To the Editor:
Chronic granulomatous disease (CGD) is a rare genetic disorder of phagocyte oxidative metabolism. In addition to infectious complications, granulomatous lesions can involve the gastrointestinal (GI) tract and can mimic ulcerative colitis or Crohn’s disease.1,2 Crohn’s-like manifestations can include oral ulcerations, bowel obstruction, enteritis, colitis, fistulae, abscess, and perianal disease.3 The inflammatory bowel disease in this setting may be severe and cause significant morbidity and adversely impact patients’ quality of life.
Narrow band imaging (NBI) is a new technology that uses 2 specific wavelengths of light, 1 blue and 1 green, to accentuate vascular structures and provide high-contrast endoscopic images of mucosal surfaces. The use of NBI is rapidly expanding in the evaluation of both upper and lower GI diseases; however, the use of NBI in CGD has not previously been reported. Herein we provide the first report on the use of NBI in CGD.
A 15-year-old boy with CGD and a history of CGD-associated colitis in clinical remission for over 4 years on low-dose prednisone (5 mg per day) presented with hyperglycemia and growth delay. Colonoscopy was performed to evaluate subclinical colitis prior to a planned prednisone taper. Colonoscopy with white light revealed mild nodularity and friability in the rectum (Fig. 1A). When NBI was applied the mucosal abnormalities were accentuated, creating an almost lunar appearance (Fig. 1B). NBI-targeted biopsy specimens revealed findings consistent with chronic active CGD-associated colitis. Based on reports of the successful use of oral 5-aminosalicylic acid compounds in CGD-associated colitis,4 the patient was started on oral mesalamine and a prednisone taper was initiated.
FIGURE 1.
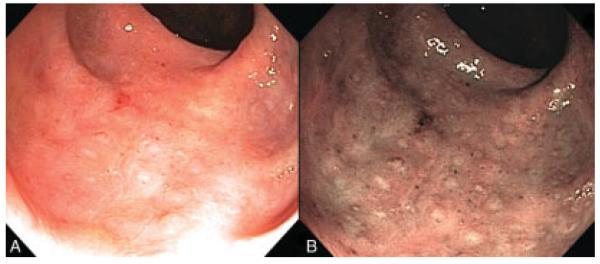
Rectal CGD seen under white light (A) and under NBI (B).
In a review of the records of 140 patients with CGD at the National Institutes of Health, GI involvement was reported in 46 (32.8%) of the patients.5 Colonic involvement occurred in 30 (65%) of these and was described as either granulomatous or ulcerative. All patients with colonic involvement were treated with steroids and antibiotics, and many received interferon-γ. While most patients responded to therapy, symptomatic relapses were common after reduction or cessation of therapy, and 2 patients required surgical intervention.
In summary, CGD frequently causes an inflammatory bowel disease with features seen in both ulcerative colitis and Crohn’s disease. NBI should be considered during the colonoscopic evaluation of patients with known or suspected CGD, as it may accentuate visualized abnormalities and improve biopsy yield.
REFERENCES
- 1.Sloan J, Cameron C, Maxwell R, et al. Colitis complicating chronic granulomatous disease. A clinicopathological case report. Gut. 1996;38:619–622. doi: 10.1136/gut.38.4.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Isaacs D, Wright V, Shaw D, et al. Chronic granulomatous disease mimicking Crohn’s disease. J Pediatr Gastroenterol Nutr. 1985;4:498–501. doi: 10.1097/00005176-198506000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Huang A, Abbasakoor F, Vaizey C. Gastrointestinal manifestations of chronic granulomatous disease. Colorectal Dis. 2006;8:637–644. doi: 10.1111/j.1463-1318.2006.01030.x. [DOI] [PubMed] [Google Scholar]
- 4.Schäppi M, Smith V, Goldblatt D, et al. Colitis in chronic granulomatous disease. Arch Dis Child. 2001;84:147–151. doi: 10.1136/adc.84.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marciano B, Rosenzweig S, Kleiner D, et al. Gastrointestinal involvement in chronic granulomatous disease. Pediatrics. 2004;114:462–468. doi: 10.1542/peds.114.2.462. [DOI] [PubMed] [Google Scholar]


