Abstract
Introduction
Here we estimate the direct medical costs to the National Health Service (NHS) of unintended pregnancies in 2010 and identify populations at risk for unintended pregnancies.
Methods
The number of unintended pregnancies in England in 2010 was estimated based on the number of induced and spontaneous abortions, live births and ectopic pregnancies reported by the NHS and Office for National Statistics. Direct medical costs associated with these were obtained from the NHS Reference Costs.
Results
In 2010, there were an estimated 225,600 unintended pregnancies in England, of which 218,100 were paid for by the NHS. Of these, 155,500 led to induced abortions, 53,900 to births, 7,500 to spontaneous abortions and 1,200 to ectopic pregnancies. These unintended pregnancies cost the NHS £193,200,000 ($306,100,000) in direct medical costs.
Discussion
London, the North West and the West Midlands should be targeted in efforts to reduce unintended pregnancies. More specifically, women between the ages of 20 and 34 years produce the greatest costs.
Keywords: Unintended pregnancy*, unwanted pregnancy*, cost analysis, budget impact, England
1. Introduction
Amongst developed countries, England has the highest rate of unintended pregnancy after the United States (US) [1–5]. Compared to the US, where contraceptive coverage is limited by insurance and reimbursement difficulties, contraception in England is provided free of charge by the National Health Service (NHS) and is used by 88% of women at risk of pregnancy [6]. Be it from method failures, improper contraceptive use, or non-use of contraception, it has previously been assumed (based on US data) that half of all pregnancies each year are unintended [4]. These pregnancies generate substantial direct costs to the NHS, but also create indirect costs – in the form of productivity decreases and welfare payments – shouldered by society at large.
Here we estimate the direct medical cost of unintended pregnancies to the NHS in 2010. In 1995, McGuire [7] calculated the medical and social cost of unintended pregnancies to the UK. Modifications to the NHS’ structure, the rise in the occurrence of cesarean sections, and other changes to the English health care industry are likely to have affected the costs of all procedures carried out under the NHS’ umbrella, making a more current analysis necessary [8]. In addition, we provide estimates by region and age group. Our analysis takes into account the large difference in costs of mistimed and unwanted births, so that medical costs are not vastly overstated [9]. Using these estimates, policy-makers and health care professionals can better target their interventions and resources at the populations that are most at risk.
2. Methods
2.1. Pregnancy outcomes
The number of live births was taken from the Office for National Statistics (ONS) 2010 birth summary tables of England and Wales [10]. The number of pregnancies leading to induced abortions was taken from the ONS 2010 abortion statistics [11]. The number of pregnancies leading to spontaneous abortions and ectopic pregnancies was estimated based on 2009–2010 data from Hospital Episode Statistics (HES), adjusted upwards as in the National Institute for Clinical Excellence (NICE) Long-Acting Reversible Contraception (LARC) Clinical Guideline [4,12,13].
Based on recent results from a study in Edinburgh, we assumed that 90%, 8% and 12% of induced abortions, births and spontaneous abortions, respectively, resulted from an unintended pregnancy (Table 1) [14]. We assumed that the proportion of ectopic pregnancies stemming from unintended pregnancies was the same as for spontaneous abortions, as the occurrence of both is independent from women’s choices.
Table 1.
Proportion of pregnancy outcomes stemming from unintended pregnancies and cost of each outcome to the NHS
| Birth | Induced abortion | Spontaneous abortion | Ectopic pregnancy | |
|---|---|---|---|---|
| Proportion unintended[13] | 12% | 90% | 8% | 8% |
| Cost per event[4,7,18] | £1,579 a ($2,455) | £919 ($1,422) | £375 ($580) | £2,426 ($3,758) |
This is the cost of an unwanted birth. The cost of an unintended birth in Table 2 is the weighted average of the costs of unwanted and mistimed births: £1,579 (1-f/(1=r)d, where f is the fraction mistimed among unintended births, r is the discount rate, and d is the number of years the mistimed birth would have been delayed; f and d are age-specific.
All estimates are age-specific, by 5-year age groups used in ONS birth and induced abortions statistics as well as HES spontaneous abortions and ectopic pregnancies statistics. In addition, estimates based on births and induced abortions are region-specific. Estimates of outcomes of unintended pregnancies (1) for each age group were summed across regions to obtain the national total by age and (2) for each region were summed across age groups to obtain the regional total. These, in turn, were divided by the corresponding number of women to obtain the rates of unintended pregnancy outcomes per 1,000 women in each age group nationally and per 1,000 women aged 15–44 in each region [15].
2.2. Costs
Not all unintended pregnancies are unwanted; most (60%) are mistimed, and would have occurred as intended births at a later date. If an unintended birth is unwanted (i.e., the woman did not want a child now or in the future), then the cost is a social deadweight loss. An unintended birth that is mistimed (i.e., occurs sooner than intended), however, would have occurred as an intended birth later. Therefore, the actual cost of the mistimed birth is the cost of not postponing that birth: if £B is the cost of an unwanted birth, the cost of a mistimed birth is only £B(1–1/(1+r)d, where r is the rate of discount and d is the number of years by which the birth would have been delayed [9]. The proportion of mistimed births and the extent of their mistiming (i.e., the number of years before the birth would have been intended) is age-specific, based on data from the US National Survey of Family Growth [16]. We used a discount rate of 3.5%, as per the NICE guidelines [17].
This analysis was conducted from the perspective of the NHS. We assumed that 100% of spontaneous abortions and ectopic pregnancies were paid for by the NHS, a percentage which dropped to 96.7% for births and 92.4% for induced abortions [11,18].
Direct medical costs of births, induced abortions, spontaneous abortions and ectopic pregnancies were taken from the 2009–2010 NHS reference costs, and converted to US dollars using the historical exchange rate of 1.5847 (Table 1) [19,20]. The cost of births is the weighted average of normal, assisted, and cesarean deliveries. The cost of induced abortions is the weighted average of medical and surgical abortions. The cost of spontaneous abortions is based on the assumption that 30% are performed by general practitioners (GPs) and the rest are managed in the hospital setting [4]. The cost to the NHS of a GP visit was taken from the Statement of Fees and Allowances, Revised Fees and Allowances 2003–2004 [21].
3. Results
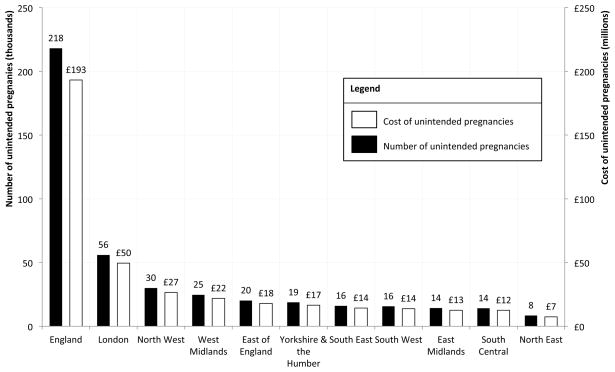
In 2010, there were an estimated 225,600 unintended pregnancies in England – 97% of which (218,100) were paid for by the NHS. Of these, 155,500 led to induced abortions, 53,900 to births, 7,500 to spontaneous abortions and 1,200 thousand to ectopic pregnancies (Table 2). London was by far the region with the largest number of unintended pregnancies (56,000), followed by the North West (30,000) and the West Midlands (24,700) (Fig. 1). The pattern remained: in 2010, there were 26.4 unintended pregnancies per 1,000 women in London compared to 18.5 in the North West and 19.5 in the West Midlands. Overall, there were 17.6 unintended pregnancies per 1,000 women in England.
Table 2.
Number of unintended pregnancy outcomes in 2010 and cost to the NHS
| Number (thousands) | Cost (millions) | |
|---|---|---|
| Births | 53.9 | £44.6 ($69.1) |
| Induced abortions | 155.5 | £142.8 ($221.2) |
| Spontaneous abortions | 7.5 | £2.8 ($4.3) |
| Ectopic pregnancies | 1.2 | £3.0 ($4.6) |
| Total | 218.1 | £193.2 ($299.2) |
Fig. 1.
Number and cost of unintended pregnancies in 2010, by region of England.
Women aged 19–24 years had the highest rate of induced abortion due to unintended pregnancies (25.9 per 1,000), compared with the national average of 12.5 per 1,000 (Table 3). In London, this rate rose to 38.1 per 1,000 in women aged 19–24 years, but also reached 26.8 and 25.5 per 1,000 for women aged 15–19 and 25–29 years, respectively. Rates of spontaneous abortion and ectopic pregnancy due to unintended pregnancy increased with women’s age. Women aged 25–29 and 30–34 years were the most likely to have a birth stemming from an unintended pregnancy, with 8.5 and 9.2 per 1,000 women, respectively, compared with a national average of 4.3 per 1,000. The greatest number of unintended pregnancies occurred to women aged 20–24 and 25–29 years, whose rates were nearly double the overall English average (32.9 and 28.8 per 1,000 compared with 17.6 per 1,000). These patterns were similar across all regions.
Table 3.
Rates of unintended pregnancy outcomes paid for by the NHS per 1,000 female residents of England in 2010
| Age (years) | Birth | Induced abortion | Spontaneous abortion | Ectopic pregnancy | Unintended pregnancy |
|---|---|---|---|---|---|
| 15–19 | 1.9 | 19.8 | 0.3 | 0.1 | 22.0 |
| 20–24 | 5.9 | 25.9 | 1.0 | 0.1 | 32.9 |
| 25–29 | 8.5 | 19.1 | 1.1 | 0.2 | 28.8 |
| 30–34 | 9.2 | 14.0 | 1.1 | 0.2 | 24.6 |
| 35–44 | 1.9 | 3.9 | 0.2 | 0.1 | 6.1 |
| 15–44 | 4.3 | 12.5 | 0.6 | 0.1 | 17.6 |
These unintended pregnancies in 2010 cost the NHS £193,200,000 ($306,100,000) in direct medical costs, £49,500,000 ($78,500,000) in London alone (1ure 1). Induced abortions represent the costliest component of this sum at £142,800,000, ($221,200,000) followed by births at £44,600,000 ($69,000,000) (Table 2).
4. Discussion
This is the first estimate of the age- and region-specific direct medical costs of unintended pregnancy to the NHS. It will come as no surprise that London showed the largest number of unintended pregnancies and highest costs associated with these. The urban setting of a cosmopolitan city, with some of the most deprived boroughs in England, is the ideal setting for unintended pregnancies: its high population density and youthful and mobile residents are the main risk factors for unintended pregnancy [22]. The North West and West Midlands emerged as having many unintended pregnancies as well – though the North West had only half as many as London, which accounted for a fourth of England’s unintended pregnancy costs.
England has high rates of teenage pregnancy compared to other European countries, with 15% of women below 20 years of age reporting at least one pregnancy compared to 6% for France and 4% for Sweden [1]. Consequently, the Department of Health and the NHS have been pursuing a variety of interventions targeting younger women. In the process, they may have overlooked the population that currently accounts for the majority of unintended pregnancies: women aged 20–29 years, who are more likely to be sexually active and cohabiting without being married than their younger counterparts [5,23]. While women aged 25–35 years are those most likely to have unintended pregnancies leading to births (8.5 per 1,000 women aged 25–29 years and 9.2 per 1,000 women aged 30–34 years), women aged 20–24 years are the most likely to have induced abortions (25.9 per 1,000) stemming from an unintended pregnancy, far above the national average (12.5 per 1,000) and well above those for teenagers (19.8 per 1,000) and women 5 years their senior (19.1 per 1,000).
Because there is no national survey from which the number of unintended pregnancies can be estimated, we used results from a study that found that 28% of pregnancies in Edinburgh were unintended; however, a further 22% of women surveyed were ambivalent, so that only 50% of pregnancies were deemed intended [14]. If all pregnancies that are not intended were classified as unintended, there would be 437,600,000 unintended pregnancies paid for by the NHS in England at a cost of £373,600,000.
This analysis addresses direct medical costs to the NHS but omits the indirect and non-medical costs of unintended pregnancies. These societal costs of unintended pregnancy, composed mainly of income maintenance and child support, were last studied by McGuire in 1995, using data that dated back to 1981 [7]. Given changes to the British welfare system (e.g., reduction in childcare tax credits and Sure Start maternity grants, end of the Health in Pregnancy Grant and Child Trust Fund) and management of the NHS, an update would be informative [24]. Another limitation of this analysis is that the fraction of mistimed among unintended births and the number of years by which mistimed births are early is based on US data. Obtaining age- and UK-specific data would allow far better estimates of the incidence and costs of unintended pregnancies.
Similar results may apply to other developed countries, particularly those in which health care costs are in majority shouldered by national health systems (e.g., Canada). In addition, countries that currently focus resources and education campaigns on teenagers (e.g., the US, France) may wish to consider whether they are not omitting a part of the problem by neglecting women aged 20–29 years.
Regardless, it is clear that improving the usage of contraception is essential to limiting the number of unintended pregnancies, particularly in the most at-risk age groups (i.e., 20–29 years) and areas (i.e., London, North West, West Midlands). The fact that 88% of British women at risk of pregnancy use contraception suggests that a large number of unintended pregnancies are due to improper contraceptive use rather than non-use of contraception. Increased uptake of LARC (including a copper IUD for emergency contraception) in the UK and elsewhere would reduce unintended pregnancies at a fraction of the cost, thereby relieving the NHS and other national health care organizations of a significant burden [25].
Acknowledgments
The authors would like to thank Alison Howell (Medaxial Group, London), Ruth Zeidman (Medaxial Group, London) and Myat Arrowsmith (Imperial College London) for their contributions to this manuscript.
This work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University, Grant R24HD047879 (JT). Neither CM nor JT have been paid by a pharmaceutical company or other agency to conduct this research.
Footnotes
Authors’ contributions
Calypso Montouchet (CM) carried out the literature search involved in building this model and developed the Excel structure for the cost analysis. She is also responsible for analyzing the data and writing the first draft of the article. James Trussell (JT) corrected the methodology and assumptions used in the model. He is also responsible for several rounds of modifications to the article text.
Conflicts of interest
Neither CM nor JT has been paid by a pharmaceutical company or other agency to conduct this research. Though CM is currently working for a pharmaceutical consultancy (Medaxial Group, London), she has not been and is not now involved in any projects whose clients could benefit from the publication of this manuscript. Moreover, all research and writing involved in this article was conducted independently from work carried out at Medaxial Group.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Darroch JE, Singh S, Frost JJ. Differences in teenage pregnancy rates among five developed countries: the roles of sexual activity and contraceptive use. Fam Plann Perspect. 2001;33:244–50. [PubMed] [Google Scholar]
- 2.Régnier-Loilier A. Evolution des naissances et des grossesses non désirées en France. 25ème Congrès International de la Population; 20 July 2005; Tours, France. [Google Scholar]
- 3.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute For Health and Clinical Excellence. Clinical Guideline 30. [Accessed: Jun 2011];Long-acting reversible Contraception: the effective and appropriate use of long-acting reversible contraception. 2005 Oct; Available at: http://www.nice.org.uk/CG030.
- 5.Denton AB, Scott KE. Unintended and unwanted pregnancy in Halifax: the rate and associated factors. Can J Public Health. 1994;85:234–8. [PubMed] [Google Scholar]
- 6.Office for National Statistics. Opinions Survey Report. [Accessed: Jun 2011];Contraception and Sexual Health. 2008/2009 41 Available at: http://www.ons.gov.uk/ons/rel/lifestyles/contraception-and-sexual-health/2008-09/index.html. [Google Scholar]
- 7.McGuire A. The Economics of Family Planning Services. Family Planning Association; 1995. [Google Scholar]
- 8.Bragg F, Cromwell DA, Edozien LC, et al. Variation in rates of caesarean section among English NHS trusts after accounting for maternal and clinical risk: cross sectional study. BMJ. 2010;341:c5065. doi: 10.1136/bmj.c5065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trussell J. Overstating the cost savings from contraceptive use. Eur J Contraception Reprod Health Care. 2008;13:219–21. doi: 10.1080/13625180802359263. [DOI] [PubMed] [Google Scholar]
- 10.Office for National Statistics. [Accessed: Aug 2011];Birth summary tables, England and Wales. 2010 Available at: http://www.ons.gov.uk/ons/rel/vsob1/birth-summary-tables--england-and-wales/2010/index.html.
- 11.Office for National Statistics, Department of Health. [Accessed: Aug 2011];Abortion Statistics, England and Wales. 2010 Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsStatistics/DH_126769.
- 12.Hospital Episode Statistics. [Accessed: Aug 2011];Ectopic pregnancies that resulted in an NHS hospital stay by age. 2009–10 Available at: http://www.hesonline.nhs.uk/Ease/servlet/AttachmentRetriever?site_id=1937&file_name=d:\efmfiles\1937\Accessing\DataTables\Annual%20maternity%20release%202010\NHS%20Maternity%20Statistics,%20England%202009-10.xls&short_name=NHS%20Maternity%20Statistics,%20England%202009-10.xls&u_id=8943.
- 13.Hospital Episode Statistics. [Accessed: Aug 2011];Miscarriages that resulted in a hospital stay by age. 2009–10 Available at: http://www.hesonline.nhs.uk/Ease/servlet/AttachmentRetriever?site_id=1937&file_name=d:\efmfiles\1937\Accessing\DataTables\Annual%20maternity%20release%202010\NHS%20Maternity%20Statistics,%20England%202009-10.xls&short_name=NHSb%20Maternity%20Statistics,%20England%202009-10.xls&u_id=8943.
- 14.Lakha F, Glasier A. Unintended pregnancy and use of emergency contraception among a large cohort of women attending for antenatal care or abortion in Scotland. Lancet. 2006;368:1782–7. doi: 10.1016/S0140-6736(06)69737-7. [DOI] [PubMed] [Google Scholar]
- 15.Office for National Statistics. [Accessed: Sept 2011];Mid-2010 Population Estimates: Quinary age groups for health areas in the United Kingdom; estimated resident population. Available at: http://www.ons.gov.uk/ons/rel/pop-estimate/population-estimates-for-uk--england-and-wales--scotland-and-northern-ireland/mid-2010-population-estimates/index.html.
- 16.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: Data From the 2002 National Survey of Family Growth series. Vital Health Stat. 2005;23:1–60. [PubMed] [Google Scholar]
- 17.National Institute for Health and Clinical Excellence. [Accessed: Jun 2011];Guide to the methods of technology appraisal. 2004 Apr; Available at: http://www.nice.org.uk/aboutnice/howwework/devnicetech/technologyappraisalprocessguides/guidetothemethodsoftechnologyappraisal.jsp. [PubMed]
- 18.National Centre for Health Outcomes and Development. [Accessed: Aug 2011];Live births in NHS hospitals. 2009–2010 Available at: https://indicators.ic.nhs.uk/download/NCHOD/Data/05B_143PC_09_V1_D.xls.
- 19.Department of Health. [Accessed: Aug 2011];NHS Reference Costs (Trusts and PCTs) 2009–2010 Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_1234569.
- 20.XE Universal Currency Converter. [Accessed: Apr 2012];Historical exchange rates. Available at: www.xe.com.
- 21.Department of Health. [Accessed: Jun 2011];Statement of Fees and Allowances, Revised Fees and Allowances 2003–2004. 2004 Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4071849.
- 22.London Sexual Health Programme, London Health Observatory, Health Protection Agency. [Accessed: Jun 2011];Project Report 3: Sex and our city (Achieving better sexual health services for London: project findings & recommendations) 2008 Available at: http://www.medfash.org.uk/publications/documents/Sex_and_our_City_PUBLISHED_ONLINE.pdf.
- 23.Forrest JD. Epidemiology of unintended pregnancy and contraceptive use. Am J Obstet Gynecol. 1994;170:1485–9. doi: 10.1016/s0002-9378(94)05008-8. [DOI] [PubMed] [Google Scholar]
- 24.Chantry C. [Accessed: Jan 2012];Evidence Submission: Benefits for Pregnant Women. Available at: http://ukpolicymatters.thelancet.com/?p=1708.
- 25.Mavranezoulli I. The cost-effectiveness of long-acting reversible contraceptive methods in the UK: analysis based on a decision-analytic model developed for a National Institute for Health and Clinical Excellence (NICE) clinical practice guideline. Hum Reprod. 2008;23:1338–45. doi: 10.1093/humrep/den091. [DOI] [PubMed] [Google Scholar]