Abstract
Chronic malnutrition in children remains highly prevalent in Laos, particularly among ethnic minority groups. There is limited knowledge of specific nutrition practices among these groups. We explored nutritional status, cultural beliefs and practices of Laos' Khmu ethnic group to inform interventions for undernutrition as part of a Primary Health Care (PHC) project. Mixed methods were used. For background, we disaggregated anthropometric and behavioural indicators from Laos' Multiple Indicator Cluster Survey. We then conducted eight focus group discussions and 33 semi‐structured interviews with Khmu villagers and health care workers, exploring beliefs and practices related to nutrition. The setting was two rural districts in Luang Prabang province, in one of which the PHC project had been established for 3 years. There was a higher prevalence of stunting in the Khmu than in other groups. Disaggregation showed nutrition behaviours were associated with ethnicity, including exclusive breastfeeding. Villagers described strong adherence to post‐partum food restrictions for women, while little change was described in intake during pregnancy. Most children were breastfed, although early introduction of pre‐lacteal foods was noted in the non‐PHC district. There was widespread variation in introduction and diversity of complementary foods. Guidance came predominantly from the community, with some input from health care workers. Interventions to address undernutrition in Khmu communities should deliver clear, consistent messages on optimum nutrition behaviours. Emphasis should be placed on dietary diversity for pregnant and post‐partum mothers, encouraging exclusive breastfeeding and timely, appropriate complementary feeding. The impact of wider governmental policies on food security needs to be further assessed.
Keywords: beliefs, child feeding, community based, education, Laos, Khmu, maternal nutrition
Introduction
Since 2009, global focus has been directed towards scaling up a set of cost‐effective direct nutrition interventions during the crucial ‘1000 days’ of opportunity – the period from the beginning of a pregnancy through to a child's second birthday (Horton et al. 2009). Three of the interventions focus on promoting good nutritional practices: exclusive breastfeeding, optimising complementary feeding and good hygiene. Evidence has been mounting on the effectiveness of community‐based and educational interventions as a means to achieving this (Hill et al. 2004; Dewey & Adu‐Afarwuah 2008; 2011a, 2011b).
Despite this attention, chronic malnutrition in children continues to be pervasive in Lao People's Democratic Republic (Laos), in common with many other low‐income and South Asian countries (UNICEF & WFP 2010). This is reflected in high rates of childhood stunting, estimated at 47.4% of children under 5 years (Department of Statistics & UNICEF 2008) and attributed to a combination of inadequate care practices, food security issues and illness (Department of Statistics & UNICEF 2008). Laos is a land‐locked, low‐resource country in Southeast Asia with a small (5.62 million), predominantly rural population. Infant and under 5 years mortality rates are among the highest in Asia (Acuin et al. 2011). The staple food is glutinous rice, though there are ongoing problems with food security, such that two out of three rural households are labelled at risk (World Food Programme 2006).
At the last census, 49 different ethnic groups were recorded in Laos, apart from the dominant Lao speakers (National Statistics Centre 2005). Cultural beliefs related to nutrition abound in all groups, and previous reviews have documented practices such as post‐partum food restrictions, colostrum withholding and introduction of pre‐lacteal foods (Gillespie et al. 2004; Holmes et al. 2007). However, there has been little in‐depth exploration of practices by specific ethnic group, which is necessary to inform nutrition interventions according to local context (World Health Organization 2008).
The Khmu are the second largest ethnic group in Laos (National Statistics Centre 2005), and are based in its mountainous northern areas. They practise subsistence agriculture, mainly shifting cultivation (Insouvanh 2006). They generally speak Khmu, a Mon‐Khmer language, although some have learnt to communicate in Lao. The Khmu are animist and divided into eight patrilineal clans with totems named after animals, birds or plants. These totems are taboo for consumption by clan members and determine whom one can marry (Gross 1999).
In the north of Laos, a successful primary health care (PHC) programme managed by Save the Children has been running for over 10 years, beginning in Sayaboury province and now extending into Luang Prabang province. Its comprehensive approach includes improving health infrastructure, as advocated by the Alma Ata declaration, and has seen significant improvements in maternal and child health indicators (Perks et al. 2006). Infant mortality in Sayaboury province is estimated at 19 per 1000 (Primary Health Care Project 2009), compared with a national rate of 42 (UNICEF 2010). The programme recognises the effects of undernutrition in local communities and currently addresses this through a combination of health worker training and community nutrition education. In‐service training for health care workers includes a module on nutrition and growth monitoring, while village‐selected health volunteers are trained in giving basic nutrition messages. In addition, communities are targeted through biannual village outreach visits, during which teams stay overnight to deliver health education at a village meeting, often using DVDs in minority languages and posters. The following day, clinical and health promotion activities are held in the village, including growth monitoring and nutrition counselling.
However, given the cultural diversity within implementation areas, Save the Children identified that this approach required further differentiation to better serve rural and isolated ethnic groups, who have higher rates of childhood stunting. Our study was carried out under the auspices of the PHC project, which is now operating in areas of majority Khmu ethnicity. The aim was to understand how to adapt the content and delivery of the PHC's current nutrition interventions for maximum impact on the Khmu ethnic group. For background, we assessed the prevalence of key nutrition behaviours among the Khmu through disaggregated analysis of a national dataset. We then explored cultural beliefs and practices, and the reasons behind these, through qualitative fieldwork. An additional aim was to explore the situational context of the Khmu, in particular their interaction with, and experience of, health care in order to inform priorities for the future.
Key messages
-
•
There is wide variation in maternal and child feeding practices among the Khmu ethnic group, in particular some practices (post‐partum food taboos and early introduction of pre‐lacteal foods) that are linked to strong cultural beliefs.
-
•
However, some of these practices are changing, particularly where there has been strong investment in strengthening the primary health care system so it provides clear, consistent messages and promotes local participation through training of community health workers.
Materials and methods
Quantitative data
We obtained access to the national dataset for the last Multiple Indicator Cluster Survey (MICS) carried out in Laos between March and June 2006 (http://www.childinfo.org). This was based on MICS3 questionnaires and consisted of a household questionnaire, a women's questionnaire (15–49 years) and a questionnaire for children under 5. Interviews were conducted in 5894 households, with an average household size of 5.6. Four thousand two hundred and four children under 5 were identified, of whom 4136 were successfully interviewed. The survey also collected anthropometric data and assessed food consumption through 24‐h dietary recall. We extracted information on relevant anthropometric and nutrition indicators and disaggregated it by ethnicity. Descriptive analyses were carried out in Stata 10 (Stata Corp, Texas).
Study site for qualitative work
Luang Prabang province is in Northern Laos (see Fig. 1). Beyond its relatively affluent capital, it is similar to many other northern rural provinces, with communities living in mountainous areas, following animist traditions and practising subsistence agriculture. Khmu people constitute roughly half of the population. The PHC programme has been active in Nan district for 3 years and began to expand into Nam Bak and Pak Ou districts from late 2010. Two districts were selected for fieldwork: District 1 – Nan district (estimated population 27 000, 36% Khmu) – and District 2 – NamBak (estimated population 79 000, 53% Khmu). In each district, two villages with majority Khmu ethnicity were chosen for qualitative focus group discussions and semi‐structured interviews; one village closer to the road, and one more remote. The population of these villages ranged from 60 to 170 families. In Nan district, 91% of the population live within 5 km or 60 minute walk of a health facility due to PHC inputs, while in NamBak district, this is true for only 43% of the population.
Figure 1.
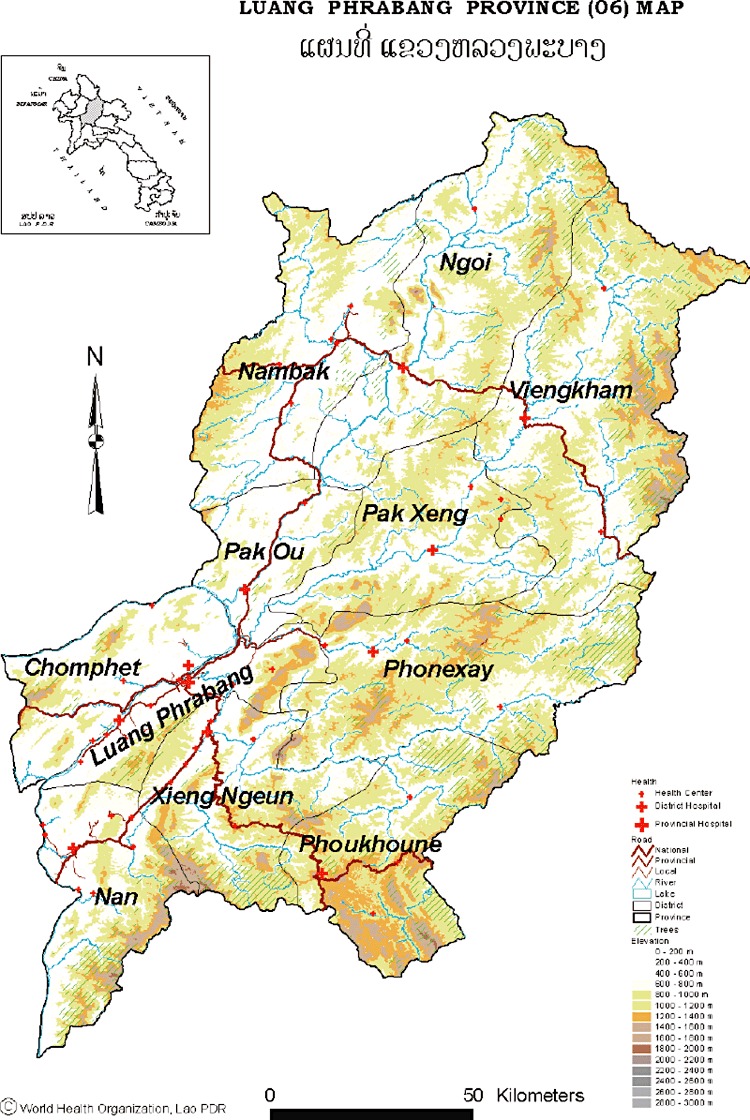
Map of Luang Prabang province.
Qualitative data collection
In the formative study, we used qualitative methods including focus group discussions and semi‐structured interviews to gather detailed information on maternal and child nutrition practices, and the influence of local cultural beliefs on them (Green & Thorogood 2009; Silverman 2009). In collaboration with nutrition advisors and local staff, we developed topic guides focusing on important periods for nutritional intake for mothers (pregnancy and post‐partum) and children (breastfeeding and complementary feeding). We asked about contextual elements such as interaction with health care, livelihoods and other aspects of Khmu culture. Ethical approval was granted by the Lao National Ethics Committee for Health Research and by the Ethics Committee of University College London in UK.
A team consisting of a researcher trained in qualitative methodology (JdS) and a Khmu research assistant (DB), accompanied by a district health official, visited each village for 3 days. Two focus group discussions were held with young mothers and older women in each village: one focusing on pregnancy and post‐partum, the other on child feeding. In addition, in‐depth interviews were held with parents, older members of the community and those in positions of responsibility (village chief, traditional birth attendant, village health volunteer). All focus group discussions and interviews were audio recorded after obtaining oral consent. We conducted 33 semi‐structured interviews: eight with young parents, six with older men and women, seven with village health volunteers and Traditional Birth Attendants (TBAs), four with village chiefs and eight with health care workers. Four health care workers were interviewed at district level (two doctors and two nurses) and four at village clinic level (mid‐level workers who receive 2 years of training.).
Recordings of focus group discussions and interviews were translated directly into English and supplemented by field notes and informal observation throughout the fieldwork. Two researchers (JdS and DB) read through transcripts and field notes repeatedly to identify emerging themes and agree upon a preliminary coding framework. A third researcher (AP) looked independently at a subset of transcripts to verify the themes in the original framework and identify additional ones. A coding framework was agreed, and the remaining transcripts were read and coded by one researcher (JdS). The framework used our main topics of interest – nutrition during pregnancy and post‐partum, breastfeeding and complementary feeding practices – and sub‐themes were identified within these broader categories. In addition, we identified important underlying themes related to the socio‐economic context, which ran through each of the categories mentioned above.
Fieldwork took place in February–March 2011 during the dry season, when villagers were most likely to be at home. Formal feedback sessions were not held in the villages as by completion of fieldwork, villagers had begun preparing rice fields for sowing. A feedback session was held with provincial and district health staff in Luang Prabang.
Results
Disaggregated analysis of national MICS data
Table 1 describes anthropometric and behavioural indicators for Laos' three main ethnic groups (National Statistics Centre 2005): Lao (55% of population), Khmu (11%) and Hmong (8%) and children from other ethnic groups for whom data were collected.
Table 1.
Data on nutrition indicators from Laos' Multiple Indicator Cluster Survey 3, 2006 (disaggregated by ethnicity)
| Lao | Khmu | Hmong | Other | Total | |
|---|---|---|---|---|---|
| Anthropometric indicators † | |||||
| Moderately underweight children <5 years | 29.7% | 31.3% | 22% | 50% | 33.7%* |
| 585/1963 | 173/553 | 121/551 | 477/955 | 1357/4031 | |
| Severely underweight children <5 years | 8.7% | 9.6% | 4.5% | 19.2% | 10.7%* |
| 171/1968 | 53/553 | 25/551 | 183/955 | 432/4031 | |
| Moderately stunted children <5 years | 40.4% | 55% | 53.3% | 60% | 48.9%* |
| 789/1954 | 301/547 | 292/548 | 568/943 | 1953/3996 | |
| Severely stunted children <5 years | 15.4% | 25.1% | 26.3% | 32.1% | 22.1%* |
| 300/1954 | 137/547 | 144/548 | 303/943 | 885/3996 | |
| Moderately wasted children <5 years | 8.8% | 3.6% | 3.5% | 11.1% | 7.9%* |
| 172/1955 | 20/550 | 19/546 | 105/946 | 316/4001 | |
| Severely wasted children <5 years | 1.9% | 1.3% | 0.7% | 2% | 1.7% |
| 38/1955 | 7/550 | 5/546 | 19/946 | 68/4001 | |
| Infants born with birthweight <2.5 kg | 7% | 5.1% | 9.5% | 15.1% | 7.8% |
| 18/255 | 2/39 | 2/21 | 5/33 | 27/348 | |
| Nutrition indicators | |||||
| Infants immediately put to breast after birth | 29% | 27.7% | 24.3% | 16.4% | 25.2%* |
| 224/773 | 62/224 | 55/226 | 62/377 | 403/1601 | |
| Women adhering to post‐partum food restriction after delivery | 80.4% | 88% | 88% | 68.9% | 79.8%* |
| 618/769 | 196/223 | 199/227 | 259/376 | 1273/1596 | |
| Infants aged 0–5 months exclusively breastfed | 16.3% | 47.3% | 57.3% | 8% | 25.1%* |
| 32/196 | 26/55 | 43/75 | 9/112 | 110/438 | |
| Infants aged 12–15 months who continue to be breastfed | 81.2% | 93.2% | 83.3% | 95.1% | 86.8% |
| 121/149 | 41/44 | 35/42 | 78/82 | 275/317 | |
| Infants aged 6–8 months receiving breastmilk and complementary foods | 37.5% | 25% | 29.6% | 63.4% | 40.2% |
| 33/88 | 7/28 | 8/27 | 26/41 | 74/184 | |
*Chi‐squared P < 0.0001. †Using WHO 2006 growth standards (moderate <−2 standard deviations; severe <−3 standard deviations below median).
There was a higher prevalence of stunting among the children from the ethnic minority groups (Khmu and Hmong). Conversely, prevalence of wasting was lower in these groups. An association between ethnicity and anthropometric indicators was observed for all categories apart from severe wasting. A high proportion of women restricted their food intake after delivery, highest among the Khmu and Hmong groups. A quarter of the children were put to the breast immediately, and a quarter of the children were exclusively breastfed, although this was higher in Khmu and Hmong groups. Most children (87% overall) continued breastfeeding until their first birthday. However, very few received complementary foods at the correct age (40% overall, 25% Khmu). For all nutrition behaviours, there was an association with ethnicity. No data were included on the discarding of colostrum.
Qualitative findings
Concepts of growth
Khmu villagers felt that their children were smaller than those of other ethnic groups, and wanted them to be tall and healthy. When asked about factors influencing growth, they described links between nutrition and growth: if children ate less, they were more likely to be small and thin. In some villages, certain foods were thought to promote physical development, rice and chillies in particular.
Pregnancy
Pregnancy was recognised as a change, and most women talked about a desire to improve their nutrition for the baby they were carrying. This involved increasing amounts of food considered as ‘good’, such as meat and fruit, in addition to their mainly vegetable‐based diet, though not the total amount consumed. Some older people mentioned that eating coconut or pork would make the baby fat and cause a more difficult birth. In another village, eating coconut was thought to make delivery easier. Some foods and substances were traditionally considered ‘amlue’ (literally, ‘not good’: taboo), and were avoided. During pregnancy, these included alcohol, betel nut, fermented fish sauce and cigarettes. New restrictions had come about as a result of information provided by health care workers through antenatal care appointments or outreach work.
Khmu communities have a strongly gendered division of work roles. Men are more involved in selection, preparation, sowing and harvesting of the rice fields, whereas women are responsible for the maintenance (e.g. weeding) of the rice field – often a much larger time commitment – as well as helping with other activities (Albone 2011). As a consequence, women continue to work throughout pregnancy, and men may be too busy or reluctant to take on their role.
Post‐partum
Almost without exception, women practised some form of food restriction post‐partum. This was commonly divided into two phases: an initial phase lasting from 2 days to 1 month and a subsequent phase from 3 months to 2 years. The initial phase begins immediately after delivery, when the woman is classified as ‘pa‐el’, or musky smelling. In this phase, she is supposed to eat and sleep separately from the family and was restricted to eating only salt, galangal (from the ginger family) and rice. In some villages, women also sat over or near a small fire in order to ‘dry’ their bodies and prevent further bleeding. Women described sticking rigidly to this restricted diet for up to 1 month despite in some cases crying with hunger.
Suan's story
Suan, about 27 years old, was interviewed post‐partum. She lived in a one‐room hut with her three children, aged ten years, two years and ten days. The room was thick with smoke from the fire in the corner, which she was sitting near in order to help dry her body. She had given birth to all three children in this room, helped only by her husband, and had cut the cord herself. She had no food restrictions during pregnancy and ate her normal diet of wild vegetables, rice and small animals from the forest such as squirrels and birds. Her husband was away in the rice field, where he had been for two days already, preparing the field for sowing, and she was uncertain when he would be back. On his return, he might bring small wild animals he had managed to hunt. During the interview, the ten‐year‐old daughter returned from school and went off to the forest to collect wild vegetables for the evening meal. In this post‐partum period, Suan was restricted to a diet of salt, rice and wild vegetables on the advice of her parents. As a consequence, her children also ate the same diet. Day to day, Suan did not spend money to buy food apart from small necessities and to buy candy (500 kip/ 0.06 USD) demanded by the two‐year‐old.
After the initial period of restriction, women were able to share food with their families and were no longer considered unclean. However, in all villages, they were encouraged to eat only certain foods, most commonly chicken, duck and vegetables. Caution was advised on eating other foods for a period of 3 months to 2 years due to the risk of pit duen, loosely translated as ‘post‐partum sickness’. Pit duen has a range of manifestations, including fever, body ache, numbness, tingling, weakness, bleeding and at worst, death. Information on foods known to have caused pit duen was shared between members of the community and handed down from parents to children (Table 2). There were some similarities between foods mentioned in the four villages: animals with red or white skin, forest animals, sour food 1 and ‘stinky food’. 2 The main person described as affected by the consumption of taboo food was the mother, and she mediated the effect on the baby; for example, if the illness continued, breastmilk supply might be affected.
Table 2.
Taboo foods mentioned for post‐partum period in village 1 and source of information
| Taboo food | Source of information | |||
|---|---|---|---|---|
| Community | Parents | Health care workers | ||
| Meat | Animals with white skin | ✓ | ✓ | |
| Animals with red skin | ✓ | ✓ | ||
| Deer | ✓ | |||
| Dog | ✓ | |||
| Bamboo rat | ✓ | |||
| Frog | ✓ | |||
| Cow | ✓ | |||
| Post‐partum pig/male pig | ✓ | |||
| Fish | Panae fish | ✓ | ✓ | |
| Snails | ✓ | |||
| Paa dek (fermented fish paste) | ✓ | ✓ | ||
| Vegetable | River weed | ✓ | ||
| Bitter, strong smelling vegetable | ✓ | ✓ | ||
| Hairy vegetables | ✓ | ✓ | ||
| Mushroom | ✓ | |||
| Dtao (type of bamboo) | ✓ | |||
| Taro leaf | ✓ | |||
| Cassava leaf | ✓ | |||
| Pumpkin leaf | ✓ | |||
| Fruit | Fruit with white sap | ✓ | ||
| Yellow papaya | ✓ | |||
| Other | Alcohol | ✓ | ||
| Smoking | ✓ | |||
| Chewing betel nut | ✓ | |||
| Monosodium glutamate | ✓ | |||
| Sour food | ✓ | ✓ | ||
| Stinky food | ✓ | ✓ | ✓ | |
| Spicy food | ✓ | ✓ | ||
In every interview and focus group discussion, powerful examples of lived experience of pit duen were mentioned. This created problems when contrasting messages (encouraging diverse consumption) were given through health care workers and mass media such as radio broadcasts. Women described being scared of trying different foods when they knew that a high risk of pit duen was involved. For those who had survived post‐partum sickness, the cure was described as a mix of traditional herbal medicines and ‘hospital’ medicine. However, women also reported that eating taboo food did not automatically cause pit duen. Some women inadvertently ate it with no adverse consequences, leading to the conclusion that food was not taboo for them. In contrast, there were some cases where women had eaten traditionally accepted food, such as chicken, and experienced symptoms of pit duen, implying that this food had become taboo for them. With this element of variability, it was difficult for women to decide what was safe or unsafe to eat, with the result that many ‘listened to their bodies’ and safeguarded their health by avoiding any foods that were associated with pit duen. The consequence was a severely restricted diet, as many taboo foods form part of everyday diets.
Interview with young mother, village 3
M: Two months after she gave birth, my sister did not avoid any food. She ate [taboo] food and she died.
I: What did she eat and why did she die?
M: She ate papaya and fermented fish mixed with tamarind, and also shrimp paste.
I: How long after she ate [that] did she get sick?
M: Five or six days afterwards, she got dizzy and [said she had a] headache and then she fell down and died.
I: Do you think she died because of the taboo food or because of something else?
M: Because she ate the taboo food.
There were some examples of ‘positive deviants’ who ate many foods without restriction. These tended to be women with regular interactions with the health care sector – commonly those trained as traditional birth attendants (TBA) – or those who had sought antenatal care and delivered in facilities. This was more marked in Nan District, which had 3 years of strengthening of the primary health care system.
Breastfeeding
Breastfeeding was common in all the villages and was observed throughout focus group discussions and interviews: ‘Everyone here breastfeeds their babies’ (FGDA2). The benefits for babies were well known, and mothers started breastfeeding on the first day. Although colostrum had traditionally been discarded and regarded as ‘dirty’, many women in both districts had heard and understood the message that it was good for the baby and, consequently, women in all four villages reported giving colostrum. Initiation of breastfeeding was also dependent on women getting their breasts ready. This involved showering both mother and baby so that they were both ‘clean’ and massaging the breasts to encourage creation of a hole in the nipple for the milk to drain through.
Infants were fed on demand, usually on crying. Problems were rarely described with the mechanics of breastfeeding, although women acknowledged that it hurt and occasionally they were shy about breastfeeding in public. If they felt their supply was low, they would drink hot water, soup or traditional medicine and, if severe, ask other mothers to wet‐nurse their babies. Some women mentioned giving their babies condensed milk as a breast milk substitute, but this was observed to make babies more sickly. Powdered milk was considered prohibitively expensive and was only used as a short‐term measure. In the district without the PHC project, many families considered that breast milk alone was insufficient for babies' needs, and pre‐lacteal feeds were introduced as early as the first day of life, mainly consisting of pre‐masticated glutinous rice barbecued in banana leaves in the fire (see Fig. 2).
Figure 2.
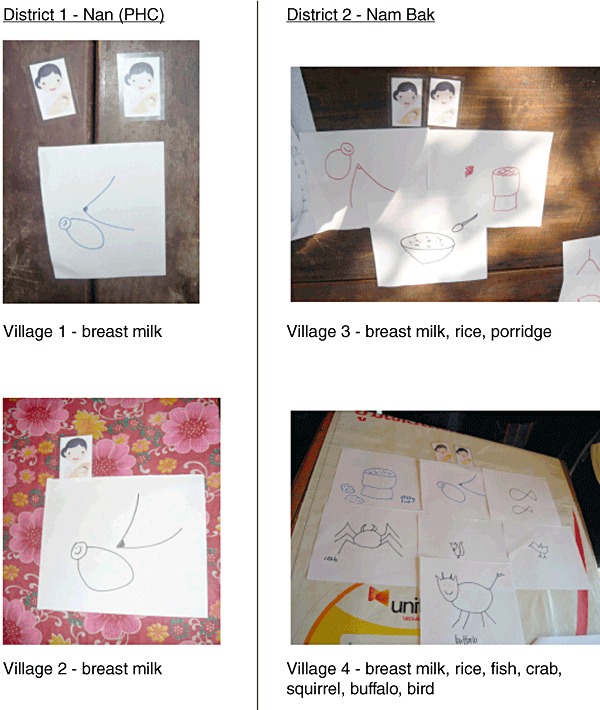
Example from focus group discussion of foods given to a newborn infant in the four villages.
If babies were thin or sickly, this was ascribed to poor quality breast milk. Quality of breast milk was understood to be affected by ill health, poor nutritional intake or ingestion of taboo food. In one village, working in hot conditions was thought to turn the breast milk sour, leading mothers to expel the initial breast milk upon returning home before feeding their babies. Continued breastfeeding was made difficult by the need for mothers to return to work in the fields. In some villages, they took their babies with them, while in others, babies were left with grandparents who fed them with glutinous rice or took them to other post‐partum mothers in the village to be wet‐nursed. Work was also the main reason for stopping breastfeeding, often around 1 year of age.
Complementary feeding
There was wide variation in the age at introduction of complementary food. In the first two villages, the message of exclusive breastfeeding for the first 6 months was eagerly repeated during focus groups and interviews. However, while the message was understood, many parents were uncertain of the exact age of their baby. Some parents used developmental milestones to initiate extra feeding: ‘When they start to sit and grab things then we will give them. If they still cannot sit then we will not give to them’ (FGDA3). There were also disparities in the foods initially introduced. Some started with khatom (rice porridge) with added small pieces of meat and vegetable. Others mentioned starting with chewed glutinous rice and then gradually introducing other foods such as small pieces of barbecued fish or meat. Some parents waited until the age of 1 year to introduce more diverse foods such as fruits due to lack of knowledge on how to prepare them for younger children.
Interview with young parents, village 1
I: So when he was 6 months what food did you give your baby? Besides rice and water what else?
F: only the rice in banana leaf, but [we] still did not mix with other food and water.
I: At what age [did] you start to give him rice mix[ed] with other kinds of food?
F: When he is one year [old]. [When he is] one year [old], he is big.
Children were fed more often than adults, although it was often up to them to demand food. If they did not want to eat, parents described trying to coax them, threatening them or giving up and buying candy. If a child was thought to be ill, spicy or salty food was avoided, and parents encouraged consumption of ‘good’ foods such as squirrel or duck. However, in many cases, parents were unsure what to do if their child was ill. Good hygiene was apparent in all four villages as participants emphasised the importance of hand washing before preparing meals and feeding children. This was facilitated by relatively easy access to water in three villages.
Contextual factors
These were grouped into five themes: access to food, poverty, sources of information, interaction with health care and attitude to change. Villagers described the constraints of subsistence agriculture on their diet and a traditional reliance on natural resources: ‘We stay with nature, we should give natural food’ (FGDA1). Income poverty resulted in few Khmu accessing food at markets and from travelling salespeople. There were some instances of families who had started to grow cash crops such as Job's tear (Coix lacryma‐jobi). Poverty was also described as a barrier to accessing health care services, which operate on a user‐fee basis. Villagers in the first district described reliance on the outreach services provided by the PHC project, at which they also felt able to develop good relationships with health care staff. For many villagers, formal health care was a relatively recent phenomenon. Health care staff were seen as better informed than community members, which seemed to inspire trust. However, this relationship of trust only extended to practices that did not contravene strongly held community beliefs. For example, in the case of post‐partum food taboos, new mothers tended to rely on their mothers for instruction on what to do.
Interview with young mother of 8‐month‐old baby, delivered in district hospital
I: and what about, did they (the doctors) tell you about what to eat after you gave birth?
M: they said [I] should not avoid any food, [I] should eat every thing – food that has good nutrition, eat apple, and meat and many more things. But my parents do not allow me to eat, they are afraid that I will get post‐partum sickness
I: and who do you listen to out of your mother and the nurse?
M: I listen to my parents
Health care workers, for their part, were familiar with differing nutrition practices among ethnic groups. Most were able to recommend nutrition actions for mothers and children in line with best practice recommendations. Some had learned basic Khmu through exposure, but all mentioned significant communication difficulties. Translation was often through other members of the family, particularly men, who had learned to speak some Lao. The staff stressed the importance of including men and grandmothers in nutrition counselling, recognising them as influential sources of information. Some Khmu villagers described feeling discriminated against when accessing health care services. Instances of being overcharged were mentioned. However, despite probing, no health care staff mentioned negative perceptions of the Khmu, and some described them as ‘easier’ to work with than other groups such as the Hmong. Change was acknowledged in the first district, and repetition of messages was cited as one of the reasons for successful behaviour change. At the feedback meeting, findings were in keeping with people's own experiences of working with Khmu communities. Reiteration was made of the fact that health care services and nutrition education need to be more inclusive of minorities.
Discussion
Our study confirms the higher prevalence of stunting in children of ethnic minority groups, particularly the Khmu, which has been described in other studies (World Food Programme 2006; Phengxay et al. 2007; Kamiya 2011). Undernutrition results from an interaction between insufficient intake and illness (Black et al. 2008). In this study, we focused on nutrition behaviours in order to inform the nutrition education component of the PHC intervention. There has also been recent regional focus on nutrition behaviours which are likely to play a significant role in contributing to the high rate of stunting (UNICEF & WFP 2010).
In terms of maternal nutrition, women describe some attempt to improve the diversity of their diet when pregnant, though not the total amount consumed. When considering energy expended on hard physical labour, which most women continue throughout pregnancy, increasing diversity alone may not be sufficient for their needs and may have consequences for fetal nutrition (Kramer & Kakuma 2003). Interestingly, the phenomenon of ‘eating down’ (Brems & Berg 1989) to ensure an easier delivery, common in other Asian cultures, was not mentioned by any villagers.
There is strong adherence to food taboos post‐partum, though there was some evidence of change in women with a strong engagement with health care. The idea of taboo is deeply embedded within Khmu culture (Gross 1999) and, indeed, post‐partum food taboos are strongly respected in all ethnic groups in Laos, even in urban areas (Holmes et al. 2007; Barennes et al. 2009). Throughout Asia, other examples of post‐partum food restriction are also common: ‘phit kam’ in Thailand (Thasanoh 2011) and 'toas' in Cambodia (White 2004). In Laos, maternal mortality is still very high – 580 per 100 000 live births in 2008 (UNICEF 2010) – and it has been suggested that post‐partum food restrictions are a manifestation of the perceived dangers of the post‐partum period. Certainly, in focus groups and interviews, women felt that adhering to food restrictions ‘safeguarded’ their health and prevented them from having to field potentially catastrophic expenditure on health care. Extreme post‐partum restriction such as that practised in the first phase, where women eat only rice, salt and galangal, is unlikely to provide enough energy, protein or micronutrients, with consequences for the nutritive quality of breast milk (Allen 1994).
Encouragingly, most babies are breastfed. However, pre‐lacteal foods, mostly glutinous rice and water, are introduced early, particularly in the second district. Previous studies had documented discarding of colostrum in the Khmu ethnic group (Gillespie et al. 2004; Holmes et al. 2007). However, change was reported in this practice with most mothers reporting feeding their babies with their ‘first yellow milk’. Factors mentioned included hearing a concordant message from multiple sources and, more importantly, the recommendation of grandparents and community elders. However, ongoing exclusive breastfeeding is hampered by the necessity for mothers to return to work. Laos is almost unique in Asia in that almost all infants are breastfed at some point, though with a low rate of exclusive breastfeeding compared to other Asian countries (Dibley et al. 2010). A recent national campaign, designed by UNICEF, has attempted to address this through training at provincial, district and village levels combined with a national media campaign.
Interestingly, breast milk substitutes were not commonly used in both districts, other than as short‐term measures. This is in contrast to other studies which have found widespread use of inappropriate substitutes such as coffee creamer (Barennes et al. 2008) in the belief that these products may be beneficial for infant health. These beliefs are encouraged by increasing exposure to advertising of infant formula on Thai television channels (Putthakeo et al. 2009). As many of the Khmu families have little disposable income and are often very physically remote, these factors also limit their ability to purchase breast milk substitutes.
There was wide variation in age at introduction of complementary foods and range of foods given to children. Although parents in the first district reported exclusive breastfeeding until the age of 6 months, we found that they were often unsure of the exact age of their child. Diversity of foods and textures was also lacking, predominantly due to limited knowledge of how to prepare foods appropriately for infants. Mashing and boiling are easily performed, and most households have the requisite implements. Findings were similar to analyses in Cambodia which suggest that younger children (6–11 months) are not fed appropriately with diverse diets, but that this may improve as they become older (Marriott et al. 2010). Timely complementary feeding is difficult in many countries in Asia but remains particularly low in Laos (Dibley et al. 2010).
Limitations
The study had some limitations. The quantitative data extraction used data collected in 2006. Since then, the Lao government has launched a national nutrition strategy and, although implementation has been variable, some of its effects will be felt now. For the qualitative component, the team was accompanied to each village and health centre by a district health official, in line with government regulations. This may have influenced the answers that participants gave. Although the research assistant (DB) was Khmu and familiar with conducting research in rural communities, linguistic and cultural differences may have influenced respondents.
Implications for future interventions
Our study aimed to advise the Primary Health Care project on how to adapt its nutrition intervention so as to have maximum impact in the Khmu ethnic group. While this group are the majority in the project areas, the intervention also needs to account for other ethnic groups. The current intervention uses in‐service training to equip health care workers to recognise undernutrition and give appropriate nutrition counselling during planned and informal clinical encounters. Community health care workers – village health volunteers and traditional birth attendants – are also encouraged, after training, to hold village meetings to share information on good nutritional practices.
From this formative study, there is some evidence that the current nutrition interventions are working. Health care workers mentioned job satisfaction and described seeing the effects of their work as additional motivation. In Sayaboury province, where the PHC project has been active for over 10 years, there are high breastfeeding rates, with a mean age at introduction of complementary foods of 5.2 months (Primary Health Care Project 2009). The structure of the intervention (in‐service training with community outreach activities) is firmly embedded within the project's roll‐out, which has been developed over a number of years with strong local ownership. However, there is scope for the content and delivery of the intervention to be adapted to help deliver clear, consistent health messages.
In terms of content, the recent Lancet series on undernutrition highlighted the importance of promoting complementary feeding and other supportive activities as the most likely strategies to decrease the prevalence of stunting (Bhutta et al. 2008). Strategies to promote complementary feeding include family counselling, nutrition education, provision of high energy and protein food supplements, provision of snacks using locally available foods and specific feeding advice and cooking demonstrations (Hill et al. 2004). Of these, the current intervention encompasses all but provision of food supplements and cooking demonstrations.
Encouraging families to provide more diverse and appropriate diets for their children has been found to be beneficial in food‐secure populations (Bhutta et al. 2008). However, food insecurity is a continuing issue in Laos, meaning that suggestions for recipes and snack foods need to be carefully considered. An intervention comprising educational messages and enhanced home‐prepared recipes delivered through group training and home visits was successful in rural China in improving food diversity, meal frequency and hygiene practices with some gains in weight and height (Shi et al. 2010).
We have therefore highlighted messages, using the Essential Nutrition Actions framework (Guyon & Quinn 2011) that reflect this focus on optimising complementary feeding, as well as identifying simple messages to improve nutrition for pregnant and post‐partum women (see Fig. 3). The training modules for health care workers and community volunteers will be reviewed to ensure that these messages are incorporated.
Figure 3.
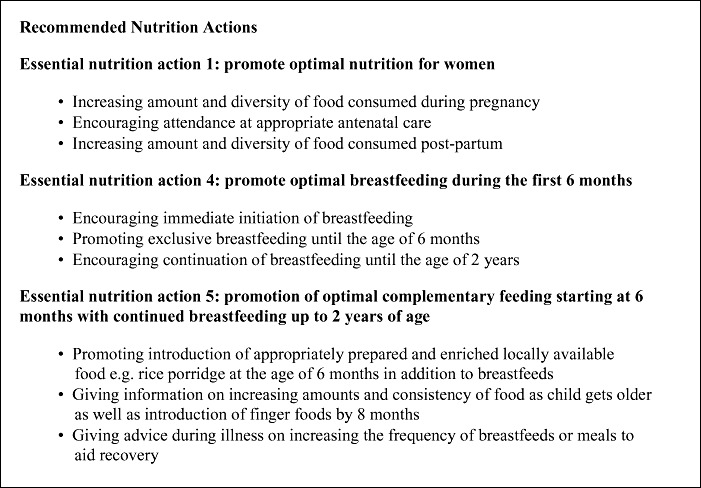
Recommended essential nutrition actions.
Delivery of these messages will continue through the current channels of planned and informal clinical encounters, as well as through community outreach. Home visits by health care workers are not feasible due to distances and transport logistics, but existing community health volunteers in each village are capable of delivering simple nutrition education messages. The PHC project has successfully utilised a system of pictorial flipcharts with basic messages on a variety of subjects as job aids for health care workers, as has been found in other studies (Jennings et al. 2010). From the results of the formative study, a pictorial flipchart has been developed on infant and young child feeding with key messages and pictures of locally available foods and recipe suggestions.
To address the issue of exclusion of ethnic minorities, it is important to include all members of the community in nutrition education, as exemplified by the outreach component, as young parents often rely on their own parents as the main source of information on appropriate feeding behaviours. Using community health workers to give nutrition education in their own language may be more acceptable to older people than health care workers from different cultural backgrounds. Although our project placed more emphasis on community‐level interventions to address maternal and child undernutrition, it is important to acknowledge health system and wider socio‐economic changes that can facilitate improvement (Montpellier Panel 2009). The PHC project promotes access to family planning to reduce repeated pregnancies that might influence maternal undernutrition and morbidity (Conde‐Agudelo et al. 2006). In addition, the project works to improve access to hygiene and sanitation in order to address issues around infection and safe food preparation (Bartram & Cairncross 2010).
Rural communities in Laos rely on natural resources for food, medicine, income and fuel, and recent government regulations have attempted to institute national resource governance for sustainable use, such as the introduction of hunting regulations and the banning of shifting cultivation, commonly used by Khmu communities (WCS Translinks 2010). Regulations clearly need to be in place in order to ensure that rural communities can continue to access resources but must form part of a coherent nutrition framework that provides viable alternatives to such communities to ensure ongoing food security.
Source of funding
This work was undertaken at the UCL Institute of Child Health, which received a proportion of funding from the Department of Health's NIHR Biomedical Research Centres funding scheme.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
JdS, LS, CP and AP conceived the study. JdS, NB and AP analysed and interpreted the data. JdS wrote the first draft of the manuscript. NB, LS, CP, AP and DO assisted in the interpretation of results. All co‐authors participated in manuscript preparation and critically reviewed all sections of the text for important intellectual content.
Acknowledgements
Thanks to Luang Prabang Provincial Health Department for facilitating the research. Thanks to Naomi Saville, Technical Advisor MIRA Nepal, and Jutta Krahn, Nutrition Consultant in Laos for help with development of topic guides and advice on nutrition and food security aspects of the project.
Re‐use of this article is permitted in accordance with the Terms and Conditions set out at http://wileyonlinelibrary.com/onlineopen#OnlineOpen_Terms.
Footnotes
Unripe fruits such as green mangoes and other indigenous sour‐tasting fruits and vegetables were described as ‘sour food’.
‘Stinky food' refers to foods that are preserved by pickling or drying, often lending a distinctive smell.
References
- Acuin C.S., Khor G.L., Liabsuetrakul T., Achadi E.L., Htay T.T., Firestone R. et al (2011) Maternal, neonatal, and child health in southeast Asia: towards greater regional collaboration. Lancet 377, 516–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albone S. (2011) Care International in Lao PDR: Study on Barriers to Accessing Maternal, Child and Reproductive Health Services for Remote Ethnic Groups and Vulnerable Urban Women. Vientiane.
- Allen L.H. (1994) Maternal micronutrient malnutrition: effects on breastmilk and infant nutrition, and priorities for intervention. SCN News , 21–24. [PubMed]
- Barennes H., Andriatahina T., Latthaphasavang V., Anderson M. & Srour L.M. (2008) Misperceptions and misuse of Bear Brand coffee creamer as infant food: national cross sectional survey of consumers and paediatricians in Laos. BMJ (Clinical Research ed.) 337, a1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barennes H., Simmala C., Odermatt P., Thaybouavone T., Vallee J., Martinez‐Aussel B. et al (2009) Postpartum traditions and nutrition practices among urban Lao women and their infants in Vientiane, Lao PDR. European Journal of Clinical Nutrition 63, 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartram J. & Cairncross S. (2010) Hygiene, sanitation, and water: forgotten foundations of health. PLoS Medicine 7, e1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta Z.A., Ahmed T., Black R.E., Cousens S., Dewey K., Giugliani E. et al (2008) What works? Interventions for maternal and child undernutrition and survival. Lancet 371, 417–440. [DOI] [PubMed] [Google Scholar]
- Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., De Onis M., Ezzati M. et al (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. [DOI] [PubMed] [Google Scholar]
- Brems S. & Berg A. (1989) Eating down during pregnancy: nutrition, obstetric and cultural considerations in the third world. Paper prepared for the 1988 and 1989 meetings of the UN Advisory Group on Nutrition of the ACC Sub‐Committee on Nutrition. Geneva: ACC/SCN.
- Conde‐Agudelo A., Rosas‐Bermudez A. & Kafury‐Goeta A.C. (2006) Birth spacing and risk of adverse perinatal outcomes: a meta‐analysis. JAMA: The Journal of the American Medical Association 295, 1809–1823. [DOI] [PubMed] [Google Scholar]
- Department of Statistics & UNICEF (2008) National Maternal and Child Nutrition Survey Final Report 2006. Vientiane.
- Dewey K.G. & Adu‐Afarwuah S. (2008) Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal & Child Nutrition 4 (Suppl. 1), 24–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dibley M.J., Senarath U. & Agho K.E. (2010) Infant and young child feeding indicators across nine East and Southeast Asian countries: an analysis of National Survey Data 2000–2005. Public Health Nutrition 13, 1296–1303. [DOI] [PubMed] [Google Scholar]
- Gillespie A., Creed‐Kanashiro H., Sirivongsa D., Sayakoummane D. & Galloway R. (2004) Consulting with Caregivers: Using Formative Research to Improve Maternal and Newborn Care and Infant and Young Child Feeding in the Lao People's Democratic Republic. HNP World Bank: Washington, DC. [Google Scholar]
- Green J. & Thorogood N. (2009) Qualitative Methods for Health Research. SAGE: London. [Google Scholar]
- Gross M. (1999) Community Portrait: Khmu[Online]. San Francisco: Wildflowers Institute. Available at: http://www.wildflowers.org/community/LaoKhmu/khmu_portrait.shtml (Accessed 31 May 2011).
- Guyon A. & Quinn V. (2011) Booklet on Key Essential Nutrition Actions. Core Group: Washington D.C. [Google Scholar]
- Hill Z., Edmond K. & Kirkwood B. (2004) Family and community practices that promote child survival, growth and development: a review of the evidence. World Health Organization.
- Holmes W., Hoy D., Lockley A., Thammavongxay K., Bounnaphol S., Xeuatvongsa A. et al (2007) Influences on maternal and child nutrition in the highlands of the northern Lao PDR. Asia Pacific Journal of Clinical Nutrition 16, 537–545. [PubMed] [Google Scholar]
- Horton S., Shekar M., McDonald C., Mahal A. & Brooks J.K. (2009) Scaling up Nutrition: What Will It Cost? World Bank: Washington. [Google Scholar]
- Imdad A., Yakoob M.Y. & Bhutta Z.A. (2011a) Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health [Electronic Resource] 11 (Suppl. 3), S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imdad A., Yakoob M.Y. & Bhutta Z.A. (2011b) Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health [Electronic Resource] 11 (Suppl. 3), S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insouvanh C. (2006) Social Exclusion and Gender Discrimination of Khmu People in the Lao PDR. Eighth Annual Southeast Asian Studies Graduate Students' Symposium. Cornell University: Ithaca, NY. [Google Scholar]
- Jennings L., Yebadokpo A.S., Affo J. & Agbogbe M. (2010) Antenatal counseling in maternal and newborn care: use of job aids to improve health worker performance and maternal understanding in Benin. BMC Pregnancy and Childbirth 10, 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamiya Y. (2011) Socioeconomic determinants of nutritional status of children in Lao PDR: effects of household and community factors. J Health Popul Nutr 29, 339–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.S. & Kakuma R. (2003) Energy and protein intake in pregnancy. Cochrane Database of Systematic Reviews (4), CD000032. [DOI] [PubMed] [Google Scholar]
- Marriott B.P., White A.J., Hadden L., Davies J.C. & Wallingford J.C. (2010) How well are infant and young child World Health Organization (WHO) feeding indicators associated with growth outcomes? An example from Cambodia. Maternal & Child Nutrition 6, 358–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montpellier Panel (2009) Scaling Up Nutrition: A Framework for Action.
- National Statistics Centre (2005) National Census – Lao People's Democratic Republic. Vientiane.
- Perks C., Toole M.J. & Phouthonsy K. (2006) District health programmes and health‐sector reform: case study in the Lao People's Democratic Republic. Bulletin of the World Health Organization 84, 132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phengxay M., Ali M., Yagyu F., Soulivanh P., Kuroiwa C. & Ushijima H. (2007) Risk factors for protein‐energy malnutrition in children under 5 years: study from Luangprabang province, Laos. Pediatrics International: Official Journal of the Japan Pediatric Society 49, 260–265. [DOI] [PubMed] [Google Scholar]
- Primary Health Care Project (2009) Sayaboury Province Cluster Sample Health Survey. Vientiane: Save the Children Australia.
- Putthakeo P., Ali M., Ito C., Vilayhong P. & Kuroiwa C. (2009) Factors influencing breastfeeding in children less than 2 years of age in Lao PDR. Journal of Paediatrics and Child Health 45, 487–492. [DOI] [PubMed] [Google Scholar]
- Shi L., Zhang J., Wang Y., Caulfield L.E. & Guyer B. (2010) Effectiveness of an educational intervention on complementary feeding practices and growth in rural China: a cluster randomised controlled trial. Public Health Nutrition 13, 556–565. [DOI] [PubMed] [Google Scholar]
- Silverman D. (2009) Doing Qualitative Research. Sage Publications: London. [Google Scholar]
- Thasanoh P. (2011) Northeast Thai Women's Experiences in Following Traditional Postpartum Practices. PhD, University of California San Francisco.
- UNICEF (2010) Lao People's Democratic Republic: Statistics[Online]. Available at: http://www.unicef.org/infobycountry/laopdr_statistics.html (Accessed 18 March 2012).
- UNICEF & WFP (2010) Asia‐Pacific Regional Workshop on the Reduction of Stunting through Improvement of Complementary Feeding and Maternal Nutrition. Bangkok.
- WCS Translinks (2010) Wildlife Management and Household Food Consumption in Lao PDR. Wildlife Conservation Society: Vientiane. [Google Scholar]
- White P.M. (2004) Heat, balance, humors, and ghosts: postpartum in Cambodia. Health Care for Women International 25, 179–194. [DOI] [PubMed] [Google Scholar]
- World Food Programme (2006) Lao PDR: Comprehensive Food Security and Vulnerability Analysis. Vientiane.
- World Health Organization (2008) Strengthening Action to Improve Feeding of Infants and Young Children 6–23 Months of Age in Nutrition and Child Health Programmes: Report of Proceedings 6–9 October 2008. Geneva.


