Abstract
Motivational Interviewing (MI) is a widely-used approach for addressing adolescent substance use. Recent meta-analytic findings show small but consistent effect sizes. However, differences in intervention format and intervention design, as well as possible mediators of change, have never been reviewed. This review of the literature summarizes the most up-to-date MI interventions with adolescents, looks at differences between intervention format and design, and discusses possible theory-based mechanisms of change. Of the 39 studies included in this review, 67% reported statistically significant improved substance use outcomes. Chi square results show no significant difference between interventions using feedback or not, or interventions combined with other treatment versus MI alone. The need for systematic investigation in theory-based mechanisms of change is presented.
Keywords: Motivational Interviewing, Adolescent, Substance Use, Alcohol, Tobacco, Marijuana
1. Introduction
A recent review by Macgowan and Engle (2010) reports that Motivational Interviewing (MI) has met the American Psychological Association’s criteria for promising treatments of adolescent substance use. MI is a client-centered counseling style directed at exploring and resolving ambivalence about changing personal behaviors (Miller & Rollnick, 2002). It differs from other treatments in that its purpose is not to impart information or skills. Rather, it emphasizes exploring and reinforcing clients’ intrinsic motivation toward healthy behaviors while supporting their autonomy. The first meta-analytic review of MI’s use with adolescents shows an overall small effect size (d = .173, 95% CI [.094, .252] N = 21) (Jensen et al., 2011). Theoretically, MI appears to be a good fit with adolescents’ developmental need to exert their independence and make decisions for themselves, while it respects their heightened levels of psychological reactance and coincides with the development of their decision-making skills (Baer & Peterson, 2002; Naar-King & Suarez, 2011).
Despite the popularity of using MI among teens, outcomes vary and effect sizes tend to be small (Jensen et al., 2011). One explanation for this variation may be related to intervention characteristics. Interventions vary with respect to treatment format or modality (e.g., group, individual, telephone, in-person, internet), and intervention design (e.g., providing assessment and feedback, pre-treatment adjunct, or post-treatment follow-up.) Understanding the influence of these characteristics can help program developers design the most effective interventions and may facilitate larger effect sizes.
In addition to understanding the influence of intervention characteristics, understanding the possible mechanisms of change working in MI interventions can also help improve program effectiveness. Apodaca and Longabaugh’s (2009) recent meta-analysis of MI’s mechanisms of change includes only one study of adolescents (McCambridge & Strang, 2004) and finds evidence that client change language (Moyers, Martin, Manuel, Hendrickson, & Miller, 2005; Moyers et al., 2007), client experience of discrepancy (McNally, Palfai, & Kahler, 2005), and certain techniques, such as decisional balance (Strang & McCambridge, 2004; LaBrie, Feres, Kenney, & Lac, 2009) are positively related to improved outcomes.
However, Apodaca and Longabaugh (2009) find evidence for client readiness, client engagement, client resistance, and client confidence to be inconsistent. They conclude that although the theories underlying MI are rich, they are not integrated into a formal and comprehensive theory, making it difficult to pursue investigations of the mechanisms of change. Applying more theory-based structure to MI intervention design and content appears warranted.
This review sets out to 1) update existing reviews with recently published adolescent MI interventions; 2) review the ability of different intervention formats to influence outcomes; 3) review the ability of different intervention designs (e.g., feedback or adjunct treatment) to influence outcomes; and 4) explore possible underlying theory-based mechanisms of change.
2. Methods
2.1 Data Sources
The article search was conducted by the first author. EB identified articles by scanning those listed on the Motivational Interviewing website (www.motivationalinterviewing.org) and reviewing all existing literature reviews of MI with adolescent substance users. Reference lists of these articles were further reviewed for relevant studies. Next, literature searches were conducted between November 1, 2011 to January 15, 2012 using the online databases Google Scholar, Medline Ovid, and PsychINFO, using the following search terms: adolescent, teen, substance use, marijuana, tobacco, smoking, alcohol, drugs, motivational interviewing, motivational intervention, motivational enhancement and brief intervention. Only peer-reviewed papers published in English were considered; no geographical limits were used.
2.2 Inclusion Criteria
Inclusion criteria for this review were these: 1) study subjects with a mean age of <18.5 years old, 2) studies had to report interventions based in MI techniques, 3) studies had to be experimental or quasi-experimental designs, and 4) papers must have presented results from a quantitative investigation on the efficacy of MI to improve substance use outcomes. Substance use included alcohol, tobacco, marijuana, hard drugs, or any combination.
2.3 Data Classification and Analytic Plan
Studies were first coded for quality. A continuous measure was developed to reflect whether the article reported the presence or absence of 1) using a manual to guide the intervention, 2) training and supervision of interventionists, and 3) coding of recorded MI sessions to determine fidelity to MI. Studies were further coded as being either individual or group formats, and utilizing face to face, telephone, computer or a combination of these modalities. We also categorized papers based on intervention design types originally identified in published meta-analyses (Burke, Arkowitz, & Menchola, 2003; Hettema, Steele, & Miller, 2005; Lundahl & Burke, 2009). These three reviews identify interventions whereby MI is delivered alone (MIO), MI is delivered with feedback (MIF), MI is delivered with another intervention (MI +), and finally, where MI is delivered with feedback and another intervention (MIF +). Chi-square Goodness of Fit analysis was utilized to determine significant differences among intervention design types. All coding was conducted by two authors (EB and CS); all disagreements were resolved through discussion. If a program had positive and negative substance use outcomes it was coded as no-effect; if outcomes were positive but not maintained at a longer follow-up, it was coded as positive.
For this review, MIO is defined as interventions that a) do not begin with assessment feedback and b) do not explicitly attempt to combine treatments. These interventions attempt to enhance motivation through the use of MI to explore and resolve ambivalence about change, and elicit client change language. Such interventions frequently examine the costs and benefits of change, discuss client goals and values and how using substances fit with these, explore past successes at behavior change or character strengths that would assist with behavior change, and utilize importance, confidence and readiness rulers that encourage clients to articulate reasons for change (Miller & Rollnick, 2002).
MIF approaches are identifiable by the use of personalized assessment feedback given to the client. Feedback can be provided in-person, on paper, via a computer, or over the phone. In these interventions, participants complete some form of a problem behavior assessment (e.g., Drinker’s, Smoker’s, or Cannabis Check-Up; Miller & Sovereign, 1989). Assessment results are then a) reviewed with the client in person or by telephone, or b) given as written feedback or via a computer interface (e.g., Internet, laptop or kiosk) (Walker, Roffman, Picciano, & Stephens, 2007). In addition to personal information about quantities, patterns and consequences of use, the results typically include a comparison to clinical or population norms. MIF interventions typically range from one session of feedback to the four-session manualized Motivational Enhancement Therapy (MET) developed in Project Match (Miller, Zweben, DiClemente, & Rychtarik,1992).
MI + interventions either a) use MI to enhance client motivation to participate in a subsequent treatment (e.g., using MI to encourage Alcoholics Anonymous group attendance, or participation in group skill-based training (Brown & Miller, 1993), b) represent a follow-up to another treatment (e.g., after an inpatient treatment program) (Kaminer, Burleson, & Burke, 2008) or c) encourage movement back and forth between the use of MI and another treatment (e.g., a counselor would use an MI approach when ambivalence arises about using the skills being taught in a cognitive behavioral program) (Simpson, Zuckoff, Page, Franklin, & Foa, 2008).
MIF + approaches include the skills of MI, the use of assessment feedback, and typically the inclusion of cognitive behavior skills training. Although the original four-session MET specifically prohibited the teaching of sobriety or refusal skills, current studies using MET often do include skills training. Hence it is important to clearly identify the components being used in interventions as intervention names are not consistently used or understood (Godley et al., 2010).
3. Results
3.1 Description of Included Studies
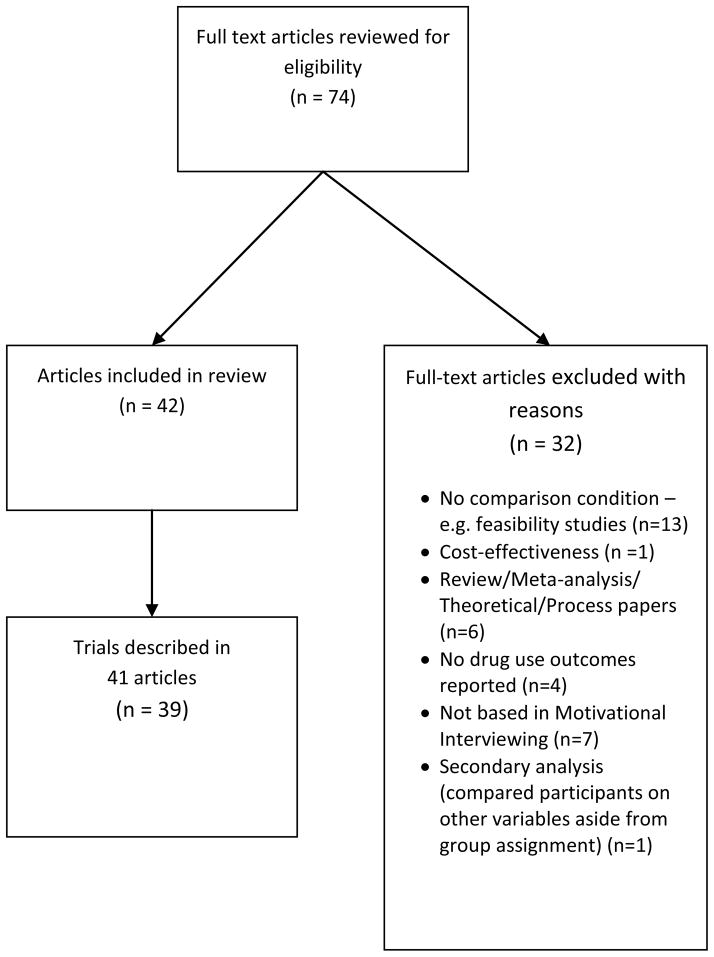
Forty-two articles met the inclusion criteria, although three publications reported additional outcomes from earlier trials. Therefore, the results from 39 unique MI trials were examined (see Figure 1 for Flow Chart). The trials targeted alcohol use (n = 9), tobacco use (n = 10), marijuana use (n = 9), substance use (n = 13), and other drugs (n = 1) (see specific studies in Table 1). Sample size in the studies ranged from <50 (n = 6), 50–99 (n = 6), 100–399 (n = 21), > 400 (n = 6). Participants were recruited from educational settings (n = 14), medical settings (n = 12), community-based services/treatment centers (n = 11), and juvenile correctional facilities (n = 2).
Figure 1.
Flow chart for articles included in the review.
Table 1.
Description of Studies Included in the Review
| Author | Year | Sample Size | Drug | Mean Age | Gender (%male) | Research Design | Follow-up | Findings | Outcome (sig at p < .05) | Ind/Gr | Intervention Design | Format/Modality | Total Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Audrain- McGovern et al. | 2011 | 355 | Tobacco | 14–18 | 45% | RCT | 3, 6 months | MI led to significantly fewer attempts to quit smoking and no differences in abstinence, but it did lead to significantly fewer cigarettes smoked. | No Effect | Ind | MIF | F2F + Tel | 2 |
| Baer, Garrett, Beadnell, Wells, & Peterson | 2007 | 117 | Substance Use | 17.9 | 56% | RCT | 1,3 months | MI did not significantly decrease substance use. MI did significantly increase service utilization. MI did not significantly increase engagement. | No Effect | Ind | MIF | F2F | 1 |
| Bailey, Baker, Webster, & Lewin | 2004 | 34 | Alcohol | 15.44 | 50% | RCT | 1,2 months | MI significantly increased readiness to change and alcohol knowledge. MI significantly decreased drinking frequency post-treatment and at 1-month follow-up. | Positive | Group | MI + | F2F | 1 |
| Battjes, Gordon, O’Grady, Kinlock, kKtz, & Sears | 2004 | 194 | Substance Use | 15.9 | 85% | Quasi Experimental | 6,12 months | Significant reductions marijuana at 6 & 12 months | Positive | Group | MI + | F2F | 2 |
| Brown et al. | 2003; 2009 | 191 | Tobacco & Substance Use | 15.4 | 38% | RCT | 1,3,6,9,12 months | MI did not significantly decrease smoking. MI significantly increased self efficacy. MI was significantly more effective than BA for adolescents with little or not intention to quit. | No Effect | Ind | MIF + | F2F + Tel + Parent | 1 |
| Colby et al. | 2005 | 85 | Tobacco | 16.3 | 71% | RCT | 1,3,6 months | MI significantly decreased self- reported smoking rate at 1-month, 3-month, and 6-month follow-up, and significantly reduced cotinine markers at 3-month follow-up, and significantly increased smoking abstinence as measured by self-report (but not biochemically) at 6-month follow- up. | Positive | Ind | MIF | F2F | 2 |
| Colby et al. | 1998 | 40 | Tobacco | 16.15 | 43% | RCT | 3 months | MI did not significantly reduce smoking. | No Effect | Ind | MIF + | F2F | 1 |
| D’Amico, Miles, Stern, & Meredith | 2008 | 42 | Substance Use | 16 | 48% | RCT | 3 months | MI significantly reduced (self- reported) marijuana use, preception of prevalence of marijuana use, number of friends using marijuana, and intentions to use marijuana. | Positive | Ind | MIO | F2F + Tel | 1 |
| Dennis et al. | 2004 | 300 | Marijuana | 13–18 | 81% | RCT | 3,6,9,12 months | All conditions had signficant pre/post results. MI interventions appeared most cost-effective. | Positive | Ind | MI + | F2F | 2 |
| Godley et al. | 2010 | 320 | Marijuana | 13–18 | 76% | RCT | 3, 6, 9, 12 months | MI group showed significantly increased abstinance and was most cost effective, but was not the most effective intervention in the trial. | Positive | Both | MIF + | F2F | 2 |
| Goti et al. | 2010 | 103 | Substance Use | 15.2 | 24% | RCT | 1 month | MI did not significantly decrease substance use. MI did significantly increase drug knowledge and perceptions of risks due to drug use. | No Effect | Ind | MIF + | F2F | 2 |
| Gray, McCambridge, & Strang | 2005 | 162 | Substance Use | 17.46 | 47% | Quasi Experimental | 3 months | MI participants drinking on average two days per month less than controls after 3 months, a significant difference. | Positive | Ind | MIO | F2F | 1 |
| Grenard et al. | 2007 | 18 | Substance Use | 16.1 | 67% | RCT | 3 months | Significant reductions in hard drugs, club drugs, # drinks in past week compared to controls. | Positive | Ind | MIF | F2F | 0 |
| Hollis et al. | 2005 | 2524 | Tobacco | 15.433 | 41% | RCT | 1,2 years | MI led to significantly greater abstinence after 2 years, particularly for those identifying as “smokers.” | Positive | Ind | MI + | F2F + Tel + Computer | 1 |
| Horn, Dino, Hamilton, & Noerachmanto | 2007 | 75 | Tobacco | 17.8 | 43% | RCT | 1,3,6 months | MI did not significantly reduce smoking. | No Effect | Ind | MIF | F2F + Tel | 1 |
| Kaminer, Burleson, & Burke; Burleson, Kaminer, & Burke | 2008; 2012 | 144 | Alcohol | 15.9 | 67% | RCT | 3,6,12 month | MI showed trends (p < .10) toward fewer alcoholic beverages per month over 12 months compared to control. No difference between Tel vs. in person. Aftercare participants had reduced risk of relapse and fewer drinking days. No difference between Tel vs In. | No Effect | Ind | MI + | F2F vs Tel | 0 |
| Kelly & Lapworth | 2006 | 56 | Tobacco | 15 | 66% | RCT | 1,3,6 | MI significantly decreased smoking at 1 month, but no significant differences at 3 months or 6 months. | Positive | Ind | MIO | F2F | 2 |
| Marsden et al. | 2006 | 342 | Ectasy, cocaine, crack- cocaine | 18.4 | 66% | RCT | 6 months | No significant differences compared to controls. | No Effect | Ind | MIF | F2F | 1 |
| Martin & Copeland | 2008 | 40 | Marijuana | 16.5 | 68% | RCT | 3 months | MI significantly decreased marijuana use and dependence symptoms. | Positive | Ind | MIF | F2F | 1 |
| Mason, Pate, Drapkin, & Sozinho | 2011 | 28 | Substance Use | 16 | 0% | RCT | 1 month | MI led to significantly less trouble due to alcohol use, less substance use before sexual intercourse, less offers for marijuana use, increased readiness to start counseling, less social stress, and greater satisfaction with the intervention. | Positive | Ind | MIF + | F2F | 3 |
| McCambridge & Strang | 2004; 2005 | 200 | Substance Use | 17.56 | 54% | GRT | 3, 12 months | MI significantly decreased cigarette, alcohol, and marijuana use. The effects disappeared by 12 months. | Positive | Ind | MIO | F2F | 1 |
| McCambridge, Slym, & Strang | 2008 | 326 | Marijuana | 17.95 | 69% | RCT | 3,6 months | No significant differences between groups. | No Effect | Ind | MIO | F2F | 2 |
| McCambridge, et al. | 2011 | 416 | Substance Use | 17.6 | 54% | Cluster RCT | 3,12 months | no statistically significant between-group differences in intention-to-treat analyses for either cigarette smoking or alcohol consumption outcomes. | No Effect | Ind | MIO | F2F | 1 |
| Monti et al. | 1999 | 94 | Alcohol | 18.4 | 64% | RCT | 3,6 moths | MI significantly decreased drinking and driving, traffic violations, alcohol-related injuried, and alcohol-related problems. There was no difference in reduction of alcohol consumption--both groups decreased use. | Positive | Ind | MIF | F2F | 1 |
| Pbert et al. | 2006 | 1148 | Tobacco | 16.85 | 37% | GRT | 6 wks, 3 months | MI significantly increased smoking abstinence at 6 weeks and 3 months. | Positive | Ind | MIO | F2F | 2 |
| Peterson et al. | 2009 | 2151 | Tobacco | approx. 16–17 | 53% | GRT | 7 days, 1,3, 6 months | MI has marginally significant (p < .10) and significant (p < .05) effects on increased prolonged smoking abstinence and duration since last cigarette at 7 days, 1 month, and 3 months. | Positive | Ind | MI + | Tel | 2 |
| Peterson, Baer, Wells, Ginzler, & Garrett | 2006 | 285 | Substance Use | 17.4 | 55% | RCT | 1,3 months | MI significantly reduced illicit drug use at 1 month. No differences for alcohol or marijuana. | Positive | Ind | MIF | F2F | 1 |
| Spirito et al. | 2004 | 152 | Alcohol | 15.6 | 64% | RCT | 3,6,12 | Significantly reduced alcohol use for those reporting high problem severity at baseline. No effect on related behaviors and problems. | Positive | Ind | MIF | F2F | 1 |
| Spirito et al. | 2011 | 125 | Alcohol | 15.45 | 29% | RCT | 3,6,12 | Drinking was significantly lower after MI at 3, 6, and 12 months, although the reductions were less dramatic over time. Family intervention improved outcomes over individual treatment. | Positive | Ind | MIF | F2F | 1 |
| Stein et al. | 2011 | 162 | Alcohol and Marijuana | 17.1 | 84% | RCT | 3 months | Led to significantly lower rates of alcohol and marijuana use. | Positive | Ind | MIF | F2F | 1 |
| Stein, Colby, Barnett,Monti, Golembeske, & Lebeau-Craven | 2006 | 105 | Alcohol and Marijuana | 17.06 | 90% | RCT | 3 months | MI led to significantly lower rates of drinking and driving, and riding in the car with a drunk driver. Similar trends were found for marijuana, but were nonsignificant. | Positive | Ind | MIF | F2F | 1 |
| Sussman, Sun, Rohrbach, & Spruijt-Metz | 2011 | 1186 | Substance Use | 16.8 | 57% | GRT | 12 months | School-based curriculum (with or without MI), showed significant reductions in alcohol use, hard drug use, and cigarette smoking. MI did not lead to further reductions. | No Effect | Ind | MI + | F2F + Tel | 2 |
| Thush et al. | 2009 | 125 | Alcohol | 17.07 | 41% | RCT | 1 month | No significant difference in drinking behavior. | No Effect | Ind | MIF | F2F | 3 |
| Waldron, Slesnick, Brody, Turner & Peterson | 2001 | 114 | Marijuana | 15.61 | 80% | RCT | 4,7 months | MI + showed some efficacy: significant change from heavy to minimal use from pretreatment to 4 month follow-up, although did not persist to 7 month follow-up. | Positive | Ind | MI + | F2F | 3 |
| Walker et al. | 2011 | 310 | Marijuana | 16 | 61% | RCT | 3, 12 months | MI led to significant reductions in marijuana use and consequences compared to educational feedback and waitlist controls at 3 mohths. At 12 months, MI still led to greater reductions in marijuana use and consequences compared to waitlist control. | Positive | Ind | MIF | F2F | 2 |
| Walker, Roffman, Stephens, Berghius, and Kim | 2006 | 97 | Marijuana | 15.75 | 48% | RCT | 3 months | No significant difference between groups in reducing marijuana use. | No Effect | Ind | MIF | F2F | 2 |
| Walton et al. | 2010 | 726 | Alcohol | 16.8 | 44% | RCT | 3,6 months | MI led to significantly reduced alcohol consequences in both the computer or in person condition. | Positive | Ind | MIF | F2F vs Computer | 2 |
| Winters & Leitten | 2007 | 79 | Substance Use | 15.57 | 62% | RCT | 1,6 months | MI led to significant reductions in drinking frequency, binge drinking, illicit drug use, and drug consequences at 6 months (with parent outperformed without parent). | Positive | Ind | MIO | F2F | 2 |
| Woodruff, Conway, Edwards, Elliott, & Crittenden | 2007 | 136 | Tobacco | 16 | 54% | GRT | post, 3, 12 months | Immediately post-treatment, MI significantly reduced smoking and increased abstinence, but these results were not maintained over time. | Positive | Group | MI + | F2F + Internet | 1 |
RCT, Randomized Controlled Trial; GRT, Group Randomized Controlled Trial; Ind, Individual; Gr; Group; MIO, MI Only; MI+, MI + another treatment; MIF, MI with Feedack; MIF+ MI with feedback + another treatment; F2F, Face to Face; Tel, Telephone. Total Quality Indicates the reported use of a manual, training & supervision, and coding of recorded sessions, range of scores 0 meaning none present, 3 meaning all present.
3.2 Quality of Included Studies
The quality of studies reviewed in this article varied in terms of research design, substance use measures, statistical methods, and therapist training/fidelity to MI. Of the 39 trials, 37 were randomized controlled trials (31 randomized by individuals, six randomized by groups), and two had quasi-experimental designs. Twenty-seven of the studies measured substance use only through self-report, 10 combined self-report with biochemical measures of substance use, and two combined self-report with official or medical records of substance use. In order to account for missing data, 21 studies employed an intent-to-treat design, including all participants regardless of whether they dropped out of the study, two studies compared the missing group to the non-missing group to insure they did not differ, two studies used sophisticated statistical techniques to handle missing data (e.g., maximization likelihood estimation procedures), one study used logical imputation to replace missing data, and 13 did not use any strategy for handling missing data. Eleven studies reported using a manual to guide the intervention, 32 studies described some type of training and supervision of study counselors, and 15 studies used some sort of rating or coding tool for assessing fidelity from audio- or video-recordings of the MI sessions.
On our continuous measure of quality, which summed the presence of reported use of a manual, MI training/supervision, and coding for fidelity, two studies reported none, 19 reported having one, 15 reported two, and three reported all of these quality indicators. Both of the studies receiving the lowest possible quality score showed positive substance use outcomes, while among the other levels of quality, approximately the same percentage of programs had positive outcomes.
3.3 Program Effects
Twenty-six trials (67%) showed significant reductions in some type of substance use. Studies showed significant reductions in at least one alcohol (n = 7; Bailey, Baker, Webster, & Lewin, 2004; Monti et al., 1999; Spirito et al., 2011; Spirito et al., 2004; Stein et al., 2011; Stein et al., 2006; Walton et al., 2010), tobacco (n = 6; Woodruff, Conway, Edwards, Elliott, & Crittenden, 2007; Colby et al., 2005; Hollis, Polen, Whitlock, & Lichtenstein, 2005; Kelly & Lapworth, 2006; Pbert et al., 2006; Peterson et al., 2009), marijuana (n = 7; Martin & Copeland, 2008; Stein et al., 2011; Stein et al., 2006; Waldron et al., 2001; Dennis, Godley, Diamond, & Tims, 2004; Godley et al., 2010; Walker et al., 2011), and “substance use” outcome (n = 8; Winters & Leitten, 2007; Battjes et al., 2004; D’Amico, Miles, Stern, & Meredith, 2008; Gray, McCambridge & Strang, 2005; Grenard et al., 2007; Mason, Pate, Drapkin, & Sozinho,2011; McCambridge & Strang, 2004; Peterson, Baer, Wells, Ginzler, & Garrett, 2006). Studies reporting positive effects included all of the studies reporting the lowest level of quality, and approximately 70% of the three other categories.
3.4 Comparison of Intervention Formats
Interventions were delivered in either group (n = 3), individual (n = 35), or a combination of group and individual formats (n = 1). All three of the group interventions showed a positive effect, while 22 (63%) of the individual studies did. The group/individual combination trial showed significant effects. Studies used a variety of modalities, including face-to-face only (n = 29), telephone only (n = 1), face-to-face + telephone (n = 4), and other modality combinations or comparisons (n = 5). Results from these studies showed 21 (72%) of the face-to-face only interventions demonstrated significant reductions in at least one substance use outcome, as did the one telephone-only intervention, one quarter of the face-to-face + telephone interventions, and 60% of the others. Due to uneven sample sizes, we were unable to conduct Chi Square Goodness of Fit analyses using modality data.
3.4a Comparing Different Treatment Modalities
Of particular interest are studies comparing different modalities. There was one test of a telephone vs. face-to-face booster (Kaminer et al., 2008), two tests of an adolescent alone vs. adolescent with parent intervention (Winters & Leitten, 2007; Spirito et al., 2011), and one test of in-person vs. computerized feedback (Walton et al., 2010). Kaminer and colleagues’ (2008) test of a face-to-face vs. telephone booster of an aftercare program for participants of a cognitive behavioral therapy intervention found no difference between the 50-minute in-person session compared to the 15–20-minute telephone intervention, and no significant effects for either group compared to the control. However, the authors note randomization failed and the control condition had significantly fewer persons with substance use disorders. In addition, when both the face-to-face and telephone groups were combined, youth who received some aftercare were less likely to relapse than youth who received no active aftercare.
In a three-group school-based intervention, Winters and Leitten (2007) tested the effect of MI with adolescents only vs. MI with adolescents + parents intervention and found the treatment conditions significantly outperformed the control, and the adolescent + parent condition significantly outperformed the adolescent only condition on most outcome variables. However, they further reported that 6-month abstinence rates did not differ across groups. Spirito and colleagues (2011) also found added significant effects of including parents in an MI intervention with alcohol-positive adolescents recruited in an emergency department. This intervention required families to return to the hospital one week later.
In a three-group randomized controlled trial of 756 urban adolescents seen in an emergency department, Walton et al. (2010) tested the use of providing feedback in face-to-face vs. computer-delivered format. They found that both intervention groups significantly outperformed the assessment-only control, and the face-to-face feedback condition significantly outperformed the computerized feedback condition. At three months, a significant decrease was found in self-reported alcohol consequences, aggression, and violence, and the effect on alcohol consequences was maintained at six months in the face-to-face condition.
Finally, in a three-group randomized controlled trial of a twelve-session classroom-based prevention program, a classroom-only condition, a classroom + three-session MI booster (one session in-person and two sessions via telephone), and an assessment-only control, Sussman and colleagues (2011) found that the MI booster did not significantly improve outcomes for any measured substance use outcome when compared to the classroom-only condition.
3.4b
Adolescent-Specific MI Adaptation represents a possible application for adolescents. For an example of including parents in MI, an inpatient psychiatric smoking cessation intervention provided parents up to four telephone counseling sessions. Compared to the brief advice condition, the study showed the MI intervention to be more effective at reducing substance use (Brown et al., 2009), but not more effective on smoking cessation (Brown et al., 2003). For an example of MI provided in a school setting, in a three-group randomized controlled trial of a twelve-session classroom-based prevention program, a classroom-only condition, a classroom + three-session MI booster (one session in-person and two sessions via telephone), and an assessment-only control, Sussman and colleagues (2011) found that the MI booster did not significantly improve outcomes for any measured substance use outcome when compared to the classroom-only condition.
3.5 Comparison of Intervention Design
In this review, studies represented MIO (n = 8), MIF (n =17), MI + (n = 9), and MIF + (n = 5) interventions. Six MIO (75%), 11 MIF (65%), seven MI + (78%), and two MIF + (40%) interventions showed a positive effect on outcomes. Chi Square Goodness of Fit analyses were used to test for differences in effectiveness based on the addition of a feedback component or the combination of other treatments with MI. The results from this comparison suggest very little difference between the intervention designs. However, caution should be used when interpreting these results due to the small number of studies represented in each category.
3.5a MI with Feedback
There was no difference between interventions containing feedback (MIF and MIF +) versus their non-feedback counterparts (MIO and MI +), χ2(1) = .64, p = .42. All 22 MI interventions with feedback (MIF and MIF+) included a face-to-face component, three added additional telephone contact, and one included additional contact with a parent. The number of sessions varied from one to more than three: one session (n = 9), two sessions (n = 6), and three or more sessions (n = 7).
3.5b MI with Additional Features
There was no significant difference between interventions with additional programs (MI + and MIF +) versus their stand-alone MI counterparts (MIO and MIF), χ2(1) = .06, p = .81. Of 14 programs where MI was added to another component (MI+ and MIF+), two interventions used MI as a post-treatment booster to maintain effects – one as an aftercare component to a CBT program (Kaminer et al., 2008), the other as motivational booster to a classroom-based prevention program (Sussman et al., 2011). Two followed advice presented by a doctor (Hollis et al.,, 2005) or video (Colby et al., 1998), one provided MIF to the adolescent and held a separate meeting with parents (Goti et al., 2010), one used MIF with a social network intervention component (Mason et al., 2011); one provided MI and made a skills-based class available for those who wanted to attend (Martin & Copeland, 2008); and seven used MI as a prelude to cognitive behavioral programs that included refusal skills, relapse prevention, and information about consequences of use (n = 5 MI + CBT; Waldron, et al, 2001; Battjes et al., 2004; Dennis et al., 2004; Woodruff et al., 2007; Peterson et al., 2009; n = 2 MIF + CBT Brown et al., 2003; Godley et al., 2010)
3.6 Potential Theory-Based Mechanisms
No studies reported mediation analyses. However, 71% of studies reported findings about potential mechanisms of change in MI interventions. Significant findings of MI’s effectiveness were reported for attitudinal constructs such as readiness/intention to change (n = 5) (Bailey et al., 2004; Colby et al., 2005; Grenard et al., 2007; D’Amico et al., 2008; Mason et al., 2011), client engagement in the treatment process (n = 2) (Peterson et al., 2006; Stein et al., 2006), implicit cognitions (Thush et al., 2009), and client perception of risk (Goti et al., 2010). Changes in behavioral constructs were found for improved drug refusal skills (Kelly & Lapworth, 2006), reduced dependence criteria (Martin & Copeland, 2008), participating in other risky behaviors (Monti et al., 1999), and client self-monitoring (McCambridge & Strang, 2005). However, non-significant findings were found for some of the same attitudinal measures: readiness/intention to change (n = 5) (Brown et al., 2003; Peterson et al., 2006; Woodruff et al., 2007; Peterson et al., 2009; Thush et al., 2009) and participation in additional treatment (Monti et al., 1999; Walker et al., 2011).
4. Discussion
4.1 Included Studies
Grenard and colleagues’ (2006) review of the MI literature (search date March 2005) found fewer than 10 studies with a mean age of less than 18, and less than 50% of these studies showed positive substance use effects. Jensen and colleagues’ (2011) meta-analysis (N = 21) does not provide search dates, however they included only one article published in as recently as 2009. The current review found more than 10 articles published since 2010. The number of MI studies published each year continues to grow. Inclusion criteria for this review differed from Grenard et al. (2006) by only focusing on adolescent literature, while criteria differed from Jensen et al. (2011) in that we had no requirement for data to calculate effect sizes. Of the studies included in this current review 67% showed a positive effect. There was no indication of a relationship between study quality and outcomes. Studies of very low quality may not have been published, however, and therefore publication bias, the “file drawer problem,” should be taken into consideration when interpreting these findings.
4.2 Intervention Format
Not surprisingly, the majority of studies represent MI interventions with individuals (n = 34), as opposed to groups (n = 4). This finding is likely due to 1) the origins of MI as a counseling style for working with individuals, 2) intervention design choices (for instance, all studies using feedback were conducted in individualized formats), and 3) recruitment setting (for instance, all interventions conducted in medical settings were conducted in person, while of the four group studies, three were conducted in community treatment centers and one was conducted on the Internet). The relationship between design, format, and other intervention characteristics, such as number and length of sessions, setting (e.g., emergency room, school, treatment program), target population (e.g., psychiatric inpatient smokers, adjudicated or rural youth) should be further explored in future reviews. Meanwhile, comparisons of different modalities suggest that 1) involving parents may improve results, 2) there is no difference between telephone or in-person follow-ups, and 3) providing feedback face-to-face is superior to computerized feedback. Future emphasis on conducting such comparisons would greatly assist the field.
4.3 Intervention Design
Although chi square statistics did not show statistical differences between intervention designs, this review highlights the need for studies to dismantle the effects of feedback with adolescents. A test of the importance of providing feedback (Walters et al., 2009) among college students (mean age 19.8 years) found that the MIF condition had significantly reduced the composite drinking measure and drinks per week, compared to the assessment-only control, MIO, and written feedback alone conditions at 6-month follow-up. Furthermore, a meta-analysis of personalized feedback interventions targeting alcohol use (n = 14; college age n = 9) found an overall effect size of d = .22, 95% CI[.16,.03], in reduced alcohol consumption (Riper et al., 2009). However, college students may differ from adolescents in significant ways, as the former tend to show lower levels of psychological reactance (Hong, Giannakopoulos, Laing, & Williams, 1994), possibly making them more receptive to normative feedback than their adolescent counterparts.
In a secondary analysis of Brown and colleagues (2003 & 2009), Apodaca and Longabaugh (2007) advised caution regarding use of feedback with adolescents. They argued that, as they found no relationship between health consequences and readiness to change, using feedback to highlight consequences may be misdirected and not important for cessation, a finding similar to results published in Colby et al. (1998). They further cited Amhrein, Miller, Yahne, Palmer, & Fulcher’s (2003) findings that while receiving feedback client change talk decreases, which suggests that feedback may inhibit change. Later results by Baer et al. (2008) suggest that change language can predict improved outcomes among adolescents, so that any activity that reduces change talk may negatively influence outcomes. Further consideration of the relationship between reactance and feedback warrants study.
4.4 Potential Mechanisms
This review revealed a pattern of investigation into attitudinal and behavioral mechanisms of change, with both factors being influenced by MI. There appears to be a prevailing interest in attitudinal measures of readiness to change (RTC), stages of change (Prochaska & DiClemente, 1982; Prochaska, DiClemente, & Norcross, 1992), and intention to change. This review identified 12 studies that measured some form of RTC and provided information about either 1) the ability of MI to influence RTC or 2) the relationship between RTC and improved substance use outcomes. Of the seven studies reporting RTC findings and having positive effects on substance use outcomes, four articles reported that the intervention also significantly influenced RTC (Bailey et al., 2004; Colby et al., 2005; Grenard et al., 2007; Mason et al., 2011); two studies showed no effect of the intervention on RTC (Peterson et al., 2006; Peterson et al., 2009); and three studies showed an effect of RTC on outcomes (Peterson et al., 2006; Peterson et al., 2009; Audrain-McGovern et al., 2011).
Two additional studies specifically addressed RTC among adolescent substance users, but did not meet criteria for inclusion in this review. Erol and Erdogan (2008) in a single group pre-post design with Turkish adolescents found that the MI condition significantly changed reported stage of change, and a randomized controlled study by Huang et al. (2010) reported significant effects of an MIF intervention on RTC among adolescent Taiwanese methamphetamine users. To further highlight the importance of RTC in MI research, some programs utilize an RTC-based protocol that dictates a different approach for interventionists depending on the individual’s stage of change (Erol & Erdogan, 2008; Hollis et al., 2004, Peterson et al., 2009). Despite contradictory findings, it appears that readiness to change should continue to be measured as a possible mechanism of change, though agreement on how to measure it should be sought.
To date, the search for mechanisms of change has been ad hoc with variables being selected by individual research teams when implementing a new intervention. A theory-based approach to determine the mechanisms of change in MI interventions is needed. Theory exists to guide the measurement of constructs related to the Process Model of MI, which proposes that the utilization of specific counseling and interpersonal skills will lead to increases in client change language, and that these client statements will predict improved substance use outcomes. These “technical” and “relational” aspects of MI (Miller & Rollnick, 2002; Miller & Rose, 2009) are clearly explicated and measurable with the use of valid and reliable MI specific coding systems (Moyers et al., 2007; Glynn & Moyers, 2009). To date there are only two investigations of the Process Model in the adolescent literature (Baer et al., 2008; Engle, Macgowan, Wagner, & Amrhein, 2010). Both studies found support for a significant relationship between client change language and substance use outcomes. Baer et al. (2008) conducted individual MI sessions in drop-in centers with homeless youth to encourage decreased substance use and increased service utilization and measured client language using the Motivational Interviewing Skills Code (2.0). Engle et al. (2010) applied the Process Model to a school-based substance use intervention group, whereby ratings of counselor empathy, group level commitment language and peer response were used to investigate associations with marijuana use outcomes at post-test, 1-, 3-, and 12-month follow-ups. They found that group leader empathy, measured with the Motivational Interviewing Treatment Integrity (2.0), was significantly related to group commitment and peer response, while group commitment language was significantly correlated with outcomes at post-test and 12-month follow-up, and peer response was significantly correlated with outcomes at 1- and 12-month follow-up.
However, no models exist to guide choices for measuring potential mechanisms of change. MI interventions are likely to target different mechanisms of change, depending on the intervention design. Where MI is combined with cognitive behavioral skills training, the program is likely focused on mediators such as perceived behavioral control or self-efficacy from the Theory of Planned Behavior (Ajzen, 1985) and Social Learning Theory (Bandura, 1977), respectively. Feedback interventions can be loosely tied to theories that use perceived norms as a determinant of a behavior (e.g., Theory of Planned Behavior), as the purpose of providing normative feedback is to address clients’ perception of their behavior in the context of others’ behavior. Finally, MIO interventions may influence cognitive dissonance by developing discrepancy between current behavior and client values and goals; self-efficacy by focusing on client past successes, strengths, and the confidence ruler; readiness to change by using the importance or readiness ruler; autonomy by emphasizing personal choice and control; and drug use expectancies by exploring pros and cons of continued use or quitting. However, a non-manualized MIO intervention may be so flexible that only through observational coding of recorded sessions could the active ingredients of the intervention actually be determined.
4.5 Conclusion
Clearly, there remains a great deal to learn about the efficacy of different designs and possible mechanisms of change in MI interventions for adolescent substance use. Perhaps findings from other health behavior areas (e.g., diet and exercise, or medication adherence) might have important insights to share. In order to move MI research forward in this area, we must develop and test theory-based models to enhance program effects. The authors of this review suggest that a working group of researchers be convened to develop a series of models that take design, target population/setting, and targeted substance into consideration so that systematic investigation can occur.
Highlights.
Of the studies included in this review 67% showed a positive effect.
No significant differences were found between interventions with or without feedback.
No significant differences were found between interventions combined or not combined with additional treatments.
There is a need for theoretical models to guide measurements of possible mechanisms of change in MI interventions.
Acknowledgments
Role of Funding Sources
This paper was supported by grants from the National Institute on Drug Abuse (DA020138) NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Contributors
All authors contributed to the study design and protocol. Ms. Barnett and Ms. Smith conducted the literature searches and developed the table, provided summaries of previous research studies. Ms Barnett wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action-Control: From Cognition to Behavior. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104(5):705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Audrain-McGovern J, Stevens S, Murray PJ, Kinsman S, Zuckoff A, Pletcher J, Wileyto EP. The efficacy of motivational interviewing versus brief advice for adolescent smoking behavior change. Pediatrics. 2011;128(1):e101–e111. doi: 10.1542/peds.2010-2174. [DOI] [PubMed] [Google Scholar]
- Baer JS, Beadnell B, Garrett SB, Hartzler B, Wells EA, Peterson PL. Adolescent change language within a brief motivational intervention and substance use outcomes. Psychology of Addictive Behaviors. 2008;22(4):570–575. doi: 10.1037/a0013022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS, Peterson PL. Motivational interviewing with adolescents and young adults. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people for change. New York: Guilford Press; 2002. pp. 320–332. [Google Scholar]
- Bailey KA, Baker AL, Webster RA, Lewin TJ. Pilot randomized controlled trial of a brief alcohol intervention group for adolescents. Drug and Alcohol Review. 2004;23(2):157–166. doi: 10.1080/09595230410001704136. [DOI] [PubMed] [Google Scholar]
- Bandura A. Toward a unifying theory of behavior change. Psychological Review. 1977;84(2):91–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Battjes RJ, Gordon MS, O’Grady KE, Kinlock TW, Katz EC, Sears EA. Evaluation of a group-based substance abuse treatment program for adolescents. Journal of Substance Abuse Treatment. 2004;27(2):123–134. doi: 10.1016/j.jsat.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Brown JM, Miller WR. Impact of motivational interviewing on participation and outcome in residential alcoholism treatment. Psychology of Addictive Behaviors. 1993;7(4):211–218. [Google Scholar]
- Brown RA, Strong DR, Abrantes AM, Myers MG, Ramsey SE, Kahler CW. Effects on substance use outcomes in adolescents receiving motivational interviewing for smoking cessation during psychiatric hospitalization. Addictive Behaviors. 2009;34(10):887–891. doi: 10.1016/j.addbeh.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R, Ramsey S, Strong D, Myers M, Kayler C, Lejuez C, Abrams D. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tobacco Control. 2003;12(Suppl 4):iv3–iv10. doi: 10.1136/tc.12.suppl_4.iv3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Colby SM, Monti PM, Barnett NP, Rohsenow DJ, Weissman K, Spirito A, Lewander WJ. Brief motivational interviewing in a hospital setting for adolescent smoking: A preliminary study. Journal of Consulting and Clinical Psychology. 1998;66(3):574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- Colby SM, Monti PM, Tevyaw TO, Barnett NP, Spirito A, Rohsenow DJ, Lewander W. Brief motivational intervention for adolescent smokers in medical settings. Addictive Behaviors. 2005;30(5):865–874. doi: 10.1016/j.addbeh.2004.10.001. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JNV, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment. 2008;35(1):53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM. The cannabis youth treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Engle B, Macgowan MJ, Wagner EF, Amrhein PC. Markers of marijuana use outcomes within adolescent substance abuse group treatment. Research on Social Work Practice. 2010;20(3):271–282. [Google Scholar]
- Erol S, Erdogan S. Application of a stage based motivational interviewing approach to adolescent smoking cessation: The transtheoretical model-based study. Patient Education and Counseling. 2008;72(1):42–48. doi: 10.1016/j.pec.2008.01.011. [DOI] [PubMed] [Google Scholar]
- Glynn LH, Moyers TB. Manual for the Motivational Interviewing Skill Code (MISC), Version 1.1: Addendum to MISC 1.0. University of New Mexico: Center on Alcoholism, Substance Abuse and Addictions (CASAA); 2009. [Google Scholar]
- Godley SH, Garner BR, Passetti LL, Funk RR, Dennis ML, Godley MD. Adolescent outpatient treatment and continuing care: Main findings from a randomized clinical trial. Drug and Alcohol Dependence. 2010;110(1–2):44–54. doi: 10.1016/j.drugalcdep.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goti J, Diaz R, Serrano L, Gonzalez L, Calvo R, Gual A, Castro J. Brief intervention in substance-use among adolescent psychiatric patients: A randomized controlled trial. European Child & Adolescent Psychiatry. 2010;19(6):503–11. doi: 10.1007/s00787-009-0060-5. [DOI] [PubMed] [Google Scholar]
- Gray E, McCambridge J, Strang J. The effectiveness of motivational interviewing delivered by youth workers in reducing drinking, cigarette and cannabis smoking among young people: Quasi-experimental pilot study. Alcohol and Alcoholism. 2005;40(6):535–539. doi: 10.1093/alcalc/agh199. [DOI] [PubMed] [Google Scholar]
- Grenard JL, Ames SL, Wiers RW, Thush C, Stacy AW, Sussman S. Brief intervention for substance use among at-risk adolescents: A pilot study. Journal of Adolescent Health. 2007;40(2):188–191. doi: 10.1016/j.jadohealth.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1(1):91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Polen MR, Whitlock EP, Lichtenstein E. Teen reach: Outcomes from a randomized, controlled trial of a tobacco reduction program for teens seen in primary medical care. Pediatrics. 2005;115(4):981–9. doi: 10.1542/peds.2004-0981. [DOI] [PubMed] [Google Scholar]
- Hong S, Giannakopoulos E, Laing D, Williams NA. Psychological reactance: Effects of age and gender. The Journal of Social Psychology. 1994;134(2):223–228. doi: 10.1080/00224545.1994.9711385. [DOI] [PubMed] [Google Scholar]
- Huang Y, Tang T, Lin C, Yen C. Effects of Motivational Enhancement Therapy on Readiness to Change MDMA and Methamphetamine Use Behaviors in Taiwanese Adolescents. Substance Use & Misuse. 2010:149–154. doi: 10.3109/10826084.2010.501664. [DOI] [PubMed] [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2011;79(4):433. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(12):1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly AB, Lapworth K. The HYP program--targeted motivational interviewing for adolescent violations of school tobacco policy. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2006;43(6):466–471. doi: 10.1016/j.ypmed.2006.06.018. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Feres N, Kenney &, Lac A. Family history of alcohol abuse moderates effectiveness of a group motivational enhancement intervention in college women. Addictive Behaviors. 2009;34(5):415–420. doi: 10.1016/j.addbeh.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. Journal of Clinical Psychology. 2009;65(11):1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- Macgowan MJ, Engle B. Evidence for optimism: behavior therapies and motivational interviewing in adolescent substance abuse treatment. Child and adolescent psychiatric clinics of North America. 2010;19(3):527. doi: 10.1016/j.chc.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin G, Copeland J. The adolescent cannabis check-up: Randomized trial of a brief intervention for young cannabis users. Journal of Substance Abuse Treatment. 2008;34(4):407. doi: 10.1016/j.jsat.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Mason M, Pate P, Drapkin M, Sozinho K. Motivational interviewing integrated with social network counseling for female adolescents: A randomized pilot study in urban primary care. Journal of Substance Abuse Treatment. 2011;41(2):148. doi: 10.1016/j.jsat.2011.02.009. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: Results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. Deterioration over time in effect of motivational interviewing in reducing drug consumption and related risk among young people. Addiction. 2005;100(4):470–478. doi: 10.1111/j.1360-0443.2005.01013.x. [DOI] [PubMed] [Google Scholar]
- McNally AM, Palfai TP, Kahler CW. Motivational interventions for heavy drinking college students: Examining the role of discrepancy-related psychological processes. Psychology of Addictive Behaviors. 2005;19(1):79–87. doi: 10.1037/0893-164X.19.1.79. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Sovereign RG. In: The check-up: A model for early intervention in addictive behaviors. Løberg T, Miller WR, Nathan PE, Marlatt GA, editors. Lisse, Netherlands: Swets & Zeitlinger Publishers; 1989. pp. 219–231. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists and Individuals with Alcohol Abuse and Dependence. U.S. Department of Helath and Human Services; 1992. [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67(6):989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan J, Amrhein PC. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism: Clinical and Experimental Research. 2007;31(s3):40s–47s. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.0 (MITI 3.0) University of New Mexico: Center on Alcoholism, Substance Abuse and Addictions (CASAA); 2007. [Google Scholar]
- Naar-King S, Suarez M. Motivational interviewing with adolescents and young adults. New York: Guilford Press; 2011. [Google Scholar]
- Pbert L, Osganian SK, Gorak D, Druker S, Reed G, ONeill KM, Sheetz A. A school nurse-delivered adolescent smoking cessation intervention: A randomized controlled trial. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2006;43(4):312–320. doi: 10.1016/j.ypmed.2006.04.006. [DOI] [PubMed] [Google Scholar]
- Peterson AV, Kealey KA, Mann SL, Marek PM, Ludman EJ, Liu J, Bricker JB. Group-randomized trial of a proactive, personalized telephone counseling intervention for adolescent smoking cessation. Journal of the National Cancer Institute. 2009;101(20):1378–1392. doi: 10.1093/jnci/djp317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson PL, Baer JS, Wells EA, Ginzler JA, Garrett SB. Short-term effects of a brief motivational intervention to reduce alcohol and drug risk among homeless adolescents. Psychology of Addictive Behaviors. 2006;20(3):254–264. doi: 10.1037/0893-164X.20.3.254. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research & Practice. 1982;19(3):276–288. [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Riper H, van Straten A, Keuken M, Smit F, Schippers G, Cuijpers P. Curbing problem drinking with personalized-feedback interventions: A meta-analysis. American Journal of Preventive Medicine. 2009;36(3):247–255. doi: 10.1016/j.amepre.2008.10.016. [DOI] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A, Page JR, Franklin ME, Foa EB. Adding motivational interviewing to exposure and ritual prevention for obsessive-compulsive disorder: An open pilot trial. Cognitive Behaviour Therapy. 2008;37(1):38–49. doi: 10.1080/16506070701743252. [DOI] [PubMed] [Google Scholar]
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, Myers M. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. The Journal of Pediatrics. 2004;145(3):396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, Monti PM. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: Results of a randomized clinical trial. Archives of Pediatrics & Adolescent Medicine. 2011;165(3):269. doi: 10.1001/archpediatrics.2010.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R, Miranda R. Enhancing substance abuse treatment engagement in incarcerated adolescents. Psychological Services. 2006;3(1):25–34. doi: 10.1037/1541-1559.3.1.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. The American Journal on Addictions. 2006;15:50–57. doi: 10.1080/10550490601003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Clair M, Lebeau R, Colby SM, Barnett NP, Golembeske C, Monti PM. Motivational interviewing to reduce substance-related consequences: Effects for incarcerated adolescents with depressed mood. Drug and Alcohol Dependence. 2011;118(2–3):475–478. doi: 10.1016/j.drugalcdep.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, McCambridge J. Can the practitioner correctly predict outcome in motivational interviewing? Journal of Substance Abuse Treatment. 2004;27(1):83–88. doi: 10.1016/j.jsat.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Sung-Mook H, Giannakopoulos E, Laing D, Williams NA. Psychological reactance: Effects of age and gender. The Journal of Social Psychology. 1994;134(2):223–8. doi: 10.1080/00224545.1994.9711385. [DOI] [PubMed] [Google Scholar]
- Sussman S, Sun P, Rohrbach LA, Spruijt-Metz D. One-year outcomes of a drug abuse prevention program for older teens and emerging adults: Evaluating a motivational interviewing booster component. Health Psychology. 2011 doi: 10.1037/a0025756. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thush C, Wiers RW, Moerbeek M, Ames SL, Grenard JL, Sussman S, Stacy AW. Influence of motivational interviewing on explicit and implicit alcohol-related cognition and alcohol use in at-risk adolescents. Psychology of Addictive Behaviors. 2009;23(1):146–151. doi: 10.1037/a0013789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron H, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69(5):802–813. [PubMed] [Google Scholar]
- Walker DD, Roffman RA, Picciano JF, Stephens RS. The check-up: In-person, computerized, and telephone adaptations of motivational enhancement treatment to elicit voluntary participation by the contemplator. Substance Abuse Treatment, Prevention, and Policy. 2007;2 doi: 10.1186/1747-597X-2-2. (1747-597X, 1747-597X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Roffman RA, Stephens RS, Wakana K, Berghuis J. Motivational enhancement therapy for adolescent marijuana users: A preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(3):628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens R, Roffman R, DeMarce J, Lozano B, Towe S, Berg B. Randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: A further test of the teen marijuana checkup. Psychology of Addictive Behaviors. 2011;25(3):474–484. doi: 10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters S, Vader A, Harris T, Field C, Jouriles E. Dismantling motivational interviewing and feedback for college drinkers: a randomized clinical trial. Journal of consulting and clinical psychology. 2009;77(1):64. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. JAMA. 2010;304(5):527. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Leitten W. Brief intervention for drug-abusing adolescents in a school setting. Psychology of Addictive Behaviors. 2007;21(2):249–254. doi: 10.1037/0893-164X.21.2.249. [DOI] [PubMed] [Google Scholar]
- Woodruff SI, Conway TL, Edwards CC, Elliott SP, Crittenden J. Evaluation of an Internet virtual world chat room for adolescent smoking cessation. Addictive Behaviors. 2007;32(9):1769–1786. doi: 10.1016/j.addbeh.2006.12.008. [DOI] [PubMed] [Google Scholar]