Abstract
Objective
The present study aimed to examine the association between maternal passive smoking during pregnancy and the risk of spontaneous PTD and to explore the potential interaction of the single or joint gene polymorphism of CYP1A1 and GSTs with maternal passive smoking on the risk of spontaneous PTD.
Method
We investigated whether the association between maternal passive smoking and PTD can be modified by 2 metabolic genes, i.e. cytochrome P4501A1 (CYP1A1) and glutathione S-transferases (GSTs), in a case-control study with 198 spontaneous preterm and 524 term deliveries in Shenzhen and Foshan, China. We used logistic regression to test gene-passive smoking interaction, adjusting for maternal socio-demographics and prepregnancy body mass index.
Results
Overall, maternal passive smoking during pregnancy was associated with higher risk of PTD (adjusted odds ratio = 2.20 [95% confidence interval: 1.56–3.12]). This association was modified by CYP1A1 and GSTs together, but not by any single genotype. For cross-categories of CYP1A1 Msp I and GSTs, maternal passive smoking was associated with higher risk of PTD among those women with CYP1A1 “TC/CC”+ GSTs “null”, but not among women with other genotypes; and this interaction was significant (OR = 2.66 [95% CI: 1.19–5.97]; P-value: 0.017). For cross-categories of CYP1A1 BsrD I and GSTs, maternal passive smoking was associated with higher risk of PTD only among those women with CYP1A1“AG/GG”+ GSTs “null”, but not among women with other genotypes; and this interaction was significant (OR = 3.00 [95% CI: 1.17–7.74]; P-value: 0.023).
Conclusions
Our findings suggest that the combined genotypes of CYP1A1 and GSTs can help to identify vulnerable pregnant women who are subject to high risk of spontaneous PTD due to passive smoking.
Introduction
Preterm delivery (PTD, <37 completed weeks of gestation) is a big clinical and public health challenge globally. Despite increased awareness and improved prenatal care, the percentage of PTD remains unacceptably high in both developed (e.g. 7% in U.S. [1]) and developing societies (e.g. 5–15% in China [2]). About 15% preterm babies die within one month after birth [3]. PTD also leads to many other short- and long-term health problems and poses enormous burden to both health care system and the child’s family [4]. Preterm delivery is often classified into spontaneous and medically indicated subgroups, and the majorities (75–85%) of PTDs are spontaneous [5]. The causes and underlying biological mechanisms of spontaneous PTD are still unclear [6], although previous studies have identified a long list of risk factors, including low socio-economic status [7], parity, maternal age [8], drug abuse, life events [9], racial origin [10], maternal active or passive smoking [11], air pollution [12], [13] intrauterine infection [14], and genetic heterogeneity [9], [15].
Maternal active smoking is a well-established risk factor for PTD, and it accounts for about 14% of all PTDs [16]. But only a relatively small proportion of smoking pregnant women end with PTD, which may be explained by the substantial variability in genetic susceptibility across individuals. Some evidences show that gene polymorphism in cytochrome P4501A1 (CYP1A1) and glutathione S-transferases (GSTs) may modify the link between maternal active smoking and PTD [17]. CYP1A1 is one of cytochrome P450 (CYP450) family genes that are responsible for phase I detoxication by converting exogenous exposures, e.g. tobacco compounds, into intermediate metabolites. CYP1A1 mutation can lead to higher enzyme activity. GSTs are one of phase II detoxication enzymes that protect cells from toxicants by conjugation with glutathione. Inherited homozygous deletion of GSTs genes can result in lack of phase II detoxification activity [18], [19], [20], which thus increases the accumulation of intermediate metabolites of exogenous in human body. Limited researches focused on the gene (CYP1A1, GSTs)-maternal active smoking on the risk PTD yielded inconsistent findings [17], [21], [22].
Passive smoking is one of the most important public health problems in many developing countries, such as China, where many non-smoking pregnant women are exposed to environmental tobacco smoke at home, workplace, and public places [23]. Perera et al. found the levels of serum cotinine and DNA adducts in passive smoking mothers were significantly higher than those in non-passive smoking mothers [24]. Some previous studies, all done in developed countries, suggest that maternal passive smoking may shorten gestational age and thus increase the risk of PTD [23]. It is unclear whether this association holds in pregnant women in developing countries. Moreover, little is known about the potential interaction between maternal passive smoking and genes (CYP1A1, GSTs) polymorphisms in the risk of PTD.
Therefore, the present study aimed to fill these important research gaps in this filed. Specially, we had 2 objectives in this study: 1) to examine the association between maternal passive smoking during pregnancy and the risk of spontaneous PTD among Chinese pregnant women; 2) to explore the potential interaction between the single or joint gene polymorphism of CYP1A1 and GSTs with maternal passive smoking on the risk of spontaneous PTD.
Materials and Methods
Study Population
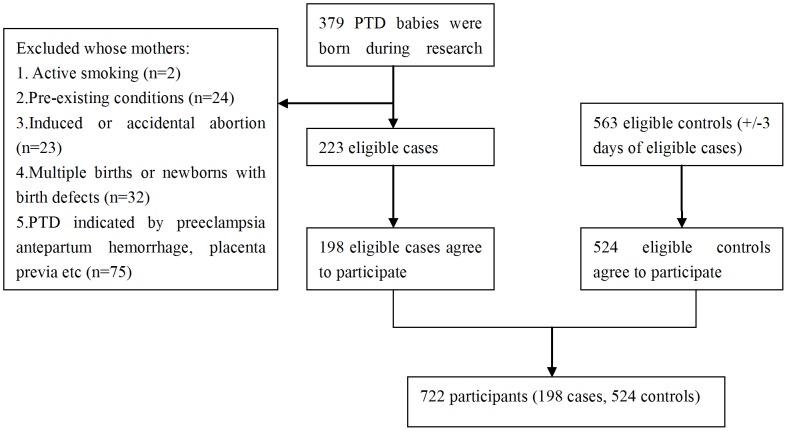
We conducted a case-control study from September 2009 to March 2011 at two Women and Children’s Hospitals at Shenzhen and Foshan, Guangdong Province, China. Figure 1 shows the flow chart of our study participants flowchart was listed in figure 1. A total of 379 preterm (gestational age <37 full weeks) babies were born in these two hospitals during the study period. Among them, 223 spontaneous singleton babies were eligible for this study (see below). Finally, 198 (88.8%) mothers of 223 eligible babies agreed to participate in the study and were included as cases. We randomly selected controls from those mothers who delivered term singleton babies (gestational age 37–42 full weeks) with normal birth weight (2500–4000 g) in the same hospital. To increase the comparability, we matched 563 eligible controls with eligible cases by delivery date (+/−3 days). Among them, 524 (93.1%) mothers of the controls agreed to participate in this study. We approached participating mothers within 12–36 hours after delivery.
Figure 1. Flow chart of study participants.
For the purpose of this study, we excluded the preterm babies whose mothers: 1) actively smoked cigarettes during pregnancy (n = 2); 2) had one or more pre-existing chronic conditions, including heart failure, chronic renal diseases, lung diseases, diabetes, hypertension, hyperthyroidism, Mediterranean anemia etc. (n = 24); 3) had induced or accidental abortion (n = 23); 4) had multiple births or newborns with birth defects (n = 32); or 5) had medically indicated PTD due to obstetric complications, such as severe preeclampsia, antepartum hemorrhage, placenta previa etc (n = 75).
All the participants understood and signed a written consent form. This study was approved by the Ethics Committees of Sun Yat-sen University in Guangzhou, China.
Data Collection
We collected data through interview, medical records review, and blood lab tests. At the postnatal face-to-face interview, each mother completed a structural questionnaire and reported her passive smoking status during pregnancy, socio-demographics, reproductive history, medical history, psychosocial stress, health behavior and lifestyles. Pregnant women were expected to complete up to 12 routine prenatal care visits for routine obstetric examinations starting from the 20th week of gestation: 2 visits during 20–27 weeks of gestation, bi-weekly during 28–35 weeks of gestation, and then weekly after 36 weeks of gestation. We obtained maternal and fetal health information from obstetrical medical records, including last menstrual period, ultrasound assessment, maternal chronic diseases, and obstetric complications. We collected maternal blood samples within 12 hours after admission to the hospital in tubes with anticoagulants (EDTA K2), and then stored blood samples in a refrigerator at temperature of −80°C.
Measures
PTD outcome
Pregnant women self-reported their last menstrual period (LMP) at the 1st prenatal care visit (usually at 8–10th week of gestation). The LMP was confirmed by early ultrasound assessment (gestational age<20 full weeks). If self-reported LMP was unavailable, ultrasound estimated LMP based on the crown-rump length in early pregnancy was used instead [25]. We calculated gestational age as the interval between LMP and delivery date. We defined PTD as gestational age less than 37 complete weeks.
Passive smoking exposures
In this study, we measured maternal passive smoking during pregnancy by combining self-report and serum cotinine test. At the interview, participants retrospectively self-reported their passive smoking status during pregnancy.
We also measured the cotinine level in maternal peripheral blood using enzyme immunoassay technique (Immunalysis Corp., Pomona, California, US; Manufacture-reported detection limit, 1 ng/ml). Briefly, we first added 10 µl of serum, calibrator, or control to 3 separate assay wells, and mixed them with 100 µl of cotinine enzyme. Then we incubated these samples for 30 minutes at room temperature, and washed the micro-plate 6 times with 350 ul buffer. Then we added 100 µl of substrate solution and measured the absorbance spectrum of samples at 450 nm using a micro-plate reader within 60 minutes.
We defined passive smoking as: 1) self-reported exposure to cigarette smoke by others (at home, work or public places) during pregnancy (n = 199), or 2) serum cotinine level ≥3 ng/ml (n = 230). This combined use of self-report and serum cotinine could reduce misclassification of passive smoking [26], [27]. Overall, there was relatively high concordance between self-reported passive smoking when serum cotinine cut-off level was set as 3 ng/ml in our sample (Kappa-value: 0.752). However, 53 women (7.3%) who did not report passive smoking but had serum cotinine level ≥3 ng/ml and 22(3.0%) women who reported passive smoking but had serum cotinine level <3 ng/ml (Table S1).
Genotypes
We purified DNA from venous whole blood samples using DNS purification kits (Takara, Biot. Ltd, China).We used polymerase chain reaction (PCR) and restriction fragment length polymorphism (RFLP) methods to genotype CYP1A1 polymorphisms. We digested PCR products by Msp I (to identify CYP1A1 m1 mutation) and BsrD I (to identify CYP1A1 m2 mutation) and then detected the genotypes of our interest, including the homozygous wild type “TT” “AA”, heterozygous variant “TC” “AG”, and homozygous variant “CC” “GG”. The PCR primers (Sangon biotech, shanghai, co., Ltd.) for CYP1A1 polymorphisms included Msp I forward 5′-CAG TGA AGA GGT GTA GCC GCT-3′ and reverse 5′-TAG GAG TCT TGT CTC ATG CCT-3′; BsrD I forward 5′-CTG TCT CCC TCT GGT TAC AGG AAG C-3′ and reverse 5′-TTC CAC CCG TTG CAG CAG GAT AGC C-3′. The PCR primers for GSTs polymorphisms included GSTM1 forward 5′-GAA CTC CCT GAA AAG CTA AG-3′ and reverse 5′-GTT GGG CTC AAA TAT ACG GTG G-3′; and GSTT1 forward 5′-TTC CTT ACT GGT CCT CAC ATC TC-3′ and reverse 5′-TCA CCG GAT CAT GGC CAG CA-3′. As the internal control, a 268-bp fragment of the human –β globin gene was coamplified with a second set of primers (5′-CAA CTT CAT CCA CGT TCA CC-3′) and (5′-GAA GAG CCA AGG ACA GGT AC-3′). Due to small numbers of participants with homozygous variant genotypes, we combined TC (n = 310) and CC (n = 127) as TC/CC, AG (n = 266) and GG (n = 71) as AG/GG. For the same reason, we combined GSTM1 and GSTT1 genotypes as a binary variable GSTs that was coded as “null” if both GSTM1 and GSTT1 were null and as “present” otherwise.
Confounders
In addition to the matched delivery date, we considered family income, maternal age, education level, and prepregnancy body mass index (BMI) as potential confounders. We classified self-reported family income as low (<1500 Renminbi [RMB, Chinese currency] monthly), middle (1500–4000 RMB monthly), and high (>4000 RMB monthly). We calculated prepregnancy BMI as self-reported prepregnancy weight in kg/height in meter2, and classified women into underweight (BMI<18.5), normal (BMI 8.5–24.0), and overweight or obese (BMI≥24.0) according to WHO guideline for Asians [28].
Statistical Analyses
We first conducted Chi-square/t-test to examine the overall characteristic balance between PTD case and control groups. Chi-square test was adopted to test the associations between maternal passive smoking during pregnancy, single gene polymorphism with the risk of PTD, we then fitted multivariable logistic regression models to estimate the odds ratios (OR) and their 95% confidence intervals (CI), adjusting for potential confounders.
To examine whether the association between maternal passive smoking and PTD could be modified by maternal CYP1A1 and GSTs polymorphisms, we tested their interactions on multiplicative scale. Specifically, we added the interaction terms “passive smoking×gene polymorphism” (products) to the multivariable logistic regression models which already included the main effect terms for passive smoking and CYP1A1 and GSTs genotypes, as well as the potential confounders. A significant departure of the OR value for an interaction term from 1 indicated the existence of interaction on a multiplicative scale. To better demonstrate joint gene-passive smoking interaction, we also classified participants into 8 exclusive groups by passive smoking status (yes vs. no), CYP1A1 (“wild” vs. “variant”), and GSTs (“present” vs. “null”). We set non-passive smoking mothers with low risk genotypes (CYP1A1 “TT” or “AA”+GSTs “present”) as the reference group and then compared it with the other 7 groups. All analyses were completed in SPSS 16.0 software (SPSS Inc, Chicago, Illinois, USA). The statistical significance level was set to <0.05 (two-sided).
Results
Table 1 shows the characteristics of our study sample. Overall, the PTD case and control groups were comparable in terms of maternal age, marital status, socio-economic status, alcohol use during pregnancy, prepregnancy BMI, and the child gender. However, mothers in the case group had lower education level (36.9% vs. 46.9% with college or higher degree), and were also more likely to be parous (32.3% vs. 24.0%), when compared with mothers in the control group.
Table 1. Comparison of characteristics between spontaneous PTD cases and controls.
| Cases (n = 198) | Controls(n = 524) | P-value | |
| Mean ± SD or N. (%) | Mean ± SD or N. (%) | ||
| Maternal age (years, mean ± SD) | 28.5±4.9 | 28.8±4.3 | 0.474 |
| Marital status (%) | |||
| Married | 193(97.5) | 502(95.8) | 0.290 |
| Unmarried | 5(2.5) | 22(4.2) | |
| Race/ethnicity (%) | |||
| Han | 191(97.0) | 507(96.9) | 0.992 |
| Minority | 6(3.0) | 16(3.1) | |
| Education level (%) | |||
| Junior high school or lower | 70(35.4) | 136(26.0) | 0.020 |
| High school | 55(27.8) | 142(27.1) | |
| College or higher | 73(36.9) | 246(46.9) | |
| Family income (%) | |||
| Low | 44(23.0) | 141(27.2) | 0.248 |
| Middle | 32(16.8) | 102(19.7) | |
| High | 115(60.2) | 276(53.2) | |
| Parity (%) | |||
| Nullparous | 134(67.7) | 398(76.0) | 0.024 |
| Parous | 64(32.3) | 126(24.0) | |
| Alcohol use during pregnancy, % | 4(2.0) | 17(3.2) | 0.383 |
| Prepregnancy BMI (kg/m2) (%) | |||
| Underweight (<18.5) | 45(22.7) | 124(23.7) | 0.606 |
| Normal (18.5–23.9) | 137(69.2) | 346(66.0) | |
| Overweight or obesity(≥24.0) | 16(8.1) | 54(10.3) | |
| Child gender (%) | |||
| Male | 109(35.6) | 257(51.3) | 0.105 |
| Female | 89(64.4) | 271(48.7) |
Table 2 shows the overall associations (main effect) of maternal passive smoking during pregnancy and single gene polymorphism with risk of PTD. The proportion of passive smoking mothers in the PTD group (49.0%) was much higher than those in the control group (29.6%), and the adjusted OR was 2.20 (95% CI: 1.56–3.12). However, the distribution of CYP1A1 Msp I, CYP1A1 BsrD I, GSTM and GSTT1 genotypes were similar between the two groups.
Table 2. Associations of maternal passive smoking during pregnancy, CYP1A1, and GSTs genotypes with risks of spontaneous PTD.
| Case (n = 198) | Control (n = 524) | Crude OR (95% CI) | ORa (95%CI) | P-value | |
| N. (%) | N. (%) | ||||
| Passive smokingduring pregnancy | |||||
| No | 101(51.0) | 369(70.4) | 1 | 1 | |
| Yes | 97(49.0) | 155(29.6) | 2.29 (1.63–3.20) * | 2.20 (1.56–3.12) | 0.000 |
| CYP1A1 Msp I | |||||
| TT | 73(36.9) | 212(40.5) | 1 | 1 | |
| TC/CC | 125(63.1) | 312(59.5) | 1.16 (0.83–1.63) | 1.15 (0.82–1.63) | 0.418 |
| CYP1A1 BsrD I | |||||
| AA | 95(48.0) | 290(55.3) | 1 | 1 | |
| AG/GG | 103(52.0) | 234(44.7) | 1.34 (0.97–1.87) | 1.30 (0.93–1.81) | 0.133 |
| GSTM1 | |||||
| Present | 97(49.0) | 275(52.5) | 1 | 1 | |
| Null | 101(51.0) | 249(47.5) | 1.15 (0.83–1.60) | 1.12 (0.80–1.57) | 0.515 |
| GSTT1 | |||||
| Present | 95(48.0) | 241(46.0) | 1 | 1 | |
| Null | 103(52.0) | 283(54.0) | 0.92 (0.67–1.28) | 0.97 (0.69–1.37) | 0.877 |
| GSTs | |||||
| Present | 137(69.2) | 386(73.7) | 1 | 1 | |
| Null | 61(30.8) | 138(26.3) | 1.25 (0.87–1.78) | 1.29 (0.89–1.87) | 0.182 |
ORa adjusted for family income, maternal age, education level and prepregnancy BMI.
GSTs “null” if both GSTM1 and GSTT1 “null”, GSTs “present” if either GSTM1 or GSTT1 “present”.
Table 3 shows the interactions between maternal passive smoking during pregnancy and single gene loci polymorphism on risk of PTD, after adjusting for potential confounders. Overall, there was no significant interaction between maternal smoking during pregnancy with any of the 4 selected gene loci (CYP1A1 Msp I, CYP1A1 BsrD I, GSTM1 and GSTT1) on multiplicative scale.
Table 3. Interaction between maternal passive smoking during pregnancy and single genotype of CYP1A1 and GSTs on risk of spontaneous PTD.
| Passivesmoking | Genotype | Case(n = 198) | Control(n = 524) | ORa(95%CI) | P-value |
| N.(%) | N.(%) | ||||
| CYP1A1 Msp I | |||||
| No | TT | 41 (20.7) | 151 (28.8) | 1 | |
| No | TC/CC | 60 (30.3) | 218 (41.6) | 0.96 (0.61–1.52) | 0.876 |
| Yes | TT | 32 (16.2) | 61 (11.6) | 1.75 (1.00–3.07)* | 0.052 |
| Yes | TC/CC | 65 (32.8) | 94 (17.9) | 2.42 (1.50–3.89)* | 0.000 |
| Interaction | 1.44 (0.71–2.92) | 0.319 | |||
| CYP1A1 BsrD I | |||||
| No | AA | 50 (25.3) | 203 (38.7) | 1 | |
| No | AG/GG | 51 (23.5) | 166 (31.7) | 1.18 (0.75–1.85) | 0.483 |
| Yes | AA | 45 (22.7) | 87 (16.6) | 1.98 (1.22–3.22)* | 0.007 |
| Yes | AG/GG | 52 (26.3) | 68 (13.0) | 2.90 (1.78–4.72)* | 0.000 |
| Interaction | 1.24 (0.62–2.47) | 0.541 | |||
| GSTM1 | |||||
| No | Present | 49 (24.7) | 195 (37.2) | 1 | |
| No | Null | 52 (26.2) | 174 (35.7) | 1.15 (0.73–1.81) | 0.519 |
| Yes | Present | 48 (24.2) | 80 (15.3) | 2.30 (1.41–3.74) | 0.001 |
| Yes | Null | 49 (24.7) | 75 (29.5) | 2.43 (1.49–3.97) | 0.000 |
| Interaction | 0.92 (0.46–1.83) | 0.806 | |||
| GSTT1 | |||||
| No | Present | 49 (24.7) | 163 (31.1) | 1 | |
| No | Null | 52 (26.2) | 206 (39.3) | 0.84 (0.53–1.33) | 0.454 |
| Yes | Present | 46 (23.2) | 78 (14.9) | 1.81 (1.10–2.98) | 0.020 |
| Yes | Null | 51 (25.8) | 77 (14.7) | 2.22 (1.37–3.62) | 0.002 |
| Interaction | 1.46 (0.73–2.91) | 0.286 | |||
| GSTs | |||||
| No | Present | 73 (36.9) | 267 (51.0) | 1 | |
| No | Null | 28 (14.1) | 102 (19.5) | 1.00 (0.60–1.66) | 0.999 |
| Yes | Present | 64 (32.3) | 119 (22.7) | 1.86 (1.24–2.81) | 0.003 |
| Yes | Null | 33 (16.7) | 36 (6.9) | 3.39 (1.95–5.91) | 0.000 |
| Interaction | 1.83 (0.84–3.96) | 0.126 | |||
ORa adjusted for family income, maternal age, education level and prepregnancy BMI.
GSTs “null” if both GSTM1 and GSTT1 “null”, GSTs “present” if either GSTM1 or GSTT1 “present”.
% for distribution within the case and control groups respectively.
Table 4 and 5 show the interactions between maternal passive smoking during pregnancy and joint gene polymorphisms on risks of PTD, after adjusted for potential confounders. Compared with non-passive smoking women with CYP1A1 “TT” and GSTs “present”, those passive smoking women with CYP1A1 “TC/CC”+ GSTs “null” had higher risk of PTD (OR = 4.72 [95% CI: 2.28–9.77]), the interaction between passive smoking and CYP1A1 “TC/CC”+ GSTs “null” was statistically significant (OR = 2.66 [95% CI: 1.19–5.97; P-value: 0.017]) on multiplicative scale (Table 4). Compared with non-passive smoking women with CYP1A1 “AA” and GSTs “present”, those passive smoking women with CYP1A1 “AG/GG”+ GSTs “null” had higher risk of PTD (OR = 7.01 [95% CI: 2.91–16.86]), the interaction between passive smoking and CYP1A1 “AG/GG”+ GSTs “null” was statistically significant (OR = 3.00 [95% CI: 1.17–7.74; P-value: 0.023]) on multiplicative scale (Table 5).
Table 4. Interaction between maternal passive smoking during pregnancy and joint genotype of CYP1A1 Msp I and GSTs on risk of spontaneous PTD.
| Passive smoking | Genotype | Case (n = 198) | Control (n = 524) | ORa(95%CI) | P-value | |
| CYP1A1 Msp I | GSTs | N. (%) | N. (%) | |||
| No | TT | Present | 30 (15.2%) | 110 (21.0%) | 1 | |
| No | TT | Null | 11 (5.6%) | 41 (7.8%) | 1.04 (0.47–2.29) | 0.918 |
| No | TC/CC | Present | 43 (21.7%) | 157 (30.0%) | 0.98 (0.57–1.67) | 0.947 |
| No | TC/CC | Null | 17 (8.6%) | 61 (11.6%) | 0.95 (0.47–1.93) | 0.902 |
| Yes | TT | Present | 25 (12.6%) | 45 (8.6%) | 1.82 (0.95–3.48) | 0.072 |
| Yes | TT | Null | 7 (3.5%) | 16 (3.1%) | 1.64 (0.61–4.41) | 0.326 |
| Yes | TC/CC | Present | 39 (19.7%) | 74 (14.1%) | 1.85 (1.04–3.26) | 0.035 |
| Yes | TC/CC | Null | 26 (13.1%) | 20 (3.8%) | 4.72 (2.28–9.77) | 0.000 |
| Interaction | 2.66 (1.19–5.97) | 0.017 | ||||
ORa adjusted for family income, maternal age, education level, prepregnancy BMI and CYP1A1 BsrD I genotype.
GSTs “null” if both GSTM1 and GSTT1 “null”, GSTs “present” if either GSTM1 or GSTT1 “present”.
% for distribution within the case and control groups respectively.
.The variable of passive smoking+CYP1A1 Msp I+ GSTs with eight levels was set as dummy independent variable, and the first level as reference category.
Table 5. Interaction between maternal passive smoking during pregnancy and joint genotype of CYP1A1 BsrD I and GSTs on risk of spontaneous PTD.
| Passive smoking | Genotype | Case (n = 198) | Control (n = 524) | ORa(95%CI) | P-value | |
| CYP1A1 BsrD I | GSTs | N. (%) | N. (%) | |||
| No | AA | Present | 38 (19.2%) | 149 (28.4%) | 1 | |
| No | AA | Null | 12 (6.1%) | 54 (10.3%) | 0.94 (0.45–1.95) | 0.863 |
| No | AG/GG | Present | 35 (17.7%) | 118 (22.5%) | 1.14 (0.67–1.95) | 0.636 |
| No | AG/GG | Null | 16 (8.1%) | 48 (9.2%) | 1.19 (0.59–2.42) | 0.613 |
| Yes | AA | Present | 30 (15.2%) | 61 (11.6%) | 1.80 (1.01–3.22) | 0.050 |
| Yes | AA | Null | 15 (7.6%) | 26 (5.0%) | 2.33 (1.11–4.89) | 0.030 |
| Yes | AG/GG | Present | 34 (17.2%) | 58 (11.1%) | 2.17 (1.23–3.83) | 0.008 |
| Yes | AG/GG | Null | 18 (9.1%) | 10 (1.9%) | 7.01 (2.91–16.86) | 0.000 |
| Interaction | 3.00 (1.17–7.74) | 0.023 | ||||
ORa adjusted for family income, maternal age, education level, prepregnancy BMI and CYP1A1 Msp I genotype.
GSTs “null” if both GSTM1 and GSTT1 “null”, GSTs “present” if either GSTM1 or GSTT1 “present”.
% for distribution within the case and control groups respectively.
The variable of passive smoking+CYP1A1 BsrD I + GSTs with eight levels was set as dummy independent variable, and the first level as reference category.
Discussion
In this case-control study among Chinese women, we examined the interactions between maternal passive smoking during pregnancy and genes (CYP1A1, GSTs) polymorphisms on the risks of spontaneous preterm delivery. We confirmed that maternal passive smoking was associated with higher risk of spontaneous preterm delivery. In addition, this increased risk was more striking for those women with the jointed genotype of CYP1A1“AG/GG”+GSTs“null”.
We found that maternal passive smoking during pregnancy was associated with more than two-fold risk of PTD, after adjusting for a series of potential confounders. This estimate is very close to a previous study (OR = 2.3[95% CI: 1.96–5.96]) [29]. Our finding adds to the literature that maternal passive smoking during pregnancy is a risk factor for PTD among women [30], [31], [32], [33]. This suggests that pregnant women should try their best to avoid passive smoking, which is especially important in developing societies, such as China where 53% males (probably including their husbands) are daily smokers [4].
There were limited evidences on interaction between CYP1A1, GSTs polymorphisms and maternal active smoking during pregnancy (no study on passive smoking so far) on the risk of PTD. Our study showed that CYP1A1 m1 (Msp I) and m2 (BsrD I) mutation and GSTs deletion alone, in the absence of maternal passive smoking during pregnancy, did not increase the risk of PTD. However, we found a significant synergy between maternal passive smoking and CYP 1A1 “AG/GG” + GSTs “null” genotype, as well as between maternal passive smoking and CYP1A1 “TC/CC” + GSTs “null” genotype; and noted that we defined GSTs “null” if both GSTT1 and GSTM1 are null to maximize the impact of GSTs null function. This suggests these genetic risk factors may amplify the high risk of PTD associated with passive smoking during pregnancy.
Preterm delivery is a complex phenotype with various pathophysiological pathways, and more than 30 single nucleotide polymorphisms (SNPs) have been found to be associated with PTD or premature rupture of the membranes [34], [35]. CYP1A1 and GSTs genes are two of many pathways that control the conversion of exogenous exposure [6]. So, it is likely that PTD cannot be explained by the variation of single gene locus [6]. This may be why we did not find interaction of passive smoking with single loci of gene mutations (CYP1A1 or GSTs). However, we did find significant interaction between joint genotypes of CYP1A1+GSTs and passive smoking, which suggests CYP1A1 combined with GSTs presents a stronger pathophysiological pathway through which passive smoking increases the risk of PTD. This is biologically plausible, because passive smoking mothers with high-risk genotypes (i.e. CYP1A1 “AG/GG” or “TC/CC”) may have the higher-activity enzymes that metabolize cigarette toxins such as PAHs, when GSTs detoxification function is null, higher levels of PAH-DNA adducts and DNA strand breakage were produced and accumulated in the maternal body. Moreover, the activated adducts can cause the placental inflammatory reaction and initiate the uterus contraction thus lead to PTD [36]. Our finding is consistent with a previous study on maternal active smoking done by Tsai et al. [17]. They found a very strong interaction between maternal active smoking and the joint genotypes (CYP1A1“AG/GG”+GSTT1 “null”) in the risk of PTD accompanied by histologic chorioamnionitis.
Study Strengths and Limitations
This study has several notable strengths. This is the first study on interaction between maternal passive smoking during pregnancy and maternal metabolism genes (e.g. CYP1A1 and GSTs) on the risk of PTD. Secondly, our combined use of self-report and serum cotinine level can largely reduce misclassification of maternal passive smoking due to recall bias and/or biomarker measurement error. Finally, we excluded women with chronic disease and medical induced PTD, which allowed us to more accurately estimate the impact of passive smoking on spontaneous PTD as well as its interaction with CYP1A1 and GSTs genes. However, some limitations should be mentioned. Firstly, the case-control design of our study could only provide suggestive but not confirmative causality regarding the association between maternal smoking during pregnancy and PTD. Secondly, there was substantial uncertainty in our estimated associations due to the relatively small sample size of PTD cases. Thirdly, although we adjusted for maternal socio-demographics and prepregnancy BMI, we could not control some other important confounders, such as air pollution during pregnancy which could increase the risk of preterm birth [37], [38]. Finally, we could not distinguish the timing (e.g. by trimester) of passive smoking during pregnancy.
Conclusion
In summary, we found maternal passive smoking during pregnancy was associated with higher risk of spontaneous PTD. The genotypes of CYP1A1 “AG/GG” or “TC/CC” + GSTs “null” seemed to amplify the risk of spontaneous PTD associated with passive smoking during pregnancy. This novel finding has important clinical and public health implications. It not only contributes to better understanding the pathogenic pathways through which maternal passive smoking increases risk of spontaneous PTD, but also helps to identify vulnerable pregnant women who are subject to high risk of spontaneous PTD due to maternal passive smoking.
Supporting Information
Concordance of maternal passive smoking measured by self-report and by maternal serum cotinine level.
(DOC)
Acknowledgments
The authors acknowledge the support of Shenzhen Women and Children’s Hospital and Foshan Women and Children’s Hospital.
Funding Statement
The research was funded by the Natural Science Foundation of China (NSFC; grant number: 30872164). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and cause of preterm birth. Lancet 371: 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Le J, Xie X, Lin ZQ, Gou WL, D W (2006) Obstetrics and Gynecology. 6rd Edition. Beijing: People’s Medical Publishing House.
- 3.Gabbe SG, Niebyl JR, Simpson JL, Annas GJ (1996) Obstetrics: Normal&?roblem Pregnancies. 3rd Edition. London: Churchill Livingstons Inc.
- 4. Zhang J, Ou JX, Bai CX (2011) Tobacco smoking in China: prevalence, disease burden, challenges and future strategies. Respirology 16: 1165–1172. [DOI] [PubMed] [Google Scholar]
- 5. Steer P (2005) The epidemiology of preterm labour. BJOG 112 Suppl 1 1–3. [DOI] [PubMed] [Google Scholar]
- 6. Gravett MG, Rubens CE, Nunes TM (2010) Global report on preterm birth and stillbirth (2 of 7): discovery science. BMC Pregnancy Childbirth 10 Suppl 1 S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Escriba-Aguir V, Clemente I, Saurel-Cubizolles M (2001) [Socio-economic factors associated with preterm delivery. Results of the European project in Spain]. Gac Sanit 15: 6–13. [DOI] [PubMed] [Google Scholar]
- 8. Monaghan SC, Little RE, Hulchiy O, Strassner H, Gladen BC (2001) Risk factors for spontaneous preterm birth in two urban areas of Ukraine. Paediatr Perinat Epidemiol 15: 123–130. [DOI] [PubMed] [Google Scholar]
- 9. Moutquin JM (2003) Classification and heterogeneity of preterm birth. BJOG 110 Suppl 20 30–33. [DOI] [PubMed] [Google Scholar]
- 10. Menon R (2008) Spontaneous preterm birth, a clinical dilemma: etiologic, pathophysiologic and genetic heterogeneities and racial disparity. Acta Obstet Gynecol Scand 87: 590–600. [DOI] [PubMed] [Google Scholar]
- 11. Jaddoe VW, Troe EJ, Hofman A, Mackenbach JP, Moll HA, et al. (2008) Active and passive maternal smoking during pregnancy and the risks of low birth weight and preterm birth: the Generation R Study. Paediatr Perinat Epidemiol 22: 162–171. [DOI] [PubMed] [Google Scholar]
- 12. Ritz B, Yu F, Chapa G, Fruin S (2000) Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology 11: 502–511. [DOI] [PubMed] [Google Scholar]
- 13. Sagiv SK, Mendola P, Loomis D, Herring AH, Neas LM, et al. (2005) A time-series analysis of air pollution and preterm birth in Pennsylvania, 1997–2001. Environ Health Perspect 113: 602–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holst D, Garnier Y (2008) Preterm birth and inflammation-The role of genetic polymorphisms. Eur J Obstet Gynecol Reprod Biol 141: 3–9. [DOI] [PubMed] [Google Scholar]
- 15. Froen JF, Pinar H, Norwitz ER (2007) Genetic epidemiologic studies of preterm birth: studies of disease or of “rescue by birth”? Am J Obstet Gynecol 197: 438–439. [DOI] [PubMed] [Google Scholar]
- 16.American Lung Association. Smoking 101 Fact Sheet; 2006 (http://www.lungusa.org/site/pp.asp?c = dv LUK9O0E&b = 39853).
- 17. Tsai HJ, Liu X, Mestan K, Yu Y, Zhang S, et al. (2008) Maternal cigarette smoking, metabolic gene polymorphisms, and preterm delivery: new insights on G × E interactions and pathogenic pathways. Hum Genet 123: 359–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bartsch H (1996) DNA adducts in human carcinogenesis: etiological relevance and structure–activity relationship. Mutat Res 340: 67–79. [DOI] [PubMed] [Google Scholar]
- 19.Bartsch H, Rojas M, Alexandrov K, Camus AM, Castegnaro M, et al.. (1995) Metabolic polymorphism affecting DNA binding and excretion of carcinogens in humans. Pharmacogenetics 5 (Spec No): S84–S90. [DOI] [PubMed]
- 20. Kriek E, Rojas M, Alexandrov K, Bartsch H (1998) Polycyclic aromatic hydrocarbon-DNA adducts in humans: relevance as bio-markers for exposure and cancer risk. Mutat Res 400: 215–231. [DOI] [PubMed] [Google Scholar]
- 21. Grazuleviciene R, Danileviciute A, Nadisauskiene R, Vencloviene J (2009) Maternal smoking, GSTM1 and GSTT1 polymorphism and susceptibility to adverse pregnancy outcomes. Int J Environ Res Public Health 6: 1282–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gracie SK, Lyon AW, Kehler HL, Pennell CE, Dolan SM, et al. (2010) All Our Babies Cohort Study: recruitment of a cohort to predict women at risk of preterm birth through the examination of gene expression profiles and the environment. BMC Pregnancy Childbirth 10: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ng SP, Zelikoff JT (2007) Smoking during pregnancy: subsequent effects on offspring immune competence and disease vulnerability in later life. Reprod Toxicol 23: 428–437. [DOI] [PubMed] [Google Scholar]
- 24. Perera FP, Tang D, Tu YH, Cruz LA, Borjas M, et al. (2004) Biomarkers in maternal and newborn blood indicate heightened fetal susceptibility to procarcinogenic DNA damage. Environ Health Perspect 112: 1133–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang X, Zuckerman B, Pearson C, Kaufman G, Chen C, et al. (2002) Maternal cigarette smoking, metabolic gene polymorphism, and infant birth weight. JAMA 287: 195–202. [DOI] [PubMed] [Google Scholar]
- 26. Delpisheh A, Topping J, Reyad M, Tang A, Brabin BJ (2007) Smoking exposure in pregnancy: use of salivary cotinine in monitoring. Br J Midwifery 15: 216–220. [Google Scholar]
- 27. Delpisheh A, Brabin L, Topping J, Reyad M, Tang AW, et al. (2009) A case-control study of CYP1A1, GSTT1 and GSTM1 gene polymorphisms, pregnancy smoking and fetal growth restriction. Eur J Obstet Gynecol Reprod Biol 143: 38–42. [DOI] [PubMed] [Google Scholar]
- 28.WHO/IASO/IOTF (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Melbourne: Health Communications Australia.
- 29. Ashford KB, Hahn E, Hall L, Rayens MK, Noland M, et al. (2010) The effects of prenatal secondhand smoke exposure on preterm birth and neonatal outcomes. J Obstet Gynecol Neonatal Nurs 39: 525–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Khader YS, Al-Akour N, Alzubi IM, Lataifeh I (2011) The association between second hand smoke and low birth weight and preterm delivery. Matern Child Health J 15: 453–459. [DOI] [PubMed] [Google Scholar]
- 31. Jaddoe VW, Troe EJ, Hofman A, Mackenbach JP, Moll HA, et al. (2008) Active and passive maternal smoking during pregnancy and the risks of low birthweight and preterm birth: the Generation R Study. Paediatr Perinat Epidemiol 22: 162–171. [DOI] [PubMed] [Google Scholar]
- 32. Fantuzzi G, Aggazzotti G, Righi E, Facchinetti F, Bertucci E, et al. (2007) Preterm delivery and exposure to active and passive smoking during pregnancy: a case-control study from Italy. Paediatr Perinat Epidemiol 21: 194–200. [DOI] [PubMed] [Google Scholar]
- 33. Gajewska E, Mojs E (2008) [The effect of environmental tobacco smoke during pregnancy on psychomotor child development]. Przegl Lek 65: 712–714. [PubMed] [Google Scholar]
- 34. Buhimschi CS, Rosenberg VA, Dulay AT, Thung S, Sfakianaki AK, et al. (2008) Multidimensional system biology: genetic markers and proteomic biomarkers of adverse pregnancy outcome in preterm birth. Am J Perinatol 25: 175–187. [DOI] [PubMed] [Google Scholar]
- 35. Crider KS, Whitehead N, Buus RM (2005) Genetic variation associated with preterm birth: a HuGE review. Genet Med 7: 593–604. [DOI] [PubMed] [Google Scholar]
- 36. Baggia S, Gravett MG, Witkin SS, Haluska GJ, Novy MJ (1996) Interleukin-1 beta intra-amniotic infusion induces tumor necrosis factor-alpha, prostaglandin production, and preterm contractions in pregnant rhesus monkeys. J Soc Gynecol Investig 3: 121–126. [DOI] [PubMed] [Google Scholar]
- 37. Chang HH, Reich BJ (2011) Miranda (2011) Time-to-event analysis of fine particle air pollution and preterm birth: results from North Carolina, 2011–2005. Am J Epidemiol 175: 91–98. [DOI] [PubMed] [Google Scholar]
- 38. Olsson D, Ekström M, Forsberg B (2012) Temporal variation in air pollution concentrations and preterm birth-a population based epidemiology study. Int J Environ Res Public Health 9: 272–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Concordance of maternal passive smoking measured by self-report and by maternal serum cotinine level.
(DOC)