Abstract
Objectives. Our objective was to examine all suicides (n = 423) in 2 geographic areas of the Veterans Health Administration (VHA) over a 7-year period and to perform detailed chart reviews on the subsample that had a VHA visit in the last year of life (n = 381).
Methods. Within this sample, we compared a group with 1 or more documented psychiatric symptoms (68.5%) to a group with no such symptoms (31.5%). The groups were compared on suicidal thoughts and behaviors, somatic symptoms, and stressors using the χ2 test and on time to death after the last visit using survival analyses.
Results. Veterans with documented psychiatric symptoms were more likely to receive a suicide risk assessment, and have suicidal ideation and a suicide plan, sleep problems, pain, and several stressors. These veterans were also more likely to die in the 60 days after their last visit.
Conclusions. Findings indicated presence of 2 large and distinct groups of veterans at risk for suicide in the VHA, underscoring the value of tailored prevention strategies, including approaches suitable for those without identified psychiatric symptoms.
Suicide is the eleventh leading cause of death in the United States and the fifth leading cause of years of potential life lost before age 65 years.1 Prevention efforts must include a focus on veterans who use Veterans Health Administration (VHA) services.2 The VHA is the largest health care system in the United States, and each year more than 1800 veterans using VHA services die by suicide,3 representing 5% to 6% of all suicides in the United States annually. Moreover, compared with the general US population, rates of suicide in veterans using VHA services are estimated to be 1.66-times higher (95% confidence interval [CI] = 1.58, 1.74) among men and 1.87-times higher (95% CI = 1.35, 2.47) among women.3
In a recent, national study of veterans who used VHA services, depression, bipolar disorder, posttraumatic stress disorder (PTSD), schizophrenia, and alcohol or drug use disorders were associated with increased risk of suicide,4 which was congruent with findings in the general literature.5,6 Interestingly, slightly less than half (i.e., 46.8%) of VHA patients who killed themselves were diagnosed with a mental disorder. The study was based on clinician diagnoses, and greater psychopathology would have undoubtedly been uncovered using research interviews. Nonetheless, the study indicated that a large proportion of VHA patients who killed themselves did not have documented (or recorded) symptoms of psychopathology.
Suicide decedents who receive psychiatric treatment differ from those who do not in demographics, diagnoses, and the type of stressors they experience,7–9 suggesting that there are likely to be important differences between decedents with and without recorded psychiatric symptoms. These findings have implications for prevention and suggest the potential need for universal strategies to reduce risk for suicide in the group without documented psychiatric symptoms. Additionally, the differences between those with and without documented psychiatric symptoms are likely to extend to patterns of service use before death, with those reporting more symptoms making greater contact with the health care system and, thus, potentially having a shorter time to death after their last visit.
The purpose of our study was to compare 2 broad groups of users of VHA services who died by suicide, a group with clinician-documented psychiatric symptoms (i.e., depression, anxiety, alcohol use disorders, drug use disorders, schizophrenia, and mania) in the last year of life, and a group with no documented symptoms. Using systematic chart reviews, we examined differences in sociodemographic characteristics, suicide-related variables (i.e., received a suicide risk assessment, suicidal ideation, suicide plan, suicide attempt), treatment contacts (i.e., received care from a mental health professional), somatic symptoms (i.e., sleep, pain), and specific stressors (i.e., occupational, relational, housing, legal) in the last year of life and at the last visit (when data were available), as well as time to death after the last visit. We hypothesized that the medical records of the group with recorded symptoms would also be more likely to show suicide-related variables, somatic symptoms, and stressors. We also explored time to death in the 2 study groups.
METHODS
Participants were all 423 suicide decedents who received VHA services between fiscal years (FYs) 2000 and 2006 from either Veterans Integrated Service Network 2 (VISN 2; upstate New York and north central Pennsylvania, n = 130) or VISN 11 (central Illinois, Indiana, Michigan, and northwest Ohio, n = 293). Analyses focused on the 381 (90.07%) participants who received VHA services during the last year of life. The 42 (9.93%) decedents who were excluded from the analyses were more likely to be non-White (χ2 = 13.60; P < .001) and younger (χ2 = 13.60; P < .05) than those who were included.
Data Sources
Comprehensive information on patient factors and treatment utilization before suicide were obtained from 3 unique sources: (1) the VHA National Patient Care Database (NPCD) and other nationwide data resources available at the Austin Automation Center, (2) the National Center for Health Statistics (NCHS) National Death Index (NDI), and (3) information contained within the VHA Computerized Patient Record System (CPRS).
NPCD and NDI data.
Using linked data from the NPCD and the NDI, the VISN 11 Serious Mental Illness Training, Research, and Education Center (SMITREC) created a National Suicide Registry that contains information about suicide on all patients who used VHA services in FYs 2000 to 2007. The NPCD was used to identify all individuals who used VHA inpatient, residential, or outpatient services between FY 2000 through the end of FY 2007 and who did not have any record of VHA service use in FYs 2008 or 2009.
The NDI draws from US mortality data regarding dates and causes of death for all US residents. Data are derived from death certificates filed in state vital statistics offices and checked for accuracy by NCHS. NDI searches were conducted for all individuals identified by the NPCD search. The NDI data request protocol matched records using social security number, last name, first name, middle initial, date of birth, race/ethnicity, gender, and state of residence. Frequently, NDI searches yielded multiple records that were potential matches. In these instances, previously established procedures were used to ensure that the individuals identified by NPCD and NDI searches were the same person.10 The NDI is considered the “gold standard” for mortality assessment information because it has the greatest sensitivity in determining vital status among all available population-level sources of mortality data.11
CPRS data.
All clinical notes about care provided within the VHA system are recorded in the CPRS medical record. Notes can be written in free form or using templates, and typically include information about the patient’s presenting problem and the type of care provided. CPRS data therefore provides information about symptoms (e.g., suicidal thoughts) or disorders that are noted in the narrative of notes and not limited to official templates that are tied to visit encounters, notations about patient stressors, or treatment plans.
Chart Reviews
Chart reviews were conducted at the Center of Excellence for Suicide Prevention located in VISN 2. They were used to extract data on documented symptoms of depression, alcohol use disorders, illicit drug use, prescription drug misuse, PTSD, mania, schizophrenia, sleep disturbance, and subjective pain. Note that symptoms were recorded whether there was a formal diagnosis, necessitating the use of chart reviews (as opposed to aggregate electronic data). Common stressors (e.g., marital or intimate relationship, employment, legal, housing) were also extracted from the charts.
One of the authors (M. V.) developed the chart review tool for a study of veterans treated for depression.12 The tool systematically assesses care provided by the VHA in the year before suicide (last year codes) as well as during the last visit (last visit codes). For each patient record, we used 2 or more independent coders who, after initial coding, met to compare results and resolve discrepancies to create a consensus record for use in analyses. When a clear consensus could not be reached, the coding decisions were staffed at a weekly consensus conference. To assess the interrater reliability before consensus, we calculated weighted kappas among raters for both last year and last visit codes. Kappas were weighted to reflect the proportion of charts coded by each pair of raters. Landis and Koch’s recommendations were used to classify kappas into poor (≤ 0.40), moderate (0.41–0.60), substantial (0.60–0.79), and outstanding (≥ 0.80) categories.13
Variables
Demographic characteristics.
Patients’ age and gender are consistently available in VHA electronic treatment records.
Psychiatric symptoms.
Chart reviews assessed symptoms whether they reached a diagnostic threshold (e.g., depressive disorder) as well as symptoms (e.g., depressive symptoms), hereafter referred to as documented or recorded symptoms. These data were used to form the 2 study groups. Kappas for reliability between pairs of raters on documented symptoms were outstanding: depression (0.95 last year, 0.86 last visit), anxiety (0.89 last year, 0.91 last visit), alcohol use disorder (0.84 last year, 0.79 last visit), mania (0.89 last year, 0.97 last visit), psychosis (0.91 last year, 0.95 last visit), illicit drug use (0.92 last year, 0.81 last visit), and misuse of prescription drugs (0.80 last year, 0.82 last visit).
Treatment contacts.
Chart reviews were used to identify the specialization of the provider seen on the last visit (nonphysician and nonmental health, nonphysician and mental health, physician and nonmental health, or physician and mental health) to examine differences in the mental health treatment received by each group. The number of days between the last visit and death was also calculated to estimate the immediacy of risk between the 2 groups. The kappa for raters’ reliability of specialization of the provider was outstanding: mental health provider (0.84 last visit).
Suicide-related variables.
Chart reviews were used to identify if a suicide risk assessment was conducted, and suicidal thoughts, plans, and previous attempts were recorded. History of suicide attempts was used because of the low number of documented suicide attempts in the year before death. Kappas for reliability of raters on suicide-related variables were substantial or outstanding: risk assessment (0.85 last year, 0.75 last visit), suicidal thoughts (0.85 last year, 0.75 last visit), suicidal plan (1.00 last year), and suicide attempts (0.82 last year); agreement on suicidal plan at the last visit was not given because it was rare.
Somatic symptoms.
Chart reviews also identified information on documented sleep and pain complaints. Sleep is a symptom of many psychiatric and physical disorders.14–16 Previous work found that VHA patients with higher self-report of pain were at moderately increased risk for suicide.17 Kappas for reliability of raters on somatic symptoms were substantial or outstanding: sleep (0.85 last year, 0.63 last visit) and pain (0.68 last year, 0.76 last visit).
Stressors.
Information about stressors was also obtained from the chart. Domains of interest included marital or intimate relationship, legal, housing, and occupational problems. Kappas for reliability between raters on somatic stressors were substantial or outstanding: marital or intimate relationship (0.75), legal (0.72), housing (0.82), and occupational (0.77).
Analyses
We compared the 2 study groups using the χ2 test. For comparisons with sample sizes less than 5, we used the Fisher exact 2-sided test. Comparisons were made on demographic characteristics, treatment contacts (received care from a mental health professional), suicide-related variables (received a suicide risk assessment, presence of suicidal ideation, suicide plan, suicide attempt), somatic symptoms (presence of sleep or pain), and stressors (presence of occupational, relational, housing, legal) for the last year and last visit, when available.
Survival analyses compared days until death for the 2 study groups using Cox proportional hazard models, which can be used for uncensored data.18,19 The day of last contact was treated as day 1 to account for the 4 deaths that occurred on the day of contact. Initial models included all demographic variables, which were removed from the models if they were associated at P > .05. Diagnosis violated the proportionality assumption. We therefore treated it as a time-varying covariate and calculated hazard ratios (HRs) over periods of time (i.e., 1–30, 31–60, 61–180, 181–365 days) within the same model. To examine the hazards of suicidal ideation, secondary analyses compared the association of suicidal ideation to time to death after controlling for documented symptoms and statistically significant demographic variables. Because suicidal ideation also violated the proportionality assumption, its HRs were calculated using the same strategy.
RESULTS
Analyses were based on the 381 patients who used services in the year preceding suicide. Of these veterans, 261 (68.5%) had clinician-documented symptoms and 120 (31.5%) had no recorded symptoms. Descriptive statistics indicated that there were differences in age and race/ethnicity between the 2 groups (see Table 1). Those with recorded symptoms were significantly more likely to receive a suicide risk assessment and report suicidal ideation and plans, the presence of occupational-, relational-, legal-, and housing-related stressors, as well as somatic symptoms such as chronic pain and sleep disturbance (see Table 2). Among those with documented symptoms, 91 of 198 (46.0%) who received a suicide risk assessment in the last year reported suicidal ideation, whereas no individuals without documented symptoms reported suicidal ideation.
TABLE 1—
Demographics Among Veterans Health Administration Suicide Decedents, by Symptom Status: VISN 2 and VISN 11, 2000–2007
| Characteristics | With Symptoms, No. (%) | Without Symptoms, No. (%) | χ2 | P |
| Total | 261 (68.5) | 120 (31.5) | ||
| Gender | … | .091a | ||
| Male | 251 (96.2) | 119 (99.2) | ||
| Female | 10 (3.8) | 1 (0.8) | ||
| Race/ethnicityb | 5.23 | .022 | ||
| White | 220 (84.3) | 89 (74.2) | ||
| Minority | 40 (15.3) | 30 (25.0) | ||
| Age, y | 40.16 | < .001 | ||
| 18–34 | 6 (2.3) | 5 (4.2) | ||
| 35–54 | 61 (23.4) | 10 (8.3) | ||
| 55–74 | 133 (51.0) | 40 (33.3) | ||
| > 75 | 61 (23.4) | 65 (54.2) | ||
| VISN center | 0.01 | 0.909 | ||
| VISN 2 | 83 (31.8) | 37 (30.8) | ||
| VISN 11 | 179 (68.6) | 82 (68.3) | ||
Note. VISN = Veterans Integrated Services Network.
One-sided Fisher exact test.
Race/ethnicity was missing for 2 participants.
TABLE 2—
Suicide-Related Variables, Somatic symptoms, and Stressors Among Veterans Health Administration Suicide Decedents, by Symptom Status: VISN 2 and VISN 11, 2000–2007
| Variables | With Symptoms (n = 261), No. (%) | Without Symptoms (n = 120), No. (%) | χ2 | P |
| Last Year | ||||
| Suicide-related variables | ||||
| Assess suicidal ideation | 198 (75.9) | 25 (20.8) | 102.56 | < .001 |
| Suicidal ideation | 91 (34.9) | 0 | … | < .001a |
| Suicidal plan | 47 (18.0) | 0 | … | < .001a |
| Suicide attempt (ever) | 24 (9.2) | 0 | … | < .052a |
| Somatic symptoms | ||||
| Sleep | 157 (60.2) | 16 (13.3) | 72.69 | < .001 |
| Pain | 219 (83.9) | 72 (60.0) | 26.04 | < .001 |
| Stressors | ||||
| Occupational | 89 (34.1) | 5 (4.2) | 38.85 | < .001 |
| Relational | 66 (25.3) | 1 (0.8) | … | < .001a |
| Housing | 36 (13.8) | 0 | … | < .001a |
| Legal | 36 (13.8) | 1 (0.8) | … | < .001a |
| Last Visit | ||||
| Treatment contact: Psychiatric treatment | 90 (34.5) | 1 (0.8) | … | < .001a |
| Suicide-related variables | ||||
| Assess suicidal ideation | 105 (40.2) | 11 (9.2) | 37.46 | < .001 |
| Suicidal ideation | 15 (5.7) | 0 | … | .003a |
| Suicidal plan | 3 (1.1) | 0 | … | .32a |
| Somatic symptoms | ||||
| Sleep | 54 (20.7) | 8 (6.7) | 11.86 | .001 |
| Pain | 98 (37.5) | 44 (36.7) | 0.03 | .869 |
Note. VISN = Veterans Integrated Services Network.
One-sided Fisher exact test.
The group with reported symptoms was significantly more likely to be seen by a mental health professional for the last visit, receive a suicide risk assessment, and have recorded suicidal ideation and sleep complaints. There was no difference in documentation of chronic pain between the 2 groups at the last visit. Among those with recorded symptoms, 15 of 105 (14.3%) who received a suicide risk assessment at the last visit reported suicidal ideation. No individuals in the group without documented symptoms reported suicidal ideation at the last visit.
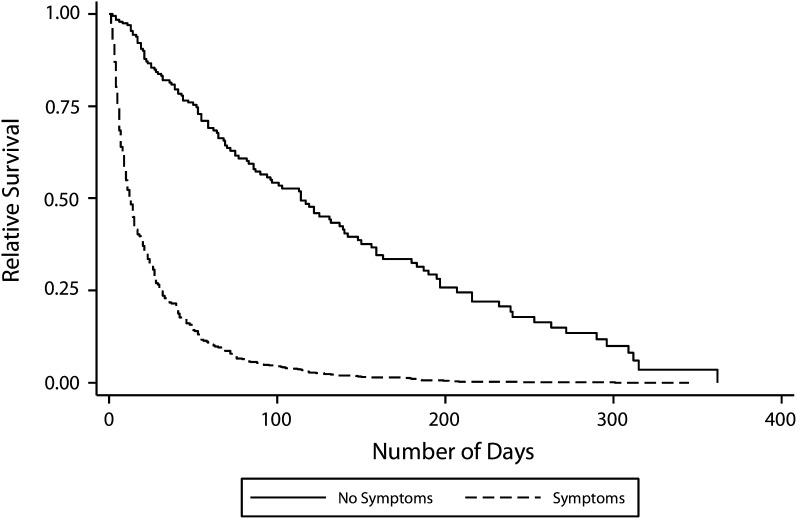
The 2 study groups differed in time to death after the last visit. Individuals with documented symptoms were almost 3 times as likely to die within 30 days of contact (HR = 2.95; 95% CI = 1.98, 4.39) and 74% more likely to die within 31 to 60 days of contact (HR = 1.74; 95% CI = 1.06, 2.85), but were not more likely to die after 60 days (61–90 days; HR = 1.32; 95% CI = 0.71, 2.43), 91 to 180 days(HR = 1.08; 95% CI = 0.64, 1.84), or 181 to 365 days (HR = 1.43;95% CI = 0.77, 2.65), after control for age cohort (HR = 1.20; 95% CI = 1.04, 1.38) and male gender (HR = 0.38; 95% CI = 0.21, 0.72). A survival curve was used to illustrate the difference in probability of death at any time point between these 2 groups (Figure 1).
FIGURE 1—
Suicide survival among Veterans Health Administration suicide decedents, by symptom status: VISN 2 and VISN 11, 2000–2007.
Note. VISN = Veterans Integrated Service Network.
Because of the potential importance of suicidal ideation, secondary analyses were conducted to compare time to death between those with documented suicidal ideation in their last year (n = 91) and those with no suicidal ideation (n = 290). Individuals with suicidal ideation were over twice as likely to die within 30 days of contact (HR = 2.19; 95% CI = 1.57, 3.05), but were not more likely to die after 30 days (31–60 days: HR = 1.75; 95% CI = 0.99, 3.08; 61–90 days: HR = 0.34; 95% CI = 0.08, 1.42; 91–180 days: HR = 0.80; 95% CI = 0.36, 1.78; 181–365 days: HR = 0.69; 95% CI = 0.26, 1.84), after control for documented symptoms (HR = 1.68; 95% CI = 1.32, 2.13), age cohort (HR = 1.24; 95% CI = 1.08, 1.43), and male gender (HR = 0.45; 95% CI = 0.24, 0.83). A survival curve was also used to illustrate the difference in probability of death at any time point between these 2 groups (Figure 2).
FIGURE 2—
Suicide survival among Veterans Health Administration suicide decedents, by ideation status: VISN 2 and VISN 11, 2000–2007.
Note. VISN = Veterans Integrated Service Network.
DISCUSSION
We examined differences in demographic characteristics, suicide-related variables, somatic symptoms, stressors, and time to death after the last visit between veteran decedents with documented symptoms in the last year of life (68.5%) and those with no such symptoms (31.5%).
As hypothesized, the group with recorded symptoms was more likely to receive a suicide risk assessment and to report suicidal ideation and a plan in the last year of life than was the group without such symptoms. Similarly, those with documented symptoms were also more likely to receive care from a mental health specialist, receive a suicide assessment, and report suicidal ideation at the last visit. Thus, the group with documented symptoms was more likely to be identified as being at high risk, providing the opportunity for intervention. These individuals might have required more intensive treatments that directly target suicide risk, such as cognitive therapy for suicide prevention20 or dialectical behavioral therapy,21,22 although the utility of such treatments with veterans remains to be demonstrated. The percentage of suicides with documented symptoms in the present study (68.5%) was considerably lower compared with that identified in postmortem psychological autopsy studies of suicide,23,24 suggesting clinical underdetection and the potential value of increased screening and improved risk recognition. Additional universal strategies would also be of benefit,25 particularly for patients who were not identified as having psychiatric symptoms despite screening efforts.
The group with recorded symptoms also had more documented somatic symptoms in the year before suicide and at the last visit than decedents without documented symptoms, with 1 exception. There was no difference in recorded chronic pain between the 2 subpopulations at the last visit. Previous research found an association between self-reported pain and risk for suicide in VHA patients.17 Nonsymptomatic high-risk veterans might be more willing to disclose pain when they are distressed, suggesting that increased pain in veterans without reported symptoms might be indicative of increased risk. Alternatively, pain might be a risk factor for suicide that was mostly independent of psychiatric symptoms.17 In addition, veterans with recorded symptoms also had more documented stressors than those with no symptoms, with occupational and relational stressors being the most prevalent. Research on the association of pain, occupational, and relational problems with suicide risk in veterans might identify important targets for selective interventions.
Individuals with documented symptoms were more likely to die by suicide within the first 60 days after contact, and those with suicidal ideation were more likely to die by suicide in the first 30 days. The associations among psychiatric problems, suicidal ideation, and time to death might have important implications for prevention efforts, with a history of greater psychiatric and suicidal symptoms indicating a need for more timely and intensive intervention. Caring letters, for example, were found to reduce risk for suicide for depressed inpatients who refused postdischarge treatment.26 For veterans with documented symptoms, the data suggested the value of implementing such letters early in the course of treatment. Additionally, this finding further highlighted the need for intensive interventions that directly target suicide risk for veterans reporting suicidal ideation.
Over 30% of the sample had no reported symptoms, which indicates problems with detection, documentation, or the absence of critical variables in the chart review. Data suggested that decedents without documented symptoms were more likely to be racial/ethnic minorities than veterans with reported symptoms. Given the meager data, it was unclear if this finding represented a true difference in symptoms between at-risk minority and majority patients in the VHA or a problem of underdetection of symptoms in minority patients. Although our analyses focused on VHA patients who received VHA services in the last year of life, approximately 10% of the veterans who killed themselves did not receive any VHA treatment services in their last year, and racial and ethnic minorities were also overrepresented in this group. Outreach efforts that are tailored to racial and ethnic minorities may be needed to increase their utilization of potentially lifesaving services.
Since these data were collected, the VHA has implemented reliable and sensitive screens for depression,27 alcohol misuse,28 and PTSD.29 The VHA has also mandated an annual suicide-risk assessment that is triggered when patients screen positive for psychiatric disorders or experience changes in treatment, such as hospitalization. Other changes include the mandated use of a standard Safety Plan with Veterans in those who are identified as being at high risk,30 and the creation of a list of high-risk veterans whose care is overseen by suicide prevention coordinators located at each VHA medical center. These strategies are designed to reduce the number of at-risk veterans whose symptoms go undetected (most relevant to the study group without documented symptoms) and to provide intensive and potentially lifesaving treatment to those with clear indications of risk (most relevant to the study group without recorded symptoms). How these VHA initiatives might have changed the results obtained in this study is unclear, and is an important topic for future study. Regardless of the VHA’s best efforts, it is inevitable that a subgroup of at-risk veterans will escape risk recognition efforts, and these patients (represented in the present study by those without documented symptoms) might benefit especially from universal prevention strategies aimed at general health promotion and safety.25
In our study, we used 2 strategies to minimize underdetection of psychopathology, first, by focusing on the year before death (rather than more distally) and, second, by coding psychiatric symptoms (rather than merely diagnoses). We identified a considerably higher percentage of suicides with psychopathology (68.5%) than that obtained in a recent cohort study of suicide among VHA patients (46.8%), which was extended more distally and relied on diagnoses,4 suggesting that we were successful to some degree. Documentation in clinical records reflects interactions between patients and providers, and we presume that the group without documented symptoms in the present study (31.5%) contained individuals who did not experience or reveal symptoms in the last year of life (nonsymptom expression) as well as those who were symptomatic, but there were failures in clinical detection or documentation (symptom nonidentification). Psychological autopsy studies estimated that nearly 90% of suicide decedents had 1 or more psychiatric disorders.23,24 Based on such data, it could be argued that the group without documented symptoms in the present study was overwhelmingly a case of nonidentification. However, it should be kept in mind that psychological autopsy studies focus on the last days and weeks of life, and there was a considerable time gap between the last appointment and the date of suicide in many patients in our study. As a result, a veteran’s mental status and life circumstances at their last treatment visit did not necessarily reflect their experience near to the time of suicide.
There were some limitations to this study. The study sample was limited to VHA patients treated in the Midwest and Northeast, with unclear generalizability to VHA patients in other regions of the country. Data were based on chart reviews, and information about the reliability, validity, or completeness of the information contained in the charts was not available. Moreover, we could not control for clinician variability in documentation. Providers might be more or less prone to document symptoms generally, which might have contributed to our finding that a broad range of symptoms were elevated in 1 of the study groups. As mentioned, there were numerous suicide prevention practices instituted in the VHA since the suicides studied here occurred, making it unclear how the results might look with a more recent sample. There were additional limitations concerning the availability of potentially important variables. Data on health care services received outside of VHA were unavailable, chart reviews did not provide exhaustive coverage for all potential risk factors such as personality disorders, and some groups were underrepresented in the sample (e.g., female veterans). Despite these limitations, the study identified 2 large and rather different at-risk groups of veterans, suggesting the need for a broad suicide prevention strategy that extends from universal (i.e., health and safety promotion) to indicated (i.e., risk recognition and treatment) approaches.
Acknowledgments
This study was funded by the Department of Veterans Affairs (VA), VISN 2 Center of Excellence for Suicide Prevention.
The authors would like to thank Heather Walters for training the coders, Liam Cerveny, Suzanne Dougherty, Sharon Fell, Elizabeth Schifano, and Patrick Walsh for conducting the chart reviews, and Brady Stephens for creating and managing the database.
Note. The VA had no role in study design; in the collection, analysis and interpretation of data; in the writing of the article; or in the decision to submit the article for publication.
Human Participant Protection
This study was approved by the Syracuse VA Medical Center Institutional Review Board.
References
- 1.Centers for Disease Control and Prevention Wisqars Injury Mortality Reports 1999-2006. 2009. Available at: http://www.cdc.gov.ezpminer.urmc.rochester.edu/ncipc/wisqars. Accessed September 25, 2009 [Google Scholar]
- 2.Blue Ribbon Report Group Report of the blue ribbon work group on suicide prevention in the Veteran population. 2008. Available at: http://www.mentalhealth.va.gov/suicide_prevention/Blue_Ribbon_Report-FINAL_June-30-08.pdf. Accessed January 5, 2010 [Google Scholar]
- 3.McCarthy JF, Valenstein M, Kim HM, Ilgen M, Zivin K, Blow FC. Suicide mortality among patients receiving care in the Veterans Health Administration health system. Am J Epidemiol. 2009;169(8):1033–1038 [DOI] [PubMed] [Google Scholar]
- 4.Ilgen MA, Bohnert AS, Ignacio RVet al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;67(11):1152–1158 [DOI] [PubMed] [Google Scholar]
- 5.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170(3):205–228 [DOI] [PubMed] [Google Scholar]
- 6.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Booth N, Owens C. Silent suicide: suicide among people not in contact with mental health services. Int Rev Psychiatry. 2000;12(1):27–30 [Google Scholar]
- 8.Law YW, Wong PW, Yip PS. Suicide with psychaitric diagnosis and without utilization of psychiatric services. BMC Public Health. 2010;10:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee HC, Lin HC, Liu TC, Lin SY. Contact of mental and non-mental healthcare providers prior to suicide in Taiwan: a population-based study. Can J Psychiatry. 2008;53(6):377–383 [DOI] [PubMed] [Google Scholar]
- 10.Sohn MW, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12(7):462–468 [DOI] [PubMed] [Google Scholar]
- 12.Valenstein M, Kim HM, Ganoczy Det al. Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. J Affect Disord. 2009;112(1-3):50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174 [PubMed] [Google Scholar]
- 14.Breslau N, Roth T, Rosenthal L, Andreski P, Sloane F. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411–418 [DOI] [PubMed] [Google Scholar]
- 15.Léger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63(1):49–55 [DOI] [PubMed] [Google Scholar]
- 16.Léger D, Guilleminault C, Bader G, Levy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25(6):625–629 [PubMed] [Google Scholar]
- 17.Ilgen MA, Zivin K, Austin KL, Bohnert AS, Czyz EK, Valenstein Met al. Severe pain predicts greater likelihood of subsequent suicide. Suicide Life Threat Behav. 2010;40:597–608 [DOI] [PubMed] [Google Scholar]
- 18.Cox DR. Regression models and life-tables. J R Stat Soc [Ser A]. 1972;B34(2):187–220 [Google Scholar]
- 19.Cleves MA, Gould WW, Gutierrez RG, Marchenko Y. An Introduction to Survival Analysis Using Stata. 2nd ed. College Station, TX: Stata Press; 2008 [Google Scholar]
- 20.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563–570 [DOI] [PubMed] [Google Scholar]
- 21.Koons CR, Robins CJ, Tweed JLet al. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behav Therapy. 2001;32(2):371–390 [Google Scholar]
- 22.Linehan MM, Comtois KA, Murray AMet al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–766 [DOI] [PubMed] [Google Scholar]
- 23.Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405 [DOI] [PubMed] [Google Scholar]
- 24.Yoshimasu K, Kiyohara C, Kazuhisa M. Suicidal risk factors and completed suicide: meta analyses based on psychological autopsy studies. Environ Health Prev Med. 2008;13(5):243–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health. 2004;94(1):37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828–833 [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two item-depression screener. Med Care. 2003;41(11):1284–1292 [DOI] [PubMed] [Google Scholar]
- 28.Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care. 2006;12(10):597–606 [PubMed] [Google Scholar]
- 29.Prins A, Ouimette P, Kimerling Ret al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry. 2003;9(1):9–14 [Google Scholar]
- 30.Stanley B, Brown GK. Safety planning: a brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice. Available online April 15, 2011. Available at: http://www.sciencedirect.com/science/journal/aip/10777229. Accessed January 5, 2010 [Google Scholar]