dearman B, Greenwood JE. A comparison of wound area measurement techniques: Visitrak versus photography. Eplasty. 2011;11:158–66. [PMC free article] [PubMed] [Google Scholar]
- 6.Wysocki AB. Wound measurement. Int J Dermatol. 1996;35:82–91. doi: 10.1111/j.1365-4362.1996.tb03266.x. [DOI] [PubMed] [Google Scholar]
- 7.Ramirez AT, Sorof HS, Schwartz MS. Experimental wound healing in man. Surg Gynecol Obstet. 1969;128:283–93. [PubMed] [Google Scholar]
- 8.Bryant JL, Brooks TL, Schmidt B, Mostow E. Reliability of wound measuring techniques in an outpatient wound center. Ostomy Wound Manage. 2001;47:44–51. [PubMed] [Google Scholar]
- 9.Kantor J, Margolis DJ. A multicentre study of percentage change in venous leg ulcer area as a prognostic index of healing at 24 weeks. Br J Dermatol. 2000;142:960–4. doi: 10.1046/j.1365-2133.2000.03478.x. [DOI] [PubMed] [Google Scholar]
- 10.Gilman TH. Parameter for measurement of wound closure. Wounds. 1990;3:95–101. [Google Scholar]
- 11.Flanagan M. Wound measurement: can it help us to monitor progression to healing? J Wound Care. 2003;12:189–94. doi: 10.12968/jowc.2003.12.5.26493. [DOI] [PubMed] [Google Scholar]
- 12.Majeske C. Reliability of wound surface area measurements. Phys Ther. 1992;72:138–41. doi: 10.1093/ptj/72.2.138. [DOI] [PubMed] [Google Scholar]
- 13.Mayrovitz HN, Soontupe LB. Wound Areas by computerised Planimetry of digital Images. Adv Skin Wound Care. 2009;22:222–29. doi: 10.1097/01.ASW.0000350839.19477.ce. [DOI] [PubMed] [Google Scholar]
- 14.Wang Y, Liu G, Yuan N, Ran X. A comparison of digital planimetry and transparency tracing methods for measuring diabetic cutaneous ulcer surface area. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22:563–6. [PubMed] [Google Scholar]


