Abstract
Background
Surgical injury can frequently lead to chronic pain. Despite the obvious importance of this problem, the first publications on chronic pain after surgery as a general topic appeared only a decade ago. This study tests the hypothesis that chronic postsurgical pain was, and still is, represented insufficiently.
Methods
We analyzed the presentation of this topic in journal articles covered by PubMed and in surgical textbooks. The following signs of insufficient representation in journal articles were used: (1) the lack of journal editorials on chronic pain after surgery, (2) the lack of journal articles with titles clearly indicating that they are devoted to chronic postsurgical pain, and (3) the insufficient representation of chronic postsurgical pain in the top surgical journals.
Results
It was demonstrated that insufficient representation of this topic existed in 1981–2000, especially in surgical journals and textbooks. Interest in this topic began to increase, however, mostly regarding one specific surgery: herniorrhaphy. It is important that the change in the attitude toward chronic postsurgical pain spreads to other groups of surgeries.
Conclusion
Chronic postsurgical pain is still a neglected topic, except for pain after herniorrhaphy. The change in the attitude toward chronic postsurgical pain is the important first step in the approach to this problem.
Keywords: neuropathic pain, persistent pain, chronic pain, postoperative pain
Introduction
The recent report of the Institute of Medicine’s committee on pain relief in the US indicated that “more than 116 million Americans have pain that persists for weeks to years.”1 The important part of this problem is chronic postsurgical pain. Aasvang and Kehlet2 estimated the incidence of chronic pain after some surgical procedures: thoracotomy (approximately 50%), breast surgery (30%), cholecystectomy (10%–20%), and inguinal herniorrhaphy (10%). When the total number of patients who undergo these surgeries each year is taken into account, those figures are stunning. Macrae3 tried to present some figures that reflect the magnitude of the chronic postsurgical pain problem. His calculations yielded at least 400,000 new cases of chronic pain each year (in the US). He also indicated4 that about 20% of patients attending chronic pain clinics name surgery as one of the causes of their chronic pain, and for about half of these patients it was the sole cause.
Despite the obvious importance of this problem, publications on chronic pain after surgery as a general topic began to appear only a decade ago.4–6 These authors analyzed more than 100 references related to chronic postsurgical pain, noting that several features were common to all publications: (1) they were strictly limited to specific operations, (2) they failed to give a detailed description of the operative approaches, and (3) they usually provided only superficial assessments of chronic pain.4,6 Their conclusion was that “chronic pain after surgery has been a neglected topic.”4
The word “postsurgical” in the term “chronic postsurgical pain” already indicates the role of surgery in its genesis. The combination of two factors related to coping with this problem gives surgery an additional importance: (1) ineffective existing treatments of neuropathic pain and (2) the importance of surgical techniques avoiding nerve injuries in the prevention of this type of chronic pain. Unfortunately, treatments for neuropathic pain, including the majority of chronic postsurgical pain cases, are not very effective. No more than 40%–60% of patients obtain pain relief; in addition, the relief is only partial.7 Existing evidence indicates that intraoperative nerve injury is the most important contributor to the development of chronic postsurgical pain.8,9 The analysis of all possible approaches for the prevention of postsurgical pain points to one reliable solution: surgical techniques that avoid nerve damage should be used wherever possible.8 As a result, although chronic postsurgical pain is a topic relevant to many specialties (surgery, anesthesiology, neurology, pain medicine, rehabilitation medicine, and psychology), currently, the most promising approach to reducing the incidence and intensity of chronic postsurgical pain is almost completely in the hands of surgeons, who can select techniques that minimize the risk of nerve damage. Therefore, the adequate presentation of chronic postoperative pain in surgical journals and textbooks is especially important.
Our study tested the hypothesis that chronic pain after surgery was, and still is, represented insufficiently. We analyzed the presentation of this topic in journal articles covered by PubMed, especially in surgical journals, and also in surgery textbooks.
Methods
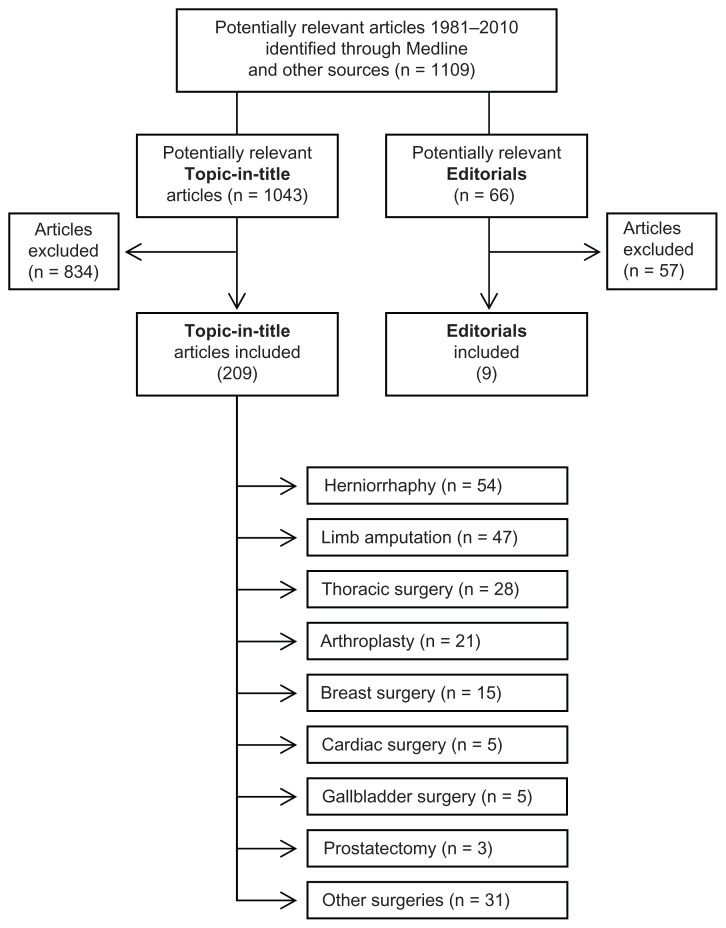
To test the study hypothesis with journal articles, we used the following three signs of insufficient representation: (1) the lack of journal editorials on chronic pain after surgery, (2) the lack of journal articles with titles clearly indicating that they are devoted to chronic postsurgical pain, and (3) the insufficient representation of chronic postsurgical pain in the top surgical journals. Concerning the analysis of textbooks, we followed the general approach used by Rabow et al.10 The representation of chronic postsurgical pain in textbooks was assessed on the basis of the presence of this topic in general chapters and in the chapters on specific surgeries, as well as on the total content volume related to chronic pain after surgery. Journal articles were collected using the National Library of Medicine’s PubMed website (http://www.ncbi.nlm.nih.gov/PubMed ). All types of articles published in English during 30 years (1981–2010) were included. Keywords related to the names of surgical interventions were added to the terms related to the chronic pain (“chronic pain” OR “neuropathy” OR “neuralgia”). Boolean operations were used in which the following variables were selected: keywords, years of publications, and type of publications. In addition to the electronic search of articles, related publications were also collected manually from the literature on chronic postsurgical pain (Figure 1).
Figure 1.
Flow chart of screened, excluded, and included articles on chronic postsurgical pain (1981–2010).
Editorials
The editorials (articles solicited by an editorial board to provide an editorial perspective on the article published in a journal) on chronic postsurgical pain were grouped into 5-year periods, starting with 1981–1985, separately for (1) all journals covered by PubMed and (2) only surgical journals.
Topic-in-title articles
To select journal articles with titles clearly indicating that they are devoted to chronic postsurgical pain (topic-in-title articles), the indication “[Title]” was added to all terms placed into PubMed search boxes. The topic-in-title type of articles were searched as representing chronic pain after surgery in general (when terms “surgery” [Title] OR “postoperative” [Title] were added to pain terms “chronic pain” [Title] OR “neuropathy” [Title]) or as representing chronic pain after specific surgeries (see Table 1). The specific surgeries were selected on the basis of preliminary PubMed searches conducted with inclusion of various specific terms of surgical interventions and specific pain-related terms (indicated in Table 1). In the preliminary searches, the indication “[Title]” in the PubMed search box was not used. The preliminary searches resulted in a total of 1043 references. The topic-in-title articles for a specific group of surgeries were counted only when a preliminary search for this group gave ten or more general (non-topic-in-title) references. Eight groups of surgeries were selected: herniorrhaphy, limb amputation, thoracic surgery, arthroplasty, breast surgery, cardiac surgery, gallbladder surgery, and prostatectomy. For inclusion as the topic-in-title publication, articles found in various searches were reviewed to make sure that they fit the definition of chronic pain after surgery. Articles with titles without certain indication of pain duration, such as “persistent,” “persisting,” “long-term,” “residual pain,” or “pain syndrome” were checked and included only if the duration of pain was 6 months or longer. If the duration of pain was indicated in the title of an article as 6 months or longer, it was also included in the database.
Table 1.
Numerical representation of topic-in-title articles on chronic pain after specific surgeries, 1981–2010a
| No | Terms of surgical interventionsb | Number of topic-in-title articles |
|---|---|---|
| 1 | Herniorrhaphy OR “hernia repair” | 54 |
| 2 | Amputationc | 47 |
| 3 | “Thoracic surgery” OR thoracotomy | 28 |
| 4 | Arthroplasty OR “knee replacement” OR “hip replacement” | 21 |
| 5 | “Breast surgery” OR “breast reconstruction” OR mastectomy | 15 |
| 6 | “Cardiac surgery” OR “CABG surgery” OR sternotomy | 13 |
| 7 | “Gallbladder surgery” OR cholecystectomy | 5 |
| 8 | Prostatectomy | 3 |
| Total | 186 |
Notes:
Electronic (via PubMed) and manual search of the literature on chronic postsurgical pain.
AND the following pain-related terms: “chronic pain” OR “neuropathy” OR “neuralgia” were added.
the following terms: “phantom pain” OR “residual limb pain” were added to the pain-related terms.
Abbreviation: CABG, coronary artery bypass grafting.
To quantitatively evaluate the response of surgical journals to the problem of chronic postsurgical pain, we analyzed the publications of topic-in-title articles in the top 20 surgical journals. It has been observed that the number of journal articles on a new and important topic rises much faster in the top specialty journals than it does in all other journals covered by PubMed.11 We also calculated the Top Journal Selectivity Index (TJSI). This index represents the ratio of the number of articles in the top 20 surgical journals to the number of articles in all journals covered by PubMed11,12 (see Discussion). We counted only articles with titles clearly announcing that they are devoted to chronic pain after surgery (topic-in-title articles). The selection of the top 20 surgical journals was based on the rank of a journal sorted by the impact factor, as indicated by Journal Citation Reports for year 2010 ( http://science.thomsonreuters.com ). The following surgical journals were included: the American Journal of Surgery, American Journal of Surgical Pathology, American Journal of Transplantation, Annals of Surgery, Annals of Surgical Oncology, Archives of Surgery, British Journal of Surgery, Dermatologic Surgery, Endoscopy, Journal of the American Academy of Orthopaedic Surgeons, American Journal of Bone and Joint Surgery, Journal of Gastrointestinal Surgery, Journal of Shoulder and Elbow Surgery, Journal of Surgical Oncology, Journal of Vascular Surgery, Journal of Thoracic and Cardiovascular Surgery, Surgical Endoscopy, Surgery, Transplantation, and World Journal of Surgery.
Textbooks
The assessment of representation of chronic postsurgical pain in the surgical textbooks was based on the analysis of three texts selected on the basis of two factors: the text should be eponymously titled (named texts) and also should be sorted as one of the top three surgical texts held in libraries as listed in the meta-catalog WorldCat (worldcat.org). The following textbooks were selected: Sabiston Textbook of Surgery, 18th ed, 2008;13 Schwartz’s Principles of Surgery, 9th ed, 2009;14 and Greenfield’s Surgery, 5th ed, 2010.15 For comparison, an anesthesiology textbook was also analyzed: Miller’s Anesthesia, 7th ed, 2010.16 All textbooks were inspected on the presence of materials related to chronic postsurgical pain (number of lines of text, tables, figures, references). The data were collected in three steps: (1) review of chapters on basic principles (examination of the table of contents, identification of chapters devoted to general topics, inspection of all pages of identified chapters), (2) review of specific surgeries (examination of text index for keywords concerning specific surgeries: limb amputation, thoracotomy, coronary artery bypass grafting, mastectomy, cholecystectomy, herniorrhaphy, and arthroplasty; inspection of all pages of identified chapters), and (3) examination of the text index (keywords concerning specific chronic pain syndromes: causalgia, complex regional pain syndrome, neuralgia, neuropathy, pain chronic, pain neuropathic, phantom pain; inspection of all pages indicated for these terms.) Each textbook was assessed by two reviewers (SG and IK). Discrepancies in the count were resolved by consensus.
Results
Editorials
The results on the representation of chronic postsurgical pain in journal editorials are presented in Table 2. Since 1981 only nine editorials were published (two in 2001–2005 and seven in 2006–2010). Seven of them appeared in anesthesiological journals (four in Anesthesiology) and none in surgical journals.
Table 2.
Editorials on chronic postsurgical pain
Topic-in-title articles
Topic-in-title articles (clearly announcing the problem of chronic postsurgical pain) are presented in Table 3. This table reflects only the number of articles that represent chronic pain after surgery in general. It indicates that the topic-in-title articles began to appear in significant numbers only relatively late, especially in surgical journals (2001–2010). Table 4 compares the numbers of topic-in-title articles on chronic and acute postsurgical pain represented as a percentage of all articles on chronic or acute pain (without the indication “surgery” and “postoperative”). The percentage of the topic-in-title type of articles on chronic postsurgical pain was 0% in 1981–1990 and rose to 0.8% in 2001–2010. Nevertheless, even in 2001–2010 it was one-seventh the number on acute postsurgical pain.
Table 3.
Topic-in-title articles on chronic postsurgical pain, 1981–2010
| Years | Numbers of articlesa | |
|---|---|---|
|
|
||
| All journalsb | Surgical journals | |
| 81–85 | 0 | 0 |
| 86–90 | 0 | 0 |
| 91–95 | 2 | 2 |
| 96–00 | 9 | 2 |
| 01–05 | 15 | 6 |
| 06–10 | 31 | 10 |
Notes:
Articles with titles clearly indicating that they are devoted to postsurgical chronic pain. Searched as articles on chronic pain after surgery in general: “chronic pain” OR “neuropathic” AND “surgery” OR “postoperative;”
including surgical journals.
Table 4.
Comparisons of topic-in-title articles on chronic and acute postsurgical pain
| Years | “Chronic pain”a AND “surgery”b IN TITLE | “Pain” NOT “chronic” AND “surgery”b IN TITLE | ||
|---|---|---|---|---|
|
|
|
|||
| Number of articles | As a percentage of “chronic pain”a onlyc | Number of articles | As a percentage of “pain” onlyc | |
| 81–90 | 0 | 0% | 626 | 6.8% |
| 91–00 | 11 | 0.6% | 1137 | 6.5% |
| 01–10 | 46 | 0.8% | 2117 | 5.8% |
Notes:
OR “neuropathic;”
OR “postoperative;”
without “surgery” or “postoperative.”
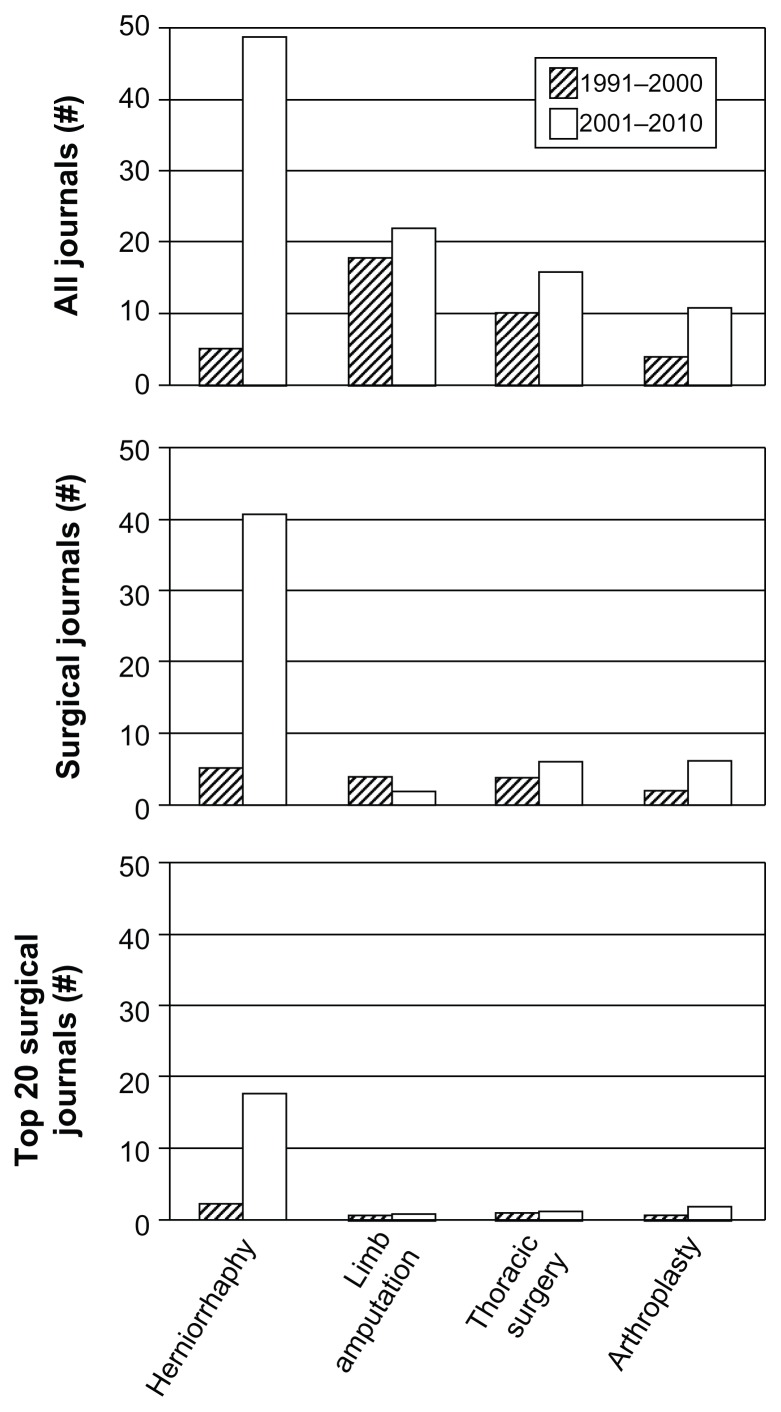
The summary of the results with the topic-in-title articles for eight specific groups of surgeries is presented in Table 1. The most publications were on herniorrhaphy (54 articles), then, in decreasing order, amputation (47), thoracic surgery (28), arthroplasty (21), breast surgery (15), and cardiac surgery (13). There were only five topic-in-title articles on gallbladder surgery and three on prostatectomy. The distribution of articles among journals of different specialties depended on the type of specific surgeries. With herniorrhaphy it was mostly surgical journals, with limb amputation mostly pain journals and disability/rehabilitation journals, and with all other surgeries mostly anesthesiology and pain journals. Table 5 presents the time-related progress in numerical representation of topic-in-title articles on chronic pain after specific surgeries in all journals and separately in all surgical journals. In surgical journals the only impressive rise was for herniorrhaphy, from five articles in 1991–2000 to 41 in 2001–2010.
Table 5.
Time-related progress in numerical representation of topic-in-title articles on chronic pain after specific surgeries
| No | Specific surgeries | All journals | Surgical journalsa | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| 81–90 | 91–00 | 01–10 | 81–90 | 91–00 | 01–10 | ||
| 1 | Herniorrhaphy | 0 | 5 | 49 | 0 | 5 | 41 |
| 2 | Limb amputation | 7 | 18 | 22 | 0 | 4 | 2 |
| 3 | Thoracic surgery | 2 | 10 | 16 | 0 | 4 | 6 |
| 4 | Arthroplasty | 6 | 4 | 11 | 2 | 2 | 6 |
| 5 | Breast surgery | 1 | 5 | 9 | 0 | 0 | 0 |
| 6 | Cardiac surgery | 1 | 4 | 8 | 0 | 1 | 0 |
| 7 | Gallbladder surgery | 0 | 4 | 1 | 0 | 1 | 0 |
| 8 | Prostatectomy | 0 | 0 | 3 | 0 | 0 | 1 |
Note:
Number of articles in all surgical journals covered by PubMed.
The publication of topic-in-title articles on chronic pain after surgery in the top 20 surgical journals is represented in Table 6. In 1991–2000 only two articles were published in the top surgical journals, but that dramatically increased (to 18) in 2001–2010. The TJSI calculated for herniorrhaphy (only for topic-in-title articles) was 36.7% in 2001–2010. That means that these articles published in the top 20 surgical journals constitute almost one-third of all articles published in journals covered by PubMed (>5000). However, the same index for the other seven surgeries was only 2.9%.
Table 6.
Top Journal Selectivity Index (TJSI) for representation of chronic pain as an adverse effect of surgery
| Topic of publications | Years | Number of articlesa | TJSI (ratio of top to all) | |
|---|---|---|---|---|
|
| ||||
| All journalsb (>5000) | Top specialty journalsc (20) | |||
| Chronic postsurgical pain: herniorrhaphy | 91–00 | 5 | 2 | |
| 01–10 | 49 | 18 | 36.7% | |
| Chronic postsurgical pain: seven specific surgeriesd | 91–00 | 45 | 1 | |
| 01–10 | 70 | 2 | 2.9% | |
Notes: TJSI represents the number of articles published in the top 20 journals to the number of articles in all journals covered by PubMed;11,12
Topic-in-title articles;
journals covered by PubMed;
top 20 surgical journals sorted by impact factor (journal citation report, 2010);
limb amputation, thoracic surgery, arthroplasty, breast surgery, cardiac surgery, gallbladder surgery, prostatectomy.
Textbooks
The textbook analysis is presented in Table 7. Only chronic pain after inguinal herniorrhaphy was present in all three surgical texts (but not in Miller’s Anesthesia). Greenfield’s Surgery mentioned chronic pain after three specific surgeries (more than the other texts in this regard); however, it did not include anything on chronic postsurgical pain in the chapters on basic principles. Orthopedic surgeries in general were included only in one of the three surgical texts; therefore, chronic pain after arthroplasty is not in the table. The number of chronic pain-related references varied from two to five in the surgical texts, and there were 12 references in Miller’s Anesthesia. The chronic pain-related figures or tables were absent in Sabiston Textbook of Surgery and Greenfield’s Surgery. There were two chronic pain-related tables in Schwartz’s Principles of Surgery. Miller’s Anesthesia included two figures and two tables related to chronic postsurgical pain. The total number of lines on chronic postsurgical pain was more or less similar: from 85 to 64 lines in the surgical texts and 100 lines in Miller’s Anesthesia. Taking into account that one page of the texts has approximately 120 lines and the total volume of the texts varies from 2000 to 3000 pages, the presentation of chronic pain after surgeries is almost negligible.
Table 7.
Presentation of chronic postsurgical pain in surgical textbooks
| Sabiston Textbook of Surgery, 2008 | Schwartz’s Principles of Surgery, 2009 | Greenfield’s Surgery, 2010 | Miller’s Anesthesia, 2010 | |
|---|---|---|---|---|
| Total number of pages | 2286 | 1776 | 2074 | 3084 |
| Total number of linesa on the topic | 85 | 70 | 64 | 100 |
| Total number of references on the topic | 4 | 2 | 5 | 12 |
| Presence of the topic in chapters | ||||
| Basic principles | + | + | − | + |
| Limb amputation | − | − | + | − |
| Thoracotomy | − | − | − | + |
| Coronary artery bypass grafting | − | − | − | + |
| Mastectomy | − | − | + | − |
| Inguinal herniorrhaphy | + | + | + | − |
Note:
Approximately 120 lines per page.
Discussion
The indices that were used in this study indicated that the topic of chronic postsurgical pain is represented insufficiently, especially in surgical journals. Only nine editorials on chronic postsurgical pain were published in 1981–2010, all in nonsurgical journals. The articles clearly announcing the problem of chronic postsurgical pain (topic-in-title articles) began to appear in significant numbers only relatively late, in 2001–2010; however, even during the last decade they were sevenfold fewer than articles on acute postsurgical pain. In 1991–2000 only two topic-in-title articles on chronic pain after surgery were published in the top 20 surgical journals. There was a clear sign that the interest in chronic postsurgical pain began to increase in 2001–2010, but only in one group of surgeries: herniorrhaphy. The topic-in-title articles in all journals with this type of surgery increased from five (1991–2000) to 49 (2001–2010). The increase in postherniorrhaphy pain reporting is in stark contrast to publications regarding other types of postsurgical pain, especially in surgical journals (Figure 2).
Figure 2.
Number of topic-in-title articles published in 1991–2000 and 2001–2010 periods on chronic pain after the four types of specific surgeries.a Notes: aAlong the vertical axis, the number (#) of articles published in all journals (including surgical journals), the number of articles published in surgical journals (including top 20 surgical journals), and the number of articles published in top 20 surgical journals (listed in the method section). Along the horizontal axis, the four types of specific surgeries with the highest number of published articles.
The most significant sign of insufficient representation of chronic postsurgical pain is found in the presentation of this topic in surgical textbooks (2008–2010 editions). The presentation of chronic postsurgical pain in less than a page for various groups of surgeries per 2000–3000 pages of a textbook is clearly inadequate. However, chronic pain after herniorrhaphy is reflected in all three surgical texts analyzed (mostly very briefly).
Over the 10 years since the publication of seminal papers presenting postsurgical chronic pain,4–6 an important change has occurred but only in one area: chronic pain after herniorrhaphy. TJSI for herniorrhaphy has reached 36.7% (Table 6). It means that approximately one-third of all articles on herniorrhaphy in all journals covered by PubMed were published in the top 20 surgical journals. TJSI represents the ratio of the number of articles in the top 20 journals of the specialty to the number of articles in all journals covered by PubMed (>5000). A surge of this index is the sign of rising interest in a publication topic. For some reason, the top journals respond more rapidly to new and important developments in a specialty.11,12,17 At a time when TJSI for chronic pain after herniorrhaphy was so high, it was ten times lower for seven other surgeries (2.9%), reflecting insignificant attention to chronic pain after these types of surgeries. Hopefully, the increased TJSI for herniorrhaphy indicates the initial change in the attitude toward chronic postsurgical pain in general and that it will soon spread to other groups of surgeries.
Such a change in attitude is necessary because of the vast number of patients with chronic postsurgical pain. Macrae3 gave some insight into the magnitude of the problem by taking the number of operations performed in the US in 1994 (only for seven groups of surgeries) and multiplying it by the lowest figures for the incidence of chronic pain for these surgeries. His calculations yielded a possible 394,000 cases of chronic postsurgical pain each year. The complete absence of editorials related to this problem in the 1990–2000 period clearly indicates that the attention of the medical community was not focused on this type of pain.
The main reason for the neglect of chronic postsurgical pain in surgical journals and textbooks was well described by Macrae in 2001: “It is hard for any doctor to accept that the treatments they offer may cause morbidity, especially if they feel that they may be to blame.”4 An additional reason might be that surgeons are less exposed to patients with developed chronic postsurgical pain than physicians in other specialties (eg, family medicine, pain medicine, neurology). At the same time, surgeons do have good reasons to feel that they are not to be blamed for chronic postsurgical pain. Although iatrogenic neuropathic pain caused by intraoperative nerve injury is the most common type of chronic postsurgical pain, this type of pain may also happen without any damage to a nerve trunk.8,9 In addition, nerve damage alone is usually not sufficient to cause chronic pain, because most of the cases of intraoperative nerve damage result in motor and sensory changes without the development of chronic pain. Chronic postsurgical pain is complex and poorly understood; there are many possible factors in its development (see reviews3,8,9).
It is accepted that chronic postsurgical pain is an inevitable consequence of surgery in a certain proportion of cases, like wound infection.3 Chronic postsurgical pain should be discussed openly, and correct information on risk should be given to prospective patients. The incidence of chronic postsurgical pain varies very widely, up to 80% with limb amputations.18 The Stabiston Textbook of Surgery13 indicates that chronic pain after open inguinal hernia repair has incidence ranging from 29% to 75%. A systematic review by Aasvang and Kehlet2 reported that the overall incidence of chronic pain after open inguinal herniorrhaphy is 18%. In a recent large prospective study, Aasvang et al19 found that the incidence of substantial pain 6 months after groin hernia repair was 12%. If patients had accurate information on their risk of chronic pain, they at least would be in the position to decide against an operation.
According to Kehlet et al,8 the analysis of all possible approaches for the prevention of chronic postsurgical pain yields only one reliable solution: to use surgical techniques that avoid nerve damage. In a subsequent study,19 these authors provided a rationale for selecting surgical techniques with a lower risk of chronic pain after groin hernia repair. They demonstrated that the incidence of “substantial pain” was significantly lower with laparoscopic than with open surgery (8.1% vs 16.0%, P < 0.02). A similar conclusion regarding chronic pain after laparoscopic versus open surgery was reached regarding cholecystectomy. Stiff et al20 indicated that right upper quadrant chronic pain was less common after laparoscopic surgery (3.4% vs 9.7%, P < 0.05).
Although chronic postsurgical pain is relevant to many specialties (eg, surgery, anesthesiology, neurology, pain medicine, and rehabilitation medicine), risk can be decreased only by surgeons, because only they can choose to use techniques with lower risk of nerve damage. Chronic postoperative pain can also include anesthesia-related nerve injuries. Cheney et al21 analyzed claims against anesthesiologists and found that 670 (16% of 4183) claims were for anesthesia-related nerve injury, including nerve injuries due to positioning of the patient after anesthesia induction. The most frequent sites of injury were the ulnar nerve (28%) and brachial plexus (20%).
Conclusion
In conclusion, chronic postsurgical pain is still insufficiently represented, especially in surgical journals and textbooks. However, there is an indication (rise in TJSI) that the interest in this topic began to increase. At present, the increase is mostly related to one specific group of surgeries: herniorrhaphy. However, it is likely that the change in the attitude toward chronic postsurgical pain will spread to other specific groups of surgeries.
Supplementary material
List of “topic-in-title” articles on chronic postsurgical pain (1981–2010)
- Aasvang E, Kehlet H. Surgical management of chronic pain after inguinal hernia repair. Br J Surg. 2005;92:795–801. doi: 10.1002/bjs.5103. [DOI] [PubMed] [Google Scholar]
- Aasvang EK, Bay-Neilsen M, Kehlet H. Pain and functional impairment 6 years after inguinal herniorrhaphy. Hernia. 2006;10:316–321. doi: 10.1007/s10029-006-0098-y. [DOI] [PubMed] [Google Scholar]
- Aasvang EK, Brandsborg B, Jensen TS, Kehlet H. Heterogeneous sensory processing in persistent postherniotomy pain. Pain. 2010;150:237–242. doi: 10.1016/j.pain.2010.03.025. [DOI] [PubMed] [Google Scholar]
- Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, et al. Predictive risk factors for persistent postherniotomy pain. Anesthesiology. 2010;112:957–969. doi: 10.1097/ALN.0b013e3181d31ff8. [DOI] [PubMed] [Google Scholar]
- Aasvang EK, Jensen KE, Fiirgaard B, Kehlet H. MRI and pathology in persistent postherniotomy pain. J Am Coll Surg. 2009;208:1023–1028. doi: 10.1016/j.jamcollsurg.2009.02.056. [DOI] [PubMed] [Google Scholar]
- Aasvang EK, Kehlet H. Chronic pain after childhood groin hernia repair. J Pediatr Surg. 2007;42:1403–1408. doi: 10.1016/j.jpedsurg.2007.03.042. [DOI] [PubMed] [Google Scholar]
- Aasvang EK, Kehlet H. The effect of mesh removal and selective neurectomy on persistent postherniotomy pain. Ann Surg. 2009;249:327–334. doi: 10.1097/SLA.0b013e31818eec49. [DOI] [PubMed] [Google Scholar]
- Alfieri S, Rotondi F, Di Giorfio A, Fumagalli U, Salzano A, Di Miceli D, et al. Groin Pain Trial Group. Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg. 2006;243:553–558. doi: 10.1097/01.sla.0000208435.40970.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amid PK, Hiatt JR. New understanding of the cause and surgical treatment of postherniorrhaphy inguinodynia and orchalgia. J Am Coll Surg. 2007;205:381–385. doi: 10.1016/j.jamcollsurg.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Asnis SE, Hanley S, Shelton PD. Sciatic neuropathy secondary to migration of trochanteric wire following total hip arthroplasty. Clin Orthop Relat Res. 1985;196:226–228. [PubMed] [Google Scholar]
- Bach S, Noreng MF, Tjellden NU. Phantom limb pain in amputees during the first 12 months following limb amputation, after preoperative lumbar epidural blockade. Pain. 1988;33:297–301. doi: 10.1016/0304-3959(88)90288-6. [DOI] [PubMed] [Google Scholar]
- Bay-Nielsen M, Perkins FM, Kehlet H. Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg. 2001;233:1–7. doi: 10.1097/00000658-200101000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisgaard T, Rosenberg J, Kehlet H. From acute to chronic pain after laparoscopic cholecystectomy: a prospective follow-up analysis. Scan J Gastroenterol. 2005;40:1358–1364. doi: 10.1080/00365520510023675. [DOI] [PubMed] [Google Scholar]
- Bittner R, Gmähle E, Gmähle B, Schwarz J, Aasvang E, Kehlet H. Lightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP) Surg Endosc. 2010;24:2958–2964. doi: 10.1007/s00464-010-1140-9. [DOI] [PubMed] [Google Scholar]
- Bosmans JC, Suurmeijer TP, Hulsink M, van der Schans CP, Geertzen JH, Dijkstra PU. Amputation phantom pain and subjective well-being: a qualitative study. Int J Rehabil Res. 2007;30:1–8. doi: 10.1097/MRR.0b013e328012c953. [DOI] [PubMed] [Google Scholar]
- Bower S, Moore BB, Weiss SM. Neuralgia after inguinal hernia repair. Am Surg. 1996;62:664–667. [PubMed] [Google Scholar]
- Bozuk M, Schuster R, Stewart D, Hicks K, Greaney G, Waxman K. Disability and chronic pain after open mesh and laparoscopic inguinal hernia repair. Am Surg. 2003;69:839–841. [PubMed] [Google Scholar]
- Brandsborg B, Nikolajsen L, Hansen CT, Kehlet H, Jensen TS. Risk factors for chronic pain after hysterectormy: a nationwide questionnaire and database study. Anesthesiology. 2007;106:1003–1012. doi: 10.1097/01.anes.0000265161.39932.e8. [DOI] [PubMed] [Google Scholar]
- Bruce J, Drury N, Poobalan AS, Jeffrey RR, Smith WC, Chambers WA. The prevalence of chronic chest and leg pain following cardiac surgery: a historical cohort study. Pain. 2003;104:265–273. doi: 10.1016/s0304-3959(03)00017-4. [DOI] [PubMed] [Google Scholar]
- Buvanendran A, Kroin JS, Della Valle CJ, Kari M, Moric M, Tuman KJ. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trial. Anesth Analg. 2010;110:199–207. doi: 10.1213/ANE.0b013e3181c4273a. [DOI] [PubMed] [Google Scholar]
- Callesen T, Bech K, Kehlet H. Prospective study of chronic pain after groin hernia repair. Br J Surg. 1999;86:1528–1531. doi: 10.1046/j.1365-2168.1999.01320.x. [DOI] [PubMed] [Google Scholar]
- Carle C, Ashworth A, Roscoe A. A survey of post-sternotomy chronic pain following cardiac surgery. Anaesthesia. 2009;64:1387. doi: 10.1111/j.1365-2044.2009.06169_1.x. [DOI] [PubMed] [Google Scholar]
- Casscells CD, Lindsey RW, Ebersole J, Li B. Ulnar neuropathy after median sternotomy. Clin Orthop Relat Res. 1993;291:259–265. [PubMed] [Google Scholar]
- Catchlove RF. Phantom pain following limb amputation in a paraplegic. A case report. Psychother Psychosom. 1983;39:89–93. doi: 10.1159/000287726. [DOI] [PubMed] [Google Scholar]
- Chauhan BM, Kim DJ, Wainapel SF. Saphenous neuropathy following coronary artery bypass surgery. N Y State J Med. 1981;81:222–223. [PubMed] [Google Scholar]
- Clarke H, Pereira S, Kennedy D, Andrion J, Mitsakakis N, Gollish J, et al. Adding gabapentin to a multimodal regimen does not reduce acute pain, opioid consumption or chronic pain after total hip arthroplasty. Acta Anaesthesiol Scand. 2009;53:1073–1083. doi: 10.1111/j.1399-6576.2009.02039.x. [DOI] [PubMed] [Google Scholar]
- Conacher ID. Percutaneous cryotherapy for post-thoracotomy neuralgia. Pain. 1986;25:227–228. doi: 10.1016/0304-3959(86)90097-7. [DOI] [PubMed] [Google Scholar]
- Conacher ID. Therapists and therapies for post-thoracotomy neuralgia. Pain. 1992;48:409–412. doi: 10.1016/0304-3959(92)90093-Q. [DOI] [PubMed] [Google Scholar]
- Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ. Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg. 2002;89:1310–1314. doi: 10.1046/j.1365-2168.2002.02206.x. [DOI] [PubMed] [Google Scholar]
- Crombie IK, Davies HT, Macrae WA. Cut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinic. Pain. 1998;76:167–171. [PubMed] [Google Scholar]
- Dajczman E, Gordon A, Kreisman H, Wolkove N. Long-term postthoracotomy pain. Chest. 1991;99:270–274. doi: 10.1378/chest.99.2.270. [DOI] [PubMed] [Google Scholar]
- De Kock M. Expanding our horizons: transition of acute postoperative pain to persistent pain and establishment of chronic postsurgical pain services. Anesthesiology. 2009;111:461–463. doi: 10.1097/ALN.0b013e3181afde28. [DOI] [PubMed] [Google Scholar]
- deJonge P, Lloyd A, Horsfall L, Tan R, O’Dwyer PJ. The measurement of chronic pain and health-related quality of life following inguinal hernia repair: a review of the literature. Hernia. 2008;12:561–569. doi: 10.1007/s10029-008-0412-y. [DOI] [PubMed] [Google Scholar]
- Dennis R, O’Riordan D. Risk factors for chronic pain after inguinal hernia repair. Ann R Coll Surg Engl. 2007;89:218–220. doi: 10.1308/003588407X178991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmond DM, Maclachlan M. Prevalence and characteristics of phantom limb pain and residual limb pain in the long term after upper limb amputation. Int J Rehabil Res. 2010;33:279–282. doi: 10.1097/MRR.0b013e328336388d. [DOI] [PubMed] [Google Scholar]
- DeVita MA, Robinson LR, Rehder J, Hattler B, Cohen C. Incidence and natural history of phrenic neuropathy occurring during open heart surgery. Chest. 1993;103:850–856. doi: 10.1378/chest.103.3.850. [DOI] [PubMed] [Google Scholar]
- Dijkstra PU, Geertzen JH, Stewart R, van der Schans CP. Phantom pain and risk factors: a multivariate analysis. J Pain Symptom Manage. 2002;24:578–585. doi: 10.1016/s0885-3924(02)00538-9. [DOI] [PubMed] [Google Scholar]
- Dijkstra PU, Reitman JS, Geertzen JH. Phantom breast sensations and phantom breast pain: a 2-year prospective study and a methodological analysis of literature. Eur J Pain. 2007;11:99–108. doi: 10.1016/j.ejpain.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Dualé C, Sibaud F, Guastella V, Vallet L, Gimbert YA, Taheri H, et al. Perioperative ketamine does not prevent chronic pain after thoracotomy. Eur J Pain. 2009;13:497–505. doi: 10.1016/j.ejpain.2008.06.013. [DOI] [PubMed] [Google Scholar]
- Ducic I, Mesbahi AN, Attinger CE, Graw K. The role of peripheral nerve surgery in the treatment of chronic pain associated with amputation stumps. Plast Reconstru Surg. 2008;121:908–914. doi: 10.1097/01.prs.0000299281.57480.77. [DOI] [PubMed] [Google Scholar]
- Eggers KA, Asai T. Postoperative brachial plexus neuropathy after total knee replacement under spinal anaesthesia. Br J Anaesth. 1995;75:642–644. doi: 10.1093/bja/75.5.642. [DOI] [PubMed] [Google Scholar]
- Ehde DM, Czerniecki JM, Smith DG, et al. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81:1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- Eklund A, Montgomery A, Bergkvist L, Rudberg C Swedish Multicentre Trial of Inguinal Hernia Repair by Laparoscopy (SMIL) study group. Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg. 2010;97:600–608. doi: 10.1002/bjs.6904. [DOI] [PubMed] [Google Scholar]
- Ellis K. A review of amputation phantom pain and nursing responsibilities. Br J Nurs. 2002;11:155–157. doi: 10.12968/bjon.2002.11.3.10063. [DOI] [PubMed] [Google Scholar]
- Erdek MA, Staats PS. Chronic pain and thoracic surgery. Thorac Surg Clin. 2005;15:123–130. doi: 10.1016/j.thorsurg.2004.10.001. [DOI] [PubMed] [Google Scholar]
- Erhan Y, Erhan E, Aydede H, Merean M, Tok D. Chronic pain after Lichtenstein and periotoneal (posterior) hernia repair. Can J Surg. 2008;51:383–387. [PMC free article] [PubMed] [Google Scholar]
- Fainsinger RL, deGara C, Perez GA. Amputation and the prevention of phantom pain. J Pain Symptom Manage. 2000;20:308–312. doi: 10.1016/s0885-3924(00)00184-6. [DOI] [PubMed] [Google Scholar]
- Fassoulaki A, Melemeni A, Staikou C, Triga A, Sarantopoulos C. Acute postoperative pain predicts chronic pain and long-term analgesic requirements after breast surgery for cancer. Acta Anaesthesiol Belg. 2008;59:241–248. [PubMed] [Google Scholar]
- Fassoulaki A, Sarantopoulos C, Melemeni A, Hogan Q. EMLA reduces acute and chronic pain after breast surgery for cancer. Reg Anesth Pain Med. 2000;25:350–355. doi: 10.1053/rapm.2000.7812. [DOI] [PubMed] [Google Scholar]
- Fassoulaki A, Triga A, Melemeni A, Sarantopoulos C. Multimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancer. Anesth Analg. 2005;101:1427–1432. doi: 10.1213/01.ANE.0000180200.11626.8E. [DOI] [PubMed] [Google Scholar]
- Ferzli GS, Edwards ED, Khoury GE. Chronic pain after inguinal herniorrhaphy. J Am Coll Surg. 2007;205:333–341. doi: 10.1016/j.jamcollsurg.2007.02.081. [DOI] [PubMed] [Google Scholar]
- Fischer SR, Christ DJ, Roehr BA. Sciatic neuropathy secondary to total hip arthroplasty wear debris. J Arthroplasty. 1999;14:771–774. doi: 10.1016/s0883-5403(99)90237-1. [DOI] [PubMed] [Google Scholar]
- Fisher K, Hanspal RS. Phantom pain, anxiety, depression, and their relation in consecutive patients with amputated limbs: case reports. BMJ. 1998;316:903–904. doi: 10.1136/bmj.316.7135.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flexman A, Ng J, Gelb A. Acute and chronic pain following craniotomy. Curr Opin Anaesthesiol. 2010;23:551–557. doi: 10.1097/ACO.0b013e32833e15b9. [DOI] [PubMed] [Google Scholar]
- Flor H, Birbaumer N. Phantom limb pain: cortical plasticity and novel therapeutic approaches. Curr Opin Anaesthesiol. 2000;13:561–564. doi: 10.1097/00001503-200010000-00013. [DOI] [PubMed] [Google Scholar]
- Flor H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002;1:182–189. doi: 10.1016/s1474-4422(02)00074-1. [DOI] [PubMed] [Google Scholar]
- Fokter SK, Repse-Fokter A, Takac I. Case report: femoral neuropathy secondary to total hip arthroplasty wear debris. Clin Orthop Relat Res. 2009;467:3032–3035. doi: 10.1007/s11999-009-0894-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franneby U, Gunnarsson U, Andersson M, et al. Validation of an inguinal pain questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg. 2008;95:488–493. doi: 10.1002/bjs.6014. [DOI] [PubMed] [Google Scholar]
- Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U. Risk factors for long-term pain after hernia surgery. Ann Surg. 2006;244:212–219. doi: 10.1097/01.sla.0000218081.53940.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher P, Allen D, Maclachlan M. Phantom limb pain and residual limb pain following lower limb amputation: a descriptive analysis. Disabil Rehabil. 2001;23:522–530. doi: 10.1080/09638280010029859. [DOI] [PubMed] [Google Scholar]
- Gerbershagen JH, Ozgur E, Dagtekin O, et al. Preoperative pain as a risk factor for chronic post-surgical pain – six month follow-up after radical prostatectomy. Eur J Pain. 2009 doi: 10.1016/j.ejpain.2008.11.020. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- Gillion JF, Fagniez PL. Chronic pain and cutaneous sensory changes after inguinal hernia repair: comparison between open and laparoscopic techniques. Hernia. 1999;3:75–80. [Google Scholar]
- Gjeilo KH, Klepstad P, Wahba A, Lydersen S, Stenseth R. Chronic pain after cardiac surgery: a prospective study. Acta Anaesthesiol Scand. 2010;54:70–78. doi: 10.1111/j.1399-6576.2009.02097.x. [DOI] [PubMed] [Google Scholar]
- Gotoda Y, Kambara N, Sakai T, et al. The morbidity, time course and predictive factors for persistent post-thoracotomy pain. Eur J Pain. 2001;5:89–96. doi: 10.1053/eujp.2001.0225. [DOI] [PubMed] [Google Scholar]
- Gottschalk A, Ochroch EA. Clinical and demographic characteristics of patients with chronic pain after major thoracotomy. Clin J Pain. 2008;24:708–716. doi: 10.1097/AJP.0b013e318174badd. [DOI] [PubMed] [Google Scholar]
- Granot M. Can we predict persistent postoperative pain by testing preoperative experimental pain? Curr Opin Anaesthesiol. 2009;22:425–430. doi: 10.1097/ACO.0b013e32832a40e1. [DOI] [PubMed] [Google Scholar]
- Grant AM, Scott NW, O’Dwyer PJ. Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair or groin hernia. Br J Surg. 2004;91:1570–1574. doi: 10.1002/bjs.4799. [DOI] [PubMed] [Google Scholar]
- Grant P, Reise O, Ovre S. Obturator neuropathy due to intrapelvic extrusion of cement during total hip replacement – report of 2 patients. Acta Orthop Scand. 2001;72:537–540. doi: 10.1080/000164701753532907. [DOI] [PubMed] [Google Scholar]
- Hanley MA, Jensen MP, Ehde DM, Hoffman AJ, Patterson DR, Robinson LR. Psychosocial predictors of long-term adjustment to lower-limb amputation and phantom limb pain. Disabil Rehabil. 2004;26:882–893. doi: 10.1080/09638280410001708896. [DOI] [PubMed] [Google Scholar]
- Hanley MA, Jensen MP, Smith DG, et al. Preamputation pain and acute pain predict chronic pain after lower extremity amputation. J Pain. 2007;8:102–109. doi: 10.1016/j.jpain.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Harden RN, Bruehl S, Stanos S, et al. Prospective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: a preliminary study. Pain. 2003;106:393–400. doi: 10.1016/j.pain.2003.08.009. [DOI] [PubMed] [Google Scholar]
- Hardy PA. Post-thoracotomy intercostal neuralgia. Lancet. 1986;1:626–627. doi: 10.1016/s0140-6736(86)92857-6. [DOI] [PubMed] [Google Scholar]
- Harvie P, Giele H, Fang C, et al. The treatment of femoral neuropathy due to pseudotumour caused by metal-on-metal resurfacing arthroplasty. Hip Int. 2008;18:313–320. doi: 10.1177/112070000801800408. [DOI] [PubMed] [Google Scholar]
- Hassan I, Jacobs AG, Baig ME, Van der Meyden CH. Bilateral axillary and suprascapular neuropathy after coronary artery bypass surgery. Cardiovasc J S Afr. 2006;17:259–261. [PubMed] [Google Scholar]
- Hayes C, Armstrong-Brown A, Burstal R. Perioperative intravenous ketamine infusion for the prevention of persistent post-amputation pain: A randomized, controlled trial. Anaesth Intensive Care. 2004;32:330–338. doi: 10.1177/0310057X0403200305. [DOI] [PubMed] [Google Scholar]
- Hazelrigg SR, Cetindag IB, Fullerton J. Acute and chronic pain syndromes after thoracic surgery. Surg Clin North Am. 2002;82:849–865. doi: 10.1016/s0039-6109(02)00031-2. [DOI] [PubMed] [Google Scholar]
- Hill A. Phantom limb pain: a review of the literature on attributes and potential mechanisms. J Pain Symptom Manage. 1999;17:125–142. doi: 10.1016/s0885-3924(98)00136-5. [DOI] [PubMed] [Google Scholar]
- Hinricha-Rocker A, Schulz K, Jarvinen I, et al. Psychosocial predictors and correlates for chronic postsurgical pain (CPSP): a systematic review. Eur J Pain. 2009;13:719–730. doi: 10.1016/j.ejpain.2008.07.015. [DOI] [PubMed] [Google Scholar]
- Hompes R, Vansteenkiste F, Pottel H, Devriendt D, Van Rooy F. Chronic pain after Kugel inguinal hernia repair. Hernia. 2008;12:127–132. doi: 10.1007/s10029-007-0295-3. [DOI] [PubMed] [Google Scholar]
- Houghton AD, Saadah E, Nicholls G, McColl L, Houghton AL. Phantom pain: natural history and association with rehabilitation. Ann R Coll Surg Engl. 1994;76:22–25. [PMC free article] [PubMed] [Google Scholar]
- Huse E, Larbig W, Birbaumer N, Flor H. Cortical reorganization and pain: empirical findings and therapeutic implication using example of phantom pain. Schmerz. 2001;15:131–137. doi: 10.1007/s004820170037. [DOI] [PubMed] [Google Scholar]
- Huse E, Larbig W, Flor H, Birbaumer N. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47–55. doi: 10.1016/s0304-3959(00)00385-7. [DOI] [PubMed] [Google Scholar]
- Huse E, Preissl H, Larbig W, Birbaumer N. Phantom limb pain. Lancet. 2001;358:1015. doi: 10.1016/S0140-6736(01)06144-X. [DOI] [PubMed] [Google Scholar]
- Iacono RP, Sandyk R, Bamford CR, Awerbuch G, Malone JM. Post-amputation phantom pain and autonomous stump movements responsive to doxepin. Funct Neurol. 1987;2:343–348. [PubMed] [Google Scholar]
- Iohom G, Abdalla H, O’Brien J, et al. The associations between severity of early postoperative pain, chronic postsurgical pain and plasma concentration of stable nitric oxide products after breast surgery. Anesth Analg. 2006;103:995–1000. doi: 10.1213/01.ANE.0000240415.49180.4A. [DOI] [PubMed] [Google Scholar]
- Jahangiri M, Jayatunga AP, Bradley JW, Dark CH. Prevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaine. Ann R Coll Surg Engl. 1994;76:324–326. [PMC free article] [PubMed] [Google Scholar]
- Jensen TS, Krebs B, Neilsen J, Rasmussen P. Immediate and long-term phantom limb pain in amputees: incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain. 1985;21:267–268. doi: 10.1016/0304-3959(85)90090-9. [DOI] [PubMed] [Google Scholar]
- Jensen TS, Krebs B, Nielsen J, Rasmussen P. Phantom limb, phantom pain and stump pain in amputees during the first 6 months following limb amputation. Pain. 1983;17:243–256. doi: 10.1016/0304-3959(83)90097-0. [DOI] [PubMed] [Google Scholar]
- Jess P, Jess T, Beck H, Bech P. Neuroticism in relation to recovery and persisting pain after laparoscopic cholecystectomy. Scand J Gastroenterol. 1998;33:550–553. doi: 10.1080/00365529850172151. [DOI] [PubMed] [Google Scholar]
- Jorgensen T, Teglbjerg JS, Wille-Jorgensen P, Bille T, Thorvaldsen P. Persisting pain after cholecystectomy. A prospective investigation. Scand J Gastroenterol. 1991;26:124–128. doi: 10.3109/00365529108996493. [DOI] [PubMed] [Google Scholar]
- Kairaluoma PM, Bachmann MS, Rosenberg PH, Pere PJ. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg. 2006;103:703–708. doi: 10.1213/01.ane.0000230603.92574.4e. [DOI] [PubMed] [Google Scholar]
- Kalliomäki ML, Meyerson J, Gunnarsson U, Gordh T, Sandblom G. Long-term pain after inguinal hernia repair in a population-based cohort; risk factors and interference with daily activities. Eur J Pain. 2008;12:214–225. doi: 10.1016/j.ejpain.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Kalso E, Mennander S, Tasmuth T, Nilsson E. Chronic post-sternotomy pain. Acta Anaesthesiol Scand. 2001;45:935–939. doi: 10.1034/j.1399-6576.2001.450803.x. [DOI] [PubMed] [Google Scholar]
- Katz J. Phantom limb pain. Lancet. 1997;350:1338–1339. doi: 10.1016/S0140-6736(05)65130-6. [DOI] [PubMed] [Google Scholar]
- Katz J. Prevention of phantom limb pain by regional anaesthesia. Lancet. 1997;349:519–520. doi: 10.1016/s0140-6736(97)80081-5. [DOI] [PubMed] [Google Scholar]
- Katz J, Asmundson GJ, McRae K, Halket E. Emotional numbing and pain intensity predict the development of pain disability up to one year after lateral thoracotomy. Eur J Pain. 2009;13:870–878. doi: 10.1016/j.ejpain.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Katz J, Cohen L. Preventive analgesia is associated with reduced pain disability 3 weeks but not 6 months after major gynecologic surgery by laparotomy. Anesthesiology. 2004;101:169–174. doi: 10.1097/00000542-200407000-00026. [DOI] [PubMed] [Google Scholar]
- Katz J, Jackson M, Kavanagh BP, Sandler AN. Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. Clin J Pain. 1996;12:50–55. doi: 10.1097/00002508-199603000-00009. [DOI] [PubMed] [Google Scholar]
- Katz J, Melzack R. Pain ‘memories’ in phantom limbs: review and clinical observations. Pain. 1990;43:319–336. doi: 10.1016/0304-3959(90)90029-D. [DOI] [PubMed] [Google Scholar]
- Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9:723–744. doi: 10.1586/ern.09.20. [DOI] [PubMed] [Google Scholar]
- Katz J, Schmid R, Snijdelaar DG, Coderre TJ, McCartney CJ, Wowk A. Pre-emptive analgesia using intravenous fentanyl plus low-dose ketamine for radical prostatectomy under general anesthesia does not produce short-term or long-term reductions in pain or analgesic use. Pain. 2004;110:707–718. doi: 10.1016/j.pain.2004.05.011. [DOI] [PubMed] [Google Scholar]
- Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- Kehlet H. Chronic pain after groin hernia repair. Br J Surg. 2008;95:135–136. doi: 10.1002/bjs.6111. [DOI] [PubMed] [Google Scholar]
- Keller JE, Stefanidis D, Dolce CJ, Iannitti DA, Kercher KW, Heniford BT. Combined open and laparoscopic approach to chronic pain after inguinal hernia repair. Am Surg. 2008;74:695–700. [PubMed] [Google Scholar]
- Keller SM, Carp NZ, Levy MN, Rosen SM. Chronic post thoracotomy pain. J Cardiovasc Surg. 1994;35:161–164. [PubMed] [Google Scholar]
- Kempster P, Gates P, Byrne E, Wilson A. Painful sciatic neuropathy following cardiac surgery. Aust N Z J Med. 1991;21:732–735. doi: 10.1111/j.1445-5994.1991.tb01378.x. [DOI] [PubMed] [Google Scholar]
- Köninger J, Redecke J, Butters M. Chronic pain after hernia repair: a randomized trial comparing Shouldice, Lichtenstein and TAPP. Langenbecks Arch Surg. 2004;389:361–365. doi: 10.1007/s00423-004-0496-5. [DOI] [PubMed] [Google Scholar]
- Krane EJ, Keller LB. The prevalence of phantom limb sensation and pain pediatric amputees. J Pain Symptom Manage. 1995;10:21–29. doi: 10.1016/0885-3924(94)00062-P. [DOI] [PubMed] [Google Scholar]
- Kristensen AD, Pedersen TA, Hjortdal VE, Jensen TS, Nikolajsen L. Chronic pain in adults after thoracotomy in childhood or youth. Br J Anaesth. 2010;104:75–79. doi: 10.1093/bja/aep317. [DOI] [PubMed] [Google Scholar]
- Kroner K, Krebs B, Skov J, Jorgensen HS. Immediate and long-term phantom breast syndrome after mastectomy: incidence, clinical characteristics and relationship to pre-mastectomy breast pain. Pain. 1989;36:327–334. doi: 10.1016/0304-3959(89)90092-4. [DOI] [PubMed] [Google Scholar]
- Lambert A, Dashfield A, Cosgrove C, et al. Randomized prospective study comparing preoperative epidural and intraoperative perineural analgesia for the prevention of postoperative stump and phantom limb pain following major amputation. Reg Anesth Pain Med. 2001;26:316–321. doi: 10.1053/rapm.2001.23934. [DOI] [PubMed] [Google Scholar]
- Landreneau RJ, Mack MJ, Hazelrigg SR, Naunheim K, Dowling RD, Ritter P, et al. Prevalence of chronic pain after pulmonary resection by thoracotomy or video-assisted thoracic surgery. J Thorac Cardiovasc Surg. 1994;107:1079–1085. doi: 10.1097/00132586-199412000-00051. [DOI] [PubMed] [Google Scholar]
- Lau H, Patil NG, Yuen WK, Lee F. Prevalence and severity of chronic groin pain after endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc. 2003;17:1620–1623. doi: 10.1007/s00464-002-8798-6. [DOI] [PubMed] [Google Scholar]
- Lautenbacher S, Huber C, Schofer D, Kunz M, Parthum A, Weber PG, et al. Attentional and emotional mechanisms related to pain as predictors of chronic postoperative pain: a comparison with other psychological and physiological predictors. Pain. 2010;151:722–731. doi: 10.1016/j.pain.2010.08.041. [DOI] [PubMed] [Google Scholar]
- Lavand’homme P, De Kock M. The use of intraoperative epidural or spinal analgesia modulates postoperative hyperalgesia and reduces residual pain after major abdominal surgery. Acta Anaesthesiol Belg. 2008;57:373–379. [PubMed] [Google Scholar]
- Leslie TA, Illing RO, Cranston DW, Guillebaud J. The incidence of chronic scrotal pain after vasectomy: a prospective audit. BJU Int. 2007;100:1330–1333. doi: 10.1111/j.1464-410X.2007.07128.x. [DOI] [PubMed] [Google Scholar]
- Loftus LS, Laronga C. Evaluating patients with chronic pain after breast cancer surgery: the search for relief. JAMA. 2009;302:2034–2035. doi: 10.1001/jama.2009.1642. [DOI] [PubMed] [Google Scholar]
- Loos MJ, Scheltinga MR, Mulders LG, Roumen RM. The Pfannensteil incision as a source of chronic pain. Obstet Gynecol. 2008;111:839–846. doi: 10.1097/AOG.0b013e31816a4efa. [DOI] [PubMed] [Google Scholar]
- Loos MJ, Verhagen T, Scheltinga MR, Roumen RM. A randomised controlled trial of injection therapy versus neurectomy for post-herniorrhaphy inguinal neuralgia: rationale and study design. Hernia. 2010;14:593–597. doi: 10.1007/s10029-010-0697-5. [DOI] [PubMed] [Google Scholar]
- Lundblad H, Kreicbergs A, Jansson KA. Prediction of persistent pain after total knee replacement for osteoarthritis. J Bone Joint Surg Br. 2008;90:166–171. doi: 10.1302/0301-620X.90B2.19640. [DOI] [PubMed] [Google Scholar]
- Macrae WA. Chronic pain after sternotomy. Acta Anaesthesiol Scand. 2001;45:927–928. doi: 10.1034/j.1399-6576.2001.450801.x. [DOI] [PubMed] [Google Scholar]
- Macrae WA. Chronic pain after surgery. Br J Anaesth. 2001;87:88–98. doi: 10.1093/bja/87.1.88. [DOI] [PubMed] [Google Scholar]
- Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101:77–86. doi: 10.1093/bja/aen099. [DOI] [PubMed] [Google Scholar]
- Maguire MF, Latter JA, Mahajan R, Beggs D, Duffy JP. A study exploring the role of intercostal nerve damage in chronic pain after thoracic surgery. Eur J Cardiothorac Surg. 2006;29:873–879. doi: 10.1016/j.ejcts.2006.03.031. [DOI] [PubMed] [Google Scholar]
- Maguire MF, Ravenscroft A, Beggs D, Duffy JP. A questionnaire study investigating the prevalence of the neuropathic component of chronic pain after thoracic surgery. Eur J Cardiothorac Surg. 2006;29:800–805. doi: 10.1016/j.ejcts.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Manikandan R, Srirangam SJ, Pearson E, Collins GN. Early and late morbidity after vasectomy: a comparison of chronic scrotal pain at 1 and 10 years. BJU Int. 2004;93:571–574. doi: 10.1111/j.1464-410x.2003.04663.x. [DOI] [PubMed] [Google Scholar]
- Manny TB, Gorbachinsky I, Hemal AK. Lower extremity neuropathy after robot assisted laparoscopic radical prostatectomy and radical cystectomy. Can J Urol. 2010;17:5390–5393. [PubMed] [Google Scholar]
- Mazzoleni R, Vokaer M, Mavroudakis N, Bartholomé EJ, Bier JC. Antiphospholipid antibodies and ischemic neuropathy following cardiac surgery. Acta Neurol Belg. 2003;103:176–178. [PubMed] [Google Scholar]
- McMahon AJ, Buckley J, Taylor A, Lloyd SN, Dean RF, Kirk D. Chronic testicular pain following vasectomy. Br J Urol. 1992;69:188–191. doi: 10.1111/j.1464-410x.1992.tb15494.x. [DOI] [PubMed] [Google Scholar]
- Melamed NB, Stya-Murti S. Obturator neuropathy after total hip replacement. Ann Neurol. 1983;13:578–579. doi: 10.1002/ana.410130519. [DOI] [PubMed] [Google Scholar]
- Meyerson J, Thelin S, Gordh T, Karlsten R. The incidence of chronic post-sternotomy pain after cardiac surgery – a prospective study. Acta Anaesthesiol Scand. 2001;45:940–944. doi: 10.1034/j.1399-6576.2001.450804.x. [DOI] [PubMed] [Google Scholar]
- Mikkelsen T, Werner MU, Lassen B, Kehlet H. Pain and sensory dysfunction 6 to 12 months after inguinal herniotomy. Anesth Analg. 2004;99:146–151. doi: 10.1213/01.ANE.0000115147.14626.C5. [DOI] [PubMed] [Google Scholar]
- Miles J. Prevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaine. Ann R Coll Surg Engl. 1995;77:71. [PMC free article] [PubMed] [Google Scholar]
- Modirian E, Shojaei H, Soroush MR, Masoumi M. Phantom pain in bilateral upper limb amputation. Disabil Rehabil. 2009;31:1878–1881. doi: 10.1080/09638280902810976. [DOI] [PubMed] [Google Scholar]
- Mulvey MR, Bagnall AM, Johnson MI, Marchant PR. Transcutaneous electrical nerve stimulation (TENS) for phantom pain and stump pain following amputation in adults. Cochrane Database Syst Rev. 2010;12:CD007264. doi: 10.1002/14651858.CD007264.pub2. [DOI] [PubMed] [Google Scholar]
- Myers MA, Harmon RL. Sacral plexopathy and sciatic neuropathy after total knee arthroplasty. Electromyogr Clin Neurophysiol. 1998;38:423–426. [PubMed] [Google Scholar]
- Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R. Chronic pain after mesh repair of inguinal hernia: a systemative review. Am J Surg. 2007;194:394–400. doi: 10.1016/j.amjsurg.2007.02.012. [DOI] [PubMed] [Google Scholar]
- Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H. Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand. 2006;50:495–500. doi: 10.1111/j.1399-6576.2006.00976.x. [DOI] [PubMed] [Google Scholar]
- Nikolajsen L, Ilkjaer S, Christensen JH, Kroner K, Jensen TS. Randomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputation. Lancet. 1997;350(9088):1353–1357. doi: 10.1016/S0140-6736(97)06315-0. [DOI] [PubMed] [Google Scholar]
- Nikolajsen L, Ilkjaer S, Kroner K, Christensen JH, Jensen TS. The influence of preamputation pain on postamputation stump and phantom pain. Pain. 1997;72:393–405. doi: 10.1016/s0304-3959(97)00061-4. [DOI] [PubMed] [Google Scholar]
- Nikolajsen L, Kristensen AD, Thillemann TM, et al. Pain and somatosensory findings in patients 3 years after total hip arthroplasty. Eur J Pain. 2009;13:576–581. doi: 10.1016/j.ejpain.2008.06.016. [DOI] [PubMed] [Google Scholar]
- Nikolajsen L, Sorensen HC, Jensen TS, Kehlet H. Chronic pain following Caesarean section. Acta Anaesthesiol Scand. 2004;48:111–116. doi: 10.1111/j.1399-6576.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- Nunchuck S, Keenan RJ, Ferson PF. Prevalence of chronic pain after pulmonary resection by thoracotomy or video-assisted thoracic surgery. J Thorac Cardiovasc Surg. 1994;107:1079–1085. doi: 10.1097/00132586-199412000-00051. [DOI] [PubMed] [Google Scholar]
- O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G. Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg. 2005;92:166–167. doi: 10.1002/bjs.4833. [DOI] [PubMed] [Google Scholar]
- Obata H, Salto S, Fujita N, Fuse Y, Ishizaki K, Goto F. Epidural block with mepivacaine before surgery reduces long-term post-thoracotomy pain. Can J Anaesth. 1999;46:1127–1132. doi: 10.1007/BF03015520. [DOI] [PubMed] [Google Scholar]
- Oberg E, Jacobsen B, Rosenberg J. Chronic pain and recurrence after laparoscopic inguinal herniorrhaphy. Surg Laparosc Endosc Percutan Tech. 2005;15:267–269. doi: 10.1097/01.sle.0000183256.27303.07. [DOI] [PubMed] [Google Scholar]
- Ochroch EA, Gottschalk A, Augostides J, et al. Long-term pain and activity during recovery from major thoracotomy using thoracic epidural analgesia. Anesthesiology. 2002;97:1234–1244. doi: 10.1097/00000542-200211000-00029. [DOI] [PubMed] [Google Scholar]
- Paajanen H. A single-surgeon randomized trial comparing three composite meshes on chronic pain after Lichtenstein hernia repair in local anesthesia. Hernia. 2007;11:335–339. doi: 10.1007/s10029-007-0236-1. [DOI] [PubMed] [Google Scholar]
- Paily A, Thornton M. Chronic pain following a Lichtenstein inguinal hernia repair: a clinical and legal dilemma. ANZ J Surg. 2009;79:517–520. doi: 10.1111/j.1445-2197.2009.04980.x. [DOI] [PubMed] [Google Scholar]
- Perttunen K, Tasmuth T, Kalso E. Chronic pain after thoracic surgery: a follow-up study. Acta Anaesthesiol Scan. 1999;43:563–567. doi: 10.1034/j.1399-6576.1999.430513.x. [DOI] [PubMed] [Google Scholar]
- Pess GM, Lusskin R, Waugh TR, Battista AE. Femoral neuropathy secondary to pressurized cement in total hip replacement: treatment by decompression and neurolysis. Report of a case. J Bone Joint Surg Am. 1987;69:623–625. [PubMed] [Google Scholar]
- Pinzur MS. Sciatic nerve block for residual limb pain following below-knee amputation. Contemp Orthop. 1991;22:290–292. [PubMed] [Google Scholar]
- Pluijms WA, Steegers MA, Verhagaen AF, Scheffer GJ, Wilder-Smith OH. Chronic post-thoracotomy pain: a retrospective study. Acta Anaesthesiol Scan. 2006;50:804–808. doi: 10.1111/j.1399-6576.2006.01065.x. [DOI] [PubMed] [Google Scholar]
- Poleshuck EL, Katz J, Andrus CH, et al. Risk factors for chronic pain following breast cancer surgery: a prospective study. J Pain. 2006;7:626–634. doi: 10.1016/j.jpain.2006.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg. 2001;88:1122–1126. doi: 10.1046/j.0007-1323.2001.01828.x. [DOI] [PubMed] [Google Scholar]
- Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003;19:48–54. doi: 10.1097/00002508-200301000-00006. [DOI] [PubMed] [Google Scholar]
- Porter SS, Black DL, Rechling FW, Mason J. Intraoperative cortical somatosensory evoked potentials for detection of sciatic neuropathy during total hip arthroplasty. J Clin Anesth. 1989;1:170–176. doi: 10.1016/0952-8180(89)90037-8. [DOI] [PubMed] [Google Scholar]
- Rho RH, Lamer TJ, Fulmer JT. Treatment of genitofemoral neuralgia after laparoscopic inguinal herniorrhaphy with fluoroscopically guided tack injection. Pain Med. 2001;2:230–233. doi: 10.1046/j.1526-4637.2001.01032.x. [DOI] [PubMed] [Google Scholar]
- Richardson C, Glenn S, Horgan M, Nurmikko T. A prospective study of factors associated with the presence of phantom limb pain six months after major lower limb amputation in patients with peripheral vascular disease. J Pain. 2007;8:793–801. doi: 10.1016/j.jpain.2007.05.007. [DOI] [PubMed] [Google Scholar]
- Richardson C, Glenn S, Nurmikko T, Horgan M. Incidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular disease. Clin J Pain. 2006;22:353–358. doi: 10.1097/01.ajp.0000177793.01415.bd. [DOI] [PubMed] [Google Scholar]
- Richardson J, Sabanathan S, Mearns AJ, Sides C, Goulden CP. Post-thoracotomy neuralgia. Pain Clin. 1994;7:87–97. [Google Scholar]
- Richardson J. Chronic pain after thoracic surgery. Acta Anaesthesiol. Scand. 2000;44:220. doi: 10.1034/j.1399-6576.2000.440215.x. [DOI] [PubMed] [Google Scholar]
- Romundstad L, Breivik H, Roald H, et al. Chronic pain and sensory changes after augmentation mammoplasty: long term effects of preincisional administration of methylprednisolone. Pain. 2006;124:92–99. doi: 10.1016/j.pain.2006.03.020. [DOI] [PubMed] [Google Scholar]
- Rosen MJ, Novitsky YW, Cobb WS, Kercher KW, Heniford BT. Combined open and laparoscopic approach to chronic pain following open inguinal hernia repair. Hernia. 2006;10:20–24. doi: 10.1007/s10029-005-0032-8. [DOI] [PubMed] [Google Scholar]
- Rozen D, Ahn J. Pulsed radiofrequency for the treatment of ilioinguinal neuralgia after inguinal herniorrhaphy. Mt Sinai J Med. 2006;73:716–718. [PubMed] [Google Scholar]
- Schley MN, Topofner S, Weich K, et al. Continuous brachial plexus blockade in combination with the NMDA receptor antagonist-memantine prevents phantom pain in acute traumatic upper limb amputees. Eur J Pain. 2007;11:299–308. doi: 10.1016/j.ejpain.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Schwab R, Willms A, Kroger A, Becker HP. Less chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repair. Hernia. 2006;10:272–277. doi: 10.1007/s10029-006-0080-8. [DOI] [PubMed] [Google Scholar]
- Searle RD, Simpson MP, Simpson KH, Milton R, Bennett MI. Can chronic neuropathic pain following thoracic surgery be predicted during the postoperative period? Interact Cardiovasc Thorac Surg. 2009;9:999–1002. doi: 10.1510/icvts.2009.216887. [DOI] [PubMed] [Google Scholar]
- Seid AS, Amos E. Entrapment neuropathy in laparoscopic herniorrhaphy. Surg Endosc. 1994;8:1050–1053. doi: 10.1007/BF00705717. [DOI] [PubMed] [Google Scholar]
- Sen H, Sizlan A, Yanarates O, Senol MG, Inangil G, Sücüllü I, et al. The effects of gabapentin on acute and chronic pain after inguinal herniorrhaphy. Eur J Anaesthesiol. 2009;26:772–776. doi: 10.1097/EJA.0b013e32832ad2fa. [DOI] [PubMed] [Google Scholar]
- Senturk M, Ozcan PE, Talu GK, et al. The effects of three different analgesia techniques on long-term postthoracotomy pain. Anesth Analg. 2002;94:11–15. doi: 10.1213/00000539-200201000-00003. [DOI] [PubMed] [Google Scholar]
- Sheridan PH, Jr, Cheriyan A, Doud J, Dornseif SE, Montoya A, Houck J, et al. Incidence of phrenic neuropathy after isolated lung transplantation. The Loyola University Lung Transplant Group. J Heart Lung Transplant. 1995;14:684–691. [PubMed] [Google Scholar]
- Sherman RA, Sherman CJ, Parker L. Chronic phantom and stump pain among American veterans: results of a survey. Pain. 1984;18:83–95. doi: 10.1016/0304-3959(84)90128-3. [DOI] [PubMed] [Google Scholar]
- Simmons C, Jr, Izant TH, Rothman RH, Booth RE, Jr, Balderston RA. Femoral neuropathy following total hip arthroplasty. Anatomic study, case reports and literature review. J Arthroplasty. 1991;6:557–566. [PubMed] [Google Scholar]
- Singh K, Phillips FM, Kuo E, Campbell M. A prospective, randomized double-blind study of the efficacy of postoperative continuous local anesthetic infusion at the iliac crest bone graft site after posterior spinal arthrodesis: a minimum of 4-year follow-up. Spine. 2007;32:2790–2796. doi: 10.1097/BRS.0b013e31815b7650. [DOI] [PubMed] [Google Scholar]
- Skandalakis JE, Skandalakis LJ, Colborn GL. Testicular atrophy and neuropathy in herniorrhaphy. Am Surg. 1996;62:775–782. [PubMed] [Google Scholar]
- Smeds S, Kald A, Löfström L. Chronic pain after open inguinal hernia repair: a longitudinal self-assessment study. Hernia. 2010;14:249–252. doi: 10.1007/s10029-009-0615-x. [DOI] [PubMed] [Google Scholar]
- Smith DG, Ehde DM, Hanley MA, et al. Efficacy of gabapentin in treating chronic phantom limb and residual limb pain. J Rehabil Res Dev. 2005;42:645–654. doi: 10.1682/jrrd.2005.05.0082. [DOI] [PubMed] [Google Scholar]
- Smith DG, Ehde DM, Legro MW, Reiber GE, del Aguila M, Boone DA. Phantom pain, residual limb, and back pain after lower extremity amputations. Clin Orthoped Relat Res. 1999;361:29–38. doi: 10.1097/00003086-199904000-00005. [DOI] [PubMed] [Google Scholar]
- Smith J, Thompson JM. Phantom limb pain and chemotherapy in pediatric amputees. Mayo Clinic Proc. 1995;70:357–364. doi: 10.4065/70.4.357. [DOI] [PubMed] [Google Scholar]
- Smith WCS, Bourne D, Squair J, Phillips DO, Chambers WA. A retrospective cohort study of post mastectomy pain syndrome. Pain. 1999;83:91–95. doi: 10.1016/s0304-3959(99)00076-7. [DOI] [PubMed] [Google Scholar]
- Solak O, Metin M, Esme H, et al. Effectiveness of gabapentin in the treatment of chronic post-thoracotomy pain. Eur J Cardiothorac Surg. 2007;32:9–12. doi: 10.1016/j.ejcts.2007.03.022. [DOI] [PubMed] [Google Scholar]
- Staerkle RF, Buchli C, Villiger P. Patient satisfaction, hernia recurrence rate, and chronic pain. 10 years after endoscopic total extraperitoneal inguinal hernia repair. Surg Laparosc Endosc Percutan Tech. 2009;19:405–409. doi: 10.1097/SLE.0b013e3181bb1bce. [DOI] [PubMed] [Google Scholar]
- Steegers MA, Snik DM, Verhagen AF, van der Drift MA, Wilder-Smith OH. Only half of the chronic pain after thoracic surgery shows a neuropathic component. J Pain. 2008;9:955–961. doi: 10.1016/j.jpain.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Stevens PE, Dibble SL, Miaskowski C. Prevalence, characteristics, and impact of postmastectomy pain syndrome: an investigation of women’s experiences. Pain. 1995;61:61–68. doi: 10.1016/0304-3959(94)00162-8. [DOI] [PubMed] [Google Scholar]
- Stiff G, Rhodes M, Kelly A, Telford K, Armstrong CP, Rees BI. Long-term pain: Less common after laparoscopic than open cholecystectomy. Br J Surg. 1994;81:1368–1370. doi: 10.1002/bjs.1800810939. [DOI] [PubMed] [Google Scholar]
- Stremmel C, Horn C, Eder S, Dimmler A, Lang W. The impact of immunological parameters on the development of phantom pain after major amputation. Eur J Vasc Endovasc Surg. 2005;30:79–82. doi: 10.1016/j.ejvs.2005.02.050. [DOI] [PubMed] [Google Scholar]
- Swanson AJG. The incidence of prepatellar neuropathy following medial meniscectomy. Clin Orthop Rel Res. 1983;181:151–153. [PubMed] [Google Scholar]
- Swenson JD, Bull DA. Postoperative ulnar neuropathy associated with prolonged ischemia in the upper extremity during coronary artery bypass surgery. Anesth Analg. 1997;85:1275–1277. doi: 10.1097/00000539-199712000-00017. [DOI] [PubMed] [Google Scholar]
- Tani Y, Miyawaki H. Femoral neuropathy caused by reinforcement ring malposition and extruded bone-cement after revision total hip arthroplasty. J Arthroplasty. 2002;17:516–518. doi: 10.1054/arth.2002.31085. [DOI] [PubMed] [Google Scholar]
- Tasmuth T, Kataja M, Blomqvist C, von Smitten K, Kalso E. Treatment-related factors predisposing to chronic pain in patients with breast cancer – a multivariate approach. Acta Oncol. 1997;36:625–630. doi: 10.3109/02841869709001326. [DOI] [PubMed] [Google Scholar]
- Tasmuth T, von Smitten K, Kalso E. Pain and other symptoms during first year after radical and conservative surgery for breast cancer. Br J Cancer. 1996;74:2024–2031. doi: 10.1038/bjc.1996.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hanswijck de Jonge P, Lloyd A, Horsfall L, Tan R, O’Dwyer PJ. The measurement of chronic pain and health-related quality of life following inguinal hernia repair: a review of the literature. Hernia. 2008;12:561–569. doi: 10.1007/s10029-008-0412-y. [DOI] [PubMed] [Google Scholar]
- van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J. Randomized clinical trial of mesh versus non-mesh primary inguinal hernia repair: long-term chronic pain at 10 years. Surgery. 2007;142:695–698. doi: 10.1016/j.surg.2007.05.019. [DOI] [PubMed] [Google Scholar]
- Vik H, Andersen KJ, Julshamn K, Todnem K. Neuropathy caused by silver absorption from arthroplasty cement. Lancet. 1985;8433:872. doi: 10.1016/s0140-6736(85)92230-5. [DOI] [PubMed] [Google Scholar]
- Vilholm OJ, Cold S, Rasmussen L, Sindrup SH. The postmastectomy pain syndrome: an epidemiological study on the prevalence of chronic pain after surgery for breast cancer. Br J Cancer. 2008;99:604–610. doi: 10.1038/sj.bjc.6604534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser E. Chronic postsurgical pain: epidemiology and clinical implications for acute pain management. Acute Pain. 2006;8:73–81. [Google Scholar]
- Vuilleumier H, Hübner M, Demartines N. Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg. 2009;33:841–845. doi: 10.1007/s00268-008-9869-1. [DOI] [PubMed] [Google Scholar]
- Wang J, Singh A, Higgins L, Warner J. Suprascapular neuropathy secondary to reverse shoulder arthroplasty: a case report. J Shoulder Elbow Surg. 2010;19:e5–e8. doi: 10.1016/j.jse.2009.10.004. [DOI] [PubMed] [Google Scholar]
- Wartan SW, Hamann W, Wedley JR, McColl I. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652–659. doi: 10.1093/bja/78.6.652. [DOI] [PubMed] [Google Scholar]
- Wassenaar EB, Raymakers JT, Rakic S. Removal of transabdominal sutures for chronic pain after laparoscopic ventral and incisional hernia repair. Surg Laparosc Endosc Percutan Tech. 2007;17:514–516. doi: 10.1097/SLE.0b013e3181462b9e. [DOI] [PubMed] [Google Scholar]
- Weiss SA, Lindell B. Phantom limb pain and etiology of amputation in unilateral lower extremity amputees. J Pain Symptom Manage. 1996;11:3–17. doi: 10.1016/0885-3924(95)00133-6. [DOI] [PubMed] [Google Scholar]
- Wicksell RK, Olsson GL. Predicting and preventing chronic postsurgical pain and disability. Anesthesiology. 2010;113:1260–1281. doi: 10.1097/ALN.0b013e3181da89f8. [DOI] [PubMed] [Google Scholar]
- Wijsmuller AR, Lange JFM, van Geldere D, Simons MP, Kleinrensink GJ, Hop WC, et al. Surgical techniques preventing chronic pain after Lichtenstein hernia repair: state-of-the-arts daily practice in the Netherlands. Hernia. 2007;11:147–151. doi: 10.1007/s10029-006-0177-0. [DOI] [PubMed] [Google Scholar]
- Wilder-Smith OH, Schreyer T, Scheffer GJ, Arendt-Neilsen L. Patients with chronic pain after abdominal surgery show less preoperative endogenous pain inhibition and more postoperative hyperalgesia: a pilot study. J Pain Palliat Care Pharmacother. 2010;24:119–128. doi: 10.3109/15360281003706069. [DOI] [PubMed] [Google Scholar]
- Wildgaard K, Iversen M, Kehet H. Chronic pain after lung transplantation: a nationwide study. Clin J Pain. 2010;26:217–222. doi: 10.1097/AJP.0b013e3181b705e4. [DOI] [PubMed] [Google Scholar]
- Wilson JA, Nimmo AF, Fleetwood-Walker SM, Colvin LA. A randomised double blind trial of the effect of pre-emptive epidural ketamine on persistent pain after lower limb amputation. Pain. 2008;135:108–118. doi: 10.1016/j.pain.2007.05.011. [DOI] [PubMed] [Google Scholar]
- Wright D, Paterson C, Scott N, Hair A, O’Dwyer PJ. Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg. 2002;235:333–337. doi: 10.1097/00000658-200203000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarnitsky D, Cripsel Y, Eisenberg E, et al. Prediction of chronic post-operative pain: pre-operative DNIC testing identifies patients at risk. Pain. 2008;138:22–28. doi: 10.1016/j.pain.2007.10.033. [DOI] [PubMed] [Google Scholar]
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pizzo PA, Clark NM. Alleviating suffering 101 – pain relief in the United States. N Engl J Med. 2012;366:197–199. doi: 10.1056/NEJMp1109084. [DOI] [PubMed] [Google Scholar]
- 2.Aasvang E, Kehlet H. Surgical management of chronic pain after inguinal hernia repair. Br J Surg. 2005;92:795–801. doi: 10.1002/bjs.5103. [DOI] [PubMed] [Google Scholar]
- 3.Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101:77–86. doi: 10.1093/bja/aen099. [DOI] [PubMed] [Google Scholar]
- 4.Macrae WA. Chronic pain after surgery. Br J Anaesth. 2001;87:88–98. doi: 10.1093/bja/87.1.88. [DOI] [PubMed] [Google Scholar]
- 5.Crombie IK, Davies HT, Macrae WA. Cut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinic. Pain. 1998;76:167–171. [PubMed] [Google Scholar]
- 6.Perkins FM, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology. 2000;93:1123–1133. doi: 10.1097/00000542-200010000-00038. [DOI] [PubMed] [Google Scholar]
- 7.Dworkin RH, O’Connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132:237–251. doi: 10.1016/j.pain.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 8.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 9.Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9:723–744. doi: 10.1586/ern.09.20. [DOI] [PubMed] [Google Scholar]
- 10.Rabow MW, Hardie GE, Fair JM, McPhee SJ. End-of-life care content in 50 textbooks from multiple specialties. JAMA. 2000;283:771–778. doi: 10.1001/jama.283.6.771. [DOI] [PubMed] [Google Scholar]
- 11.Kissin I. Can a bibliometric indicator predict the success of a drug? Scientometrics. 2011;86:785–795. [Google Scholar]
- 12.Kissin I, Bradley EL., Jr Top Journal Selectivity Index: is it acceptable for drugs beyond the field of analgesia? Scientometrics. 2011;88:589–597. [Google Scholar]
- 13.Townsend CM, Jr, Beauchamp RD, Evers BM, Mattox KL. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 18th ed. Philadelphia, PA: Saunders/Elsevier; 2008. [Google Scholar]
- 14.Brunicardi F, Andersen D, Billiar T, et al. Schwartz’s Principles of Surgery. 9th ed. New York, NY: McGraw-Hill Medical Pub Division; 2009. [Google Scholar]
- 15.Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Simeone DM, Upchurch GR. Greenfield’s Surgery: Scientific Principles and Practice. 5th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincot Williams & Wilkins; 2010. [Google Scholar]
- 16.Miller RD, Eriksson LI, Fleisher LA, Weiner-Kronish JP. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone Elsevier; 2010. [Google Scholar]
- 17.Kissin I, Bradley EL., Jr Top Journal Selectivity Index and ‘me-too’ drugs. Scientometrics. 2012;91:131–142. [Google Scholar]
- 18.Sherman RA, Sherman CJ, Parker L. Chronic phantom and stump pain among American veterans: results of a survey. Pain. 1984;18:83–95. doi: 10.1016/0304-3959(84)90128-3. [DOI] [PubMed] [Google Scholar]
- 19.Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, et al. Predictive risk factors for persistent postherniotomy pain. Anesthesiology. 2010;112:957–969. doi: 10.1097/ALN.0b013e3181d31ff8. [DOI] [PubMed] [Google Scholar]
- 20.Stiff G, Rhodes M, Kelly A, Telford K, Armstrong CP, Rees BI. Long-term pain: less common after laparoscopic than open cholecystectomy. Br J Surg. 1994;81:1368–1370. doi: 10.1002/bjs.1800810939. [DOI] [PubMed] [Google Scholar]
- 21.Cheney FW, Domino KB, Caplan RA, Posner KL. Nerve injury associated with anesthesia: a closed claims analysis. Anesthesiology. 1999;90:1062–1069. doi: 10.1097/00000542-199904000-00020. [DOI] [PubMed] [Google Scholar]
- 22.Macrae WA. Chronic pain after sternotomy. Acta Anaesthesiol Scand. 2001;45:927–928. doi: 10.1034/j.1399-6576.2001.450801.x. [DOI] [PubMed] [Google Scholar]
- 23.Gottschalk A, Raja SN. Severing the link between acute and chronic pain: the anesthesiologists role in preventive medicine. Anesthesiology. 2004;101:1083–1085. doi: 10.1097/00000542-200411000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Eisenach JC. Preventing chronic pain after surgery: who, how and when? Reg Anesth Pain Med. 2006;31:1–3. doi: 10.1016/j.rapm.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 25.Romundstad L, Stubhaug A. Glucocorticoids for acute and persistent postoperative neuropathic pain: what is the evidence? Anesthesiology. 2007;107:371–373. doi: 10.1097/01.anes.0000279487.27940.5c. [DOI] [PubMed] [Google Scholar]
- 26.Loftus LS, Laronga C. Evaluating patients with chronic pain after breast cancer surgery: the search for relief. JAMA. 2009;302:2034–2035. doi: 10.1001/jama.2009.1642. [DOI] [PubMed] [Google Scholar]
- 27.De Kock M. Expanding our horizons: transition of acute postoperative pain to persistent pain and establishment of chronic postsurgical pain services. Anesthesiology. 2009;111:461–463. doi: 10.1097/ALN.0b013e3181afde28. [DOI] [PubMed] [Google Scholar]
- 28.Lavand’homme P. Chronic pain after vaginal and cesarean delivery: a reality questioning our daily practice of obstetric anesthesia. Int J Obstet Anesth. 2010;19:1–2. doi: 10.1016/j.ijoa.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Rappaport BA, Cemy I, Sanhai WR. Action on the prevention of chronic pain after surgery: public-private partnerships, the future of analgesic drug development. Anesthesiology. 2010;112:509–510. doi: 10.1097/ALN.0b013e3181cf4279. [DOI] [PubMed] [Google Scholar]
- 30.Enck RE. Postsurgical chronic pain. Am J Hosp Palliat Care. 2010;27:301–302. doi: 10.1177/1049909110369530. [DOI] [PubMed] [Google Scholar]