Abstract
Stress fractures occur following excessive use and are commonly seen in athletes, in whom the lower limbs are frequently involved. Delayed diagnosis and management of these injuries can result in significant long-term damage and athlete morbidity. A high index of suspicion may facilitate diagnosis, but clinical presentation may be non-specific. In this regard, imaging in the form of plain radiograph, CT, MRI and bone scintigraphy may be of value. This article reviews the incidence, presentation, radiological findings and management options for athletes with stress fractures of the lower limb.
Stress fractures were originally reported in 1855 by Breithaupt, a Prussian military surgeon, who observed these injuries in military recruits with foot pain following long marches [1]. Today, stress fractures of the bone resulting from excessive use are well recognised as affecting the active and athletic population. Stress fractures have been reported to account for 2% of total sports injuries in athletes [2].
Stress injuries can affect almost any bone, but the vast majority (up to 95%) affect the lower extremity. Therefore, this paper will review site-specific stress injuries of the lower extremity and pelvis.
Pathomechanics of stress injuries
Most people are familiar with the concept of structural failure of rigid materials due to repeated application of relatively minor stresses, individually well within the capacity of the material to resist. This phenomenon achieves worldwide notoriety when the aluminium components of aircraft fail in this way. The science of this failure now seems well understood, using concepts of crack propagation, cycles to failure and metal fatigue to describe it. Bone is also a rigid material that is routinely exposed to repeated application of stresses and may fail in an apparently similar fashion. Bone, however, is a living material, capable of growth, repair and remodelling in response to stress, but is also subject to disease and influences on its metabolism that will modulate the consequences of exposure to repeated stresses. The stresses to which bone is exposed will also vary widely, from the activities of daily living through repeated higher stresses, such as the training programme of an athlete, to the single major traumas that cause immediate fracture. Consequently, many terms are used to describe fractures that occur when a single major trauma has not occurred—march fracture, stress fracture, fatigue fracture, insufficiency fracture, incremental fracture, osteoporotic fracture and low-trauma fracture being the most common. Some of these terms are relatively site specific (march fracture in the metatarsal for example), and others imply a particular pathological predisposition (insufficiency fracture in osteoporosis and incremental fracture in Paget’s disease). Some are precipitated by a single episode of trauma not considered sufficient to break a normal bone and some of these fractures have been eponymously described—Colles’ fractures for example. In order to categorise fracture types using the terms already in widespread use, we suggest that definitions for some of these terms are developed that reflect the suspected underlying pathophysiological mechanisms.
Fatigue fracture could be used to describe fractures with an aetiology closest to that seen in aluminium metal fatigue, i.e. cyclical repetitive injury to a rigid structure with little or no capacity for repair. Cortical bone has the lowest rate of bone turnover and this may be further reduced in some conditions (aluminium bone disease or pyknodysostosis [3] (Figure 1) and bisphosphonate therapy are examples). Repetitive low-trauma fractures in cortical bone in these conditions are recognised—the mid-shaft transverse fracture of the femur in patients on bisphosphonates for example. In this fracture type, there may be no unusual frequency or magnitude to the precipitating stress. A painful pre-fracture state with characteristic imaging appearances has been described in this condition (Figure 2), which may be an indication for prophylactic intramedullary nailing.
Figure 1.

Incomplete chronic fatigue fracture (white arrow) of the anterior tibia in a male with pyknodysostosis.
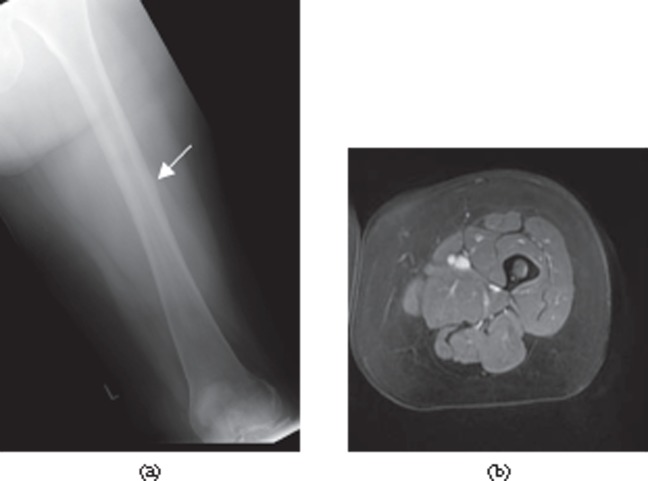
Figure 2.
Fatigue pre-fracture in a middle-aged female with breast cancer on bisphosphonate therapy. Plain radiograph (a) demonstrates focal cortical thickening on the lateral mid-shaft (white arrow). MRI axial short tau inversion–recovery image (b) shows endosteal and periosteal high signal around the focal cortical thickening.
Repetitive stresses to normal bone may also result in fracture if the magnitude of the individual stresses or the frequency of stress application exceeds the capacity of the bone to repair microfractures. This may occur from unaccustomed exercise in the non-athlete or a change in the training programme in an athlete. The bone remodelling that is needed to adapt to these altered demands requires an increase in bone turnover, the initial consequence of which is bone resorption, which paradoxically increases the risk of a fracture in the short term. In addition, the bone response is slower than that of the stressed musculature, the increased strength of which then adds to the stresses on the bones. These should be termed repetitive increased stress fractures, but this would invariably be shortened to stress fracture.
When bone is abnormally weak, owing to osteoporosis, fractures of all types will occur more easily. Fractures at sites of (normally) high trabecular bone content are particularly common in osteoporosis. When there is a single episode of identified trauma, then the term insufficiency fracture is suitable, but when fracture occurs during normal activity there may be a contribution from repetitive stress or fatigue; consequently, these terms are not exclusive and could be combined—some calcaneal fractures, for example, may be insufficiency stress fractures.
While a repetitive stress fracture in an athlete may appear to be a specific type of fracture, in practice its aetiology may also be multifactorial, particularly when the patient is a keen amateur rather than an elite athlete, or if the fracture is at a site of high trabecular bone content. Female athletes have a higher incidence of stress fractures, which may also be the result of relative insufficiency. Consideration of the mechanisms described above and a search for relevant risk factors is therefore still essential in any stress fracture.
Histological studies of stress fractures confirm that the initial response of bone to repetitive stress is increased osteoclastic activity, which is greater than the osteoblastic new bone formation, temporarily weakening the bone. With continued repetitive stress, microfractures occur and bone marrow oedema would be seen on magnetic resonance scanning. Periosteal new bone then forms and may be visible on plain radiography, but if the repetitive stress continues then full cortical fracture will ensue. This sequence can, however, be interrupted by early diagnosis and appropriate management with more rapid healing and return to pain-free training.
Imaging stress fractures
Several imaging modalities are currently being employed to aid clinicians in the diagnosis of stress fractures and to provide prognostic information. These imaging modalities are most effective when selected on the basis of a thorough history and examination.
Radiographic findings of periosteal reaction, fracture line or reactive sclerosis may not manifest until 3–4 weeks after the onset of injury; and may not be observed at all if patients alter their activity level in response to the pain.
As the earliest features on imaging are bone marrow oedema on MRI and increased activity on bone scintigraphy, these modalities are of particular value for early diagnosis, at a time when the plain radiograph is still normal. Although bone scintigraphy has high sensitivity in the diagnosis of stress injuries, it has lower specificity, since increased activity may be related to other conditions such as infection, bone infarction and neoplastic processes. MRI is favoured as it is more specific and does not impose an ionising radiation burden on the patient. Nevertheless, the differential diagnoses to consider include transient marrow oedema syndromes, Brodie’s abscess and osteoid osteoma. Consequently, targeted thin section CT may also be of value in selected cases.
Site-specific stress fractures in athletes
Stress fractures in athletes may be recurrent. Identified risk factors include running, a high weekly running mileage, morphological features of biomechanical significance (high longitudinal arch to the foot, leg length inequality and excessive forefoot varus) and menstrual irregularities in females. Tibial or fibular recurrent fractures were commonest in males, whereas females had the highest proportion of foot and ankle fractures. There is a trend towards fractures in cortical bone sites in males and in trabecular bone sites in females. Table 1 shows the percentage of site-specific lower limb and pelvic fractures, predominant sporting associations and bone type.
Table 1. Lower limb stress fractures in athletes.
| Site | Stress fractures [2,4] (%) | Predominant sporting associations | Predominant bone type |
| Metatarsals | 8.0–24.6 | Second and third metatarsal distal shaft and neck: long-distance runners | Cortical |
| Jones fracture: long-distance runners | |||
| Tarsals | 7.0–25.3 | Calcaneum: long-distance runners; jumpers | Trabecular |
| Navicular: track and field athletes; rugby and basketball players | |||
| Talus: long-distance runners; gymnasts | |||
| Tibia | 16.0–49.1 | Transverse (posterior): long-distance runners | Cortical |
| Transverse (anterior): jumpers | |||
| Longitudinal: long-distance runners | |||
| Fibula | 1.3–12.1 | Long-distance runners; jumpers | Cortical |
| Femur | 4.2–48.0 | Neck: long distance runners | Trabecular |
| Shaft: long distance runners; gymnasts | Cortical | ||
| Pelvis | 1.3–5.6 | Sacrum: long-distance runners | Trabecular |
| Apophyseal: soccer players; gymnasts | Cortical | ||
| Pubic rami: long-distance runners | Cortical |
Although upper limb injuries of this type may occur, particularly in gymnasts, the vast majority of stress fractures occur in the lower limb. Some of these fractures are prone to delayed union, non-union or displacement and require early diagnosis and more aggressive management. These include fractures of the femoral neck, anterior mid-tibia, navicular, talar body and any fracture with an intra-articular component. Conversely, fractures at low risk of complication are those in the fibula, the other tarsal bones and the distal metatarsal shaft.
Metatarsals
Stress fractures of the metatarsals account for between 9% and 24.6% of stress fractures in athletes [2,4]. These fractures were first described in military recruits as march fractures, and most often involve the neck and distal shafts of the second and third metatarsals.
Plain radiographic evaluation may reveal normal appearances. 2–3 weeks after the injury, periosteal bone reaction may be visible on radiographs. MRI has high sensitivity in the diagnosis of these fractures, depicting oedema of the bone marrow and periosteum. A hypointense fracture line may also be visible on MRI (Figure 3).
Figure 3.
Second metatarsal stress fracture. Initial plain radiograph (a) showed normal appearances apart from an incidental sessile exostosis on the first metatarsal shaft. Sagittal short tau inversion–recovery MR image (b) obtained the following day depicted marrow and periosseous soft-tissue oedema around the second metatarsal with a subtle cortical break superiorly (white arrow). Plain radiograph after 2 months (c) revealed a minimally displaced healing fracture.
These fractures are usually treated with activity modification and immobilisation with a cast or stiff-soled shoe. Most athletes can expect to return to sporting activity within 4–6 weeks [5].
Stress fractures of the fifth metatarsal base occurring approximately 1.5 cm distal to the tubercle, at the junction of the metaphysis and diaphysis (Jones’ fracture), deserve special mention as high-performance athletes with this injury may benefit from early operative intervention in the form of intramedullary screw fixation [6]. These high-risk fractures have a propensity to delayed or non-union, and refracture. It is therefore important to differentiate these fractures from the more common avulsion fractures occurring at the metatarsal tuberosity. Three radiographic appearances of a Jones’ fracture have been described: acute fractures characterised by a narrow fracture line and absence of intramedullary sclerosis (Figure 4); fractures with delayed union characterised by widening of the fracture line and evidence of intramedullary sclerosis; and fractures with non-union characterised by complete obliteration of the medullary canal by sclerotic bone [7]. Marrow oedema may be seen on MRI in the acute phase. A hypointense fracture line with or without adjacent hypointense sclerotic bone is usually evident.
Figure 4.

Jones’ fracture of the fifth metatarsal. Plain radiograph depicting a narrow fracture line distal to the tubercle without adjacent sclerosis.
Tarsals
Stress fractures affecting the tarsal bones account for 10.0–25.3% of stress fractures in athletes [2,4]. Of these, the calcaneum is the most affected, manifesting as heel pain aggravated by running and jumping and posterosuperior calcaneal tenderness on examination [8]. Plain radiographs often depict a sclerotic line at the posterosuperior aspect of the calcaneum that is parallel to the posterior cortex and perpendicular to the trabecular bone (Figure 5). Less common locations for calcaneal stress fractures are adjacent to the medial tuberosity and the anterior process. MRI can be employed to differentiate stress fractures from other pathology that may cause pain in the same region, such as Achilles tendinosis, retrocalcaneal bursitis or plantar fasciitis. A favourable response has been reported with limitation of activity for 3–6 weeks [9].
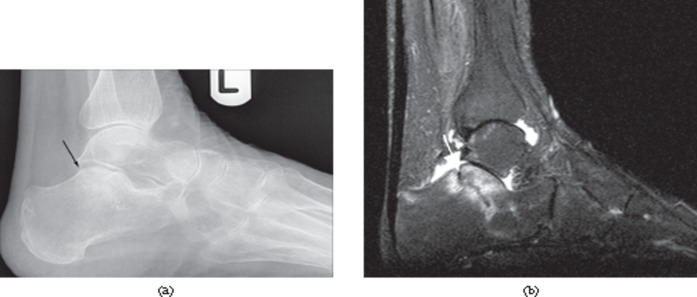
Figure 5.
Calcaneal stress fracture. Plain radiograph (a) depicts a sclerotic line traversing the posterosuperior calcaneum (black arrow), paralleling the posterior cortex. Sagittal short tau inversion–recovery magnetic resonance image (b) of the same patient demonstrates a hypointense sclerotic line (white arrow), surrounded by hyperintense marrow oedema.
Navicular stress fractures are relatively rare, accounting for up to 2.4% of all stress fractures [10]. The navicular bone is subject to impingement by adjacent metatarsals and talus. Navicular stress fractures are regarded as high-risk injuries owing to high incidence of delayed or non-union, particularly at the relatively avascular central third of the bone (Figure 6) [11].
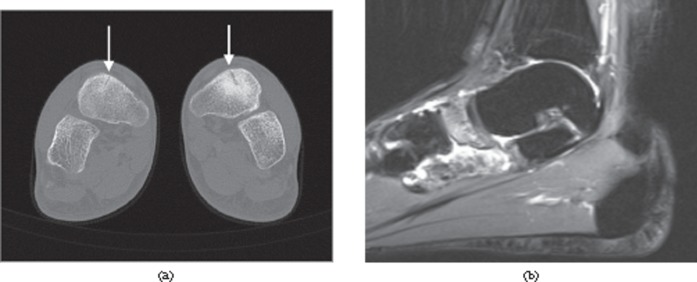
Figure 6.
Bilateral navicular stress fractures seen on CT (a, white arrows). In the acute phase, marrow oedema is evident on MRI (b). Courtesy of Dr J Healy, Chelsea and Westminster Hospital, London, UK.
As navicular stress fractures are difficult to diagnose both clinically and radiographically, a strong index of suspicion should be maintained in athletes presenting with mid-foot or arch pain. Plain radiographs often fail to depict the fracture, probably because most of these are partial fractures occurring in the sagittal plane [10]. MRI, with its higher sensitivity, is a reasonable choice for the assessment of athletes with mid-foot pain in whom navicular fracture is suspected. Presence of marrow oedema can add useful information with regards to acuity of the fracture.
Undisplaced navicular stress fractures are usually treated for 6–8 weeks with a non-weight-bearing cast. Screw fixation, with or without autologous bone grafting, is used for displaced fractures, when non-operative treatment fails or when time is of the essence [10,11].
Stress fractures of the talus are rare and have been described in long-distance runners [12] and female gymnasts [13]. These fractures have been reported to affect the talar neck [14], body [13,14] and lateral process [12]. There has been dispute about whether stress fractures of the talus should be considered as high- or low-risk stress injuries [14].
Tibia
The tibia is the most commonly involved bone, accounting for up to almost half of stress fractures reported in some series [2,4]. Tibial stress injuries include various types of bone lesions that represent a continuum of abnormalities occurring in response to abnormal repetitive stress. A study by Fredericson et al [15] described a spectrum of findings on MRI, starting with periosteal oedema, then progressing to marrow involvement and ultimately frank cortical stress fracture. Terms such as tibial stress fractures, medial tibial stress syndrome, soleus syndrome and shin splints have been used, sometimes interchangeably, to describe this continuum of stress-related injuries. The last three terms are usually used to describe stress injury without the presence of a fracture line.
These stress injuries typically affect the distal two-thirds of the posteromedial tibia of runners. Activity-related lower leg pain, along with palpation tenderness along the posteromedial edge of the tibia, is seen in tibial stress fractures and medial tibial stress syndrome [16].
Two types of tibial stress fractures have been described—transverse and longitudinal. Transverse fractures are more common and can occur on the compression side (posterior) or tension side (anterior). Posterior transverse fractures of the tibial shaft are most commonly seen in long-distance runners. Plain radiographs can be normal or depict a transverse fracture line seen perpendicular to the cortex (Figure 7). Tension stress transverse fractures of the anterior tibial shaft occur more commonly in jumpers, and have a higher propensity for non-union and progression to an acute complete fracture [16,17].
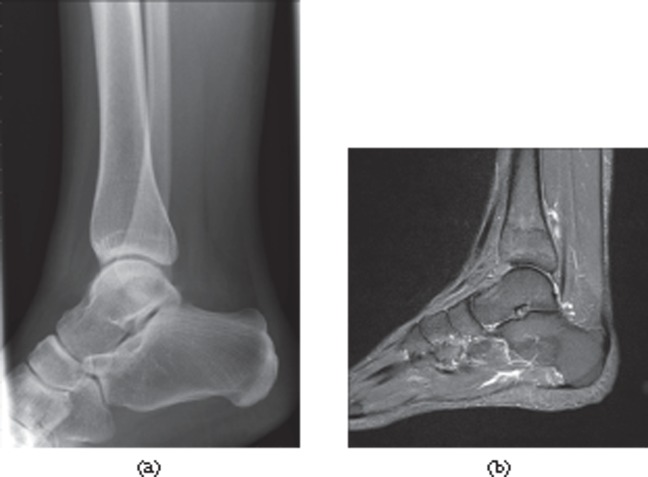
Figure 7.
Posterior tibial stress fracture. Plain radiographs (a) were reported as normal. Sagittal magnetic resonance image (b) depicts a transverse hypointense line of the posterior tibia with adjacent marrow oedema.
Longitudinal fractures account for up to 10% of tibial stress fractures [18]. Plain radiography is relatively insensitive for detecting these fractures, given the orientation of the fracture line. The X-ray beam must pass through the fracture at right angles to the cortex or tangentially across the fracture to demonstrate it. CT has played an important role in diagnosis and can depict fracture lines not visible on MRI [18,19].
Posteromedial cortex tibial stress fractures respond favourably to discontinuation of the inciting activity. Most tibial stress fractures heal within 4–8 weeks, with an average time to return to full sports of 8–12 weeks [9].
Fibula
Stress fractures of the fibula account for 1.3–12.1% of stress fractures in athletes [2,4]. These fractures were first described at the turn of the 20th century in military recruits. In 1956, the first large series describing fibular fractures in a group of 50 athletes (principally runners) was reported [20]. The most common site is the lower fibula, just proximal to the tibiotalar syndesmosis [20,21], but fractures of the proximal fibula have also been reported [22-24].
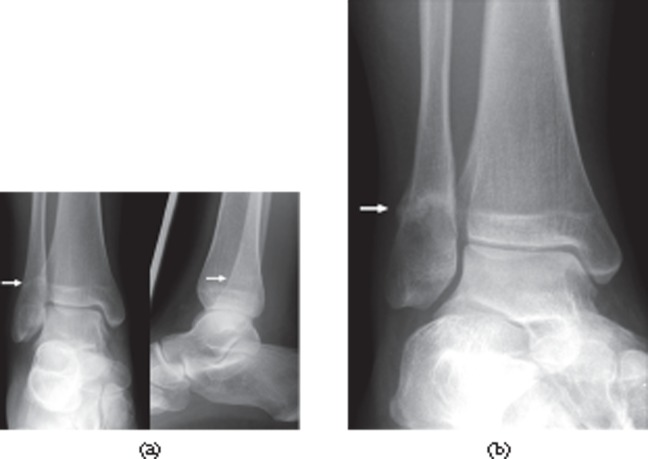
Most fibular stress fractures can be diagnosed by clinical presentation and radiographs. Palpation over the fracture site elicits pain. In the early stages, radiographic findings are subtle (Figure 8a) or absent. The earliest radiographic change is that of hazy periosteal reaction. With progression, callus or a fracture line may be visualised (Figure 8b). Stress fractures of the fibula are regarded as low-risk injuries with good prognosis when diagnosed early and treated with a 3–6 week period of rest. Without treatment, symptoms may persist for 3–6 months [9].
Figure 8.
Distal fibular stress fracture in a runner. Initial plain radiographs (a) depict subtle sclerosis and cortical break (white arrows) of the distal fibula. Subsequent plain radiograph obtained weeks later (b) depicts callus at the fracture site.
Femur
Stress fractures of the femur account for approximately 4.2–48.0% of stress fractures in athletes [2,4]. These fractures are commoner in female athletes, especially runners [25]. Annual incidence rates of 20% in young female athletes have been reported [26]. Femoral neck fractures are associated with the classic “female athlete triad” of amenorrhoea, osteoporosis and eating disorders [27,28].
Stress fractures of the femur can occur at the femoral neck or shaft. Femoral neck stress fractures are often classified as tension side (superolateral or transverse) or compression side (inferolateral), with the contention that tension side fractures are associated with poorer prognosis and are potentially unstable [29,30]. Displacement of femoral neck fractures is the main determinant of outcome, potentially leading to a reduction in the patient's activity level and complications such osteonecrosis, refractures and pseudoarthroses [31].
The femoral shaft is particularly susceptible to repetitive stresses on the medial compression side of the femur at the junction of the proximal and middle thirds. This location serves as the origin of the vastus medialis muscle and the insertion of the adductor brevis muscle, both of which have been implicated as causative factors in the development of stress fractures at this site [9,16].
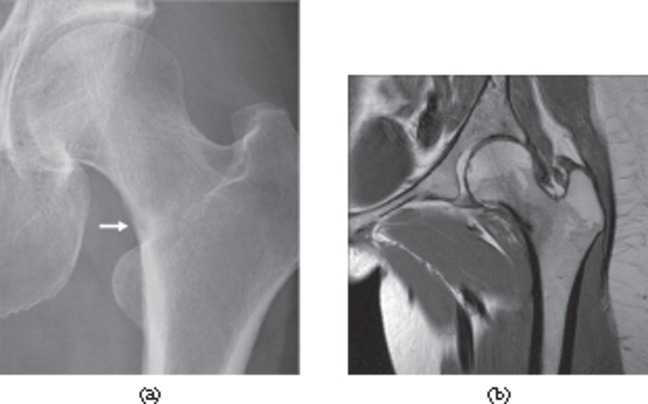
Plain radiographs in femoral stress fractures are usually normal, contributing to the delay in diagnosis. A high index of suspicion is required in an athlete presenting with insidious-onset exertional groin or thigh pain, as early diagnosis and management can prevent progression of the stress fracture into a displaced fracture. In this regard, MRI may be useful, depicting marrow oedema on the compression or tension sides of the femur and a hypointense fracture line (Figure 9).
Figure 9.
Compression side femoral stress fracture in a long-distance runner. Subtle periosteal reaction and fracture line of the inferomedial femoral neck are evident on plain radiograph (a). Coronal T1 weighted MRI (b) confirms the finding of a fracture line and adjacent marrow oedema. Courtesy of Dr C Oh, Royal Preston Hospital, Preston, UK.
Treatment of femoral stress fractures may consist initially of rest for stable, compression side injuries. Surgery may be employed to treat tension side or transverse fractures, and cases of refractory compression side fractures.
Pelvis
Stress fractures of the pelvis account for 1.3–5.6% of stress fractures seen in athletes [2,4].
Fractures of the sacrum have predominantly been described in long-distance runners, particularly females [32-35], but have also been reported in hockey players [36,37], a basketball player [38], an amateur tennis player [39] and a volleyball player [33]. Sacral stress fractures are also associated with the female athlete triad. Radiographs are of limited value owing to overlying bowel gas. More than 85% of sacral fractures are missed on plain radiographs [36]. CT may enable visualisation of a fracture line but entails radiation in a cohort of relatively young patients. MRI and single photon emission CT have both been used to evaluate patients in whom sacral fractures are suspected. Treatment usually takes the form of a period of rest [9].
In young adolescent athletes with back pain, it is important to consider spondylolysis, stress fractures of the lower lumbar vertebra (Figure 10), as an alternative diagnosis.
Figure 10.

L5 pars interarticularis defect (spondylolysis) seen on sagittal T2 weighted image in an adolescent. Courtesy of Dr C Soh, Salford Royal Hospital, Salford, UK.
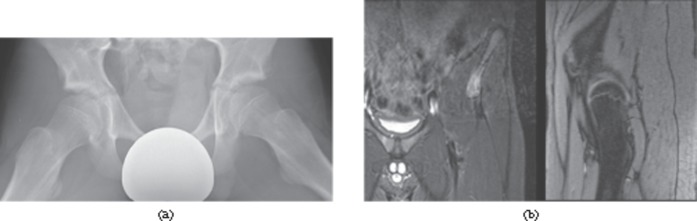
Apophyseal avulsion fractures of the pelvis in adolescent competitive athletes are seen in soccer players, gymnasts, runners and baseball players [40-42]. The lesions are usually the consequence of forceful muscle–tendon contractions during sport activities. These can occur at the ischial tuberosity, anterior inferior iliac spine (Figure 11), anterior superior iliac spine, superior corner of the pubic symphysis and the iliac crest. Plain radiographs may demonstrate separation of the apophysis or periosteal reaction. MRI has greater sensitivity and can depict marrow oedema in patients in whom radiographs are normal. These fractures are usually treated with rest and activity modification [40].
Figure 11.
Avulsion fracture of the anterior inferior iliac spine (AIIS) in an adolescent athlete. Plain radiograph (a) demonstrates subtle avulsion fracture of the AIIS. Coronal and sagittal short tau inversion–recovery images (b) depict marrow oedema of the AIIS. Courtesy of Dr R Mehan, Royal Bolton Hospital, Bolton, UK.
Stress fractures occurring at the pubic rami have been reported in runners [43,44] and Australian football players [45]. These usually occur on the inferior rami, adjacent to the symphysis pubis. Pubic rami fractures may manifest as undisplaced fracture lines on radiographs, but marrow oedema is usually evident on MRI before radiographs are positive. Stress fractures of the pubic rami have a high healing rate following 6–10 weeks of rest. There is a small risk of non-union or refracture in patients in whom an adequate rest period is not enforced [9].
Conclusion
Stress fractures are relatively common in athletes, particularly in long-distance runners. Strong clinical suspicion in concert with radiological imaging (in the form of plain radiographs, MRI, CT or bone scan) play important roles in the detection of stress injuries in athletes. Early recognition and treatment of stress fractures reduce athletic morbidity and allow timely return to high-level activity. It is therefore important for radiologists to be aware of mechanisms leading to, and locations of, stress injuries, to facilitate timely diagnosis.
References
- 1.Breithaupt ZVR. Pathologie monschuchew fusser. Med Zeittung 1855;24:169, 170–5 [Google Scholar]
- 2.Wentz L, Liu PY, Haymes E, Ilich JZ. Females have a greater incidence of stress fractures than males in both military and athletic populations: a systemic review. Mil Med 2011;176:420–30 [DOI] [PubMed] [Google Scholar]
- 3.Fratzl-Zelman N, Valenta A, Roschger P, Nader A, Gelb BD, Fratzl P, et al. Decreased bone turnover and deterioration of bone structure in two cases of pycnodysostosis. J Clin Endocrinol Metab 2004;89:1538–47 [DOI] [PubMed] [Google Scholar]
- 4.Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med 1987;15:46–58 [DOI] [PubMed] [Google Scholar]
- 5.Monteleone GP., Jr Stress fractures in the athlete. Orthop Clin North Am 1995;26:423–32 [PubMed] [Google Scholar]
- 6.Rosenberg GA, Sferra JJ. Treatment strategies for acute fractures and nonunions of the proximal fifth metatarsal. J Am Acad Orthop Surg 2000;8:332–8 [DOI] [PubMed] [Google Scholar]
- 7.Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am 1984;66:209–14 [PubMed] [Google Scholar]
- 8.Berger FH, de Jonge MC, Maas M. Stress fractures in the lower extremity. The importance of increasing awareness amongst radiologists. Eur J Radiol 2007;62:16–26 [DOI] [PubMed] [Google Scholar]
- 9.Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med 2001;29:100–11 [DOI] [PubMed] [Google Scholar]
- 10.Khan KM, Brukner PD, Kearney C, Fuller PJ, Bradshaw CJ, Kiss ZS. Tarsal navicular stress fracture in athletes. Sports Med 1994;17:65–76 [DOI] [PubMed] [Google Scholar]
- 11.Coris EE, Kaeding CC, Marymont JV. Tarsal navicular stress injuries in athletes. Orthopedics 2003;26:733–7; quiz 738–9 [DOI] [PubMed] [Google Scholar]
- 12.Black KP, Ehlert KJ. A stress fracture of the lateral process of the talus in a runner. A case report. J Bone Joint Surg Am 1994;76:441–3 [DOI] [PubMed] [Google Scholar]
- 13.Rossi F, Dragoni S. Talar body fatigue stress fractures: three cases observed in elite female gymnasts. Skeletal Radiol 2005;34:389–94 [DOI] [PubMed] [Google Scholar]
- 14.Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamaki HK. Outcomes of stress fractures of the talus. Am J Sports Med 2006;34:1809–14 [DOI] [PubMed] [Google Scholar]
- 15.Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med 1995;23:472–81 [DOI] [PubMed] [Google Scholar]
- 16.Fredericson M, Jennings F, Beaulieu C, Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging 2006;17:309–25 [DOI] [PubMed] [Google Scholar]
- 17.Brown RR, Rosenberg ZS. MR imaging of exercise-induced lower leg pain. Magn Reson Imaging Clin N Am 2001;9:533–52, x [PubMed] [Google Scholar]
- 18.Anderson MW, Ugalde V, Batt M, Greenspan A. Longitudinal stress fracture of the tibia: MR demonstration. J Comput Assist Tomogr 1996;20:836–8 [DOI] [PubMed] [Google Scholar]
- 19.Saifuddin A, Chalmers AG, Butt WP. Longitudinal stress fractures of the tibia: MRI features in two cases. Clin Radiol 1994;49:490–5 [DOI] [PubMed] [Google Scholar]
- 20.Devas MB, Sweetnam R. Stress fractures of the fibula; a review of fifty cases in athletes. J Bone Joint Surg Br 1956;38B:818–29 [DOI] [PubMed] [Google Scholar]
- 21.Burrows HJ. Fatigue fractures of the fibula. J Bone Joint Surg Br 1948;30B:266–79 [PubMed] [Google Scholar]
- 22.Blair WF, Hanley SR. Stress fracture of the proximal fibula. Am J Sports Med 1980;8:212–13 [DOI] [PubMed] [Google Scholar]
- 23.DiFiori JP. Stress fracture of the proximal fibula in a young soccer player: a case report and a review of the literature. Med Sci Sports Exerc 1999;31:925–8 [DOI] [PubMed] [Google Scholar]
- 24.Lehman TP, Belanger MJ, Pascale MS. Bilateral proximal third fibular stress fractures in an adolescent female track athlete. Orthopedics 2002;25:329–32 [DOI] [PubMed] [Google Scholar]
- 25.Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med 2001;29:521–33 [DOI] [PubMed] [Google Scholar]
- 26.Brukner P, Bennell K. Stress fractures in female athletes. Diagnosis, management and rehabilitation. Sports Med 1997;24:419–29 [DOI] [PubMed] [Google Scholar]
- 27.Kovacevic D, Mariscalco M, Goodwin RC. Injuries about the hip in the adolescent athlete. Sports Med Arthrosc 2011;19:64–74 [DOI] [PubMed] [Google Scholar]
- 28.Kang L, Belcher D, Hulstyn MJ. Stress fractures of the femoral shaft in women's college lacrosse: a report of seven cases and a review of the literature. Br J Sports Med 2005;39:902–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fullerton LR, Jr, Snowdy HA. Femoral neck stress fractures. Am J Sports Med 1988;16:365–77 [DOI] [PubMed] [Google Scholar]
- 30.Devas MB. Stress fractures of the femoral neck. J Bone Joint Surg Br 1965;47:728–38 [PubMed] [Google Scholar]
- 31.Johansson C, Ekenman I, Tornkvist H, Eriksson E. Stress fractures of the femoral neck in athletes. The consequence of a delay in diagnosis. Am J Sports Med 1990;18:524–8 [DOI] [PubMed] [Google Scholar]
- 32.Johnson AW, Weiss CB, Jr, Stento K, Wheeler DL. Stress fractures of the sacrum. An atypical cause of low back pain in the female athlete. Am J Sports Med 2001;29:498–508 [DOI] [PubMed] [Google Scholar]
- 33.Shah MK, Stewart GW. Sacral stress fractures: an unusual cause of low back pain in an athlete. Spine (Phila Pa 1976) 2002;27:E104–8 [DOI] [PubMed] [Google Scholar]
- 34.Major NM, Helms CA. Sacral stress fractures in long-distance runners. AJR Am J Roentgenol 2000;174:727–9 [DOI] [PubMed] [Google Scholar]
- 35.Fredericson M, Salamancha L, Beaulieu C. Sacral stress fractures: tracking down nonspecific pain in distance runners. Phys Sportsmed 2003;31:31–42 [DOI] [PubMed] [Google Scholar]
- 36.Southam JD, Silvis ML, Black KP. Sacral stress fracture in a professional hockey player: a case report. Orthopedics 2010;33:846. [DOI] [PubMed] [Google Scholar]
- 37.Slipman CW, Gilchrist RV, Isaac Z, Lenrow DA, Chou LH. Sacral stress fracture in a female field hockey player. Am J Phys Med Rehabil 2003;82:893–6 [DOI] [PubMed] [Google Scholar]
- 38.Crockett HC, Wright JM, Madsen MW, Bates JE, Potter HG, Warren RF. Sacral stress fracture in an elite college basketball player after the use of a jumping machine. Am J Sports Med 1999;27:526–8 [DOI] [PubMed] [Google Scholar]
- 39.Silva RT, De Bortoli A, Laurino CF, Abdalla RJ, Cohen M. Sacral stress fracture: an unusual cause of low back pain in an amateur tennis player. Br J Sports Med 2006;40:460–1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hebert KJ, Laor T, Divine JG, Emery KH, Wall EJ. MRI appearance of chronic stress injury of the iliac crest apophysis in adolescent athletes. AJR Am J Roentgenol 2008;190:1487–91 [DOI] [PubMed] [Google Scholar]
- 41.Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol 2001;30:127–31 [DOI] [PubMed] [Google Scholar]
- 42.Pisacano RM, Miller TT. Comparing sonography with MR imaging of apophyseal injuries of the pelvis in four boys. AJR Am J Roentgenol 2003;181:223–30 [DOI] [PubMed] [Google Scholar]
- 43.Noakes TD, Smith JA, Lindenberg G, Wills CE. Pelvic stress fractures in long distance runners. Am J Sports Med 1985;13:120–3 [DOI] [PubMed] [Google Scholar]
- 44.Pavlov H, Nelson TL, Warren RF, Torg JS, Burstein AH. Stress fractures of the pubic ramus. A report of twelve cases. J Bone Joint Surg Am 1982;64:1020–5 [PubMed] [Google Scholar]
- 45.Verrall GM, Henry L, Fazzalari NL, Slavotinek JP, Oakeshott RD. Bone biopsy of the parasymphyseal pubic bone region in athletes with chronic groin injury demonstrates new woven bone formation consistent with a diagnosis of pubic bone stress injury. Am J Sports Med 2008;36:2425–31 [DOI] [PubMed] [Google Scholar]