Abstract
Objective
To help understand physician movement out of Manitoba by determining the factors that influence Manitoba medical graduates’ choices about practice locations.
Design
Cross-sectional, within-stage, mixed-model survey.
Setting
Manitoba.
Participants
All University of Manitoba medical graduates from classes 1998 to 2009 for whom we had valid contact information (N = 912 of 943 graduates) were invited in August 2009 to participate in a survey.
Main outcome measures
Demographic information; ratings, on a 5-point scale, of the importance when choosing first practice locations of 12 practice characteristics, 3 recruitment strategies, and 4 location characteristics listed in the survey; free-text narratives on unlisted factors; and estimates of likely practice location upon completion of training for recent graduates still in residency training.
Results
Completed surveys were received from 331 (35.1%) graduates of the surveyed classes, 162 (53.3%) of whom chose Manitoba for their first practice location. Multiple regression analyses indicated that graduates choosing Manitoba for their first practice location were significantly more likely to have done their residency training in Manitoba (P < .05), whether or not they gave a high rating to the importance of being near family and friends. Also, graduates choosing Manitoba were significantly more likely to be recent graduates (P = .007) and less likely to be members of a visible minority (P = .018). These associations were robust even when analyses were restricted to responses from practitioners without cause to estimate practice locations. Early self-selection of graduates during entry into specific residency programs, results of the residency match process, and “putting down roots” during residency years were 3 important interrelated themes identified through qualitative analyses.
Conclusion
Residency education in Manitoba is the overwhelming factor influencing graduates’ choice of Manitoba as their first practice location, regardless of graduates’ rating of the importance of being near family or friends. Graduates’ narratives provided insights into the complexities of choosing practice locations and enhanced the interpretive and theoretical validity of the study findings. More extensive studies involving all Canadian residents could further define the role residency location plays in physician practice location.
Résumé
Objectif
Comprendre les raisons qui font en sorte que les médecins quittent le Manitoba, en identifiant les facteurs qui influencent le choix de l’endroit où ils vont pratiquer.
Type d’étude
Enquête transversale de modèle mixte en cours de stage.
Contexte
Le Manitoba.
Participants
Tous les étudiants en médecine de l’Université du Manitoba ayant obtenu leur diplôme entre 1998 et 2009 et que nous avons réussi à contacter ont été invités à participer à l’enquête, en août 2009.
Principaux paramètres à l’étude
Caractéristiques démographiques; importance attribuée, au moment de choisir le premier lieu de pratique, à 12 caractéristiques de pratique, 3 stratégies de recrutement et 4 caractéristiques du lieu, tels qu’énumérées dans l’enquête; rédaction d’un texte libre sur des facteurs non mentionnés; et, pour les récents diplômés n’ayant pas terminé leur résidence, ce qu’ils prévoient comme lieu probable de pratique à la fin de la formation.
Résultats
Des enquêtes complétées ont été reçues de 331 diplômés des années visées (35,1 %), dont 162 avaient choisi le Manitoba comme lieu initial de pratique. L’analyse de régression a montré que les diplômés qui choisissent le Manitoba comme lieu initial de pratique étaient significativement plus susceptibles d’avoir fait leur résidence au Manitoba (P < ,05), quelle que soit l’importance qu’ils attachent au fait d’être près de leur famille ou de leurs amis. Ces diplômés étaient aussi plus susceptibles d’être des diplômés récents (P = ,007) et moins susceptibles d’appartenir à une minorité visible (P = ,018). Les associations trouvées étaient fortes, même lorsque l’analyse se limitait aux réponses des médecins qui n’avaient pas de raison de prévoir un lieu de pratique. L’analyse qualitative a révélé trois importants thèmes étroitement reliés, soit : le fait pour un diplômé de choisir précocement un stage particulier de résidence, les résultats du processus de jumelage de la résidence et « le développement de racines » au cours de la résidence.
Conclusion
Au Manitoba, la formation en cours de résidence est ce qui a le plus d’importance pour déterminer le choix du Manitoba comme premier lieu de pratique, et ce, quelle que soit l’importance attribuée par les diplômés au fait d’être près de leur famille ou de leurs amis. Les textes fournis par les participants ont permis de mieux comprendre la complexité du choix du lieu de pratique et ont ainsi renforcé la validité interprétative et théorique des résultats de l’étude. Des études portant sur l’ensemble des résidents du Canada pourraient mieux définir de quelle façon l’endroit où le médecin a fait sa résidence influence le choix de son lieu de pratique.
In 2001, in the midst of ongoing concern about physician shortages in Manitoba, specifically in rural and remote Manitoba, it was reported that up to two-thirds of Manitoba-trained physicians left the province after residency.1 More recent reports suggested that Manitoba was the third-highest source of Canadian-educated physicians emigrating to the United States and was among 4 provinces and territories in the country that had consistently lost physicians to other provinces.2–4 Little information is available to understand the reasons for emigration of Manitoba medical graduates, 90% of whom were Manitoba residents at the time of admission into medical school. In fact, few studies have examined factors related to provincial retention of Canadian medical school graduates.4
Medical schools operate under a social accountability framework that includes responsibility to their regions, and they aspire to a sustainable health care system for the future.5–8 Accordingly, we sought to study our region’s attraction and retention of medical graduates during a period of perceived medical human resource scarcity by reporting first practice locations of Manitoba medical graduates and determining the factors influencing graduates’ choice of first practice locations. Our findings might offer insight into the determinants of first practice locations for all Canadian medical graduates and might be especially relevant to those provinces experiencing physician emigration.
METHODS
All University of Manitoba medical graduates from classes 1998 to 2009 for whom we had valid contact information (N = 912 of 943 graduates) were invited in August 2009 to participate in a survey. Contact information was provided by the university alumni office from updated address information on file. After receiving ethics board approval for the study, surveys were distributed electronically to 484 graduates (53.1%) and by mail to 428 graduates (46.9%). Electronic survey recipients received 2 reminders about survey completion, and paper survey recipients were reminded once. When contact information was missing from the alumni office files or when surveys were undeliverable at the addresses on file and returned to sender, additional, systematic efforts were made to locate graduates’ whereabouts. For all such missing contact information, the Scott’s medical directories, publicly accessible online physician databases maintained by provincial colleges of physicians and surgeons, and the Google search engine were used to find more recent or alternate contact information. If graduates with outdated contact information were known to be in residency programs anywhere in Canada, surveys were mailed care-of the specific residency programs (after obtaining permission from the programs). Despite these efforts, about 76 (8.1%) of our 943 graduates could not be located. When surveys were not returned to sender, it was assumed that they were successfully delivered to the recipients. All respondents were guaranteed privacy and confidentiality.
Questionnaire construction was in part influenced by previous studies.9,10 The questionnaire gathered information on graduates’ first practice locations, first residency locations, and demographic characteristics, and listed factors potentially influencing Manitoba medical graduates’ choice of first practice location (Box 1). Graduates were asked to rate each factor on a scale of 1 (no importance) to 5 (very important). In accordance with the within-stage, mixed-model design,11 open-ended questions were included in the questionnaire to collect free-text narratives on unlisted factors that respondents believed were important with respect to where one ultimately chooses to practice. All participants who were still in residency training when responding to the survey were asked to indicate their best approximation of their expected practice location upon completion of their training. No attempt was made to gather locations of graduates’ subsequent residency programs, if any.
Box 1. Factors, as listed in the survey, that potentially influenced Manitoba medical graduates’ choice of first practice location: Graduates ranked each factor on a scale of 1 (no importance) to 5 (very important).
Practice characteristics
Discipline not offered elsewhere
Academic or professional reputation
Good morale among colleagues
Variety of clinical experiences offered
Good on-call schedule
Research opportunities
Emphasis on primary care
Ethnic diversity of patients or staff
Good salary or other financial incentives
Supportive of applicants with children
Opportunity for part-time work or for job-sharing
Recruitment strategies
Positive interview experience
Previous experience with the program
Location characteristics
Location near spouse or significant other
Educational or job opportunities for spouse or significant other
Location near family or friends
All surveys returned by March 31, 2010, were compiled in a spreadsheet database and analyzed using Excel 2007 and SAS, version 9.1. Graduates’ ratings of factors were reclassified as high (rating of 4 or 5) or low (rating of 1, 2, or 3). Descriptive data were compared between graduates choosing first practice locations within and outside Manitoba using χ2 tests, independent-samples t tests, or Mann-Whitney tests. Factors associated (P ≤ .10) with geographic location in bivariate analyses were selected for inclusion in a multiple logistic regression model. Associations from the regression model were expressed as odds ratios with 95% CIs. Stratified variables were introduced into this model when an association at the bivariate level was known to be modified by the presence of a third, confounding variable. Final influential factors were determined based on P < .05. The fit of the logistic regression model was determined by the Hosmer-Lemeshow statistic.12,13 Qualitative data, collected in the form of free-text narrative comments, were reduced via exploratory thematic analysis and were displayed in lists. Finally, the results of qualitative and quantitative approaches were compared and integrated into a coherent whole discussion.
RESULTS
Survey respondents
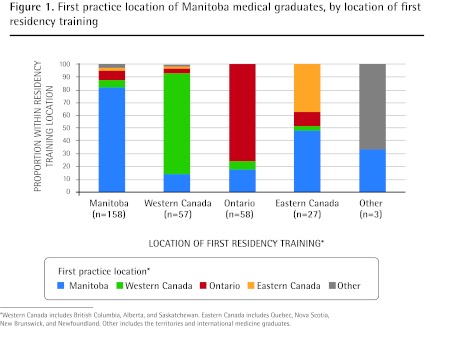
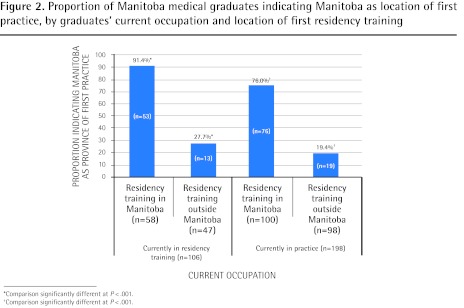
Completed surveys were received from 331 (35.1%) graduates, of whom 198 (59.8%) were in practice, 131 (39.6%) were in residency training, and 2 (0.6%) were pursuing nonphysician careers. Table 1 shows the representativeness of the survey respondents relative to the entire population of Manitoba medical graduates. Twenty-five (19.1%) residents were unsure of their future practice locations, but they did not differ significantly from the 106 residents who estimated their future locations. These 25 residents were not included in analyses, nor were the 2 nonphysicians. Of the remaining 304 respondents who were included in subsequent analyses, 162 (53.3%) chose Manitoba for their first practice location. As depicted in Figures 1 and 2, the proportion choosing Manitoba was significantly associated with location of first residency training (P < .05) and current occupation (P < .001).
Table 1.
Representativeness of survey respondents relative to all Manitoba medical graduates from 1998 to 2009
| CHARACTERISTIC | SURVEY RESPONDENTS, N (%) (N = 331*) | MANITOBA MEDICAL GRADUATES, N (%) (N = 943*) |
|---|---|---|
| Year of graduation | ||
| • 1998–2000 | 76 (23.0) | 211 (22.4) |
| • 2001–2003 | 71 (21.5) | 219 (23.2) |
| • 2004–2006 | 93 (28.1) | 246 (26.1) |
| • 2007–2009 | 79 (23.9) | 267 (28.3) |
| Sex | ||
| • Female | 154 (46.5) | 397 (42.1) |
| • Male | 162 (48.9) | 546 (57.9) |
| Location of residency training | ||
| • Manitoba | 171 (51.7) | 496 (52.6) |
| • Rest of Canada | 153 (46.2) | 433 (45.9) |
| • International | 3 (0.9) | 9 (1.0) |
| Medical specialty | ||
| • Family medicine | 122 (36.9) | 328 (34.8) |
| • Other specialty | 206 (62.2) | 599 (63.5) |
Numbers do not add up to 331 survey respondents or 943 graduates owing to missing responses or unknown information.
Figure 1.
First practice location of Manitoba medical graduates, by location of first residency training
*Western Canada includes British Columbia, Alberta, and Saskatchewan. Eastern Canada includes Quebec, Nova Scotia, New Brunswick, and Newfoundland. Other includes the territories and international medicine graduates.
Figure 2.
Proportion of Manitoba medical graduates indicating Manitoba as location of first practice, by graduates’ current occupation and location of first residency training
*Comparison significantly different at P < .001.
†Comparison significantly different at P < .001.
Bivariate analyses and stratified bivariate analyses
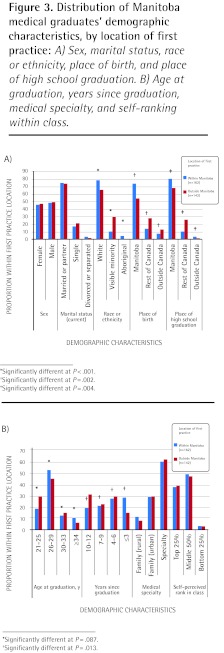
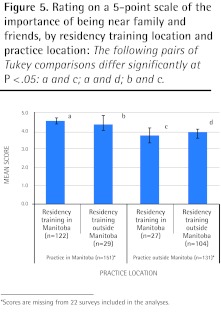
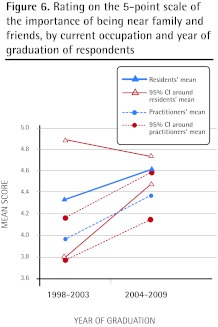
Race or ethnicity (P < .001), place of birth (P = .002), place of high school graduation (P = .004), and number of years since graduation (P = .013) were significantly associated with the choice of Manitoba as the first practice location (Figures 3A and 3B). Those choosing Manitoba, compared with those not choosing Manitoba, were less likely to rate as important a good on-call schedule (3.96 vs 4.18; P = .08), more likely to rate as important a practice supportive of applicants with children (3.43 vs 2.98; P = .01), and more likely to rate as important being near family or friends (4.52 vs 3.95; P < .001) (Figure 4). Being near family or friends was rated higher by those choosing Manitoba for their first practice location, irrespective of the location of residency training (Figure 5). Being near family or friends was rated higher by recent graduate cohorts and residents than earlier graduate cohorts and practitioners (Figure 6).
Figure 3.
Distribution of Manitoba medical graduates’ demographic characteristics, by location of first practice: A) Sex, marital status, race or ethnicity, place of birth, and place of high school graduation. B) Age at graduation, years since graduation, medical specialty, and self-ranking within class.
*Significantly different at P < .001.
†Significantly different at P =.002.
‡Significantly different at P =.004.
*Significantly different at P = .087.
†Significantly different at P = .013.
Figure 4.
Mean scores on 5-point rating scale on survey items for Manitoba medical graduates, by location of first-practice.
*Significantly different at P = .08.
†Significantly different at P = .01.
‡Significantly different at P < .001.
Figure 5.
Rating on a 5-point scale of the importance of being near family and friends, by residency training location and practice location: The following pairs of Tukey comparisons differ significantly at P < .05: a and c; a and d; b and c.
*Scores are missing from 22 surveys included in the analyses.
Figure 6.
Rating on the 5-point scale of the importance of being near family and friends, by current occupation and year of graduation of respondents
Multivariate analysis
Preliminary multiple logistic regression analysis suggested that graduates choosing Manitoba for their first practice location were significantly more likely to have had residency training in Manitoba (P < .05), to be recent graduates (P = .007), and to rate the importance of being near family or friends as high (P < .001), and were less likely to report being members of visible minorities (P = .018). When confounding between the importance of being near family or friends and location of residency training was stratified, residency training in Manitoba emerged as the main predictor of Manitoba as the first practice location (Table 2). Because recent graduates were potentially more likely to have estimated their future practice locations, the model was also applied to the 198 practitioner respondents only. As the magnitude of the associations did not vary considerably between the models, only results from the more inclusive model are presented here.
Table 2.
Results of multiple logistic regression analysis of associations between Manitoba medical graduate demographic, practice, and location characteristics, and the choice of Manitoba as first practice location: Analysis based on data from 260 respondents with complete information on all variables in the model.
| CHARACTERISTIC |
FIRST PRACTICE LOCATION, N
|
ODDS RATIO (95% CI) | P VALUE | |
|---|---|---|---|---|
| IN MANITOBA (N = 136) | OUTSIDE MANITOBA (N = 124) | |||
| Graduate demographic characteristics | ||||
| • Race or ethnicity | ||||
| -Visible minority | 15 | 39 | 0.36 (0.15–0.84) | .018 |
| -Aboriginal | 6 | 1 | 3.00 (0.10–93.44) | .530 |
| -White* | 115 | 84 | 1.00 | NA |
| • Place of birth | ||||
| -Within Manitoba | 106 | 71 | 1.91 (0.82–4.46) | .135 |
| -Outside Manitoba* | 30 | 53 | 1.00 | NA |
| • Place of high school graduation | ||||
| -Within Manitoba | 117 | 88 | 1.51 (0.56–4.09) | .419 |
| -Outside Manitoba* | 19 | 36 | 1.00 | NA |
| • Age at graduation from medical program† | 136 | 124 | 1.01 (0.92–1.11) | .869 |
| • Years since medical graduation† | 136 | 124 | 0.82 (0.72–0.95) | .007 |
| • Current occupation | ||||
| -Medical practice | 83 | 91 | 1.08 (0.41–2.88) | .870 |
| -Residency training including fellowships* | 53 | 33 | 1.00 | NA |
| Practice characteristics | ||||
| • Good on-call schedule | ||||
| -High rating‡ | 107 | 103 | 0.49 (0.20–1.21) | .123 |
| -Low rating*‡ | 29 | 21 | 1.00 | NA |
| • Supportive of applicants with children | ||||
| -High rating‡ | 78 | 59 | 1.12 (0.54–2.31) | .755 |
| -Low rating*‡ | 58 | 65 | 1.00 | NA |
| • Being near family or friends | ||||
| -High rating‡ (Manitoba residency) | 101 | 19 | 20.74 (9.52–45.17) | < .001 |
| -Low rating‡ (Manitoba residency) | 9 | 8 | 4.77 (1.34–17.01) | .016 |
| -Low rating‡ (residency outside Manitoba) | 4 | 20 | 0.84 (0.23–3.03) | .787 |
| -High rating‡ (residency outside Manitoba)* | 22 | 77 | 1.00 | NA |
NA—not applicable.
Reference category.
Continuous variable.
A high rating was a score of 4 or 5 on the 5-point scale of importance. A low rating was a score of 1, 2, or 3 on the 5-point scale.
Qualitative analysis
Eighty-nine (29.3%) of the graduates (24 residents and 65 practitioners) provided written narratives on factors influencing their current geographic locations. Interrelated themes identified as determining first practice locations, whether in Manitoba or elsewhere in Canada, were early self-selection of graduates during entry into specific residency programs for personal and professional reasons; results of the residency match process; the needs of the regional or local health care system and the corresponding influence on the structure and curricula of residency programs; and personal life events such as establishment of permanent relationships and “putting down roots” during residency years.
Medical students who were older, had partners, or were raising children when entering medical school usually reported having planned early for a Manitoba residency and subsequent Manitoba practice. Rural-origin students choosing Manitoba for their first practice location attributed their choice to their rural roots. Loan repayment obligations and return-of-service agreements (offered through nonuniversity sources) were also given credit for a few graduates’ decisions to begin practice in Manitoba. Opportunities to work in rural and remote areas and for underserviced populations were also quoted as reasons for choosing practice in Manitoba.
Among the reasons listed for practising outside Manitoba were a preference for practices and policies followed by health care systems in other provinces, “big-city living,” the need to pay off debts, a lack of opportunities in Manitoba for chosen specialties, and negative experiences while in medical school in Manitoba. Several respondents commented that they actively chose residencies outside Manitoba hoping to broaden their horizons, “see the world,” and acquire diversity of training. They had welcomed exposure to different perspectives and the experience of different living and working environments, and after all this “life happened.” From that point on, location of practice was less of an actively pursued choice and more of maintaining status quo, as graduates tended to see no compelling argument against staying in their now-familiar locations. A proportion of respondents insisted that the “randomness” of the results of the Canadian Resident Matching Service determined their residency location and consequently their first practice location. A couple of respondents thought that the recruitment strategies employed by the regional health authorities and the province were not strong enough to lure graduates “back home.”
DISCUSSION
A little more than half (53.3%) of our survey respondents chose Manitoba for their first practice location. This proportion is smaller than the proportion (two-thirds) reported to leave the province after residency.1 In fact, most (76.0%) Manitoba medical graduates who began residency training in Manitoba reported Manitoba as the location of their first practices.
Our quantitative analysis suggests that residency training in Manitoba is a strong predictor of first practice location, which supports related observations made elsewhere. Graduates from Memorial University of Newfoundland were more likely to practise in Newfoundland if they completed at least some postgraduate training in the province.4 Specialists who participated in the Northern Ontario Postgraduate Specialty training in northeastern Ontario were more likely to practise in northeastern Ontario than non-participants.14 Similarly, graduates of Canadian medical schools were more likely to practise in the United States if they completed postgraduate training in the United States.15 However, are graduates more likely to choose residencies in locations that they want to practise in or are they more likely to practise in locations that they chose for their residencies? Similar questions have been raised elsewhere.14,15 In 1996, McKendry et al suggested that Canadian physicians who emigrated to the United States had decided early to choose a US-based residency.15 Our findings, however, suggest that graduates were more likely to begin practice in locations where they happened to receive residency training.
Ninety percent of those admitted into the Manitoba medical faculty are originally from Manitoba. Our data, gathered from this relatively homogeneous group (with confounding factors such as being near family and friends), indicate that location of residency training is probably the factor that has the greatest effect when it comes to determining first practice location. Appreciating the necessity of maintaining a balance between the need to retain graduates and the need to enrich graduates’ training and experiences, we suggest that increasing the number and type of postgraduate medical residency training positions in the province might be one strategy to further enhance the retention of medical graduates in the province.
Our data also suggest that, after adjusting for age at graduation and current occupation (ie, whether currently a practitioner or a medical resident), recent graduates were more likely to choose Manitoba as their first practice location compared with early graduates. Whether this is the result of a period effect or another factor is unclear at this time. Interestingly, when compared with residents and recent graduates, practitioners and early graduates were less likely to rate being near family or friends as important. Residents and recent graduates are both estimating their first practice locations as well as estimating the importance of the listed factors in choosing first practice locations, whereas practitioners and most early graduates have already experienced choosing their first practice locations. Responses from the latter group might better reflect the realities and compromises needed in making such crucial decisions, while responses from the former group give an insight into the hopes and ideals of those planning for future practice. Despite such differences, responses from both groups of participants were valuable and informative.
The open-ended, text-based comments were effective in differentiating respondents’ actions from intent and allowed a better understanding of the subjective complexities they faced. While few factors listed in the survey were rated as significantly different in importance between those choosing Manitoba and those not choosing Manitoba, the narratives revealed new factors and explanations for the respondents’ choices about practice locations. Important reasons and influential factors might exist that help graduates as a group determine their first practice locations, but these and other stated factors appear to be unique and of varied importance when we consider individual physicians.
Given some of our findings, the question of developing selective and weighted admission criteria to enhance retention of resident graduates in Manitoba might need to be balanced with the concerns of those promoting national work force mobility and national resident matching, such as the Canadian Resident Matching Service. Such “dialectic” human resource concerns and tensions owing to variable access to training might continue to be inherent factors in considering both future regional physician resource pressures and fair accessibility issues.
Other new findings include results from the multivariate model that race and ethnicity were associated with the choice of Manitoba as first practice location. Respondents who reported being visible minorities (n = 54) were 0.35 times as likely as white graduates (n = 203) to choose a Manitoba location for their first practices. Further, although it was not a statistically significant finding, aboriginal respondents appeared to choose Manitoba as their first practice location nearly 3 times as often as white graduates. However, the number of aboriginal respondents was very low (n = 7). Both of these findings warrant further investigation.
Limitations
One limitation of our study might lie in the fact that first practice location is not predictive of subsequent practice location at 2, 5, or 10 years after graduation. By narrowly defining our outcome variable in this way, we limited our understanding of the rate and pattern of subsequent movement of our graduates after gaining experience in their residencies and first practice locations. Despite this limitation, our study could provide an important contribution to Canadian literature in this area. About two-thirds of Canadian-trained physicians who started working in the year 2000 remained in the same jurisdiction after a period of about 8 years.3 Ryten et al reported that peak times for moving were before starting residency training (ie, immediately on graduation) and on completion of residency training.16 It appears that relatively few graduates move 1, 2, or 3 years after graduation.3,16
Another potential limitation of our study was that the location of first residency training was assumed to be the location in which residency training was completed. Based on narrative data, we estimated that at least about 5% of the survey respondents completed their residency training in geographic locations different from those of their first residency programs. As well, we intentionally did not provide a fixed definition of the term first practice location so as to keep the responses broad in scope. While no respondents questioned us about the specifics of the term, we recognize this might also be a limitation with respect to the specificity of our findings.
Strengths and contributions
Our study suggests that irrespective of the importance of influential factors, residency location might be of utmost importance when physician graduates choose their first practice locations. However, as evidenced by our qualitative data, graduates’ needs and intentions vary at the individual’s decision-making level. While our approach suggests that studies on physician retention might benefit from mixed-methods research, our results support the idea that, while a quantitative statistical approach to physician retention might speak to defining factors regarding the larger population of graduating physicians, it might not be as effective as a qualitatively informed narrative approach to understanding the unique personal factors affecting individual graduates. Consequently, a strength of our study is that graduates’ narratives provided both overlapping and differential insights into the complex issue of choosing a practice location, and enhanced the interpretive and theoretical validity of the study findings.
Conclusion
Among the factors analyzed, residency education in Manitoba is the strongest predictor influencing graduates’ choice of Manitoba as their first practice location. A future study on the effect of residency training locations on practice locations among all Canadian residents might further clarify the role residency location plays in physician retention in all Canadian provinces, including Manitoba. Additionally, as few quantitatively measured factors listed in the survey differed significantly between those choosing Manitoba and those not choosing Manitoba, future studies in this area will benefit from the use of a mixed-methods approach to understanding the complexities inherent in physician retention.
EDITOR’S KEY POINTS
Few studies have examined factors related to provincial retention of Canadian medical school graduates. This study sought to examine Manitoba’s attraction and retention of medical graduates during a period of perceived medical human resource scarcity by reporting first practice locations of Manitoba medical graduates and determining the factors influencing graduates’ choice of first practice locations.
Among the factors analyzed, residency education in Manitoba was the strongest predictor influencing graduates’ choice of Manitoba as their first practice location. Preliminary multiple logistic regression suggested that graduates choosing Manitoba for their first practice location were also more likely to be recent graduates and to rate being near family or friends as important, and less likely to report being members of visible minorities
POINTS DE REPÈRE DU RÉDACTEUR
Peu d’études ont porté sur les facteurs qui font en sorte que les diplômés des facultés de médecine canadiennes restent dans leur province. Cette étude voulait déterminer ce qui attire et retient au Manitoba les diplômés en médecine à un moment où on perçoit une insuffisance de personnel médical, et ce, en examinant ce que les diplômés manitobains choisissent comme premier lieu de pratique ainsi que les facteurs qui influencent ce choix.
Parmi les facteurs étudiés, le fait d’avoir fait sa résidence au Manitoba était celui qui permettait de mieux prédire le choix du Manitoba comme premier lieu de pratique. Les résultats préliminaires d’une analyse de régression logistique multiple donnaient à croire que les diplômés qui choisissent le Manitoba pour débuter leur pratique étaient aussi plus susceptibles d’avoir été diplômés récemment et d’attacher de l’importance au fait d’être près de leur famille ou de leurs amis, tandis qu’ils étaient moins susceptibles d’appartenir à une minorité visible.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors were involved in the concept and design of the study. Drs Raghavan, Martin, and Sandham acquired the data. Dr Raghavan analyzed and interpreted the data, and drafted the article. Dr Fleisher contributed to the interpretation of data and revised the article for important intellectual content. All authors contributed to the review and revision of the manuscript and all authors approved the final version for submission.
Competing interests
None declared
References
- 1.Square D. Manitoba increases med school enrolment in an attempt to fight doctor deficit. CMAJ. 2001;164(3):395. [PMC free article] [PubMed] [Google Scholar]
- 2.Phillips RL, Jr, Petterson S, Fryer GE, Jr, Rosser W. The Canadian contribution to the US physician workforce. CMAJ. 2007;176(8):1083–7. doi: 10.1503/cmaj.060525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canadian Institute for Health Information . Supply, distribution and migration of Canadian physicians, 2008. Ottawa, ON: Canadian Institute for Health Information; 2009. Available from: https://secure.cihi.ca/estore/product-Series.htm?pc=PCC34. Accessed 2012 Oct 16. [Google Scholar]
- 4.Mathews M, Rourke JT, Park A. National and provincial retention of medical graduates of Memorial University of Newfoundland. CMAJ. 2006;175(4):357–60. doi: 10.1503/cmaj.060329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rourke J. How can medical schools contribute to the education, recruitment and retention of rural physicians in their region? Bull World Health Organ. 2010;88(5):395–6. doi: 10.2471/BLT.09.073072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Social accountability. A vision for Canadian medical schools. Ottawa, ON: Health Canada; 2001. Available from: www.afmc.ca/fmec/pdf/sa_vision_canadian_medical_schools_en.pdf. Accessed 2010 Sep 9. [Google Scholar]
- 7.Rourke J. Social accountability in theory and practice. Ann Fam Med. 2006;4(Suppl 1):S45–8. doi: 10.1370/afm.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strasser RP, Lanphear JH, McCready WG, Topps MH, Hunt DD, Matt MC. Canada’s new medical school: the Northern Ontario School of Medicine: social accountability through distributed community engaged learning. Acad Med. 2009;84(10):1459–64. doi: 10.1097/ACM.0b013e3181b6c5d7. [DOI] [PubMed] [Google Scholar]
- 9.Aagaard EM, Julian K, Dedier J, Soloman I, Tillisch J, Pérez-Stable EJ. Factors affecting medical students’ selection of an internal medicine residency program. J Natl Med Assoc. 2005;97(9):1264–70. [PMC free article] [PubMed] [Google Scholar]
- 10.Jarratt LG, Leonardson GR, Nord WJ. Practice location factors influencing South Dakota School of Medicine graduates. S D J Med. 1989;42(12):15–21. [PubMed] [Google Scholar]
- 11.Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educ Res. 2004;33(2):14–26. [Google Scholar]
- 12.Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. Cary, NC: SAS Institute Inc; 1995. [Google Scholar]
- 13.Hosmer DW, Taber S, Lemeshow S. The importance of assessing the fit of logistic regression models: a case study. Am J Public Health. 1991;81(12):1630–5. doi: 10.2105/ajph.81.12.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hogenbirk JC, Mian O, Pong RW. Postgraduate specialty training in northeastern Ontario and subsequent practice location. Rural Remote Health. 2011;11(2):1603. [PubMed] [Google Scholar]
- 15.McKendry RJ, Wells GA, Dale P, Adams O, Buske L, Strachan J, et al. Factors influencing the emigration of physicians from Canada to the United States. CMAJ. 1996;154(2):171–81. [PMC free article] [PubMed] [Google Scholar]
- 16.Ryten E, Thurber AD, Buske L. The class of 1989 and physician supply in Canada. CMAJ. 1998;158(6):723–8. [PMC free article] [PubMed] [Google Scholar]