Abstract
Background and objective
Surgery in a paediatric setting stresses children and their parents. Previous studies have focused on children and the preoperative period; however, the 24 h after child surgery are highly stressful for parents as their child is still physically recovering and physician–parent communication is vital. The aims of this study are to investigate the impact of three levels of severity of paediatric surgery on mothers’ and fathers’ anxiety and stress and to identify factors that contribute to parental anxiety and acute stress symptoms in the first 24 h after child surgery.
Patients and methods
A total of 154 parents (91 mothers, 63 fathers) of children who had just undergone elective surgery for a major intervention (n = 41), minor intervention (n = 64) or day surgery (n = 49) completed questionnaires aimed at assessing levels of state anxiety and acute stress symptoms. Social network, socio-economic status and parental health locus of control were evaluated as contributors.
Results
Parents reported high levels of state anxiety (26% had scores on the state scale 2 standard deviations above the norm) and acute stress symptoms (28% in at least one of the four acute stress disorder symptom categories). Child’s type of surgery is related to parental anxiety [F(2,134) = 38.12, P = 0.0001, η2 = 0.175] and acute stress symptoms [F(2,133) = 31.21, P = 0.0001, η2 = 0.133]. Parental state anxiety was predicted by parent’s gender, trait anxiety and health external locus of control. Parent’s number of acute stress symptoms was predicted by parental trait anxiety, health external locus of control, parent’s level of education and the number of social contacts.
Conclusions
There is a need to take into consideration parental anxiety and distress in the 24 h after child surgery. Parental well-being is related to several characteristics including the severity of child surgery; these aspects should be taken into consideration when interacting with parents in the aftermath of their child’s surgery.
Keywords: paediatric surgery, parental anxiety and acute stress symptoms, parent–physician communication
Introduction
Surgery in a paediatric setting involves a considerable amount of stress for children and for their parents (Landolt et al. 1998, 2003; Hug et al. 2005). Because children depend on parents for support and guidance in coping with new or stressful situations, parents play a critical role in paediatric surgery (Piira et al. 2003). It is proven that high-quality maternal behavioural style exhibited in positive affect, attitudes and/or interaction may reduce the impact of the child’s biological vulnerability. However, the effectiveness of some parents in supporting their child may be compromised because they themselves become emotionally involved in the event (e.g. Ievers et al. 1994).
Peri-surgery distress in paediatric patients and parental pre-surgery distress have been previously studied; however, parental psychological response in the aftermath of their child’s surgery has never been investigated. This lack should be filled in as in this time window parents are of paramount importance because the child is still physically recovering, may experience physical reactions to surgery or anaesthesia, and is in need of parental comfort and support. Immediately after surgery, the child’s physical status may also prevent his or her direct communication with health professionals, and parents are responsible for information exchange with medical staff. Parents have a unique role in children’s pain management (Piira et al. 2003), but sometimes they have difficulties accepting the role of helping their child manage the stressful experience of surgery. In the aftermath of surgery, when the child is still undergoing treatment, parental anxiety and distress may be high, and it is a sensitive period for communication between parents and health professionals. In this time window, parents should collaborate with doctors and nurses to help the child cope with post-surgery distress, so they need to be competent and prepared to interact collaboratively with professionals in deciding appropriate care for their child (Becker & Grunwald 2000; Hurst 2001). However, parents who are psychologically distressed are less able to understand communications and take general information (Montgomery et al. 1999). Knowing which are those parents more at risk for high level of psychological distress, in the 24 h after their child’s surgery, may help professionals better direct their communicative efforts. It is worth noting that parental psychological responses vary in intensity and can be adaptive or may become disruptive to functioning (Kazak et al. 2004).
The aims of this study are to investigate the impact of three levels of severity of paediatric elective surgery on mothers’ and fathers’ anxiety and stress and to identify factors that contribute to parental anxiety and acute stress symptoms in the first 24 h after child surgery.
Methods
Participants
Altogether 154 parents (91 mothers and 63 fathers) corresponding to 154 children who underwent surgery in the previous 24 h participated in this study. Only one parent in one family was included because only one was allowed to be at the child’s bed in the 24 h after their child’s surgery; we expect that the parent present was the primary caregiver. Table 1 shows socio-demographic information, child characteristics and psychosocial covariates for both mothers and fathers. Of the 160 parents who were contacted, 96% agreed to participate and 4% refused for unspecified reasons. Patients were grouped following three main types of paediatric surgery intervention categories (Welch et al. 1986): patients in the day surgery group (32.47%) were hospitalized for 12–24 h for surgery such as testicular interventions (n = 30) or excision of cysts (n = 19). The minor intervention group (40.91%) included hospitalizations of more than 24 h for more intrusive surgeries such as tonsillectomy (n = 7), circumcision (n = 21), hypospadias (n = 15), gastroesophageal reflux (n = 14) and appendicitis (n = 14). Patients in the major intervention group (26.62%) had one of the major body cavities opened (the abdomen, the chest or the skull) that could stress vital organs: major congenital malformations (n = 14), laparotomy (n = 5), thoracotomy (n = 1), craniotomy (n = 10) and liver or kidney trauma (n = 4) (Welch et al. 1986). All of the three groups of surgeries were elective and planned; consequently, parents had been given information about it. No emergency interventions were included in the sample. The three groups of children did not significantly differ for number of previous medical experiences (i.e. surgeries or hospitalizations).
Table 1.
Characteristics of the sample
| All (n = 154) | Mothers (n = 91) | Fathers (n = 63) | |
|---|---|---|---|
| Type of surgery | |||
| Day surgery (%) | 50 | 30 (60) | 20 (40) |
| Minor intervention (%) | 63 | 40 (64) | 23 (36) |
| Major intervention (%) | 41 | 21 (51) | 20 (49) |
| Parent’s age (years) | |||
| Mean (SD) | 35.5 (6.42) | 36.3 (5.92) | 34.94 (6.72) |
| SES | |||
| Lower (%) | 37 | 23 (62) | 14 (38) |
| Middle (%) | 83 | 46 (55) | 37 (45) |
| Upper (%) | 35 | 23 (66) | 12 (34) |
| Parental education (years) | |||
| Mean (SD) | 13.18 (3.4) | 12.23 (4.12) | 14.15 (2.53) |
| Child’s age (years) | |||
| Mean (SD) | 4.08 (2.63) | 4.23 (2.59) | 3.86 (4.23) |
| Child’s gender | |||
| Male (%) | 95 | 67 (71) | 28 (29) |
| Female (%) | 59 | 24 (41) | 35 (59) |
| Parent’s number of social contacts | |||
| Mean (SD) | 60.19 (44.5) | 70.15 (51.82) | 50.23 (31.72) |
| Level of parental trait anxiety | |||
| Mean (SD) | 40.24 (11.17) | 43.48 (12.48) | 35.55 (8.65) |
| Parental health locus of control: internal* | |||
| Mean (SD) | 4.46 (1.02) | 4.5 (0.99) | 4.4 (1.06) |
| Parental health locus of control: external* | |||
| Mean (SD) | 3.20 (1.43) | 3.35 (1.48) | 2.99 (1.33) |
On a three-factor health locus of control 5-point scale.
SD, standard deviation; SES, socio-economic status.
Procedure and measures
The Ethics Committee of the hospital approved the study, and written consent was obtained from all parents. Parents were recruited at the child’s bedside. All children were hospitalized when parents filled in questionnaires.
Dependent measures were the State–Trait Anxiety Inventory (Spielberger et al. 1983) and the Post-traumatic Stress Symptom Inventory. This last one is a checklist of 19 symptoms described by the DSM-IV for acute stress disorder (ASD). Following Winston and colleagues (2002), we also describe the level of broad distress in terms of clinically significant levels of symptoms, that is, the presence of at least one symptom for each symptom category (Dissociation, Re-experiencing, Avoidance, Arousal).
Independent measures were the Social Network questionnaire (readapted from Weinraub & Wolf 1983) and the Parent Health Locus of Control Scale (De Vellis & De Vellis 1993) which assesses parents’ beliefs about the type of control (internal or external) over the health of their children. Individual scales correspond to beliefs in Child, Divine, Fate, Media, Parental and Professional Influence over child health.
Results
Results address two main questions regarding parental anxiety and acute stress: (i) Do parents report clinically significant levels of state anxiety and acute stress symptoms in the 24 h following their child’s surgery?; and (ii) What are the main sources of parental anxiety and the number of acute stress symptoms?
Mothers’ and fathers’ levels of state anxiety for the three different types of surgery are shown in Table 2. The first row shows the number of parents who reported clinically significant levels of state anxiety, and the second row reports mean levels of state anxiety. All parents manifest high levels of state anxiety. Altogether, 46.8% (n = 72) of parents had scores on the state scale which were 1–2 SDs (standard deviations) above the normal level of anxiety in the adult Italian population, and 26% (n = 40) of parents had scores which were 2 SDs or more above the norm. As shown in Table 2, the type of surgery was significant for both parents. Parents’ gender was also significant [F(1,153) = 6.55, P = 0.012 and η2 = 0.044], and mothers [mean (M) = 48.05, standard error (SE) = 1.56] were more anxious than fathers (M = 44.16, SE = 1.53).
Table 2.
Descriptive statistics
| All | Day surgery (n = 49) | Minor surgery (n = 64) | Major surgery (n = 41) | F | P-value | |
|---|---|---|---|---|---|---|
| Mothers | n = 91 | n = 29 | n = 41 | n = 21 | d.f. = 2,88 | |
| Clinically significant state anxiety (n/%) | 15 (16.5) | 0 | 3 (3.3) | 12 (13.2) | ||
| State anxiety levels (M/SD) | 48.05 (14.29) | 39.38 (10.41)a | 47.53 (11.45)b | 61.05 (14.74)c | 19.99 | ≤0.001 |
| Acute stress present (n/%)* | 25 (27.5) | 2 (2.2) | 9 (9.9) | 14 (15.4) | ||
| Acute stress symptom (n/SD) | 4.43 (4.65) | 1.58 (2.38)a | 4.34 (4.29)b | 8.52 (4.84)c | 18.94 | ≤0.001 |
| Dissociation (n/%) | 25 (27.47) | 2 (2.2) | 9 (9.9) | 14 (15.38) | ||
| Re-experiencing (n/%) | 50 (54.9) | 7 (7.7) | 11 (12.1) | 32 (35.16) | ||
| Avoidance (n/%) | 15 (16.5) | 0 | 7 (7.7) | 8 (8.8) | ||
| Arousal (n/%) | 24 (26.4) | 3 (3.3) | 10 (11) | 11 (12.1) | ||
| Fathers | n = 63 | n = 20 | n = 23 | n = 20 | d.f. = 2,60 | |
| Clinically significant state anxiety (n/%) | 6 (9.5) | 0 | 1 (1.6) | 5 (7.9) | ||
| State anxiety levels (M/SD) | 44.16 (12.10) | 38.00 (8.20)a | 41.65 (10.07)a | 53.20 (12.64)b | 11.63 | ≤0.001 |
| Acute stress present (n/%)* | 18 (28.6) | 4 (6.3) | 2 (3.2) | 12 (19) | ||
| Acute stress symptom (M/SD) | 4.56 (4.53) | 3.55 (4.25)a | 2.48 (2.48)a | 7.95 (4.84)b | 11.36 | ≤0.001 |
| Dissociation (n/%) | 11 (17.18) | 2 (3.2) | 4 (6.3) | 5 (7.9) | ||
| Re-experiencing (n/%) | 35 (55.6) | 4 (6.3) | 12 (19) | 19 (30.16) | ||
| Avoidance (n/%) | 15 (23.8) | 2 (3.2) | 2 (3.2) | 11 (17.5) | ||
| Arousal (n/%) | 15 (23.8) | 4 (6.3) | 2 (3.2) | 9 (14.3) |
Subgroups with different superscript letters are significantly different adjusting for Bonferroni inequality (α = 0.0167).
At least one clinically significant symptom present in each symptom category for acute stress symptoms (Dissociation, Re-experiencing, Avoidance, Arousal).
d.f., degree of freedom; SD, standard deviation.
An ANCOVA was conducted with state anxiety as the dependent variable, type of surgery and parent’s gender as factors, and parent’s and child’s age, parent’s level of education, number of social contacts, parental trait anxiety, internal and external PHLoC (parent health locus of control) as covariates. All independent variables were entered as covariates as a single block before the factors. No significant interaction was found between type of surgery and parent’s gender. Table 3 shows that the type of surgery highly influenced parental state anxiety, and uniquely explained 17% of the variance.
Table 3.
ANCOVA with parental levels of state anxiety as dependent variable
| F | d.f. | η2 | P < 0.05 | Coefficients estimate (β) | |
|---|---|---|---|---|---|
| Type of child surgery | 18.85 | 2 | 0.174 | 0.001 | Minor vs. Day 7.74, t(152) = 1.93, P = 0.005 Major vs. Day 17.79, t(152) = 4.06, P = 0.001 |
| Parent’s gender | 6.07 | 1 | 0.013 | 0.007 | Mothers vs. Fathers 4.51, t(152) = −1.37, P = 0.173 |
| Parent’s age | 2.24 | 1 | 0.016 | ns | |
| Parent’s level of education | 0.37 | 1 | 0.003 | ns | |
| Child’s age | 0.35 | 1 | 0.003 | ns | |
| Number of social contacts | 0.12 | 1 | 0.001 | ns | |
| Parental trait anxiety | 14.04 | 1 | 0.113 | 0.001 | 0.368 |
| PHLoC: internal influence | 2.27 | 1 | 0.016 | ns | |
| PHLoC: external influence | 7.63 | 1 | 0.051 | 0.007 | −1.811 |
| Group error | 141 |
R2 = 0.489 (adjusted R2 = 0.446).
d.f., degree of freedom; ns, not significant; PHLoC, parent health locus of control.
Parent’s gender, parental trait anxiety and PHLoC external influence were significant predictors. Mothers were significantly more anxious than fathers, and parents who were more endogenously anxious (trait) were also more anxious in this specific situation (state). Parental health locus of control (external influence) predicted lower levels of state anxiety.
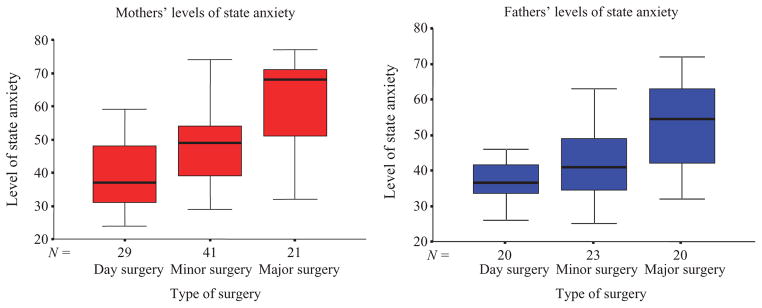
Figure 1 shows that mothers’ state anxiety increased monotonically as the type of child surgical intervention became more severe, and fathers’ state anxiety increased only for major surgery.
Figure 1.
Distributions of mothers’ and fathers’ level of anxiety in relation to different types of surgery.
Mothers’ and fathers’ number of acute stress symptoms for the three different types of child surgery is shown in Table 2. Forty-three parents (27.9%) reported symptoms present in at least one of the four ASD symptoms categories. Re-experiencing was the symptom category most often reported by both parents (n = 85, 55.2%), and Avoidance the least (n = 30, 19.5%). Mothers’ and fathers’ distress did not differ [F(1,153) = 0.028, not significant]. Only 24 parents (16%) met the DSM-IV criteria for ASD, that is, at least one symptom for re-experiencing, three symptoms for dissociation, one symptom for avoidance and one for arousal. All these parents had anxiety levels ≥2 SDs above norm. This high-risk group was predominantly found in the major surgeries (n = 18).
An ANCOVA was conducted with number of acute stress symptoms as dependent variable, type of surgery as factor and independent variables (Table 1) as covariates. As shown in Table 4, no interactions emerged and the type of surgery explained 13% of the variance. Also, parent’s level of education, number of social contacts, trait anxiety and parental health locus of control (external influence) were predictor variables. Parents with higher level of education and health locus of control (external influence) experienced a lower number of acute stress symptoms. Again, parents with a higher trait anxiety also had more acute stress symptoms.
Table 4.
ANCOVA with parental number of acute stress symptoms as dependent variable
| F | d.f. | η2 | P < 0.05 | Coefficients estimate (β) | |
|---|---|---|---|---|---|
| Type of child surgery | 12.72 | 2 | 0.153 | 0.001 | Minor vs. Day 3.63, t(152) = 0.26, P = 0.049 Major vs. Day 5.31, t(152) = 3.52, P = 0.001 |
| Parent’s gender | 1.33 | 1 | 0.009 | ns | |
| Parent’s age | 0.20 | 1 | 0.001 | ns | |
| Parent’s level of education | 7.39 | 1 | 0.050 | 0.007 | −1.19 |
| Child’s age | 0.19 | 1 | 0.001 | ns | |
| Number of social contacts | 13.33 | 1 | 0.086 | 0.001 | 0.03 |
| Parental trait anxiety | 8.96 | 1 | 0.059 | 0.003 | 0.09 |
| PHLoC: internal influence | 0.67 | 1 | 0.005 | ns | |
| PHLoC: external influence | 6.70 | 1 | 0.045 | 0.01 | −0.59 |
| Group error | 133 |
R2 = 0.465 (adjusted R2 = 0.419).
d.f., degree of freedom; ns, not significant; PHLoC, parent health locus of control.
Discussion
The anxiety and stress of most parents of children who underwent surgery in the previous 24 h were within normal limits. However, more than 25% of our sample showed clinically significant state anxiety and 16% met criteria suggestive of ASD. Children’s type of surgery related to parental levels of anxiety and distress. Both mothers and fathers showed higher anxiety and distress when their children underwent a major surgery as compared with day surgery. However, mothers also showed significantly higher levels of anxiety as compared with fathers (Norberg et al. 2005). This may be because in Italy (as we suspect elsewhere) it is principally mothers who spend day and night next to the child during the post-surgical period. Also, women may be more sensitive to degrees of child risk than men.
The number of parents’ symptoms of acute stress increases in intensity of surgical intervention. High distress was linked not only with parents’ trait anxiety, but also with their number of social contacts and years of education. Parents who feel worst appear to be more in need of support and help from other people, such as relatives and friends. Parents with more years of education suffer fewer acute stress symptoms and appear to be more able to cope with their child’s situation. In addition, parents’ beliefs about external control of the health of their child related to their level of anxiety. Parental external health locus of control was associated, in our sample, with lower levels of anxiety; this is different to what has been reported in the literature where external locus of control reflects decreases in parents’ perceived personal control over their child’s health and is associated with higher levels of anxiety and distress (Kain et al. 2006; Wijnberg-Williams et al. 2006). The reason for this result may be dictated by the fact that locus of control may fluctuate with environmental events. After the child’s surgery, parents who are more likely to attribute medical outcomes to doctors instead of their own efforts may report lower levels of anxiety and stress as they rely in healthcare providers.
These findings should be interpreted with caution because of a number of limits. First, we only considered parental anxiety and distress, and assessment of children’s reactions would have been useful as well. However, in the critical window that immediately follows child surgery, child assessment is not always possible because of sedation and post-intervention status. Second, we measured parents’ anxiety and acute distress symptoms only during the 24 h following their children’s surgery; further testing is needed to show whether and how parental distress waxes or wanes as time after surgery goes by. Third, only one caregiver from a family was included in the study; both parents would have allowed individuating different possible patterns of post-traumatic stress symptoms and anxiety in the family unit.
Clinical implications
Contacts and communication between doctors, nurses or other healthcare professionals with parents in paediatric surgery are routine. In such settings, parents’ compliance during the pre-and post-operative period is crucial. In addition, communication as well as exchange of information between patients and health professionals is more frequent and more important in the immediate aftermath of surgery than later on. After child surgery, the recipients of such information are principally parents, because children are often unable to sustain or understand this information on account of their age or the short-term consequences of anaesthesia or analgesia. Parents’ anxiety or distress at the time may interfere with their ability to communicate with health professionals and so correctly understand physicians’ explanations and prescriptions. As a matter of fact, parents who are psychologically distressed are less able to take in information and do not simply need more information as a consequence of their disorder, but rather need to be engaged in a different kind of information-sharing process (Montgomery et al. 1999).
Our results identified some factors that impact on parental distress, in particular parental levels of anxiety and stress symptoms: type of child surgery and parent’s gender. As state anxiety and acute stress increase, parents need more targeted care (Scrimin et al. 2005), that is, more support and information to better understand post-operative treatments, pain or problems.
Some suggestions might be given in relation to our results. First, the type of child surgery (day surgery vs. minor surgery vs. major surgery) should be taken into primary consideration by healthcare professionals leading to differentiated supportive care. Parents of children who undergo major surgery deserve special attention because they are the group most at risk for developing high levels of anxiety or acute stress symptoms. For this reason, health professionals might tender support and information to both parents repetitively. In addition, parents of children who underwent major surgery should be given the opportunity to consult a psychologist. However, comprehensive information about post-operative care should be given to all parents of children who underwent surgery including day surgery or minor surgery (universal care) (Kazak et al. 2004; Scrimin et al. 2005). Second, healthcare professionals can enhance parental adjustment to child surgery and foster more effective communication by acknowledging and responding to differences between mothers and fathers. For example, when dealing with children’s day or minor surgery, special supportive care should focus on mothers, and in the context of children’s major surgeries, both mothers and fathers are in need of targeted attention. It is then useful to monitor the number of relatives and friends who visit because parents need to be supported by other people. Parents should be offered more support with more frequent talks and communication aimed at giving more information about their child or clarifying aspects that parents may not have completely understood. And parents who have external perceptions of the control on their child’s health suffer the most. For this reason, it might be useful to assign parents small tasks regarding their child’s health (i.e. measuring their child’s temperature) from the beginning of hospitalization to increase parents’ perceptions of internal control vis-à-vis their child’s well-being. Last, when there is a need to communicate and give or gather information, it is useful to interact with both parents. In this way, mothers and fathers may better understand the message and choose to give more importance to either the instrumental or the affective behaviours that are aimed at improved communication. That is, when consulting a health professional, patients have two basic needs: cognitive need (to be informed, to know and to understand) and emotional need (to be taken seriously, to feel known and understood). Healthcare professionals are assumed to possess instrumental skills (problem-solving, asking questions and providing information) and socio-emotional skills (establishing a therapeutically effective relationship, reflecting feelings and showing empathy and concern). Depending on the specific needs of the patient, or parent, and the goal of the interview, a balance between instrumental and affective behaviours should characterize effective communication. It is likely that different combinations of behaviours are used by health professionals to achieve more effective interactions with parents who have different anxiety and stress characteristics.
Key messages.
Our results identified the type of child surgery and parent’s gender as main factors related to parental levels of anxiety and stress symptoms.
Parents, especially mothers, may be anxious also in response to minor child surgeries.
The type of child surgery (day surgery vs. minor surgery vs. major surgery) should be taken into primary consideration by healthcare professionals leading to differentiated supportive care.
Healthcare professionals should acknowledge the differences between mothers and fathers: when dealing with children’s minor surgery, special supportive care should focus on mothers, and in the context of children’s major surgeries, both parents are in need of targeted attention.
When there is a need to communicate and give or gather information, it is useful to interact with both parents to allow better understanding of the message and improve communication.
References
- Becker PT, Grunwald PC. Contextual dynamics of ethical decision making in the NICU. Journal of Perinatal Neonatal Nursing. 2000;14:58–72. doi: 10.1097/00005237-200009000-00007. [DOI] [PubMed] [Google Scholar]
- De Vellis BM, De Vellis RF. Development and validation of the parent health locus of control scale. Health Education Quarterly. 1993;20:211–225. doi: 10.1177/109019819302000213. [DOI] [PubMed] [Google Scholar]
- Hug M, Tonz M, Kaiser G. Parental stress in paediatric day-case surgery. Pediatric Surgery International. 2005;2:94–99. doi: 10.1007/s00383-004-1333-1. [DOI] [PubMed] [Google Scholar]
- Hurst I. Mothers’ strategies to meet their needs in the newborn intensive care nursery. Journal of Perinatal Neonatal Nursing. 2001;15:65–82. doi: 10.1097/00005237-200109000-00006. [DOI] [PubMed] [Google Scholar]
- Ievers CE, Drotar D, Dahms WT, Doershuk CF, Stern RC. Maternal child-rearing behavior in three groups: cystic fibrosis, insulin-dependent diabetes mellitus, and healthy children. Journal of Pediatric Psychology. 1994;19:681–687. doi: 10.1093/jpepsy/19.6.681. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Mayes LC, Caldwell-Andrews AA, Saadat S, McClain B, Wang SM. Preoperative anxiety and postoperative pain and behavioural recovery in young children undergoing surgery. Pediatrics. 2006;118:651–658. doi: 10.1542/peds.2005-2920. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Alderfer AM, Rourker MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. Journal of Pediatric Psychology. 2004;29:211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- Landolt M, Boehler U, Schwager C, Schallberger U, Nuessli R. Post traumatic stress disorder in paediatric patients and their parents: findings from an exploratory study. Journal of Paediatrics and Child Health. 1998;34:539–543. doi: 10.1046/j.1440-1754.1998.00303.x. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath M, Ribi K. Incidence and associations of parental and child posttraumatic stress symptoms in paediatric patients. Journal of Child Psychology and Psychiatry. 2003;44:1199–1207. doi: 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- Montgomery C, Lydon A, Lloyd K. Psychological distress among cancer patients and informed consent. Journal of Psychosomatic Research. 1999;46:241–245. doi: 10.1016/s0022-3999(98)00089-0. [DOI] [PubMed] [Google Scholar]
- Norberg AL, Lindblad F, Boman KK. Parental traumatic stress during and after paediatric cancer treatment. Acta Oncologica. 2005;44:382–388. doi: 10.1080/02841860510029789. [DOI] [PubMed] [Google Scholar]
- Piira T, Sugiura T, Champion GD, Donnelly N, Cole ASJ. The role of parental presence in the context of children’s medical procedures: a systematic review. Child: Health, Care and Development. 2003;31:233–243. doi: 10.1111/j.1365-2214.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Scrimin S, Axia G, Tremolada M, Pillon M, Capello F, Zanesco L. Conversational strategies with parents of newly diagnosed leukemic children: an analysis of 4880 conversational turns. Supportive Care in Cancer. 2005;13:287–294. doi: 10.1007/s00520-004-0679-1. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State–Trait Anxiety Inventory (Form Y) Consulting Psychologists Press; Palo Alto, CA, USA: 1983. [Google Scholar]
- Weinraub M, Wolf BM. Effect of stress and social supports on mother–child interactions in single and two parent families. Child Development. 1983;54:1297–1311. [PubMed] [Google Scholar]
- Welch KJ, Randolph JG, Ravitch MM, O’Neill JA, Rowe MI. Paediatric Surgery. 4. Year Book Medical Publishers; Chicago, IL, USA: 1986. [Google Scholar]
- Wijnberg-Williams BJ, Kamps WA, Klip EC, Hoekstra-Weebers JE. Psychological adjustment of parents of pediatric cancer patients revisited: five years later. Psychooncology. 2006;15:1–8. doi: 10.1002/pon.927. [DOI] [PubMed] [Google Scholar]
- Winston FK, Kassam-Adams N, Vivarelli-O’Neill C, Ford J, Newman E, Baxt C. Acute distress disorder symptoms in children and their parents after paediatric traffic injury. Paediatrics. 2002;109:90–97. doi: 10.1542/peds.109.6.e90. [DOI] [PubMed] [Google Scholar]