To the Editor:
With great interest, we read the article by Dispenzieri et al1 in the June 2012 issue of Mayo Clinic Proceedings in which they reported their investigation of the association of polyclonal immunoglobulin free light chains (FLCs) and the mortality rate in a large population of normal persons. The authors concluded that nonclonal elevation of FLCs is a significant predictor of worse overall survival in persons without plasma cell disorders. The increased risk of death was independent of renal function, sex, and age but not restricted to any particular cause of death. As also discussed in the editorial that introduced this paper,2 normal immunoglobulin production is accompanied by an excess of FLC synthesis. Free light chains are secreted by plasma cells and can be found in body fluids such as blood, synovial and cerebrospinal fluid, urine, and saliva. Although FLCs have been considered spillover products of antibody synthesis, FLCs can also have diverse biological activities, including antiangiogenic, prothrombinase, proteolytic, and complement-activating activities.3
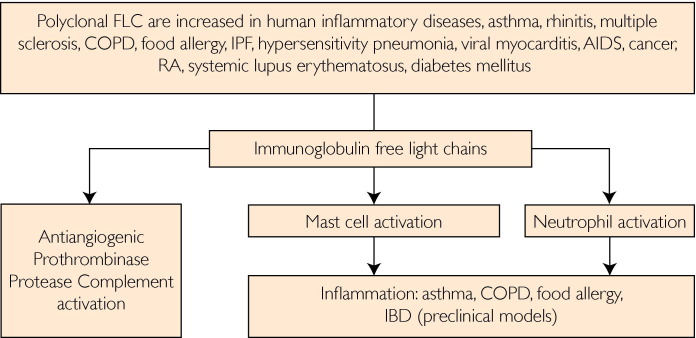
In addition, we have described that FLCs can trigger inflammation via activation of mast cells.4 Passive sensitization of mice with antigen-specific FLCs followed by antigen challenge induces an immediate hypersensitivity-type response.4 Mast cells may not be the sole cellular target for FLCs, because neutrophils and neural cells have also been found to respond to FLCs.5,6 In previous work, we showed that FLCs may play a crucial role in the pathogenesis of disease in preclinical models for asthma, inflammatory bowel disease, and food allergy.7-10 In extension to these studies, we found increased local or systemic FLC concentrations in patients with food allergy10 inflammatory bowel disease,8 rheumatoid arthritis,11 viral myocarditis,12 and upper and lower airway diseases such as rhinitis,13 asthma,7 idiopathic pulmonary fibrosis and hypersensitivity pneumonia,14 and chronic obstructive pulmonary disease (Figure).5 Therapeutic intervention with rituximab in patients with rheumatoid arthritis showed that decreases in FLCs correlate with a decrease in disease activity.11 Our studies suggest that FLCs may be responsible for an antigen-specific initiation and perpetuation of chronic inflammation.
FIGURE.
Immune disorders associated with increased immunoglobulin free light chains (FLC) and effector functions of immunoglobulin FLC leading inflammatory diseases via mast cell and neutrophil activation. COPD = chronic obstructive pulmonary disease; IBD = inflammatory bowel disease; IPF = idiopathic pulmonary fibrosis; RA = rheumatoid arthritis.
These findings may be of particular importance in relation to the study described by Dispenzieri et al.1 Increased FLCs could stimulate the progression of chronic inflammatory responses via the activation of specific immune cells. It would therefore be of interest in future studies to investigate whether polyclonal FLC concentrations may also be associated with specific markers of cellular activation. These data, including those from Mayo Clinic Proceedings,1 suggest that measurement of FLCs may not only be important to investigate aberrant FLCs leading to plasma cell disorders but may also give insight into ongoing inflammatory immune reactions.
References
- 1.Dispenzieri A., Katzmann J.A., Kyle R.A. Use of nonclonal serum immunoglobulin free light chains to predict overall survival in the general population. Mayo Clin Proc. 2012;87(6):517–523. doi: 10.1016/j.mayocp.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drayson M.T. Using single protein biomarkers to predict health and disease in diverse patient populations: a new role for assessment of immunoglobulin free light chains [editorial] Mayo Clin Proc. 2012;87(6):505–507. doi: 10.1016/j.mayocp.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thio M., Blokhuis B.R., Nijkamp F.P., Redegeld F.A. Free immunoglobulin light chains: a novel target in the therapy of inflammatory diseases. Trends Pharmacol Sci. 2008;29(4):170–174. doi: 10.1016/j.tips.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Redegeld F.A., van der Heijden M.W., Kool M. Immunoglobulin-free light chains elicit immediate hypersensitivity-like responses. Nat Med. 2002;8(7):694–701. doi: 10.1038/nm722. [DOI] [PubMed] [Google Scholar]
- 5.Braber S., Thio M., Blokhuis B.R. An association between neutrophils and immunoglobulin free light chains in the pathogenesis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(8):817–824. doi: 10.1164/rccm.201104-0761OC. [DOI] [PubMed] [Google Scholar]
- 6.Rijnierse A., Kroese A.B., Redegeld F.A. Immunoglobulin-free light chains mediate antigen-specific responses of murine dorsal root ganglion neurons. J Neuroimmunol. 2009;208(1-2):80–86. doi: 10.1016/j.jneuroim.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Kraneveld A.D., Kool M., van Houwelingen A.H. Elicitation of allergic asthma by immunoglobulin free light chains. Proc Natl Acad Sci U S A. 2005;102(5):1578–1583. doi: 10.1073/pnas.0406808102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rijnierse A., Redegeld F.A., Blokhuis B.R. Ig-free light chains play a crucial role in murine mast cell-dependent colitis and are associated with human inflammatory bowel diseases. J Immunol. 2010;185(1):653–659. doi: 10.4049/jimmunol.0901129. [DOI] [PubMed] [Google Scholar]
- 9.van Esch B.C., Schouten B., Blokhuis B.R. Depletion of CD4+CD25+ T cells switches the whey-allergic response from immunoglobulin E- to immunoglobulin free light chain-dependent. Clin Exp Allergy. 2010;40(9):1414–1421. doi: 10.1111/j.1365-2222.2010.03500.x. [DOI] [PubMed] [Google Scholar]
- 10.Schouten B., van Esch B.C., van Thuijl A.O. Contribution of IgE and immunoglobulin free light chain in the allergic reaction to cow's milk proteins. J Allergy Clin Immunol. 2010;125(6):1308–1314. doi: 10.1016/j.jaci.2010.02.039. [DOI] [PubMed] [Google Scholar]
- 11.Groot Kormelink T., Tekstra J., Thurlings R.M. Decrease in immunoglobulin free light chains in patients with rheumatoid arthritis upon rituximab (anti-CD20) treatment correlates with decrease in disease activity. Ann Rheum Dis. 2010;69(12):2137–2144. doi: 10.1136/ard.2009.126441. [DOI] [PubMed] [Google Scholar]
- 12.Matsumori A., Shimada M., Jie X., Higuchi H., Groot Kormelink T., Redegeld F.A. Effects of free immunoglobulin light chains on viral myocarditis. Circ Res. 2010;106(9):1533–1540. doi: 10.1161/CIRCRESAHA.110.218438. [DOI] [PubMed] [Google Scholar]
- 13.Powe D.G., Groot Kormelink T., Sisson M. Evidence for the involvement of free light chain immunoglobulins in allergic and nonallergic rhinitis. J Allergy Clin Immunol. 2010;125(1):139–145.e1-3. doi: 10.1016/j.jaci.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 14.Groot Kormelink T., Pardo A., Knipping K. Immunoglobulin free light chains are increased in hypersensitivity pneumonitis and idiopathic pulmonary fibrosis. PLoS One. 2011;6(9):e25392. doi: 10.1371/journal.pone.0025392. [DOI] [PMC free article] [PubMed] [Google Scholar]