Abstract
Objectives. We sought to examine rates of suicide among individuals receiving health care services in Veterans Health Administration (VHA) facilities over an 8-year period.
Methods. We included annual cohorts of all individuals who received VHA health care services from fiscal year (FY) 2000 through FY 2007 (October 1, 1999–September 30, 2007; N = 8 855 655). Vital status and cause of death were obtained from the National Death Index.
Results. Suicide was more common among VHA patients than members of the general US population. The overall rates of suicide among VHA patients decreased slightly but significantly from 2000 to 2007 (P < .001). Male veterans between the ages of 30 and 64 years were at the highest risk of suicide.
Conclusions. VHA health care system patients are at elevated risk for suicide and are appropriate for suicide reduction services, although the rate of suicide has decreased in recent years for this group. Comprehensive approaches to suicide prevention in the VHA focus not only on recent returnees from Iraq and Afghanistan but also on middle-aged and older Veterans.
Reducing suicide within the United States is a national priority.1,2 Over 30 000 individuals in the US die by suicide every year, with an annual age-adjusted rate of approximately 11 suicides per 100 000 persons.3 Recent public and policy attention has focused on suicide among veterans generally and among individuals receiving services from the Veterans Health Administration (VHA). VHA patients are more likely to have characteristics related to higher risk of suicide, including older age, male gender, and substantial medical and psychiatric morbidities.4,5 Recent studies provide inconsistent information regarding the relative risk of suicide in veterans. Kaplan et al.6 found that male veterans who responded to the US National Health Interview Survey were twice as likely to report a suicide attempt as nonveteran males. Additionally, McCarthy et al.7 found that, compared with rates for the general US population, suicide rates of VHA users in 2000 to 2001 were 1.66 times higher in men and 1.87 times higher in women. By contrast, other studies of specific cohorts of Veterans have failed to find that the risk of suicide is substantially higher than that found in the general population, except within specific high-risk subgroups (e.g. veterans with a mental disorder).8–14 Similarly, a recent large-scale study of older men found that Veteran status did not significantly increase suicide risk.15
Research regarding changes over time in suicidal behaviors is also limited. Kessler et al.16 found that rates of nonfatal suicide attempts did not change over nearly 2 decades. In the general US population, suicide rates increased 2%–3% from 1999 through 2005.17 However, changes in suicidal behaviors observed in the general population may not apply to Veterans generally and to high-risk individuals receiving VHA services in particular, who may be more accessible for suicide prevention efforts.
Monitoring suicide rates among Veterans is also important because of concerns regarding the impact of the conflicts in Iraq (Operation Iraqi Freedom [OIF]) and Afghanistan (Operation Enduring Freedom [OEF]). OEF/OIF Veterans have elevated rates of psychiatric and substance use disorders,18–21 and Congress has mandated implementation of a comprehensive VHA suicide prevention program, which began in 2007.22 However, a 2008 report observed that suicide rates among OEF/OIF Veterans were not greater than those among the general population.13 Better data are needed to examine whether suicide rates among VHA patients have changed since the start of the wars in Iraq and Afghanistan, as well as to assess the general stability of rates among patients receiving health care in the VHA, which is the largest integrated health system in the United States. Data on trends in suicide rates among VHA patients also would provide a baseline for assessing the potential impact of initiatives designed to reduce suicide risk.
Our study documents potential changes in the rates of suicide among all male and female users of VHA services between fiscal years (FYs) 2000 and 2007. Yearly rates of suicide in Veterans seeking treatment at the VHA were also compared with rates of suicide within the general US population over this time period, both overall and within demographic subgroups defined by age and gender. Based on prior research of Veterans receiving VHA services,7 we hypothesized that the rate of suicide would be elevated among VHA patients compared with the general population.
METHODS
For our study, we included all patients who utilized VHA services between Fiscal Years 2000 and 2007 (FY00 and FY07). Fiscal years begin on October 1st of the prior calendar year and continue through September 30th of the calendar year (e.g., FY00 includes October 1, 1999 to September 30, 2000). A total of 8 855 655 individuals received inpatient or outpatient VHA services between FY00 and FY07. Of those, 101 959 individuals (1.2%) were excluded because of invalid or missing data or non-US residences. The Veterans Affairs (VA) Ann Arbor institutional review board approved this project. Annual demographic information on the VHA user population is available in Appendix 1 (available as a supplement to the online version of this article at http:www.ajph.org).
Data Sources
Data came from the VA's National Patient Care Database (NPCD) and the Centers for Disease Control and Prevention's (CDC's) National Death Index (NDI). NPCD records all VHA inpatient or outpatient visits. NDI data identified vital status and cause of death and were acquired for VA program planning. NDI searches were conducted for all individuals with VHA use between FY00 and FY07 and who did not receive VHA services during FY08, thereby obviating costly searches for individuals whose VHA use post-FY07 indicated survival through the end of FY07. The NDI compiles death records from state vital statistics offices, and it has the greatest sensitivity in determining vital status among population-level sources.23 Established procedures identified “true” matches when the search resulted in multiple potential matches.24
The CDC's Web-based Injury Statistics Query and Reporting System (WISQARS)25 was used to compare VHA suicide rates to those of the general population. WISQARS provides suicide rates by age and gender in the US population.
Measures
Age categories included those aged 18 to 29 years, 30 to 64 years, and 65 years and older; these were chosen to represent young, middle, and older adulthood, respectively, and because suicide rates are relatively stable within each of these groups. Because information regarding race/ethnicity was not consistently available in the NPCD, race/ethnicity was not included in analyses. Suicide deaths were identified using International Classification of Diseases, Tenth Revision, codes X60–X84, Y87.0, and U03.26
For each annual cohort, patients were included if they received VHA services in either that year or the prior fiscal year and were alive at the start of that year. For example, an individual who used VHA services in FY00 and survived all of FY01 contributed one year of risk time for suicide in FY01. If an individual did not use VHA services in FY00 but did in FY01 and was alive at the end of FY01, the individual was considered to have entered the cohort of VHA patients half way through the year (on average) and contributed half of a person-year toward the suicide rate for FY01. If an individual met criteria to be defined as part of the cohort of VHA patients for a given fiscal year as already defined died in that fiscal year from any cause, their contribution toward the person-years calculation for that fiscal year was also half a year.
Analyses
We calculated annual rates of suicide by dividing the number of suicides observed in each fiscal year by the person-years accrued during that period, multiplied by 100 000. We calculated confidence intervals with the Poisson method for all rates.27
To compare VHA rates to those of the general population, we calculated Standardized Mortality Ratios (SMRs) for age and gender subgroups for each year, using the WISQARS data as the reference group.28 Data from WISQARS were categorized by calendar year and rates of suicide for the VHA are organized by fiscal year. Although this was not an exact temporal match, SMRs were calculated for time periods with a 9-month overlap for each 12-month period. We used indirect standardization29 which uses age-specific mortality rates from the standard US population to derive expected deaths in the VA user population. We calculated 95% confidence intervals for the SMRs using an exact method based on the Poisson distribution,27 and the rate among the VHA population was considered significantly higher than that among the general population when the confidence interval did not include zero. We further tested changes over time in the rate of suicide between FY00 and FY07 by creating Poisson regression models. Poisson regression is a generalized linear modeling technique based on the Poisson distribution and provides standardized parameter estimates (B) that represent the estimated difference in the log of expected counts, holding other variables constant. The procedure models the count of suicides given the total population at risk, with a separate observation for each year.
RESULTS
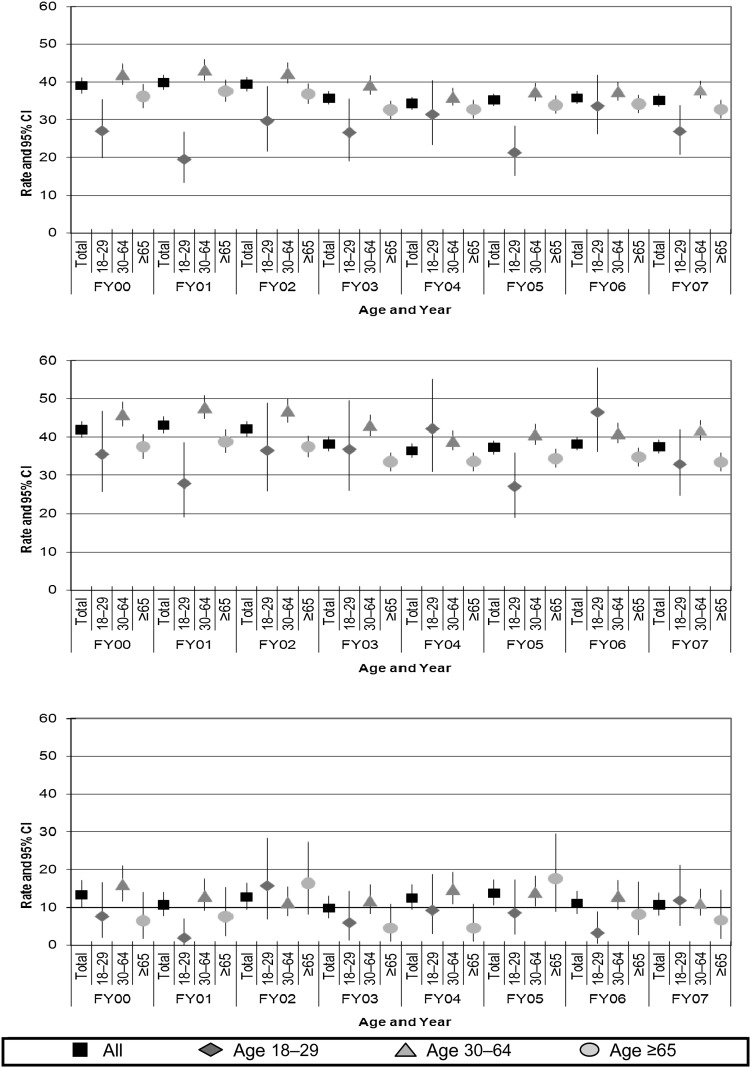
From FY00 to FY07, annual VHA rates of suicide mortality ranged from 34.3 to 39.8 suicides per 100 000 person-years (Figure 1a). Figure 1b and 1c displays the age-stratified rates of suicide for male and female VHA users. Among male VHA users, the annual rates of suicide ranged from 36.4 to 43.1 suicides per 100 000 person-years, while among female VHA users, the annual rates of suicide ranged from 9.8 to 13.7. The rate of suicide was lower among male VHA users aged 65 years and older than among male VHA users age 30–64; in all years, the lower limit of the confidence interval around the rate of suicide for male VHA users aged 30–64 years was greater than the upper limit of the confidence interval around the rate of suicide for male VHA users aged 65 years and older (Table 1).
FIGURE 1—
Rate per 100 000 person-years and 95% confidence intervals (CIs) of suicide by age and fiscal year (FY), among (a) all Veterans Health Administration (VHA) users, (b) male VHA users, and (c) female VHA users: FY2000–FY2007.
TABLE 1—
Number of Suicides and Suicide Rates per 100 000 Person-Years Among VHA Users, by Gender and Age: Fiscal Year (FY) 2000–FY2007
| FY2000 |
FY2001 |
FY2002 |
FY2003 |
FY2004 |
FY2005 |
FY2006 |
FY2007 |
|||||||||
| Suicides, No. | Rate (95% CI) | Suicides, No | Rate (95% CI) | Suicides, No | Rate (95% CI) | Suicides, No | Rate (95% CI) | Suicides, No | Rate (95% CI) | Suicides, No | Rate (95% CI) | Suicides, No | Rate (95% CI) | Suicides, No | Rate (95% CI) | |
| All VHA users | ||||||||||||||||
| Total | 1453 | 39.0 (37.0, 41.0) | 1609 | 39.8 (37.9, 41.8) | 1741 | 39.4 (37.5, 41.2) | 1694 | 35.7 (34.1, 37.5) | 1692 | 34.3 (32.7, 36.0) | 1785 | 35.2 (33.6, 36.9) | 1855 | 35.8 (34.2, 37.5) | 1841 | 35.1 (33.5, 36.8) |
| Age 18–29 y | 47 | 27.0 (19.8, 35.3) | 32 | 19.5 (13.4, 26.8) | 46 | 29.7 (21.7, 38.9) | 41 | 26.6 (19.1, 35.4) | 52 | 31.4 (23.4, 40.4) | 40 | 21.3 (15.2, 28.3) | 71 | 33.6 (26.2, 41.8) | 64 | 26.9 (20.7, 33.8) |
| Age 30–64 y | 863 | 42.0 (39.2, 44.8) | 925 | 43.2 (40.5, 46.0) | 960 | 42.3 (39.7, 45.1) | 943 | 39.2 (36.7, 41.7) | 904 | 36.0 (33.7, 38.4) | 969 | 37.4 (35.0, 39.7) | 995 | 37.5 (35.2, 39.9) | 1024 | 37.9 (35.6, 40.3) |
| Age ≥ 65 y | 543 | 36.2 (33.2, 39.3) | 652 | 37.6 (34.8, 40.6) | 735 | 36.8 (34.2, 39.5) | 710 | 32.6 (30.2, 35.0) | 736 | 32.7 (30.4, 35.1) | 776 | 33.9 (31.6, 36.4) | 789 | 34.1 (31.7, 36.5) | 753 | 32.7 (30.4, 35.1) |
| Male VHA users | ||||||||||||||||
| Total | 1401 | 41.9 (39.8, 44.2) | 1566 | 43.1 (41.0, 45.3) | 1689 | 42.1 (40.1, 44.1) | 1653 | 38.2 (36.4, 40.1) | 1638 | 36.4 (34.7, 38.2) | 1724 | 37.3 (35.5, 39.1) | 1805 | 38.2 (36.5, 40.0) | 1791 | 37.5 (35.8, 39.3) |
| Age 18–29 y | 43 | 35.5 (25.7, 46.8) | 31 | 27.9 (19.0, 38.6) | 38 | 36.5 (25.9, 49.0) | 38 | 36.8 (26.1, 49.5) | 47 | 42.2 (31.0, 55.1) | 35 | 27.1 (18.9, 36.0) | 69 | 46.5 (36.2, 58.1) | 56 | 32.9 (24.8, 42.0) |
| Age 30–64 y | 819 | 46.0 (42.9, 49.2) | 888 | 47.8 (44.7, 51.0) | 927 | 46.9 (43.9, 50.0) | 908 | 43.1 (40.3, 45.9) | 858 | 39.0 (36.5, 41.7) | 924 | 40.7 (38.1, 43.3) | 952 | 41.0 (38.4, 43.6) | 986 | 41.8 (39.2, 44.5) |
| Age ≥ 65 y | 539 | 37.5 (34.4, 40.7) | 647 | 38.8 (35.9, 41.9) | 724 | 37.5 (34.8, 40.3) | 707 | 33.5 (31.1, 36.0) | 733 | 33.6 (31.2, 36.0) | 765 | 34.4 (32.0, 36.9) | 784 | 34.8 (32.4, 37.2) | 749 | 33.4 (31.1, 35.9) |
| Female VHA users | ||||||||||||||||
| Total | 52 | 13.3 (10.0, 17.2) | 43 | 10.6 (7.7, 14.0) | 52 | 12.7 (9.5, 16.4) | 41 | 9.8 (7.1, 13.1) | 54 | 12.5 (9.4, 16.0) | 61 | 13.7 (10.5, 17.4) | 50 | 11.0 (8.2, 14.3) | 50 | 10.6 (7.9, 13.8) |
| Age 18–29 y | 4 | 7.6 (2.1, 16.6) | 1 | 1.9 (0.1, 7.0) | 8 | 15.7 (6.8, 29.3) | 3 | 5.9 (1.2, 14.3) | 5 | 9.2 (3.0, 18.8) | 5 | 8.5 (2.8, 17.4) | 2 | 3.2 (0.4, 8.8) | 8 | 11.8 (5.1, 21.2) |
| Age 30–64 y | 44 | 16.1 (11.7, 21.1) | 37 | 13.0 (9.2, 17.5) | 33 | 11.3 (7.8, 15.5) | 35 | 11.7 (8.2, 15.9) | 46 | 14.8 (10.8, 19.3) | 45 | 14.0 (10.2, 18.3) | 43 | 13.0 (9.4, 17.2) | 38 | 11.1 (7.9, 14.9) |
| Age ≥ 65 y | 4 | 6.4 (1.7, 14.0) | 5 | 7.5 (2.4, 15.3) | 11 | 16.3 (8.1, 27.3) | 3 | 4.5 (0.9, 10.8) | 3 | 4.5 (0.9, 10.9) | 11 | 17.6 (8.8, 29.5) | 5 | 8.2 (2.7, 16.8) | 4 | 6.6 (1.8, 14.5) |
Note. VHA = Veterans Health Administration; CI = confidence interval.
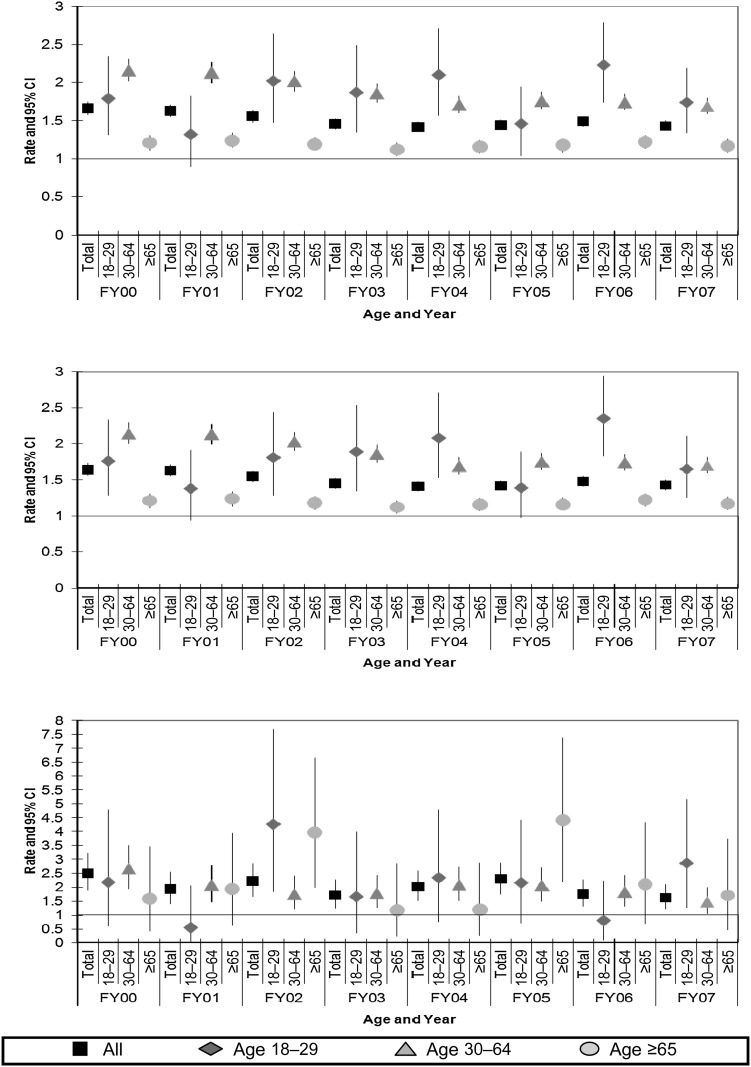
Table 2 reports the SMRs for comparisons of suicide mortality among VHA users compared with the general US population, by age and gender subgroups. Over 8 years, SMRs for suicide for all VHA users ranged from 1.42 to 1.66 (Figure 2a). Each year, the lower limit of the 95% confidence interval exceeded 1.0, indicating excess suicide mortality. This was also observed for the SMRs for each age group (18–29 years, 30–64 years, and 65 years and older) when male and female VHA users were combined, except in FY01 among VHA users between the ages of 18 and 29. From FY00 to FY07, the SMRs for the middle age group (30–64 years) were consistently higher than that for the oldest age group (65 years and older), and confidence intervals did not overlap. There was insufficient statistical power to compare the excess suicide mortality in the youngest age group with that in the other age groups.
TABLE 2—
Standardized Mortality Ratio of Suicide Fatality (With 95% Confidence Intervals [CIs]), by Gender and Age Group: VHA Users, FY2000–FY2007
| FY2000, SMR (95% CI) | FY2001, SMR (95% CI) | FY2002, SMR (95% CI) | FY2003, SMR (95% CI) | FY2004, SMR (95% CI) | FY2005, SMR (95% CI) | FY2006, SMR (95% CI) | FY2007, SMR (95% CI) | |
| All VHA users | ||||||||
| Total | 1.66 (1.58, 1.75) | 1.63 (1.55, 1.71) | 1.56 (1.49, 1.63) | 1.46 (1.39, 1.53) | 1.42 (1.36, 1.49) | 1.44 (1.38, 1.51) | 1.49 (1.42, 1.55) | 1.43 (1.37, 1.50) |
| Age 18–29 y | 1.79 (1.32, 2.34) | 1.32 (0.90, 1.82) | 2.02 (1.48, 2.64) | 1.87 (1.35, 2.49) | 2.10 (1.57, 2.71) | 1.46 (1.04, 1.94) | 2.23 (1.74, 2.78) | 1.74 (1.34, 2.19) |
| Age 30–64 y | 2.16 (2.02, 2.31) | 2.13 (1.99, 2.27) | 2.02 (1.89, 2.15) | 1.86 (1.74, 1.98) | 1.71 (1.60, 1.82) | 1.76 (1.65, 1.88) | 1.74 (1.64, 1.85) | 1.69 (1.59, 1.80) |
| Age ≥ 65 y | 1.21 (1.11, 1.31) | 1.24 (1.15, 1.34) | 1.19 (1.11, 1.28) | 1.12 (1.04, 1.21) | 1.16 (1.07, 1.24) | 1.18 (1.09, 1.26) | 1.22 (1.14, 1.31) | 1.17 (1.09, 1.26) |
| Male VHA users | ||||||||
| Total | 1.64 (1.56, 1.73) | 1.63 (1.55, 1.71) | 1.55 (1.47, 1.62) | 1.45 (1.38, 1.52) | 1.41 (1.34, 1.48) | 1.42 (1.36, 1.49) | 1.48 (1.41, 1.55) | 1.43 (1.36, 1.50) |
| Age 18–29 y | 1.76 (1.28, 2.33) | 1.38 (0.94, 1.91) | 1.81 (1.28, 2.44) | 1.89 (1.34, 2.54) | 2.08 (1.53, 2.71) | 1.39 (0.97, 1.89) | 2.35 (1.83, 2.94) | 1.65 (1.25, 2.11) |
| Age 30–64 y | 2.14 (2.00, 2.29) | 2.13 (1.99, 2.27) | 2.03 (1.90, 2.16) | 1.86 (1.74, 1.98) | 1.69 (1.58, 1.81) | 1.75 (1.64, 1.87) | 1.74 (1.63, 1.85) | 1.70 (1.60, 1.81) |
| Age ≥ 65 y | 1.21 (1.11, 1.31) | 1.24 (1.14, 1.33) | 1.18 (1.09, 1.27) | 1.12 (1.04, 1.21) | 1.16 (1.07, 1.24) | 1.16 (1.08, 1.25) | 1.22 (1.14, 1.31) | 1.17 (1.09, 1.26) |
| Female VHA users | ||||||||
| Total | 2.50 (1.87, 3.22) | 1.93 (1.40, 2.55) | 2.22 (1.66, 2.86) | 1.71 (1.23, 2.27) | 2.02 (1.52, 2.59) | 2.29 (1.75, 2.89) | 1.76 (1.31, 2.28) | 1.62 (1.20, 2.10) |
| Age 18–29 y | 2.18 (0.59, 4.78) | 0.55 (0.01, 2.05) | 4.27 (1.84, 7.69) | 1.66 (0.34, 3.99) | 2.34 (0.76, 4.79) | 2.16 (0.70, 4.43) | 0.80 (0.10, 2.23) | 2.87 (1.24, 5.17) |
| Age 30–64 y | 2.67 (1.94, 3.52) | 2.07 (1.46, 2.79) | 1.75 (1.21, 2.40) | 1.78 (1.24, 2.42) | 2.08 (1.52, 2.72) | 2.06 (1.50, 2.70) | 1.83 (1.32, 2.42) | 1.48 (1.05, 1.99) |
| Age ≥ 65 y | 1.58 (0.43, 3.47) | 1.93 (0.63, 3.95) | 3.98 (1.99, 6.65) | 1.18 (0.24, 2.85) | 1.19 (0.25, 2.87) | 4.41 (2.20, 7.37) | 2.11 (0.69, 4.33) | 1.71 (0.46, 3.74) |
Note. VHA = Veterans Health Administration; CI = confidence interval; FY = fiscal year.
FIGURE 2—
Standardized mortality ratios and 95% confidence intervals (CIs) of suicide, by age and fiscal year (FY), as compared with the general population among (a) all Veterans Health Administration (VHA) users, (b) male VHA users, and (c) female VHA users: FY2000–FY2007.
Figures 2b and 2c present the total and age-group specific SMRs for men and women. Among male VHA users in the age groups of 30–64 years and 65 years and older, the SMR of suicide mortality was stable and significantly elevated over all years (ranges of 1.69–2.14 and 1.12–1.24, respectively). For male patients, excess suicide mortality was higher for middle age than for older groups, with nonoverlapping confidence intervals. For male VHA users aged 18–29 years, the range of SMRs from FY00 to FY07 was 1.38–2.35. The SMR for men aged 65 years and older was below that of men aged 18–29 years (with nonoverlapping 95% confidence intervals) for FY02, FY03, FY04, and FY06.
The suicide rate for VHA users decreased between FY00 and FY07, with a parameter estimate for each FY of −0.022 (P < .001, after control for age and gender). Examining confidence intervals for the annual rates in Table 1 indicates the rate of suicide decreased most notably around FY03. Gender- and age-stratified Poisson regression modeling indicated that the rate of suicide decreased for men aged 30–64 years (B = −0.025; P < .001) and men aged 65 years and older (B = −0.020,;P = .007).
Inspection of the annual rates and their confidence intervals in Figure 1b suggests the drop in the suicide rate was most pronounced around FY03 for men aged 30–64 years because the lower limit of the confidence intervals for FY01 and FY02 are greater than the upper limit of the confidence intervals for the rates of FY04 through FY07 in this age–gender group. The confidence intervals around the estimates of the rate of suicide for the smaller group of those aged 18–29 years were wide and overlapped for all years; no significant changes were found in rates of suicide in this group (B = 0.015; P = .49).
As demonstrated in Figure 1c, the rate of suicide for female VHA users was less stable over time than for male VHA users; confidence intervals were wide, particularly for women aged 18–29 years and aged 65 years and older. No significant time trends in the suicide rate were found among female VHA users; age–group stratified models resulted in standardized parameter estimates between −0.021 and 0.029 (all P > .05). Consequently, it cannot be concluded that the overall trends represent true changes in the rate of suicide for these groups.
The estimated SMRs for males aged 30–64 years were consistently lower between FY04 to FY07 than for FY00 to FY02, with nonoverlapping confidence intervals. This shift suggests that suicide risk for male VHA users aged 30–64 years decreased relative to men of the same age in the general population around FY03. Age-stratified SMRs for suicide mortality among female VHA users had wide confidence intervals and did not indicate a consistent trend in suicide rates for female VHA users relative to females in the United States.
DISCUSSION
In each of the 8 years from 2000 to 2007, suicide was consistently more common among those who used VHA services than in the general US age- and gender-matched population. However, Poisson regression tests indicate that rates among VHA users decreased over time (B = −0.022; P < .001). Rates of suicide in the most recent years were significantly lower than those found in the earlier portion of the observation period, with the middle year of 2003 serving as a transition year. This shift in 2003 may signify an increased awareness and sensitivity to mental health issues in the VHA following the initiation of OIF, which began the same year; Seal et al.30 found that rates of mental health diagnoses increased significantly after the start of OIF among first-time users of VHA services returning from Iraq and Afghanistan over a 2-year period. The reductions in suicide rates found in the present study appear to be largely driven by lower rates of suicide after 2004 among men aged 30–64 years, and, to a lesser degree, by men in the 65 years and older age group. Although suicide rates decreased over time among male veterans in the middle age group, their rates remained consistently higher than either older or younger veterans. These results differ from the typical pattern observed in the United States, in which rates of suicide are highest in older males.3
Examining suicide in veterans over the past several years is of particular importance because of the potential impact of the conflicts in Iraq and Afghanistan on suicide risk. These concerns are largely driven by recent findings documenting an elevated prevalence of suicide risk factors among individuals who served in Iraq or Afghanistan.4,5 However, suicide has multiple causal pathways that are influenced by a variety of components, such as biological (e.g., gender), socioeconomic (e.g., employment status), and other factors (e.g., access to firearms) and confer increased risk of suicidal behaviors and suicide among specific cohorts.2,15,16,31 Mental health problems associated with these recent conflicts may not directly lead to increased rates of suicide among VHA users. No increase in rates of suicide was observed since the start of the conflict in Afghanistan; in fact, we observed a statistically significant (P < .001) decrease in the suicide rate among VHA health system users between FY00 and FY07. These results are broadly consistent with a prior report noting no significant difference between rates of suicide in a smaller cohort of recent returnees from Iraq and Afghanistan and the general population.13
Our study evaluated rates in the entire population of VHA patients, which provided a greater precision to detect smaller differences than prior research on Veteran suicides. This is consistent with the fact that the SMRs calculated in the present study often fell within the 95% confidence intervals reported in many of the studies with null results.8–15 Additionally, many prior reports on suicide rates among Veteran populations were limited by determining vital status from data from the Beneficiary Identification Records Locator Subsystem (BIRLS) and Social Security Administration (SSA) files10,32 which have poorer sensitivity to detect vital status than does the NDI.23
These data are particularly important for any nationwide suicide prevention efforts. For example, between 2000 and 2007, the 13 626 suicides found among adults seen in the VHA represented 5.5% of the total 248 179 US adult suicides during this time period; while the VHA provides care for approximately 5 000 000 patients per year, representing approximately 2% of the US population. Our findings establish a baseline for examining the potential impact of comprehensive suicide-reduction strategies. Prior research in smaller European countries has examined changes in regional or even national suicide rates as a method for determining the impact of broad-based suicide-reduction programs.33–35 By establishing clear data on the baseline rates of suicide among users of VHA system, more specific data are available on the potential impact of VHA suicide prevention efforts.
In our study, middle-aged men were at the highest risk for suicide. It is not known why these individuals were at elevated risk, but several potential explanations exist. Within the VHA system, these individuals represent Vietnam-era veterans who may be a cohort at higher risk for suicide caused by overall morbidity, or to ongoing social, economic or psychiatric difficulties. Also, recent data indicates that suicide rates among middle-aged adults in the US have increased over the past 7 years.17 It is possible that the factors leading to this broad increase in this age group are particularly difficult for Veterans. Additionally, our results support the focus of VHA's ongoing efforts at suicide prevention. Although it is clearly important to target recent returnees, VA's approach to suicide prevention among veterans also includes an emphasis on targeting veterans from past conflicts.15
An important limitation of our study is that we did not have reliable data on race across all years. Data on military duty characteristics and prior research indicates that National Guard veterans may have a particularly high rate of suicide.36,37 Because there is a several year lag in the dissemination of US mortality data, the analyses we present do not include data from more recent years. The population is predominantly male and of middle age, thus estimates in other subgroups of individuals are less precise. Our study focused on examining SMRs in specific age and gender subgroups; however, we did not control for other differences in case mix. The methods for calculating risk in the present study are novel and it is possible that differing methods for calculating risk would have yielded other results. However, the results were consistent to ±0.2 when compared with an a prior publication7 that used an exact method to calculate rates for FY01. Additionally, the precision of the estimation of SMRs was diminished by the fact that the last 3 months of every calendar year were included in the subsequent fiscal year. However, the general lack of change in the rates of suicide in the United States increases the likelihood that this had minimal impact on the calculation of SMRs. The comparison group for calculating SMRs includes some veterans, likely diminishing the differences between groups used in our primary analyses. Finally, our sample was restricted to veterans utilizing VHA services, which represents approximately 20% of all veterans in the United States (≥ 5.5 million out of ≥ 24 million).38
Despite these limitations, to our knowledge this is the first comprehensive study of suicide mortality among patients receiving health care in a large national health care system. These findings indicate that there has been no increase in suicide rates among the VHA population of patients since the start of the conflicts in Iraq and Afghanistan; in fact, suicide rates among the VHA patient population have decreased since FY2000. However, VHA users are at increased risk for suicide compared with individuals the same age and gender in the general population. Comprehensive approaches to suicide prevention in the VHA should focus not only on recent returnees but also on middle-aged and older Veterans.
Acknowledgments
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Mental Health Services. Input from VA's Office of Mental Health Services shaped the design and conduct of the study, the collection, management, analysis, and interpretation of the data, and the preparation, review, and approval of the manuscript.
Human Participation Statement
Approval was granted to this study by the Ann Arbor VA Human Subjects Committee.
References
- 1.Office of the Surgeon General The Surgeon General's Call to Action to Prevent Suicide. Washington, DC: Department of Health and Human Services, US Public Health Service, 1999 [Google Scholar]
- 2.Institute of Medicine Reducing Suicide: A National Imperative. Washington, DC: National Academies Press; 2002 [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Web-based Injury Statistics Query and Reporting System: Leading Causes of Death Reports. Atlanta, GA: Centers for Disease Control and Prevention; 2008 [Google Scholar]
- 4.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs Medical Centers sicker? Arch Intern Med. 2000;160:3252–3257 [DOI] [PubMed] [Google Scholar]
- 5.Lambert MT, Fowler DR. Suicide risk factors among veterans: risk management in the changing culture of the Department of Veterans Affairs. J Ment Health Admin. 1997;24:350–358 [DOI] [PubMed] [Google Scholar]
- 6.Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: a prospective population-based study. J Epidemiol Community Health. 2007;61:619–624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCarthy JF, Valenstein M, Kim HM, Ilgen M, Zivin K, Blow FC. Suicide mortality among patients receiving care in the Veterans Health Administration health system. Am J Epidemiol. 2009;169:1033–1038 [DOI] [PubMed] [Google Scholar]
- 8.Boyle CA, Decoufle P. Postdischarge mortality from suicide and motor-vehicle injuries among Vietnam-era veterans. N Engl J Med. 1987;317:506–507 [DOI] [PubMed] [Google Scholar]
- 9.Watanabe KK, Kang HK. Military service in Vietnam and the risk of death from trauma and selected cancers. Ann Epidemiol. 1995;5:407–412 [DOI] [PubMed] [Google Scholar]
- 10.Bullman TA, Kang HK. The risk of suicide among wounded Vietnam veterans. Am J Public Health. 1996;86:662–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cypel Y, Kang H. Mortality patterns among women Vietnam-era veterans: results of a retrospective cohort study. Ann Epidemiol. 2008;18:244–252 [DOI] [PubMed] [Google Scholar]
- 12.Kang HK, Bullman TA. Mortality among US veterans of the Persian Gulf War. N Engl J Med. 1996;335:1498–1504 [DOI] [PubMed] [Google Scholar]
- 13.Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300:652–653 [DOI] [PubMed] [Google Scholar]
- 14.Thomas TL, Kang HK, Dalager NA. Mortality among women Vietnam veterans, 1973–1987. Am J Epidemiol. 1991;134:973–980 [DOI] [PubMed] [Google Scholar]
- 15.Miller M, Barber C, Azrael D, Calle E, Lawler E, Mukamal K. Suicide among US veterans: a prospective study of 500,000 middle-aged and elderly men. Am J Epidemiol. 2009;170:494–500 [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–2495 [DOI] [PubMed] [Google Scholar]
- 17.Hu G, Wilcox HC, Wissow L, Baker SP. Mid-life suicide: an increasing problem in US Whites, 1999–2005. Am J Prev Med. 2008;35:589–593 [DOI] [PubMed] [Google Scholar]
- 18.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032 [DOI] [PubMed] [Google Scholar]
- 19.Milliken CS, Auchterloni JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component solidiers returning from the Iraq War. JAMA. 2007;298:2141–2148 [DOI] [PubMed] [Google Scholar]
- 20.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103 788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476–482 [DOI] [PubMed] [Google Scholar]
- 21.West AN, Weeks WB. Mental distress among younger veterans before, during, and after the invasion of Iraq. Psychiatr Serv. 2006;57:244–248 [DOI] [PubMed] [Google Scholar]
- 22. Joshua Omvig Veterans Suicide Prevention Act of 2007, Pub. L. No. 110-110, 121 Stat. 1031.
- 23.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12:462–468 [DOI] [PubMed] [Google Scholar]
- 24.Sohn MW, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Center for Injury Prevention and Control Office of Statistics and Programming. WISQARS Fatal Injuries: Mortality Reports. Available at: http://www.cdc.gov/injury/wisqars/fatal.html. Accessed September 3, 2010
- 26.World Health Organization International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva, Switzerland: World Health Organization; 2004 [Google Scholar]
- 27.Ulm K. A simple method to calculate the confidence interval of a standardized mortality ratio (SMR). Am J Epidemiol. 1990;131:373–375 [DOI] [PubMed] [Google Scholar]
- 28.Hennekens C. Buring J. Epidemiology in Medicine. Boston, MA: Little, Brown and Company; 1987 [Google Scholar]
- 29.Pagano M, Gauvreau K. Principles of Biostatistics. 2nd edition Belmont, CA: Wadsworth Inc., 2000 [Google Scholar]
- 30.Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaplan MS, McFarland BH, Huguet N. Firearm suicide among veterans in the general population: findings from the national violent death reporting system. J Trauma. 2009;67:503–507 [DOI] [PubMed] [Google Scholar]
- 32.Bullman TA, Kang HK. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. J Nerv Ment Dis. 1994;182:604–610 [DOI] [PubMed] [Google Scholar]
- 33.Rihmer Z, Rutz W, Pihlgren H. Depression and suicide on Gotland. An intensive study of all suicides before and after a depression-training programme for general practitioners. J Affect Disord. 1995;35:147–152 [DOI] [PubMed] [Google Scholar]
- 34.Rutz W, von Knorring L, Walinder J. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr Scand. 1992;85:83–88 [DOI] [PubMed] [Google Scholar]
- 35.Szanto K, Kalmar S, Hendin H, Rihmer Z, Mann JJ. A suicide prevention program in a region with a very high suicide rate. Arch Gen Psychiatry. 2007;64:914–920 [DOI] [PubMed] [Google Scholar]
- 36.Zoroya G. More Army Guard, Reserve soldiers committing suicide. USA Today. Published January 20, 2011. Available at: http://www.usatoday.com/news/military/2011-01-20-suicides20_ST_N.htm. Accessed February 26, 2011
- 37.Department of Defense (DOD) Army releases December and 2010 suicide data. Published January 19, 2011. Available at: http://www.defense.gov/utility/printitem.aspx?print=http://www.defense.gov/Releases/Release.aspx?ReleaseID=14213. Accessed February 26, 2011 [Google Scholar]
- 38.Department of Veterans Affairs National Center for Veterans Analysis and Statistics data. Available at: http://www.va.gov/vetdata/index.asp. Accessed July 5, 2011