Abstract
Objectives. We evaluated the Families OverComing Under Stress program, which provides resiliency training designed to enhance family psychological health in US military families affected by combat- and deployment-related stress.
Methods. We performed a secondary analysis of Families OverComing Under Stress program evaluation data that was collected between July 2008 and February 2010 at 11 military installations in the United States and Japan. We present data at baseline for 488 unique families (742 parents and 873 children) and pre–post outcomes for 331 families.
Results. Family members reported high levels of satisfaction with the program and positive impact on parent–child indicators. Psychological distress levels were elevated for service members, civilian parents, and children at program entry compared with community norms. Change scores showed significant improvements across all measures for service member and civilian parents and their children (P < .001).
Conclusions. Evaluation data provided preliminary support for a strength-based, trauma-informed military family prevention program to promote resiliency and mitigate the impact of wartime deployment stress.
More than 1.7 million children in the United States have a parent serving in the military. Since September 11, 2001, approximately 900 000 children have had a parent who deployed multiple times as part of Operation Iraqi Freedom or Operation Enduring Freedom. For a decade, children and their parents have negotiated repeated separations and subsequent family reunions in the context of wartime risk. Recent studies have begun to document the psychological health impact of wartime deployments on service members, spouses, and children, suggesting that greater attention should be paid to the implementation and evaluation of selective prevention strategies that target at-risk families and promote resilience across the military community.1–4
Deployed service members are often exposed to a landscape of chronic stressors, potential traumatic events, and harsh environmental risk factors during combat duty. Among those service members returning from deployment to Iraq, 16% to 17% meet criteria for depression, posttraumatic stress disorder (PTSD), or generalized anxiety.5 Repeated deployments or exposure to adverse conditions have been associated with higher rates of combat-related psychological health problems, traumatic brain injury, substance abuse, and marital conflict.6–15
Extended separations in the context of combat deployment may also affect psychological health for the at-home spouse and children. Recent evidence suggests that distress levels of at-home family members increase as the number of deployment months increases.16 Military children may also be vulnerable to emotional and behavior disruptions, including heightened anxiety and academic difficulties.1,17–21 Consistent with the larger literature on child distress,22 psychological symptoms in military parents predict child adjustment problems.16,23,24 Additionally, the cumulative length of parental deployments correlates with increased risk for depression and behavioral disruptions in school-aged children16 and with increased distress in adolescents.24
Interventions that target families facing adversity and build on family strengths to reduce psychological distress have been shown to have a positive effect on parent and child adjustment and to provide sustained benefits.25 In randomized controlled trials involving families in challenging circumstances (i.e., parental medical illness, parental depression), targeted family interventions that strengthen parent–child relationships, promote effective parenting practices, and increase family understanding have consistently demonstrated positive outcomes in child development and psychological health over time.25–28 Effective coping skills, particularly those that address traumatic stress reactions, are associated with enhanced stress management,29–31 and effective caregiver–child relationships support the development of child adaptive skills such as emotional and behavioral regulation.32,33
The FOCUS (Families OverComing Under Stress) project for military families emerged from foundational research on a previously described family-centered preventive intervention model and then was adapted and manualized by a University of California, Los Angeles (UCLA)–Harvard intervention development team at Marine Corps Base, Camp Pendleton.34,35 The program was subsequently implemented as a large-scale demonstration program for the US Marine Corps and US Navy, funded by the US Navy's Bureau of Medicine and Surgery. Importantly, potential barriers to accessing mental health services have been addressed by a FOCUS implementation emphasis on being strength and skills based, practical, and easily accessible and applicable for military families. Implementation also includes strong military leadership involvement and community partnership to ensure active outreach and family engagement.
FOCUS provides education and skills training for military parents and children. Training is designed to enhance coping with deployment-related experiences, including possible combat-related psychological or physical injury in the service member. Through a structured narrative approach, family members share their unique perspectives of deployment-related experiences, thereby enhancing understanding, bridging communication, and increasing family cohesion and support. This process mobilizes theoretically and empirically supported family resiliency processes.36,37 FOCUS also integrates the US Navy and US Marine Corps stress continuum model,38 which categorizes deployment stress into 4 color zones—green, yellow, orange, and red—reflecting an increasing level of risk for psychological distress, injury, and disorder and providing a framework to guide risk identification and referral. Details regarding the FOCUS program foundation, model, and implementation are described elsewhere.34,39
We hypothesized that parents completing the program would report improved understanding of deployment and combat stress, improved family skills (emotional regulation, communication, family goal setting, management of stress reminders and triggers) and intrafamilial support, satisfaction with the program, and a likelihood of recommending the program to others. We also hypothesized that families who completed the program would experience improved individual psychological health outcomes and improved family functioning. To our knowledge, this is the first systematic program evaluation examining the effectiveness of a trauma-informed, selective prevention program for military families experiencing wartime deployments.
METHODS
We conducted the evaluation as part of the FOCUS service delivery project funded by the US Navy's Bureau of Medicine and Surgery. We performed a secondary analysis of de-identified data originally collected (July 2008–February 2010) to customize delivery and improve program quality. The program-level data we have presented is from 11 US Marine Corps and US Navy installations located in California (4 sites); North Carolina; Hawaii; Okinawa, Japan; Virginia (2 sites); Mississippi; and Washington State.
FOCUS family resiliency training is delivered to individual families in 8 sessions scheduled according to the family's convenience. Parent and family sessions last 90 minutes and child sessions last 30–60 minutes, depending on the child's developmental level. Although standardized and manualized to ensure that each family learns core FOCUS skills, the intervention allows flexibility and customization to address specific family goals and needs. FOCUS providers (called resiliency trainers) are master- or doctoral-level specialists in child and family mental health. They complete extensive web-based and in-person initial training from UCLA-based supervisors and then participate in weekly reviews of the intervention delivery with their team and with supervisors. UCLA staff also provide ongoing training, intervention materials, emergency support, and technical assistance. Centralized management of the program ensures adherence to program fidelity, coordinated military partnerships, and ongoing quality improvement processes.
An innovative Internet-based “cloud-computing” management system (described in Lester et al.34) is used for quality control and to track implementation. The web-based, real-time assessment provides immediate feedback, enabling families to receive appropriate psychoeducational materials, a customized intervention protocol, and timely service referrals if needed. The assessment protocol includes standardized psychological health and coping measures that children, parents, and FOCUS providers complete. We obtained community norms for comparison and cutoffs for clinically significant symptoms from instrument-specific published sources (e.g., a scoring manual, meta-analyses, or similar peer-reviewed data). For measures with psychometrically established properties, we have reported Cronbach α for this sample. Cronbach α is a measure of the internal consistency (reliability) of responses on a questionnaire. Values that fall between 0.70 and 1.0 are acceptable.
Demographics and Descriptive Assessments
Parents answer general demographic and deployment history questions at intake. Active duty parents then complete the PTSD Checklist-Military,40 a 17-item self-report measure to assess the severity of PTSD symptoms in the past month. Non–active duty parents complete the PTSD Checklist-Civilian.40 Both the PTSD Checklist-Military and the PTSD Checklist-Civilian are administered at entry to guide program delivery (e.g., to identify need for referral or skills to target in intervention); we include them here to provide a description of population risk. A score of ≥ 30 is considered clinically significant for screening purposes in primary care settings.41,42
Parent and Family Outcome and Process Assessments
Parent emotional distress was used to assess psychological distress symptoms. Brief Symptom Inventory (BSI) 1843 is an abbreviated version of the widely used BSI,44 a self-report inventory with extensively published psychometric data and community norms by gender. Parents complete the BSI at program entry and at 1 and 4 to 6 months postintervention. Cronbach α for this sample was excellent (0.91). We have reported details for global severity and prevalence of clinically significant symptoms of anxiety and depression. BSI norms are gender specific, and both genders were represented in non–active duty and active duty groups. Thus, all pre–post analyses of the BSI included gender as a covariate. To determine family adjustment, parents complete the McMaster Family Assessment Device (FAD),45 used to assess problem solving, communication, roles, affective responsiveness, affective involvement, behavior control, and general functioning. The FAD is administered at program entry and exit. For this sample, Cronbach α was excellent (0.92). An FAD general functioning score ≥ 2 is considered unhealthy functioning.45
The FOCUS resiliency trainer completes a Global Assessment of Functioning (GAF) rating for each family member at entry, midpoint, and exit. GAF is a numeric scale (0–100) of overall current functioning that can be used with adults and children. Scores are characterized as follows: moderate to severe impairment (0–50); variable or single area difficulty (51–70); and slight or no impairment across all areas of home, school, and peers (71–100).
Upon completing FOCUS, parents are asked to rate their perception of change. Adapted from a previous prevention trial,47 this 29-item scale assesses the parents’ perception of improvement regarding 6 core intervention domains, including communication, problem solving, emotional regulation, managing trauma reminders, goal setting, and overall family support. Ratings anchors are 1 = less than before, 4 = same as before, and 7 = much more than before. Cronbach α was excellent (0.96).
At the time of program completion, parents are asked to rate their overall satisfaction with their family's participation in the program on the basis of how harmful or helpful the program was (1 = very harmful to 7 = very helpful), the parent's satisfaction with the program (1 = very dissatisfied to 7 = very satisfied), and whether the parent would recommend this program to another family (1 = definitely not recommend to 7 = definitely recommend).
Child Outcome Assessments
Child psychological adjustment at baseline and follow-up was assessed using the Strengths and Difficulties Questionnaire–Parent Report (SDQ),48 a widely used instrument with subscales for conduct problems, emotional symptoms, and prosocial behavior as well as a summary score of total difficulties. Normative data are available for both genders and for individuals aged 4 to 18 years. For simplicity, we have reported details for the total score and prevalence of clinically significant conduct problems and prosocial behaviors for the age groups specified in the SDQ manual.
Child coping was assessed using the Kidcope measure,49 a self-report checklist to assess the use of various types of coping strategies in youths. Children aged 7 to 18 years complete the coping measure at baseline and program exit. Cronbach α was acceptable (0.73).
We analyzed continuous intake data (e.g., comparing those with and those without post data on severity of distress) using analysis of variance. We analyzed categorical intake data (e.g., prevalence of clinically significant distress) with the χ2 test. We analyzed pre–post change score continuous data using the single-sample t test, comparing data to the null hypothesis (no change) or to community norms when available, using the paired sample t test, or using the mixed model linear models when comparing groups. We analyzed pre–post categorical data with the χ2 and the McNemar tests. We addressed violations of normality or homogeneity of variance assumptions with nonparametric tests (e.g., the Mann–Whitney U test) that confirm results by providing a more conservative analysis without such assumptions.
RESULTS
There were 488 families (742 parents) enrolled in FOCUS family resiliency training from July 2008 through February 2010. Participants were self-referred (51.2%) or referred by providers (42.6%), including military medical, mental health, social services, chaplain, or school staff, with 6.2% indicating another referral source such as a military volunteer or a friend. The mean number of active duty parent deployments since the birth of the family's first child was 4.51 (SD = 4.78). Of 488 families, 331 (67.8%) completed the intervention; 89 (18.2%) were unable to complete it because of relocation or deployment, 42 (8.6%) reported the family was too busy to complete the program, 13 (2.7%) reported they no longer needed services, and 13 (2.7%) had not completed the program for unspecified “other” reasons.
Non–active duty and active duty parents enrolled in the program did not differ from each other on self-reported family functioning (FAD) or BSI distress levels, and both groups were significantly more distressed than were community norms. Non–active duty (mean = 1.93; SD = 0.54) and active duty (mean = 2.02; SD = 0.51) parents reported less healthy family functioning compared with community norms (mean = 1.84; SD = 0.43; t741 = 6.32; P < .001). On the global severity index of the BSI, both non–active duty (mean = 10.82; SD = 10.60) and active duty (mean = 7.89; SD = 9.20) parents had elevated distress relative to gender-specific community norms (females: mean = 8; t471 = 5.67; P < .001; males: mean = 5; t268 = 4.87; P < .001). Notably, 33.7% (n = 150) of non–active duty parents were above the cutoff of 30 for elevated posttraumatic stress symptoms at intake compared with 23.3% (n = 69) of active duty parents.
SDQ scores for boys enrolled in the program (mean = 13.54; SD = 6.9) were significantly higher than were those of normative data (mean = 7.63; SD = 5.9; t486 = 18.86; P < .001), as were scores for girls enrolled in the program (mean = 11.11; SD = 6.3 vs norms mean = 6.56; SD = 5.2; t378 = 4.55; P < .001).
There were no substantive differences in parent or child outcomes as a function of military branch, thus results are from combined data.
Characteristics of Participating Families
We have reported pre- and postintervention data from 331 families representing 466 parents (300 non–active duty and 166 active duty), with pre- and postassessment for at least 1 parent and 493 children from those families. The BSI was not part of the original follow-up assessment (it was added after the program's initial implementation for service delivery needs), and thus matched data for the BSI are available for only 287 parents (221 non–active duty and 66 active duty).
Non–active duty primary caretakers were predominantly female (97.2%). Of the 166 active duty caretakers, 27 (16.3%) were female. Most parents (95.6%) were married. The mean age of parents was 34.39 (SD = 6.04), with no difference between non–active duty and active duty parents. Posttraumatic stress symptoms were assessed once, soon after intake, showing elevations (PTSD Checklist ≥ 30) among 94 (31.3%) of non–active duty and 35 (21.2%) of active duty parents and no difference between families who completed intervention versus those who did not.
Reflecting the age demographics of the child population within the military at large, there were more children aged 3 to 7 years (61.1%) than aged 8 to 10 years (19.0%) or aged 11 years and older (19.9%). There were more boys (55.1%) than girls (44.9%).
Families and parents who completed the intervention were more likely to be self-referred, less distressed on the BSI and FAD, and older than noncompleters. Children who completed the intervention did not differ from those who did not at intake on the SDQ.
Implementation Process Outcomes
Perception of change and parent satisfaction ratings (from 0 to 7) were completed by 363 parents. Mean values ranged from 5.52 (SD = 0.79) for improvements in emotional regulation to 6.05 (SD = 0.95) for improvements in understanding combat stress and parent–child stress reactions, indicating a high degree of perceived change. Parent satisfaction mean ratings were also high, with 6.51 (SD = 0.69) for overall helpfulness to their family; a satisfaction with the program rating of 6.58 (SD = 0.62); and a willingness to recommend the program to another family rating of 6.70 (SD = 0.60). Ratings were similar for active duty and non–active duty parents.
Intervention Effects
Parental distress, family functioning, and global functioning levels at intake and postintervention are shown in Table 1. There were no significant time × group effects on any outcome.
TABLE 1.
Changes in Parental Distress, Family Functioning, and Global Functioning at Intake and Postintervention: Families OverComing Under Stress, United States and Japan, July 2008–February 2010
| Non–Active Duty, Mean (SD) |
Normative Data, Mean (SD) |
Active Duty, Mean (SD) |
||||||
| Intake | Post | Female | Male | Intake | Post | Time Effect (95% CI) | Group Effect (95% CI) | |
| BSI global severity index | 0.56 (0.56) | 0.29 (0.33) | 0.35 (0.37) | 0.25 (0.24) | 0.47 (0.53) | 0.21 (0.38) | 0.27*** (0.21, 0.33) | 0.09a (0.01, 0.18) |
| BSI anxiety | 0.65 (0.67) | 0.37 (0.43) | 0.44 (0.54) | 0.26 (0.31) | 0.52 (0.59) | 0.28 (0.41) | 0.27*** (0.20, 0.35) | 0.10a (0.01, 0.21) |
| BSI depression | 0.69 (0.73) | 0.32 (0.47) | 0.36 (0.56) | 0.21 (0.33) | 0.60 (0.68) | 0.18 (0.32) | 0.38*** (0.30, 0.47) | 0.13** (0.03, 0.23) |
| Family Assessment Device, general functioningb | 1.89 (0.54) | 1.73 (0.43) | 1.84 (0.43) | 1.84 (0.43) | 2.00 (0.49) | 1.82 (0.46) | 0.68*** (0.13, 0.20) | 0.09* (0.01, 0.18) |
| Global Assessment of Functioning | 72.54 (10.78) | 78.13 (9.53) | … | … | 74.46 (11.54) | 79.46 (9.43) | −5.40*** (−6.05, −4.75) | 1.43a (0.36, 3.21) |
Note. BSI = brief symptom inventory; CI = confidence interval. Family and global functioning increase and distress declines over time. BSI was analyzed with gender as covariate.
Not significant.
A Family Assessment Device score ≥ 2 refers to unhealthy functioning.
*P < .05; **P < .01; ***P < .001.
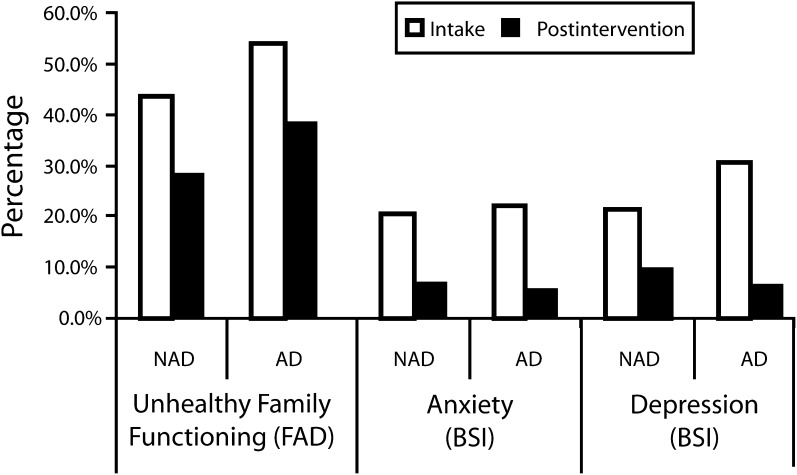
Change scores showed significant improvements across all measures for non–active duty parents and active duty parents (P < .001). BSI-assessed parental distress and FAD-assessed unhealthy family functioning were significantly reduced, and post scores were at or better than normative data. The provider GAF rating for global functioning was significantly improved after intervention, despite mean intake scores indicating minimal impairment at the outset. Figure 1 illustrates the percentage of parents with clinically meaningful impairments in family functioning and anxiety and depression symptoms at intake and postintervention. Both non–active duty families and active duty families demonstrated significant decreases in prevalence of impairment and distress symptoms from pre- to postintervention (all P values < .001).
FIGURE 1.
Reduction in prevalence of parental symptoms by phase (intake or postintervention): Families OverComing Under Stress, United States and Japan, July 2008–February 2010.
Note. BSI = Brief Symptom Inventory43; FAD = McMaster Family Assessment Device.41 All non–active duty (NAD) and active duty (AD) pre–post changes are significant (P < .001). Unhealthy functioning is indicated by a FAD score ≥ 2; only percentages > 2 are shown. We used BSI manual gender-specific clinically significant symptoms cutoffs; The figure shows percentages greater than the cutoff.
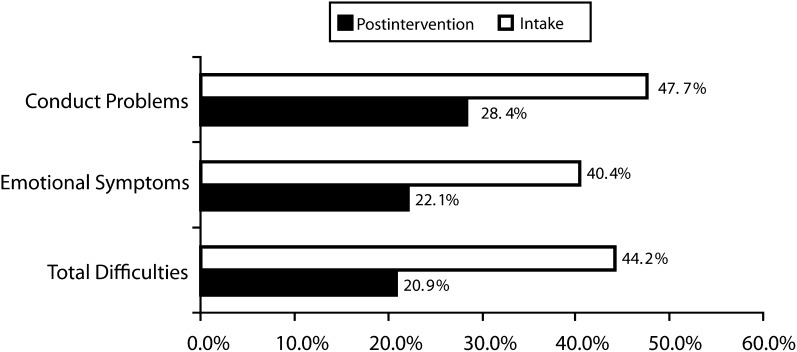
The SDQ total difficulties score and the prosocial behaviors subscale, by age and gender, are in Table 2. At intake, girls and boys in every age group were rated as significantly less adjusted than were comparative gender- and age-specific norms (P < .001). Change scores indicate significant reductions in the total difficulties score for boys and girls across all age groups (P < .001) and significant improvements in prosocial behaviors (P < .05 to P < .001). Figure 2 shows the prevalence of clinically significant conduct problems, emotional symptoms, and total difficulties at intake and postintervention. Reductions in the prevalence of children with clinically significant symptoms over time were all significant (P < .001).
TABLE 2.
Changes in Child Adjustment on the Strengths and Difficulties Questionnaire at Intake and Postintervention: Families OverComing Under Stress, United States and Japan, July 2008–February 2010
| Girls (n = 216) |
Boys (n = 277), Mean (SD) |
|||||||
| Age, y | Intake, Mean (SD) | Post, Mean (SD) | Norms, Mean (SD) | Intake, Mean (SD) | Post, Mean (SD) | Norms, Mean (SD) | Time Effect (95% CI) | Gender Effect (95% CI) |
| Total difficulties | ||||||||
| 3–7a | 11.59 (5.65) | 8.25 (5.20) | 6.8 (5.1) | 13.54 (6.93) | 9.71 (5.70) | 7.9 (5.5) | 3.59*** (2.98, 4.20) | 1.62** (0.43, 2.80) |
| 8–10b | 11.00 (7.23) | 7.41 (5.52) | 6.4 (5.1) | 13.47 (6.78) | 9.98 (6.57) | 7.9 (6.4) | 3.54*** (2.51, 4.57) | 2.55* (0.22, 4.88) |
| ≥ 11c | 11.63 (6.97) | 7.59 (5.72) | 6.5 (5.5) | 14.55 (6.59) | 10.25 (6.27) | 7.1 (5.8) | 4.17*** (3.03, 5.32) | 2.75* (0.43, 5.06) |
| Prosocial behavior | ||||||||
| 3–7a | 8.13 (1.97) | 8.86 (1.55) | 8.6 (1.7) | 7.21 (2.01) | 8.28 (1.78) | 8.2 (2.0) | −0.89*** (−0.69, −1.10) | −0.68*** (−0.32, −1.04) |
| 8–10b | 8.32 (1.90) | 8.80 (1.76) | 9.0 (1.5) | 7.61 (2.15) | 8.19 (1.75) | 8.6 (1.8) | −0.52** (−0.17, −0.88) | −0.64d (0.02, −1.29) |
| ≥ 11c | 8.24 (1.90) | 9.12 (1.36) | 8.9 (1.6) | 7.55 (2.06) | 8.07 (2.02) | 8.5 (1.9) | −0.65*** (−0.30, −1.00) | −0.93** (−0.29, −1.57) |
Note. CI = confidence interval; NS = not significant. Time × gender effects were not significant and are not shown. Total difficulties decline and prosocial behavior increases.
Sample size is n = 295: 131 girls and 164 boys.
Sample size is n = 101: 44 girls and 57 boys.
Sample size is n = 97: 41 girls and 56 boys.
Not significant.
*P < .05; **P < .01; ***P < .001.
FIGURE 2.
Reduction in prevalence of child symptoms by phase (intake or postintervention): Families OverComing Under Stress, United States and Japan, July 2008–February 2010.
Note. The single-sample t-test against null hypothesis (no change) was significant (P < .001) for all scales. Subscales are from the Strengths and Difficulties Questionnaire.46 Per the manual, the cutoff for “normal,” conduct problems: 2; emotional symptoms: 3; total difficulties: 13. Percentages greater than normal are shown.
Children aged 7 years and older who completed a self-report of coping at intervention intake and exit (Kidcope; n = 298) evidenced significant increases in the use of positive coping strategies. McNemar tests indicated improvements in emotional regulation, problem solving, cognitive restructuring, and increased use of social support (all P values significant at P < .001).
DISCUSSION
Increased attention has been paid to identifying the psychological health needs of service members and their families and to identifying and responding to gaps in the continuum of preventive care for military families.27,50 This has led to the proliferation of expanded and new programs and resources to address the needs of military families. Despite the expansion of family services provided by the public and private sectors, there has been limited systematic evaluation of these programs to guide national screening and prevention efforts. Our evaluation provides both implementation process and effectiveness findings that demonstrate the acceptability, feasibility, and effectiveness of strength-based, family-centered skills training designed to promote resilience and mitigate wartime deployment distress in military families.
The implementation and process outcomes provide preliminary evidence that recipients of FOCUS perceive that the program addresses relevant issues facing them during deployment and reintegration transitions. Consistent with the implementation of FOCUS as a selective prevention program, families entering the program may be proactively seeking to enhance coping in the face of increased challenges or may already be experiencing deployment distress. About one third of individuals entering the program were also referred to other social support and mental health providers, indicating the potential for selective prevention as a gateway to other services when needed.
Consistent with recent studies of military families who experienced wartime deployments, parents and children entering FOCUS were more likely to report symptoms of psychological distress than were nonmilitary gender-matched peers.2,16,24 Notably, non–active duty spouses were as vulnerable to distress, including posttraumatic stress symptoms, as were their active duty partners. Military family experts have noted that the stress demands of civilian spouses may equal or even surpass their active duty partners because they lack the support of being embedded in a cohesive unit, they frequently lack clear information on the risk status of their loved one, and they are unable to act instrumentally on his or her behalf.51 Child distress was common at program entry, underscoring the relevance of providing selective preventive services that may provide early mitigation of child psychological distress.25
As anticipated, both parents and children participating in FOCUS demonstrated significant improvement in emotional and behavioral adjustment. Further, children's prosocial behaviors and positive coping skills increased from initiation of training to postintervention. The reductions in psychological distress for both service members and spouse parents are noteworthy given the brevity of the intervention and the importance of parental psychological health and effective parenting to family and child resilience and adaptation.2,36,52
FOCUS enhances family resilience processes and targets individual parent and child distress. The model provides individual and family level training in resiliency skills and builds on existing family strengths and increases family cohesion, communication, and support and the maintenance of consistent care routines in the home—all core characteristics of resilient families.36,53 On standardized assessment, we found that family adjustment improved significantly. We hypothesized that reduced parental distress and improved family adjustment would support positive child adaptation. Significant postintervention reductions in emotional and behavioral problems for boys and girls in all age groups support this hypothesis.
This evaluation also provides initial information regarding the challenges of implementing family prevention services for a mobile military population. Of the approximately 30% of families who initiated services but did not complete the intervention, more than half (18.2%) did not complete because of work-related relocations or deployments. Despite this “artificially inflated” attrition rate, almost 70% of families enrolled completed the FOCUS intervention, representing service completion rates much higher than those of community child mental health services (25%–60%; for review, see Greeno et al.54). The evaluation also indicates that more distressed parents may have had greater difficulty completing the program, suggesting that higher risk families may require greater outreach and engagement, processes to bridge services during relocations, or improved identification and support for referral.
We conducted this service program evaluation on an existing data set, and it is limited by the lack of a control group. We have addressed the absence of a control group in several ways. We conducted analysis of change scores, verifying that reductions in symptoms occurred among those parents and children who were above and below clinical cutoffs at baseline. Reductions in the prevalence of clinically significant distress after intervention also suggest meaningful improvement. Both parents and children gave satisfaction ratings, and parents also rated the degree of perceived change around the core family domains, which were the intended targets for intervention change. Children also self-reported on specific ways of coping with a self-selected problem, indicating the process by which mental health symptoms may have improved. Also, clinician ratings of change augmented participant self-report measures. Although child developmental processes could have contributed to the positive outcomes, the brief nature of the intervention makes it unlikely that nonintervention changes could account for such rapid improvement across all age groups. An “attention-control” group in future evaluation studies may help to verify the active ingredients of positive intervention change.
Despite its limitations, this evaluation provides preliminary evidence that FOCUS for military families is feasible, is well tolerated, and can lead to significant benefits for parents, children, and families. Future examination of implementation challenges and program evaluation of FOCUS services in other service branches and for geographically dispersed populations, such as the National Guard and Reservists, will be important to provide information about program generalizability for other military branches.
Acknowledgments
The US Department of the Navy, Bureau of Medicine and Surgery (contract No. N00189-09-C-Z057) and the Frederick R. Weisman Philanthropic Foundation and Discretionary Trust supported Families OverComing Under Stress.
Human Participant Protection
The University of California, Los Angeles institutional review board approved this evaluation.
References
- 1.Lincoln A, Swift E, Shorteno-Fraser M. Psychological adjustment and treatment of children and families with parents deployed in military combat. J Clin Psychol. 2008;64(8):984–992 [DOI] [PubMed] [Google Scholar]
- 2.Palmer C. A theory of risk and resilience factors in military families. Mil Psychol. 2008;20(3):205–217 [Google Scholar]
- 3.Waldrep DA, Cozza SJ, Chun RS. The impact of deployment on the military family. : The National Center for Post Traumatic Stress Disorder, The Iraq War Clinician Guide. 2nd ed Washington, DC: Department of Veterans Affairs; 2004:83–86 [Google Scholar]
- 4.National Research Council, Institute of Medicine. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: National Academies Press; 1994 [PubMed] [Google Scholar]
- 5.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22 [DOI] [PubMed] [Google Scholar]
- 6.Baker DG, Heppner P, Niloofar Aet al. Trauma exposure, branch of service, and physical injury in relation to mental health among U.S. veterans returning from Iraq and Afghanistan. Mil Med. 2009;174(8):773–778 [PubMed] [Google Scholar]
- 7.Erbes C, Westermeyer J, Engdahl B, Johnsen E. Post-traumatic stress disorder and service utilization in a sample of service members from Iraq and Afghanistan. Mil Med. 2007;72(4):359–363 [DOI] [PubMed] [Google Scholar]
- 8.Gibbs DA, Martin SL, Kupper LL, Johnson RE. Child maltreatment in enlisted soldiers’ families during combat-related deployments. JAMA. 2007;298(5):528–535 [DOI] [PubMed] [Google Scholar]
- 9.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463 [DOI] [PubMed] [Google Scholar]
- 10.Lew HL, Poole JH, Guillory SB, Salerno RM, Leskin G, Sigford BJ. Persistent problems after traumatic brain injury: the need for long-term follow-up and coordinated care. J Rehabil Res Dev. 2006;43(2):vii–x [DOI] [PubMed] [Google Scholar]
- 11.McCarroll JE, Fan Z, Newby JH, Ursano RJ. Trends in US army child maltreatment reports: 1990–2004. Child Abuse Rev. 2008;17(2):108–118 [Google Scholar]
- 12.Okie S. Traumatic brain injury in the war zone. N Engl J Med. 2005;352(20):2043–2047 [DOI] [PubMed] [Google Scholar]
- 13.Rentz ED, Marshall SW, Loomis D, Casteel C, Martin SL, Gibbs DA. Effects of deployment on the occurrence of child maltreatment in military and nonmilitary families. Am J Epidemiol. 2007;165(10):1199–1206 [DOI] [PubMed] [Google Scholar]
- 14.Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vasterling JJ, Proctor SP, Friedman MJet al. PTSD symptom increases in Iraq-deployed soldiers: comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. J Trauma Stress. 2010;23(1):41–51 [DOI] [PubMed] [Google Scholar]
- 16.Lester P, Peterson K, Reeves Jet al. The long war and parental combat deployment: effects on military children and at-home spouses. J Am Acad Child Adolesc Psychiatry. 2010;49(4):310–320 [PMC free article] [PubMed] [Google Scholar]
- 17.Flake EM, Davis BE, Johnson PL, Middleton LS. The psychosocial effects of deployment on military children. J Dev Behav Pediatr. 2009;30(4):271–278 [DOI] [PubMed] [Google Scholar]
- 18.Chandra A, Burns RM, Tanielian TLet al. Understanding the Impact of Deployment on Children and Families: Findings From a Pilot Study of Operation Purple Camp Participants. Santa Monica, CA: RAND; 2008 [Google Scholar]
- 19.Chartrand MM, Frank DA, White LF, Shope TR. Effect of parents’ wartime deployment on the behavior of young children in military families. Arch Pediatr Adolesc Med. 2008;162(11):1009–1014 [DOI] [PubMed] [Google Scholar]
- 20.Rosen LN, Teitelbaum JM, Westhuis DJ. Children's reactions to the Desert Storm deployment: initial findings from a survey of army families. Mil Med. 1993;158(7):465–469 [PubMed] [Google Scholar]
- 21.Huebner AJ, Mancini JA, Wilcox RM, Grass SR, Grass GA. Parental deployment and youth in military families: exploring uncertainty and ambiguous loss. Fam Relat. 2007;56(2):112–122 [Google Scholar]
- 22.Rutter M, Quinton D. Parental psychiatric disorder: effects on children. Psychol Med. 1984;14(4):853–880 [DOI] [PubMed] [Google Scholar]
- 23.Cozza SJ, Chun RS, Polo JA. Military families and children during operation Iraqi Freedom. Psychiatr Q. 2005;76(4):371–378 [DOI] [PubMed] [Google Scholar]
- 24.Chandra A, Lara-Cinisomo S, Jaycox LHet al. Children on the homefront: the experience of children from military families. Pediatrics. 2009;125(1):16–25 [DOI] [PubMed] [Google Scholar]
- 25.National Research Council and Institute of Medicine Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment and Prevention. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 26.Beardslee WR, Avery MW, Ayoub C, Watts CL. Family connections: helping Early Head Start/Head Start staff and parents address mental health challenges. Zero to Three. 2009;29(6):34–42 [Google Scholar]
- 27.Rotheram-Borus MJ, Lee MB, Gwadz M, Draimin B. An intervention for parents with AIDS and their adolescent children. Am J Public Health. 2001;91(8):1294–1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lester P, Rotheram-Borus MJ, Elia C, Elkavich A, Rice E. TALK: teens and adults learning to communicate. : LeCroy CW, Evidence-Based Treatment Manuals for Children and Adolescents. New York: Oxford University Press; 2008:170–285 [Google Scholar]
- 29.Compas BE, Phares V, Ledoux N. Stress and coping preventive interventions with children and adolescents. : Bond LA, Compas BE, Primary Prevention and Promotion in the Schools. Beverly Hills, CA: Sage; 1989:60–89 [Google Scholar]
- 30.Patterson JM, McCubbin HI. Adolescent coping style and behaviors: conceptualization and measurement. J Adolesc. 1987;10(2):163–186 [DOI] [PubMed] [Google Scholar]
- 31.Layne CM, Saltzman WR, Poppleton Let al. Effectiveness of a school-based psychotherapy program for war-exposed adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2008;47(9):1048–1062 [DOI] [PubMed] [Google Scholar]
- 32.Spoth RL, Kavanagh K, Dishion T. Family-centered preventive intervention science: toward benefits to larger populations of children, youth, and families. Prev Sci. 2002;3(3):145–152 [DOI] [PubMed] [Google Scholar]
- 33.Sroufe LA. Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev. 2005;7(4):349–367 [DOI] [PubMed] [Google Scholar]
- 34.Lester P, Leskin G, Woodward Ket al. Wartime deployment and military children: applying prevention science to enhance family resilience. : MacDermid Wadsworth S, Riggs D, Risk and Resilience in U.S. Military Families. New York: Springer; 2010:149–173 [Google Scholar]
- 35.Saltzman WR, Lester P, Pynoos Ret al. FOCUS for Military Families: Individual Family Resiliency Training Manual. 2nd ed; 2009. [unpublished manual] [Google Scholar]
- 36.Walsh F. Strengthening Family Resilience. 2nd ed New York: Guilford Press; 2006 [Google Scholar]
- 37.MacDermid SM, Samper R, Schwarz R, Nishida J, Nyaronga D. Understanding and Promoting Resilience in Military Families. West Lafayette, IN: Military Family Research Institute, Purdue University; 2008 [Google Scholar]
- 38.Nash WP. U.S. Marine Corps and Navy combat and operational stress continuum model: a tool for leaders. : Ritchie EC, Combat and Operational Behavioral Health. Washington, DC: Borden Institute Textbook of Military Psychiatry; 2011:107–119 [Google Scholar]
- 39.Lester P, Mogil C, Saltzman Wet al. Families OverComing Under Stress: implementing family-centered prevention for military families facing wartime deployments and combat operational stress. Mil Med. 2011;176(1):19–25 [DOI] [PubMed] [Google Scholar]
- 40.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Presented at the Ninth Annual Meeting of ISTSS; October 1993; San Antonio, TX [Google Scholar]
- 41.Walker EA, Newman E, Dobie DJ, Ciechanowski P, Katon W. Validation of the PTSD Checklist in an HMO sample of women. Gen Hosp Psychiatry. 2002;24(6):375–380 [DOI] [PubMed] [Google Scholar]
- 42.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76(2):272–281 [DOI] [PubMed] [Google Scholar]
- 43.Derogatis LR. Brief Symptom Inventory 18 (BSI-18): Administration, Scoring, and Procedures Manual. Minneapolis: National Computer Systems Pearson, Inc; 2001 [Google Scholar]
- 44.Derogatis LR. Brief Symptom Inventory (BSI): Administration, Scoring, and Procedures Manual. 3rd ed. Minneapolis: National Computer Systems Pearson, Inc; 1993 [Google Scholar]
- 45.Ryan CE, Epstein NB, Keitner GI, Miller IW, Bishop DS. Evaluation and Treating Families: The McMaster Approach. New York: Routledge; 2005 [Google Scholar]
- 46.Diagnostic and Statistical Manual of Mental Disorders. Rev 4th ed Washington, DC: American Psychiatric Association; 2000 [Google Scholar]
- 47.Beardslee WR, Gladstone TRG, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: evidence of parental and child change. Pediatrics. 2003;112:e119–e131 [DOI] [PubMed] [Google Scholar]
- 48.Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177:534–539 [DOI] [PubMed] [Google Scholar]
- 49.Spirito A, Stark LJ, Williams C. Development of a brief coping checklist for use with pediatric populations. J Pediatr Psychol. 1988;13(4):555–574 [DOI] [PubMed] [Google Scholar]
- 50.Department of Defense Task Force on Mental Health An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board; 2007 [Google Scholar]
- 51.Nash W. Combat Operational Stress Control: The Family Dynamic. Presented at a Professional Development Training Course of the Department of the Navy; 2009; Washington, DC [Google Scholar]
- 52.Gewirtz A, Forgatch M, Wieling E. Parenting practices as potential mechanisms for child adjustment following mass trauma. J Marital Fam Ther. 2008;34(2):177–192 [DOI] [PubMed] [Google Scholar]
- 53.Walsh F. A family resilience framework: innovative practice applications. Fam Relat. 2002;51(2):130–137 [Google Scholar]
- 54.Greeno CG, Anderson CM, Stork E, Kelleher KJ, Shear K, Mike G. Treatment after assessment in a community children's mental health clinic. Psychiatr Serv. 2002;53(5):624–626 [DOI] [PubMed] [Google Scholar]