Abstract
Objectives. We sought to compare suicide rates among veterans utilizing Veterans Health Administration (VHA) services versus those who did not.
Methods. Suicide rates from 2005 to 2008 were estimated for veterans in the 16 states that fully participated in the National Violent Death Reporting System (NVDRS), using data from the National Death Index, NVDRS, and VHA records.
Results. Between 2005 and 2008, veteran suicide rates differed by age and VHA utilization status. Among men aged 30 years and older, suicide rates were consistently higher among VHA utilizers. However, among men younger than 30 years, rates declined significantly among VHA utilizers while increasing among nonutilizers. Over these years, an increasing proportion of male veterans younger than 30 years received VHA services, and these individuals had a rising prevalence of diagnosed mental health conditions.
Conclusions.The higher rates of suicide for utilizers of VHA among veteran men aged 30 and older were consistent with previous reports about which veterans utilize VHA services. The increasing rates of mental health conditions in utilizers younger than 30 years suggested that the decreasing relative rates in this group were related to the care provided, rather than to selective enrollment of those at lower risk for suicide.
Since the start of the wars in Afghanistan and Iraq, there has been increasing interest in suicide among American military veterans. This reflects a number of important issues. First, veterans constitute a sizeable population that has been identified as being at increased risk for suicide by some1,2 but not all,3 research studies. Second, there is increasing evidence that suicide may be a consequence of the stresses related to the experience of deployment and combat.4 Third, there have been concerns about the extent to which the Veterans Health Administration (VHA), the Department of Veterans Affairs (VA) health care system, has addressed the needs of veterans, especially those who have returned from service in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF), the wars in Afghanistan and Iraq.
Since the start of OEF and OIF, there have been a number of reports on rates and risk factors for death from suicide among all American veterans, independent of whether they have received VHA health care services,1–3,5–9 as well as a greater number of reports on those who utilize VHA services,10–22 and on mixed samples.23 Currently, the literature is not clear as to whether rates in veterans as a whole are higher than those for other Americans after controlling for demographic variables. However, there is evidence for increased rates in veterans utilizing VHA health care services. To date, there have been no reports of comparisons between veterans who utilize VHA services (utilizers) and those who do not (nonutilizers). This information is critical to advance a population-based approach to suicide prevention in veterans; to evaluate how the burden of suicide is distributed in the total veteran population; and to assess how completely VHA, the nation’s largest integrated health care system, addresses the needs of the population it was established to serve.
Comparisons between suicide rates among veterans who are VHA utilizers versus nonutilizers can also provide information on the impact of recent changes in the VHA and the patients it serves. Toward the end of 2005, VHA began to implement a mental health strategic plan based on recommendations from the President’s New Freedom Commission on Mental Health24 as well as recognition of the mental health needs of returning veterans. At the same time, VHA began to increase the budget for mental health services to support this strategy. As a result of these enhancements, systemwide VA mental health staffing increased 26.1%, from 13 667 at the start of 2005 to 17 234 at the end of 2008. Over this same period, the total number of veterans seen per year in VHA increased 3.6%, from 5.02 million in 2005 to 5.20 million in 2008; the number with diagnosed mental health conditions increased 15.0%, from 1.45 to 1.69 million; and the percentage of veteran patients with mental health conditions increased by 11.1%, from 28.9% to 32.1%.25
Veterans returning from OEF and OIF are all eligible for VHA services during the first 5 years after they return from deployment without additional requirements. For veterans who served in previous eras, VHA eligibility is determined by factors such as service-connected health conditions, disability, age, and income.26 The differences in eligibility requirements, as well as differences in the recency of deployment and the acuity of deployment-related conditions, suggest the importance of testing for differences between age groups both when comparing suicide rates in veterans who are VHA utilizers versus nonutilizers and when evaluating changes in rates over time.
For our study, we compared rates of suicide and assessed changes over time among veterans who utilized VHA health care services and those who did not, by gender, age group, and year. Given greater morbidity among those veterans who received VHA services, we hypothesized that suicide rates were higher among veterans who were VHA utilizers than those who were nonutilizers. Given the magnitude of VHA mental health enhancements, we hypothesized that rates among VHA utilizers would decrease over time. Finally, given greater acuity of mental health problems in OEF and OIF veterans, we hypothesized that among VHA utilizers decreases in rates would be greater among younger than older veterans.
METHODS
Suicide rates for veterans using VHA health services and for other veterans were estimated using VHA administrative data, vital status, and cause of death records from the National Center for Health Statistics’ National Death Index (NDI),27 and state-level information on suicides among veterans, by gender and age, from the Center for Disease Control and Prevention’s National Violent Death Reporting System (NVDRS).28 Clinical information from the VHA’s electronic health records was not utilized because it was not available for those who did not utilize VHA services.
Suicide rates, expressed as suicide deaths per 100 000 person-years, were estimated for veterans in the 16 states that fully participated in NVDRS from 2005 to 2008 (Alaska, Colorado, Georgia, Kentucky, Maryland, Massachusetts, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, Rhode Island, South Carolina, Utah, Virginia, and Wisconsin).
Suicide mortality among individuals receiving VHA services was estimated using VHA administrative data included in the National Patient Care Database and NDI data using previously described methods.19,21 Briefly, we identified all patients with VHA inpatient or outpatient encounters from 2005 to 2008 who had no VHA encounters in subsequent years, and we queried the NDI to determine these individuals’ vital status, and, for those who died, their cause of death. To estimate state-level suicide rates, VHA users who died from suicide were assigned to specific states based on the location of the VHA medical center where they last received services. Rates among VHA users were estimated for each year, sex, and age group (18–29, 30–64, and 65 years and older), using the total number of suicides among those who received VHA services in the 16 NVDRS states, divided by the total number of veterans receiving care from VHA medical centers in those states.
The NVDRS provided information on the total number of suicide deaths among veterans, independent of whether they received VHA services, by year, sex, and age category for each of the 16 states from 2005 to 2008 based on the methods detailed in their coding manual.29 NVDRS data included information on each decedent’s veteran status, which was used in previous studies.2,8,9 This was assessed from an indicator of whether the decedent ever served in the US Armed Forces, which was derived from the standardized death certificates in the NVDRS states and is included in a section that is usually completed by funeral directors on the basis of all of the information and reports available to them.30,31 For each year, gender, and age group, suicide rates among all veterans in the NVDRS states were estimated from the total number of veteran suicides identified by NVDRS divided by the total number of veterans in those states. Data on the size of the total veteran population, and for veterans who were VHA utilizers versus nonutilizers, were derived from the Veteran Population (VetPop) 2007 file32 maintained by the VA.
The nature of the data use agreements between NVDRS and the states precluded disclosure of identifying information on decedents. Consequently, suicide rates for nonutilizers were estimated indirectly, using the relevant numerators and denominators for the 16 states. The numerators were estimated from the total number of veterans identified as having died from suicide in NVDRS data for the 16 states minus the number of suicide deaths among VHA utilizers in these states. Denominators were estimated by subtracting the number of individuals served by VA facilities in the NVDRS states from the total number of veterans in those states as indicated from the VetPop 2007 data.
Statistical analyses were conducted using Predictive Analytics SoftWare Statistics 18 (SPSS Statistics, Hong Kong). Comparisons of suicide rates were conducted using the generalized linear modeling command, with Poisson log linear modeling for counts.
RESULTS
Suicide counts, populations, and rates in the 16 states for 2005–2008, overall and by VHA user status, are presented in Table 1 for veteran women and in Table 2 for veteran men. These provided information by year for veterans in the 16 states, overall and by age category.
TABLE 1—
Suicide Counts, At Risk Populations, and Suicide Rates Among Veteran Women, Overall and by Veterans Health Administration User Status: 16 National Violent Death Reporting System States, 2005–2008
| Ages, y | All Veteran Women |
VA Utilizer Women |
VA Nonutilizer Women |
||||||
| Suicides, No. | Population, No. | Suicide Rate | Suicides, No. | Population, No. | Suicide Rate | Suicides, No. | Population, No. | Suicide Rate | |
| 2005 | |||||||||
| All | 50 | 527 208 | 9.48 | 9 | 110 904 | 8.12a | 41 | 416 304 | 9.85 |
| 18–29 | 10 | 59 507 | 16.81a | 0 | 16 102 | 0.00a | 10 | 43 405 | 23.04a |
| 30–64 | 36 | 387 007 | 9.30 | 8 | 82 765 | 9.67a | 28 | 304 242 | 9.20 |
| ≥ 65 | 4 | 80 694 | 4.96a | 1 | 12 036 | 8.31a | 3 | 68 658 | 4.37a |
| 2006 | |||||||||
| All | 65 | 536 668 | 12.11 | 16 | 114 654 | 13.96a | 49 | 422 014 | 11.61 |
| 18–29 | 9 | 59 280 | 15.18a | 2 | 16 931 | 11.81a | 7 | 42 349 | 16.53a |
| 30–64 | 53 | 396 950 | 13.35 | 13 | 85 751 | 15.16a | 40 | 311 199 | 12.85 |
| ≥ 65 | 3 | 80 438 | 3.73a | 1 | 11 972 | 8.35a | 2 | 68 466 | 2.92a |
| 2007 | |||||||||
| All | 72 | 545 600 | 13.20 | 21 | 119 327 | 17.60 | 51 | 426 521 | 11.96 |
| 18–29 | 9 | 58 791 | 15.31a | 2 | 17 269 | 11.58a | 7 | 41 769 | 16.76a |
| 30–64 | 60 | 407 003 | 14.74 | 19 | 90 338 | 21.03a | 41 | 316 665 | 12.95 |
| ≥ 65 | 3 | 79 806 | 3.76a | 0 | 11 720 | 0.00a | 3 | 68 086 | 4.41a |
| 2008 | |||||||||
| All | 55 | 517 566 | 10.63 | 18 | 118 812 | 15.15a | 37 | 398 754 | 9.28a |
| 18–29 | 9 | 58 614 | 15.35a | 4 | 15 988 | 25.02a | 5 | 42 626 | 11.73a |
| 30–64 | 43 | 376875 | 11.41 | 14 | 88 531 | 15.81a | 29 | 288 344 | 10.06 |
| ≥ 65 | 3 | 82 077 | 3.66a | 0 | 14 293 | 0.00a | 3 | 67 784 | 4.43a |
Rates based on small sample sizes must be interpreted with caution, as they are sensitive to small differences in counts.
TABLE 2—
Suicide Counts, at Risk Populations, and Suicide Rates Among Veteran Men, Overall and by Veteran Health Administration User Status: 16 National Violent Death Reporting System States, 2005–2008
| Ages, y | All Veteran Men |
VA Utilizer Men |
VA non-Utilizer Men |
||||||
| Suicides, No. | Population, No. | Suicide Rate | Suicides, No. | Population, No. | Suicide Rate | Suicides, No. | Population, No. | Suicide Rate | |
| 2005 | |||||||||
| All | 1767 | 6 193 444 | 28.53 | 423 | 1151 260 | 36.74 | 1344 | 5 042 184 | 26.66 |
| 18–29 | 100 | 222 255 | 44.99 | 17 | 31 966 | 53.18a | 83 | 190 289 | 43.62 |
| 30–64 | 931 | 3 636 370 | 25.60 | 217 | 594 346 | 36.51 | 714 | 3 042 024 | 23.47 |
| ≥ 65 | 736 | 2 334 819 | 31.52 | 189 | 524 948 | 36.00 | 547 | 1 809 871 | 30.22 |
| 2006 | |||||||||
| All | 1600 | 6 118 208 | 26.15 | 396 | 1 049 666 | 37.73 | 1204 | 5 068 542 | 23.75 |
| 18–29 | 104 | 229 848 | 45.25 | 15 | 33 827 | 44.34a | 89 | 196 021 | 45.40 |
| 30–64 | 900 | 3 575 049 | 25.17 | 219 | 548 316 | 39.94 | 681 | 3 026 733 | 22.50 |
| ≥ 65 | 596 | 2 313 311 | 25.76 | 162 | 467 523 | 34.65 | 434 | 1 845 788 | 23.51 |
| 2007 | |||||||||
| All | 1787 | 6 052 918 | 29.52 | 391 | 1 072 818 | 36.45 | 1396 | 4 980 100 | 28.03 |
| 18–29 | 137 | 241 339 | 56.77 | 18 | 38 544 | 46.70a | 119 | 202 795 | 58.68 |
| 30–64 | 965 | 3 490 677 | 27.65 | 216 | 563 769 | 38.31 | 749 | 2 926 908 | 25.59 |
| ≥ 65 | 685 | 2 320 902 | 29.51 | 157 | 470 504 | 33.37 | 528 | 1 850 398 | 28.53 |
| 2008 | |||||||||
| All | 1843 | 5 982 534 | 30.81 | 435 | 1 085 111 | 40.09 | 1408 | 4 897 423 | 28.75 |
| 18–29 | 144 | 250 070 | 57.58 | 14 | 42 113 | 33.24a | 130 | 207 957 | 62.51 |
| 30–64 | 992 | 3 406 930 | 29.12 | 248 | 575 991 | 43.06 | 744 | 2 830 939 | 26.28 |
| ≥ 65 | 707 | 2 325 534 | 30.40 | 173 | 467 007 | 37.04 | 534 | 185 8527 | 28.73 |
Rates based on small sample sizes must be interpreted with caution, as they are sensitive to small differences in counts.
Among all veteran women in the 16 states, approximately 21.8% utilized VHA services: 28.1% of veteran women younger than 30 years, 22.2% of those aged 30 to 64 years, and 15.5% of those 65 years and older. There were no significant changes in suicide rates between 2005 and 2008. Suicide rates for veteran women were lower than those observed for men, overall, for each of the age categories and among both VHA utilizers and nonutilizers. The relatively low numbers of suicides among women in these states precluded meaningful comparisons between rates in utilizers and nonutilizers across the years.
For veteran men in the 16 states, approximately 17.9% utilized VHA services: 15.5% of those younger than 30 years, 16.2% of those aged 30–64 years, and 20.8% of those 65 years and older. The proportion of veterans younger than 30 years who utilized VHA health care increased significantly from 14.3% in 2005 to 16.8% in 2008 (average of 0.87% per year). There were no significant changes over time for those aged 30–64 years or for those aged 65 years and older.
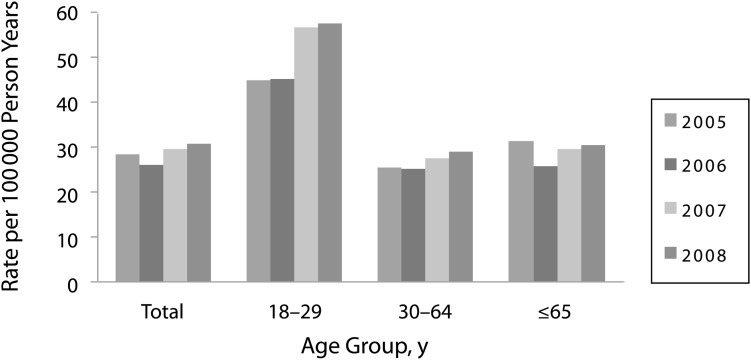
Further, among all veteran men, for those aged 30–64 years and those aged 65 years and older, there were no significant changes in suicide rates over time (Figure 1). For each of these groups, suicide rates for utilizers were consistently higher than for nonutilizers (Figure 2).
FIGURE 1—
Suicide rates among veteran men, by year and age group: 16 National Violent Death Reporting System states, 2005–2008
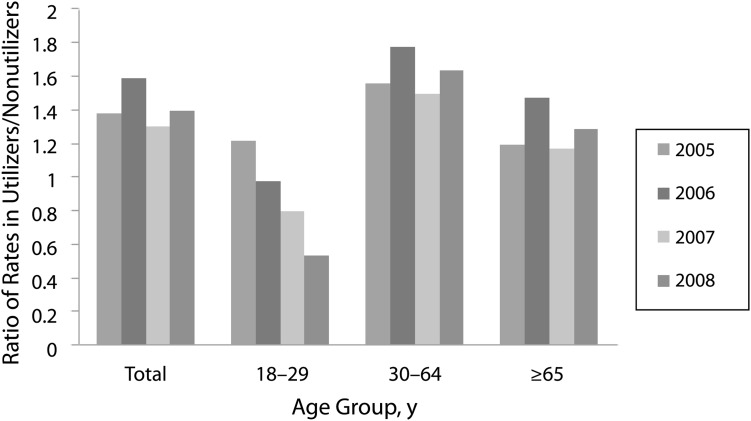
FIGURE 2—
Ratio of suicide rates among veteran men utilizing Veterans Affairs health care services and among nonutilizers, by year and age group: 16 National Violent Death Reporting System states, 2005–2008
However, for all men younger than 30 years, suicide rates increased from 2005 to 2008 (Poisson log linear model; Wald χ21 = 5.559; P = .018), with significant increases among nonutilizers (Wald χ21 = 9.204; P = .002) but no significant increases among utilizers (Table 2; Figure 1). When models considered both differences between years and between VHA utilizers versus nonutilizers, the interaction term was significant (Wald χ21 = 4.949; P = .026), reflecting decreasing suicide rates in utilizers compared with nonutilizers over time (Figure 2). In 2005, rates were 21.9% higher in young male utilizers than in nonutilizers; by 2008, rates among young male utilizers were 46.8% lower (Figure 2).
A number of the findings reported here identified veteran men younger than age 30 as an important subgroup. Men younger than age 30 as a proportion of the total number of men in the 16 states receiving VA health care services increased from 2.8% in 2005 to 3.2% in 2006, to 3.6% in 2007, and to 3.9% in 2008 (Table 2). During this period, there were also substantial increases (> 50%) in the proportion of these young men who served in Afghanistan or Iraq, and in those diagnosed with a substance use disorder, depression, posttraumatic stress disorder (PTSD), another anxiety disorder, or any mental health condition. There were marginal increases in the proportion with diagnoses of bipolar disorder and decreases in the proportion with diagnoses of schizophrenia (Table 3).
TABLE 3—
OEF/OIF Status and Clinical Characteristics of Veteran Men Younger Than 30 Years Utilizing the Veterans Health Administration: 16 National Violent Death Reporting System States, 2005–2008
| 2005, % | 2006, % | 2007, % | 2008, % | |
| OEF/OIF | 3.60 | 47.61 | 57.57 | 63.75 |
| SUD | 5.28 | 6.33 | 8.18 | 10.36 |
| Depression | 11.28 | 12.70 | 15.30 | 18.23 |
| PTSD | 7.93 | 11.50 | 16.65 | 21.68 |
| Other anxiety | 5.17 | 6.08 | 7.93 | 9.71 |
| Bipolar | 1.95 | 2.00 | 2.19 | 2.37 |
| Schizophrenia | 1.27 | 1.23 | 1.16 | 1.08 |
| Any MH condition | 23.16 | 27.04 | 33.53 | 39.42 |
Note. MH = mental health; OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; PTSD = posttraumatic stress disorder; SUD = substance use disorder.
DISCUSSION
The findings reported here are important for 2 reasons. First, they demonstrated the feasibility and utility of linking information from NVDRS, NDI, and VHA sources to compare outcomes in veterans who utilized VHA healthcare services and those who did not. Second, they constituted the first reported comparison of suicide rates between veteran utilizers and nonutilizers.
The findings presented here demonstrated that for veteran men overall, for those aged 30–64 years, and for those 65 years and older, suicide rates among VHA utilizers were persistently higher than for nonutilizers. Other findings demonstrated important trends among veteran men younger than 30 years. The number of these veterans and the proportion of them using VHA services increased from 2005–2008. Suicide rates increased in the overall population of young veteran men in parallel with the rates in VHA service nonutilizers, as opposed to nonsignificant changes in VHA service utilizers. Most significantly, from 2005–2008, there were dramatic decreases in suicide rates in young male VHA utilizers relative to nonutilizers. We noted that in the general US population in the 16 states, the Web-based Injury Statistics Query and Reporting System/NVDRS web site indicated that suicide rates in 2008 were 19.4 per 100 000 among men age 18 to 29 years, and 25.1 and 28.3 among men age 30–64 and 65 years and older, respectively. Finally, findings were consistent with previous reports that suicide rates were higher for men than for women, both in veteran and nonveteran populations.19,33 Given the lower prevalence of suicide in women and the relatively low proportion of veterans who were women, it was not feasible to compare rates among veteran women by VHA utilization status in the 16 NVDRS states. Consequently, this discussion focused on findings among veteran men.
The results for all veteran men, for those aged 30–64 years and for those aged 65 years and older, were consistent with reported comparisons of suicide rates between VHA utilizers and age- and gender-matched individuals in the general population.19 As discussed previously,19 these findings might be related to selection of those who were more likely to be mentally ill, chronically ill, disabled, and economically disadvantaged by the eligibility criteria for enrollment in VHA.26 Several lines of investigation supported selective use of VHA services by those with risk factors for suicide. Research conducted before the first Gulf War demonstrated that high illness levels and service connected disability were associated with use of VA health care services.34 Research between the first Gulf War and OEF/OIF demonstrated that veterans who were unemployed and with greater levels of disability were more likely to use VA relative to non-VA outpatient health care services.35 Findings from the first years of OEF and OIF demonstrated that the proportion of enrollees with serious mental illness in VHA was greater than that in private insurance plans or the Military Treatment System, and comparable to the proportion among Medicaid recipients; the proportion of those with depression was greater in the VA than any of the other coverage systems.36 Finally, findings that PTSD predicted use of VHA services among Vietnam-era veterans37 were consistent with recent unpublished findings that PTSD and other mental health conditions predicted VHA use among OEF and OIF veterans. The findings reported here were consistent with the hypothesis that suicide rates were higher among veterans who received VHA services than among those who did not receive VHA services. The results did not, however, confirm the hypothesis that mental health enhancements led to decreases over time in suicide rates. We noted that VHA mental health enhancements continued beyond 2008, and further monitoring is needed to determine whether these enhancements led to decreases in suicide rates.
Our findings demonstrate important trends among veteran men younger than 30 years. First, suicide rates increased between 2005 and 2008 in the total population of young veteran men in the 16 states included in NVDRS. Although the mechanisms underlying this increase remain to be determined, it is important to note that this effect appeared to parallel the increases observed among active duty service members.38,39 Second, as hypothesized, rates among young utilizers decreased relative to those among nonutilizers. In principle, this effect could occur for either of 2 reasons. First, it could result from selection factors, if over time, the young men who came to VHA for services were increasingly at lower risk for suicide. Alternatively, the relative decline among VHA utilizers could occur as a result of enhancements in access to effective treatments or if VHA services became more effective at preventing suicide. Given that mental health conditions are major risk factors for suicide,21 the increasing prevalence of mental health conditions in male VHA utilizers younger than 30 years (Table 3) appeared inconsistent with the possibility that the relative decreases in suicide rates in the young men served by VHA could be because of the enrollment of patients at lower risk. Accordingly, it was likely that the observed decreases in suicide rates for young male utilizers were because of enhancements in the effectiveness of VHA services. The findings presented in Figure 2 could be explained by assuming that young veteran men represented a group for whom the outcomes of care were most sensitive to these enhancements, possibly as a reflection of the acuity of their mental health conditions.
There were multiple potential limitations involved with the data sources and the necessary assumptions for completing these analyses. Of course, study findings might not be generalizable to the entire United States or the entire VHA health care system, to the extent that the 16 NVDRS states were not representative of the nation or the VHA health system, for example, with respect to the geographic distribution of veterans and patterns of VHA utilization. Also, there were constraints related to measurement. Most concerning was the possibility that the NVDRS indicators of veterans status were derived from responses regarding whether decedents had ever served in the US Armed Forces. In some cases, positive responses might have included nonveterans (e.g., active duty personnel, National Guard members who were never activated or deployed), and negative responses might have failed to identify veterans (e.g., those with previous service in the Coast Guard or Public Health Services; veteran decedents whose survivors were unaware of their veteran status). This raised important concerns regarding study findings, as secular trends in suicide mortality among activity duty personnel could affect the assessment of trends in suicide mortality among veterans who did not utilize VHA services. Certainly further research is needed to address this concern. Finally, we noted 3 other sources of potential measurement error. First, the source of veteran population counts was based on census data, information from the Department of Defense, and updates estimated using actuarial methods. Given the recent increases in the number of veterans returning from Afghanistan and Iraq, there might have been greater imprecision in the veteran population estimates, particularly for younger veterans. Second, because it was not possible to directly match individuals who were counted as veteran suicides by NVDRS with the VHA data, the calculation of rates among veteran nonutilizers was perforce estimated; rates for utilizers and nonutilizers were calculated for the 16 states from the number of individuals identified by VHA as utilizers in these states and, for nonutilizers, by the total number counted by NVDRS minus the number identified by VHA. Third, although the NVDRS attributed individuals to states based on the location of their deaths, the VHA attributed veterans to states based on the location of the facility where they last received VHA services. Consequently, the different processes might have resulted in mismatches and noise or bias in the findings.
Mindful of these concerns, we noted that this study applied existing data to investigate pressing public health and health policy questions. Study findings offered new perspectives regarding suicide among veterans and differences in suicide rates between VHA utilizers and nonutilizers. The most significant findings might be the consistently higher rate of suicide among VHA utilizers aged 30–64 years and those 65 years and older and, among veterans younger than 30 years, the observed decreasing rates in VHA utilizers relative to nonutilizers between 2005 and 2008. Although definitive explanations for these findings will require additional research, the available evidence suggested that the increased rates in men aged 30–64 years and in elder populations might be because of the selective use of VHA services by individuals at increased risk, whereas among veterans younger than 30 years, the decreasing rates in VHA utilizers relative to nonutilizers might result from the ongoing enhancements in VHA mental health services.
Acknowledgments
This study was funded by the VA Office of Mental Health Services.
Human Participants Protection
This study was approved by the Ann Arbor VA Medical Center Institutional Review Board.
References
- 1.Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: a prospective population-based study. J Epidemiol Community Health. 2007;61:619–624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McFarland BH, Kaplan MS, Huguet N. Datapoints: self-inflicted deaths among women with U.S. military service: a hidden epidemic? Psychiatr Serv. 2010;61:1177. [DOI] [PubMed] [Google Scholar]
- 3.Miller M, Barber C, Azrael D, Calle EE, Lawler E, Mukamal KJ. Suicide among US veterans: a prospective study of 500,000 middle-aged and elderly men. Am J Epidemiol. 2009;170:494–500 [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine Deployment-Related Stress and Health Outcomes. Vol 6 Washington, DC: National Academy Press; 2007 [Google Scholar]
- 5.Boscarino JA. External-cause mortality after psychologic trauma: the effects of stress exposure and predisposition. Compr Psychiatry. 2006;47:503–514 [DOI] [PubMed] [Google Scholar]
- 6.Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300:652–653 [DOI] [PubMed] [Google Scholar]
- 7.Maynard C, Boyko EJ. Datapoints: suicide rates in the Washington State veteran population. Psychiatr Serv. 2008;59:1245. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan MS, McFarland BH, Huguet N. Characteristics of adult male and female firearm suicide decedents: findings from the National Violent Death Reporting System. Inj Prev. 2009;15:322–327 [DOI] [PubMed] [Google Scholar]
- 9.Kaplan MS, McFarland BH, Huguet N. Firearm suicide among veterans in the general population: findings from the National Violent Death Reporting System. J Trauma. 2009;67:503–507 [DOI] [PubMed] [Google Scholar]
- 10.Kausch O, McCormick RA. Suicide prevalence in chemical dependency programs: preliminary data from a national sample, and an examination of risk factors. J Subst Abuse Treat. 2002;22:97–102 [DOI] [PubMed] [Google Scholar]
- 11.Thompson R, Kane VR, Sayers SL, Brown GK, Coyne JC, Katz IR. An assessment of suicide in an urban VA Medical Center. Psychiatry. 2002;65:327–337 [DOI] [PubMed] [Google Scholar]
- 12.Thompson R, Katz IR, Kane VR, Sayers SL. Cause of death in veterans receiving general medical and mental health care. J Nerv Ment Dis. 2002;190:789–792 [DOI] [PubMed] [Google Scholar]
- 13.Desai RA, Dausey DJ, Rosenheck RA. Mental health service delivery and suicide risk: the role of individual patient and facility factors. Am J Psychiatry. 2005;162:311–318 [DOI] [PubMed] [Google Scholar]
- 14.Zivin K, Kim HM, McCarthy JFet al. Suicide mortality among individuals receiving treatment for depression in the Veterans Affairs health system: associations with patient and treatment setting characteristics. Am J Public Health. 2007;97:2193–2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai RA, Dausey D, Rosenheck RA. Suicide among discharged psychiatric inpatients in the Department of Veterans Affairs. Mil Med. 2008;173:721–728 [DOI] [PubMed] [Google Scholar]
- 16.Mills PD, DeRosier JM, Ballot BA, Shepherd M, Bagian JP. Inpatient suicide and suicide attempts in Veterans Affairs hospitals. Jt Comm J Qual Patient Saf. 2008;34:482–488 [DOI] [PubMed] [Google Scholar]
- 17.Desai MM, Rosenheck RA, Desai RA. Time trends and predictors of suicide among mental health outpatients in the Department of Veterans Affairs. J Behav Health Serv Res. 2008;35:115–124 [DOI] [PubMed] [Google Scholar]
- 18.Ilgen MA, Downing K, Zivin Ket al. Exploratory data mining analysis identifying subgroups of patients with depression who are at high risk for suicide. J Clin Psychiatry. 2009;70:1495–1500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCarthy JF, Valenstein M, Kim HM, Ilgen M, Zivin K, Blow FC. Suicide mortality among patients receiving care in the Veterans Health Administration health system. Am J Epidemiol. 2009;169:1033–1038 [DOI] [PubMed] [Google Scholar]
- 20.Pfeiffer PN, Ganoczy D, Ilgen M, Zivin K, Valenstein M. Comorbid anxiety as a suicide risk factor among depressed veterans. Depress Anxiety. 2009;26:752–757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ilgen MA, Bohnert AS, Ignacio RVet al. Psychiatric diagnoses and risk of suicide in veterans. Arch Gen Psychiatry. 2010;67:1152–1158 [DOI] [PubMed] [Google Scholar]
- 22.llgen, MA, Zivin K, Austin KLet al. Severe pain predicts greater likelihood of subsequent suicide. Suicide Life Threat Behav. 2010;40:597–608 [DOI] [PubMed] [Google Scholar]
- 23.Flood AM, Boyle SH, Calhoun PSet al. Prospective study of externalizing and internalizing subtypes of posttraumatic stress disorder and their relationship to mortality among Vietnam veterans. Compr Psychiatry. 2010;51:236–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The President’s New Freedom Commission on Mental Health Achieving the Promise. Transforming Mental Health Care in America. Final Report. 2003. Available at: http://store.samhsa.gov/product/SMA03-3831. Accessed January 20, 2012 [Google Scholar]
- 25.Department of Veterans Affairs Administrative Data. Washington, DC: Department of Veterans Affairs; 2011 [Google Scholar]
- 26.Veterans Health Administration Enrollment Priority Groups. Available at: http://www.va.gov/healthbenefits/resources/priority_groups.asp. Accessed January 10, 2012
- 27.Centers for Disease Control and Prevention, National Center for Health Statistics. National Death Index. . Available at: http://www.cdc.gov/nchs/data_access/ndi/about_ndi.htm. Accessed January 10, 2012.
- 28.Centers for Disease Control and Prevention National Violent Death Reporting System. Available at: http://www.cdc.gov/ViolencePrevention/NVDRS/index.html. Accessed January 10, 2012
- 29.National Center for Injury Prevention, Control, Centers for Disease Control and Prevention National Violent Death Reporting System Coding Manual Version 3. 2008. Available at: http://www.cdc.gov/violenceprevention/NVDRS/coding_manual.html. Accessed January 10, 2012 [Google Scholar]
- 30.National Center for Health Statistics, Centers for Disease Control and Prevention Medical Examiners’ and Coroners’ Handbook on Death registration and Fetal Death Reporting (2003 Revision). Available at: http://www.cdc.gov/nchs/data/misc/hb_me.pdf. Accessed January 10, 2012
- 31.National Center for Health Statistics, Centers for Disease Control and Prevention. Funeral Directors’ Handbook on Death Registration and Fetal Death Reporting (2003 Revision). Availableat: http://www.cdc.gov/nchs/data/misc/hb_fun.pdf. Accessed January 10, 2012
- 32.Department of Veterans Affairs VetPop 2007. Available at: http://www.va.gov/VETDATA/Demographics/Demographics.asp. Accessed January 10, 2012
- 33.Centers for Disease Control and Prevention National Suicide Statistics at a Glance. Available at: http://www.cdc.gov/violenceprevention/suicide/statistics/aag.html. Accessed January 10, 2012
- 34.Rosenheck R, Massari L. Wartime military service and utilization of VA health care services. Mil Med. 1993;158:223–228 [PubMed] [Google Scholar]
- 35.Elhai JD, Grubaugh AL, Richardson JD, Egede LE, Creamer M. Outpatient medical and mental healthcare utilization models among military veterans: results from the 2001 National Survey of Veterans. J Psychiatr Res. 2008;42:858–867 [DOI] [PubMed] [Google Scholar]
- 36.Gibson TB, Lee TA, Vogeli CSet al. A four-system comparison of patients with chronic illness: The Military Health System, Veterans Health Administration, Medicaid, and Commercial Plans. Mil Med. 2009;174:936–943 [DOI] [PubMed] [Google Scholar]
- 37.Rosenheck R, Fontana A. Do Vietnam-era veterans who suffer from posttraumatic stress disorder avoid VA mental health services? Mil Med. 1995;160:136–142 [PubMed] [Google Scholar]
- 38.United States Army Army Health Promotion, Risk reduction, and Suicide Prevention Report. 2010. Available at: http://www.army.mil/article/42934. Accessed January 10, 2012 [Google Scholar]
- 39.Department of Defense Task Force on the Prevention of Suicide by Members of the Armed Forces Executive Summary. 2010. Available at: http://www.health.mil/dhb/downloads/TaskForce2010/Suicide%20Prevention%20Task%20Force_EXEC%20SUM_08-20-10%20v6.doc. Accessed January 10, 2012 [Google Scholar]