Abstract
PURPOSE
An informed decision to accept a health care intervention requires an understanding of its likely benefit. This study assessed participants' estimates of the benefit, as well as minimum acceptable benefit, of screening for breast and bowel cancer and medication to prevent hip fracture and cardiovascular disease.
METHODS
Three general practitioners sent questionnaires to all registered patients aged 50 to 70 years. Patients agreeing to participate in the study were asked to estimate the number of events (fractures or deaths) prevented in a group of 5,000 patients undergoing each intervention over a period of 10 years, and to indicate the minimum number of events avoided by the intervention that they considered justified its use. The proportions of participants that overestimated each intervention's benefit were calculated, and univariate and multivariable analyses of predictors of response were performed.
RESULTS
The participation rate was 36%: 977 patients were invited to participate in the study, and 354 returned a completed questionnaire. Participants overestimated the degree of benefit conferred by all interventions: 90% of participants overestimated the effect of breast cancer screening, 94% overestimated the effect of bowel cancer screening, 82% overestimated the effect of hip fracture preventive medication, and 69% overestimated the effect of preventive medication for cardiovascular disease. Estimates of minimum acceptable benefit were more conservative, but other than for cardiovascular disease mortality prevention, most respondents indicated a minimum benefit greater than these interventions achieve. A lower level of education was associated with higher estimates of minimum acceptable benefit for all interventions.
CONCLUSION
Patients overestimated the risk reduction achieved with 4 examples of screening and preventive medications. A lower level of education was associated with higher minimum benefit to justify intervention use. This tendency to overestimate benefits may affect patients' decisions to use such interventions, and practitioners should be aware of this tendency when discussing these interventions with patients.
Key words: cancer screening, coronary artery disease, osteoporosis, health promotion, atherosclerosis/prevention & control, bone loss/prevention & control
INTRODUCTION
General practitioners are encouraged to recommend screening and preventive interventions to their patients by professional guidelines, expert opinion and incentive payments.1,2 Patients are also directly encouraged to participate in a range of national screening programs. Many of these interventions have well-established benefits, but the absolute risk reductions they confer are typically small, requiring large numbers of well people to engage in them to achieve a benefit. To make an informed decision to accept such an intervention requires an individual to balance the intervention's potential benefits and harms, which requires an appreciation of the magnitude of the intervention's benefits.
Patients' expectations may exceed the established reduction in adverse outcomes achieved with breast cancer screening3-5 and with medication for cardiovascular disease prevention,6-8 but there is little, if any, information on patients' expectations of the benefit of bowel cancer screening and of treatments that reduce the risk of fracture.
New Zealand has a well-developed primary care system with a high uptake of preventive interventions. For example, a recent review of the national mammography screening program found that 66% of eligible women had attended for screening in the preceding 2 years.9 In the first quarter of 2010 in the Canterbury region (the region studied in this report), 20% of those aged 50 years and older received a prescription for a statin, and 4% of people in this age-group received a prescription for a bisphosphonate (Paul Bridgford, Pegasus Health, e-mail communication, March 17, 2011). New Zealand patients' expectations of the benefit of preventive interventions are unknown.
This study sought to quantify patients' expectations of 2 screening programs, one (breast cancer screening) already offered and another (bowel cancer screening) that is currently being piloted in another region of New Zealand.10 We also examined patients' expectations of preventive medications for cardiovascular disease and hip fracture. For all interventions, we presented participants with a range of possible absolute risk reductions. We also sought to determine the minimum acceptable benefit that participants considered would justify their use of these interventions.
METHODS
Three general practitioners in Christchurch, New Zealand, took part in the study. All patients aged 50 to 70 years registered with these doctors were eligible to participate. A paper questionnaire was developed to assess the patients' expectations of the benefits of 4 preventive interventions. The doctors mailed study information, consent forms, and questionnaires to these patients. Patients agreeing to participate were asked to complete the questionnaire and accompanying consent form and return them in a prepaid envelope. No follow-up was made for nonresponders. Ethical approval was granted by the Upper South B Regional Ethics Committee, ethics reference number URB/10/EXP/031. The study was conducted from December 2010 to January 2011.
For each intervention, the questionnaire presented participants with a scenario of 5,000 people aged 50 to 70 years undergoing the intervention for 10 years. In the case of breast cancer screening, participants were asked to consider 5,000 women undergoing screening, but for the other interventions sex was not specified. Specific screening modalities or medications were not suggested. For each intervention, participants were asked to select from 1, 5, 50, 100, 500, or 1,000 deaths or fractures they believed would be avoided. They were then asked to choose from the same list of options to indicate the minimum number of events avoided for each intervention (lives saved or hip fractures prevented) that they considered justified accepting the intervention (Supplemental Appendix, available at http://annfammed.org/content/10/6/495/suppl/DC1).
Data Management and Statistical Analysis
Results from the participants' completed questionnaires were entered into a Microsoft Access database. SAS 9.2 (SAS Institute Inc) was used for most analyses (http://www.sas.com), although confidence intervals around proportions were calculated from OpenEpi (Open Source Epidemiologic Statistics for Public Health; http://www.openepi.com), using mid P values. The proportion of participants that overestimated the benefit of each intervention was calculated. Similarly, proportions were calculated for overestimation of the minimum acceptable benefit for each intervention, relative to the benefit that the intervention actually achieves. The associations between sociodemographic characteristics, participants' experience of screening for or diagnosis of the relevant conditions, and responses were calculated over the full range of possible responses, using ordinal logistic regression with cumulative odds. Univariate associations were investigated first, and then multivariable models were carried out. Results were considered statistically significant at P = .05.
Actual Benefits of Interventions
Breast Cancer Screening
Estimates of breast cancer mortality reduction with 10 years of screening range from 1 death avoided for every 337 women screened to 1 death avoided for every 2,500.11-14 For the example in the questionnaire, the correct range of number of deaths avoided would therefore be 2 to 15. We considered estimates of 1 or 5 as being correct and 50, 100, 500 or 1,000 to be overestimates.
Bowel Cancer Screening
Bowel cancer screening using fecal occult blood testing (FOB) reduces bowel cancer mortality15 The absolute reduction in bowel cancer mortality with FOB screening is 1 to 2 deaths avoided per 1,000 people screened over 10 years.16,17 For the example in the questionnaire, the correct range of number of deaths avoided would therefore be 5 to 10. We considered answers of 5 to be correct, 1 to be an underestimate, and 50, 100, 500 or 1,000 to be overestimates.
Hip Fracture Prevention
Alendronate achieves a 53% relative risk reduction for hip fracture among those at high risk of fracture.18 There is little evidence for the benefit of bisphosphonates beyond 5 years of use, but 1 study that examined use up to 10 years found no significant difference in risk between those treated for 5 and 10 years.19 The average 10-year hip fracture risk for a 60-year-old woman has been calculated as 2.3%.20 If we assume this risk for the hypothetical group of 5,000 people treated for 10 years, then the number of fractures we would expect to avoid would be 54. We considered 50 to be the correct answer, 1 or 5 to be an underestimate, and 100, 500 or 1,000 to be overestimates.
Cardiovascular Disease Prevention
Treatment of hypertension and hyperlipidemia in primary prevention of cardiovascular disease reduces morbidity and mortality.21-23 Antihypertensive medications achieve a 13% relative reduction in mortality,21 and statins achieve relative reductions in mortality of 12% to 17% (absolute reductions of 0.15 to 0.17 deaths per 100 per year).22,23 For the example in the questionnaire, the correct range of number of deaths avoided would be 75 to 85. We considered 50 or 100 to be correct answers, 1 or 5 to be underestimates, and 500 or 1,000 to be overestimates.
RESULTS
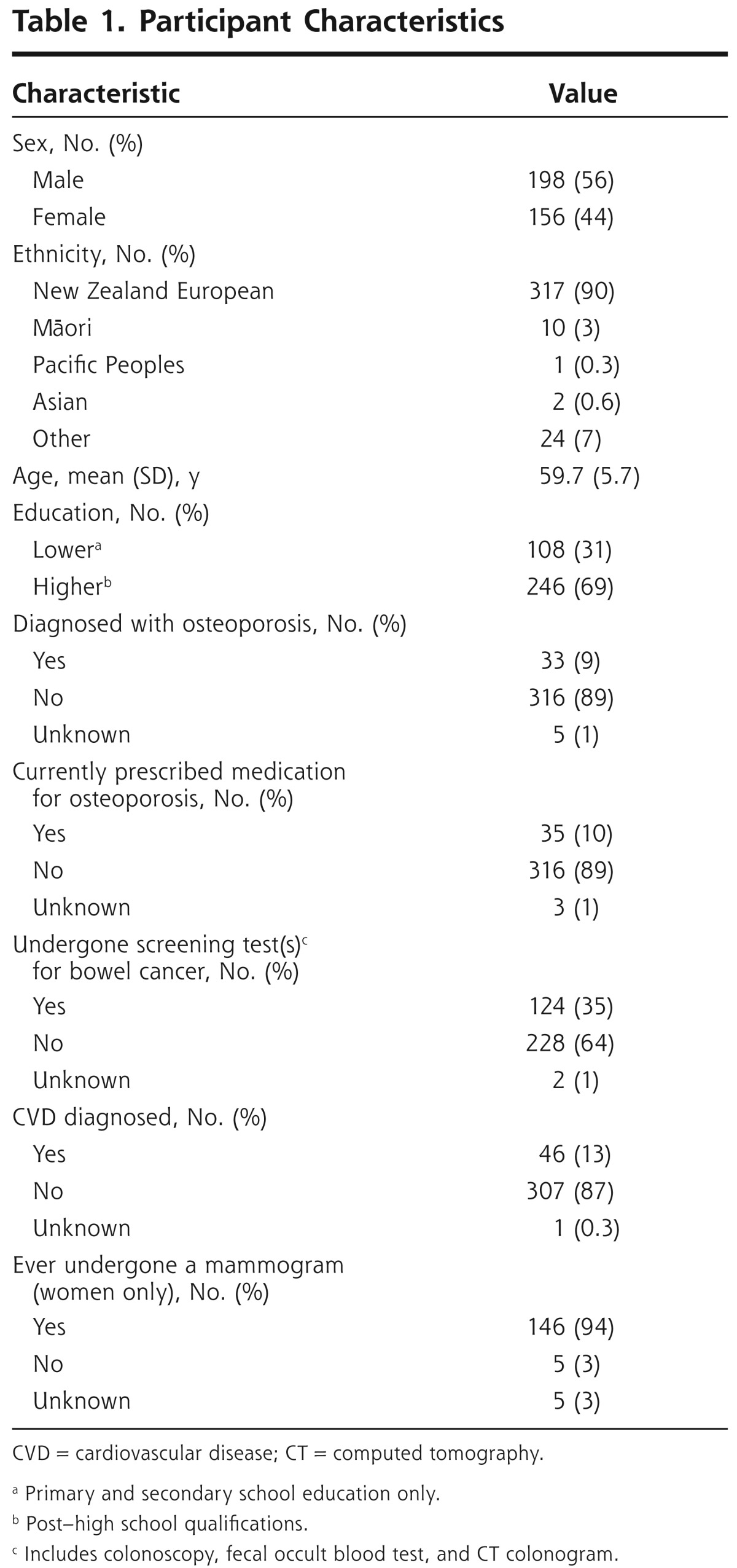
We received 354 completed questionnaires from the 977 patients invited to participate, a participation rate of 36%. Participants' mean age was 59.7 years, 56% were male, and 69% had post–high school educational qualifications compared with 40% in the 2006 New Zealand census.24 Among our participants, 90% identified themselves as New Zealand European, 3% as Māori, 0.6% as Asian, and 0.3% as Pacific Peoples; 7% listed other (which may include Europeans not born in New Zealand). By comparison, ethnicity data for patients aged 50 to 70 years enrolled with these doctors were European 91%, Māori 5%, Asian 2%, and Pacific Peoples 0.2%, which was similar to that for all patients enrolled in the Canterbury District (European 89%, Māori 4%, Asian 4%, and Pacific Peoples 2%) (Paul Bridgford, Pegasus Health, e-mail communication, May 1, 2012). Participant characteristics are shown in Table 1.
Table 1. Participant Characteristics.
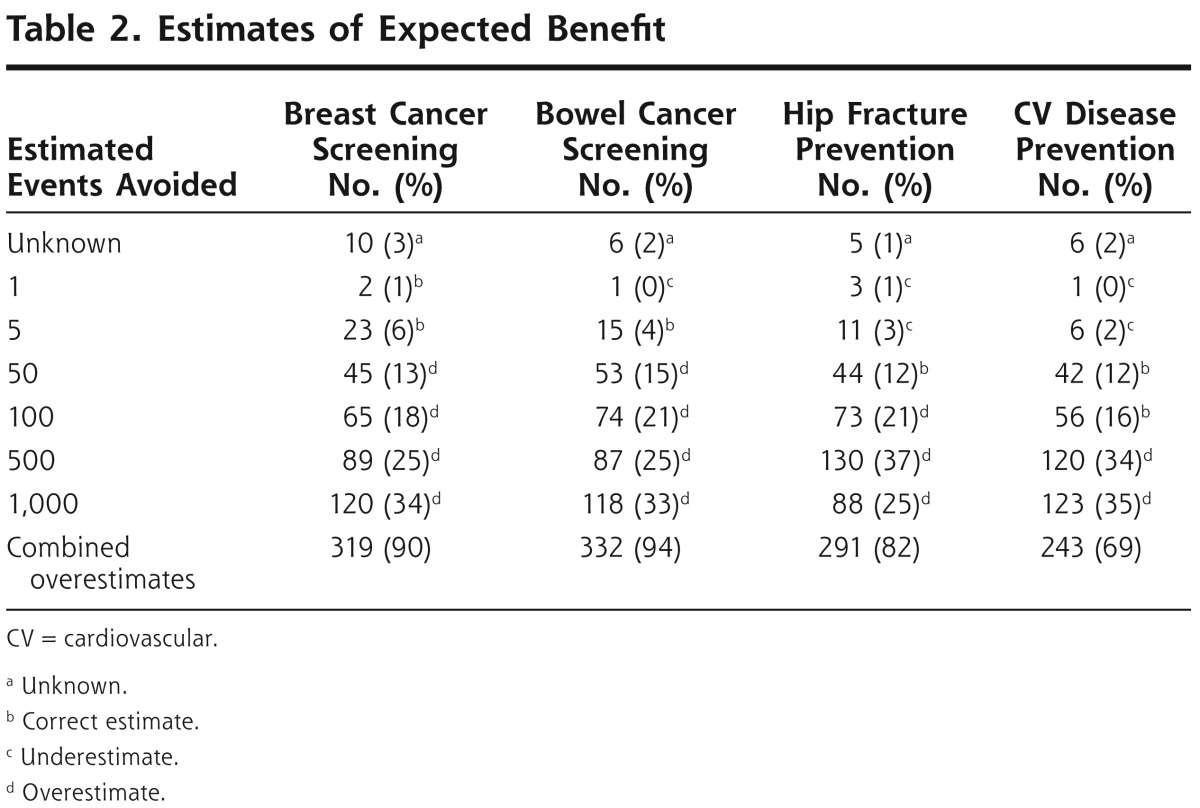
Estimates of Expected Benefit
Most participants overestimated the benefit of all interventions (Table 2). The associations between sociodemographic characteristics with past experience of screening for or history of disease and responses were calculated over the full range of possible responses, using ordinal logistic regression with cumulative odds. Multivariable models were constructed with predictors for estimation of benefit (Table 3). A lower level of education was a significant predictor for overestimating the benefit of breast cancer with bowel cancer screening and for cardiovascular disease prevention.
Table 2. Estimates of Expected Benefit.
Table 3. Predictors of Overestimating Expected Benefit.
| Predictor | Breast Cancer Screening | Bowel Cancer Screening | Hip Fracture Prevention | CVD Prevention | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| % (95% CI) | ORa (95% CI) | % (95% CI) | ORa (95% CI) | % (95% CI) | ORa (95% CI) | % (95% CI) | ORa (95% CI) | |
| Age, y | ||||||||
| 50-54 | 86 (77-92) | 0.6 (0.3-1.0) | 89 (81-95) | 0.6 (0.3-1.0) | 80 (71-88) | 1.2 (0.7-2.2) | 70 (59-79) | 0.7 (0.4-1.3) |
| 55-59 | 90 (82-95) | 0.6 (0.3-1.1) | 95 (88-98) | 0.5 (0.3-0.8) | 83 (73-90) | 1.0 (0.6-1.8) | 62 (51-72) | 0.5 (0.3-1.0) |
| 60-64 | 98 (93-100) | 0.9 (0.5-1.6) | 98 (93-100) | 0.7 (0.4-1.3) | 87 (79-92) | 1.3 (0.7-2.2) | 75 (66-83) | 0.9 (0.5-1.7) |
| 65-70 | 95 (88-98) | 1.0 | 100 (96-100) | 1.0 | 82 (72-89) | 1.0 | 74 (63-83) | 1.0 |
| P value | .12 | .05 | .73 | .13 | ||||
| Sex | ||||||||
| Male | 92 (88-95) | 1.0 | 94 (90-97) | 1.0 | 83 (78-88) | 1.0 | 67 (60-73) | 1.0 |
| Female | 93 (89-97) | 1.0 (0.7-1.6) | 97 (93-99) | 1.5 (1.0-2.2) | 84 (77-89) | 1.0 (0.7-1.6) | 73 (66-80) | 1.3 (0.9-2.0) |
| P valueb | .81 | .058 | .84 | .18 | ||||
| Educationc | ||||||||
| Lower | 97 (93-99) | 1.0 | 98 (94-100) | 1.0 | 86 (79-92) | 1.0 | 78 (69-85) | 1.0 |
| Higher | 91 (87-94) | 0.6 (0.4-1.0) | 94 (91-97) | 0.5 (0.3-0.8) | 82 (77-87) | 0.8 (0.5-1.1) | 66 (60-72) | 0.6 (0.4-0.9) |
| P valued | .03 | .002 | .19 | .026 | ||||
| Past experiencee | ||||||||
| No | – | – | 96 (93-98) | 1.0 (0.6-1.4) | 84 (79-98) | 0.9 (0.5-1.7) | 69 (64-74) | 1.0 (0.6-1.8) |
| Yes | – | – | 94 (89-97) | 1.0 | 80 (66-90) | 1.0 | 76 (61-86) | 1.0 |
| P valued | – | .85 | .82 | .98 | ||||
CVD = cardiovascular disease; OR = odds ratio.
OR calculated from multivariable logistic regression with the proportional odds assumption, across all response levels excluding unknown. OR >1.0 indicates higher estimates of effectiveness.
df = 3.
df = 1.
Lower = primary or secondary school only. Higher = post-school qualification.
Prior bowel cancer screening, diagnosis of osteoporosis or current medication for osteoporosis, and history of vascular disease. Breast cancer screening—only 5 women had never been screened so not included in the mode.
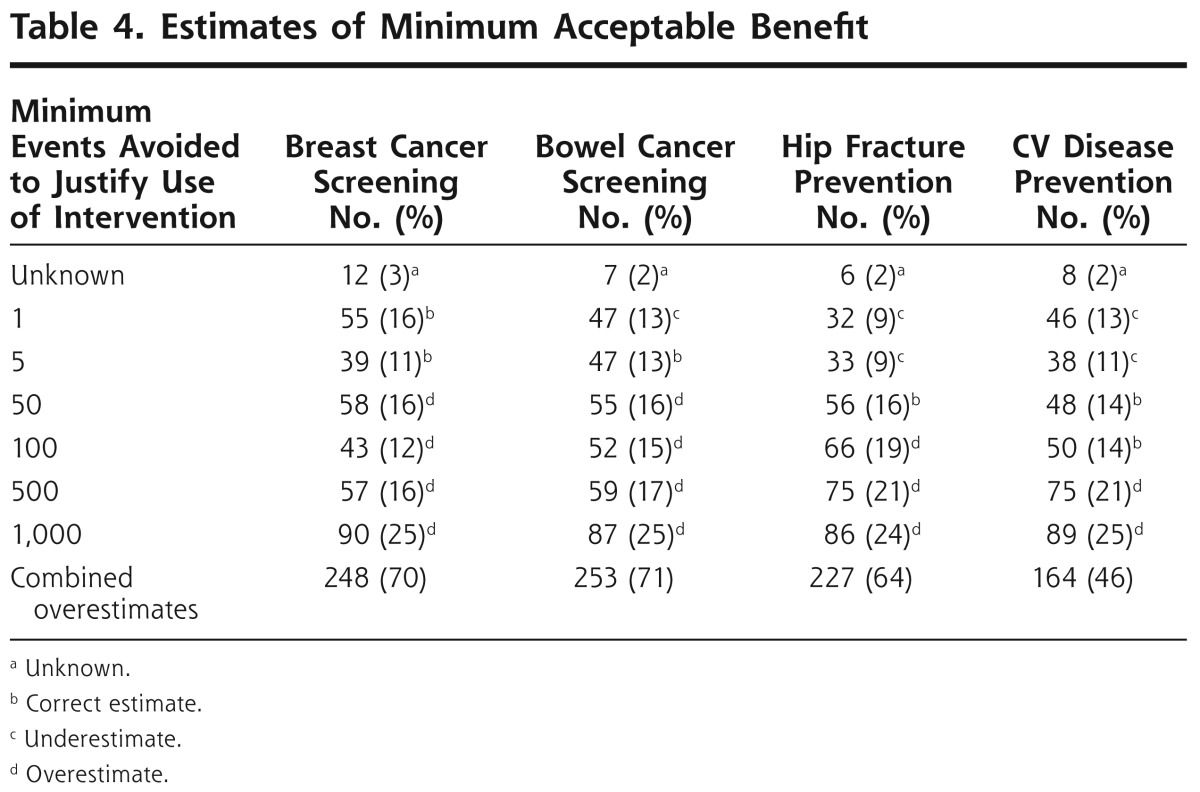
Minimum Acceptable Benefit
Participants were asked to indicate the minimum number of lives saved or hip fractures prevented that they considered justified the use of each intervention. These estimates were more conservative than the estimates of the expected benefit of the interventions, but most participants indicated a minimum acceptable benefit greater than that actually achieved for all interventions other than for cardiovascular disease prevention (Table 4).
Table 4. Estimates of Minimum Acceptable Benefit.
The associations between sociodemographic characteristics and past experience of screening for or history of disease and responses were calculated over the full range of possible responses, using ordinal logistic regression with cumulative odds. Multivariable models were constructed with predictors for estimation of minimum level of acceptable benefit (Table 5). A lower level of education was a significant predictor for indicating a higher level for minimum acceptable benefit for all interventions (P <.001). Increasing age was associated with indicating a greater minimum acceptable benefit for breast (P <.001) and bowel (P = .001) cancer screening and cardiovascular disease prevention (P = .006).
Table 5. Predictors of Overestimating Minimum Acceptable Benefit.
| Predictor | Breast Cancer Screening | Bowel Cancer Screening | Hip Fracture Prevention | CVD Prevention | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| % (95% CI) | ORa (95% CI) | % (95% CI) | ORa (95% CI) | % (95% CI) | ORa (95% CI) | % (95% CI) | ORa (95% CI) | |
| Age, y | ||||||||
| 50-54 | 58 (46-68) | 0.4 (0.2-0.7) | 56 (45-66) | 0.4 (0.2-0.7) | 52 (42-63) | 0.7 (0.4-1.2) | 28 (19-39) | 0.5 (0.3-0.9) |
| 55-59 | 71 (60-80) | 0.8 (0.4-1.3) | 70 (59-79) | 0.7 (0.4-1.3) | 64 (53-74) | 1.0 (0.6-1.8) | 48 (37-58) | 1.0 (0.6-1.8) |
| 60-64 | 81 (72-88) | 1.5 (0.9-2.5) | 84 (75-90) | 1.2 (0.7-2.0) | 71 (62-79) | 1.3 (0.7-2.2) | 59 (49-69) | 1.3 (0.8-2.3) |
| 65-70 | 78 (68-86) | 1.0 | 79 (69-87) | 1.0 | 71 (61-81) | 1.0 | 51 (40-62) | 1.0 |
| P valueb | <.0001 | .0006 | .11 | .006 | ||||
| Sex | ||||||||
| Male | 68 (61-74) | 1.0 | 70 (64-76) | 1.0 | 63 (56-69) | 1.0 | 42 (35-49) | 1.0 |
| Female | 78 (71-84) | 1.4 (0.9-2.0) | 78 (70-84) | 1.4 (1.0-2.1) | 68 (61-75) | 1.3(0.9-2.0) | 54 (46-62) | 1.6 (1.1-2.3) |
| P valuec | .12 | .081 | .16 | .022 | ||||
| Educationd | ||||||||
| Lower | 84 (76-90) | 1.0 | 86 (79-92) | 1.0 | 82 (74-89) | 1.0 | 67 (58-76) | 1.0 |
| Higher | 67 (61-73) | 0.4 (0.2-0.6) | 67 (61-73) | 0.4 (0.2-0.5) | 54 (48-60) | 0.4 (0.3-0.7) | 38 (32-45) | 0.4 (0.3-0.5) |
| P valuec | <.0001 | <.0001 | .0001 | <.0001 | ||||
| Past experiencee | ||||||||
| No | – | – | 73 (67-78) | 0.8 (0.5-1.2) | 65 (60-71) | 1.0 (0.5-1.8) | 48 (42-53) | 1.0 (0.6-1.8) |
| Yes | – | – | 73 (64-80) | 1.0 | 62 (47-75) | 1.0 | 47 (33-61) | 1.0 |
| P valuec | – | .3 | .93 | .95 | ||||
VD = cardiovascular disease; OR = odds ratio.
OR calculated from multivariable logistic regression with the proportional odds assumption, across all response levels excluding unknown. OR >1.0 indicates higher estimates of benefit.
df = 3.
df = 1.
Lower = primary or secondary school only. Higher = post-school qualification.
Prior bowel cancer screening, diagnosis of osteoporosis or current medication for osteoporosis, and history of vascular disease. Breast cancer screening—only 5 women had never been screened so not included in the mode.
DISCUSSION
Participants overestimated the benefits of all interventions. Estimates of minimum acceptable benefit were more conservative, but most exceeded the benefit actually achieved with any of the interventions other than cardiovascular disease prevention. A lower level of education was associated with higher estimates of the benefit of all interventions, other than hip fracture prevention, and with higher levels of minimum acceptable benefit for all interventions. Increasing age was associated with higher levels of minimum acceptable benefit for all interventions other than hip fracture prevention.
This study is the first of New Zealand patients' expectations of these interventions. We examined expectations of bowel cancer screening and hip fracture risk reduction, areas that have not previously been well assessed. This study used absolute risk as the format for presenting the effect of interventions, which is well understood by patients and is the preferred means of communicating risk reduction.25 We examined the effect of patients' age, level of education, and previous experience of screening or disease on their estimates of the interventions' benefits. We are not aware of previous work that has examined these factors as potential modifiers of expectation of benefit, other than for cardiovascular disease prevention.
Our response rate of 36% and our recruitment strategy may have introduced selection bias. Low response rate is a well-recognized problem of mailed questionnaires26 and may have been exacerbated in our case by the timing of the study—the time frame was short and included the Christmas and New Year period, when many New Zealanders take summer holidays. No follow-up reminders were given. Ethnicity data for our sample achieved reasonably representative proportions of European and Māori participants, but Asian and Pacific Peoples participants were underrepresented. Our participants had a high level of education, and female participants had a high level of participation in breast cancer screening. Because all participants were enrolled as patients of 3 Christchurch general practitioners, it is possible that participants' responses were related to information they had received in the course of their usual care that was in some way not typical. These factors may limit the generalizability of our findings.
Participants were asked to consider only mortality reduction or reduction in hip fractures. This prevented participants from expressing other benefits of the preventive medications—for example reductions in the risk of stroke, myocardial infarction, or other fractures. It is possible that some of the overestimation we observed could have been due to participants including these benefits in their estimates. For the 2 cancer-screening examples, participants may have included the perceived benefit of earlier diagnosis in their estimates of benefit.
That participants were asked to choose from a range of possible answers may have prevented some from indicating a correct answer. For example, a participant who wished to indicate that the expected number of deaths avoided with breast cancer screening was 15 (which we consider to be a correct estimate) could not select this and would have to choose between the 2 closest options of 5 and 50.
Our participants may have struggled with the large population risk denominators in that risk may be more readily communicated using smaller group sizes.27 Small denominators are, however, difficult to achieve when communicating small-magnitude risks and benefits; for example, when discussing cancer screening, a large denominator is required to ensure a whole number numerator.
Our findings of overestimation of the benefits of cardiovascular disease prevention and breast cancer screening are consistent with those of previous studies of perceptions of the benefits of lipid-lowering and hypertension treatment6-8,28 and studies of women's perceptions of mammography screening.3,4
Poor numeracy is a common and important finding among patients.29 Patients with poor numeracy give more pessimistic estimates of their lifetime risk of breast cancer30 and are more likely to give inaccurate estimates of the benefit of cancer screening,31 which may account for our finding of greater over-estimation among participants who had lower educational attainment.
Our findings suggest that patients overestimate the benefit of widely used preventive medications and screening programs. Such overestimation may impair their ability to make informed decisions about their use of these interventions. It is not clear why patients have overly optimistic expectations, but some commentators have pointed to deficiencies in the quality of information provided to patients in, for example, leaflets promoting breast cancer screening, which may give a misleading impression of the benefits and harms of screening.32 The use of decision aids to assist patients who are considering screening or treatment has been shown to increase patients' knowledge about the intervention and reduce decisional conflict, and it reduces acceptance of the offered intervention.33 It is possible that use of decision aids may reduce patients' tendency to overestimate intervention benefits and thus improve their ability to make an informed decision to accept or decline the intervention. There may be a conflict between ensuring informed consent and encouraging uptake of an effective intervention. Some commentators have suggested instead a policy of informed uptake rather than informed decision making, in which decision aids aim to increase participation, as well as informing patients,34 but this view remains controversial.35,36
Doctors may also have a poor understanding of the magnitude of benefit of some preventive treatments37 and have difficulty in interpreting the results of screening tests,25 which may impair their ability to facilitate informed decision making by their patients.
We did not assess patients' perceptions of the harms associated with screening and preventive interventions, but this consideration is equally important for a patient deciding whether to accept such an intervention. The communication of harm has been less well studied than the communication of benefit, but it is likely that perception of harms is affected by the method with which they are described.38-41
Our findings suggest that doctors should be aware that many patients have overly optimistic expectations of the benefits of preventive interventions and screening. This misperception may impair informed decision making about the use of such interventions, and physicians should consider using decision aids with patients when discussing these interventions. The use of decision aids may be particularly important when discussing these interventions with older patients and those with a lower level of education.
Acknowledgments
Funding support: Funding was provided by Pegasus Health Charitable Ltd, Christchurch, New Zealand.
Footnotes
Conflicts of interest: authors report none.
To read or post commentaries in response to this article, see it online at http://www.annfammed.org/content/10/6/495.
Previous presentation: A version of this report was presented at the Royal New Zealand College of General Practitioners Conference, September 4, 2011, Auckland, New Zealand.
References
- 1.Cooper A, Nherera L, Calvert N, O'Flynn N, Turnbull N, Robson J, et al. Clinical Guidelines and Evidence Review for Lipid Modification: Cardiovascular Risk Assessment and the Primary and Secondary Prevention of Cardiovascular Disease. Londo: National Collaborating Centre for Primary Care and Royal College of General Practitioners. National Institue for Health and Clinical Excellence; 2008. www.nice.org.uk/nicemedia/live/11982/40742/40742.pdf [Google Scholar]
- 2.Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355(4):375-384 [DOI] [PubMed] [Google Scholar]
- 3.Domenighetti G, D'Avanzo B, Egger M, Berrino F, Perneger T, Mosconi P, et al. Women's perception of the benefits of mammography screening: population-based survey in four countries. Int J Epidemiol. 2003;32(5):816-821 [DOI] [PubMed] [Google Scholar]
- 4.Gigerenzer G, Mata J, Frank R. Public knowledge of benefits of breast and prostate cancer screening in Europe. J Natl Cancer Inst. 2009;101(17):1216-1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwartz LM, Woloshin S, Fowler FJ, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291(1):71-78 [DOI] [PubMed] [Google Scholar]
- 6.Trewby P, Reddy A, Trewby C, Ashton V, Brennan G, Inglis J. Are preventive drugs preventive enough? A study of patients' expectation of benefit from preventive drugs. Clin Med. 2002;2(6):527-533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lytsy P, Westerling R. Patient expectations on lipid-lowering drugs. Patient Educ Couns. 2007;67(1-2):143-150 [DOI] [PubMed] [Google Scholar]
- 8.Leaman H, Jackson PR. What benefit do patients expect from adding second and third antihypertensive drugs? Br J Clin Pharmacol.. 2002;53(1):93-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page A, Taylor R. BreastScreen Aotearoa Independent Monitoring Report: Screening and Asessment of Women Attending BSA (Women screened January 2008 - December 2009). http://www.nsu.govt.nz/files/BSA/BSA_IM_Dec_09_Screening_and_assessment_reportFinal.pdf
- 10.Bowel cancer screening. National Screening Unit website. www.nsu.govt.nz/other-screening-areas/818.asp Accessed Mar 2011
- 11.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gøtzsche P, Nielsen M. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2011. January 19;(1):CD001877(1). [DOI] [PubMed] [Google Scholar]
- 13.Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast-cancer mortality in Norway. N Engl J Med. 2010;363(13):1203-1210 [DOI] [PubMed] [Google Scholar]
- 14.Welch HG. Screening mammography—a long run for a short slide? N Engl J Med. 2010;363(13):1276-1278 [DOI] [PubMed] [Google Scholar]
- 15.Hewitson P, Glasziou Paul P, Irwig L, Towler B, Watson E. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database Syst Rev. 2007. January 24;(1):CD001216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scholefield JH, Moss S, Sufi F, Mangham CM, Hardcastle JD. Effect of faecal occult blood screening on mortality from colorectal cancer: results from a randomised controlled trial. Gut. 2002;50(6):840-844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandel JS, Church TR, Ederer F, Bond JH. Colorectal cancer mortality: effectiveness of biennial screening for fecal occult blood. J Natl Cancer Inst. 1999;91(5):434-437 [DOI] [PubMed] [Google Scholar]
- 18.Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008. January 23;(1):CD001155. [DOI] [PubMed] [Google Scholar]
- 19.Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, et al. Effects of continuing or stopping Alendronate after 5 years of treatment. JAMA. 2006. December 27;296(24):2927-2938 [DOI] [PubMed] [Google Scholar]
- 20.Kanis JA, Johnell O, Oden A, et al. Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int. 2000;11(8):669-674 [DOI] [PubMed] [Google Scholar]
- 21.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brugts JJ, Yetgin T, Hoeks SE, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ. 2009;338:b2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor F, Ward K, Moore Theresa HM, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011. January 19;(1):CD004816 http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD004816/frame.html [DOI] [PMC free article] [PubMed]
- 24.Statistics New Zealand website. http://www.stats.govt.nz/Census/2006CensusHomePage.aspx
- 25.Gigerenzer G. Reckoning With Risk. Learning to Live With Uncertainty.London: Penquin Books; 2002 [Google Scholar]
- 26.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129-1136 [DOI] [PubMed] [Google Scholar]
- 27.Garcia-Retamero R, Galesic M. Using plausible group sizes to communicate information about medical risks. Patient Educ Couns. 2011;84(2):245-250 [DOI] [PubMed] [Google Scholar]
- 28.Steel N. Thresholds for taking antihypertensive drugs in different professional and lay groups: questionnaire survey. BMJ. 2000;320(7247):1446-1447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: theory and practice. Ann Behav Med. 2008;35(3):261-274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davids SL, Schapira MM, McAuliffe TL, Nattinger AB. Predictors of pessimistic breast cancer risk perceptions in a primary care population. J Gen Intern Med. 2004;19(4):310-315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127(11):966-972 [DOI] [PubMed] [Google Scholar]
- 32.Jørgensen KJ, Gøtzsche PC. Content of invitations for publicly funded screening mammography. BMJ. 2006;332(7540):538-541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2009. July 8;(3):CD001431. [DOI] [PubMed] [Google Scholar]
- 34.Bekker HL. Decision aids and uptake of screening. BMJ. 2010; 341:c5407. [DOI] [PubMed] [Google Scholar]
- 35.Dalton CB. Editorial was amoral. BMJ. 2010. November 23;341:c6648. [DOI] [PubMed] [Google Scholar]
- 36.Hudson B. Information v promotion. BMJ. 2010. November 23;341:c6650. [DOI] [PubMed] [Google Scholar]
- 37.Sapre N, Mann S, Elley CR. Doctors' perceptions of the prognostic benefit of statins in patients who have had myocardial infarction. Intern Med J. 2009;39(5):277-282 [DOI] [PubMed] [Google Scholar]
- 38.Berry DC, Knapp P, Raynor DK. Provision of information about drug side-effects to patients. Lancet. 2002;359(9309):853-854 [DOI] [PubMed] [Google Scholar]
- 39.Knapp P, Raynor DK, Berry DC. Comparison of two methods of presenting risk information to patients about the side effects of medicines. Qual Saf Health Care. 2004;13(3):176-180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Waters EA, Weinstein ND, Colditz GA, Emmons KM. Reducing aversion to side effects in preventive medical treatment decisions. J Exp Psychol Appl. 2007;13(1):11-21 [DOI] [PubMed] [Google Scholar]
- 41.Hudson B, Toop L, Mangin D, Pearson J. Risk communication methods in hip fracture prevention: a randomised trial in primary care. Br J Gen Pract. 2011;61(589):e469-e476 [DOI] [PMC free article] [PubMed] [Google Scholar]