Abstract
We describe the course and likely pathophysiology of impending anterior ischemic optic neuropathy (AION) and retinal vein occlusion in a 56-year-old man with polycythemia vera managed with interferon alpha for 2 years. Our patient presented with decreased vision, scintillating scotomata, and floaters. Fundus examination findings and results of a fluorescein angiogram led to the diagnosis of impending AION and retinal vein occlusion. Considering that both polycythemia vera and interferon have possible influences on vascular occlusion and optic disc edema, we stopped interferon treatment and immediately attempted to treat the polycythemia vera empirically with pentoxifylline and any interferon-associated inflammation with prednisone. Our patient experienced complete resolution of fundus abnormalities and return of normal vision within 3 weeks, which may be attributed to our successful treatment of both etiologies. Thus, further study is warranted to elucidate the treatment of both polycythemia vera and interferon-induced impending AION.
Keywords: optic disc edema, interferon alpha, vascular occlusion, Roth spot, autoantibody, pentoxifylline
Case report
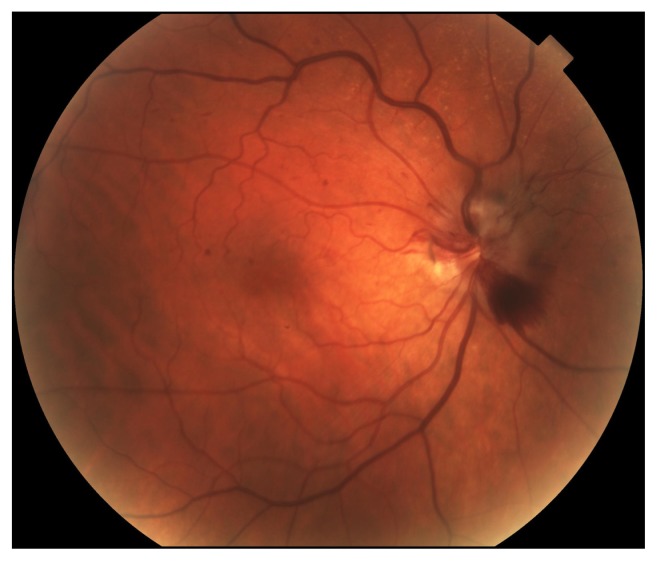
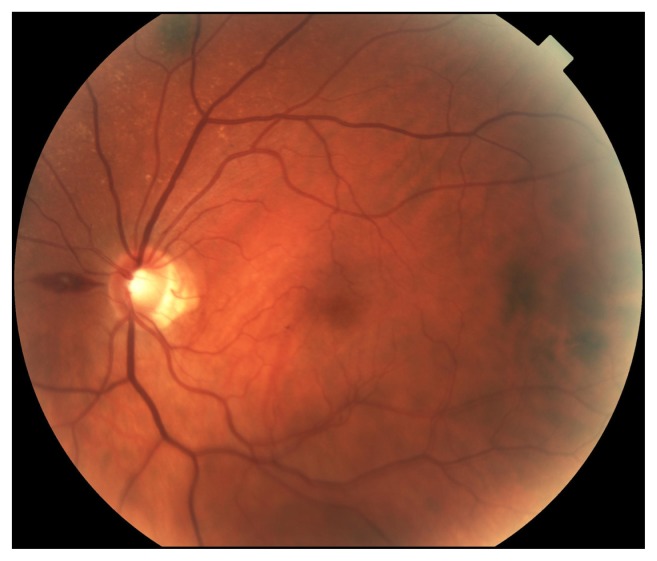
A 56-year-old Caucasian male with polycythemia vera controlled with interferon alpha treatment for 2 years presented to our institution with decreased vision, greater on the right than left, scintillating scotomata, and floaters. His hematocrit the week prior was 39.9%. On examination, his best corrected visual acuity was 20/20 in both eyes (OU). Intraocular pressures were 14 mmHg in the right eye (OD) and 12 mmHg in the left eye (OS). He saw 8/8 AO test plates OU with equal brightness sense OU. There was a trace afferent papillary defect OD. Fundus examination on the right showed nerve fiber layer swelling at 12 and 6 o’clock, a very distended and tortuous superior branch retinal vein, one flame-shaped peripapillary hemorrhage, and one preretinal hemorrhage alongside areas of ischemia at the inferior pole (Figure 1). The left eye showed one peripapillary hemorrhage with a white center (Roth spot) with slight retinal nerve fiber layer swelling at the optic disc margin superiorly and inferiorly, but much less venous distention (Figure 2). Fluorescein angiography confirmed impending retinal vein occlusion with delayed transit time (20 seconds for the right superior hemi vein), more in OD than OS, but no choroidal infarction. Interferon was stopped immediately, and the patient started pentoxifylline 400 mg every day to treat polycythemia vera, and prednisone 40 mg every day to counter any interferon-induced inflammation. Within 3 weeks, his vision became clear, the afferent papillary defect resolved, and fundus examination revealed complete resolution of the aforementioned vascular abnormalities. He was slowly tapered down to prednisone 7.5 mg every other day and maintained on pentoxifylline 400 mg three times a day.
Figure 1.
Fundus examination OD at presentation revealing nerve fiber layer swelling at 12 and 6 o’clock, a very distended and tortuous superior branch retinal vein, one flame-shaped peripapillary hemorrhage, and one preretinal hemorrhage alongside areas of ischemia at the inferior pole.
Abbreviation: OD, right eye.
Figure 2.
Fundus examination OS at presentation showing one Roth spot with slight retinal nerve fiber layer swelling at the optic disc margin superiorly and inferiorly, but much less venous distention than OD.
Abbreviations: OD, right eye; OS, left eye.
Discussion
Here we describe the course and likely pathophysiology of interferon alpha and polycythemia vera-associated impending AION, retinal vessel ischemia, and hemorrhage. Our patient’s bilateral optic disc edema did not have the supporting signs or symptoms of elevated intracranial pressure or malignant hypertension. He also did not have a complete AION because resolution was complete. In fact, our patient’s optic disc edema was concentrated at the superior and inferior poles, corresponding to the locations of venous compromise. Thus, considering the associated retinal venous distention and hemorrhage, we attributed the patient’s optic disc edema to impending AION and his delayed filling on fluorescein angiogram to retinal vein occlusion. We attribute these fundus examination findings to axoplasmic stasis and retinal hemorrhage resulting from optic and retinal vascular occlusion and venous backflow,1 all likely secondary to complications of interferon and polycythemia vera. Interferon has been documented to cause occlusion directly, possibly from inflammation.2 Interferon may produce autoantibodies and incite inflammation in the vessels of the optic disc,2 contributing to an impending AION. This can cause optic nerve ischemia and fiber swelling,1 which can progress further to retinal vein occlusion and hemorrhage, as well as to AION with permanent losses of visual field and visual acuity.3
The preretinal hemorrhages and Roth spots seen in our patient have been documented as complications with both interferon4 as well as myeloproliferative disorders.5 Polycythemia vera poses additional risk factors for retinal vein occlusion, including higher whole blood viscosity, reduced red cell deformability,6 and abnormal red cell adhesion. Diminished membrane fluidity of red blood cells plays a role in microvascular occlusion in patients with polycythemia vera.7 In addition, JAK2 kinase mutation in patients with polycythemia vera causes abnormal phosphorylation of CD 239 on red blood cells, which allows its ligation with the laminin alpha5 chain on the apical surface of endothelial cells.8 This adhesion has been demonstrated to be strong enough to withstand sheer stresses of postcapillary venules.8 Thus, polycythemia vera-associated red blood cell adhesion may be another strong factor in the pathophysiology of venous occlusion.6 Considering that both polycythemia vera and interferon are possible influences on vascular occlusion and optic disc edema and the pathophysiology described, we immediately attempted to treat the polycythemia vera empirically with pentoxifylline to increase red blood cell fluidity and the interferon-associated inflammation with prednisone. Our patient also had a history of hypotension to 95/65 mmHg, which was monitored, given that hypotension is a risk factor for AION.9 Our patient experienced complete resolution of fundus abnormalities and return of normal vision, which may be attributed to successful treatment of both etiologies, though there remains the possibility of spontaneous resolution. Thus, further study is warranted to elucidate the treatment of both polycythemia vera and interferon-induced impending AION.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Van Stavern GP. Optic disc edema. Semin Neurol. 2007;27(3):233–243. doi: 10.1055/s-2007-979684. [DOI] [PubMed] [Google Scholar]
- 2.Bajaire BJ, Paipilla DF, Arrieta CE, Oudovitchenko E. Mixed vascular occlusion in a patient with interferon-associated retinopathy. Case Report Ophthalmol. 2011;2(1):23–29. doi: 10.1159/000323942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fraunfelder FW, Fraunfelder FT. Interferon alfa-associated anterior ischemic optic neuropathy. Ophthalmology. 2011;118(2):408–411. doi: 10.1016/j.ophtha.2010.03.063. [DOI] [PubMed] [Google Scholar]
- 4.Hayasaka S, Nagaki Y, Matsumoto M, Sato S. Interferon associated retinopathy. Br J Ophthalmol. 1998;82(3):323–325. doi: 10.1136/bjo.82.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang PK, Sanjay S. Visual disturbance as the first symptom of chronic myeloid leukemia. Middle East Afr J Ophthalmol. 2011;18(4):336–338. doi: 10.4103/0974-9233.90143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wautier MP, Héron E, Picot J, Colin Y, Hermine O, Wautier JL. Red blood cell phosphatidylserine exposure is responsible for increased erythrocyte adhesion to endothelium in central retinal vein occlusion. J Thromb Haemost. 2011;9(5):1049–1055. doi: 10.1111/j.1538-7836.2011.04251.x. [DOI] [PubMed] [Google Scholar]
- 7.Ambrus JL, Ambrus CM, Dembinsky W, et al. Thromboembolic disease susceptibility related to red cell membrane fluidity in patients with polycythemia vera and effect of phlebotomies. J Med. 1999;30(5/6):299–304. [PubMed] [Google Scholar]
- 8.Wautier MP, El Nemer W, Gane P, et al. Increased adhesion to endothelial cells of erythrocytes from patients with polycythemia vera is mediated by laminin alpha5 chain and Lu/BCAM. Blood. 2007;110(3):894–901. doi: 10.1182/blood-2006-10-048298. [DOI] [PubMed] [Google Scholar]
- 9.Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009;28(1):34–62. doi: 10.1016/j.preteyeres.2008.11.002. [DOI] [PubMed] [Google Scholar]