Abstract
We previously reported that mice lacking alpha/beta and gamma interferon receptors (IFN-α/βR and -γR) uniformly exhibit paralysis following infection with the dengue virus (DENV) clinical isolate PL046, while only a subset of mice lacking the IFN-γR alone and virtually no mice lacking the IFN-α/βR alone develop paralysis. Here, using a mouse-passaged variant of PL046, strain S221, we show that in the absence of the IFN-α/βR, signaling through the IFN-γR confers approximately 140-fold greater resistance against systemic vascular leakage-associated dengue disease and virtually complete protection from dengue-induced paralysis. Viral replication in the spleen was assessed by immunohistochemistry and flow cytometry, which revealed a reduction in the number of infected cells due to IFN-γR signaling by 2 days after infection, coincident with elevated levels of IFN-γ in the spleen and serum. By 4 days after infection, IFN-γR signaling was found to restrict DENV replication systemically. Clearance of DENV, on the other hand, occurred in the absence of IFN-γR, except in the central nervous system (CNS) (brain and spinal cord), where clearance relied on IFN-γ from CD8+ T cells. These results demonstrate the roles of IFN-γR signaling in protection from initial systemic and subsequent CNS disease following DENV infection and demonstrate the importance of CD8+ T cells in preventing DENV-induced CNS disease.
INTRODUCTION
The four serotypes of dengue virus (DENV1 to -4) belong to the Flaviviridae family, which also includes West Nile virus (WNV), St. Louis encephalitis virus (SLEV), Japanese encephalitis virus (JEV), and yellow fever virus (YFV). More than 2.5 billion people live in areas where DENV is endemic, and approximately 50 million people are infected each year (17). DENV generally manifests as an acute systemic infection that is cleared within 14 days (46). In most cases, infected individuals develop a febrile illness (dengue fever [DF]) characterized by flu-like symptoms, often accompanied by retro-orbital pain, ostealgia, and maculopapular rash. In nearly 500,000 cases per year, patients develop severe vascular leakage, which may result in hypovolemic shock (dengue hemorrhagic fever/dengue shock syndrome [DHF/DSS]), ultimately leading to fatality rates as high as 10 to 15% in some countries or more than 25,000 deaths worldwide each year (15, 17). In a subset of both DF and DHF/DSS cases (16), DENV infection was linked to encephalitis and signs of encephalopathy, including lethargy, confusion, seizure, and coma, as well as delayed neurological symptoms, such as paralysis of extremities, loss of sensation, and psychosis (2, 21, 23, 30, 36, 38, 43). DENV-induced neurological disease is being increasingly recognized as an important component of dengue disease in humans independent of DF and DHF/DSS (24). The prevalence of DENV-induced neurological disease has been estimated to be 4.2% of DENV cases (44) and as high as 18% of undiagnosed suspected viral central nervous system (CNS) infections in regions where DENV is endemic (21, 23).
In the last decade, DENV has increasingly been linked to neurological disease in both the presence and absence of DF. Viruses of the Flaviviridae family generally cluster in a phylogenetic pattern that mirrors the typical disease manifestations they cause (13); for example, encephalitic flaviviruses cluster together. DENV, however, usually causes hemorrhagic illness but is genetically more homologous to the encephalitic viruses, including WNV, SLEV, and JEV, than it is to other hemorrhagic flaviviruses, such as YFV, based on several analyses of the nonstructural (NS) proteins NS3 and NS5 (11, 13). The close relationship of DENV to encephalitic flaviviruses may help explain the capacity of DENV to cause neurological disease and, possibly, infection of the CNS in humans (6, 37). Additionally, DENV-induced paralysis has been reported in numerous mouse models (4, 49), but only a few studies have investigated this phenomenon (1, 18, 20). Presently, whether DENV infects the CNS in natural human infections continues to be a subject of debate (25, 30, 32).
Mice lacking the alpha/beta interferon and gamma interferon receptors (IFN-α/βR and IFN-γR) in the 129/Sv genetic background (AG129) are highly susceptible to disease resembling human DHF/DSS, as well as paralysis, following infection with mouse-passaged variants of DENV2 clinical isolate PL046 (5, 35, 40, 51). In contrast, congenic mice lacking only IFN-α/βR (A129) are largely protected from DENV-induced paralysis (39). Using the DENV2 clinical isolate PL046, we previously reported that IFN-α/βR signaling is essential for early control of DENV infection, while IFN-γR activity is more important for protection against DENV-induced paralysis (39). In the present study, we used the mouse-adapted DENV2 strain S221, which can induce a lethal DHF/DSS-like disease in both AG129 and A129 mice, to investigate the role of IFN-γR signaling during DENV infection by comparing the doubly-deficient AG129 mice with the singly-deficient A129 mice.
MATERIALS AND METHODS
Mice.
129/Sv mice deficient in the IFN-α/β receptor (A129) or both the IFN-α/β receptor and the IFN-γ receptor (AG129) were housed under specific-pathogen-free conditions. All experiments were approved by the Animal Care Committee at the La Jolla Institute for Allergy and Immunology (LIAI). The mice were age and sex matched. Mice between 5 and 6 weeks of age were inoculated intravenously in the lateral tail vein with 200 μl of the DENV2 strain S221 in phosphate-buffered saline (PBS) (Invitrogen) containing 10% fetal bovine serum (FBS) (Gemini Bio-Products). For survival studies, mice were sacrificed when moribund or upon developing signs of progressive paralysis.
Cell cultures and viral stocks.
C6/36 cells were obtained from the American Type Culture Collection and cultured at 28°C in Leibovitz's L-15 medium (Gibco) supplemented with penicillin, streptomycin, HEPES, and 10% FBS. The DENV2 strain S221 is a triple-plaque-purified clone from the D2S10 quasispecies population found to contain 2 mutations in the envelope protein relative to PL046 which enable the induction of acute lethal disease, like D2S10 (40). Strain S221 was amplified in C6/36 cells and purified using a sucrose density gradient, as described previously (35). Genomic equivalents (GE) were quantified by real-time reverse transcription-PCR (RT-PCR). Based on a standard baby hamster kidney cell (BHK-21) plaque assay, there are approximately 5 × 104 GE/PFU for strain S221.
Viral RNA isolation.
Mice were euthanized by isoflurane inhalation. Blood was collected into serum separator tubes (Sarstedt), and mice were perfused with 30 to 60 ml of PBS. Small intestines were collected into PBS, filleted longitudinally, rinsed, and chopped into small pieces before being placed into RNAlater reagent (Qiagen). All other organs were harvested directly into RNAlater reagent. Subsequently, organs were homogenized for 3 min in 1 ml of tissue lysis buffer (buffer RLT) with β-mercaptoethanol (Qiagen) using a Mini-BeadBeater-8 (BioSpec Products) or TissueLyser (Qiagen). After homogenization, tissues were centrifuged (5 min, 16,000 × g, 4°C) to pellet the debris. For liver and small intestine, 200 μl of tissue homogenate was homogenized for an additional minute. RNA was isolated from tissues using the RNeasy minikit (Qiagen), while RNA from serum was isolated using the QIAmp viral RNA minikit (Qiagen). After elution, RNA was snap frozen in liquid N2 and stored at −80°C.
Quantitative RT-PCR.
Quantitative real-time RT-PCR was performed according to a published protocol (19), using a MyiQ single-color real-time PCR detection system (Bio-Rad) with a one-step quantitative RT (qRT)-PCR kit (Quanta Biosciences). To generate the DENV2 standard curve, serial dilutions of a known concentration of DENV2 genomic RNA were transcribed in vitro (MAXIscript kit; Ambion) from a plasmid containing the cDNA template of the S221 3′ untranslated region (UTR). After transcription, DNA was digested with DNase I, and RNA was purified using the RNeasy minikit (Qiagen) and then quantified by spectrophotometry. To control for RNA quality and quantity in tissues, the level of 18S rRNA was measured as described previously (12) in parallel real-time RT-PCRs. A relative 18S standard curve was made from serial dilutions of total splenic RNA.
Immunohistochemistry.
Spleens were embedded in O.C.T. compound (Sakura). Sections (6 μm) were cut and stored at −80°C. Frozen sections were thawed and fixed for 10 min in acetone at room temperature, followed by 8 min in 1% paraformaldehyde in 100 mM dibasic sodium phosphate containing 60 mM lysine and 7 mM sodium periodate at pH 7.4 on ice. Sections were blocked with 1% bovine serum albumin (BSA) (Sigma) and 5% normal goat serum (Caltag Laboratories) in PBS. Sections were stained overnight with purified rabbit polyclonal anti-DENV NS3 (a generous gift from the Novartis Institute for Tropical Diseases, Singapore) and, for brain sections, with phycoerythrin (PE) anti-CD8β (clone YTS156.7.7; BioLegend). After washing, the sections were stained with DyLight 649-labeled goat anti-rabbit IgG (Jackson ImmunoResearch). Images were recorded using a Marianas deconvolution fluorescence microscope (3i) and adjusted and stitched together using Fiji before final preparation in Adobe Photoshop.
T cell depletions.
LTF2 (IgG2b isotype control antibody) and 2.43 (IgG2b anti-mouse CD8) antibodies (Bio-XCell) were administered intraperitoneally in 200 μl of PBS. A129 mice were given 500 μg of antibody 5, 4, and 3 days before infection. On the day of infection, mice received 5 × 108 GE of strain S221 intravenously (i.v.) and another 500 μg or 1 mg of antibody intraperitoneally (i.p.). Mice were given the same dose of antibody every 3 days as maintenance. As assessed by flow cytometry, this protocol depleted ≥95% of their CD8+ T cells.
Intracranial IFN-γ blockade.
Mice intravenously inoculated with strain S221, as described above, were injected intracranially with 100 μg of the IFN-γ neutralizing monoclonal antibody XMG1.2 or isotype control (Bio-XCell) in 30 μl of PBS 4, 6, and 8 days after infection. Brains were harvested 10 days after infection and processed to quantitate 18S and DENV RNA levels as described above.
T cell adoptive transfers.
Donor spleens and inguinal and brachial lymph nodes were collected from A129 mice 6 days after intravenous inoculation with 5 × 108 GE of strain S221. Tissues were homogenized through 70-μm strainers, and CD8+ T cells were isolated using the CD8α+ T cell isolation kit II (Miltenyi) for untouched isolation. Cells were enriched to 90% purity as determined by flow cytometry, and 3 × 107 cells were administered intravenously into recipient A129 and AG129 mice. Recipients were immediately infected intracranially with 5 × 108 GE of strain S221. Three days later, brains were collected and 18S and DENV RNA levels were quantitated as described above.
Isolation of splenocytes for fluorescence-activated cell sorting.
Blood was collected by cardiac puncture, and spleens were homogenized through a 70-μm strainer (BD Biosciences). Red blood cells were lysed with red blood cell (RBC) lysis buffer (eBioscience). Lymphocytes from the brain and spinal cord were isolated using a previously described protocol (9). Brain and spinal cord samples were first homogenized through a 40-μm strainer (BD Biosciences) and then layered onto a Percoll gradient and centrifuged (20 min, 500 × g, 22°C). For intracellular DENV antigen staining, spleens were collected into RPMI medium (Gibco) containing 10% fetal calf serum (Gemini Bio-Products) and stored on ice. Tissues were minced and digested for 20 min at 37°C with agitation in RPMI medium containing 10% fetal calf serum and 1.5 mg/ml collagenase VIII (Sigma) in approximately 5 ml. Tissues were immediately washed in RPMI medium, and digests were collected via centrifugation. Resuspended tissues were pressed through 70-μm strainers (BD) using the plungers of 3-ml syringes (BD). Liberated cells were collected and pelleted by centrifugation. Cells were resuspended in a 14.7% OptiPrep (Sigma) solution diluted in 150 mM NaCl with 10 mM HEPES at pH 7.4 and layered over 22.2% OptiPrep solution diluted in the same buffer. Cells were spun for 20 min at 750 × g at 25°C, washed immediately afterward with RPMI medium, and plated in 96-well plates.
Flow cytometry assays.
For intracellular cytokine staining, cells were stimulated in 96-well U-bottom plates for 5 h with 1 μg/ml of the H-2b-restricted epitopes M60–67 or NS4B99–107, which were identified previously (50), in the presence of brefeldin A (GolgiPlug; BD Biosciences). The cells were washed and the Fc receptors were blocked by incubating cells with supernatant from 2.4G2-producing hybridoma cells. The cells were then stained with eFluor 450 anti-CD4, PerCP-eFluor 710 anti-CD8α, or PerCP-eFluor 710 rat IgG2aκ and Alexa Fluor 488 anti-CD3ε (eBioscience). The cells were subsequently fixed and permeabilized using the BD Cytofix/Cytoperm kit and stained with allophycocyanin (APC) anti-IFN-γ (eBioscience).
For DENV antigen staining, FcγRs were blocked with 1 μg of monoclonal antibody (MAb) 2.4G2, which binds to CD16/32. The cells were stained with several antibodies, including APC-eFluor 780 anti-Gr-1 (Pharmingen) and PE anti-F4/80 (BioLegend), or appropriately labeled isotype controls. The cells were fixed and permeabilized using the Cytofix/Cytoperm kit (BD). For intracellular staining, all steps were performed in 1× BD Perm/Wash buffer. Cells were blocked briefly and stained for 30 min with biotinylated 2H2, which binds to DENV (prM/M) protein, or the isotype control antibody. After washing, the cells were stained with APC-streptavidin (BioLegend). The gate for DENV antigen-positive cells was set at 1% of the isotype control staining. All flow cytometry data were collected using an LSRII (BD Biosciences) and analyzed using FlowJo software (Tree Star).
Measurement of IFN-γ.
Tissues were harvested into 10% FBS/PBS containing a protease inhibitor cocktail (Calbiochem) and homogenized for 3 min using a TissueLyser (Qiagen). Samples were centrifuged (4 min, 16,000 × g, 4°C) to pellet the debris, and IFN-γ in the supernatants was measured using the mouse IFN-γ enzyme-linked immunosorbent assay (ELISA) Ready-SET-Go! kit (eBioscience).
Statistical analyses and regression analysis of survival data.
Data were analyzed with Prism 5.0 (GraphPad). Statistical significance was determined using the unpaired t test with Welch's correction with the exception of analysis of the IFN-γ ELISA data, which were analyzed using the Kruskal-Wallis one-way analysis of variance (ANOVA) test followed by Dunn's multiple comparison test. For analyses of the survival data, linear regression was performed on the log-transformed viral dosages versus survival percentage in Prism 5.0 (GraphPad). The statistically significant linear regression line equations were used to calculate 50% lethal doses (LD50s).
RESULTS
AG129 mice are 140-fold more susceptible to DENV-induced lethal disease than A129 mice.
To assess the relative susceptibility of A129 and AG129 mice to DENV-induced acute systemic disease, mice were inoculated intravenously with various doses of the mouse-passaged DENV2 strain S221. A129 mice were administered strain S221 at 1 × 1011, 2 × 1011, 5 × 1011, 1 × 1012, or 2 × 1012 genomic equivalents (GE), and AG129 mice were administered strain S221 at 1 × 109, 2 × 109, 5 × 109, 1 × 1010, or 2 × 1010 GE. Following infection, the mice were monitored one to three times each day for signs of disease. The results of three independent survival experiments are shown in Fig. 1A. Between 2 and 6 days after infection, all A129 and AG129 mice developed systemic disease characterized by ruffled fur, hunched posture, and lethargy, as previously reported in AG129 mice (5, 35, 40, 51). Depending on the viral dose, various numbers of mice died with systemic disease signs between 4 and 8 days after infection, as indicated by the white area of the survival curves in Fig. 1A.
Fig 1.
AG129 mice are 140-fold more susceptible than A129 mice to DENV-induced lethal systemic disease and develop lethal paralysis at low doses. (A) Survival of A129 mice infected with 1 × 1011, 2 × 1011, 5 × 1011, 1 × 1012, or 2 × 1012 GE of strain S221 administered i.v. (n = 4 to 8 mice per group) (left column) and survival of AG129 mice infected with 1 × 109, 2 × 109, 5 × 109, 1 × 1010, or 2 × 1010 GE of strain S221 i.v. (n = 4 to 7 mice per group) (right column). The dotted lines and gray areas in the survival curves represent the time frames during which lethal paralysis developed in the absence of signs of systemic disease. Results are pooled from 3 independent experiments. (B) Survival of AG129 mice infected with 5 × 104, 5 × 106, or 5 × 108 GE of strain S221 i.v. (n = 9 mice per group). The dotted lines and gray areas in the survival curves represent the time frames during which lethal paralysis developed in the absence of signs of systemic disease. Results are pooled from 2 independent experiments.
We also observed strain-specific disease traits. AG129 mice that survived systemic disease usually appeared healthy for 1 to 3 days before developing and succumbing to progressive paralysis by 12 days after infection (Fig. 1A, gray area). In contrast, nearly all the A129 mice showed no signs of paralysis throughout the experiment. In less than 20% of the A129 mice, mild impairment of hind-limb movement was observed in those suffering from systemic disease. Signs of systemic disease always preceded death of the A129 mice, and all A129 mice that survived through day 8 recovered completely (including those mice that exhibited mild impairment of hind-limb movement). The LD50 for systemic disease was calculated to be 3.7E11 GE of strain S221 in A129 mice and 2.7E9 GE of strain S221 in AG129 mice (mortality data in the white area of the survival curves in Fig. 1) based on the regression analysis of survival percentages versus the log value of viral dose (data not shown). Lethal systemic disease was dependent on viral dose, as indicated by the statistically significant direct correlation (P = 0.023 for A129, P = 0.009 for AG129). These experiments show that A129 mice are approximately 140-fold more resistant to systemic dengue-mediated lethality than are AG129 mice, quantifying the protective effect of IFN-γR activity in vivo. Additionally, functional IFN-γR is sufficient to protect A129 mice from paralysis.
DENV-induced paralysis in AG129 mice is largely independent of viral dose.
To determine if a correlation exists between virus dose and lethal paralysis, age- and sex-matched AG129 mice were intravenously administered 5 × 104, 5 × 106, or 5 × 108 GE of strain S221 (doses below the threshold for inducing lethal systemic disease), and their survival was monitored (Fig. 1B). All mice that eventually developed paralysis showed inhibited movement of the hind limbs that progressed to total hind-limb paralysis within 5 days. Mice succumbed to paralytic disease between 16 and 24 days after infection, and there were no significant differences in survival time between the doses. In fact, when comparing the highest dose (5 × 108 GE) to the lowest dose (5 × 104 GE), a 10,000-fold difference, lethal paralysis developed at approximately the same time (between 16 and 24 days after infection in all mice). The occurrence of lethal paralysis was independent of viral dose in this range, as indicated by the approximately horizontal linear regression curve and the lack of statistical significance (data not shown; P = 0.667). Of the 27 total mice used, 3 survived the 30-day experiment without manifesting paralysis. Two of these mice were administered a dose of 5 × 106 GE, and one was administered 5 × 108 GE. Thus, although lethal systemic dengue was highly dose dependent, both the severity and time to onset of paralysis were independent of viral dose in the AG129 mice infected with doses below what is required to induce lethal systemic disease. The timelines for manifestation of DENV disease signs in A129 and AG129 mice at high doses (≫LD50), at the LD50, and at low doses (≪LD50) are summarized in Fig. 2.
Fig 2.
Summary of signs of disease in A129 and AG129 mice at various DENV doses. The disease phenotypes following infection with high viral doses (≫LD50s), the approximate LD50, and low viral doses (≪LD50s). Listed on the left are the signs of disease. The bars on the right indicate the relative incidence of the corresponding sign of disease at that time point after infection. Black bars represent most mice (>50%), dark-gray bars represent some mice (20 to 50%), and light-gray bars represent few mice (<20%) experiencing the signs of disease indicated during the time intervals specified by the length of the bars.
IFN-γR signaling restricts DENV replication in the spleen and bone marrow within 24 h of infection.
Having quantified the effect of IFN-γR signaling in resistance against lethal systemic dengue, we next assessed the effect of this pathway on viral replication. A129 and AG129 mice were inoculated with 5 × 108 GE of strain S221, the highest dose that did not induce lethal systemic disease in AG129 mice. The levels of viral RNA in the serum, kidney, heart, spleen, bone marrow, lungs, liver, brain, spinal cord, mesenteric lymph node, small intestine, and skin were measured 1, 2, 4, and 6 days after infection. The tissues were homogenized, RNA was isolated, and both viral RNA and host 18S rRNA were quantified by qRT-PCR.
At 12 h after infection, the levels of viral RNA in the spleen, serum, and bone marrow were equivalent (data not shown). However, by 24 h after infection, viral RNA levels were 5-fold higher in the serum, spleen, and bone marrow of AG129 relative to A129 mice (Fig. 3A). At this early time point, there were no other differences in the levels of viral RNA between the two mouse strains except in the lungs, where the levels were 14-fold higher in AG129 mice than A129 mice. By 48 h after infection, viral RNA levels were 7-, 11-, and 41-fold higher in the serum, spleen, and bone marrow, respectively, of AG129 relative to A129 mice (Fig. 3A). These results support a role for the IFN-γR pathway in inhibiting DENV replication in the spleen and bone marrow early after infection.
Fig 3.
IFN-γR signaling restricts DENV replication in the spleen and bone marrow within 24 h of infection. (A) Viral RNA levels in the serum, spleen, bone marrow, and mesenteric lymph nodes (MLN) were quantified by qRT-PCR 1, 2, 4, and 6 days after infection (5 × 108 GE of strain S221 i.v. on day 0) of A129 (black squares) and AG129 (white squares) mice. Symbols represent means ± standard errors of the mean (SEM) (n = 5). Results are representative of data from 2 independent experiments. P values from two-tailed unpaired t test with Welch's correction (95% confidence interval [CI]): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001; error bars represent the SEM, and n is the number of mice per group. Dashed lines denote limits of detection. (B) Representative immunohistochemical staining of spleen sections 12, 24, 48, and 72 h after infection of A129 or AG129 mice (5 × 108 GE of strain S221 i.v. on day 0). Sections were stained for DENV NS3 (white) (120 to 170 low-magnification images were stitched together into one image). Results are representative of data from more than 3 independent experiments. (C) Representative FACS staining of splenocytes isolated from A129 or AG129 mice 48 after infection (5 × 108 GE of strain S221 i.v.). Cells were gated based on absent or low expression of Gr-1 and high expression of F4/80 (shown on the left). DENV expression (stained with clone 2H2, anti-DENV prM/M protein) in the Gr-1negative or low F4/80high population is shown on the right. Results are representative of data from 3 independent experiments. FSC, forward scatter; SSC, side scatter.
To assess viral infection in the spleen in greater detail, fluorescent immunohistochemistry (FIHC) was carried out on frozen tissue sections by staining them with rabbit polyclonal antibodies raised against purified DENV nonstructural protein 3 (NS3), which is expressed at high levels only at sites of viral replication. For comparison between the AG129 and A129 mice, images of spleen sections were stitched together to visualize the whole section (Fig. 3B). At 12 h postinfection, NS3 was detected in the marginal zone of the spleen as defined rings surrounding the white pulp and appeared at equivalent frequencies and intensities in the AG129 and A129 mice. By 24 h, DENV replication had extended toward the red pulp, with a similar amount of NS3 detected in the two strains (Fig. 3B). At 48 h postinfection, the frequency of NS3+ cells was clearly higher in the AG129 mice than in the A129 mice, although NS3 expression was observed throughout the red pulp in both mouse strains (Fig. 3B). In order to quantify the infected cells, splenocytes from the A129 and AG129 mice were isolated 48 h after infection and stained with antibodies against Gr-1, F4/80, and DENV premembrane/membrane protein (prM/M) (stained with biotinylated clone 2H2, anti-DENV prM/M protein) and analyzed by flow cytometry. The AG129 mice had greater than 3-fold more prM/Mpositive Gr-1negative or low F4/80high cells than the A129 mice (Fig. 3C, subgating shown on the left and DENV antigen staining shown on the right), corroborating the difference observed by immunohistochemistry at this time point. Finally, by 72 h, viral replication had diminished in both mice, and NS3 was detectable only at low levels in the red pulp around the outer rim of the spleen of the AG129 and A129 mice (Fig. 3B). Collectively, these data suggest that IFN-γR-dependent signaling restricts DENV replication in the spleen by limiting the number of infected cells.
IFN-γR signaling reduces systemic levels of DENV by day 4 after infection.
The levels of viral RNA in all tissues increased between 1 and 2 days after infection in both AG129 and A129 mice (Fig. 3A, 4A, and 5A). However, on day 2 after infection, viral RNA levels increased more in the AG129 than in the A129 mice, becoming 6- to 120-fold higher in the serum, spleen, bone marrow, liver, skin, spinal cord, and brain. Between 2 and 4 days after infection in AG129 mice, the levels of viral RNA increased substantially in all tissues except the spleen, bone marrow, lymph nodes, and serum (Fig. 3A, 4A, and 5A). During this time in the A129 mice, however, the levels of viral RNA in all tissues decreased or changed only slightly, except in the skin (Fig. 3A, 4A, and 5A). As a result, by day 4 after infection, viral RNA levels were approximately 20- to 3,000-fold higher in tissues of AG129 mice compared to A129 mice, indicating that IFN-γR signaling controls the systemic viral load.
Fig 4.
IFN-γR-dependent signaling reduces systemic levels of DENV by day 4 after infection. (A) Viral RNA levels in the skin, kidneys, small intestine, lungs, heart, and liver were quantified by qRT-PCR 1, 2, 4, and 6 days after infection (5 × 108 GE of strain S221 i.v. on day 0) of A129 (black squares) and AG129 (white squares) mice. Symbols represent means ± SEM (n = 5). Results are representative of 2 independent experiments. P values from two-tailed unpaired t test with Welch's correction (95% CI): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001; error bars represent SEM, and n is the number of mice per group. Dashed lines denote limits of detection. (B) Detection of IFN-γ in serum or homogenates of the spleen, brain, and spinal cord by ELISA. Tissues were obtained from naïve A129 mice at 2, 4, and 6 days after infection (5 × 108 GE of strain S221 i.v. on day 0). Bars represent means ± SEM (n = 4). Results are representative of data from 2 independent experiments. P values from the Kruskal-Wallis one-way ANOVA test followed by Dunn's multiple comparison test (95% CI): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001; error bars represent SEM, and n is the number of mice per group. ND indicates that IFN-γ was not detected.
Fig 5.
DENV-specific IFN-γ+ CD8+ T cells infiltrate the CNS of A129 and AG129 mice. (A) Viral RNA levels in the spinal cord and brain were quantified by qRT-PCR 1, 2, 4, and 6 days after infection (5 × 108 GE of strain S221 i.v. on day 0) of A129 (black squares) and AG129 (white squares) mice. Symbols represent means ± SEM (n = 5). Results are representative of data from 2 independent experiments. P values from two-tailed unpaired t test with Welch's correction (95% CI): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001; error bars represent SEM, and n is the number of mice per group. Dashed lines denote limits of detection. (B) Representative immunohistochemical staining of brain sections 6 days after infection of A129 mice (5 × 108 GE of strain S221). Sections were stained for CD8 (upper panel on left, red on right) and DENV NS3 (lower panel on left, green on right). (C, left) Representative staining of CD8+ cells isolated from blood or spleens of A129 mice before infection (naïve) or 2, 4, and 6 days after infection (5 × 108 GE S221) or AG129 mice 6 days after infection (5 × 108 GE of strain S221). Cells were stimulated with the DENV epitope M60–67 and stained for the presence of intracellular IFN-γ. Results are representative of data from 2 independent experiments. (C, right) Representative staining of CD8+ cells isolated from brains or spinal cords of A129 mice before infection (naïve) or 6 days after infection (5 × 108 GE of strain S221) or AG129 mice 6 days after infection (5 × 108 GE of strain S221). Cells were stimulated with the DENV epitopes M60–67 and stained for the presence of intracellular IFN-γ. Results are representative of data from 2 independent experiments.
IFN-γ levels are elevated 2 days after infection and remain elevated in the serum until 4 days after infection.
To further investigate the control of viral replication by IFN-γR signaling, we measured IFN-γ levels in the serum and tissue homogenates from the spleen, brain, and spinal cord of A129 mice (Fig. 4B). IFN-γ levels in the serum and spleen were most elevated at 2 and 4 days after infection, correlating with the time at which major differences in systemic viral levels became evident between the A129 and AG129 mice. The serum IFN-γ concentration was elevated at days 2 and 4, while spleen IFN-γ content decreased between days 2 and 4. In the brain and spinal cord, the levels of IFN-γ were similar in naïve and infected mice. These data suggest that the spleen is an initial and major site of IFN-γ production in this mouse model of DENV infection.
IFN-γR signaling mediates control of DENV replication in the CNS.
The results shown in Fig. 3A and 4A indicate that the rate of viral clearance in extraneural tissues was similar in the A129 and AG129 mice between days 4 and 6 postinfection. However, this was not the case for the spinal cord and brain, where infection in the AG129 mice, but not the A129 mice, continued to increase (Fig. 5A). At day 6 after infection, viral RNA was 100,000-fold higher in the spinal cord and 900-fold higher in the brain of the AG129 mice than in the A129 mice, demonstrating the late involvement of the IFN-γR signaling in mediating DENV clearance from the CNS. Taken together, the results thus far demonstrate that the IFN-γR pathway acts early during infection to help limit systemic DENV replication and again at later times to clear infection from the CNS.
CD8+ T cells are critical for clearance of DENV from the CNS and prevention of paralysis in A129 mice.
We previously reported that DENV-specific CD8+ T cells are critical for the clearance of DENV2 strain S221 from mice lacking IFN-α/βR (50). Immunohistochemistry showed focal CD8+ infiltrates near DENV NS3-expressing cells in brain tissue sections at this time point (Fig. 5B). Using one of the epitopes identified previously, we tracked the DENV2-specific CD8+ T cell response in the spleen and blood of the A129 mice during the first 6 days of infection or AG129 mice day 6 after infection (Fig. 5C, left). The DENV-specific CD8+ T cell response was first detected in the spleen and blood on day 4 after infection, and the responses were comparable in magnitude at day 6 in the A129 and the AG129 mice. In contrast, few or no CD8+ T cells were detected in the brain and spinal cord 4 days after infection (data not shown), while substantial numbers of DENV-specific CD8+ T cells were apparent in the CNS of A129 and AG129 mice by 6 days after infection (Fig. 5C, right).
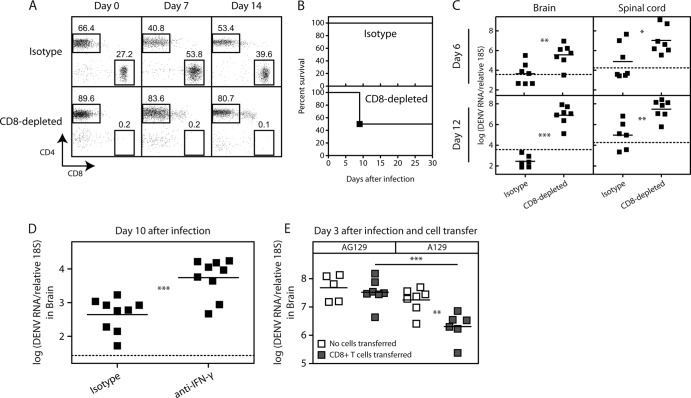
To assess the contribution of CD8+ T cells to defense against DENV, depleting antibodies were administered to A129 mice. The efficacy of depletions was monitored by FACS of blood cells on days 0, 7, and 14 after DENV infection (Fig. 6A). Half of the A129 mice depleted of CD8+ T cells developed paralysis, while none of the A129 mice that were administered the isotype control antibody developed paralysis (Fig. 6B). Depletion of CD8+ T cells from the A129 mice resulted in 80- and 140-fold increases in levels of virus in the brain and spinal cord, respectively, relative to the isotype control antibody-treated A129 mice on day 6 after infection (Fig. 6C). This effect was even more pronounced day 12 after infection, at which time virus levels were 28,000- and 310-fold higher in the brain and spinal cord, respectively, in the CD8-depleted mice.
Fig 6.
CD8+ T cells use IFN-γ to clear DENV infection from the CNS of A129 mice. (A) Representative staining of CD3+ populations in the blood of A129 mice before infection (day 0) or day 7 or 14 after infection (5 × 108 GE of strain S221), stained for CD4 and CD8 to assess efficacy of antibody-mediated CD8+ T cell depletion in mice administered anti-CD8 or isotype control antibodies (n = 5 mice per group). Results are representative of data from 2 independent experiments. (B) Survival of A129 mice infected with 5 × 108 GE of strain S221 i.v. and treated with isotype control or CD8-depleting antibody (n = 6 mice per group). Results are pooled from 2 independent experiments. (C) Viral RNA levels in the spinal cord and brain were quantified by qRT-PCR 6 or 12 days after infection of A129 mice (5 × 108 GE of strain S221 i.v.) that were treated with isotype control or CD8-depleting antibody. Symbols represent individual mice. Results are representative of data from 2 independent experiments. P values from two-tailed unpaired t test with Welch's correction (95% CI): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001. Dashed lines denote limits of detection. (D) Viral RNA levels in the brain were quantified by qRT-PCR 10 days after infection of A129 mice (5 × 108 GE of strain S221 i.v.) that were intracranially administered isotype control or IFN-γ-blocking antibody on days 4, 6, and 8. Symbols represent individual mice. Results are pooled from 2 independent experiments. P values from two-tailed unpaired t test with Welch's correction (95% CI): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001. The dashed line denotes limit of detection. (E) Viral RNA levels in the brain were quantified by qRT-PCR 3 days after intracranial infection (5 × 108 GE of strain S221 intracranially) of A129 or AG129 mice that were intravenously administered either CD8+ T cells isolated from DENV-infected A129 mice on day 6 after infection (gray squares) or no cells (white squares). Symbols represent individual mice. Results are representative of 2 independent experiments. P values from two-tailed unpaired t test with Welch's correction (95% CI): * P is ≤0.05, ** P is ≤0.01, and *** P is ≤0.001.
To assess the role of IFN-γ on DENV clearance from the CNS of A129 mice, IFN-γ in the brain was blocked by intracranially injecting 100 μg of the monoclonal antibody XMG1.2, which neutralizes IFN-γ, or isotype control 4, 6, and 8 days after intravenous inoculation with 5 × 108 GE of strain S221. Brains harvested 10 days after infection were found to contain 12-fold more viral RNA when the mice were treated with IFN-γ-blocking antibody relative to the isotype control (Fig. 6D).
To confirm the importance of IFN-γ produced by CD8+ T cells in mediating DENV clearance from the CNS, we sought an experimental setup where equivalent levels of DENV replication occurred in the CNS of A129 and AG129 mice. We found that for at least 3 days following intracranial inoculation, levels of DENV in the brain were equivalent in the A129 and AG129 mice. Using this system, we adoptively transferred 3 × 107 CD8+ T cells from A129 mice taken 6 days after intravenous infection with 5 × 108 GE of strain S221. Recipient mice were administered CD8+ T cells intravenously and then immediately inoculated intracranially with 5 × 108 GE of strain S221. Three days later, brains were harvested, and viral RNA levels in the brain were quantified (Fig. 6E). On average, the A129 mice that received CD8+ T cells had 9-fold less DENV RNA than the A129 control mice that did not receive T cells, whereas the AG129 mice that received CD8+ T cells had statistically equivalent levels relative to the AG129 mice that did not receive T cells. Collectively, these results demonstrate an important role for CD8+ T cells and IFN-γR signaling in mediating DENV clearance from the CNS.
DISCUSSION
We have investigated the roles of IFN-γR signaling in preventing two forms of DENV-induced disease in mice: systemic disease, which occurs early after infection and is associated with vascular leakage, and paralysis, which occurs as a later consequence of infection. Our data demonstrate that IFN-γR-dependent protection from systemic disease and paralysis, respectively, is associated with a reduction in systemic and CNS levels of DENV replication. Intravenous transfer of CD8+ T cells from DENV-infected A129 mice was sufficient to reduce the levels of DENV in the brain of intracerebrally infected A129 mice but not AG129 mice. Although these results suggest that CD8+ T cells prevent paralysis in A129 mice by clearing DENV infection from the CNS in an IFN-γR-dependent manner, this remains to be causally demonstrated due to technical limitations. Overall, these results contribute to our understanding of the role of the host immune system in determining the outcome of DENV infection.
We previously reported that unlike A129, G129, and wild-type mice, AG129 mice are highly susceptible to DENV2 isolate PL046-induced paralysis when administered doses above 105 PFU (39). In our previous studies, high levels of DENV were found in the spleen and lymph nodes 3 days after infection and in the brain and spinal cord 7 days after infection in AG129 mice, and low levels of DENV were found to be systemically present in both AG129 and A129 mice 3 days after infection. The present study expands these data by more precisely comparing the kinetics of DENV replication by qRT-PCR and FIHC in AG129 and A129 mice (40). The combination of using a different virus strain (S221, a triple-plaque-purified clone of D2S10, which was derived from PL046 by serial passage through AG129 mice [35, 51]), and new assays for detecting viral replication in the present study allowed (i) quantification of differences in susceptibility of A129 and AG129 mice to DHF/DSS-like disease, (ii) assessment of the tissue-specific restriction of viral replication by IFN-γR signaling throughout the time course of infection, and (iii) assessment of the importance of IFN-γR signaling and CD8+ T cells in the clearance of DENV from the CNS.
The analysis of viral RNA kinetics in tissues revealed that early after infection, the mice with functional IFN-γR had reduced levels of DENV only in the spleen, bone marrow, and serum relative to those in AG129 mice. The reduction of DENV replication observed in the spleen and bone marrow likely accounts for the lower levels of virus in the serum starting at day 2 after infection, since less DENV is released from infected cells into the bloodstream. Levels of DENV RNA in most tissues of the A129 mice did not significantly change between 2 and 4 days after infection, with the exception of the skin, in which the levels of virus increased greatly. This observation is interesting considering the skin is an important site of early DENV replication in humans (27, 47). Overall, these data demonstrate that IFN-γR activity causes decreased systemic levels of virus, which is likely a result of reducing early viral replication in the spleen and bone marrow and then maintaining an antiviral state to limit DENV dissemination and further systemic replication. This direct antiviral effect of IFN-γ against encephalitic flaviviruses has been described for extraneural tissues of mice infected with WNV (42), as well as in the serum and spleen of mice infected with Murray Valley encephalitis virus (29) and against the nonencephalitic flavivirus YFV (26, 31). In both the A129 and AG129 mice, DENV was cleared between days 4 and 6 postinfection at approximately the same rate in all tissues examined, with the exception of the CNS. This suggests that extraneural clearance is independent of IFN-γR, although it is dependent on CD8+ T cells (48, 50). However, A129 mice, but not AG129 mice, clear DENV from the brain in an IFN-γR-dependent manner. Taken together, these data demonstrate that IFN-γR plays a role in restricting DENV replication in extraneural tissues and in clearing DENV infection from the CNS but not extraneural tissues.
Recovery from viral encephalomyelitis with preservation of CNS function requires noncytolytic clearance of infected neurons rather than direct killing, as the regenerative capacity of CNS neurons is limited. Accordingly, Binder and Griffin observed that CD8+ T cells cleared Sindbis virus, an alphavirus, from specific sites within the CNS via IFN-γ-dependent activation of an antiviral state in infected neurons (7). Similarly, our data imply that T cell-mediated IFN-γ-dependent activation, rather than T cell-mediated cytotoxicity, seems to contribute to DENV clearance from the CNS. However, with a virulent lineage I strain of WNV, IFN-γ-deficient, but not perforin-deficient, CD8+ T cells efficiently clear infection from the CNS of mice (41). Perforin-dependent cytotoxic activity may be protective due to the urgent need to limit replication before the accumulation of WNV in the CNS. Thus, it is possible that, under certain conditions, DENV-specific CD8+ T cells may also use cytotoxic mechanisms to control CNS infection.
The low incidence of paralysis reported in human DENV cases calls into question the relevance of dengue mouse models that often exhibit paralysis, such as those using DENV strains New Guinea C, 16681, PL046, the mouse serum-passaged PL046 derivative D2S10, and a mouse brain-passaged derivative of P23085; all of these viral strains replicate in the mouse CNS, and some of them cause systemic manifestations depending on the parameters of infection and mouse genotype (4, 8, 10, 14, 22, 28, 40). The results of our study, as well as those of others, may help explain the propensity of these viruses to cause paralysis in mice. Perhaps DENV's extreme susceptibility to the murine type I IFN-signaling pathway (33, 34), the molecules of which differ sufficiently from human analogues to prevent DENV-mediated inhibition (3), limits extraneural antigen availability and results in a blunted cellular immune response. Accordingly, we have observed that the breadth and magnitude of DENV-specific T cell responses in wild-type mice are lower than in IFN-α/β receptor-deficient mice (45, 48, 50). Combined with the immune-privileged status of the CNS and the capacity of DENV for infection of the CNS, a blunted T cell response may favor efficient DENV replication in the CNS.
In summary, IFN-γR signaling plays a critical role in the host defense against DENV at two distinct phases: early in limiting systemic DENV replication and dissemination, which protects against systemic DHF/DSS-like disease, and late in clearing infection from the CNS, which is associated with paralysis.
ACKNOWLEDGMENTS
We thank Chris Benedict and Stuart T. Perry at the LIAI for experimental advice. We also thank Olga Turovskaya, Sarala Joshi, and Satoshi Fukuyama for technical help.
The project described here was supported by NIH grants U01 AI082185 to S.S. and U54 AI057157 from Southeast Regional Center of Excellence for Emerging Infections and Biodefense to P. F. Sparling. We have no competing financial interests to declare.
Footnotes
Published ahead of print 12 September 2012
REFERENCES
- 1. An J, Zhou DS, Kawasaki K, Yasui K. 2003. The pathogenesis of spinal cord involvement in dengue virus infection. Virchows Arch. 442:472–481 [DOI] [PubMed] [Google Scholar]
- 2. Angibaud G, Luaute J, Laille M, Gaultier C. 2001. Brain involvement in dengue fever. J. Clin. Neurosci. 8:63–65 [DOI] [PubMed] [Google Scholar]
- 3. Ashour J, et al. 2010. Mouse STAT2 restricts early dengue virus replication. Cell Host Microbe 8:410–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Atrasheuskaya A, Petzelbauer P, Fredeking TM, Ignatyev G. 2003. Anti-TNF antibody treatment reduces mortality in experimental dengue virus infection. FEMS Immunol. Med. Microbiol. 35:33–42 [DOI] [PubMed] [Google Scholar]
- 5. Balsitis SJ, et al. 2010. Lethal antibody enhancement of dengue disease in mice is prevented by Fc modification. PLoS Pathog. 6:e1000790 doi:10.1371/journal.ppat.1000790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bhoopat L, et al. 1996. Immunohistochemical characterization of a new monoclonal antibody reactive with dengue virus-infected cells in frozen tissue using immunoperoxidase technique. Asian Pac. J. Allergy Immunol. 14:107–113 [PubMed] [Google Scholar]
- 7. Binder GK, Griffin DE. 2001. Interferon-gamma-mediated site-specific clearance of alphavirus from CNS neurons. Science 293:303–306 [DOI] [PubMed] [Google Scholar]
- 8. Butrapet S, et al. 2000. Attenuation markers of a candidate dengue type 2 vaccine virus, strain 16681 (PDK-53), are defined by mutations in the 5′ noncoding region and nonstructural proteins 1 and 3. J. Virol. 74:3011–3019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Campanella M, Sciorati C, Tarozzo G, Beltramo M. 2002. Flow cytometric analysis of inflammatory cells in ischemic rat brain. Stroke 33:586–592 [DOI] [PubMed] [Google Scholar]
- 10. Chen HC, et al. 2004. Lymphocyte activation and hepatic cellular infiltration in immunocompetent mice infected by dengue virus. J. Med. Virol. 73:419–431 [DOI] [PubMed] [Google Scholar]
- 11. Cook S, Holmes EC. 2006. A multigene analysis of the phylogenetic relationships among the flaviviruses (family: Flaviviridae) and the evolution of vector transmission. Arch. Virol. 151:309–325 [DOI] [PubMed] [Google Scholar]
- 12. Dinchuk JE, et al. 2000. Aspartyl beta-hydroxylase (Asph) and an evolutionarily conserved isoform of Asph missing the catalytic domain share exons with junctin. J. Biol. Chem. 275:39543–39554 [DOI] [PubMed] [Google Scholar]
- 13. Gaunt MW, et al. 2001. Phylogenetic relationships of flaviviruses correlate with their epidemiology, disease association and biogeography. J. Gen. Virol. 82:1867–1876 [DOI] [PubMed] [Google Scholar]
- 14. Gualano RC, Pryor MJ, Cauchi MR, Wright PJ, Davidson AD. 1998. Identification of a major determinant of mouse neurovirulence of dengue virus type 2 using stably cloned genomic-length cDNA. J. Gen. Virol. 79:437–446 [DOI] [PubMed] [Google Scholar]
- 15. Gubler DJ. 2002. Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol. 10:100–103 [DOI] [PubMed] [Google Scholar]
- 16. Gubler DJ, Kuno G, Waterman SH. 1983. Neurologic disorders associated with dengue infection, p 290–301 In Pang T, Pathmanatan R. (ed), Proceedings of the International Conference on Dengue/DHF University of Malaysia Press, Kuala Lumpur, Malaysia [Google Scholar]
- 17. Gubler DJ, Meltzer M. 1999. Impact of dengue/dengue hemorrhagic fever on the developing world. Adv. Virus Res. 53:35–70 [DOI] [PubMed] [Google Scholar]
- 18. Hotta S. 1952. Experimental studies on dengue. I. Isolation, identification and modification of the virus. J. Infect. Dis. 90:1–9 [DOI] [PubMed] [Google Scholar]
- 19. Houng HH, Hritz D, Kanesa-thasan N. 2000. Quantitative detection of dengue 2 virus using fluorogenic RT-PCR based on 3′-noncoding sequence. J. Virol. Methods 86:1–11 [DOI] [PubMed] [Google Scholar]
- 20. Hsieh MF, et al. 2006. Both CXCR3 and CXCL10/IFN-inducible protein 10 are required for resistance to primary infection by dengue virus. J. Immunol. 177:1855–1863 [DOI] [PubMed] [Google Scholar]
- 21. Jackson ST, et al. 2008. Dengue infection in patients presenting with neurological manifestations in a dengue endemic population. West Indian Med. J. 57:373–376 [PubMed] [Google Scholar]
- 22. Johnson AJ, Roehrig JT. 1999. New mouse model for dengue virus vaccine testing. J. Virol. 73:783–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kankirawatana P, et al. 2000. Dengue infection presenting with central nervous system manifestation. J. Child Neurol. 15:544–547 [DOI] [PubMed] [Google Scholar]
- 24. Kautner I, Robinson MJ, Kuhnle U. 1997. Dengue virus infection: epidemiology, pathogenesis, clinical presentation, diagnosis, and prevention. J. Pediatr. 131:516–524 [DOI] [PubMed] [Google Scholar]
- 25. Kumar R, et al. 2008. Dengue encephalopathy in children in Northern India: clinical features and comparison with non dengue. J. Neurol. Sci. 269:41–48 [DOI] [PubMed] [Google Scholar]
- 26. Lee E, Lobigs M. 2008. E protein domain III determinants of yellow fever virus 17D vaccine strain enhance binding to glycosaminoglycans, impede virus spread, and attenuate virulence. J. Virol. 82:6024–6033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Limon-Flores AY, et al. 2005. Dengue virus inoculation to human skin explants: an effective approach to assess in situ the early infection and the effects on cutaneous dendritic cells. Int. J. Exp. Pathol. 86:323–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lin YL, et al. 1998. Study of dengue virus infection in SCID mice engrafted with human K562 cells. J. Virol. 72:9729–9737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lobigs M, Mullbacher A, Wang Y, Pavy M, Lee E. 2003. Role of type I and type II interferon responses in recovery from infection with an encephalitic flavivirus. J. Gen. Virol. 84:567–572 [DOI] [PubMed] [Google Scholar]
- 30. Lum LC, Lam SK, Choy YS, George R, Harun F. 1996. Dengue encephalitis: a true entity? Am. J. Trop. Med. Hyg. 54:256–259 [DOI] [PubMed] [Google Scholar]
- 31. Meier KC, Gardner CL, Khoretonenko MV, Klimstra WB, Ryman KD. 2009. A mouse model for studying viscerotropic disease caused by yellow fever virus infection. PLoS Pathog. 5:e1000614 doi:10.1371/journal.ppat.1000614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Miagostovich MP, et al. 1997. Retrospective study on dengue fatal cases. Clin. Neuropathol. 16:204–208 [PubMed] [Google Scholar]
- 33. Perry ST, Buck MD, Lada SM, Schindler C, Shresta S. 2011. STAT2 mediates innate immunity to dengue virus in the absence of STAT1 via the type I interferon receptor. PLoS Pathog. 7:e1001297 doi:10.1371/journal.ppat.1001297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Perry ST, Prestwood TR, Lada SM, Benedict CA, Shresta S. 2009. Cardif-mediated signaling controls the initial innate response to dengue virus in vivo. J. Virol. 83:8276–8281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prestwood TR, Prigozhin DM, Sharar KL, Zellweger RM, Shresta S. 2008. A mouse-passaged dengue virus strain with reduced affinity for heparan sulfate causes severe disease in mice by establishing increased systemic viral loads. J. Virol. 82:8411–8421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Qiu FX, Gubler DJ, Liu JC, Chen QQ. 1993. Dengue in China: a clinical review. Bull. World Health Organ. 71:349–359 [PMC free article] [PubMed] [Google Scholar]
- 37. Ramos C, et al. 1998. Dengue virus in the brain of a fatal case of hemorrhagic dengue fever. J. Neurovirol. 4:465–468 [DOI] [PubMed] [Google Scholar]
- 38. Renganathan A, Ng WK, Tan C. 1996. Transverse myelitis in association with dengue infection. Neurol. J. Southeast Asia 1:61–63 [Google Scholar]
- 39. Shresta S, et al. 2004. Interferon-dependent immunity is essential for resistance to primary dengue virus infection in mice, whereas T- and B-cell-dependent immunity are less critical. J. Virol. 78:2701–2710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Shresta S, Sharar KL, Prigozhin DM, Beatty PR, Harris E. 2006. Murine model for dengue virus-induced lethal disease with increased vascular permeability. J. Virol. 80:10208–10217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shrestha B, Samuel MA, Diamond MS. 2006. CD8+ T cells require perforin to clear West Nile virus from infected neurons. J. Virol. 80:119–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shrestha B, et al. 2006. Gamma interferon plays a crucial early antiviral role in protection against West Nile virus infection. J. Virol. 80:5338–5348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Solomon T, et al. 2000. Neurological manifestations of dengue infection. Lancet 355:1053–1059 [DOI] [PubMed] [Google Scholar]
- 44. Thisyakorn U, Thisyakorn C, Limpitikul W, Nisalak A. 1999. Dengue infection with central nervous system manifestations. Southeast Asian J. Trop. Med. Public Health 30:504–506 [PubMed] [Google Scholar]
- 45. Weiskopf D, et al. 2011. Insights into HLA-restricted T cell responses in a novel mouse model of dengue virus infection point toward new implications for vaccine design. J. Immunol. 187:4268–4279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Whitehead SS, Blaney JE, Durbin AP, Murphy BR. 2007. Prospects for a dengue virus vaccine. Nat. Rev. Microbiol. 5:518–528 [DOI] [PubMed] [Google Scholar]
- 47. Wu SJ, et al. 2000. Human skin Langerhans cells are targets of dengue virus infection. Nat. Med. 6:816–820 [DOI] [PubMed] [Google Scholar]
- 48. Yauch LE, et al. 2010. CD4+ T cells are not required for the induction of dengue virus-specific CD8+ T cell or antibody responses but contribute to protection after vaccination. J. Immunol. 185:5405–5416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yauch LE, Shresta S. 2008. Mouse models of dengue virus infection and disease. Antiviral Res. 80:87–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yauch LE, et al. 2009. A protective role for dengue virus-specific CD8+ T cells. J. Immunol. 182:4865–4873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zellweger RM, Prestwood TR, Shresta S. 2010. Enhanced infection of liver sinusoidal endothelial cells in a mouse model of antibody-induced severe dengue disease. Cell Host Microbe 7:128–139 [DOI] [PMC free article] [PubMed] [Google Scholar]