Abstract
Recent epidemiological data show that older adults comprise a growing age group of drug users and new AIDS cases in the United States. Prevention and intervention studies show that risk behaviors leading to HIV infection are increasing among older users, particularly among the socially vulnerable. Yet older adults remain an under-researched population of drug users and little is known about their risk behaviors. Our aim is to address this gap in knowledge on older users by comparing contextual factors that influence risk behaviors and harm reduction strategies practiced by older drug users living in different communities. This study is based on ethnographic fieldwork in suburban and inner-city neighborhoods in a large metropolitan area in the southeastern USA. Interviewers conducted face-to-face, in-depth, life-history interviews with 69 older adults (age 45 and older) who used heroin, cocaine, and/or methamphetamine. Findings show that while risk behaviors were similar among older adult drug users living in suburban and inner-city environments, the provision of harm reduction education and paraphernalia varied widely. The results show the need for the expansion of harm reduction services focused on older adult drug users who are homeless, uninsured, or socially isolated. This application-oriented research will inform healthcare and treatment providers and generate new directions for future collaborative harm reduction services aimed to decrease the spread of HIV and other infectious diseases associated with drug use.
For the past decade, researchers have articulated the need for studies that are specific to persons who use drugs and engage in risk behaviors as older adults (Auerbach 2003; Boeri 2004; Pach, Gorman, and 2002; Sampson and Laub 2002, 2003). The emerging older adult population forms the fastest growing age category of drug users in the United States (Gfroerer et al. 2002; Gomberg, Linsanky, and Zucker 1998), and older adults who use drugs are exposed to increasing health risks such as HIV/AIDS and other blood-borne and sexually transmitted infections (Anderson and Levy 2003; Nokes and Emlet 2006; Emlet 2006; Johnson and Sterk, 2003; Levy 1998). We have little in-depth knowledge on the drug use risk-patterns of the contemporary older drug user population or the risk and protective factors emanating from their social environments. For example, research on drug use among older adults in suburban environments is practically nonexistent (Page and Singer 2010). Due to the lack of knowledge about this age group, some call the aging of drug users an “invisible epidemic” (Blow 2000; Levin and Kruger 2000). The impact of this epidemic is already overwhelming substance abuse health services, and a better understanding of risk behavior patterns among older adult drug users is essential for the development of interventions and treatment for this population in the future.
BACKGROUND
Drug users typically were assumed to age out of drug use. Based on analysis of data collected by the Federal Bureau of Narcotics, Winick (1962) proposed that 70% of narcotic users become drug inactive between the ages of 23 and 37. Winick's hypothesis was known as the “maturing out thesis.” Others confirmed the age of 35 or 36 as the age when narcotic users generally mature out of drug use (Petersen 1983; Rosenberg 1997). Data archives often defined an older age group by this approximate maturing out age. Using 35 as the start of an older age category, trend data from 1979 to 1999 showed an increase in drug use among the 35 and older age group while all other age groups showed a decrease during this same time period (SAMHSA 1999, 2000a, 2000b). This trend has been linked to the cohort known as the baby boomers (Boeri, Sterk, and Elifson 2006; Gfroerer et al. 2003).
Contemporary baby boomers are not following the drug use patterns of previous generation. Glantz (1995) contends that the baby boomers are our first real cohort of drug-users, and they are likely to have drug-related problems when they get older. Although the cohort has been defined differently, the last baby boomers were born in 1964 or 1965 (Alwin 1998; Keister and Deeb-Sossa 2001; Morgan 1998). Consequently, the contemporary baby boomer cohort is age 45 and older. We used this age to define the current older adult drug user population.
In this paper we present our findings of a comparison study between baby boomer drug users who live in an urban setting and those who live in a suburban setting. The suburban study participants (n=34) were primarily white methamphetamine users, and the inner-city participants (n=35) were primarily African Americans who used heroin and crack cocaine. The participants were drawn from community-based studies in a large metropolitan area in the southeastern USA. Our aim is to compare contextual factors that influence risk behaviors and harm reduction strategies practiced by older drug users living in urban and suburban communities. A more in-depth understanding of risk behaviors and how older adults approach harm reduction strategies is needed to better apply the wealth of information we have learned after 30 years of research on the transmission of HIV and other infectious diseases among drug-using populations.
HIV Risks Behaviors among Drug Users
In the US, new HIV/AIDS cases due to injection drug use increased 42% from 1998 to 2003, and injection drug use continued to be one the most frequently cited modes of transmission of HIV worldwide (UNODC 2007). Heroin, cocaine and methamphetamine present a risk factor for transmission of HIV and other infectious diseases through injection drug use. Risky sexual behaviors are the primary mode of HIV transmission among non-injectors (Centers for Disease Control and Prevention [CDC] 2008a).
Research findings consistently show that the older drug-using population is at high risk for HIV transmission through unsafe injection practices (Boeri, Sterk and Elifson 2008; CDC 2008b; Kwiatkowski and Booth 2003; Levy, Ory, and Crystal 2003). Nokes and Emlet (2006) identified older injection drug users as having increased HIV-risk exposure but less access to HIV-related health services. In addition, sexual risk behaviors leading to HIV infection associated with drug use were found to be increasingly prevalent among older users (Anderson and Levy 2003).
Social Influences on Drug Use and Risk Behaviors
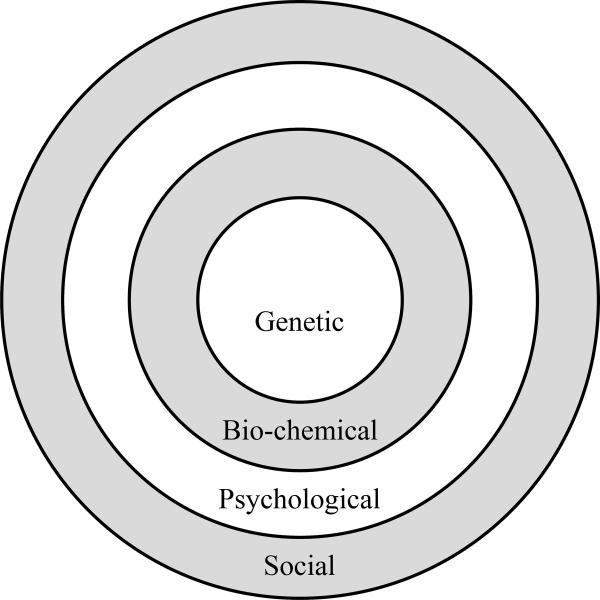
We know that risk behaviors among drug users are socially learned (Berkman and Glass 2000; Bluthenthal and Watters 1995). Moreover, historical events impact patterns of drug use, and policy changes influence the social dynamics and social norms surrounding drug use (Faupel 1991; Musto 1999). Since drug use risk behaviors are also influenced by psychological, biochemical, and genetic factors, a brief discussion of these influences is presented here, illustrated by Figure 1 (Boeri 2002).
Figure 1.
Integrated Causal Model
Starting from the inner circle, Figure 1 represents those genetic influences that may pre-dispose drug users to become addicted (Schuckit 1984; Zickler 1999). Many drug treatment practitioners embrace the genetic pre-disposition component, which in turn affects the drug users perspectives as well. The layer surrounding the inner circle represents physiological and biochemical (a.k.a. pharmacological) influences on drug addiction, some of which were identified by earlier researchers as iatrogenic causes (Dai 1937; Lindesmith 1938). For example, long-term drug users have been found to have physiological changed that can influence continued dysfunctional drug behavior (Dole 1980), and for heroin users, the addictive properties of opiates were drawn from shared knowledge gained among the user's social networks more than the drugs' pharmacological properties (Lindesmith 1968). The scientific focus promoted by recent research has raised more interest in the neuroscience of drug addiction, particularly in CAT scan images of the brain on drugs (Leshner and Koob 1999). However, these physiological and chemical influences can be the result of social and psychological conditions as well (Goode 1999). Without records of brain activities and functions of the user before initiating use of drugs, it is difficult to identify how drug users are affected by physiological and bio-chemical changes known as “metabolic imbalances” (Dole and Nyswander 1965; Milkman and Sunderwirth 1995).
The next layer in the concentric circle represents psychological factors, such as early childhood trauma and mental disorders, found to associated with initiation into and continued use of both licit and illicit drugs (Jessor and Jessor 1977; Kaplan 1975; Miller 1995). Psychological factors are believed to be a primary cause for what is commonly known as addiction, particularly by addiction treatment that uses therapeutic models developed by psychologists. Morgan and Zimmer (1997), who prefer to use the term drug dependence, argue that the defining element is “compulsion or loss of control” (p. 142), and they describe addiction as a social construction. Their viewpoint highlights the social influences on drug dependence, as illustrated by the outer layer in Figure 1.
This integrated model incorporates all identified causes of drug use, but not all are the causes for all drug users. For many users, the social context of drug use, their life experiences, the neighborhoods where they live, and myriad other social factors are the primary influences on their drug use. Research studies drawing from community based samples give ample evidence that initiation and progression in drug use appears to be influenced primarily by social factors, and social conditions (Agar 1973; Akers 1998; Becker 1953; Biernacki 1986; Boshears, Boeri and Harbry 2011; Inciardi, Lockwood and Pottieger 1993; Lindesmith 1938, 1968; Rosenbaum 1981; Sterk 1999). For example, availability of drugs and drug-using social networks are influential factors in experimenting with drugs, especially during adolescence (Akers et al. 1979; Cloward and Ohlin 1960; Johnson 1973; Kandel 1980). Moreover, insight provided by scholars employing a political economy conceptual model explain how “health and well-being are intrinsically related to social, economic and political realities at both the macro and micro levels” (Romero-Daza, Weeks and Singer 2003: 236). In sum, while not ignoring the potential genetic, physiological, and psychological causes of drug dependence, our model suggests that problematic drug use for many can be addressed by a greater focus on the social conditions of the user.
Addressing the social influences to a greater degree, Zinberg (1979, 1984) proposed a model that describes the interaction between the mind of the user (set) and the social setting. The concept of “set” is defined as “the user's personality and his or her attitudes toward taking the drug,” and the concept of “setting” is defined as “the characteristics of the physical and social setting in which use occurs” (1979: 308). The perceived effects and behavioral consequences of a particular drug vary according to how the user's set interacts with the social settings of drug use (Becker 1953; Reinarman and Levine 1997). Extending our understanding of set and setting, Faupel (1991) proposed that the pattern of individual drug careers is based on the availability of drugs and their life structure. Availability includes initiation into different drugs, access to drugs through social relationships, and ability to afford increased use of drugs. Life structure refers to “the constellation of roles that patterns behavior in a regular and predictable manner” (Faupel 1991: 443).
We know that the influences discussed above affect younger and older users differently. Previous literature found substantial differences between older and younger users in physiological reaction to drugs, social support, emotional responses, peer relations, and risk behaviors (Capel and Peppers 1978; Emlet 2006; King et al. 1994; Levin and Kruger 2000; Levy 1998). Research tends to focus on samples of younger users, yet, recent increases in older adult drug use and those with HIV/AIDS has led to a greater need to understand the set and setting of older drug users (CDC 2008s, 2008b; Kwiatkowski and Booth 2003; Levy, Ory, and Crystal 2003). In this paper we examine how the social environment impacts risk behaviors among older drug users by comparing those who live and use in inner-city communities and those who live and use in suburban neighborhoods.
METHODS
The data used for this paper were drawn from two studies on active and inactive users of heroin, cocaine/crack and methamphetamine. These drugs were chosen because they represent the three major drugs of use associated with the transmission of infectious diseases (Brecht et al. 2008; Hser et al. 2008). Active use was defined as having used one of these drugs at least one time in the past month. Inactive use was defined as having used one of these drugs for at least six consecutive months in the past but not in the last month. For the purposes of distinguishing the studies, we describe each study separately. We employed the same methods of recruitment in both studies, which were conducted in a southeastern metropolitan area of the United States.
The Methamphetamine Use in the Suburbs Study (SUBURBAN)
The SUBURBAN study was focused on methamphetamine users who lived in the suburbs. To capture turning points in and out of drug use, both active and inactive users were enrolled in the study. To be eligible, participants must have been residing in the suburbs of the city at the time of use, be 18 years or older at the time of the interview, and be an active or inactive user of methamphetamine. For this paper on baby boomer drug users, only those age 45 and older were included in the analysis presented here.
The data instruments were designed to collect in-depth life histories and drug histories using both quantitative and qualitative research strategies (Bruckner and Meyer 1998; Clausen 1998; Elder 1999; Laub and Sampson 2003; Scott and Alvin 1998). We also used interview tools developed to avoid recall bias and provide triangulation data for verification, as well as to address issues of validity and reliability (Carlson, Siegal and Falck 1995; Clatts, Davis and Atillasoy 1995; Needle and Coyle 1997; Nichter et al. 2004).i
The Older Drug User Study (CITY)
The CITY study was focused on older adults who were active or inactive users of heroin, cocaine or methamphetamine. To be eligible to enroll in the study, participants had to be 45 or older. Those who lived in one marginalized inner-city neighborhood were used in the analysis presented in this paper.
Using a retrospective longitudinal design, we collected data for every year of life from birth with the help of a computer-assisted survey. Three sources of direct data were collected: survey data, a life history matrix, and an in-depth digitally recorded life-history interview. Strategies such as a timeline and memory cues were used to integrate the collection of both qualitative and quantitative data in a parsimonious and time efficient manner (Murphy et al. 2010; Sobell et al.1988).
Recruitment
Participants in both studies were recruited using targeted, snowball, and theoretical sampling methods (Glaser and Strauss 1967; Strauss and Corbin 1998; Watters and Biernacki 1989). Typically, recruitment involved spending many hours walking city streets or driving around suburban neighborhoods, frequenting commercial establishments, especially bars, and talking to potential participants. Flyers were posted in a wide variety of public settings to advertise the study. We also employed local key informants (community consultants) when needed to break into a new network (Bluthenthal and Watters 1995; Page and Singer 2010).
The investigator's university Institutional Review Board (IRB) approved the studies' protocols. All participants read and signed or agreed verbally to a consent form before participating. Interviews were conducted in private places such as the participants' homes, hotel rooms, library rooms, offices, and the interviewers' cars. Participants were paid a nominal fee for their time ($25 for the SUBURBAN interviews and $40 for the longer CITY interviews).ii The choice of cash or gift certificate was offered. We secured a federal “Certificate of Confidentiality” that protected the study data and researchers from court subpoena.
Sample
Among the SUBURBAN sample, 34 participants were age 45 or older at the time of their interviews. The demographics of the SUBURBAN sample, as shown in Table 1, were 65 percent male and 79 percent white. Seventy-one percent were active users at the time of the study. Half (50%) were current or former injecting drug users (IDU). Ages ranged from 45 to 65, with a mean age of 49.4. None reported being HIV positive, but four (12%) reported having been diagnosed with hepatitis C.
Table 1.
Demographics of Older Users
| SUBURBAN (n=34) Percent (n) | CITY (n=35) Percent (n) | |
|---|---|---|
| Female | 35% (12) | 34% (12) |
| Male | 65% (22) | 63% (22)* |
| African American | 21% (7) | 91% (32) |
| White | 79% (27) | 9% (3) |
| Age Range (mean) | 45–65 (49.4) | 45–65 (51.9) |
| Active eligible drug use | 71% (24) | 77% (27) |
| IDU Ever | 50% (17) | 57% (20) |
| HIV | 0 | 9% (3) |
| AIDS | 0 | 3% (1) |
| HEPATITIS C | 12% (4) | 26% (9) |
One transgender
Among the CITY sample, 35 participants lived and used in the inner-city neighborhood focused on for this paper. The demographics of the older CITY subsample, shown on Table 1, were 63 percent male and 91 percent African American. Fifty-seven percent had injected drugs, and 77 percent were active users at the time of the study. Ages ranged from 45 to 65, with a mean of 51.9. Three had been diagnosed as HIV positive, one with AIDS, and nine reported having been diagnosed with hepatitis C.
Demographic differences are not meant to be representative of inner-city and suburban population of older drug users but are noted here as differences between our study samples. For example, the majority of CITY older users were African American, and while CITY and SUBURBAN samples did not differ substantially in terms of active drug use and injection history, more of the CITY users had been diagnosed with HIV, AIDS, or hepatitis C.
Analysis
All qualitative interviews were transcribed. Analysis of qualitative interviews involved finding systematic patterns or relationships among categories identified by reading and re-reading the transcripts (Agar 1980). Grounded theory method guided the analysis that started with open coding of the data, followed by more focused coding (Glaser and Strauss 1967; Strauss and Corbin 1998). For this paper we employed a modified version of grounded theory, which incorporates existing conceptual frameworks into concepts that emerge from the data (Charmaz 2001; Boeri et al. 2008).iii
FINDINGS
In this section, we present the findings of our qualitative analysis of the interview transcripts that represent a comparison between inner-city older drug users and older methamphetamine users who lived in the suburbs during their time of use. We organized risk behavior- and harm reduction-related quotes by the social context of suburban users and inner-city users. Quotes represent findings reported by most participants as well as those indicating a new conceptual category. Conversations are distinguished by an asterisk (*) indicating a question asked by the interviewer, followed by the response on the next line. To maintain confidentiality, we identify quotes only by the participant's gender.
Risk Behaviors Among Older Users in Suburban Environments
Most of the suburban older users lived in deteriorating working class neighborhoods that were negatively affected by the recent recession. Some lived in trailer parks with gravel yards and dirt roads. A few were homeless at the time of the interview. However, most had been raised in middle or upper-middle class families. A few maintained their middle-class status; others recently became poor or encountered life events that had a negative effect on their social and economic status.
Many of the suburban users had heard about AIDS and risk behaviors while they were in high school or college through health awareness education. For example, a former injector who was raised and lived in upper-middle class neighborhoods recalled how she became aware of risks related to injection drug use:
*Why did you use your own needles?
So I wouldn't get AIDS.
*How did you know about AIDS?
AIDS came around in 1983, when I was in college.
*So you knew—you had education about it?
Yeah.
*And what about Hepatitis C? What do you know about that?
I know you can get that from dirty needles.
*Any other way you can get it?
I heard you can get it from sex but I don't think you can. (mumbles) Or blood. Hepatitis C is—I can't remember… blood I think it is. I don't remember.
*Is there anything else you do with meth that might transfer diseases?
I didn't do anything that can transfer diseases because I was (pause) real careful.
*And did you use condoms when you had sex?
No (laughs) Yeah, real careful huh? (sarcastically stated) I was real careful with drugs—not with sex.
This woman illustrates the lack of education regarding hepatitis C expressed by many of our middle and upper-middle class respondents. We found that while suburban drug users were educated regarding HIV, they were not informed on how viral hepatitis could be transmitted or treated. It appears that HIV/AIDS was a focus in health education classes, but hepatitis C was rarely discussed. Furthermore, while most of the suburban older adults had sex education in school, sexual risk behaviors were not discussed with health providers as older adults.
Some of the older suburban drug users became aware of their infectious disease status through a church program, which appeared to have influenced their sexual risk behaviors. For example, a male and former frequent injector said he never got HIV or hepatitis C because he was careful regarding injection and sexual practices:
No, I'm thankful to God for that. You know I got tested at the church in September and I was [negative], and I thank God for that. But I mean, that's why I don't, certain women I won't touch. I mean they can strip down to the skin bone and I won't, because I have certain things that I refuse to do.
Both males and females reported that they were more aware of sexual risk due to their involvement in religious groups.
Many suburban males became aware of their own status after they had been tested through work environments:
Oh yes. I've been tested and everything. I've worked many shops where I've had to take the hepatitis shots over a three-month period. You know you get one, you get another, and then you get your last one. And I've been tested for it. I can go out here and give plasma or anything, and I don't have nothing.
Women, however, were rarely tested at their work environments, which tended to be service work (e.g., food server, office staff). More often, they were tested when pregnant or when in jail.
Harm Reduction Among Older Users in Suburban Environments
Most suburban users who were knowledgeable of injection risk behaviors did not know where to obtain harm reduction paraphernalia in the suburbs. This was made clear in our focus group interviews with female injectors who disagreed on how difficult it was to obtain clean syringes or other harm reduction materials in the suburbs. The poorer women were especially affected by the lack of access to clean syringes, as was revealed in a focus group conversation between participants about an injecting network in the suburbs:
* So you can boil your own [syringes]?
Female 1: Yeah, but a lot of people, a lot of junkies are not trying to go through all that rigmarole of having to boil something out…And then a lot of people don't have access to like water or boiling the water.
Female 2: Yeah they use dirt wa—creek water.
Female 1: I've seen somebody use lake water.
Female 3: I've seen people use creek, I've seen people use spit.
Female 1: I know when I did it that way and when I had like access to boxes of them, I'd give so and so a bag. Because I know how hard it is to come by. I know the risks of, you know, using—you can give yourself a disease by keeping old ones. Because I mean blood grows bacteria. And I just think that people should have easier access to them. It would decrease disease definitely by half, if not more.
If the suburban user was a diabetic, or knew a diabetic, using clean needles was not a problem; however most of the older women did not have knowledge of where to obtain clean needles. Many of the poorer women did not have access to transportation to obtain needles at a pharmacy and relied on friends or shared with a partner.
Despite state laws essentially prohibiting syringe exchange, a vibrant harm reduction non-profit organization conducted syringe exchange in the city. We discussed syringe exchange programs in our focus group with suburban users. Women who were unaware of such programs were typically enthusiastic at our suggestion to bring this to the suburbs:
* What if we raise money for [harm reduction staff] to come out here and give [syringes] away. They sometimes pay former users to give out to people that need it. Because they're trusted [by other drug users].
Female 1: I would absolutely do it. One hundred percent. For free. I mean I would do it for free. Because I know how hard it was for me and I know, I've seen, to this day I see so many people struggle with it. And it just breaks my heart. Because, people are, like I said, people are going to do what they're going to do no matter what.
* Should all the clinics just give out needles?
Female 2: Yeah, because people's not going to stop doing it.
Female 3: It's not just the clinic. A lot of people don't have access to those. They need to be able to walk into a drug store anywhere, instead of the clinics, also.
Some of the more savvy suburban injectors indicated that they went to the city to obtain clean syringes:
No. I didn't share no needles. One thing I did, I always made sure I had—you can go down to [the city], these stores like I was telling you about. You can go anytime and get a syringe and they'll give it to you in a little brown paper bag, brand new one with a needle.
While this woman went to the city for her syringes, we found that most of the women did not know it was so easy to access syringes in the city, and if they did, they often had no transportation to go there.
Many of the older suburban drug users revealed that in “the old days” they would share drug paraphernalia, as was the case for one person who learned he had hepatitis C:
Yeah, we did share them (syringes). A lot of the time, uh, what was this, past '80, You didn't think anything about it `til hepatitis came around. I got hepatitis B, in 1980. I got hepatitis C, too, I found out a year ago.
The man quoted above was diagnosed while he was in a city hospital, and he relied on the staff at the city hospital to prescribe a treatment and provide needed medical attention for hepatitis C. Like many of the suburban users, he had a fairly good understanding of HIV and AIDS, including how it was treated, but he did not know what to do when diagnosed with hepatitis C.
Hepatitis C is a complicated disease that is not treated in a consistent manner. Typically, doctors will not treat drug users until they stop using drugs, although some studies find that drug use does not interfere with treatment (Sylvestre 2006). When suburban drug users became aware of their positive status, they did not know where to go to find treatment. Medical staff were often at a loss as well. After one mother we interviewed revealed that her daughter, who also injected drugs, tested positive for hepatitis C, she broke down in tears while explaining that they did not know where to get healthcare for her since they were without health insurance. Our research staff inquired among local clinics and found only one doctor who would treat her under the stipulation that she was drug-free. A year later, in a follow-up interview, we learned that mother and daughter were still having trouble finding continued care:
*You said that you went to the clinic and they denied you.
She went to [County] Clinic, [County] Health Department. They found out she had hepatitis C. Took her to Social Security. They denied her.
*Why?
You tell me.
*They didn't give a reason?
They didn't even give me medical help. I didn't ask for a check. I wanted medical help for her and they denied me.
*So what did she…
She's just like—she's just like, giving up.
Those in the suburbs who knew of their positive hepatitis C status often said they went into the city for continued care.
I'm went on up at [the city public hospital] to check on the treatment that they have, but the way they talk about the sick that it'll make you and stuff. They're talking about you need a good year and don't plan on anything to do, cause you'll be sick all the time.
This male respondent had worked in construction and was a truck driver, which provided him with more mobility and with greater knowledge of the services offered in the city. Most of the older users in the suburban study, specifically those who lived in marginalized neighborhoods, were not aware of services for treating infectious diseases. Moreover, they were ashamed to ask due to the stigmatization association with injection drug use. Many, in fact, did not know their status for HIV or hepatitis C.
Risk Behaviors Among Older Users in Inner City Environments
The older users in the inner-city sample lived in an area of the city that had once been a working and middle-class African American community. After years of neglect, and being ignored by the city officials, many homeowners left the area, and abandoned houses could be found on every street. Drugs were sold on the corners by young men to passing cars driven by people who came to the area primarily for heroin or crack. Sex workers walked the streets at night. Most of the older users who stayed in this area lived in boarding houses or were homeless.
In contrast to older drug users who lived in the suburbs, many of the inner-city older users said they did not have risk awareness taught in school. As expressed by one male: “No we didn't have sex education then…. I went to a segregated school—there was no sexual education.”
Similar to those living in the suburbs, older drug users who lived in the city recounted having multiple partners or being engaged in sex work, particularly in their younger years. Some began exchanging sex for drugs when they were older. Street level sex work was more common among the inner city older users than those living in the suburbs, but like the suburban drug users, condom use was sporadic. For example, on older woman who reported having “only about 200 clients” a year said, “I never use condoms.” A transgendered sex worker who had been working in the sex industry for many years explained why condom use was inconsistent:
*Did you use condoms sometimes?
Sometimes, yeah. Even till this day, I still use condoms sometimes.
*Why don't you use it all the time?
Some don't like it and some, you know, you have a problem with using condoms, and they'll be like never mind. But money is like, in your head, and you're like ok, well fine. We don't have to use it, but I would never let them ejaculate in my mouth because that's disgusting. That shit's disgusting.
This sex worker, similar to many, revealed that satisfying the client, and obtaining money for it, was more important than practicing safe sex. Some reported behaviors that they thought partially protected them from infectious diseases, as shown in the quote above.
Although the users in both studies had frequent encounters with the criminal justice system, being in prison or jail was a more common experience for the inner-city drug users than those who lived in the suburbs. While many of the men said they did not have sex in prison, others claimed that it was common but condoms were not available. Jails and prisons, which are extreme risk environments for infectious diseases, offered little risk education and no access to condoms. One male participant who said he had sexual relations in prison revealed:
The prison I went to at that time, there was no reform education. They didn't care if you changed your life when you got out there. All they was there to keep you in conservation, there was no drug abuse classes, no substance abuse classes, no parenting classes, there was no sex education when I went to prison, none of that…I never use condoms.
More than suburban users, the inner-city older drug users in our study reported higher levels of violence in their social environments. Despair caused by the belief that this aspect of their lives would never change appeared to be a strong influence on their use of drugs. The concurrent influences of prison, violence, and poverty permeated the lives of many inner-city aging drug users. One older woman expressed how she coped with increasing violence and hopelessness:
When I found out about my kidney, I just found out about a year ago, do you know a dark cloud came over me. I was depressed. Now I had stopped using for six years and I started back using two years ago. My youngest boy, my second child, he killed a person. He was thirteen years old. It was all over the news and everything…I gave up. I started getting high every day.
This woman, previously a crack smoker, changed her drug of choice: “That's when the heroin came in—to medicate me.”
The rapid spread of HIV in the city environment left an impression on the older drug users who lost many of their old “running buddies” (fellow drug users) to AIDS. For some, this social environment influenced their resolve to practice harm reduction techniques. Such was the case for one man who sought to reduce his risks in both his sexual and drug use behaviors:
I'm gonna give you the truth, I wasn't a dog, I wasn't a person that would go, would go and lay down with anyone. Anytime I got the desire to have sex, I wouldn't do it. I had to have a desire for a woman. And I was scared that I would get AIDS or syphilis or something like that because back in the `80s, and things it was, it was a plague from [urban neighborhood] all the way through here, and I wouldn't do it because I was scared of myself using them syringes and things…you know.
Sadly, or ironically, living in an area of the city where the AIDS epidemic hit hardest, the most marginalized of drug users benefitted by being exposed to AIDS awareness and risk reduction prevention initiatives focused on this community.
Harm Reduction Among Older Users in Inner City Environments
The non-profit organization mentioned earlier, hereafter referred to as the Urban Harm Reduction Center, began operating on the streets of this city's open drug market neighborhood in the early 1990s. Many of the urban users said they learned about safer injection practices through the Urban Harm Reduction Center. According to the center's website they are a:
Community-based prevention and wellness organization committed to improving the overall health and wellbeing of marginalized individuals and communities. [The Urban Harm Reduction Center] provides education and tiered risk reduction programs through partnerships, to empower adults in the prevention, diagnosis and treatment of substance use, HIV/AIDS, STDs, hepatitis, and other communicable diseases.
Beyond a vibrant syringe exchange program in the city, their staff also reached incarcerated individuals through their work with the city drug court, and they engaged in outreach to street sex workers. Some of our inner-city participants reported working or volunteering at the center in order to help educate others. Such was the case for one inner-city participant who continued to use drugs, but with more knowledge and awareness of risk behaviors:
Well actually—I've always been a part of this here [Urban Harm Reduction]. When I was using I would come here, and it was on [street name], and work with them. And I would be just high, and I would come in there and work with them—and go back and do my thing.
This participant, like others who used the services, did not stop using drugs, but she decreased her own risk behaviors while spreading awareness of harm reduction to other drug users.
The work of the Urban Harm Reduction was successful, as shown by the fact that virtually everyone in this area knew of the center and injecting drug users participated in their syringe exchange program. For example, an older male who had been using drugs for years claimed the Urban Harm Reduction staff educated him regarding HIV transmission:
*When did you first hear about AIDS?
At a place called [Urban] Harm Reduction. I think in the `90s. I think in the early `90s when I first.
*And when did you start hearing about condoms as a public health concern?
When we heard about AIDS how, that's when people started utilizing `em and stuff. I think back in the early `90s, I believe. You know, I think it's the early 90's
For some of the injectors and former injectors living in this area, harm reduction and access to clean syringes came too late. Such was the case for one older user who started injecting late in life:
*When did you find out that you had HIV?
Six years ago.
*That's when you were forty-nine?
Yeah…a year after I started.
*So when you were forty-nine you got HIV from a person you had one-time sex with?
No, I didn't have no sex with that faggot. We were shooting drugs. We were drug partners. I didn't know the bastard was gay or nothing.
*You were shooting drugs?
We always shared drugs, that's all.
*Why did you share drugs with him?
If I didn't have it [syringe], he had it—you know what I mean?
*Did you know that needles weren't good for you to share with people?
Yeah, but you know…I was real stupid to the game…they really beat me bad behind needles, you know.
*What were you thinking at the time?
I cleaned it out good and stuff like that. There were always blood spots in the cooker.
*Did you share his needles or the cooker?
The cooker, sometimes when he was mixing it up there were spots of blood in it…and you know I don't have no more money. Do you feel me? Yeah…At the time I didn't think that it meant nothing. But it meant a whole lot at the time.
DISCUSSION
Although there are many similarities among older drug users who live in suburban environments and inner-city neighborhoods, here we focused on their differences in risk behaviors. These differences were related to their social context and their awareness of behaviors that increase their risk of contracting infectious diseases. The social context of the inner-city presented greater challenges for older drug users in terms of social violence and vulnerability to being incarcerated, which increased their risk for infectious diseases, but living in the city also provided drug users with greater awareness of risks and more access to harm reduction paraphernalia that were unavailable to suburban users. Both urban and suburban users who were incarcerated reported a lack of access to condoms while in jail or prison, but those who lived in the city reported more time incarcerated than those who lived in the suburbs.
Differences were also found regarding when and how users in the different environments became aware of the risks for communicable diseases. Suburban older users appeared to have been informed earlier in their lives regarding the transmission of communicable diseases, specifically those who attended college, whereas older drug users in the city learned later in their drug use trajectories about behaviors to prevent and reduce risk—for some too late. Regardless of when they learned about the risks of unsafe sexual and drug use practices, access to harm reduction paraphernalia was a problem.
The Urban Harm Reduction Center was the primary mode of obtaining clean syringes and other harm reduction paraphernalia (e.g., condoms, cotton, clean water) for urban users. In contrast, the majority of older drug users living in the suburbs relied on relatives or friends who had diabetes to supply clean syringes. Others learned how to ask for syringes in pharmacies without arousing suspicion. Few suburban users had heard of the Urban Harm Reduction Center, and if they did, they often lacked transportation to the city to use its services.
A significant risk behavior for both suburban and city older drug users was found among those who engaged in sex work or sex for drugs. Both urban and suburban users reported engaging in multiple sex relations for work, money, or drugs without using condoms. City drug users appeared to have more access to sexual clients and, therefore, more sexual partners.
While those who had insurance reported no problems accessing healthcare, the majority of older drug users we interviewed did not have health insurance. Those who had Medicaid could obtain free or reduced-cost health services, but they needed to have access to medical facilities. City users could use public transportation to access healthcare clinics, and for emergencies many were given rides to clinics by staff from the Urban Harm Reduction Center and other non-profit organizations who were familiar with the health issues of drug users. Suburban users without a car were more isolated, and many reported a dire lack of public healthcare due to transportation issues. Moreover, they reported that few suburban healthcare workers were aware of the specific issues associated with injection drug use, and harm reduction strategies were rarely discussed with suburban healthcare staff.
Limitations and Future Research
The major limitation of this study is that it is not representative of all older drug users. As an exploratory qualitative study, a probability sample was not required. The goal was to gain a better understanding of older drug users' risk behaviors, specifically a comparison of those living in the city and those in the suburbs, and for this aim a small sample was sufficient. The themes and implications proposed here need to be further examined and verified in future studies with larger samples.
CONCLUSION
Our aim to compare the risk behaviors of older adults by social context of urban versus suburban settings resulted in evidence of similarities regarding risk behaviors but differences in access to risk reduction strategies. While similar risk behaviors were found among older adults who living the suburbs and the inner-city, the surprising finding was that those in the city had some advantages over those in suburban areas. We found that although inner-city older users have greater exposure to violence in their communities and increased opportunities for more partners when engaged in sex work, they also have more access to healthcare and harm reduction paraphernalia than do their counterparts in the public service desert of suburban communities. This finding supports recent reports of rising poverty and concomitant lack of services in the suburbs (Allard and Roth 2010).
Our findings add to emerging research showing that older drug users are particularly vulnerable for contracting infectious diseases and more needs to be done to reach this aging population (Anderson and Levy 2003; Boeri et al. 2008; Emlet 2006; Hser et al. 2004; Johnson and Sterk 2003; Levy et al. 2003). While the social context of the city had many disadvantages, older adults in the city were aware of where to find healthcare services and harm reduction paraphernalia. They also began to share information and resources for risk awareness with other drug users after their contact with the Urban Harm Reduction Center. The message of harm reduction not only gave them motivation to monitor their own risk behaviors, but also appeared to provide them with a goal of passing the message on to others.
In conclusion, we suggest that harm reduction should be extended to reach those needing such services in suburban areas. In addition, since sexual activities are occurring in prisons and jails, condoms and safe sex awareness literature needs to be incorporated. While harm reduction strategies such as syringe exchange are not legal in all states, harm reduction services are widely acknowledged and accepted by public health officials and many in law enforcement as a positive activity. Those working with older drug users, such as prison officials, social workers, and public health workers, could help reduce the transmission of infectious diseases by incorporating harm reduction strategies that reduce risk behaviors among this population. Providing harm reduction services in the suburbs and small towns might be accomplished through a mobile vehicle that uses existing Urban Harm Reduction Centers located in the cities as a base.
Our finding that harm reduction initiatives provide greater risk awareness and lowers risk behaviors among older adult drug users is supported by previous literature (Cohen and Csete 2006; MacPherson, Mulla and Richardson 2006). Recently, the Global Commission on Drug Policy (2011) recommended that more harm reduction efforts are needed worldwide. We suggest that increased effort should be made to extend harm reduction beyond the city into suburban and rural areas, as well as into criminal justice institutions, in the United States.
Acknowledgments
The project described was supported by Award Numbers R15DA021164 and 1R21DA025298 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Footnotes
We used a retrospective longitudinal design for the first 100 participants and a prospective longitudinal design for an additional subsample of 30 female users. A life history matrix collected face-to-face with paper and pencil helped to focus the participant on retrospective life events as well as to develop rapport between interviewer and participant and establish an additional validating strategy. A brief drug history matrix was used to collect data on first use of each drug, past 6 months use, past 30-day use and routes of administration. An audio-recorded, in-depth life history interview followed the completion of the matrices. The interviewer employed the matrices during the interview to focus the participant on changes in drug use, social roles and risk behaviors. For example, the life history matrix informed the interviewer on which questions to focus or explore more deeply, and the drug history matrix guided questions on drug use and drug-related risk behaviors, as well as provided a tool for memory recall. The subsample of 30 female methamphetamine users employed the same instruments and mixed methods design but also included two follow-up interviews and more questions on risk behaviors. Additionally, we conducted four focus groups with self-selected women who desired to participate in this type of interview.
Reimbursement for participants has been shown to be ethical and useful in collecting research on stigmatized behaviors, such as drug use (Kaplan and Lambert 1995; Wiebel 1990).
We began by open coding the transcribed interviews from both studies to identify categories that were eventually organized into a conceptual scheme. During the first stage of open coding, the team of three researchers each coded the same five transcripts using known trajectory-informed categories (e.g., initiation, progression, cessation, relapse) and adding codes for new concepts found in the data. The research team discussed the coding process at weekly meetings to promote reliability between coders. The team then organized the codes into the main themes and sub-themes or categories. At least two coders coded each interview transcript and added new codes as needed. We followed an iterative model of triangulation to establish validity. The iterative model of triangulating data throughout the study—comparing information collected from various data sources, and addressing issues of validity and reliability as the study progresses—has been shown to provide greater confidence in understanding complex information (Boeri 2007; Rhodes and Moore 2001). Since initial coding began with the first interviews and continued during the data collection, we were able to clarify inconsistencies found between data sources in further data collection.
REFERENCES
- Agar Michael. The Professional Stranger: An Informal Introduction to Ethnography. Academic Press; New York: 1980. [Google Scholar]
- Agar Michael. Ripping and Running. Seminar Press; New York: 1973. [Google Scholar]
- Akers Ronald L. Social Learning and Social Structure: A General Theory of Crime and Deviance. Northeastern University Press; Boston, MA: 1998. [Google Scholar]
- Akers Ronald L., Kron Marvin D., Lanza-Kaduce Lonn, Radosevich Marcia. Social Learning and Deviant Behavior: A Specific Test of a General Theory. American Sociological Review. 1979;44:636–55. [PubMed] [Google Scholar]
- Allard Scott, Ross Benjamin. The Metropolitan Policy Program at Brookings. Brookings; Washington DC: 2010. Strained Suburbs: The Social Service Challenges of Rising Suburban Poverty. [Google Scholar]
- Alwin Duane F. The Political Impact of the Baby Boom: Are there Persistent Generational Differences in Political Beliefs and Behaviors? Generations. 1998;22(1):46–54. [Google Scholar]
- Anderson Tammy L., Levy Judith A. Marginality among Older Injectors in Today's Illicit Drug Culture: Assessing the Impact of Ageing. Addiction. 2003;98:761–70. doi: 10.1046/j.1360-0443.2003.00388.x. [DOI] [PubMed] [Google Scholar]
- Auerbach Judith D. HIV/AIDS and Aging: Interventions for Older Adults: Foreword. Journal of Acquired Immune Deficiency. 2003;33:S37–38. [PubMed] [Google Scholar]
- Becker Howard S. Becoming a Marijuana User. The American Journal of Sociology. 1953;59:235–42. [Google Scholar]
- Berkman Lisa F., Glass Thomas. Social Integration, Social Networks, Social Support, and Health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. pp. 174–90. [Google Scholar]
- Biernacki Paul. Pathways from Heroin Addiction: Recovery without Treatment. Temple University Press; Philadelphia: 1986. [Google Scholar]
- Blow Frederic C. Substance Abuse among Baby Boomers: An Invisible Epidemic. In: Blow FC, editor. Substance Abuse among Baby Boomers. 2000. DHHS Publication No. SMA 98-3179. [Google Scholar]
- Bluthenthal Ricky N., Watters John K. Multimethod Research from Targeted Sampling to HIV Risk Environments. In: Lambert EY, Ashery RS, Needle RH, editors. Qualitative Methods in Drug Abuse and HIV Research. US Government Printing Office; Washington DC: 1995. pp. 212–30. NIDA Research Monograph 157 NIH Publication No. 95-4025. [PubMed] [Google Scholar]
- Boeri Miriam W. A Third Model of Triangulation: Continuing the Dialogue with Rhineberger, Hartmann and Van Valey. Journal of Applied Social Science. 2007;1(1):52–48. [Google Scholar]
- Boeri Miriam W. Hell, I'm an Addict but I Ain't No Junkie. An Ethnographic Analysis of Aging Heroin Users. Human Organization. 2004;63(2):236–45. [Google Scholar]
- Boeri Miriam W. PhD dissertation. Department of Sociology, Georgia State University; Atlanta: 2002. I'm An Addict but I Ain't no Junkie: An Ethnographic Analysis of the Drug Career of Baby Boomers. [Google Scholar]
- Boeri Miriam W., Sterk Claire E., Elifson Kirk W. Reconceptualizing Categories of Early and Late-Onset: A Life Course Analysis of Older Heroin Users. The Gerontologist. 2008;48:637–45. doi: 10.1093/geront/48.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeri Miriam W., Sterk Claire E., Elifson Kirk W. Baby Boomer Drug Users: Career Phases, Social Control and Social Learning Theory. Sociological Inquiry. 2006;76(2):264–91. [Google Scholar]
- Boshears Paul, Boeri Miriam, Harbry Liam. Addiction and Sociality: Perspectives from Methamphetamine Users in Suburban USA. Addiction Research and Theory. 2011;19(4):289–301. doi: 10.3109/16066359.2011.566654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brecht May-Lynn, Huang David, Evans Elizabeth, Hser Yih-Ing. Polydrug Use and Implications for Longitudinal Research: Ten-year Trajectories for Heroin, Cocaine, and Methamphetamine Users. Drug and Alcohol Dependence. 2008;96:193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruckner Erika, Mayer Karl Ulrich. Collecting Life History Data. In: Giele Janet Z., Elder Glen H., Jr., editors. Methods of Life Course Research: Qualitative and Quantitative Approaches. Sage; Thousand Oaks, CA: 1998. pp. 469–99. [Google Scholar]
- Capel WC, Peppers LG. The Aging Addict: A Longitudinal Study of Known Abusers. Addictive Diseases: An International Journal. 1978;3(3):389–403. [PubMed] [Google Scholar]
- Carlson Robert G., Siegal Harvey A., Falck Russel S. Qualitative Research Methods in Drug Abuse and AIDS Prevention Research: An Overview. In: Lambert Elizabeth Y., Ashery Rebecca S., Needle Richard H., editors. Qualitative Methods in Drug Abuse and HIV Research. US Government Printing Office; Washington DC: 1995. pp. 6–26. NIDA Research Monograph, 157 NIH Publication No. 95-4025. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV/AIDS Surveillance Report, 2006. Vol. 18. US Department of Health and Human Services; Atlanta: 2008a. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV/AIDS among Persons Aged 50 and Older CDC HIV/AIDS Fact Sheet, February. US Department of Health and Human Services; Atlanta: 2008b. [Google Scholar]
- Charmaz Kathy. Grounded Theory. In: Emerson Robert M., editor. Contemporary Field Research: Perspectives and Formulations. Waveland Press; Prospect Heights, IL: 2001. pp. 335–52. [Google Scholar]
- Clatts Michael C., Davis W. Rees, Atillasoy Aylin. Hitting a Moving Target: The Use of Ethnographic Methods in the Evaluation of AIDS Outreach Programs for Homeless Youth in NYC. In: Lambert Elizabeth Y., Ashery Rebecca S., Needle Richard H., editors. Qualitative Methods in Drug Abuse and HIV Research. US Government Printing Office; Washington DC: 1995. pp. 117–35. NIDA Research Monograph, 157 NIH Publication No. 95-4025. [PubMed] [Google Scholar]
- Clausen John A. Life Reviews and Life Stories. In: Giele Janet Z., Elder Glen H., Jr., editors. Methods of Life Course Research: Qualitative and Quantitative Approaches. Sage; Thousand Oaks, CA: 1998. pp. 189–211. [Google Scholar]
- Cloward Richard A., Ohlin Lloyd E. Delinquency and Opportunity. Free Press; New York: 1960. [Google Scholar]
- Cohen Jonathan, Csete Joanne. As Strong as the Weakest Pillar: Harm Reduction, Law Enforcement and Human Rights. International Journal of Drug Policy. 2006;17:101–03. [Google Scholar]
- Dai Bingham. Opium Addiction in Chicago. Patterson Smith; Montclair, NJ: 1937. [Google Scholar]
- Dole Vincent P. Addictive Behavior. Scientific American. 1980;243:138–54. doi: 10.1038/scientificamerican1280-138. [DOI] [PubMed] [Google Scholar]
- Dole Vincent P., Nyswander Marie E. A Medical Treatment for Diacetylmorphine (Heroin) Addiction. Journal of the American Medical Association. 1965;193:646–50. doi: 10.1001/jama.1965.03090080008002. [DOI] [PubMed] [Google Scholar]
- Elder Glen H., Jr. Children of the Great Depression: Social Change in Life Experience. Westview; Boulder, CO: 1999. [Google Scholar]
- Emlet Charles A. You're Awfully Old to Have this Disease': Experiences of Stigma and Ageism in Adults 50 Years and Older Living with HIV/AIDS. The Gerontologist. 2006;46:781–90. doi: 10.1093/geront/46.6.781. [DOI] [PubMed] [Google Scholar]
- Faupel Charles E. Shooting Dope: Career Patterns of Hard-Core Heroin Users. University of Florida Press; Gainesville, FL: 1991. [Google Scholar]
- Gfroerer Joseph, Penne Michael, Pemberton Michael, Folsom Ralph. Substance Abuse Treatment Need among Baby Boomers in 2020: The Impact of the Aging Baby-Boom Cohort. Drug and Alcohol Dependence. 2003;69:127–35. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- Gfroerer Joseph, Penne Michael, Pemberton Michael, Folsom Ralph. The Aging Baby Boom Cohort and Future Prevalence of Substance Abuse. In: Korper SP, Council CL, editors. Substance Use by Older Adults: Estimates of Future Impact on the Treatment System. U.S. Department of Health and Human Services; U.S. Government Printing Office; Rockville, MD: 2002. Publication No. SMA 03-3763, Analytical Series A-21:79-93. [Google Scholar]
- Glantz Meyer D. Alcohol and Drug Abuse Weekly. 1995;7(36) [Google Scholar]
- Glaser Barney G., Strauss Anslem. Discovery of Grounded Theory. Aldine; New York: 1967. [Google Scholar]
- Global Commission on Drug Policy War on Drugs: Report of the Global Commission on Drug Policy. 2011 Retrieved June 2011 at www.globalcommissionondrugs.org.
- Gomberg Edith Linsanky, Zucker Robert A. Substance Use and Abuse in Old Age. In: Nordhus Inger Hilde, Vanden Gary R., Berg Stig, Fromholt Pia., editors. Clinical Geropsychology. American Psychological Association; Washington: 1998. pp. 189–204. [Google Scholar]
- Goode Erich. Drugs in American Society. 5th ed. McGraw-Hill College; New York: 1999. [Google Scholar]
- Hser Yih-Ing, Gelberg Lillian, Hoffman Valerie, Grella Christine, McCarthy William, Anglin M. Douglas. Health Conditions among Aging Narcotics Addicts: Medical Examination Results. Journal of Behavioral Medicine. 2004;27:607–22. doi: 10.1007/s10865-004-0005-x. [DOI] [PubMed] [Google Scholar]
- Hser Yih-Ing, Huang David, Brecht Mary-Lynn, Li Libo, Evans Elizabeth. Contrasting Trajectories of Heroin, Cocaine and Methamphetamine Use. Journal of Addictive Diseases. 2008;27:13. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inciardi James A., Lockwood Dorothy, Pottieger Anne E. Women and Crack Cocaine. MacMillam; New York: 1993. [Google Scholar]
- Jessor Richard, Jessor Shirley L. Problem Behavior and Psychosocial Development: A Longitudinal Study of Youth. Academic Press; New York: 1977. [Google Scholar]
- Johnson Bruce D. Marihuana Users and Drug Subcultures. Wiley-Interscience; New York: 1973. [Google Scholar]
- Johnson Wendell, Sterk Claire E. Late-Onset Crack Users: An Emergent HIV Risk Group. Journal of Acquired Immune Deficiency Syndromes. 2003;33:S229–32. [PubMed] [Google Scholar]
- Kandel Denise B. Drug and Drinking Behavior among Youth. Annual Review of Sociology. 1980;6:235–85. [Google Scholar]
- Kaplan Charles D., Lambert Elizabeth Y. The Daily Life of Heroin-Addicted Persons: The Biography of Specific Methodology. In: Lambert Elizabeth Y., Ashery Rebecca S., Needle Richard H., editors. Qualitative Methods in Drug Abuse and HIV Research. US Government Printing Office; Washington, DC: 1995. pp. 100–16. NIDA Research Monograph, 157 NIH Publication No. 95-4025. [PubMed] [Google Scholar]
- Kaplan Howard B. Self-Attitudes and Deviant Behavior. Goodyear; Pacific Palisades, CA: 1975. [Google Scholar]
- Keister Lisa A., Deeb-Sossa Natalia. Are Baby Boomers Richer than their Parents? Intergenerational Patterns of Wealth Ownership in the United States. Journal of Marriage and the Family. 2001;63(2):599–80. [Google Scholar]
- King Christopher J., Van Hasselt Vincent B., Segal Daniel L., Hersen Michel. Diagnosis and Assessment of Substance Abuse in Older Adults: Current Strategies and Issues. Addictive Behaviors. 1994;19(1):41–55. doi: 10.1016/0306-4603(94)90050-7. [DOI] [PubMed] [Google Scholar]
- Kwiatkowski Carol F., Booth Robert E. HIV Risk Behaviors among Older American Drug Users. Journal of Acquired Immune Deficiency Syndromes. 2003;33:S131–37. doi: 10.1097/00126334-200306012-00010. [DOI] [PubMed] [Google Scholar]
- Laub John H., Sampson Robert J. Shared Beginnings, Divergent Lives: Delinquent Boys to Age 71. Harvard University Press; Cambridge, MA: 2003. [Google Scholar]
- Leshner Alan, Koob George F. Drugs of Abuse and the Brain. Proceedings of the Association of American Physicians. 1999;111:99–108. doi: 10.1046/j.1525-1381.1999.09218.x. [DOI] [PubMed] [Google Scholar]
- Levin Saul M., Kruger Janice., editors. Substance Abuse among Older Adults: A Guide for Social Service Providers. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2000. [Google Scholar]
- Levy Judith A. AIDS and Injecting Drug Use in Later Life. Research on Aging. 1998;20:776–97. [Google Scholar]
- Levy Judith A., Ory Marcia G., Crystal Stephen., editors. The Graying of the AIDS Epidemic: HIV/AIDS and People Age 50 and Older. Journal of Acquired Immune Deficiency. 2003;33(S2):59–67. [Google Scholar]
- Lindesmith Alfred R. Addiction and Opiates. Aldine; Chicago: 1968. [Google Scholar]
- Lindesmith Alfred R. A Sociological Theory of Drug Addiction. American Journal of Sociology. 1938;43:593–61. [Google Scholar]
- MacPherson Donald, Mulla Zarina, Richardson Lindsey. The Evolution of Drug Policy in Vancouver, Canada: Strategies for Preventing Harm from Psychoactive Substances. International Journal of Drug Policy. 2006;17:127–32. [Google Scholar]
- Milkman Harvey, Sunderwirth Stanley. Doorway to Excess. In: Inciardi JA, McElrath K, editors. The American Drug Scene: An Anthology. Roxbury; Los Angeles: 1995. pp. 12–22. [Google Scholar]
- Miller Norman S. Addiction Psychiatry: Current Diagnosis and Treatment. Wiley; New York: 1995. [Google Scholar]
- Morgan David L. Facts and Figures about the Baby Boom. Generations. 1998;22(1):10–16. [Google Scholar]
- Morgan John, Zimmer Lynn. The Social Pharmacology of Smokeable Cocaine: Not All It's Cracked Up to Be. In: Reinarman Craig, Levine Harry G., editors. Crack in America: Demon Drugs and Social Justice. University of California Press; Berkeley: 1997. pp. 131–70. [Google Scholar]
- Murphy Debra A., Hser Yih-Ing, Huang David, Brecht Mary-Lynn, Herbeck Diane. Self Report of Longitudinal Substance Use: A Comparison of the UCLA Natural History Interview and the Addiction Severity Index. The Journal of Drug Issues. 2010;40(2):495–515. doi: 10.1177/002204261004000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musto David F. The American Disease: Origins of Narcotic Control. 3rd ed. Oxford University Press; New York: 1999. [Google Scholar]
- Needle Richard H., Coyle Susan. Community Based Outreach Risk Reduction Strategy to Prevent Risk Behaviors in Out-of-Treatment Injection Drug Users. NIDA/NIH Consensus Development Document; Rockville MD: 1997. [Google Scholar]
- Nichter Mark, Quintero Gilbert, Nichter Mimi, Mock Jeremiah, Shakib Sohaila. Qualitative Research: Contributions to the Study of Drug Use, Drug Abuse and Drug Use(r)-Related Interventions. Substance Use & Misuse. 2004;39(10–12):1907–69. doi: 10.1081/ja-200033233. [DOI] [PubMed] [Google Scholar]
- Nokes Kathleen M., Emlet Charles A. Health Issues of Older Adults with HIV/AIDS. In: Burbank PM, editor. Vulnerable Older Adults: Health Care Needs and Interventions. Springer; New York: 2006. pp. 209–234. [Google Scholar]
- Pach Alfred, III, Gorman E. Michael. An Ethno-epidemiological Approach for the Multi-site Study of Emerging Drug Abuse Trends: The Spread of Methamphetamine in the United States of America. Bulletin on Narcotics. 2002;Vol LIV Mos. 1 and 2. [Google Scholar]
- Page J. Bryan, Singer Merrill. Comprehending Drug Use: Ethnographic Research at the Social Margins. Rutgers University Press; New Brunswick, NJ: 2010. [Google Scholar]
- Petersen David M. Illegal Drug Use, Older Addicts, and the Maturing Out Hypothesis. In: Glantz Meyer D., Petersen David M., Whittington Frank J., editors. Drugs and the Elderly: Adult Research Issues. National Institute on Drug Abuse: Department of Health and Human Services; 1983. pp. 45–7. [Google Scholar]
- Reinarman Craig, Levine Harry G. Crack in Context: America's Latest Demon Drug. In: Reinarman Craig, Levine Harry G., editors. Crack in America: Demon Drugs and Social Justice. University of California Press; Berkeley: 1997. pp. 1–17. [Google Scholar]
- Rhodes Thomas, Moore David. On the Qualitative in Drug Research: Part One. Addiction Research and Theory. 2001;9:279–97. [Google Scholar]
- Romero-Daza Margaret Weeks, Singer Merrill. Nobody Gives a Damn if I live or Die”: Violence, Drugs, AND Street-Level Prostitution in Inner-City Hartford, Connecticut. Medical Anthropology. 2003;22:233–59. doi: 10.1080/01459740306770. [DOI] [PubMed] [Google Scholar]
- Rosenbaum Marsha. Women on Heroin. Rutgers University Press; New Brunswick., NJ: 1981. [Google Scholar]
- Rosenberg Helen. Use and Abuse of Illicit Drugs among Older People. In: Gurnack Anne M., editor. Older Adults' Misuse of Alcohol, Medicines, and Other Drugs: Research and Practice Issues. Springer; New York: 1997. pp. 206–27. [Google Scholar]
- Sampson Robert J., Laub John H. Crime in the Making: Pathways and Turning Points through Life. Harvard University Press; Cambridge, MA: 1993. [Google Scholar]
- Sampson Robert J., Laub John H. Crime and Deviance in the Life Course. Annual Review of Sociology. 1992;18:63–84. [Google Scholar]
- Schuckit Marc A. Drug and Alcohol Abuse: A Clinical Guide to Diagnosis and Treatment. 2nd ed. Plenum; New York: 1984. [Google Scholar]
- Scott Jacqueline, Alvin Duane. Retrospective versus Prospective Measurement of Life Histories in Longitudinal Research. In: Giele Janet Z., Elder Glen H., Jr., editors. Methods of Life Course Research: Qualitative and Quantitative Approaches. Sage; Thousand Oaks, CA: 1998. pp. 98–127. [Google Scholar]
- Sobell Linda C., Sobell Mark B., Leo Gloria I., Cancilla Anthony. Reliability of a Timeline Method: Assessing Normal Drinkers' Reports of Recent Drinking and a Comparative Evaluation across Several Populations. British Journal of Addiction. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Sterk Claire E. Fast Lives: Women Who Use Crack Cocaine. Temple University Press; Philadelphia: 1999. [Google Scholar]
- Strauss Anselm, Corbin Juliet. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 2nd ed. Sage; Thousand Oaks, CA: 1998. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) National Household Survey on Drug Abuse Main Findings 1998. 2000a. DHHS Pub. No. (SMA) 00-3381. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Summary Findings from the 1999 National Household Survey on Drug Abuse. 2000b. DHHS Pub. No. (SMA) 00-3466. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Summary of Findings from the 1998 National Household Survey on Drug Abuse. 1999. DHHS Pub. No. (SMA) 99-3328. [Google Scholar]
- Sylvestre Diane. Approaching Treatment for Hepatitis C Infection in Substance Users. Clinical Infectious Diseases. 2006;41:S79–82. doi: 10.1086/429501. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) World Drug Report. 2007. United Nations Publication ISBN 978-92-1-148222-5. [Google Scholar]
- Watters John, Biernacki Patrick. Targeted Sampling: Options for the Study of Hidden Populations. Social Problems. 1989;36:416–30. [Google Scholar]
- Wiebel W. Wayne. Identifying and Gaining Access to Hidden Populations. In: Lambert Elizabeth., editor. The Collection and Interpretation of Data from Hidden Populations. U.S. Government Printing Office; Washington, DC: 1990. pp. 4–11. National Institute on Drug Abuse Research Monograph 98. DHHS Pub. No. (ADM) 90-1678. [PubMed] [Google Scholar]
- Winick Charles. Maturing Out of Narcotic Addiction. Bulletin on Narcotics. 1962;6:1. [Google Scholar]
- Zickler Patrick. Twin Studies Help to Define the Role of Genes in Vulnerability to Drug Abuse. NIDA Notes. 1999;14(4) Bethesda, MD: Department of Health and Human Studies, National Institutes of Health. [Google Scholar]
- Zinberg Norman E. Drug, Set, and Setting: The Basis for Controlled Intoxicant Use. Yale University Press; New Haven, CT: 1984. [Google Scholar]
- Zinberg Norman E. Nonaddictive Opiate Use. In: DuPont Robert I., Goldstein Avram, O'Donnel John., editors. Handbook on Drug Abuse. National Institute on Drug Abuse; Rockville, MD: 1979. pp. 303–13. [Google Scholar]
- Zinberg Norman, Lewis DC. Narcotic Usage. A Spectrum of a Difficult Medical Problem. New England Journal of Medicine. 1964;270:989–93. doi: 10.1056/NEJM196405072701906. [DOI] [PubMed] [Google Scholar]