Abstract
Context
Long-distance running (greater than 3000 m) is often recommended to maintain a healthy lifestyle. Running injury rates increase significantly when weekly mileage extends beyond 40 miles cumulatively. With the development of running analysis and other diagnostic tests, injuries to the leg secondary to bone, musculotendinous, and vascular causes can be diagnosed and successfully managed.
Evidence Acquisition
Searches used the terms running, injuries, lower extremity, leg, medial tibial stress syndrome, compartment syndrome, stress fractures, popliteal artery entrapment, gastrocnemius soleus tears, and Achilles tendinopathy. Sources included Medline, Google Scholar, and Ovid from 1970 through January 2012.
Results
Tibial stress fractures and medial tibial stress syndrome can sometimes be prevented and/or treated by correcting biomechanical abnormalities. Exertional compartment syndrome and popliteal artery entrapment syndrome are caused by anatomic abnormalities and are difficult to treat without surgical correction.
Conclusion
Leg pain due to bone, musculotendinous, and vascular causes is common among long-distance runners. Knowledge of the underlying biomechanical and/or anatomic abnormality is necessary to successfully treat these conditions.
Keywords: running, jogging, leg injuries
Long-distance running (greater than 3000 m) is frequently recommended to maintain a healthy lifestyle.121 Between 37% to 56% of recreational runners who steadily train and participate in a long-distance run periodically will sustain a running-related injury each year.136 A retrospective study of adolescent runners (13-18 years) demonstrated a lifetime prevalence of previous running injury (68% in girls and 59% in boys) with strong associations with higher mileage and faster performance.132 Known predictors of lower extremity injury include running greater than 40 miles per week and previous lower extremity injury.52,56,141 While training errors lead to the majority of running injuries, biomechanical factors, such as foot insufficiency, muscle weakness, genu varum, and high Q-angle, contribute to 40% of running injuries.79
A recent systematic review of the incidence of leg injuries among long-distance runners found that most injuries involve the knee (7.2%-50%), lower leg (9%-32.2%), foot (5.7%-39.3%), or thigh (3.4%-38.1%).135 The differential for leg pain is broad: skeletal (medial tibial stress syndrome, stress fractures), musculotendinous (tendinosis, myopathy), vascular (exertional compartment syndrome, venous thrombosis, popliteal artery entrapment syndrome, vascular claudication), neurologic (nerve entrapment, lumbosacral radiculopathy, neurogenic claudication), infectious, and neoplastic.144 In a study of over 2000 running-related injuries, the most common leg injuries were medial tibial stress syndrome (4.9%), Achilles tendinopathy (4.8%), tibial stress fractures (3.3%), and gastrocnemius/soleus strains/tears (1.3%).131
Many of the skeletal, musculotendinous, and vascular running ailments can be explained by anatomy and basic biomechanics. A recent Cochrane review found little evidence for the effectiveness of stretching and/or conditioning for the prevention of lower limb soft tissue running injuries.146 However, knee braces and custom insoles were effective for reducing anterior knee pain and medial tibial stress syndrome in runners, respectively.146 Overall, evidence for interventions reducing lower limb pain and injury after intense running was considered weak.146
In addition to standard physical examination and imaging techniques (Table 1), new tools (running studies) have emerged for the detection and treatment of these injuries. Gait retraining is currently being studied as a viable option for preventing tibial stress fractures and other running-related injuries.27,98
Table 1.
Common diagnostic testing findings.
| Diagnosis: Modality | Findings |
|---|---|
| Chronic exertional compartment syndrome | |
| Compartment pressure testing | Intracompartmental pressures: > 15 mm Hg before exercise, > 30 mm Hg 1 min after exercise, > 20 mm Hg 5 min after exercise |
| Tibial stress fractures | |
| Magnetic resonance imaging | Cortical thickening, periosteal reaction, or fracture line |
| Bone scan | Focal uptake on all 3 phases |
| Medial tibial stress syndrome | |
| Bone scan | Diffuse linear uptake within the distal 1/3 of the posteromedial tibia on delayed images |
| Popliteal artery entrapment syndrome | |
| Duplex ultrasound | Decrease in peak systolic flow through popliteal artery with resisted plantar flexion and knee flexed to 15° |
| Magnetic resonance imaging/angiography | Medial deviation and compression, thrombosis, and/or aneurysm of the popliteal artery with an associated muscle anomaly (hypertrophied muscle, aberrant fibrous band, abnormal intercondylar origin of medial gastrocnemius) |
| Angiography | Medial deviation and precise, focal narrowing of the popliteal artery |
| Medial head of gastrocnemius strain/rupture | |
| Ultrasound | Partial or complete disruption of the medial gastrocnemius at the musculotendinous junction or fluid between aponeuroses of medial head of gastrocnemius and soleus without muscle rupture |
| Magnetic resonance imaging | Partial or complete disruption of fibers and hematoma at musculotendinous junction of medial head of gastrocnemius |
Biomechanics of Running
There are 3 phases of running gait—stance, swing, and float. As running speed increases, less time is spent in the stance phase.40,77 Normal running gait begins with lateral heel strike, followed by foot pronation during midstance, and foot supination during push-off.36,40 Proper running gait is critical to absorb the impact of striking the ground; insufficient or excessive pronation or supination alters force dissipation in the kinetic chain (muscles, ligaments, tendons, and bones).40 In developed countries, most individuals wear running shoes and land on their heels.77 The rear-foot strike running pattern is facilitated by elevated and cushioned heels of modern running shoes during which ground reaction forces reach 1.5 to 3 times body weight.77 Three common recommendations include (1) motion control shoe for low arches, (2) cushioned trainer shoe for high arches, and (3) stability shoes for normal arches.8,22 While these modifications have gained popularity within the running community to combat injury, there are currently limited data to suggest that these measures, based on arch type or foot shape, can reduce injury rates.67,68,109
Recently, biomechanics research has emerged to support the advantages of “barefoot” running. These runners generate smaller collision forces than individuals wearing standard cushioned running shoes.77 The ability of “minimalist” runners to absorb impact more efficiently than shod runners may result from adaptations of dense plantar mechanoreceptors; the somatosensory feedback is likely diminished in shod runners.111,112,125 To date, no clinical studies substantiate the claims of injury reduction using a “minimalist” style.
Video Gait Analysis
While running gait is highly variable, there are certain abnormalities correlated with injury.36 Dynamic gait analyses allow for identification of biomechanical factors not obvious with standard static examinations.51 More sophisticated methods, such as electromyography, accelerometers, electrogoniometers, and gyroscopes, are generally reserved for research purposes.51
Observational gait analysis (ie, patient walking in the hallway) can provide some useful information but is fraught with error because multiple motion segments are difficult to assess simultaneously.105 Viewing in multiple planes provides the truest picture of running form.105 Videotape observational gait analysis (VOGA) enhances accuracy of gait analyses and is performed from head to toe using anterior, posterior, and lateral views on a standard treadmill.99 Force plates determine precise kinetic and kinematic forces. Treadmill analyses are applicable to ground running110 within 1 standard deviation, if the treadmill surface is sufficiently stiff and belt speed regulated.89 While gait analysis may help identify biomechanical abnormalities, it is unclear if these corrections will prevent or help treat lower extremity injuries.
Medial Tibial Stress Syndrome
Medial Tibial Stress Syndrome, Anatomy and Biomechanics
Medial tibial stress syndrome is thought to be a periostitis caused by abnormal traction by the deep flexor43 and/or soleus muscles.32 A recent review cautions that histologic studies have failed to provide evidence for periostitis as an underlying etiology. Mismatch between bony resorption and formation with resultant overloading of the tibial cortex is a likely etiology of medial tibial stress syndrome.94 Anatomic evidence suggests that either the soleus or an aponeurotic band connects the medial soleus to the posteromedial tibia and can impart traction stress to the periosteum when the soleus contracts and stretches.15,58,86
Static and dynamic measurements have been studied to determine which anatomical (limb length, ankle dorsiflexion, first metatarsophalangeal joint extension, and arch height) and biomechanical (center of pressure excursion, malleolar valgus index, and gait velocity) factors were associated with medial tibial stress syndrome.12 Subjects with medial tibial stress syndrome had significantly greater visual analog pain levels and slower gait velocity.12 Medial tibial stress syndrome is associated with an imbalance of foot pressure (greater on the medial foot), excessive pronation, sudden increase in intensity and/or duration of training, and an uneven training terrain.103,120 These factors increase soleus strain by eccentric contraction to resist pronation. In a separate study, decreased hip internal rotation, increased ankle plantar flexion, and positive navicular drop were associated with medial tibial stress syndrome.92
Nonoperative Treatment
Treatment strategies for medial tibial stress syndrome frequently include rest and cross-training using low-impact activities such as stationary biking and underwater running.38 Once symptoms resolve, training should slowly accelerate (10% to 25% every 3 to 6 weeks).73
The efficacy of physical therapy and nonsteroidal anti-inflammatory drugs is questionable. In military recruits, aspirin, phenylbutazone, heel-cord stretching exercises, and/or short walking cast for 1 week provided no significant decrease in the duration of shin splints compared to rest alone.6 Off-the-shelf orthotics and calf stretching can improve medial tibial stress syndrome, even with chronic pain.78 Extracorporal shockwave therapy has shown promise; the value of the pneumatic leg brace is unknown.91,93 Circumferential straps19 and taping55 have not been shown to effectively dampen posteromedial tibial stress. Unfortunately, current evidence does not support any prevention method for medial tibial syndrome.26
Operative Treatment
Surgical outcomes studies on medial tibial stress syndrome are of poor methodological quality and design.94,137 The most effective surgical procedures involve release of the deep posterior compartment, including the soleus sling and removal of a strip of posteromedial tibia periosteum (Figure 1).32,145 A recent series of operatively treated cases noted good/excellent results in 69% and fair/poor results in 31% at 30 months postoperatively.145 Only 41% returned to their previous level of athletic activity.145 Complications occur frequently (hematoma, localized paresthesias, numbness, and stress fractures).32,60,145
Figure 1.
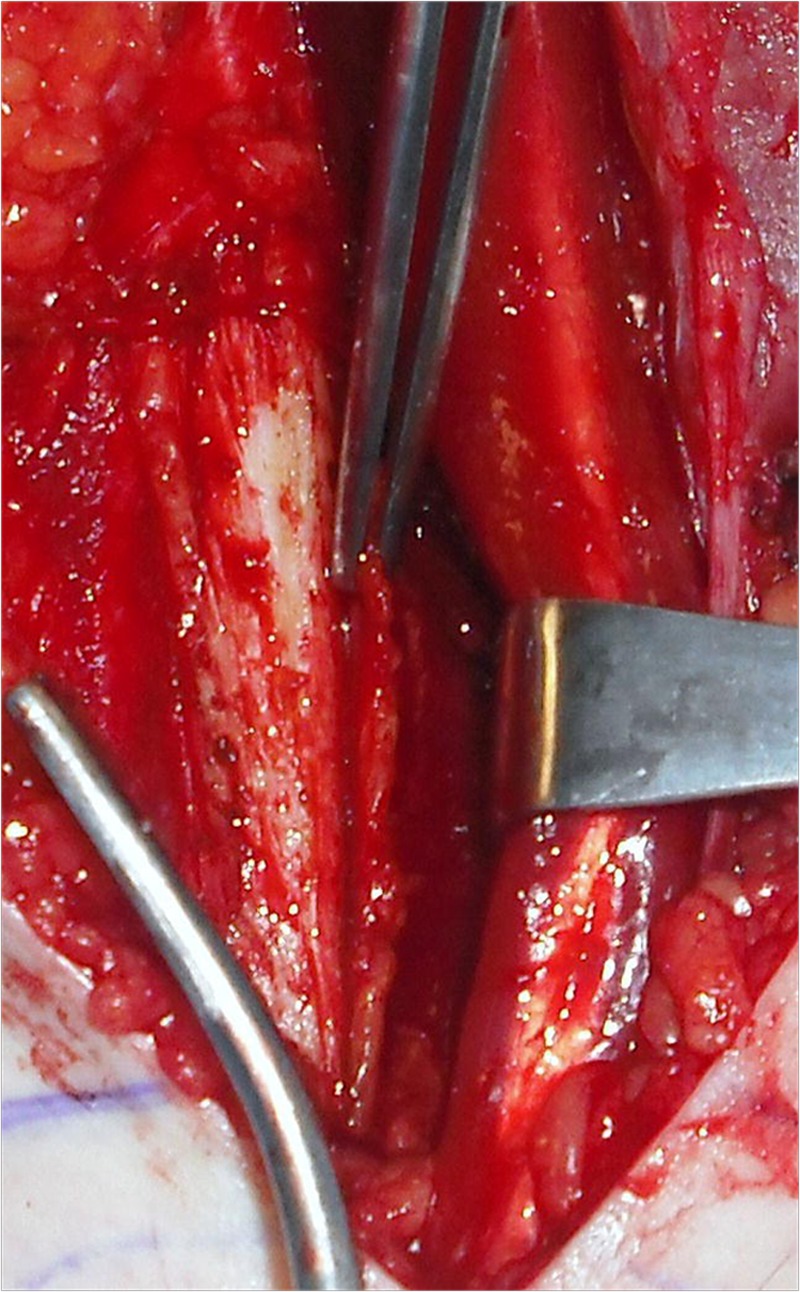
Posteromedial tibial stress syndrome is treated by release of the deep posterior leg fascia and excision of the posteromedial tibial periosteum (held by forceps).
Noninsertional Achilles Tendinopathy
Anatomy and Biomechanics
During running, the Achilles tendon loading exceeds 12.5 times the runner’s body weight.69,70 The gastrocnemius-soleus complex allows the Achilles tendon, the strongest tendon in the body,59,62 to absorb tremendous energy before strain injury occurs.59,62 The tendon fibers spiral 90° instead of vertically increasing potential elongation and energy production.2,97 The tendon can stretch up to 4% before microscopic damage occurs; macroscopic rupture occurs at strain levels greater than 8%.61
Factors influencing Achilles tendinopathy are both intrinsic and mechanical. Intrinsic factors (regional hypovascularity, endocrine or metabolic diseases, genetic makeup) can predispose the tendon to degeneration.137 Mechanical factors (overuse and lack of flexibility) increase tendon strain surpassing the energy-absorbing ability and leading to microtears.137 Training errors (technique, inappropriate footwear, inconsistent surfaces) are associated with degeneration.62,137 Excessive lateral heel strike and compensatory foot pronation can result in uneven force generation from the gastrocnemius and soleus muscles and overloading certain areas of the Achilles tendon.57,124 Altered knee kinematics and reduced proximal muscle activity (rectus femoris and gluteus medius) are associated with Achilles tendinopathy.9,35
Nonoperative Treatment
Relative rest and nonsteroidal anti-inflammatory drugs reduce pain produced by inflammation in the acute phase; physical therapy and orthoses can correct underlying mechanics contributing to this injury.24,25,83,101,102 Total abstention from running is recommended acutely; later in the disease process, light loading may be helpful in stimulating healing and remodeling of collagen fibers.80,142 Evidence for deep friction massage, soft tissue mobilization, and stretching is limited28,45; therapeutic techniques should incorporate eccentric strengthening of the triceps surae.3,4,64,127
A recent review of conservative treatments for chronic Achilles tendinopathy found strong evidence for heavy load eccentric exercise.118 Nonsteroidal anti-inflammatory drugs and shock wave therapy are not proven treatments, corticosteroid injections should be avoided,118 and other injections (ie, platelet-rich plasma injections) are still experimental.118 The majority of patients with Achilles tendinopathy recover fully with exercise alone.123 Reduced neuromuscular activity of the gastrocnemius muscle during weightbearing in patients suffering with Achilles tendinopathy should be a focus of treatment.13 Heel lifts of 12 to 15 mm can decrease strain in the Achilles tendon pain25,95 and resolve symptoms in up to 75% of runners.119,122,139 Devices that limit hindfoot eversion may also avert Achilles tendinopathy by preventing excessive pronation during midstance115; braces and splints have not been beneficial.118
Operative Treatment
Several techniques are available for Achilles tendinopathy and share basic tenets: longitudinal incision within the tendon to detect lesions and excision of fibrotic adhesions and degenerated nodules.80 If large lesions are excised, reconstructive procedures, including local transfers (flexor hallucis longus), may be necessary.143 Surgical success rates of 70% to 85% have been reported.130 In the largest follow-up study to date, Paavola et al noted that 11% of patients had postoperative complications with 3.2% requiring additional procedures. The most common complications were skin necrosis and wound infection.102
To reduce the risk of skin-related problems, outpatient percutaneous longitudinal tenotomy has been introduced.81 This procedure decreases tendon strain and improves local circulation for better nourishment and healing.41,81,133 In middle- and long-distance runners, 37 of 48 patients reported excellent25 or good12 results at an average of nearly 2 years following this procedure.81
Tibial and Fibular Stress Fractures
Anatomy and Biomechanics
The tibial shaft is the most common site of lower extremity stress fracture in runners and accounts for nearly 50% of all stress fractures in athletes.48 Stress fractures along the anterior cortex are associated with the radiographic “dreaded black line” and sluggish healing often necessitating operative treatment (Figure 2). Fibular stress fractures occur less frequently and represent 4.6% to 21% of all athletic stress fractures.47,96
Figure 2.
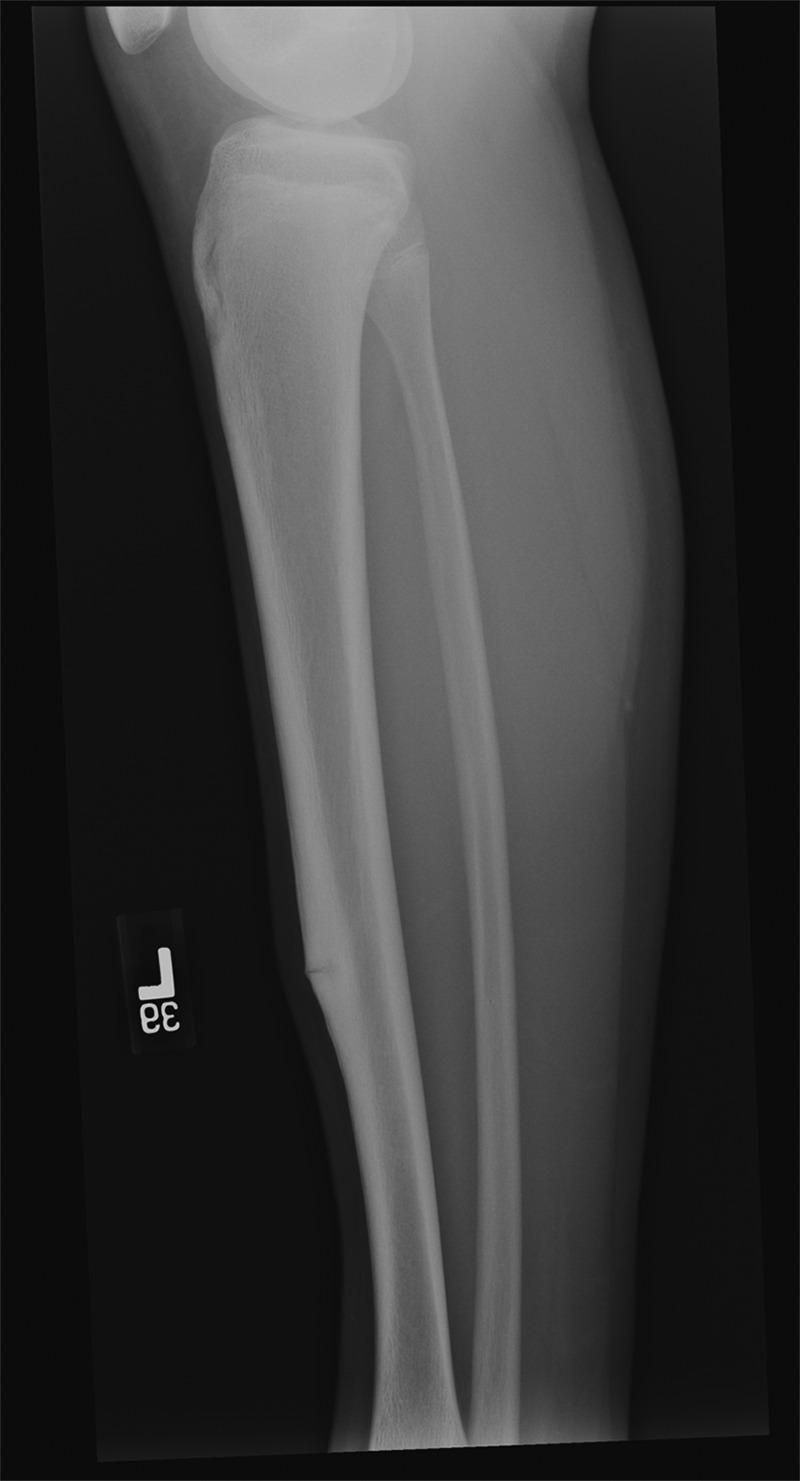
Lateral radiograph of the tibia demonstrates “dreaded black line,” which is a poor prognostic indicator of spontaneous healing.
Normally, bone remodels to match demands according to Wolf’s law.48 When under repetitive loads without sufficient time to remodel, bone will fatigue and fail.48 The initial microdamage inevitably propagates into macroscopic damage if stress continues (Figure 3).63 In the tibia, the resulting stress fracture usually occurs on the compression side and involves the posteromedial cortex in a transverse orientation.17 High-risk tibial stress fractures occur less frequently along the anterior cortex of the midtibia or medial malleolus. The mechanism of injury may be repetitive ankle plantar flexor contractions.48 Fibular stress fractures typically occur within the shaft, 5 to 6 cm proximal to the lateral malleolus corresponding to the attachment site of these same tendons.21
Figure 3.
(a) Bone scan demonstrates increased tracer uptake in the proximal tibia in both immediate and delayed phase images consistent with a proximal tibial stress fracture. (b) and (c) Magnetic resonance imaging clearly shows a distal tibial stress fracture line on both T1 and T2 weighted images.
Risk factors for tibial stress fractures in male runners are difficult to predict; low bone mineral density and lean mass in lower limb, menstrual imbalance, and low-fat diet are associated with stress fractures in female runners.16 Menstrual irregularities and high weekly training mileage place runners at high risk of recurrence.72 Biomechanical abnormalities (leg-length discrepancy, peak hip adduction, rearfoot eversion angles during stance phase of running) have also been linked to tibial stress fractures in women.39,106 Vertical instantaneous load rate and peak knee adduction and internal rotation forces do not appear to play a role in development of tibial stress fractures.106
Systemic reviews have failed to definitively link foot type with tibial stress injury. However, extremes of foot type, including high longitudinal arch and excessive forefoot varus, may predispose runners to tibial stress fractures.11 Running on a treadmill and longer foot pronation lessen the risk of developing a tibial stress fracture.50,88
Nonoperative Treatment
Fibular and low-risk tibial stress fractures often respond to a period of rest ranging from 4 to 8 weeks.48,63 Low-risk stress fractures occur in locations that have adequate vascularity and are under less strain than high-risk stress fractures (eg, anterior tibia, tension-side of femoral neck, navicular, base of the fifth metatarsal). Progressive return to sports is initiated with cross-training followed by higher impact activities.41,54
A variety of interventions have been proposed to hasten return to play and/or assist in the treatment of tibial stress fractures with a propensity for sluggish healing.48 Coupled electric fields and extracorporeal shock wave therapy may improve treatment of these fractures14,96; pneumatic leg braces show conflicting results.5,129 Pulsed ultrasound114 and bone stimulators147 have not been effective. Bisphosphonates may accelerate the healing process for tibial stress fractures128 and/or preventing their occurrence.87
Operative Treatment
Despite appropriate treatment, some tibial stress fractures fail to heal and result in the “dreaded black line,” sclerosis, and/or cyst formation.147 The anterior, tension-sided tibial stress fractures are at an elevated risk for delayed healing (presumably from hypovascularity). However, there is still a role for conservative care: operative intervention does not guarantee healing and may lead to complications such as infection, pain at the nail insertion site, or completion of the fracture.147
The surgical treatment of choice is an intramedullary nail.23 Alternately, drilling with bone grafting has shown favorable results.90 These techniques may allow for faster return to sports with minimal morbidity.90
Gastrocnemius-Soleus Strain/Rupture
Anatomy and Biomechanics
The multipennate gastrocnemius and soleus muscles are commonly strained due to their complex structure,20 accounting for 3.6% of all reported soccer injuries.7 The medial head of the gastrocnemius originates from the medial femoral condyle and fuses with the smaller lateral head before joining the soleus aponeurosis to form the Achilles tendon.20 The gastroc is a “fast action” muscle composed largely of type IIb fibers and spans 2 joints, making it susceptible to strain injuries.31 The soleus only crosses the ankle joint and consists largely of type I slow-twitch fibers and is less likely to be injured.20
Injury to medial head of the gastrocnemius (Figure 4) is caused by sudden dorsiflexion of a plantar flexed foot with the knee in extension or sudden extension of the knee with the ankle dorsiflexed.89 Running studies indicate that this injury occurs near touchdown and is associated with faster-than-normal running speeds and inappropriate body posture, which causes altered muscle length and shock absorption.71 The injury has a predilection for the poorly conditioned, middle-aged athlete with “thick calves” who is engaged in strenuous activity.74
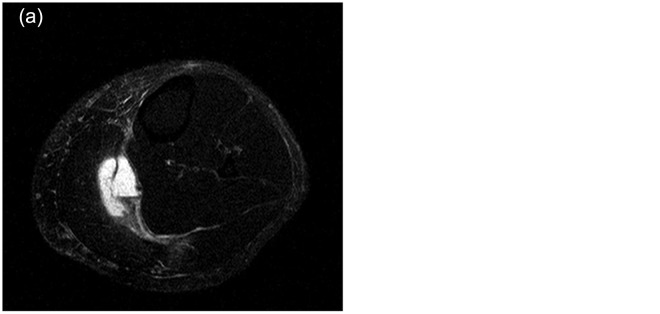
Figure 4.
(a) and (b) Axial and sagittal T2-weighted magnetic resonance images demonstrate a fluid collection at the musculotendinous junction of the medial head of the gastrocnemius correlating with a tear.
Nonoperative Treatment
Medial head of gastrocnemius and soleus strains are treated nonoperatively with a combination of ice, analgesics, and casting/splinting (night splint or CAM boot), depending on the extent of injury. In severe strains and ruptures, casting in plantar flexion for 3 weeks, followed by neutral boot/cast for an additional 3 weeks, may suffice.89 Dorsiflexion to neutral is expected at 1-month postinjury, while return to preinjury level may be achieved by 2 months.84,85 Ultrasound can be used to confirm healing.74 Compression of the limb decreases hematoma size and facilitates healing.75
Operative Treatment
Although controversial, surgical repair for complete ruptures of the medial head of the gastrocnemius may be indicated acutely in those unable to maintain full body weight on the metatarsal heads with the ankle in maximal plantar flexion and/or a palpable defect.89 The surgical technique involves direct reapproximation of the tendon edges at the musculotendinous junction.89 Fasciotomy is indicated if a large hematoma precipitates a compartment syndrome.31,74
Chronic Exertional Compartment Syndrome
Anatomy and Biomechanics
During heavy exercise, fluid accumulates within the interstitial space of skeletal muscle,107 increasing mass up to 20%.116 The buildup of interstitial fluid combined with limited expansion of the fascial compartments, especially the anterior and lateral leg compartments, may lead to elevated intramuscular pressures, causing capillary occlusion.107 The decreased blood flow can result in cell hypoxia, increased dependence on anaerobic metabolism, production of lactate,107 and eventual cell death. Recent studies have failed to link stiffness and thickness of muscle fascia to chronic exertional compartment syndrome.29 However, low muscle capillary supply is a possible pathogenic factor.37
There are limited data on risk factors for chronic exertional compartment syndrome. The mechanism remains elusive though landing style,65 muscle type composition,140 and capillary density within skeletal muscle37 may be contributors.
Nonoperative Treatment
Cessation of the inciting activity remains the only nonoperative measure to effectively treat chronic exertional compartment syndrome long-term.42 In cases when elevated postexercise compartment pressures are associated with abnormally increased distal vascular resistance (decreased postexercise ankle-brachial index, biphasic arterial waveforms in distal extremity, slow-flow velocity), lumbar sympathetic blockade has been proposed as a method of increasing blood flow to muscle during exercise.44 With a lumbar sympathetic block, the normal reflex sympathetic adrenergic-mediated vasoconstrictive effect in vessels supplying the working muscle is blunted, so the vasodilating effects of accumulating local metabolites predominates.44
Operative Treatment
Fasciotomy is the mainstay of treatment for those athletes who wish to return to sporting activities.32,42,100 The procedure involves releasing the fascia overlying the anterior and lateral compartments and, if necessary, the superficial and deep posterior compartments. While a variety of fasciotomy techniques have been described, 78% to 92% of athletes can expect to return to their previous level of function.42,53,138
Less invasive techniques such as endoscopic and percutaneous fasciotomies using a fasciotome have been developed to minimize surgical incision size and soft tissue disruption and allow swifter return to sports.42,66 Despite these advantages, minimally invasive techniques may inadequately release and/or increase risk of injury to neurovascular structures (superficial peroneal nerve, saphenous nerve, and saphenous vein).54
A structured rehabilitation program maximizes functional outcome after surgery.117 Patients are progressed from “PRICE” to full range of motion by focusing on soft tissue mobility via stretching, neurodynamic mobilization, strengthening, and ultimately biomechanical analysis of the athlete during sport specific activities.117
Popliteal Artery Entrapment Syndrome
Anatomy and Biomechanics
Before bifurcating into the anterior and posterior tibial arteries, the popliteal artery normally courses beneath and between the medial and lateral heads of the gastrocnemius, adjacent to the plantaris and popliteus muscles, and through the tendinous arch of the soleus.10 Alterations of the normal structural relationships can cause compression of the popliteal artery.47,108 Most cases of popliteal artery compression are caused by anatomic variations formed during embryonic stages of development30 and include an abnormal attachment of the medial head of the gastrocnemius within the intracondylar notch,104 medial course of the popliteal artery,1 and/or aberrant fibrous bands.1,113 More recently, a “functional” variation has been attributed to hypertrophy of surrounding musculature.10 Care must be taken to distinguish popliteal artery entrapment syndrome from chronic exertional compartment syndrome, as the 2 disorders occur in the same population and present with similar symptoms.134
In the development of popliteal artery entrapment syndrome, the popliteal artery is focally compressed against the medial femoral condyle during forceful plantar flexion.27,40 With repeated constriction, the artery can sustain damage to its wall and form aneurysms and/or stenotic lesions leading to thrombosis and/or embolic events.27,40
For reasons unknown, men are more prone to the disease.47,126
Nonoperative Treatment
Because of the progressive nature of the entrapment, nonoperative management has a limited role. Early detection and intervention can limit progression of the process and lead to more favorable outcomes by minimizing arterial damage.34,82,148
Operative Treatment
While thrombolytic therapy is controversial in limiting the extent of subsequent bypass grafting,148 surgical intervention is the hallmark of treatment for ischemic symptomatic patients.18,100 Decompression of the lesion by division of the medial head of the gastrocnemius is often necessary to prevent recurrence.34,82,148
The need for vascular surgery depends on the chronicity of the vascular compression.76,148 In long-standing entrapment, the popliteal artery may sustain irreversible vessel wall damage and is prone to atherosclerosis, aneurysm, and thrombosis.49 Bypass grafting appears to be the treatment of choice.46,47,76 Vein patching and endovascular treatments have had limited success.49
Many patients return to previous activities following surgical intervention113; those with decompression alone tend to have better outcomes than decompression plus reconstruction.34,82
Conclusion
Chronic exertional compartment syndrome, tibial stress fractures, posteromedial tibial stress syndrome, popliteal artery entrapment syndrome, gastrocnemius-soleus strains/tears, and Achilles tendinopathy are common running ailments. While no clear evidence exists that these injuries can be prevented, most can be treated successfully by considering underlying anatomical and biomechanical causes. The majority of tibial stress fractures, gastrocnemius-soleus strains/tears, and Achilles tendinopathy are effectively managed with an appropriate balance of relative rest and therapy. Chronic exertional compartment syndrome and popliteal artery entrapment syndrome, both thought to be caused by anatomic abnormalities, are often remedied by surgical intervention.
Footnotes
The following author declared potential conflicts of interest: Michael Plakke, MS, received a grant from the Ben Franklin Fund.
References
- 1. Aktan Ikiz ZA, Ucerler H, Ozgur Z. Anatomic variations of popliteal artery that may be a reason for entrapment. Surg Radiol Anat. 2009;31:695-700 [DOI] [PubMed] [Google Scholar]
- 2. Alexander RM, Bennet-Clark HC. Storage of elastic strain energy in muscle and other tissues. Nature. 1977;265:114-117 [DOI] [PubMed] [Google Scholar]
- 3. Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000;29:135-146 [DOI] [PubMed] [Google Scholar]
- 4. Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360-366 [DOI] [PubMed] [Google Scholar]
- 5. Allen CS, Flynn TW, Kardouni JR, et al. The use of a pneumatic leg brace in soldiers with tibial stress fractures—a randomized clinical trial. Mil Med. 2004;169:880-884 [DOI] [PubMed] [Google Scholar]
- 6. Andrish JT, Bergfeld JA, Walheim J. A prospective study on the management of shin splints. J Bone Joint Surg Am. 1974;56:1697-1700 [PubMed] [Google Scholar]
- 7. Armfield DR, Kim DH, Towers JD, Bradley JP, Robertson DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803-842 [DOI] [PubMed] [Google Scholar]
- 8. Asplund CA, Brown DL. The running shoe prescription: fit for performance. Phys Sportsmed. 2005;33:17-24 [DOI] [PubMed] [Google Scholar]
- 9. Azevedo LB, Lambert MI, Vaughan CL, O’Connor CM, Schwellnus MP. Biomechanical variables associated with Achilles tendinopathy in runners. Br J Sports Med. 2009;43:288-292 [DOI] [PubMed] [Google Scholar]
- 10. Baltopoulos P, Filippou DK, Sigala F. Popliteal artery entrapment syndrome: anatomic or functional syndrome? Clin J Sport Med. 2004;14:8-12 [DOI] [PubMed] [Google Scholar]
- 11. Barnes A, Wheat J, Milner C. Association between foot type and tibial stress injuries: a systematic review. Br J Sports Med. 2008;42:93-98 [DOI] [PubMed] [Google Scholar]
- 12. Bartosik KE, Sitler M, Hillstrom HJ, Palamarchuk H, Huxel K, Kim E. Anatomical and biomechanical assessments of medial tibial stress syndrome. J Am Podiatr Med Assoc. 2010;100(2):121-132 [DOI] [PubMed] [Google Scholar]
- 13. Baur H, Muller S, Hirschmuller A, Cassel M, Weber J, Mayer F. Comparison in lower leg neuromuscular activity between runners with unilateral mid-portion Achilles tendinopathy and healthy individuals. J Electromyogr Kinesiol. 2011;21:499-505 [DOI] [PubMed] [Google Scholar]
- 14. Beck BR, Matheson GO, Bergman G, et al. Do capacitively coupled electric fields accelerate tibial stress fracture healing? A randomized controlled trial. Am J Sports Med. 2008;36:545-553 [DOI] [PubMed] [Google Scholar]
- 15. Beck BR, Osternig LR. Medial tibial stress syndrome: the location of muscles in the leg in relation to symptoms. J Bone Joint Surg Am. 1994;76:1057-1061 [DOI] [PubMed] [Google Scholar]
- 16. Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996;24:810-818 [DOI] [PubMed] [Google Scholar]
- 17. Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-111 [DOI] [PubMed] [Google Scholar]
- 18. Boskamp M, Ijpma FF, Meerwaldt R, Blomme AM. Serious morbidity associated with popliteal artery entrapment syndrome. Clin J Sport Med. 2009;19:435-437 [DOI] [PubMed] [Google Scholar]
- 19. Bouche RT, Johnson CH. Medial tibial stress syndrome (tibial fasciitis): a proposed pathomechanical model involving fascial traction. J Am Podiatr Med Assoc. 2007;97:31-36 [DOI] [PubMed] [Google Scholar]
- 20. Bryan Dixon J. Gastrocnemius vs soleus strain: how to differentiate and deal with calf muscle injuries. Curr Rev Musculoskelet Med. 2009;2:74-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burrows HJ. Fatigue fractures of the fibula. J Bone Joint Surg Br. 1948;30:266-279 [PubMed] [Google Scholar]
- 22. Butler RJ, Hamill J, Davis I. Effect of footwear on high and low arched runners’ mechanics during a prolonged run. Gait Posture. 2007;26:219-225 [DOI] [PubMed] [Google Scholar]
- 23. Chang PS, Harris RM. Intramedullary nailing for chronic tibial stress fractures: a review of five cases. Am J Sports Med. 1996;24:688-692 [DOI] [PubMed] [Google Scholar]
- 24. Clancy WG, Jr, Neidhart D, Brand RL. Achilles tendonitis in runners: a report of five cases. Am J Sports Med. 1976;4:46-57 [DOI] [PubMed] [Google Scholar]
- 25. Clement DB, Taunton JE, Smart GW. Achilles tendinitis and peritendinitis: etiology and treatment. Am J Sports Med. 1984;12:179-184 [DOI] [PubMed] [Google Scholar]
- 26. Craig DI. Medial tibial stress syndrome: evidence-based prevention. J Athl Train. 2008;43:316-318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech (Bristol, Avon). 2011;26:78-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cyriax J. Manipulation trials. Br Med J. 1980;280:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dahl M, Hansen P, Stal P, Edmundsson D, Magnusson SP. Stiffness and thickness of fascia do not explain chronic exertional compartment syndrome. Clin Orthop Relat Res. 2011;469:3495-3500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Delaney TA, Gonzalez LL. Occlusion of popliteal artery due to muscular entrapment. Surgery. 1971;69:97-101 [PubMed] [Google Scholar]
- 31. Delgado GJ, Chung CB, Lektrakul N, et al. Tennis leg: clinical US study of 141 patients and anatomic investigation of four cadavers with MR imaging and US. Radiology. 2002;224:112-119 [DOI] [PubMed] [Google Scholar]
- 32. Detmer DE. Chronic shin splints: classification and management of medial tibial stress syndrome. Sports Med. 1986;3:436-446 [DOI] [PubMed] [Google Scholar]
- 33. di Marzo L, Cavallaro A, Sciacca V, et al. Diagnosis of popliteal artery entrapment syndrome: the role of duplex scanning. J Vasc Surg. 1991;13:434-438 [DOI] [PubMed] [Google Scholar]
- 34. di Marzo L, Cavallaro A, Sciacca V, Mingoli A, Tamburelli A. Surgical treatment of popliteal artery entrapment syndrome: a ten-year experience. Eur J Vasc Surg. 1991;5:59-64 [DOI] [PubMed] [Google Scholar]
- 35. Donoghue OA, Harrison AJ, Laxton P, Jones RK. Lower limb kinematics of subjects with chronic achilles tendon injury during running. Res Sports Med. 2008;16:23-38 [DOI] [PubMed] [Google Scholar]
- 36. Dugan SA, Bhat KP. Biomechanics and analysis of running gait. Phys Med Rehabil Clin N Am. 2005;16:603-621 [DOI] [PubMed] [Google Scholar]
- 37. Edmundsson D, Toolanen G, Thornell LE, Stal P. Evidence for low muscle capillary supply as a pathogenic factor in chronic compartment syndrome. Scand J Med Sci Sports. 2010;20:805-813 [DOI] [PubMed] [Google Scholar]
- 38. Edwards PH, Jr, Wright ML, Hartman JF. A practical approach for the differential diagnosis of chronic leg pain in the athlete. Am J Sports Med. 2005;33:1241-1249 [DOI] [PubMed] [Google Scholar]
- 39. Ferber R, Noehren B, Hamill J, Davis IS. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010;40:52-58 [DOI] [PubMed] [Google Scholar]
- 40. Fields KB, Bloom OJ, Priebe D, Foreman B. Basic biomechanics of the lower extremity. Prim Care. 2005;32:245-251 [DOI] [PubMed] [Google Scholar]
- 41. Friedrich T, Schmidt W, Jungmichel D, Horn LC, Josten C. Histopathology in rabbit Achilles tendon after operative tenolysis (longitudinal fiber incisions). Scand J Med Sci Sports. 2001;11:4-8 [DOI] [PubMed] [Google Scholar]
- 42. Fronek J, Mubarak SJ, Hargens AR, et al. Management of chronic exertional anterior compartment syndrome of the lower extremity. Clin Orthop Relat Res. 1987;220:217-227 [PubMed] [Google Scholar]
- 43. Garth WP, Jr, Miller ST. Evaluation of claw toe deformity, weakness of the foot intrinsics, and posteromedial shin pain. Am J Sports Med. 1989;17:821-827 [DOI] [PubMed] [Google Scholar]
- 44. Gebauer A, Schultz CR, Giangarra CE. Chronic exercise-induced leg pain in an athlete successfully treated with sympathetic block. Am J Sports Med. 2005;33:1575-1578 [DOI] [PubMed] [Google Scholar]
- 45. Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31:531-535 [DOI] [PubMed] [Google Scholar]
- 46. Goh BK, Tay KH, Tan SG. Diagnosis and surgical management of popliteal artery entrapment syndrome. ANZ J Surg. 2005;75:869-873 [DOI] [PubMed] [Google Scholar]
- 47. Gourgiotis S, Aggelakas J, Salemis N, Elias C, Georgiou C. Diagnosis and surgical approach of popliteal artery entrapment syndrome: a retrospective study. Vasc Health Risk Manag. 2008;4:83-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Harrast MA, Colonno D. Stress fractures in runners. Clin Sports Med. 2010;29:399-416 [DOI] [PubMed] [Google Scholar]
- 49. Henry MF, Wilkins DC, Lambert AW. Popliteal Artery Entrapment Syndrome. Curr Treat Options Cardiovasc Med. 2004;6:113-120 [DOI] [PubMed] [Google Scholar]
- 50. Hetsroni I, Finestone A, Milgrom C, et al. The role of foot pronation in the development of femoral and tibial stress fractures: a prospective biomechanical study. Clin J Sport Med. 2008;18:18-23 [DOI] [PubMed] [Google Scholar]
- 51. Higginson BK. Methods of running gait analysis. Curr Sports Med Rep. 2009;8:136-141 [DOI] [PubMed] [Google Scholar]
- 52. Hootman JM, Macera CA, Ainsworth BE, Martin M, Addy CL, Blair SN. Predictors of lower extremity injury among recreationally active adults. Clin J Sport Med. 2002;12:99-106 [DOI] [PubMed] [Google Scholar]
- 53. Howard JL, Mohtadi NG, Wiley JP. Evaluation of outcomes in patients following surgical treatment of chronic exertional compartment syndrome in the leg. Clin J Sport Med. 2000;10:176-184 [DOI] [PubMed] [Google Scholar]
- 54. Hutchinson MR, Bederka B, Kopplin M. Anatomic structures at risk during minimal-incision endoscopically assisted fascial compartment releases in the leg. Am J Sports Med. 2003;31:764-769 [DOI] [PubMed] [Google Scholar]
- 55. Jackson SW, Bailey D. Shin splints in the young athlete: a non-specific diagnosis. Physician Sportsmed. 1975;3:45-51 [DOI] [PubMed] [Google Scholar]
- 56. Jacobs SJ, Berson BL. Injuries to runners: a study of entrants to a 10,000 meter race. Am J Sports Med. 1986;14:151-155 [DOI] [PubMed] [Google Scholar]
- 57. James SL, Bates BT, Osternig LR. Injuries to runners. Am J Sports Med. 1978;6:40-50 [DOI] [PubMed] [Google Scholar]
- 58. James T. Chronic lower leg pain in sport. Aust Fam Physician. 1988;17:1041-1045 [PubMed] [Google Scholar]
- 59. Jarvinen TA, Kannus P, Paavola M, Jarvinen TL, Jozsa L, Jarvinen M. Achilles tendon injuries. Curr Opin Rheumatol. 2001;13:150-155 [DOI] [PubMed] [Google Scholar]
- 60. Jarvinnen M, Aho H, Niittymaki S. Results of the surgical treatment of the medial tibial syndrome in athletes. Int J Sports Med. 1989;10:55-57 [DOI] [PubMed] [Google Scholar]
- 61. Jozsa L KP. Human Tendons: Anatomy, Physiology, and Pathology. Champaign, IL: Human Kinetics; 1997 [Google Scholar]
- 62. Kader D, Saxena A, Movin T, Maffulli N. Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med. 2002;36:239-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kaeding CC, Yu JR, Wright R, Amendola A, Spindler KP. Management and return to play of stress fractures. Clin J Sport Med. 2005;15:442-447 [DOI] [PubMed] [Google Scholar]
- 64. Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. Br J Sports Med. 2007;41:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kirby RL, McDermott AG. Anterior tibial compartment pressures during running with rearfoot and forefoot landing styles. Arch Phys Med Rehabil. 1983;64:296-299 [PubMed] [Google Scholar]
- 66. Kitajima I, Tachibana S, Hirota Y, Nakamichi K, Miura K. One-portal technique of endoscopic fasciotomy: chronic compartment syndrome of the lower leg. Arthroscopy. 2001;17:33. [DOI] [PubMed] [Google Scholar]
- 67. Knapik JJ, Brosch LC, Venuto M, et al. Effect on injuries of assigning shoes based on foot shape in air force basic training. Am J Prev Med. 2010;38:S197-S211 [DOI] [PubMed] [Google Scholar]
- 68. Knapik JJ, Trone DW, Swedler DI, et al. Injury reduction effectiveness of assigning running shoes based on plantar shape in Marine Corps basic training. Am J Sports Med. 2010;38:1759-1767 [DOI] [PubMed] [Google Scholar]
- 69. Komi PV. Relevance of in vivo force measurements to human biomechanics. J Biomech. 1990;23(suppl 1):23-34 [DOI] [PubMed] [Google Scholar]
- 70. Komi PV, Fukashiro S, Jarvinen M. Biomechanical loading of Achilles tendon during normal locomotion. Clin Sports Med. 1992;11:521-531 [PubMed] [Google Scholar]
- 71. Kong PW. Gastrocnemius injury during running: a case report. Int J Sports Med. 2009;30:46-52 [DOI] [PubMed] [Google Scholar]
- 72. Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk factors for recurrent stress fractures in athletes. Am J Sports Med. 2001;29:304-310 [DOI] [PubMed] [Google Scholar]
- 73. Kortebein PM, Kaufman KR, Basford JR, Stuart MJ. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32:S27-S33 [DOI] [PubMed] [Google Scholar]
- 74. Kwak HS, Han YM, Lee SY, Kim KN, Chung GH. Diagnosis and follow-up US evaluation of ruptures of the medial head of the gastrocnemius (“tennis leg”). Korean J Radiol. 2006;7:193-198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Kwak HS, Lee KB, Han YM. Ruptures of the medial head of the gastrocnemius (“tennis leg”): clinical outcome and compression effect. Clin Imaging. 2006;30:48-53 [DOI] [PubMed] [Google Scholar]
- 76. Lambert AW, Wilkins DC. Popliteal artery entrapment syndrome: collaborative experience of the Joint Vascular Research Group. Br J Surg. 1998;85:1367-1368 [DOI] [PubMed] [Google Scholar]
- 77. Lieberman DE, Venkadesan M, Werbel WA, et al. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature. 2010;463:531-535 [DOI] [PubMed] [Google Scholar]
- 78. Loudon JK, Dolphino MR. Use of foot orthoses and calf stretching for individuals with medial tibial stress syndrome. Foot Ankle Spec. 2010;3:15-20 [DOI] [PubMed] [Google Scholar]
- 79. Lysholm J, Wiklander J. Injuries in runners. Am J Sports Med. 1987;15:168-171 [DOI] [PubMed] [Google Scholar]
- 80. Maffulli N, Kader D. Tendinopathy of tendo achillis. J Bone Joint Surg Br. 2002;84:1-8 [DOI] [PubMed] [Google Scholar]
- 81. Maffulli N, Testa V, Capasso G, Bifulco G, Binfield PM. Results of percutaneous longitudinal tenotomy for Achilles tendinopathy in middle- and long-distance runners. Am J Sports Med. 1997;25:835-840 [DOI] [PubMed] [Google Scholar]
- 82. Marzo L, Cavallaro A, Mingoli A, Sapienza P, Tedesco M, Stipa S. Popliteal artery entrapment syndrome: the role of early diagnosis and treatment. Surgery. 1997;122:26-31 [DOI] [PubMed] [Google Scholar]
- 83. Mayer F, Hirschmuller A, Muller S, Schuberth M, Baur H. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Br J Sports Med. 2007;41:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. McClure JG. Gastrocnemius musculotendinous rupture: a condition confused with thrombophlebitis. South Med J. 1984;77:1143-1145 [DOI] [PubMed] [Google Scholar]
- 85. Menz MJ, Lucas GL. Magnetic resonance imaging of a rupture of the medial head of the gastrocnemius muscle: a case report. J Bone Joint Surg Am. 1991;73:1260-1262 [PubMed] [Google Scholar]
- 86. Michael RH, Holder LE. The soleus syndrome: a cause of medial tibial stress (shin splints). Am J Sports Med. 1985;13:87-94 [DOI] [PubMed] [Google Scholar]
- 87. Milgrom C, Finestone A, Novack V, et al. The effect of prophylactic treatment with risedronate on stress fracture incidence among infantry recruits. Bone. 2004;35:418-424 [DOI] [PubMed] [Google Scholar]
- 88. Milgrom C, Finestone A, Segev S, Olin C, Arndt T, Ekenman I. Are overground or treadmill runners more likely to sustain tibial stress fracture? Br J Sports Med. 2003;37:160-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Miller WA. Rupture of the musculotendinous juncture of the medial head of the gastrocnemius muscle. Am J Sports Med. 1977;5:191-193 [DOI] [PubMed] [Google Scholar]
- 90. Miyamoto RG, Dhotar HS, Rose DJ, Egol K. Surgical treatment of refractory tibial stress fractures in elite dancers: a case series. Am J Sports Med. 2009;37:1150-1154 [DOI] [PubMed] [Google Scholar]
- 91. Moen MH, Bongers T, Bakker EW, et al. The additional value of a pneumatic leg brace in the treatment of recruits with medial tibial stress syndrome; a randomized study. J R Army Med Corps. 2010;156:236-240 [DOI] [PubMed] [Google Scholar]
- 92. Moen MH, Bongers T, Bakker EW, et al. Risk factors and prognostic indicators for medial tibial stress syndrome. Scand J Med Sci Sports. 2012;22:34-39 [DOI] [PubMed] [Google Scholar]
- 93. Moen MH, Rayer S, Schipper M, et al. Shockwave treatment for medial tibial stress syndrome in athletes: a prospective controlled study. Br J Sports Med. 2012;46:253-257 [DOI] [PubMed] [Google Scholar]
- 94. Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: a critical review. Sports Med. 2009;39:523-546 [DOI] [PubMed] [Google Scholar]
- 95. Mohr R. Achilles tendinitis: rationale for use and apllication of orthotics. Foot Ankle Clin. 1997;2:439-456 [Google Scholar]
- 96. Moretti B, Notarnicola A, Garofalo R, et al. Shock waves in the treatment of stress fractures. Ultrasound Med Biol. 2009;35:1042-1049 [DOI] [PubMed] [Google Scholar]
- 97. Movin T, Kristoffersen-Wiberg M, Shalabi A, Gad A, Aspelin P, Rolf C. Intratendinous alterations as imaged by ultrasound and contrast medium-enhanced magnetic resonance in chronic achillodynia. Foot Ankle Int. 1998;19:311-317 [DOI] [PubMed] [Google Scholar]
- 98. Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45:691-696 [DOI] [PubMed] [Google Scholar]
- 99. O’Connor FG, Hoke B, Torrance A. Video gait analysis. In: Textbook of Running Medicine. New York, NY: McGraw-Hill; 2001:59-66 [Google Scholar]
- 100. Ohara N, Miyata T, Oshiro H, Shigematsu H. Surgical treatment for popliteal artery entrapment syndrome. Cardiovasc Surg. 2001;9:141-144 [DOI] [PubMed] [Google Scholar]
- 101. Paavola M, Kannus P, Paakkala T, Pasanen M, Jarvinen M. Long-term prognosis of patients with achilles tendinopathy: an observational 8-year follow-up study. Am J Sports Med. 2000;28:634-642 [DOI] [PubMed] [Google Scholar]
- 102. Paavola M, Orava S, Leppilahti J, Kannus P, Jarvinen M. Chronic Achilles tendon overuse injury: complications after surgical treatment. An analysis of 432 consecutive patients. Am J Sports Med. 2000;28:77-82 [DOI] [PubMed] [Google Scholar]
- 103. Pell RFt, Khanuja HS, Cooley GR. Leg pain in the running athlete. J Am Acad Orthop Surg. 2004;12:396-404 [DOI] [PubMed] [Google Scholar]
- 104. Pillai J, Levien LJ, Haagensen M, Candy G, Cluver MD, Veller MG. Assessment of the medial head of the gastrocnemius muscle in functional compression of the popliteal artery. J Vasc Surg. 2008;48:1189-1196 [DOI] [PubMed] [Google Scholar]
- 105. Plastaras CT, Rittenberg JD, Rittenberg KE, Press J, Akuthota V. Comprehensive functional evaluation of the injured runner. Phys Med Rehabil Clin N Am. 2005;16:623-649 [DOI] [PubMed] [Google Scholar]
- 106. Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS. Biomechanical predictors of retrospective tibial stress fractures in runners. J Biomech. 2008;41:1160-1165 [DOI] [PubMed] [Google Scholar]
- 107. Qvarfordt P, Christenson JT, Eklof B, Ohlin P, Saltin B. Intramuscular pressure, muscle blood flow, and skeletal muscle metabolism in chronic anterior tibial compartment syndrome. Clin Orthop Relat Res. 1983;179:284-290 [PubMed] [Google Scholar]
- 108. Radonic V, Koplic S, Giunio L, Bozic I, Maskovic J, Buca A. Popliteal artery entrapment syndrome: diagnosis and management, with report of three cases. Tex Heart Inst J. 2000;27:3-13 [PMC free article] [PubMed] [Google Scholar]
- 109. Richards CE, Magin PJ, Callister R. Is your prescription of distance running shoes evidence-based? Br J Sports Med. 2009;43:159-162 [DOI] [PubMed] [Google Scholar]
- 110. Riley PO, Dicharry J, Franz J, Della Croce U, Wilder RP, Kerrigan DC. A kinematics and kinetic comparison of overground and treadmill running. Med Sci Sports Exerc. 2008;40:1093-1100 [DOI] [PubMed] [Google Scholar]
- 111. Robbins S, Gouw GJ, McClaran J, Waked E. Protective sensation of the plantar aspect of the foot. Foot Ankle. 1993;14:347-352 [DOI] [PubMed] [Google Scholar]
- 112. Robbins SE, Hanna AM. Running-related injury prevention through barefoot adaptations. Med Sci Sports Exerc. 1987;19:148-156 [PubMed] [Google Scholar]
- 113. Rosset E, Hartung O, Brunet C, et al. Popliteal artery entrapment syndrome: anatomic and embryologic bases, diagnostic and therapeutic considerations following a series of 15 cases with a review of the literature. Surg Radiol Anat. 1995;17:161-169 [DOI] [PubMed] [Google Scholar]
- 114. Rue JP, Armstrong DW, 3rd, Frassica FJ, Deafenbaugh M, Wilckens JH. The effect of pulsed ultrasound in the treatment of tibial stress fractures. Orthopedics. 2004;27:1192-1195 [DOI] [PubMed] [Google Scholar]
- 115. Ryan M, Grau S, Krauss I, Maiwald C, Taunton J, Horstmann T. Kinematic analysis of runners with achilles mid-portion tendinopathy. Foot Ankle Int. 2009;30:1190-1195 [DOI] [PubMed] [Google Scholar]
- 116. Schissel DJ, Godwin J. Effort-related chronic compartment syndrome of the lower extremity. Mil Med. 1999;164:830-832 [PubMed] [Google Scholar]
- 117. Schubert AG. Exertional compartment syndrome: review of the literature and proposed rehabilitation guidelines following surgical release. Int J Sports Phys Ther. 2011;6:126-141 [PMC free article] [PubMed] [Google Scholar]
- 118. Scott A, Huisman E, Khan K. Conservative treatment of chronic Achilles tendinopathy. CMAJ. 2011;183:1159-1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Segesser B, Nigg BM. [Tibial insertion tendinoses, achillodynia, and damage due to overuse of the foot-etiology, biomechanics, therapy] [author’s translation]. Orthopade. 1980;9:207-214 [PubMed] [Google Scholar]
- 120. Sharma J, Golby J, Greeves J, Spears IR. Biomechanical and lifestyle risk factors for medial tibia stress syndrome in army recruits: a prospective study. Gait Posture. 2011;33:361-365 [DOI] [PubMed] [Google Scholar]
- 121. Shipway R, Holloway I. Running free: embracing a healthy lifestyle through distance running. Perspect Public Health. 2010;130:270-276 [DOI] [PubMed] [Google Scholar]
- 122. Shrier I, Matheson GO, Kohl HW., 3rd Achilles tendonitis: are corticosteroid injections useful or harmful? Clin J Sport Med. 1996;6:245-250 [PubMed] [Google Scholar]
- 123. Silbernagel KG, Brorsson A, Lundberg M. The majority of patients with Achilles tendinopathy recover fully when treated with exercise alone: a 5-year follow-up. Am J Sports Med. 2011;39:607-613 [DOI] [PubMed] [Google Scholar]
- 124. Smart GW, Taunton JE, Clement DB. Achilles tendon disorders in runners—a review. Med Sci Sports Exerc. 1980;12:231-243 [PubMed] [Google Scholar]
- 125. Squadrone R, Gallozzi C. Effect of a five-toed minimal protection shoe on static and dynamic ankle position sense. J Sports Med Phys Fitness. 2011;51:401-408 [PubMed] [Google Scholar]
- 126. Stager A, Clement D. Popliteal artery entrapment syndrome. Sports Med. 1999;28:61-70 [DOI] [PubMed] [Google Scholar]
- 127. Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986;208:65-68 [PubMed] [Google Scholar]
- 128. Stewart GW, Brunet ME, Manning MR, Davis FA. Treatment of stress fractures in athletes with intravenous pamidronate. Clin J Sport Med. 2005;15:92-94 [DOI] [PubMed] [Google Scholar]
- 129. Swenson EJ, Jr, DeHaven KE, Sebastianelli WJ, Hanks G, Kalenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. Am J Sports Med. 1997;25:322-328 [DOI] [PubMed] [Google Scholar]
- 130. Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy: a critical review. Am J Sports Med. 2001;29:315-320 [DOI] [PubMed] [Google Scholar]
- 131. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95-101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Tenforde AS, Sayres LC, McCurdy ML, Collado H, Sainani KL, Fredericson M. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PM R. 2011;3:125-131 [DOI] [PubMed] [Google Scholar]
- 133. Testa V, Maffulli N, Capasso G, Bifulco G. Percutaneous longitudinal tenotomy in chronic Achilles tendonitis. Bull Hosp Jt Dis. 1996;54:241-244 [PubMed] [Google Scholar]
- 134. Turnipseed WD. Functional popliteal artery entrapment syndrome: a poorly understood and often missed diagnosis that is frequently mistreated. J Vasc Surg. 2009;49:1189-1195 [DOI] [PubMed] [Google Scholar]
- 135. van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41:469-480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. van Mechelen W. Running injuries: a review of the epidemiological literature. Sports Med. 1992;14:320-335 [DOI] [PubMed] [Google Scholar]
- 137. van Sterkenburg MN, van Dijk CN. Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1367-1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Verleisdonk EJ, Schmitz RF, van der Werken C. Long-term results of fasciotomy of the anterior compartment in patients with exercise-induced pain in the lower leg. Int J Sports Med. 2004;25:224-229 [DOI] [PubMed] [Google Scholar]
- 139. Viitasalo JT, Kvist M. Some biomechanical aspects of the foot and ankle in athletes with and without shin splints. Am J Sports Med. 1983;11:125-130 [DOI] [PubMed] [Google Scholar]
- 140. Wallensten R, Karlsson J. Histochemical and metabolic changes in lower leg muscles in exercise-induced pain. Int J Sports Med. 1984;5:202-208 [DOI] [PubMed] [Google Scholar]
- 141. Walter SD, Hart LE, McIntosh JM, Sutton JR. The Ontario cohort study of running-related injuries. Arch Intern Med. 1989;149:2561-2564 [PubMed] [Google Scholar]
- 142. Welsh RP, Clodman J. Clinical survey of Achilles tendinitis in athletes. Can Med Assoc J. 1980;122:193-195 [PMC free article] [PubMed] [Google Scholar]
- 143. Wilcox DK, Bohay DR, Anderson JG. Treatment of chronic achilles tendon disorders with flexor hallucis longus tendon transfer/augmentation. Foot Ankle Int. 2000;21:1004-1010 [DOI] [PubMed] [Google Scholar]
- 144. Wilder RP, Magrum E. Exertional compartment syndrome. Clin Sports Med. 2010;29:429-435 [DOI] [PubMed] [Google Scholar]
- 145. Yates B, Allen MJ, Barnes MR. Outcome of surgical treatment of medial tibial stress syndrome. J Bone Joint Surg Am. 2003;85:1974-1980 [DOI] [PubMed] [Google Scholar]
- 146. Yeung SS, Yeung EW, Gillespie LD. Interventions for preventing lower limb soft-tissue running injuries. Cochrane Database Syst Rev. 2011;7:CD001256. [DOI] [PubMed] [Google Scholar]
- 147. Young AJ, McAllister DR. Evaluation and treatment of tibial stress fractures. Clin Sports Med. 2006;25:117-128 [DOI] [PubMed] [Google Scholar]
- 148. Zund G, Brunner U. Surgical aspects of popliteal artery entrapment syndrome: 26 years of experience with 26 legs. Vasa. 1995;24:29-33 [PubMed] [Google Scholar]