Abstract
Most vaccines available in the United States (US) have been incorporated into vaccination schedules for infants and young children, age groups particularly at risk of contracting infectious diseases. High universal vaccination coverage is responsible for substantially reducing or nearly eliminating many of the diseases that once killed thousands of children each year in the US.
Despite the success of infant vaccinations, periods of low vaccination coverage and the limited immunogenicity and duration of protection of certain vaccines have resulted in sporadic outbreaks, allowing some diseases to spread in communities. These challenges suggest that expanded vaccination coverage to younger infants and adolescents, and more immunogenic vaccines, may be needed in some instances.
This review focuses on the importance of infant immunization and explores the successes and challenges of current early childhood vaccination programs and how these lessons may be applied to other invasive diseases, such as meningococcal disease.
Keywords: immunization, pediatrics, childhood vaccinations, infants, high-risk populations, meningococcal disease, Neisseria meningitidis, Haemophilus influenzae, Streptococcus pneumoniae
Impact of Vaccines on Public Health
In the US and around the world, people are living longer as a result of advances in medical science and public health interventions. Global life expectancy increased from 48 y in 1955 to 66 y in 2000, and life expectancy in the US increased from 47 y in 1900 to 77 y in 2000.1,2 Twenty-five of the 30 y of increased life expectancy in the US population over the course of the 20th century are attributable to advances in public health.3 One of the century’s greatest and perhaps most impactful medical advances was the development and widespread use of vaccination against multiple infectious diseases.3,4 Through vaccination, endemic smallpox has been eradicated worldwide, poliomyelitis has been eliminated in the Western hemisphere, and diseases such as measles, rubella, tetanus, diphtheria and Hib, once responsible for significant morbidity and mortality in the US and other parts of the world, have been controlled.3 A 2007 study by the CDC’s National Center for Immunization and Respiratory Diseases found vaccines introduced prior to 1980, including those for poliomyelitis, diphtheria, pertussis, tetanus, measles, mumps and rubella, reduced US cases of each respective disease by > 92% and mortality by ≥ 99% (Table 1) from peak levels.5 Vaccines introduced since 1980 for hepatitis A, hepatitis B, varicella and Hib have reduced US morbidity and mortality attributable to these diseases by ≥ 80%.5
Table 1. Percent reduction in mortality from selected vaccine-preventable infectious diseases5,8,9.
| Vaccine Preventable Diseases | % Reduction Since Vaccination (average annual prevaccine vs postvaccine deaths) | Prevaccination Years to Post-Vaccination Data in 2005 |
|---|---|---|
| Pertussis |
99.2 |
1934–1943 |
| Diphtheria |
100 |
1936–1945 |
| Polio (acute) |
100 |
1941–1950 |
|
Hemophilus influenzae type b (Hib)* |
~99.6 |
1980s |
| Tetanus |
99.8 |
1947–1949 |
| Measles |
99.8 |
1953–1962 |
| Hepatitis B (acute)† |
80.2 |
1982–1991 |
|
Streptococcus pneumoniae* |
~94 |
Before 2000 |
| Meningococcal disease‡ |
N/A |
|
| Varicella |
87.6 |
1990–1994 |
| Mumps |
100 |
1963–1968 |
| Rubella | 100 | 1966–1968 |
Notes: *< 5 y of age. †Postvaccine deaths in 2006. ‡Meningococcal disease epidemiology fluctuates over time. Adapted from Roush SW, et al. JAMA. 2007; 298(18):2155–2163.
Infants and young children were and remain the target population for the majority of vaccines due to the high risk of morbidity and mortality in this population.6,7 Infectious diseases, including the now vaccine-preventable diarrheal diseases, diphtheria, measles, pertussis, and influenza, were the leading causes of death in US children at the beginning of the 20th century. However, from 1900 to 1998, with the advent of widespread, universal infant and childhood vaccination programs, the proportion of US pediatric mortality due to infectious disease decreased from 61.6% to 2%.4,7 During the first decade of the 21st century, use of the measles, polio, and diphtheria-tetanus-pertussis vaccines prevented an estimated 2.5 million deaths in children aged < 5 y around the world each year.2
Expanded vaccination coverage has been cited by public health authorities as one of the most cost-effective ways to advance global welfare.2 A 2011 economic analysis of the impact of vaccination in the US found that by vaccinating each US birth cohort with the current recommended infant and childhood immunization schedule, about 42,000 deaths and 20 million cases of disease are prevented, resulting in direct cost savings of almost $14 billion and total societal cost savings of $69 billion.1,10 According to GAVI, universal childhood vaccination of 243 million children could prevent 4 million future deaths worldwide from 2011 to 2015.11 However, the public health success of vaccines has not been without challenges. Disparities in coverage, such as those between developed and developing countries, rural and urban populations, and along racial and socioeconomic lines, remain an ongoing issue.2,12 Declines in vaccine coverage also have been attributed to parental concerns about the safety of and need for vaccines13-16 and an increase in alternative vaccination schedules (i.e., delaying doses, administration of doses at older than the recommended age, splitting up components, or refusal of certain vaccines) requested by parents as a result of these concerns.17 This is important as studies have shown inadequate vaccine coverage can leave populations vulnerable to outbreaks of disease.15,18 As advances in vaccinology allow us to create more sophisticated vaccines against an expanding list of pathogens, it is important for us to apply lessons that can be learned from the past pioneering century of vaccine development to ensure vulnerable populations are protected.
Vaccination Scheduling Decisions
Immunization schedules are primarily standardized by age group to protect the high-risk and high-incidence groups. Many factors, including disease epidemiology, the nature of the vaccine, and the age and ability of a recipient to respond to the vaccine, are used to make informed decisions regarding the optimal vaccination schedule.19 Vaccines are usually recommended based on the youngest age group at highest risk and the availability of demonstrated safety and immunogenicity data for that group.20 For example, the initiation of the pertussis vaccine is routinely recommended for infants aged 2 mo. The greatest risk of serious complications from pertussis occurs in early infancy, however, infants aged < 1 mo do not respond immunologically to the vaccine compared with older infants.19 Alternatively, some vaccines are only recommended for certain high-risk groups or only in certain areas where a disease is common. For instance, the yellow fever vaccine is recommended for persons aged ≥ 9 mo who are traveling to or living in areas at risk for transmission of the yellow fever virus, such as South America and Africa.21
The majority of the vaccines available in the US are recommended for universal/routine vaccination of all eligible infants and very young children.6 In the US in 1900, by age 2 y, infants and children had received 1 vaccine against 1 disease—smallpox. By the year 2000, children by age 2 y received vaccines against 11 diseases in 7 vaccines: diphtheria-tetanus-acellular-pertussis, MMR, inactivated polio, Hib, varicella, conjugate pneumococcal and hepatitis B vaccines (Table 2).14 In the past 10 y, vaccines for rotavirus, hepatitis A, and influenza have been added to the list of ACIP-recommended vaccines for infants and toddlers.6 Although this makes for a crowded infant immunization schedule, it is anticipated that the number of injections at any given visit will be alleviated with combination vaccines currently in development.
Table 2. Increase in vaccines over the 20th century In the US14.
| Year | Number of Vaccines | Possible Number of Injections by 2 y of Age | Possible Number of Injections at a Single Visit |
|---|---|---|---|
| 1900* |
1 |
1 |
1 |
| 1960† |
5 |
8 |
2 |
| 1980‡ |
7 |
5 |
2 |
| 2000§ | 11 | 20 | 5 |
Notes: *In 1990, children received the smallpox vaccine. †In 1960, children received the smallpox, diphtheria, tetanus, whole-cell pertussis, and polio vaccines. The diphtheria, tetanus, and whole-cell pertussis vaccines were given in combination (DTP), and the polio vaccine (inactivated) was given as a series of three injections. ‡In 1980, children received the DTP, polio and MMR vaccines. The DTP and MMR vaccines were given in combination and the polio vaccine (live, attenuated) was given by mouth. §In 2000, children received the diphtheria-tetanus-acellular-pertussis, MMR, inactivated polio, Hib, varicella, conjugate pneumococcal and hepatitis B vaccines. Reproduced with permission from Pediatrics14, Copyright © 2002 by the AAP.
Why are infants targeted? From an immunologic standpoint, this age group is particularly at risk of contracting infectious diseases. Infants have immature, or naive, immune systems, which renders them more susceptible to viral and bacterial infections.14,22,23 Moreover, although infants receive antibodies from their mother, the declining protection they confer—the degree and duration of which depends on the immunological history of the mother—also leaves infants vulnerable to infection.14,24 An example of the importance of the immunologic history of the mother and antibody transfer is the resurgence of measles in the US from 1989 through 1991, when the incidence rate in infants aged < 1 y was more than double the rate in other age groups. Many of the infants who developed infection were children of young mothers who had never been exposed to wild-type measles virus, but who had instead acquired their immunity from vaccination. Because of this lack of exposure, smaller amounts of antibody were transferred to infants, resulting in a more rapid waning of these protective antibodies. Of note, low vaccination coverage also significantly contributed to the cause of this measles resurgence.25
In the US, vaccination programs have substantially reduced the burden of vaccine-preventable infectious diseases.5 Although vaccine recommendations exist for all age groups, it is important to reiterate that infants and young children remain the principal recipients for most vaccines because of the high risk of morbidity and mortality in these young age groups.6,7,20 Universal vaccination, accomplished through routine and catch-up vaccination, is a key element of quality health care.20
Successes and Challenges of Vaccination Programs: Case Examples
Diphtheria, Tetanus, and Pertussis vaccines
Vaccines for diphtheria, tetanus, and pertussis were developed in 1923, 1927 and 1926, respectively.3 In the years preceding the development of these vaccines, approximately 176,000, 1,300 and 147,000 cases of diphtheria, tetanus and pertussis were reported annually in the US.3 The development of these individual prophylactics resulted in significant reductions in cases of and deaths from the respective diseases.25 For example, by 1945, the number of diphtheria cases had already dropped to 19,000.25 Routine use of a combined vaccine, diphtheria toxoid incorporated with tetanus toxoid and whole-cell pertussis vaccine (DTP vaccine), began in the 1940s25; with the introduction of the DTP vaccine into the childhood immunization schedule, diphtheria, tetanus, and pertussis cases declined further, and by the 1970s, approximately 200, 50 to 100, and 5,000 cases of diphtheria, tetanus and pertussis, respectively, were reported annually in the US.25 Concerns about safety of whole-cell pertussis DTP vaccines led to the development of more purified (acellular) pertussis vaccines, which are currently used in combined DTaP vaccines in the US.25
The primary vaccination schedule for DTaP in the US consists of four doses, with the fourth dose recommended to be administered to toddlers aged 15 through 18 mo. For infants and toddlers who complete primary vaccination before age 4, a fifth dose is recommended before they enter school.25 Primary DTaP vaccine coverage among young children in the US is relatively high. Between 2006 and 2010, vaccine coverage with three or more doses among children aged 19 through 35 mo was in the range of 95% to 96.2%, and coverage with four or more doses was between 83.9% and 85.2%.26 For diphtheria and tetanus, high-vaccine coverage has resulted in low numbers of reported cases. Only 5 cases of diphtheria have been reported since 2000, and an average of 31 cases of tetanus occurred annually from 2000 through 2007.25 Reported cases of diphtheria and tetanus have mostly been in patients who have either never been vaccinated or in patients who did not complete the primary series or have not received appropriate booster vaccinations.25
Despite high DTaP vaccination coverage in children, pertussis incidence has increased since the 1980s, with approximately 26,000 cases reported in 2004 in the US.25 Although the annual incidence of pertussis from 2001 to 2003 was highest in infants aged < 6 mo, there has been an age-associated shift in the proportion of cases in recent years, with adolescents (aged 11–18 y) and adults (aged ≥ 19 y) representing an increasing number of cases. In 2004 and 2005, the majority of pertussis cases occurred in these age groups.25 Waning of immunity after vaccination or natural infection has been proposed as a contributing cause of the reemergence of pertussis.27,28 Duration of immunity to pertussis infection following vaccination with DTaP or DTP has been estimated to last 4 to 12 y, and immunity following natural infection has been estimated to last 7 to 20 y.27 With the increasing incidence of pertussis infection in adolescents, the US has included an adolescent Tdap booster vaccination in the vaccination schedule.28 However, average vaccination coverage in this age group was only 55.6% and 68.7% in 2009 and 2010, respectively.29 A single dose of Tdap is also recommended for adults aged 19 through 64 y as well as adults aged ≥ 65 y who may have contact with an infant aged < 12 mo.25
MMR
Just prior to the introduction of their respective live, attenuated vaccines in 1963, 1967 and 1969, annual average reported cases of measles, mumps, and rubella/congenital rubella syndrome were 503,000, 152,000 and 48,000, respectively, in the US—although these figures are thought to represent only a fraction of the millions of cases that occurred each year.3,4,25,30 In 1971, these three vaccines were combined into the MMR vaccine that is still in use today.4 In 1983, 20 y after the measles vaccine was first licensed, only 1,497 cases of measles were reported in the US. Fewer than 200 cases of measles per year have been reported in the US since 1997.25 The number of mumps cases in the US declined from approximately 5,700 cases in 1989 to 258 cases in 2004. Since 2004, two outbreaks have occurred, one in 2006 that affected approximately 6,600 college students, and one from 2009 to 2010 that caused about 3,500 cases, mainly in the Orthodox Jewish communities in New York, although the index case was infected in the UK.25 In 2003, a record low of 7 cases of rubella were reported in the US, prompting the CDC to declare the infection no longer endemic in 2004.25
A high coverage rate is an important element in the success of the MMR vaccine in controlling disease and eliminating endemic infections. In the US, coverage in toddlers aged 19 through 35 mo for the MMR vaccine was ≥ 90% from 2006 through 2010.26 According to the CDC, the 2006 and 2009 mumps outbreaks occurred largely in settings where prolonged, close person-to-person contact facilitated disease transmission that was likely limited by high-vaccination coverage among the affected and surrounding communities.25 Most reported US rubella cases since the mid-1990s have been in Hispanic young adults born outside the country in areas where rubella vaccination is not routine.25 From 1989 to 1991, measles, which reached a low of 1,500 in 1983, experienced a resurgence in the US. In those 3 y, 9,600 to 27,800 cases were reported annually. This outbreak was largely attributed to vaccination coverage, estimated to be as low as 50% of school-aged children in the affected areas, and an increase in the susceptibility of infants to infection.25 An intensive vaccination campaign increased coverage rates in children aged 2 y from 70% in 1990 to 91% in 1997; measles cases declined dramatically to a low of 37 in 2004. However, in 2008, 140 cases of measles were reported—the highest incidence since 1996. Although 89% of these cases were imported from or associated with cases imported from outside the US, the increase was not due to an increase in imported cases, but rather an increase in transmission after the virus was imported, according to the CDC. Ninety-one percent of the reported cases in 2008 were in individuals who had not been vaccinated, and most of the cases associated with importation were in school-aged, vaccine-eligible children whose parents had chosen not to have them vaccinated for personal or religious reasons.25 Fortunately, worldwide, vaccination coverage for measles continues to increase. From 2000 to 2008, increasing coverage resulted in a 78% decrease in measles cases, preventing an estimated 12.7 million deaths.2
The importance of vaccine coverage in preventing measles outbreaks is perhaps best illustrated by the situation in the UK, where in 1998 Andrew Wakefield contended, based on research he and others published in The Lancet, that the combination MMR vaccine could be linked to autism.13,31 Whereas coverage rates for the MMR vaccine had been > 90% in 1995 and endemic transmission of the infection had been disrupted,15 after Dr Wakefield’s widely publicized assertions, MMR vaccination rates declined from 91% in 1998 to an estimated 80% overall in 2003, with even lower rates in London.13,15,18 As the MMR vaccine coverage rate dropped, there was an increase in measles outbreaks in the UK.18 A 2008 study estimated that in 2004–2005, 800,000 school children were completely unvaccinated in England, and approximately 1.3 million children aged 2 through 17 y were susceptible to measles. The study model predicted an outbreak of up to 100,000 cases could occur based on the vaccine coverage estimates.15 In early 2010, the possible link between the MMR vaccine and autism was retracted.32
Vaccinating Infants Against Infection with Encapsulated Bacteria
Studies have shown that the infant immune system is capable of generating functional T cells. Because of this, infants generally respond well to T-cell dependent antigens, including protein antigen. However, compared with older children and adults, B-cell responses are lower in infants, rendering them particularly vulnerable to polysaccharide-coated pathogens, such as the primary pathogens that cause bacterial meningitis, Hib, S. pneumoniae, and N. meningitidis, which are T-cell independent.14 In the US, vaccines for two of these pathogens, S. pneumoniae and Hib, became available in the late 1970s and mid-1980s, respectively.5,25 However, the first of these vaccines were polysaccharide-based, and because of the lower T cell–independent response in this age group, were not as immunogenic in children aged < 2 y. Subsequently, vaccines to protect infants from disease caused by these two pathogens were created through the process of conjugation, whereby the polysaccharide is bonded to a protein carrier, changing the vaccine antigen from T-cell independent to T-cell dependent, greatly improving immunogenicity.25 Routine vaccination with conjugate vaccines against these two diseases has resulted in reduced morbidity and mortality.
Hib
The most common forms of serious Hib disease are invasive pneumonia and meningitis.33 A vaccine against Hib was licensed in the US in 1985.3 Prior to the development of a targeted vaccine, these encapsulated bacterial organisms were the leading cause of bacterial meningitis and other invasive bacterial infections in children aged < 5 y.25 Young children aged < 18 mo were especially impacted by invasive Hib disease, with 60% to 70% of cases occurring in this age group.25,34 A population-based surveillance study just before vaccine licensure in the US reported the annual number of Hib cases to be approximately 20,000.3 With the development of efficacious Hib vaccines, invasive Hib disease has been virtually eliminated in the US and Canada.34 In the US, the Hib vaccination program has resulted in a > 99% reduction in invasive disease.25
Hib vaccination programs have been successful in drastically reducing invasive Hib disease likely in part due to advances in vaccine development as well as high vaccine coverage in vulnerable age groups.25,34 The first-generation Hib vaccine (HbPV), comprising the capsular PRP, was not effective in the vulnerable age group of children aged < 18 mo.25,34 Additionally, during the period of its use, vaccine coverage with HbPV was low and never reached > 35% in some areas.34 The first Hib conjugate vaccine was licensed in 1987 for use in children aged 18 mo; Hib polysaccharide conjugate vaccines feature enhanced antibody protection and elicit booster responses.25,34 From 1988 to 1990, vaccine coverage with these vaccines ranged from 20% to 70%, and incidence rates of H influenzae meningitis and invasive Hib disease began to sharply decline.34-36 In 1990, conjugate vaccines were licensed for use in children aged 15 mo as well as for children aged 2 mo.35 With vaccine coverage finally reaching an estimated 90% in 1995, incidence of invasive Hib disease in the US in 1996 and 1997 had declined by 97% since 1987.34,36
Vaccine coverage with currently licensed Hib conjugate vaccines has remained relatively high in the US. From 2006 to 2010, vaccination coverage with > 3 doses of Hib conjugate vaccines in children aged 19 through 35 mo has ranged from 83.6% to 93.4%.26 Global vaccination coverage has also increased in recent years, with the number of countries using Hib vaccine increasing from 62 to 161 from 2000 through 2009. The CDC estimated this increase in vaccine coverage has prevented approximately 130,000 deaths due to pneumonia and meningitis annually among children aged < 5 y.2
S. pneumoniae
S. pneumoniae is a major cause of pneumonia, meningitis, and sepsis, resulting in nearly 1 million childhood deaths worldwide each year.37 The first pneumococcal polysaccharide vaccine (PPSV14) was licensed in the US in 1977, although efforts to develop a pneumococcal vaccine began as early as 1911.25 In 1983, PPSV23 was licensed and replaced PPSV14.25 PPSV23, although effective in most healthy adults, resulted in poor antibody responses in children aged < 2 y, the age group with the highest rates of pneumococcal disease.25 In 2000, the first pneumococcal conjugate vaccine (PCV7), which is highly immunogenic in infants and young children, was licensed in the US.25 A large clinical trial showed that PCV7 reduced invasive disease caused by vaccine serotypes by 97%. In addition, PCV7 was able to reduce invasive disease caused by all serotypes, including those not in the vaccine, by 89%.25 Prior to the introduction of PCV7, approximately 63,000 cases of invasive pneumococcal disease occurred annually, with children aged < 5 y accounting for about 25% of cases.38 Within this age group, 80% of disease was caused by 1 of the 7 serotypes included in the vaccine.37 Following the introduction of PCV7, an estimated 211,000 pneumococcal infections and 13,000 deaths were prevented from 2000 through 2007.37 The incidence of invasive pneumococcal disease in children aged < 5 y decreased from 99 cases per 100,000 population during 1998–1999 to 21 cases per 100,000 population in 2008.25 Although incidence of disease caused by 1 of the 7 serotypes included in PCV7 declined after its introduction, an increase in cases caused by nonvaccine serotypes, especially serotype 19A, have been observed.37
A second conjugate pneumococcal vaccine (PCV13) was licensed in 2010 in the US, replacing PCV7. PCV13 is recommended for use in children aged 2 mo through 5 y.25 This vaccine added an additional 6 serotypes to those in PCV7, including serotype 19A. In 2008, a total of 61% of invasive pneumococcal disease in children aged < 5 y was caused by serotypes included in PCV13, of which 43% was caused by serotype 19A.25 In comparison, serotypes included in PCV7 were responsible for less than 2% of cases.
Vaccination coverage with the PCVs in children has increased rapidly since the introduction of PCV7. Only 9% of children born in 1999 had received at least three doses of PCV7 by the age of 24 mo, compared with 93% of children born in 2006.37 Coverage estimates have continued to increase among children aged 19 to 35 mo, with 68% receiving at least four doses of PCV in 2006, increasing to 83% in 2010.26 Coverage has also expanded globally, with 44 countries (11% of the global birth cohort) vaccinating with PCV by the end of 2009.2
Applying Historical Lessons to Invasive Meningococcal Disease
Meningococcal disease is a global problem, annually affecting > 500,000 people and leading to > 50,000 deaths.39 In the US, approximately 1,000 to 3,500 cases of meningococcal disease are reported per year (1990–2009),9 with the highest peak of incidence among young infants and a second peak of incidence in adolescents (Fig. 1).40 N meningitidis is the only bacterium that typically generates large outbreaks of bacterial meningitis,41 with the largest outbreaks typically occurring in Africa.42
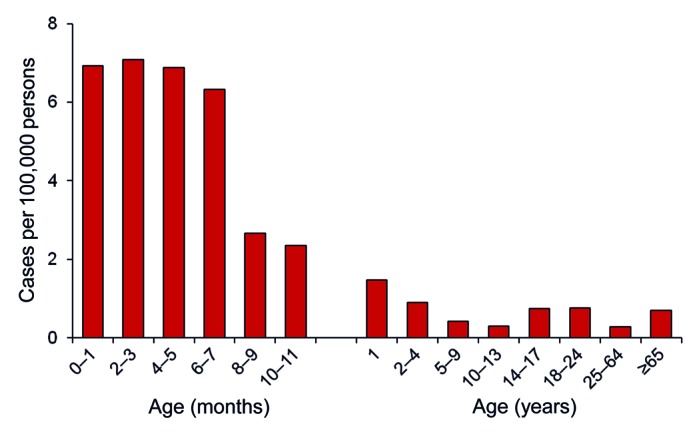
Figure 1. Estimated annual number of cases of meningococcal disease by age group (1998–2007)40
Approximately 11% to 19% of meningococcal survivors suffer permanent damage, including limb amputations, hearing loss, and neurological disabilities.43,44 Despite appropriate treatment and supportive care, the overall meningococcal disease case-fatality rate in the US is approximately 12%.40,44
Meningococcal Vaccine Development
N meningitidis is a leading cause of bacterial meningitis and sepsis; almost all invasive disease is attributable to five meningococcal serogroups: A, B, C, Y and W-135.42 In the US, there are two available quadrivalent meningococcal conjugate vaccines available against serogroups A, C, W, and Y of N meningitidis: a meningococcal diphtheria toxoid conjugate vaccine approved for persons aged 9 mo through 55 y and a meningococcal CRM197 conjugate vaccine approved for persons aged 2 through 55 y.45-47 A MPSV4 is also available.48
A Need for Meningococcal Vaccination in Infants and Early Childhood
A combined approach of immunizing the two highest-risk age groups, infants and adolescents/college students, could have a great impact by reducing morbidity and mortality from invasive meningococcal disease.49 In addition, since N. meningitidis carriage rates are highest in adolescents and young adults,50 vaccinating adolescents with a meningococcal conjugate vaccine may decrease carriage and lead to herd immunity in unimmunized populations.49 In order to maximize vaccination strategies and achieve herd immunity, coverage rates must remain high (≥ 90%) to reduce circulation of the viruses or bacteria that cause the vaccine-preventable disease. Coverage rates for currently recommended infant vaccines remain very high.26 In adolescents, meningococcal conjugate vaccination coverage has increased slowly from 11.7% in 2006 to 62.7% in 2010 and, to date, no evidence of herd immunity has been observed.29,45,51 Additionally, because infants have frequent, routinely scheduled health care visits, vaccination rates may be much more achievable in infants and young children than they are in adolescents.
MCC vaccines, implemented in both Canada and the UK, have successfully illustrated the impact that high-coverage rates, large catch-up campaigns (covering both infants and adolescents), and advantages conferred from conjugate (vs plain polysaccharide) vaccines can have on the burden of disease.
MenC
In the UK in November 1999, a national immunization program for MenC was introduced in response to a noted increase in the number of cases of serogroup C meningococcal disease. MCC vaccines were introduced into the routine immunization schedule for infants aged 2, 3 and 4 mo, with a catch-up campaign implemented for all children and adolescents aged < 18 y. Vaccine coverage was > 90% for infants and approximately 85% for children and adolescents in the catch-up group, resulting in a significant reduction in the number of serogroup C cases.52 The vaccination campaign with MCC also decreased the prevalence of carriage of meningococci that expressed serogroup C in vaccinated persons, which likely contributed to a herd effect—a 67% reduction in serogroup C disease incidence was observed in unvaccinated populations.53,54
In 2001, a mass immunization campaign, targeting persons aged 2 mo through 20 y, was implemented in Quebec, Canada, to control a serogroup C meningococcal disease outbreak.55 Vaccine coverage with a MCC vaccine in the targeted age group was 82.1%, with higher coverage in children aged 6 through 16 y compared with younger and older age groups.56 In 2002, one dose of MCC was added to the routine immunization schedule for infants aged 12 mo. Vaccine coverage increased, and by 2006, 93.4% of children had been vaccinated by age 2 y.55 After the mass immunization campaign, serogroup C disease declined significantly. In the age groups where coverage was close to or > 90% (age groups 0–4 and 5–16 y), a substantial decrease in the incidence of serogroup C disease was observed as early as 2002 compared with the poorly vaccinated (17–21 y) or unvaccinated (≥ 22 y) age groups, where incidence did not start to decline until 2003.55 There was no observed change in the incidence of serogroups B and Y.56
Challenges for Current Vaccines
Although the many advances in the field of vaccinology in the 20th century have had a dramatically positive effect on the health of populations around the world, there remains room for improvement. In addition to developing new vaccines against diseases, some important challenges concerning existing vaccines involve extending the duration of protection, expanding their use to all at-risk populations, and minimizing the risk of adverse events. Challenges also remain in the implementation of vaccine programs, particularly in improving the rates of vaccine coverage.
As evidenced by the resurgence of pertussis in US adolescents and adults, improving the duration of protection afforded by current vaccines has implications for both vaccinated populations and those who are not vaccinated. Beyond extending protection from disease in an individual, herd immunity also is improved, reducing the risk that an infant who has not yet been vaccinated or individuals who cannot be vaccinated will be exposed to a pathogen. By reducing the need for booster doses of vaccines later in life, extending the duration of protection also could profoundly improve the cost-effectiveness of vaccines, particularly of the costlier newer vaccines, and make vaccine programs easier to implement. Improving the immune response in infants also could help eliminate the need for multiple doses of vaccines, simplifying the crowded schedule in this age group. Some of the advances in molecular biology and genetic engineering, including recombinant protein production, reverse vaccinology, and reverse genetics, which are being applied to create vaccines for new target pathogens, could potentially be used to improve the immunogenicity and duration of protection of current vaccines.57,58 Recent research in immunology also could be applied to improving current vaccines in the form of adjuvants, which can increase the adaptive immune response to vaccine antigens.58
Another shortcoming of some current vaccines is their inability to be used in all at-risk populations. For example, currently, infants receive their first dose of MMR vaccine at the age of 12 mo.6 This age was decided upon at a time when many infants were born to mothers who had acquired immunity through natural exposure to the virus.59 However, most infants today are born to mothers who were vaccinated against measles, and studies have found that passive antibodies conferred to infants from mothers vaccinated against measles wane more quickly than those conferred to infants from mothers who had natural virus exposure.59,60 Unfortunately, studies have also found that infants aged < 6 mo—particularly those in whom passively acquired antibodies have waned—have much lower immune responses to the measles vaccine than older infants.60–62 Given the resurgence of measles in the wake of declining vaccination coverage, young infants represent an at-risk group for measles for which no vaccine is available. Young infants, particularly those aged < 7 mo,40 are also at increased risk for meningococcal disease. Although vaccines are available that provide protection from disease against multiple serogroups (A, C, W-135 and Y) for infants as young as age 9 mo, none are approved for use in the vulnerable population of younger infants, and none protect against disease caused by serogroup B. However, the FDA is currently reviewing an application to extend the indication for the meningococcal CRM197 conjugate vaccine to infants as young as age 2 mo. In addition, the FDA is also reviewing an application for a new vaccine to provide protection for this age group and others against serogroup B disease.
The pertussis vaccine and the oral poliovirus vaccine provide examples of the value of reexamining current vaccines in light of new research and technologies to improve their safety. Although the safety of many vaccines has been well established by their use in millions of individuals around the world, there remain risks with vaccination, including reports of sometimes severe allergic reactions and association with the autoimmune disorder, Guillain–Barré syndrome. The switch from oral to injected, inactivated polio vaccine eliminated the very rare but very real occurrence of polio vaccine-associated paralysis in children,63 and the replacement of whole-cell pertussis vaccine with acellular vaccine resulted in less frequent adverse events, including fewer seizures and hospitalizations.64 As the prevalence of disease declines due to vaccination, and the risk from disease becomes less evident to the public, the importance of minimizing vaccine adverse reactions will become more significant.
Improving Vaccine Coverage
Recently in the US, a powerful antivaccine lobby and growing antivaccination public sentiment has had a demonstrable effect on vaccination regulations and coverage levels. (Some of the most insightful analyses of the effect of antivaccine groups on public health can be found in Deadly Choices: How the Anti-Vaccine Movement Threatens Us All by Paul Offit MD, Chief of the Division of Infectious Diseases and Professor of Immunologic and Infectious Diseases at the Children’s Hospital of Philadelphia, PA.)65 Certain vaccinations are required for children entering public schools, typically against some or all of the following diseases: mumps, measles, rubella, diphtheria, pertussis, tetanus and polio.66 It is these requirements that have helped to keep vaccine coverage levels high in children. However, in 2010–2011, in 8 US states (Alaska, Colorado, Minnesota, Vermont, Washington, Oregon, Michigan, and Illinois), > 1 in 20 kindergarteners attending public school did not have all the vaccinations required for school attendance.67 Exemption rates have reached as high as 20% to 50% in certain counties such as those in northeast Washington state.67 The list of states allowing vaccine exemptions for philosophical (nonreligious) reasons grew from 15 to 20 from 2000 to 2010.67 Given the erosion of this incentive to prompt parents to have children vaccinated and the rhetoric of antivaccine groups, it becomes more important than ever for health care providers to give strong recommendations to parents to have children vaccinated. In a study of parental acceptance of human papillomavirus vaccination (for which no school requirement exists), the primary influence given by parents for vaccinating their child was health care provider recommendation.68 Some pediatricians, mindful of the risks to other patients posed by having unvaccinated children in offices and waiting rooms, have begun instituting policies requiring all patients to receive the recommended regimen of vaccines according to schedule or else they can no longer be seen by physicians in the practice.65 These pediatricians have no desire to deny health care to patients. Rather, they stress to parents the vital importance of vaccines for the health of their children and others.
Conclusions
History has shown that the introduction of safe and effective vaccines, coupled with immunization policies emphasizing universal infant immunization, has reduced disease incidence and related deaths from many serious childhood infectious diseases by more than 90%. Lessons learned from these vaccines and immunization strategies can be applied to other diseases that impose a significant burden in infants. Future vaccines may continue to focus on the newborn and infant populations, which are still vulnerable to potentially vaccine-preventable illnesses. Several prenatal and infant vaccines are currently in early clinical development for the prevention of a number of infectious diseases, including meningococcal disease [A, C, W, Y and B (currently in phase II studies)], group B streptococcus (phase II), and RSV (phase I, II). Perhaps the most important lesson learned from experience with current vaccines that can be applied to new vaccines may be the need to remove barriers to achieving and maintaining optimal coverage levels. Technology can make vaccines more immunogenic, safe, and durable and can expand the list of diseases that can be prevented. No matter how immunogenic, durable, or safe a vaccine, however, it must first be administered to protect from disease.
Acknowledgments
Writing and editorial assistance was provided by Stephanie Brewer PhD, of International Meetings and Science Inc., which was supported by Novartis Vaccines and Diagnostics. The authors retained content and editorial control throughout and received no other compensation.
Glossary
Abbreviations:
- ACIP
Advisory Committee on Immunization Practices
- CDC
Centers for Disease Control and Prevention
- CRM197
diphtheria cross-reacting material, a nontoxic variant of diphtheria toxin
- DTaP
diphtheria, tetanus and pertussis vaccine
- DTP
diphtheria, tetanus, pertussis vaccine
- FDA
Food and Drug Administration
- GAVI
(formerly) Global Alliance for Vaccines and Immunisations
- HbPV
Haemophilus B polysaccharide vaccine
- Hib
Haemophilus influenzae type b
- MCC
meningococcal C-conjugate vaccine
- MenC
meningococcal C conjugate vaccine
- MMR
measles-mumps-rubella vaccine
- MPSV4
meningococcal polysaccharide vaccine
- N meningitidis
Neisseria meningitidis
- PCV
pneumococcal conjugate vaccine
- PCV7
7-valent pneumococcal conjugate vaccine
- PCV13
13-valent pneumococcal conjugate vaccine
- PPSV14
14-valent polysaccharide vaccine
- PPSV23
23-valent polysaccharide vaccine
- PRP
polyribosyl ribitol phosphate
- RSV
respiratory syncytial virus
- S aureus
Staphylococcus aureus
- S pneumoniae
Streptococcus pneumoniae
- Tdap
combined tetanus, diphtheria and pertussis vaccine
Disclosure of Potential Conflicts of Interest
C.J.H. has received honoraria from GlaxoSmithKline and Novartis Vaccines and Diagnostics for lectures and service on advisory boards. C.M.H. has no conflicts of interest to disclose. L.O. has no conflicts of interest to disclose.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/19204
References
- 1.Centers for Disease Control and Prevention (CDC) Ten great public health achievements--United States, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60:619–23. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Ten great public health achievements--worldwide, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60:814–8. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Impact of vaccines universally recommended for children--United States, 1990-1998. MMWR Morb Mortal Wkly Rep. 1999;48:243–8. [PubMed] [Google Scholar]
- 4.Offit PA. Vaccinated: One Man’s Quest to Defeat the World’s Deadliest Diseases. Washington, DC: Smithsonian, 2007. [Google Scholar]
- 5.Roush SW, Murphy TV, Vaccine-Preventable Disease Table Working Group Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298:2155–63. doi: 10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Recommended Immunization Schedule for Persons Aged 0 Through 6 Years—United States 2011. http://www.cdc.gov/vaccines/recs/schedules/downloads/child/0-6yrs-schedule-pr.pdf. Accessed September 2, 2011.
- 7.Guyer B, Freedman MA, Strobino DM, Sondik EJ. Annual summary of vital statistics: trends in the health of Americans during the 20th century. Pediatrics. 2000;106:1307–17. doi: 10.1542/peds.106.6.1307. [DOI] [PubMed] [Google Scholar]
- 8.Advisory Committee on Immunization Practices Preventing pneumococcal disease among infants and young children. Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2000;49(RR-9):1–35. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Summary of notifiable diseases: United States, 2009. MMWR Morb Mortal Wkly Rep. 2011;58:1–100. [PubMed] [Google Scholar]
- 10.Zhou F. Updated economic evaluation of the routine childhood immunization schedule in the United States. Presented at the 45th National Immunization Conference. Washington, DC; March 28–31, 2011. [Google Scholar]
- 11.GAVI Alliance web site. http://www.gavialliance.org/about/. Accessed July 19, 2011.
- 12.Bloom DE. The value of vaccination. In Curtis N et al, eds. Hot Topics in Infection and Immunity in Children VII. Advances in Experimental Medicine and Biology, 697. New York, NY: Springer Science+Business Media, LLC, 2011; DOI: 10.1007/978-1-4419-7185-2_1. [Google Scholar]
- 13.Offit PA. Autism’s False Prophets. Bad Science, Risky Medicine, and the Search for a Cure. New York, NY: Columbia University Press, 2008. [Google Scholar]
- 14.Offit PA, Quarles J, Gerber MA, et al. Addressing parents’ concerns: do multiple vaccines overwhelm or weaken the infant’s immune system? Pediatrics. 2002;109:124–9. doi: 10.1542/peds.109.1.124. 2002. [DOI] [PubMed] [Google Scholar]
- 15.Choi YH, Gay N, Fraser G, Ramsay M. The potential for measles transmission in England. BMC Public Health. 2008;8:338. doi: 10.1186/1471-2458-8-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics. 2008;122:718–25. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- 17.Dempsey AF, Schaffer S, Singer D, Butchart A, Davis M, Freed GL. Alternative vaccination schedule preferences among parents of young children. Pediatrics. 2011;128:848–56. doi: 10.1542/peds.2011-0400. [DOI] [PubMed] [Google Scholar]
- 18.Jansen VA, Stollenwerk N, Jensen HJ, Ramsay ME, Edmunds WJ, Rhodes CJ. Measles outbreaks in a population with declining vaccine uptake. Science. 2003;301:804. doi: 10.1126/science.1086726. [DOI] [PubMed] [Google Scholar]
- 19.Atkinson WL, Pickering LK, Watson JC, Peter G. General immunization practices. In: Plotkin SA and Orenstein WA. Vaccines 4th edition. Philadelphia, PA: WB Saunders, 2004:p91. [Google Scholar]
- 20.National Center for Immunization and Respiratory Diseases General recommendations on immunization --- recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–64. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. CDC Health Information for International Travel 2012. New York, NY: Oxford University Press; 2012. [Google Scholar]
- 22.Jaspan HB, Lawn SD, Safrit JT, Bekker LG. The maturing immune system: implications for development and testing HIV-1 vaccines for children and adolescents. AIDS. 2006;20:483–94. doi: 10.1097/01.aids.0000210602.40267.60. [DOI] [PubMed] [Google Scholar]
- 23.Velilla PA, Rugeles MT, Chougnet CA. Defective antigen-presenting cell function in human neonates. Clin Immunol. 2006;121:251–9. doi: 10.1016/j.clim.2006.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zinkernagel RM. Maternal antibodies, childhood infections, and autoimmune diseases. N Engl J Med. 2001;345:1331–5. doi: 10.1056/NEJMra012493. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases. Atkinson W, Wolfe S, Hamborsky J, eds. 12th ed. Washington DC: Public Health Foundation, 2011. [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) National and state vaccination coverage among children aged 19-35 months--United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1157–63. [PubMed] [Google Scholar]
- 27.Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24(Suppl):S58–61. doi: 10.1097/01.inf.0000160914.59160.41. [DOI] [PubMed] [Google Scholar]
- 28.Zepp F, Heininger U, Mertsola J, Bernatowska E, Guiso N, Roord J, et al. Rationale for pertussis booster vaccination throughout life in Europe. Lancet Infect Dis. 2011;11:557–70. doi: 10.1016/S1473-3099(11)70007-X. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) National and state vaccination coverage among adolescents aged 13 through 17 years--United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1117–23. [PubMed] [Google Scholar]
- 30.Bloch AB, Orenstein WA, Stetler HC, Wassilak SG, Amler RW, Bart KJ, et al. Health impact of measles vaccination in the United States. Pediatrics. 1985;76:524–32. [PubMed] [Google Scholar]
- 31.Wakefield AJ, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998;351:637–41. doi: 10.1016/S0140-6736(97)11096-0. [DOI] [PubMed] [Google Scholar]
- 32.The Lancet Editors Retraction—Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 2010;375:45. doi: 10.1016/S0140-6736(10)60175-4. [DOI] [PubMed] [Google Scholar]
- 33.Watt JP, Levine OS, Santosham M. Global reduction of Hib disease: what are the next steps? Proceedings of the meeting Scottsdale, Arizona, September 22-25, 2002. J Pediatr. 2003;143(Suppl):S163–87. doi: 10.1067/S0022-3476(03)00576-6. [DOI] [PubMed] [Google Scholar]
- 34.Wenger JD. Epidemiology of Haemophilus influenzae type b disease and impact of Haemophilus influenzae type b conjugate vaccines in the United States and Canada. Pediatr Infect Dis J. 1998;17(Suppl):S132–6. doi: 10.1097/00006454-199809001-00008. [DOI] [PubMed] [Google Scholar]
- 35.Adams WG, Deaver KA, Cochi SL, Plikaytis BD, Zell ER, Broome CV, et al. Decline of childhood Haemophilus influenzae type b (Hib) disease in the Hib vaccine era. JAMA. 1993;269:221–6. doi: 10.1001/jama.1993.03500020055031. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC) Progress toward eliminating Haemophilus influenzae type b disease among infants and children--United States, 1987-1997. MMWR Morb Mortal Wkly Rep. 1998;47:993–8. [PubMed] [Google Scholar]
- 37.Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, Bennett NM, et al. Active Bacterial Core Surveillance/Emerging Infections Program Network Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis. 2010;201:32–41. doi: 10.1086/648593. [DOI] [PubMed] [Google Scholar]
- 38.Robinson KA, Baughman W, Rothrock G, Barrett NL, Pass M, Lexau C, et al. Active Bacterial Core Surveillance (ABCs)/Emerging Infections Program Network Epidemiology of invasive Streptococcus pneumoniae infections in the United States, 1995-1998: Opportunities for prevention in the conjugate vaccine era. JAMA. 2001;285:1729–35. doi: 10.1001/jama.285.13.1729. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization WHO position paper on Meningococcal vaccines. Wkly Epidemiol Rec. 2002;77:329–40. [Google Scholar]
- 40.Cohn AC, MacNeil JR, Harrison LH, Hatcher C, Theodore J, Schmidt M, et al. Changes in Neisseria meningitidis disease epidemiology in the United States, 1998-2007: implications for prevention of meningococcal disease. Clin Infect Dis. 2010;50:184–91. doi: 10.1086/649209. [DOI] [PubMed] [Google Scholar]
- 41.Girard MP, Preziosi MP, Aguado MT, Kieny MP. A review of vaccine research and development: meningococcal disease. Vaccine. 2006;24:4692–700. doi: 10.1016/j.vaccine.2006.03.034. [DOI] [PubMed] [Google Scholar]
- 42.Harrison LH, Trotter CL, Ramsay ME. Global epidemiology of meningococcal disease. Vaccine. 2009;27(Suppl):B51–63. doi: 10.1016/j.vaccine.2009.04.063. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Vaccines and Preventable Diseases. Factsheet: Meningococcal Disease and Meningococcal Vaccines (August 26, 2009). http://www.cdc.gov/vaccines/vpd-vac/mening/vac-mening-fs.htm. Accessed June 26, 2011.
- 44.Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. N Engl J Med. 2001;344:1378–88. doi: 10.1056/NEJM200105033441807. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention (CDC) Updated recommendations for use of meningococcal conjugate vaccines---Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72–6. [PubMed] [Google Scholar]
- 46.Sanofi Pasteur Inc. Menactra Prescribing Information. Swiftwater, PA. 2011. [Google Scholar]
- 47.Novartis Vaccines and Diagnostics. MENVEO Prescribing Information. March 2011.
- 48.National Center for Immunization and Respiratory Diseases General recommendations on immunization—recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–64. [PubMed] [Google Scholar]
- 49.Lingappa JR, Rosenstein N, Zell ER, Shutt KA, Schuchat A, Perkins BA, Active Bacterial Core surveillance (ABCs) team Surveillance for meningococcal disease and strategies for use of conjugate meningococcal vaccines in the United States. Vaccine. 2001;19:4566–75. doi: 10.1016/S0264-410X(01)00209-2. [DOI] [PubMed] [Google Scholar]
- 50.Christensen H, May M, Bowen L, Hickman M, Trotter CL. Meningococcal carriage by age: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:853–61. doi: 10.1016/S1473-3099(10)70251-6. [DOI] [PubMed] [Google Scholar]
- 51.Centers for Disease Control and Prevention (CDC) Vaccination coverage among adolescents aged 13-17 years—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57:1100–3. [PubMed] [Google Scholar]
- 52.Trotter CL, Andrews NJ, Kaczmarski EB, Miller E, Ramsay ME. Effectiveness of meningococcal serogroup C conjugate vaccine 4 years after introduction. Lancet. 2004;364:365–7. doi: 10.1016/S0140-6736(04)16725-1. [DOI] [PubMed] [Google Scholar]
- 53.Maiden MC, Ibarz-Pavón AB, Urwin R, Gray SJ, Andrews NJ, Clarke SC, et al. Impact of meningococcal serogroup C conjugate vaccines on carriage and herd immunity. J Infect Dis. 2008;197:737–43. doi: 10.1086/527401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramsay ME, Andrews NJ, Trotter CL, Kaczmarski EB, Miller E. Herd immunity from meningococcal serogroup C conjugate vaccination in England: database analysis. BMJ. 2003;326:365–6. doi: 10.1136/bmj.326.7385.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.De Wals P, Deceuninck G, Lefebvre B, Boulianne N, De Serres G. Effectiveness of serogroup C meningococcal conjugate vaccine: a 7-year follow-up in Quebec, Canada. Pediatr Infect Dis J. 2011;30:566–9. doi: 10.1097/INF.0b013e31820e8638. [DOI] [PubMed] [Google Scholar]
- 56.De Wals P, Deceuninck G, Boulianne N, De Serres G. Effectiveness of a mass immunization campaign using serogroup C meningococcal conjugate vaccine. JAMA. 2004;292:2491–4. doi: 10.1001/jama.292.20.2491. [DOI] [PubMed] [Google Scholar]
- 57.Plotkin SA. Vaccines: past, present and future. Nat Med. 2005;11(Suppl):S5–11. doi: 10.1038/nm1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Plotkin SA, Plotkin SL. The development of vaccines: how the past led to the future. Nat Rev Microbiol. 2011;9:889–93. doi: 10.1038/nrmicro2668. [DOI] [PubMed] [Google Scholar]
- 59.Maldonado YA, Lawrence EC, DeHovitz R, Hartzell H, Albrecht P. Early loss of passive measles antibody in infants of mothers with vaccine-induced immunity. Pediatrics. 1995;96:447–50. [PubMed] [Google Scholar]
- 60.Manikkavasagan G, Ramsay M. Protecting infants against measles in England and Wales: a review. Arch Dis Child. 2009;94:681–5. doi: 10.1136/adc.2008.149880. [DOI] [PubMed] [Google Scholar]
- 61.Gans HA, Arvin AM, Galinus J, Logan L, DeHovitz R, Maldonado Y. Deficiency of the humoral immune response to measles vaccine in infants immunized at age 6 months. JAMA. 1998;280:527–32. doi: 10.1001/jama.280.6.527. [DOI] [PubMed] [Google Scholar]
- 62.Gans HA, Yasukawa LL, Alderson A, Rinki M, DeHovitz R, Beeler J, et al. Humoral and cell-mediated immune responses to an early 2-dose measles vaccination regimen in the United States. J Infect Dis. 2004;190:83–90. doi: 10.1086/421032. [DOI] [PubMed] [Google Scholar]
- 63.WHO Consultative Group The relation between acute persisting spinal paralysis and poliomyelitis vaccine--results of a ten-year enquiry. Bull World Health Organ. 1982;60:231–42. [PMC free article] [PubMed] [Google Scholar]
- 64.Rosenthal S, Chen R, Hadler S. The safety of acellular pertussis vaccine vs whole-cell pertussis vaccine. A postmarketing assessment. Arch Pediatr Adolesc Med. 1996;150:457–60. doi: 10.1001/archpedi.1996.02170300011001. [DOI] [PubMed] [Google Scholar]
- 65.Offit PA. Deadly Choices: How the Anti-Vaccine Movement Threatens Us All. New York, NY: Basic Books, 2011. [Google Scholar]
- 66.Centers for Disease Control and Prevention. State vaccination requirements. http://www.cdc.gov/vaccines/vac-gen/laws/state-reqs.htm. Accessed December 16, 2011.
- 67.Stobbe MAP. IMPACT: More kids skip school shots in 8 states. Associated Press. November 28, 2011. http://news.yahoo.com/ap-impact-more-kids-skip-school-shots-8-085128437.html. Accessed December 16, 2011.
- 68.Davis K, Dickman ED, Ferris D, Dias JK. Human papillomavirus vaccine acceptability among parents of 10- to 15-year-old adolescents. J Low Genit Tract Dis. 2004;8:188–94. doi: 10.1097/00128360-200407000-00005. [DOI] [PubMed] [Google Scholar]


