Abstract
Although poor partner support is a key risk factor for depression in pregnant and postpartum women, partners are not generally involved in treatment beyond psychoeducation. The aim of this "proof of concept" study was to test safety, acceptability, and feasibility of Partner-Assisted Interpersonal Psychotherapy (PA-IPT), an intervention that includes the partner as an active participant throughout treatment. Women more than 12 weeks estimated gestational age and less than 12 weeks postpartum were invited to participate if they fulfilled DSM-IV criteria for Major Depressive Disorder and reported moderate symptom severity (HAM-D17 ≥16). The open trial included eight acute-phase sessions and a 6-week follow-up assessment. Ten couples completed the acute phase treatment and nine presented for a 6-week follow-up assessment. There were no study-related adverse events, and no women had symptomatic worsening from intake to Session Eight. All partners attended all sessions, no couples dropped out of treatment, and all reported positive treatment satisfaction at the conclusion of the study. Nine of ten women (90 %) met the criteria for clinical response (HAM-D17=9) at the conclusion of acute phase treatment, and eight of the nine (89 %) presenting at a 6-week follow-up assessment met criteria for symptomatic recovery. Incorporating partners in the treatment of major depressive disorders during the perinatal period is safe, acceptable, and feasible, but needs further testing in a larger population to evaluate efficacy.
Keywords: Postpartum depression, Perinatal, Pregnancy, Antenatal, Depression, Partners
Background
Depression during pregnancy and the postpartum, “perinatal” depression, poses serious concerns because of the negative consequences for mother, baby, partners, and families (Field et al. 2010; Wee et al. 2011; Goodman 2004). Combined estimates of the point prevalence rate for major depressive disorder (MDD) range from 8.5 % to 11 % at different times during pregnancy and from 6.5 % to 12.9 % at different times during the first postpartum year, with the incidence of a new episode during the first 3 months being as high as 14.5 % (Gaynes et al. 2005). Research has identified numerous risk factors for perinatal depression, such as young age, low income, lower educational attainment, history of depression and or anxiety, family history of depression, low self-esteem, adverse life/events, relationship dissatisfaction, low social support, unintended pregnancy, domestic violence, and single status (Field et al. 2006; Boyce 2003; Milgrom et al. 2008; Lancaster et al. 2010). Consistently, one of the strongest contributors to perinatal depression across studies is poor social support, particularly from the partner (O'Hara 1986; O'Hara and Swain 1996; Robertson et al. 2004). Interestingly, even a woman’s perception of adequate partner support has the power of moderating emotional and physical distress (Dennis and Ross 2006).
Treatments specific to depression in the perinatal context with traditional pharmacological approaches as well as adaptations to existing non-pharmacological treatments are actively under investigation (Dennis and Ross 2007; Dennis and Allen 2008; Yonkers et al. 2009). The American Psychiatric Association (APA) and the American College of Obstetricians and Gynecologists stated in a joint report that, although antidepressant use during pregnancy was well studied and considered a safe treatment choice for women with moderate to severe symptoms, “patients with mild to moderate depression can be treated by psychosocial approaches including individual and group psychotherapy in lieu of medication” (Yonkers et al. 2009, p. 7). Furthermore, the APA, in recent practice guidelines for the treatment of MDD, recommended psychosocial and psychological treatments without medication therapy as a first-line treatment for women with mild or mild–moderate depression (Gelenberg et al. 2010). Evidence-based psychotherapies such as Interpersonal Psychotherapy (IPT) and Cognitive Behavioral Therapy (CBT) have been adapted for use with pregnant and postpartum women, providing efficacious alternatives for women with strong preferences against the use of medication when pregnant or lactating (Bonari et al. 2005; Chabrol et al. 2004; Spinelli and Endicott 2003; Bledsoe and Grote 2006; Milgrom et al. 2005; Brandon and Freeman 2011).
The use of partners in the treatment of psychiatric illness was first conceptualized in the 1970s (Hafner et al. 1983; Hafner 1977, 1981), but literature on spouse- or partner-assisted therapies has been sparse in the last two decades. Partner-assisted therapies view healthy partners as a potential resource with social support value, a shift from the stance of marital or couples therapy in understanding individual problems as symptoms of relationship discord (Jacobson et al. 1989; Carter et al. 2011). Given the stressors occurring during the transition to parenthood, relationship support during this time has been recommended (Misri et al. 2000; Glade et al. 2005). This manuscript will describe Partner-Assisted Interpersonal Psychotherapy (PA-IPT), an innovative approach to non-pharmacological treatment of depression during pregnancy and the postpartum, and present data from a safety, acceptability, and feasibility open-label trial of PA-IPT with ten couples.
Theoretical rationale for Partner-Assisted Interpersonal Psychotherapy
Attachment theory provides a framework useful for understanding the connection between relationships and dysphoria, as well as a theoretical basis for why an approach including partners could have incremental value in the treatment of perinatal depression (Marchand-Reilly and Reese-Weber 2005; Whiffen and Johnson 1998). Studies of attachment in adults have suggested romantic partners derive comfort and security from one another, want to be with their partner (particularly in times of distress), and protest when the partner is unavailable (Crowell and Waters 1994; Hazan and Shaver 1987). The process of pregnancy and childbirth particularly involves increased needs, demands, and expectations for both parents, yet the feelings of hopelessness, helplessness, and worthlessness characterizing maternal depression often put additional burden on the non-depressed partner to initiate and maintain positive interpersonal exchanges (Davey et al. 2006). Partners, in turn, who may not understand depression as an illness and withdraw from negative interactions, perhaps seem unhelpful and unwittingly contribute to a continuous cycle of conflict and withdrawal (Kung 2000). It is important to recognize that, from this perspective, the partner is not the problem. Rather, he/she has simply been reacting to situations without a complete understanding of what depression is or the woman’s unique perceptions of what partner support would look or feel like (Dennis and Ross 2006). The aim of PA-IPT is to interrupt the interpersonal milieu by shifting focus upon the illness (and the woman’s affective experience of the illness), and to assist the partner (spouse, romantic partner, significant other, or family member) in the role of supporter/coach (Hafner et al. 1983; Baucom et al. 1998). We hypothesize that inviting the partner to participate in psychotherapy sessions can address depressive symptoms by: (1) providing the partner psychoeducation about depression, (2) increasing partner awareness of the patient’s experience of depression, and (3) teaching the partner how to respond and support the patient as she practices and gains competency in strategies for managing her emotions and stressors (Fig. 1).
Fig. 1.
Hypothesized mechanisms of action
Partner-Assisted Interpersonal Psychotherapy goals
A primary goal of PA-IPT is for the partner to become a literal therapy “partner,” extending the therapy to life between sessions. A therapist may take advantage of identified common factors associated with good outcomes by modeling for the partner behaviors and communications that express hopefulness for improvement, trust, warmth, understanding, acceptance, kindness, and confidence in the therapeutic process (Lambert 2005). The partner’s role in PA-IPT is to hear the patient’s articulation of what support she needs, learn how to respond to her so that she perceives the availability of such requested support, explore other resources for support for both of them, and engage the identified individuals/avenues to secure help. As partners learn the importance of their own support and how to express it in a way the woman feels supported, they may, in turn, feel more empowered and less helpless in the face of the depression (Davey et al. 2006).
Theory of change in the Partner-Assisted Approach
Reduction of depressive symptoms is expected to occur through the processes of:
Identifying the existing maternal and paternal stressors
Identifying the dyadic expectations each hold around the roles of “mother” and “father”
Uncovering core emotions around the stressors and expectations, exploring the realities and modifying appraisals where indicated
Enlisting the partner in accepting the woman’s feelings and responding in a “language” that she perceives as supportive
Assessing the couple’s interactions, illuminating negativity and experimenting with more positive interchanges
Increasing the partner’s emotional and instrumental support, thereby reducing the maternal stressors
The dyadic relationship may improve; however, relationship dysfunction is framed as a breakdown in the support system and not as marital conflict needing negotiation. Through increasing the empathy, acceptance, and support the partners have for one another, the couple can be expected to feel better about themselves, each other, their relationship, and the transition to parenthood.
Partner-Assisted Interpersonal Psychotherapy adaptation
Partner-Assisted IPT is constructed for depressed women who need increased partner support, not constructed for depressed women who report a distressed relationship. Serious relationship discord contraindicates this use of the partner; in the presence of anger and hostility the “patient” role assigned to the woman might create or contribute to a dysfunctional balance of power in the relationship. Following the model of IPT, depression is framed as an illness, but the symptoms are characterized as an opposing force or an “undertow” restricting the woman’s capacity to address her own and her partner’s needs. Constructing an interpersonal formulation of the patient's distress, PA-IPT links depressive symptoms to particular interpersonal events or contexts (Stuart and Robertson 2003; Stuart 2006; Klerman et al. 1984). As is common in individual IPT for perinatal depression, the potential for depressive symptoms to accompany the adjustments to self-identity and role that occur during the transition to parenthood is explored (Spinelli 2001; Segre et al. 2004). In PA-IPT this occurs in three-dimensional dialogue, with the therapist reflecting and supporting to each partner their explorations of doubt, ambivalence, and anxiety about the dual journeys of depression and early parenthood. Therapy sessions provide a forum for partners to explore this important life transition with one another, guided by a clinician alert to mismatches between expectations and realistic goals. Other material from interpersonal relationships may emerge in sessions, but the primary foci are on the woman’s depression, partner support, and the measures these two individuals can take to protect their harmonious move into parenthood.
Partner-Assisted IPT incorporates specific elements borrowed from Emotionally Focused Couple Therapy (EFCT), an evidence-based couple intervention also based upon attachment theory. The EFCT approach to couple therapy aims to strengthen the interpersonal bond and address relationship distress by highlighting the attachment needs humans have of one another and restructuring the ways partners express these needs. In PA-IPT, techniques borrowed from EFCT move the target from relationship distress (Johnson 2004) to “depression” distress, as it is experienced by both partners. With the goal of reducing depressive symptoms in individuals who have preserved relationship satisfaction, the partner is identified as an attachment figure from who increased support and understanding is vital for strengthening the woman’s movements toward recovery. Pinpointing and addressing each partner’s attachment needs, specifically within the context of the transition to parenthood, directs the non-depressed partner’s attention to needs he or she can attend to in the depressed mate (Whiffen and Johnson 1998). Focus is placed first at what the partner already does, before examining additional maternal needs. As in EFCT, the therapist models positivity and nonjudgment, tenderly evoking from the woman her experience of depression and her increased needs for support at this time of her life.
Hypotheses
The primary hypotheses of the proof of concept project were that PA-IPT would be safe (no women would worsen), feasible (partners would attend), and acceptable (couples would complete treatment and report satisfaction). We expected fewer depressive symptoms and maintenance of response through the 6-week follow-up. Further, it was expected that relationship satisfaction as reported by participant and partner would improve over the course of the treatment.
Secondary aims included the investigation of:
Prevalence of depression in partners
Response of partners’ depressive symptoms to treatment
Number of treatments that can be reasonably attended by couples
Rate of depressive symptom response in both partners
Cultural sensitivity of the model and techniques
Methods
Experimental design
This was an open-series proof of concept study to investigate the safety, acceptability, and feasibility of PA-IPT in perinatal women with MDD. The primary outcomes were the ability to recruit participants, treatment response at midpoint and final session, session attendance, and couple satisfaction with treatment. Participants were educated concerning the rationale for PA-IPT, the exploratory nature of the approach, and the protections of the informed consent process. As is common in psychotherapy development, the first author was the sole therapist in this open series group of participants (Rounsaville and Carroll 2001). Investigator bias was addressed by the use of independent raters for the screening process and all HAM-D patient interviews.
The respective Institutional Review Boards of the University of Texas Southwestern Medical Center approved study recruitment and participation between January 2008 and December 2010 (actual period of enrollment was June 2008 through February 2010). A Certificate of Confidentiality was obtained from the National Institutes of Health. The University of North Carolina at Chapel Hill Institutional Review Board approved data analysis from March 2011 through February 2012.
Recruitment
Eligible participants were recruited from women visiting the Women’s Mental Health Center (WMHC) of the University of Texas Southwestern Medical Center for evaluation and treatment for mood disorders in the context of reproductive events. Patients of the WMHC were referred from community and university-affiliated obstetricians. The study was not limited to heterosexual couples; however, no same-sex couples presented to the WMHC for treatment during the course of the study enrollment.
Inclusion and exclusion Criteria
Women who were 18 years or older, more than 12 weeks estimated gestational age or less than 12 weeks postpartum, married or cohabiting with their partner for a minimum of 6 months, either not receiving psychotropic medication or on a stable regimen (more than 4 weeks), and English-speaking were invited to present study participation information to their partners. Exclusion criteria were comorbid substance abuse/dependence, cognitive disorder or schizophrenia, presence of psychotic or manic symptoms, endorsed partner violence, untreated partner psychiatric illness, ongoing individual psychotherapy, and/or the preference to initiate pharmacological treatment.
Participants
During the time of enrollment, 15 women met study inclusion criteria and were invited to participate. Those with interested partners were scheduled for a second visit to the WMHC, at which the process of consent was completed and both partners received the Structured Clinical Interview for the Diagnosis of Axis I Mental Disorders (SCID-IV, Research version) and the Hamilton Rating Scale for Depression, 17-Item (HAM-D17). They were considered study eligible if the woman met full criteria for MDD and if her HAM-D17 score was greater than 16. The screening process spanned two clinic visits.
Two women were excluded because partners had untreated psychiatric illness; the women continued individual treatment at the WMHC and their partners were referred to community mental health providers. Eleven women and their partners fulfilled the above-mentioned inclusion and exclusion criteria. One couple was disqualified after Session Two, at which time partner violence (female upon male) was revealed. Two women who met study criteria were on stable doses of antidepressants (one pregnant and one postpartum) at study entry, and one pregnant woman was on a stable dose of an antipsychotic (continuation of drug prescribed to her from her native country). An additional pregnant participant who responded to PA-IPT but had history of severe postpartum depression chose to initiate an antidepressant prophylactically a few weeks before delivery. See Table 1 for demographic summary.
Table 1.
Demographic characteristics of participants Enrolled in PAT study
| Characteristic | Women (N = 11)a | Partners (N = 11)a | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | |
| Age (years) | 30 | 5.3 | 22–40 | 30.3 | 5.6 | 20–39 |
| Relationship length (years) | 3.2 | 1.4 | 0.5–11 | 3.2 | 1.4 | 0.5–11 |
| Education (years) | 15.6 | 2.1 | 12–20 | 14.2 | 2.3 | 11–16 |
| N | Percent | N | Percent | |||
| Race | ||||||
| Latina/o | 4 | 36.4 | 4 | 36.4 | ||
| Caucasian | 5 | 45.4 | 5 | 45.4 | ||
| African American | 2 | 18.2 | 2 | 18.2 | ||
| Employment Status | ||||||
| Full-time employed | 6 | 54.6 | 10 | 91.0 | ||
| Part-time | 1 | 9 | 0 | |||
| Unemployed | 4 | 36.4 | 1 | 9.0 | ||
| Perinatal Status | ||||||
| Primigravida | 7 | 63.6 | ||||
| Multigravida | 4 | 36.4 | ||||
| Pregnant at intake | 8 | 72.7 | ||||
| Delivered before Session 8 | 3 | 27.3 | ||||
| Postpartum at Intakea | 3 | 27.3 | ||||
| Marital Status | ||||||
| Married | 8 | 72.7 | ||||
| Living together | 3 | 27.3 | ||||
| Other children in home | 5 | 45.4 | ||||
| Household income | ||||||
| >$100,000 | 4 | 36.4 | ||||
| $80,000–99,999 | 2 | 18.2 | ||||
| $60,000–79,000 | 0 | |||||
| $40,000–59,999 | 3 | 27.2 | ||||
| $20,000–30,999 | 0 | |||||
| <19,999 | 2 | 18.2 | ||||
One couple excluded after Session Two
Procedures
Couples attended eight weekly psychotherapy sessions, with 12 weeks allowed for completion of the eight sessions to accommodate unexpected events and changes in schedule. All sessions were video-recorded and reviewed by the investigator with consultant experts in EFCT (Susan Johnson, PhD) and IPT (Scott Stuart, MD). The consultant experts, along with the first author, assessed sessions for their use of EFCT and IPT techniques while also evaluating them for adherence to the provisional PA-IPT manual outline. Independent raters conducted the HAM-D17 evaluations of the patients, meeting twice during the course of the study for reliability testing. At each session, participants and partners completed the Edinburgh Postnatal Depression Scale (EPDS) to assess the woman’s depressive symptoms. At intake, Session Four (midpoint), Session Eight, and at 6–8 weeks postpartum (or 6–8 weeks following last session if enrolled postpartum), all participants received the HAM-D17 and completed the Dyadic Adjustment Scale (DAS). Study staff contacted individuals who completed the acute treatment early in their pregnancy monthly by telephone until delivery, administering the EPDS to monitor depressive symptoms and ensure care in the event response was not maintained. Gift card incentives ($25) were distributed at three data collection points to compensate for the additional time required to complete the questionnaires and HAM-D17 interview.
Measures
In addition to the study demographic survey, participants completed the following clinician- and self-report measures.
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) is a clinician-administered, semistructured interview widely used in research to facilitate diagnosis of psychiatric illness across populations according to the Diagnostic Manual of Mental Disorders-IV (Summerfeldt and Antony 2002; APA 2000). The Screening, Mood Disorders, and Mood Differential modules were utilized during the screening visits to establish or rule out a diagnosis of MDD in participants.
The HAM-D17 is a 17-question multiple choice clinician-rated instrument that rates the severity of a patient’s depression (Hamilton 1960). The revised 17-item version is the most widely used outcome measure in treatment studies of MDD, and has been previously used in studies of perinatal women suffering from depression (Moran and O'Hara 2006; Spinelli and Endicott 2003). Interrater reliability was tested at intervals throughout the study period and, for total scores, averaged 0.97. The Ham-D17, like other traditional depression screening and severity measures, is susceptible to inflation due to the overlapping symptoms of depression and characteristics of pregnancy. Therefore, the scores for inclusion in the sample (16 versus the common threshold of 14) and to assume response (9 versus the common threshold of 6) were similarly elevated in an effort to prevent false diagnosis and missed response (Spinelli 1997; Rush et al. 2006).
The EPDS was developed specifically for the screening and assessment of postpartum depression (Cox et al. 1987), but has become widely used during the entire perinatal period (Gaynes et al. 2005). Total scores on this ten-item, multiple-choice scale range from 0 to 30, with higher scores reflective of greater symptom severity. Also included was the EPDS—Partner version, yielding a report of the woman’s symptomatology as observed by her partner (Moran and O'Hara 2006).
The DAS is one of the most commonly used self-report measures for the assessment of relationship satisfaction or adjustment, and has been previously utilized in perinatal research (Heyman et al. 1994; Misri et al. 2000; Terry et al. 1991; Spanier 1976). Participants evaluated several aspects of their relationship on 32 items yielding scores on four subscales: Dyadic Satisfaction, Dyadic Cohesion, Dyadic Consensus, and Affectional Expression. The theoretical range of total scores possible is 0–151, and those that fall below 100 suggest relationship distress (Spanier and Filsinger 1983).
Study intervention
Acute treatment for the target of depressive symptoms consisted of three phases of treatment carried out over eight sessions. The first phase of PA-IPT is characterized by accessing the depressive experience from the perspectives of both partners, eliciting how they each understand the events or stressors that may have occurred prior to the onset of her depression and any associations they may have made between a “trigger” and the symptoms. The middle phase of treatment aims to explore the role expectations each partner has of self and other, and interactions between them that are perceived as supportive, or conversely, unsupportive. The final phase consolidates changes, explores additional sources of support, and processes what the experience of therapy has been like for each partner.
At each session, the patient completes the EPDS and her partner completes the EPDS-P (reporting depressed symptoms partner observed in the woman over the past 7 days); the forms are then compared, with explorations of item response agreement and disagreement to demonstrate partner attunement to patient symptom burden. Changes in the agreement on the EPDS symptoms ratings over sessions are highlighted, demonstrating the utility of the new ways of communicating or giving attention to continuing discrepancies. Symptom presentation unique to the patient is identified and, in the final phase, reviewed as strategies are outlined for quick intervention if there are signs of recurrence or relapse.
To portray their support system, each partner completes the IPT “Circle of Closeness,” identifying in three concentric circles those individuals in their social environment according to level of intimacy (Stuart and Robertson 2003). The Circle of Closeness is periodically utilized as a point of reference, helping identify which family members or friends may be able to fill in gaps of support that remain or are anticipated to occur at later points in the transition to parenthood. Communication analyses surrounding targeted incidents or needs are collaboratively conducted, and the therapist invites the couple to engage in role-plays to demonstrate new ways of asking for help. In later sessions, these alterations in communication are explored for both their potential effect and their likelihood of recurrence (or the willingness of partner to modify behaviors).
The manual draft aimed to demonstrate cultural sensitivity, operationalized in treatment by explorations of the couple’s family of origin and their own enduring role expectations as influenced by culture and society. The therapist stance is to explore differences with curiosity and openness, recognizing and validating the varied perceptions of maternal and paternal roles while also drawing attention to the mutual desire to parent competently.
Focus group meeting
Four couples attended a focus group held in the last quarter of the project (one couple was lost to follow-up, one couple had moved out of the state, one partner worked two jobs and another partner worked nights, one couple had a last-minute illness, and one couple could not arrange evening childcare). Conducted by an independent consultant trained in focus group methodology, in a semistructured format the couples responded to specific questions regarding the intervention and the therapist (Table 2).
Table 2.
Focus group
| Partner-Assisted Interpersonal Therapy Focus Group Purpose Statement: To describe and quantify patient and partner satisfaction with PAT. |
|---|
| Questions about the Intervention: |
| Directed to the patients: |
| How did PAT therapy address your depression? |
| How about the way you perceived your partner’s support? |
| Directed to the partners: |
| How did PAT impact your understanding of depression? |
| How about the way you understood your partner? |
| What are the key points about perinatal depression that you think partners of depressed women would need to better understand? |
| Directed to both: |
| What was the most surprising to you about the intervention? |
| What about PAT would you change? |
| What do you think helped the most? |
| What do you think about the measures you were asked to complete? |
| What challenged you in the intervention? |
| Was anything about the therapy or your therapist harmful to you or your relationship with your partner? |
| How easy or difficult was it for you to come to the Women’s Mental Health Center for treatment? |
| What kind of changes did you and your partner make in your daily life that may be due to PAT? |
| Did you find yourself and your partner discussing sessions outside of therapy? If so, what sorts of things did you talk about? |
| What is the session that you remember the best? |
| How would you describe PAT to someone who wanted to know more about it? |
| Do you have any other comments that didn’t fit into any of these topics? |
| Questions about the therapist: |
| What was your therapist like? |
| If you were to go to someone for therapy again, what would you look for in a therapist? |
Study outcome measures
Safety
Participant worsening over the eight session series (i.e., increasing HAM-D17 score from intake, suicidal ideation) or an adverse event (i.e., hospitalization or suicidal act) occurring at any time during the acute phase of treatment would signal poor safety.
Acceptability
Participant retention along with data collected at a post-study focus group will assess acceptability.
Feasibility
The recruitment record and participant session attendance test the feasibility of offering the intervention to perinatal couples.
Depressive symptoms
Clinician ratings of depressive symptoms would be performed at intake, Session Four, Session Eight, and between 6–8 weeks post-treatment. Self-report ratings (EPDS) from each partner about her symptoms would be obtained prior to each session.
Relationship functioning
Relationship satisfaction (DAS) would be evaluated at intake, Session Four, Session Eight, and at follow-up.
Statistical plan
The primary outcome measure was the change in clinician-rated HAM-D17 scores (depressive symptoms) from intake at Session Eight. As the focus of this study was to demonstrate the feasibility and safety of PA-IPT in a small sample, no statistical power analyses were conducted to establish sample size. Total sample size of ten couples (20 participants) was set for this open-series feasibility trial. To examine the change in the HAM-D17, DAS, and EDPS for mothers and partners over time, a two-way analysis of variance (ANOVA) with two within factors, session (HAM-D17: 0, 4, 8, and 9; EPDS: 0, 4, and 8; DAS: 0 and 8) and person (patient and partner) was performed. Assumptions of the statistical tests were checked for violations. When even small levels of skew were observed, additional nonparametric analyses confirmed the accuracy of the statistical results. IBM SPSS version 19 (IBM, Inc., Chicago, IL) was used to conduct the analyses.
Results
Primary aims
Safety
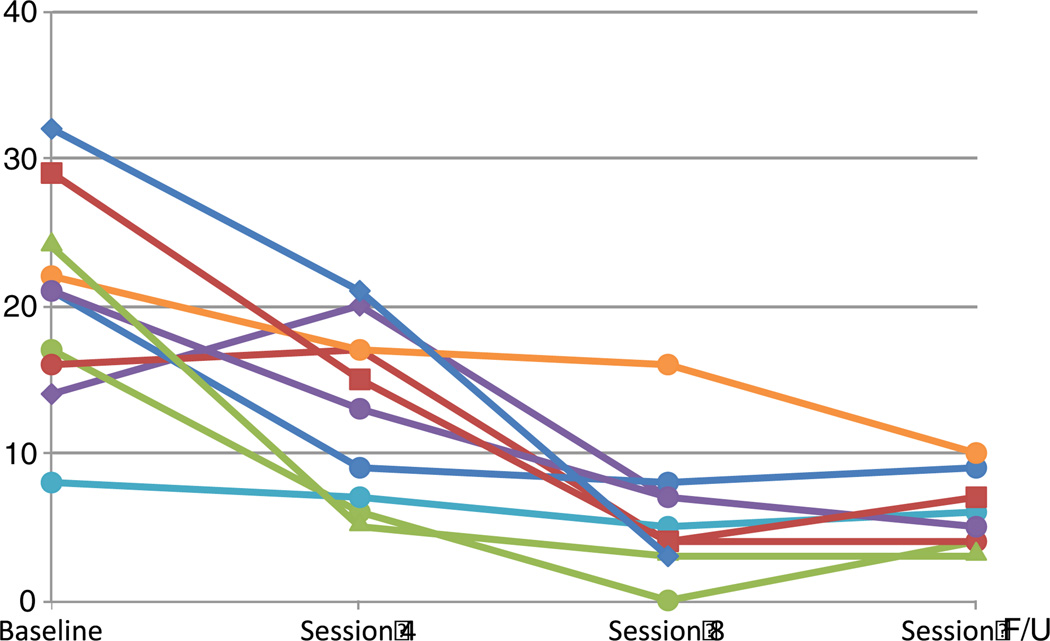
Overall, no patients worsened as evidenced by the clinician-rated HAM-D instrument, and there were no study-related adverse events. There were significant differences in depressive symptoms (HAM-D17) for the interaction of session by person (p<0.001) and the main effects of session (p=0.001) and person (p<0.001; see Fig. 2). Women had high levels of depressive symptoms at intake (mean ± standard deviation [SD]: 19.11±6.13) that declined significantly by Session Eight (6.00±4.47) and remained low at the 6-week follow-up evaluation (5.89±2.37). One woman did not meet the study criteria for full symptom response (HAM-D17=9; participant’s HAM-D scores at Session Eight and at follow-up were 16 and 10, respectively).
Fig. 2.
Symptom response of women (Hamilton Rating Scale for Depression, 17-item)
Acceptability
All couples attended all sessions, and all partners expressed at the final session that they had received personal benefit from the treatment. At the focus group meeting, attendees uniformly endorsed the therapy as critical to her recovery and their adjustment to parenthood. One father related, “a valuable part of it, the discussion, was having some dedicated time talking about my point of view and, kind of, the sort of things I was going through even in supporting her.” Another partner expressed, “it’s a lot easier to be supportive if you know something is coming your way and it is not your fault.” Women expressed that the techniques they learned helped them communicate their needs “you, know, putting my point across in a way where it would not cause arguments.” They felt the illness was something they were dealing with as a couple, rather than as individuals; “it reminded me that there were still some issues that we needed to address together instead of just me trying to cover what I was going through.” Suggestions for improving the therapy included having a group meeting midway; couples stated they were enjoying the focus group so much that they wished they had met one another earlier. One partner, during the focus group meeting, voiced the wish for “more strategies, like practicing at home.” All couples believed that the length was adequate (eight sessions), and that the follow-up had been instrumental in assuring them that they were managing well. Most patients and partners agreed that they were initially reluctant to come to a “women’s mental health center,” but the desperation of their circumstances drove them to overcome the feelings of stigma.
Feasibility
The willingness of the initial 11 partners in the sample to participate was high. In the final sample of ten couples, there were no dropouts. Only one couple completing the acute phase was lost to follow-up.
Secondary aims
Prevalence of depression in partners
Two of ten partners met criteria for past episodes of MDD, and one of the two partners experienced symptom recurrence over the course of the acute phase.
Response of partners’ depressive symptoms to treatment
All ten partners entered the study with low levels of depressive symptoms, and symptoms remained low throughout all sessions in nine partners (HAM-D17 at Session One: 3.22±3.53; at 6-week follow-up: 2.67±3.50).
Feasibility of intervention duration
In view of the ongoing questions surrounding the optimum number of psychotherapy sessions for the treatment of depression, an important secondary aim for this project was to identify the number of sessions that could be reasonably attended by couples. With the exception of the couple mentioned above who failed to respond, symptom response was steady throughout treatment with seven women scoring below the threshold for “probable” depression on the EPDS (threshold of 12) by Session Four (midpoint) and nine of ten women scoring below threshold by Session Seven. That there were no dropouts and perfect session attendance suggests that eight sessions were not onerous to woman or partner.
Couple attunement to depressive symptoms
On the weekly EPDS ratings, there were significant main effects of session (p<0.001) and person (p=0.050). Women had high levels of EDPS at intake (17.30±4.47) that declined by Session Eight (6.00±3.97). Partners, on the other hand, rated the intensity of women’s depressive symptoms lower at intake (EPDS-P scores mean±SD=13.80±3.36). However, by Session Eight, partner ratings demonstrated more agreement with women’s ratings (6.10±4.48).
Relationship satisfaction
As measured by the DAS, there were no significant main effects of session (p=0.189) or person (p=0.328), and the interaction between session and person was also non-significant (p=0.537). Average scores for women at intake were lower than those of partners (103.10±9.39 versus 105.10±13.68), and scores for women and partners were increased at Session Eight (108.00±16.49 versus 112.70±12.65).
Discussion
The aims of this pilot study were to test the safety, acceptability, and feasibility of PA-IPT in a small group of patients, one of the first steps in the stage model of behavioral therapy development as proposed by Rounsaville and Carroll (2001). The project reported fulfilled the aims of Stage 1a of the model: specifying the theoretical rationale for the approach along with a theory of change, producing a first draft of the treatment manual, and conducting a pilot test. The next steps to accomplish (Stage 1b) are iteratively refining the treatment, completing the manual, constructing an adherence/competence measure, and developing a training program (all currently in process). Still later tasks are performing randomized clinical trials to evaluate the efficacy of the pilot-tested treatment and explore mechanisms of action (Stage II), and testing the generalizability and transportability of treatments in large population studies (Stage III) (Rounsaville and Carroll 2001). This structure provides the framework for the ongoing development of PA-IPT.
We demonstrated that including partners in the treatment of perinatal depression is safe, and that the proposed partner-assisted adaptation of IPT is acceptable to couples. Further, the lack of attrition in this pilot suggests that partners can be engaged and retained for the acute course of treatment. Committed partners often attend prenatal visits, sonography appointments, prepared childbirth classes, and neonatal check-ups; in our experience, the invitation to partners to join the psychotherapy sessions was viewed in the same manner. Albeit a small group of participants, there was considerable racial, ethnic, and socioeconomic diversity in the sample, suggesting that our attention to cultural differences was sufficient to attract and engage partners of diverse cultures and socioeconomic status.
Our secondary aims were to attend to partner mental health and relationship satisfaction. Of the two partners reporting psychiatric history significant for MDD, one experienced relapse during the acute phase of treatment without response to PA-IPT. This suggests that it may be difficult if not impossible for a depressed partner to provide the level of support (emotional and instrumental) requested by PA-IPT. It also confirms the need for attention to partner mental health over the perinatal period, particularly when maternal depression is present and the partner also has history of depression (Wee et al. 2011). Even in the absence of partner depression, clinicians including partners need to be mindful of partner burden, and watchful for signs of caregiver stress or “burnout” (Roberts et al. 2006; Kasuya et al. 2000).
The partner (and woman) nonresponsive to treatment also demonstrated the limitations of PA-IPT for addressing serious discord. Although this couple’s conflict had been minimized in early sessions, it was fully disclosed during the third and fourth sessions. As the therapist made the recommendation to discontinue PA-IPT and arrange for both individual treatment and couples therapy from an outside provider, the couple asked to remain in study treatment but to just “avoid conversations about our relationship.” An agreement was made to continue for two more weeks and, if there were no improvements in symptoms (either woman or partner), they would be withdrawn from the study. The last half of treatment progressed as planned, and the therapist was cautious to notice when session content was moving toward their conflict, reminding the couple that the agreement was to postpone focus on this area for a later time with a couples therapist. By follow-up, both woman and partner were much improved symptomatically and expressed the intention to pursue couples therapy in the near future. Nevertheless, beyond concerns that PA-IPT could exacerbate inequitable distributions of power in a relationship by identifying the woman as a “patient,” serious relationship discord prevents the partner from authentically increasing support and the woman from altering either her perceptions or expectations of her partner.
Practical features of treatment are important for optimizing PA-IPT. The reticence of participants to visit a mental health clinic supports the growing belief that perinatal mental health services might be more acceptable in the OB/Gyn/Birthing Center environment (Grote et al. 2004). The brief structure of the treatment would suit such contexts. Although the original protocol required the eight-session acute phase to take place over a 10-week period, there was a need for greater flexibility, particularly with patients who delivered their babies during the acute phase (N=3). We subsequently revised the protocol to extend the time, allowing 12 weeks for the eight sessions.
Other suggestions made by the IPT and EFCT experts along with the participants have been implemented in the refined PA-IPT manual. One subtle change was made in the use of the EPDS and EPDS-P as an intervention: originally, the therapist collected the completed measures, calculated the scores, and presented the differences to the couple. The IPT expert recommended allowing the couples to simply exchange the instruments and comment on the differences themselves, attending more to individual items and less to the overall score. This greatly contributed to the effectiveness of the intervention and was employed with the last half of the sample. The desire cited for discrete assignments between sessions directed at the partner was fascinating in view of the existing constant focus of PA-IPT on the between-session changes in supportive behaviors and communications occurring over the course of treatment. Because we are concerned that specific assignments to the partner rather than to the couple can implicitly communicate that the partner is part of the problem, we revised the treatment to include specific assignments of actions to do together, such as increasing physical activity by walking together at the end of the day and using the time to talk, or another activity congruent with the couples interests and hobbies.
Feasibility studies such as this one have inherent limitations in addition to small sample size. We acknowledge that the sample was selected on the basis of the partner’s willingness to participate in the treatment, and volunteer and social desirability biases must also be considered (Spinelli and Endicott 2003; Misri et al. 2000). Because we wanted to investigate the feasibility of engaging couples across the perinatal period, the sample was heterogeneous in terms of parity, estimated gestational age, parturition, and weeks postpartum (Table 1). However, the excellent retention rate allows us to suggest that couples can commit to psychotherapy treatment when appointments can be flexible, and that childbirth along with early postpartum “chaos” may not disrupt treatment. The lack of a control or comparison group requires consideration of potential confounders such as time, therapist, and regression-to-the-mean effects.
Future directions
Investigating the efficacy and effectiveness of PA-IPT is only possible with larger randomized controlled trials. Further, it is unclear whether the specific techniques of IPT and EFCT are particularly helpful, or if mechanisms of change are more connected to the partner’s participation. Given that the central goal is to include the partner into the treatment, future work might investigate incorporating partners into other theoretical approaches, such as CBT.
Longitudinal work could address other important questions: Does including partners into treatment improve couple dynamics past the acute period of treatment? Are there differences in parenting practices of couples that engage in short-term psychotherapy for maternal depression? Do infant outcomes demonstrate secondary health and psychological benefits?
Summary
This small safety, acceptability, and feasibility study suggests that the perinatal period provides an important window of opportunity for drawing partners into the treatment of maternal distress. In addition to reducing depressive symptoms, PA-IPT imparts important knowledge to partners regarding the disease course of MDD, validates their own experiences of coping with the depressive experience, and alerts them to early warning symptoms of relapse.
Acknowledgments
This research received support from Grant Number K23MH085007 (PI: Anna R. Brandon, PhD) from the National Institute of Mental Health (NIMH). Dr. Brandon also acknowledges support from Grant Number KL2RR024983 (PI: Milton Packer, MD) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). Anna Brandon, PhD, and Linda Hynan, PhD, both received support from Grant Number UL1 RR024982, the North And Central Texas Clinical and Translational Sciences Initiative (PI: Milton Packer, MD) awarded by the NIH. Geetha Shivakumar, MD, acknowledges support from a VISN 17 Research Division New Investigator Award. Robin B. Jarrett, PhD, reports support by Grant Number K24-MH001571 (PI: Robin B. Jarrett, PhD) from the NIMH.
Footnotes
Conflicts of interest The authors have no conflicts of interest to disclose.
Contributor Information
Anna R. Brandon, Email: anna_brandon@med.unc.edu, Department of Psychiatry, Women’s Mood Disorders Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA; Department of Psychiatry, 10616 Neurosciences Hospital, University of North Carolina at Chapel Hill, Campus Box 7160, Chapel Hill, NC 27599-7160, USA.
Nadia Ceccotti, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA.
Linda S. Hynan, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA Department of Clinical Sciences, The University of Texas Southwestern Medical Center, Dallas, TX, USA.
Geetha Shivakumar, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA; Dallas VA Medical, Center, Dallas, TX, USA.
Neysa Johnson, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA.
Robin B. Jarrett, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA
References
- American Psychiatric Association (APA) diagnostic and statistical manual of mental disorders-fourth edition, Text Revision (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Baucom DH, Shoham V, Mueser KT, Daiuto AD, Stickle TR. Empirically supported couple and family interventions for marital distress and adult mental health problems. J Consult Clin Psychol. 1998;66(1):53–88. doi: 10.1037//0022-006x.66.1.53. [DOI] [PubMed] [Google Scholar]
- Bledsoe SE, Grote NK. Treating depression during pregnancy and the postpartum: a preliminary meta-analysis. Res Soc Work Pract. 2006;16(2):109–120. [Google Scholar]
- Bonari L, Koren G, Einarson T, Jasper J, Taddio A, Einarson A. Use of antidepressants by pregnant women: evaluation of perception of risk, efficacy of evidence based counseling and determinants of decision making. Arch Women's Ment Health. 2005;8(4):214–220. doi: 10.1007/s00737-005-0094-8. [DOI] [PubMed] [Google Scholar]
- Boyce PM. Risk factors for postnatal depression: a review and risk factors in Australian populations. Arch Women's Ment Health. 2003;6(Suppl2):s43–s50. doi: 10.1007/s00737-003-0005-9. [DOI] [PubMed] [Google Scholar]
- Brandon AR, Freeman MP. When she says "no" to medication: psychotherapy for antepartum depression. Curr Psychiatry Reports. 2011;13(6):459–466. doi: 10.1007/s11920-011-0230-2. [DOI] [PubMed] [Google Scholar]
- Carter W, Grigoriadis S, Ravitz P, Ross LE. Conjoint IPT for postpartum depression: literature review and overview of a treatment manual. Am J Psychother. 2011;64(4):373–392. doi: 10.1176/appi.psychotherapy.2010.64.4.373. [DOI] [PubMed] [Google Scholar]
- Chabrol H, Teissedre F, Armitage J, Danel M, Walburg V. Acceptability of psychotherapy and antidepressants for postnatal depression among newly delivered mothers. J Reprod Infant Psychol. 2004;22(1):5–12. [Google Scholar]
- Cox J, Holden J, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Crowell JA, Waters E. Bowlby's theory grown up: the role of attachment in adult love relationships. Psychol Inq. 1994;5(1):34. [Google Scholar]
- Davey SJ, Dziurawiec S, O'Brien-Malone A. Men's voices: postnatal depression from the perspective of male partners. Qual Heal Res. 2006;16(2):206–220. doi: 10.1177/1049732305281950. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Allen K. Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression. Cochrane Database Systematic Reviews. 2008;(4) doi: 10.1002/14651858.CD006795.pub2. CD006795. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Ross L. Women's perceptions of partner support and conflict in the development of postpartum depressive symptoms. J Adv Nurs. 2006;56(6):588–599. doi: 10.1111/j.1365-2648.2006.04059.x. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Ross LE. Psychosocial and psychological interventions for treating antenatal depression. Cochrane Database of Systematic Reviews. 2007;(3) doi: 10.1002/14651858.CD006309.pub2. CD006309. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M. Prenatal depression effects and interventions: a review. Infant Behav Dev. 2010;33(4):409–418. doi: 10.1016/j.infbeh.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Hernandez-Reif M, Diego M. Risk factors and stress variables that differentiate depressed from nondepressed pregnant women. Infant Behav Dev. 2006;29(2):169–174. doi: 10.1016/j.infbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. Perinatal depression: prevalence, screening accuracy and screening outcomes. Agency for Healthcare Research and Quality, Rockville. 2005 doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelenberg AJ, Freeman MP, Markowitz J, Rosenbaum JF, Thase ME, Trivedi MH, et al. American Psychiatric Association practice guidelines for the treatment of patients with major depressive disorder. 3rd ed. Arlington, VA: American Psychiatric Association; 2010. p. 152. [Google Scholar]
- Glade AC, Bean RA, Vira R. A prime time for marital/relational intervention: a review of the transition to parenthood literature with treatment recommendations. Am J Fam Ther. 2005;33:319–336. [Google Scholar]
- Goodman JH. Paternal postpartum depression, its relationship to maternal depression, and implications for family health. J Adv Nurs. 2004;45:26–35. doi: 10.1046/j.1365-2648.2003.02857.x. [DOI] [PubMed] [Google Scholar]
- Grote NK, Bledsoe SE, Swartz HA, Frank E. Feasibility of providing culturally relevant, brief interpersonal psychotherapy for antenatal depression in an obstetrics clinic: a pilot study. Res Soc Work Pract. 2004;14(6):397–407. [Google Scholar]
- Hafner R. The husbands of agoraphobic women and their influence on treatment outcome. Br J Psychiatry. 1977;131:289–294. doi: 10.1192/bjp.131.3.289. [DOI] [PubMed] [Google Scholar]
- Hafner R. Spouse-aided therapy in psychiatry: an introduction. Aust NZ J Psychiatry. 1981;15(4):329–337. doi: 10.3109/00048678109159456. [DOI] [PubMed] [Google Scholar]
- Hafner R, Badenoch A, Fisher J, Swift H. Spouse-aided versus individual therapy in persisting psychiatric disorders: a systematic comparison. Fam Process. 1983;22(3):385–399. doi: 10.1111/j.1545-5300.1983.00385.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol, Neurosurgury, Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazan C, Shaver P. Romantic love conceptualized as an attachment process. J Personal Soc Psychol. 1987;52:511–524. doi: 10.1037//0022-3514.52.3.511. [DOI] [PubMed] [Google Scholar]
- Heyman RE, Sayers SL, Bellack AS. Global marital satisfaction versus marital adjustment: an empirical comparison of three measures. J Fam Psychol. 1994;8(4):432–446. [Google Scholar]
- Jacobson NS, Holtzworth-Munroe A, Schmaling KB. Marital therapy and spouse involvement in the treatment of depression, agoraphobia, and alcoholism. J Consult Clin Psychol. 1989;57(1):5–10. doi: 10.1037//0022-006x.57.1.5. [DOI] [PubMed] [Google Scholar]
- Johnson SM. The practice of emotionally focused couple therapy: creating connection. 2nd edn. New York: Brunner-Routledge; 2004. [Google Scholar]
- Kasuya RT, Polgar-Bailey P, Takeuchi R. Caregiver burden and burnout. A guide for primary care physicians. Postgrad Med. 2000;108(7):119–123. doi: 10.3810/pgm.2000.12.1324. [DOI] [PubMed] [Google Scholar]
- Klerman G, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal psychotherapy of depression. New York: Basic Books; 1984. [Google Scholar]
- Kung WW. The intertwined relationship between depression and marital distress: elements of marital therapy conducive to effective treatment outcome. J Marital Fam Ther. 2000;26(1):51–63. doi: 10.1111/j.1752-0606.2000.tb00276.x. [DOI] [PubMed] [Google Scholar]
- Lambert MJ. Early response in psychotherapy: further evidence for the importance of common factors rather than "placebo effects". J Clin Psychol. 2005;61(7):855–869. doi: 10.1002/jclp.20130. [DOI] [PubMed] [Google Scholar]
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM, Johnson TR. Risk factors for depressive symptoms during pregnancy: a systematic review. Peripartum length of stay for women with depressive symptoms during pregnancy. Am J Obstetetrics & Gynecol. 2010;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand-Reilly JF, Reese-Weber M. Husbands' and wives' attachment orientations and depressive symptoms: predictors of positive and negative conflict behaviors in the marriage. J Adult Dev. 2005;12(1):85–89. [Google Scholar]
- Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, Ericksen J, Ellwood D, Buist A. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108(1–2):147–157. doi: 10.1016/j.jad.2007.10.014. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Negri LM, Gemmill AW, McNeil M, Martin PR. A randomized controlled trial of psychological interventions for postnatal depression. Br J Clin Psychol. 2005;44(4):529–542. doi: 10.1348/014466505X34200. [DOI] [PubMed] [Google Scholar]
- Misri S, Kostaras X, Fox D, Kostaras D. The impact of partner support in the treatment of postpartum depression. Can J Psychiatr. 2000;45:554–558. doi: 10.1177/070674370004500607. [DOI] [PubMed] [Google Scholar]
- Moran T, O'Hara M. A partner-rating scale of postpartum depression: the Edinburgh Postnatal Depression Scale - Partner (EPDS-P) Arch Women's Ment Health. 2006;9(4):173–180. doi: 10.1007/s00737-006-0136-x. [DOI] [PubMed] [Google Scholar]
- O'Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry. 1986;43(6):569–573. doi: 10.1001/archpsyc.1986.01800060063008. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, Swain M. Rates and risk of postpartum depression: aA meta-analysis. Int RevPsychiatry. 1996;8:37–54. [Google Scholar]
- Roberts SL, Bushnell JA, Collings SC, Purdie GL. Psychological health of men with partners who have post-partum depression. Aust N Z J Psychiatry. 2006;40(8):704–711. doi: 10.1080/j.1440-1614.2006.01871.x. [DOI] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM. A stage model of behavioral therapies research: getting started and moving on from Stage 1. Clin Psychol Sci Pract. 2001;8(2):133–142. [Google Scholar]
- Rush AJ, Kraemer HC, Sackeim HA, Fava M, Trivedi MH, Frank E, Ninan PT, Thase ME, Gelenberg AJ, Kupfer DJ, Regier DA, Rosenbaum JF, Ray O, Schatzberg AF. Report by the ACNP Task Force on response and remission in major depressive disorder. Neuropsychopharmacology. 2006;31(9):1841–1853. doi: 10.1038/sj.npp.1301131. [DOI] [PubMed] [Google Scholar]
- Segre LS, Stuart S, O'Hara MW. Interpersonal psychotherapy for antenatal and postpartum depression. Prim Psychiatry. 2004;11(3):52–56. 66. [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38(1):15–28. [Google Scholar]
- Spanier GB, Filsinger EE. The dyadic adjustment scale. In: Filsinger EE, editor. Marriage and family assessment: a sourcebook for family therapy. Beverly Hills: Sage; 1983. pp. 155–168. [Google Scholar]
- Spinelli M. Interpersonal psychotherapy for depressed antepartum women: a pilot study. Am J Psychiatry. 1997;154(7):1028–1030. doi: 10.1176/ajp.154.7.1028. [DOI] [PubMed] [Google Scholar]
- Spinelli M, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education for depressed pregnant women. Am J Psychiatry. 2003;160(3):555. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- Spinelli MA, editor. Interpersonal psychotherapy for antepartum depressed women. management of psychiatric disorders in pregnancy. London: Hodder Arnold; 2001. [Google Scholar]
- Stuart S. Interpersonal psychotherapy: a guide to the basics. Psychiatr Ann. 2006;36(8):542–550. [Google Scholar]
- Stuart S, Robertson M. Interpersonal psychotherapy: a clinician's guide. London: Arnold; 2003. [Google Scholar]
- Summerfeldt LJ, Antony MM. Structured and semistructured diagnostic interviews. New York: Guilford Press; 2002. [Google Scholar]
- Terry DJ, McHugh TA, Noller P. Role dissatisfaction and the decline in marital quality across the transition to parenthood. Aust J Psychol. 1991;43(3):129–132. doi: 10.1080/00049539108260136. [DOI] [PubMed] [Google Scholar]
- Wee KY, Skouteris H, Pier C, Richardson B, Milgrom J. Correlates of ante- and postnatal depression in fathers: a systematic review. J Affect Disord. 2011;130(3):358–377. doi: 10.1016/j.jad.2010.06.019. [DOI] [PubMed] [Google Scholar]
- Whiffen VE, Johnson SM. An attachment theory framework for the treatment of childbearing depression. Clin Psychol Sci Pract. 1998;5(4):478–492. [Google Scholar]
- Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, Ramin S, Chaudron L, Lockwood C. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114(3):703–713. doi: 10.1097/AOG.0b013e3181ba0632. [DOI] [PMC free article] [PubMed] [Google Scholar]