Abstract
Objective
To investigate associations between anthropometric measurements and total body fat, abdominal adipose tissue, and cardiovascular disease risk factors in a large biracial sample.
Patients and Methods
This study is limited to cross-sectional analyses of data from participants attending a baseline visit between January 26, 1996, and February 1, 2011. The sample included 2037 individuals aged 18 to 69 years: 488 African American women (24%), 686 white women (34%), 196 African American men (9%), and 667 white men (33%). Anthropometry included weight; hip circumference; waist circumference; waist-hip, waist-height, and weight-height ratios; body adiposity index; and body mass index. Body fat and percentage of fat were measured by dual-energy x-ray absorptiometry, and abdominal visceral and subcutaneous adipose tissue were measured by computed tomography. Bivariate correlations, logistic regression models, and receiver operator characteristic curves were used, and analyses were stratified by sex and race.
Results
In each sex-by-race group, all anthropometric measures were highly correlated with percentage of fat, fat mass, and subcutaneous adipose tissue and moderately correlated with visceral adipose tissue, with the exception of the waist-hip ratio. The odds of having an elevated cardiometabolic risk were increased more than 2-fold per SD increase for most anthropometric variables, and the areas under the curve for each anthropometric measure were significantly greater than 0.5.
Conclusion
Several common anthropometric measures were moderately to highly correlated with total body fat, abdominal fat, and cardiovascular disease risk factors in a biracial sample of women and men. This comprehensive analysis provides evidence of the linkage between simple anthropometric measurements and the purported pathways between adiposity and health.
Abbreviations and Acronyms: AUC, area under the curve; BAI, body adiposity index; BMI, body mass index; CT, computed tomography; CVD, cardiovascular disease; DXA, dual-energy x-ray absorptiometry; HC, hip circumference; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; PCLS, Pennington Center Longitudinal Study; ROC, receiver operating characteristic; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue; WC, waist circumference
Numerous anthropometric measurements and indices have been proposed to assess adiposity in clinical, research, and surveillance settings because they require less expense and expertise than laboratory techniques, such as dual-energy x-ray absorptiometry (DXA), computed tomography (CT), and magnetic resonance imaging. Anthropometric measurements are used as proxies for more direct measurements of total body fat and fat stored in specific body depots, such as the abdomen. Anthropometry can be used to assess body composition as such or to derive some insight into health risks associated with either excess adiposity or specific patterns of adipose tissue distribution. Recently, the body adiposity index (BAI) was posited as a new anthropometric measure to assess health risk using hip circumference (HC) and height,1 and although a relatively new measure, its utility has not been compared with other anthropometric measures. Several studies have examined the associations between anthropometric measurements and total body fat,2,3 depot-specific adiposity,4,5 and health outcomes, such as chronic disease risk factors,6 incident disease,7,8 or mortality.9,10 However, the degree to which different anthropometric measurements are associated with direct measurements of adiposity and chronic disease risk factors has rarely been examined in the same cohort of individuals.
The primary purpose of this study was to investigate the associations among several common anthropometric measurements, including the newly proposed BAI and (1) total body fat, (2) abdominal adipose tissue, and (3) cardiovascular disease (CVD) risk factors in a large biracial sample of men and women. A secondary purpose was to determine the relationship between DXA-determined total body fat and CT-derived abdominal adiposity and CVD risk factors.
Patients and Methods
Study Population
The Pennington Center Longitudinal Study (PCLS) is an ongoing investigation of the associations among obesity, lifestyle factors, and the development of chronic diseases, such as type 2 diabetes mellitus and CVD.11 This study is limited to cross-sectional analyses of data from participants attending a baseline visit between January 26, 1996, and February 1, 2011. The sample consists of 2037 volunteers (488 African American women [24%], 686 white women [34%], 196 African American men [9%], and 667 white men [33%]) between 18 and 69 years of age from a single-center urban recruitment site with a suburban and rural catchment area. Race was self-identified by the participants. Each participant provided written informed consent, and all PCLS procedures were approved by the Pennington Biomedical Research Center institutional review board. All measurements were completed within 60 days of one another.
Anthropometry
Standardized anthropometric measurements were obtained on all participants. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer, and weight was measured to the nearest 0.1 kg using a digital scale after all outer clothing and shoes were removed. Waist circumference (WC) was measured at the midpoint between the inferior border of the ribcage and the superior aspect of the iliac crest using an inelastic measuring tape. Hip circumference was measured to the nearest 0.1 cm at the level of the trochanters. Participants stood relaxed but erect with arms at their side. Waist-hip, waist-height, and weight-height ratios were all calculated as the ratios between their respective components. The BAI was calculated ([hip circumference in centimeters]/[height in meters])1.5−18.1 Body mass index (BMI) was calculated as the weight (in kilograms) divided by the height (in meters squared).
Total Body Fat
Total body fat mass (in kilograms) and percentage of fat were measured by DXA. A QDR4500 whole-body scanner (Hologic, Bedford, MA) was used for 856 participants (42%; from years 2001 to 2011), whereas a QDR2000 scanner (Hologic) was used for 1185 participants (58%; from years 1996 to 2006). A validation study (n=32) was performed to develop regression equations to convert QDR2000 data to the current QDR4500 output.11 For both DXA instruments, a single phantom was used before each day's data collection to confirm calibration.
Abdominal Adipose Tissue
Abdominal visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) areas (in centimeters squared) were measured using CT on a subsample of 225 African American women (25%), 343 white women (38%), 68 African American men (8%), and 264 white men (29%) at the Baton Rouge General Medical Center, Baton Rouge, Louisiana. For the measurement, participants lay in a supine position with arms overhead to obtain a cross-sectional image at the L4-L5 intervertebral space. Three different CT scanners were used for the PCLS: GE High Speed Advantage (1996-2000), GE LightSpeed Plus (2000-2007), and GE LightSpeed VCT (2007-2011) (General Electric Company, Fairfield, CT). Computed tomography scanners were calibrated daily to air. The CT images were transferred to the Pennington Biomedical Research Center for analysis with commercially available software (Analyze; Analyze Direct, Rochester, MN).
CVD Risk Factors
Blood pressure measurements were taken manually using a stethoscope and standard sphygmomanometer or, in some cases, using a validated Omron automatic measuring device. Resting blood pressure measurements were obtained after a 5-minute rest, with the participant in a semirecumbent position in a quiet room. Serum triglycerides, total cholesterol, high-density lipoprotein cholesterol (HDL-C), and glucose were assayed from a 12-hour fasting blood draw with participants refraining from alcohol or vigorous physical activity at least 24 hours before blood withdrawal. Samples were analyzed on a Beckman Coulter Chemistry Analyzer (Beckman Coulter, Brea, CA). Low-density lipoprotein cholesterol (LDL-C) was estimated using the Friedewald equation.12
Elevated Cardiometabolic Health Risk
Elevated cardiometabolic health risk was defined as the presence of 2 or more CVD risk factors. The presence of an elevated risk factor was defined as having high blood pressure, glucose level, and triglyceride level or low HDL-C level based on metabolic syndrome criteria.13 High blood pressure was defined as a systolic blood pressure of 130 mm Hg or higher, a diastolic blood pressure of 85 mm Hg or higher, or reported hypertension. A high glucose level was defined as a fasting glucose level of 100 mg/dL or higher (to convert to mmol/L, multiply by 0.0555) or reported diabetes, and high triglyceride level was defined as 150 mg/dL or higher (to convert to mmol/L, multiply by 0.0113). Low HDL-C level was defined as less than 40 mg/dL for men or less than 50 mg/dL for women (to convert to mmol/L, multiply by 0.0259).
Statistical Analyses
Because of previously found differences in body composition across the sex-by-race groups in the PCLS,11 the present analyses were stratified by sex and race. Associations among anthropometric measurements, measures of body fat, abdominal adipose tissue, and CVD risk factors were explored using Pearson correlations within each sex-by-race group. Logistic regression models were used to compute odds ratios of having elevated cardiometabolic risk per SD of each anthropometric measure. Receiver operating characteristic (ROC) curves were computed to compare the clinical utility of the anthropometric measurements to predict elevated cardiometabolic risk. Data management and analysis were undertaken using SAS version 9.2 statistical software and procedures (SAS Institute Inc, Cary, NC), and SPSS statistical software version 19.0 (IBM, Armonk, NY) was used to perform the ROC analysis.
Results
Sample characteristics are reported in Table 1. The prevalence of elevated risk factors ranged from 7.4% (36 of 488) for high triglyceride level in African American women to 36.6% (244 of 667) for high glucose level in white men. The percentage of participants who had 2 or more cardiometabolic risk factors ranged from 26.0% (51 of 196) in African American men to 37.5% (250 of 667) in white men.
TABLE 1.
| Characteristic | African American womenc (n=488) | White womenc (n=686) | African American menc (n=196) | White menc (n=667) |
|---|---|---|---|---|
| Age (y) | 37.7 (11.7) | 41.7d (12.7) | 32.7e (11.5) | 36.0d,e (13.4) |
| Weight (kg) | 82.5 (17.3) | 76.9d (17.4) | 88.9e (15.4) | 89.1e (15.9) |
| Height (cm) | 163.3 (6.0) | 163.8 (5.9) | 177.7e (7.12) | 178.0e (6.6) |
| Hip circumference (cm) | 109.5 (11.8) | 108.1 (13.4) | 103.0e (9.8) | 104.0e (9.1) |
| Waist circumference (cm) | 90.3 (13.7) | 86.6d (14.4) | 91.6 (13.0) | 95.5d,e (13.9) |
| Waist-hip ratio | 0.82 (0.07) | 0.80d (0.07) | 0.89e (0.07) | 0.92d,e (0.08) |
| Waist-height ratio | 0.55 (0.08) | 0.53d (0.09) | 0.52e (0.07) | 0.54d (0.08) |
| Weight-height ratio (kg/cm) | 0.50 (0.1) | 0.47d (0.10) | 0.50 (0.08) | 0.50e (0.08) |
| BAI | 34.6 (5.8) | 33.6d (6.6) | 25.6e (4.3) | 25.9e (4.2) |
| BMI (kg/m2) | 30.9 (6.1) | 28.7d (6.2) | 28.1e (4.6) | 28.1 (4.7) |
| Percentage of fat | 37.4 (5.9) | 36.9 (7.3) | 20.8e (6.7) | 24.1d,e (6.7) |
| Fat mass (kg) | 31.6 (10.7) | 29.4d (11.5) | 19.3e (8.7) | 22.3d,e (9.6) |
| Total cholesterol (mg/dL) | 190.5 (36.3) | 202.1d (37.7) | 182.1e (32.1) | 191.4d,e (38.9) |
| HDL-C (mg/dL) | 57.3 (13.0) | 56.4 (13.9) | 49.8e (12.2) | 45.3d,e (10.5) |
| LDL-C (mg/dL) | 116.6 (32.4) | 122.3d (32.2) | 114.6 (29.5) | 120.8d (33.8) |
| Glucose (mg/dL) | 97.9 (18.0) | 95.9 (15.5) | 96.8 (15.5) | 99.9d,e (17.8) |
| Triglycerides (mg/dL) | 82.8 (42.5) | 115.8d (65.7) | 88.0 (50.4) | 127.5d,e (79.6) |
| SBP (mm Hg) | 119.1 (13.5) | 115.9d (13.1) | 118.7 (11.1) | 119.8e (12.2) |
| DBP (mm Hg) | 76.7 (8.7) | 73.9d (8.2) | 75.3 (9.0) | 76.8e (8.7) |
| High blood pressure (%)f | 29.9 | 22.6d | 24.5 | 28.0e |
| High glucose (%)g | 32.2 | 25.9d | 30.6 | 36.6e |
| High triglycerides (%)h | 7.4 | 24.5d | 10.7d | 28.8d |
| Low HDL-C (%)i | 29.9 | 36.2d | 25.0d | 32.8d |
| ≥2 Risk factors (%) | 28.5 | 29.0d | 26.0 | 37.5e |
BAI = body adiposity index; BMI = body mass index; DBP = diastolic blood pressure; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; SBP = systolic blood pressure.
SI conversion factors: To convert total, HDL-C, and LDL-C to mmol/L, multiply by 0.0259; to convert glucose to mmol/L, multiply by 0.0555; and to convert triglycerides to mmol/L, multiply by 0.0113.
Mean values for continuous variables are presented as mean (SD), and categorical variables are presented as a percentage of the sample.
P<.05 between races, within sex.
P<.05 between sexes, within race.
High blood pressure was defined as a blood pressure of 130/85 mm Hg or higher or reported hypertension.
High blood glucose level was defined as a glucose level of 100 mg/dL or higher or reported type 2 diabetes mellitus.
High triglyceride level was defined as a triglycerides level of 150 mg/dL or higher.
Low HDL-C was defined as an HDL-C level of less than 40 mg/dL in men and less than 50 mg/dL in women.
In each sex-by-race group, all anthropometric measures were highly correlated with percentage of fat and fat mass, with the exception of the waist-hip ratio, which had a moderate correlation in men and a low correlation in women, and height, which was not correlated with percentage of fat or fat mass (Figure 1). The same pattern was revealed for SAT: in each sex-by-race group, all anthropometric measures were highly correlated with SAT, with the exception of the waist-hip ratio, which had a moderate correlation in men and a low correlation in women, and height, which was not correlated with SAT (Figure 2A). The anthropometric measures were moderately correlated with VAT across sex-by-race groups, with the exception of height, which was not correlated with VAT (Figure 2B). Because height was not correlated with adiposity, it was excluded from the analysis with CVD risk factors. The anthropometric measures were moderately correlated with CVD risk factors across sex-by-race groups (Table 2). Notably, there was a general lack of association between anthropometric measurements and cholesterol, particularly LDL-C, among African American women.
FIGURE 1.
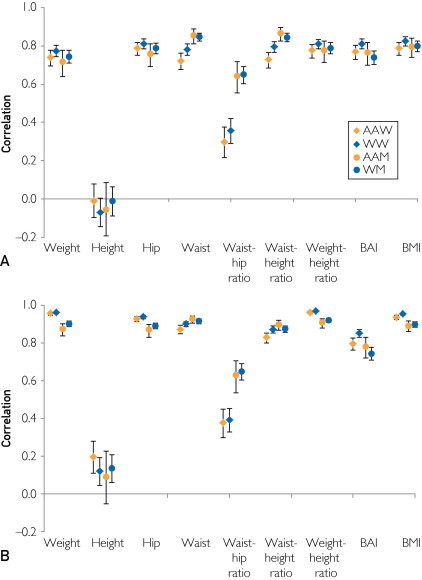
Correlations between anthropometric measures and (A) percentage body fat and (B) total fat mass in each sex-by-race group. Error bars indicate 95% confidence intervals. AAM = African American men; AAW = African American women; BAI = body adiposity index; BMI = body mass index; WM = white men; WW = white women.
FIGURE 2.
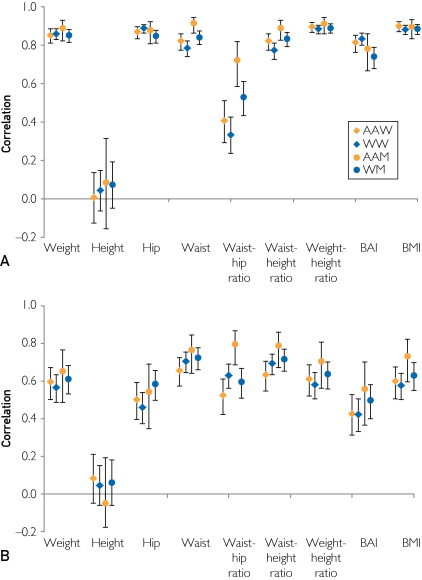
Correlations between anthropometric measures and (A) abdominal subcutaneous adipose tissue and (B) abdominal visceral adipose tissue in each sex-by-race group. Error bars indicate 95% confidence intervals. AAM = African American men; AAW = African American women; BAI = body adiposity index; BMI = body mass index; WM = white men; WW = white women.
TABLE 2.
Correlations Between Anthropometric Measures and Cardiovascular Disease Risk Factors in Each Sex-by-Race Groupa
| Group | Cholesterol | HDL-C | LDL-C | Glucose | Triglycerides | SBP | DBP |
|---|---|---|---|---|---|---|---|
| African American women (n=488) | |||||||
| Weight | 0.05 | −0.20 | 0.09 | 0.24 | 0.20 | 0.24 | 0.24 |
| Hip circumference | 0.04 | −0.15 | 0.07 | 0.18 | 0.14 | 0.22 | 0.19 |
| Waist circumference | 0.09 | −0.23 | 0.13 | 0.32 | 0.26 | 0.28 | 0.27 |
| Waist-hip ratio | 0.12 | −0.21 | 0.14 | 0.34 | 0.29 | 0.22 | 0.23 |
| Waist-height ratio | 0.10 | −0.22 | 0.13 | 0.30 | 0.26 | 0.27 | 0.27 |
| Weight-height ratio | 0.06 | −0.21 | 0.10 | 0.23 | 0.19 | 0.25 | 0.24 |
| BAI | 0.05 | −0.14 | 0.08 | 0.13 | 0.13 | 0.19 | 0.18 |
| BMI | 0.07 | −0.21 | 0.11 | 0.22 | 0.19 | 0.24 | 0.24 |
| White women (n=686) | |||||||
| Weight | 0.19 | −0.31 | 0.24 | 0.26 | 0.30 | 0.20 | 0.28 |
| Hip circumference | 0.20 | −0.26 | 0.23 | 0.19 | 0.26 | 0.21 | 0.27 |
| Waist circumference | 0.23 | −0.32 | 0.25 | 0.32 | 0.39 | 0.23 | 0.29 |
| Waist-hip ratio | 0.16 | −0.23 | 0.15 | 0.33 | 0.36 | 0.13 | 0.16 |
| Waist-height ratio | 0.24 | −0.31 | 0.25 | 0.32 | 0.39 | 0.24 | 0.28 |
| Weight-height ratio | 0.21 | −0.31 | 0.25 | 0.26 | 0.32 | 0.22 | 0.28 |
| BAI | 0.21 | −0.23 | 0.24 | 0.18 | 0.27 | 0.24 | 0.25 |
| BMI | 0.21 | −0.30 | 0.25 | 0.26 | 0.32 | 0.23 | 0.28 |
| African American men (n=196) | |||||||
| Weight | 0.15 | −0.33 | 0.22 | 0.25 | 0.26 | 0.25 | 0.25 |
| Hip circumference | 0.18 | −0.36 | 0.24 | 0.23 | 0.29 | 0.18 | 0.18 |
| Waist circumference | 0.23 | −0.39 | 0.29 | 0.33 | 0.33 | 0.21 | 0.28 |
| Waist-hip ratio | 0.20 | −0.27 | 0.25 | 0.32 | 0.26 | 0.17 | 0.30 |
| Waist-height ratio | 0.24 | −0.38 | 0.31 | 0.32 | 0.33 | 0.18 | 0.26 |
| Weight-height ratio | 0.18 | −0.35 | 0.25 | 0.25 | 0.28 | 0.24 | 0.25 |
| BAI | 0.21 | −0.34 | 0.27 | 0.20 | 0.28 | 0.12 | 0.14 |
| BMI | 0.19 | −0.36 | 0.27 | 0.25 | 0.28 | 0.22 | 0.24 |
| White men (n=667) | |||||||
| Weight | 0.21 | −0.29 | 0.17 | 0.27 | 0.35 | 0.24 | 0.36 |
| Hip circumference | 0.20 | −0.30 | 0.17 | 0.26 | 0.34 | 0.21 | 0.31 |
| Waist circumference | 0.30 | −0.30 | 0.25 | 0.32 | 0.42 | 0.25 | 0.39 |
| Waist-hip ratio | 0.32 | −0.21 | 0.27 | 0.29 | 0.38 | 0.20 | 0.34 |
| Waist-height ratio | 0.31 | −0.29 | 0.26 | 0.32 | 0.43 | 0.24 | 0.36 |
| Weight-height ratio | 0.23 | −0.30 | 0.19 | 0.28 | 0.38 | 0.25 | 0.37 |
| BAI | 0.22 | −0.26 | 0.18 | 0.22 | 0.35 | 0.17 | 0.25 |
| BMI | 0.25 | −0.30 | 0.20 | 0.28 | 0.39 | 0.24 | 0.36 |
Values in bold are significant at the P<.05 level. BAI = body adiposity index; BMI = body mass index; DBP = diastolic blood pressure; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; SBP = systolic blood pressure.
The odds of having elevated cardiometabolic risk were increased more than 2-fold per SD increase for most of the anthropometric variables (Figure 3). The results of sex- and race-specific ROC curves predicting 2 or more elevated CVD risk factors are reported in Table 3. The areas under the curve (AUCs) for each anthropometric measure were significantly greater than 0.5. The BAI exhibited a significantly lower AUC compared with WC in all groups except African American men, and BAI had a significantly lower AUC than BMI among white men. Bivariate correlations among percentage of fat, VAT, and CVD risk factors are presented in Table 4. Although the correlations were low, both percentage of fat and VAT were positively correlated with most risk factors and negatively correlated with HDL-C.
FIGURE 3.
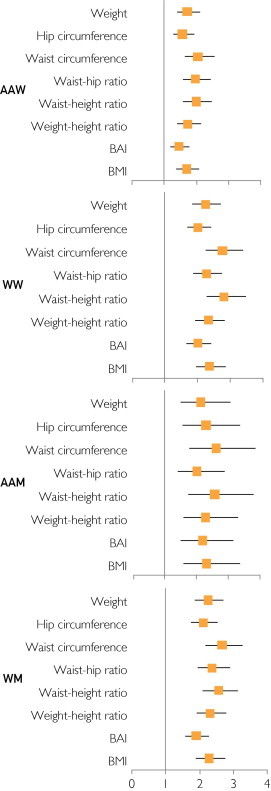
Results of logistic regression analyses predicting 2 or more elevated cardiovascular disease risk factors from anthropometric measurements. The effect size is represented by an odds ratio and corresponding 95% confidence interval. AAM = African American men; AAW = African American women; BAI = body adiposity index; BMI = body mass index; WM = white men; WW = white women.
TABLE 3.
AUCs and 95% CIs for the Anthropometric Measures Predicting 2 or More Cardiovascular Disease Risk Factors in Each Sex-by-Race Group
| Group | AUC (95% CI) |
|---|---|
| African American women | |
| Weight | 0.669 (0.620-0.719) |
| Hip circumference | 0.637 (0.586-0.687) |
| Waist circumference | 0.703 (0.656-0.750) |
| Waist-hip ratio | 0.686 (0.636-0.737) |
| Waist-height ratio | 0.696 (0.648-0.744) |
| Weight-height ratio | 0.667 (0.617-0.716) |
| BAI | 0.612 (0.560-0.664) |
| BMI | 0.661 (0.611-0.711) |
| African American men | |
| Weight | 0.698 (0.617-0.780) |
| Hip circumference | 0.713 (0.633-0.793) |
| Waist circumference | 0.746 (0.674-0.819) |
| Waist-hip ratio | 0.690 (0.611-0.769) |
| Waist-height ratio | 0.745 (0.672-0.817) |
| Weight-height ratio | 0.711 (0.628-0.794) |
| BAI | 0.696 (0.611-0.781) |
| BMI | 0.711 (0.626-0.797) |
| White women | |
| Weight | 0.719 (0.678-0.761) |
| Hip circumference | 0.692 (0.650-0.735) |
| Waist circumference | 0.764 (0.725-0.802) |
| Waist-hip ratio | 0.713 (0.671-0.755) |
| Waist-height ratio | 0.767 (0.729-0.805) |
| Weight-height ratio | 0.728 (0.687-0.768) |
| BAI | 0.689 (0.646-0.731) |
| BMI | 0.730 (0.690-0.770) |
| White men | |
| Weight | 0.713 (0.672-0.754) |
| Hip circumference | 0.701 (0.661-0.742) |
| Waist circumference | 0.746 (0.707-0.784) |
| Waist-hip ratio | 0.719 (0.679-0.759) |
| Waist-height ratio | 0.740 (0.701-0.778) |
| Weight-height ratio | 0.723 (0.683-0.763) |
| BAI | 0.678 (0.637-0.719) |
| BMI | 0.720 (0.680-0.760) |
AUC = area under the curve; BAI = body adiposity index; BMI = body mass index; CI = confidence interval.
TABLE 4.
Correlations Among Percentage of Fat, VAT, and CVD Risk Factors in Each Sex-by-Race Groupa
| Group | Cholesterol | HDL-C | LDL-C | Glucose | Triglycerides | SBP | DBP |
|---|---|---|---|---|---|---|---|
| African American women (n=225) | |||||||
| Percentage of fat | 0.09 | −0.08 | 0.09 | 0.15 | 0.20 | 0.16 | 0.15 |
| VAT | 0.14 | −0.20 | 0.14 | 0.41 | 0.40 | 0.30 | 0.21 |
| White women (n=343) | |||||||
| Percentage of fat | 0.20 | −0.20 | 0.22 | 0.21 | 0.24 | 0.02 | 0.08 |
| VAT | 0.24 | −0.29 | 0.21 | 0.37 | 0.45 | 0.22 | 0.21 |
| African American men (n=68) | |||||||
| Percentage of fat | 0.21 | −0.39 | 0.27 | 0.35 | 0.34 | 0.22 | 0.51 |
| VAT | 0.14 | −0.29 | 0.27 | 0.58 | 0.36 | 0.22 | 0.41 |
| White men (n=264) | |||||||
| Percentage of fat | 0.27 | −0.17 | 0.21 | 0.22 | 0.34 | 0.19 | 0.30 |
| VAT | 0.24 | −0.25 | 0.14 | 0.35 | 0.48 | 0.30 | 0.38 |
CVD = cardiovascular disease; DBP = diastolic blood pressure; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; SBP = systolic blood pressure; VAT = visceral fat.
Values in bold are significant at the P<.05 level.
Discussion
The present study simultaneously compared the ability of several popular anthropometric measurements to predict total body fat, CT-measured abdominal fat, and CVD risk factors in a large biracial sample of men and women. Each anthropometric measure exhibited moderate to high correlations with adiposity and CVD risk factors, and all variables were significant predictors of elevated cardiometabolic risk. Prior studies have suggested the use of one anthropometric measure over another. For example, BMI predicts fat mass14 and mortality10; WC predicts abdominal visceral adiposity,15 CVD risk factors,16 and mortality9; and BAI predicts percentage of fat.1 The present findings suggest that all anthropometric measurements performed similarly and consistently in estimating adiposity and CVD risk and the slight differences in correlations observed may not have clinical relevance or implications for health.
Because DXA and other imaging methods are not readily available in most epidemiological studies, finding a clinical measurement that captures general adiposity is important. It has been previously shown that BMI and BAI perform similarly when estimating percentage of fat.17 The present analyses indicate that weight, HC, WC, waist-height ratio, weight-height ratio, BAI, and BMI may be interchangeable measures for fat mass and percentage of fat because each was highly correlated with both fat mass (0.75-0.96) and percentage of fat (0.72-0.87) over all of the sex-by-race groups. Waist-hip ratio, however, was only moderately correlated with fat mass (0.38-0.65) and percentage of fat (0.30-0.65). Because waist-hip ratio is a measure of fat distribution, reflecting whether fat is deposited as an android (at trunk) or a gynoid (at the gluteofemoral region) pattern, it does not appear to adequately capture total fat mass.
Estimating depot-specific adipose tissue is also important because VAT and SAT may convey unique health risks.18 In the present study, each anthropometric measure was highly correlated with SAT, with the exception of waist-hip ratio. Most anthropometric measurements were only moderately or weakly correlated with VAT, with the strongest associations emerging for WC (0.61-0.71) and waist-height ratio (0.59-0.74). Waist-height ratio has previously shown the highest correlation (0.83) with intra-abdominal fat compared with WC, waist-hip ratio, or BMI.19 The present findings align with those in a prior study by Rankinen and colleagues,15 who compared the correlations between BMI, waist, and waist-hip ratio and visceral adiposity. In their study, all anthropometric measures performed moderately well in men (0.74-0.82), whereas the waist-hip ratio (0.39-0.49) was lower in women compared with BMI and WC (0.69-0.81). A robust anthropometric measure that reflects the deleterious effects of fat stored in the abdomen is needed. Although WC is often proposed as this measure because it has the strongest correlation with VAT, WC is actually a better indicator of total body fat mass (0.87-0.93). Future research is warranted to find a clinical measure that is highly correlated with VAT and SAT in a manner that takes into account the potential confounding effect of total adiposity.
Total and depot-specific fat, especially at excess levels, is used to predict health risk. Nearly all anthropometric measurements in the present study demonstrated low to moderate correlations with each CVD risk factor, but HC and BAI demonstrated no association with some risk factors. Of importance, differences among anthropometric measurements in associations with cardiometabolic risk were small. A previous study also found small differences among adiposity measures in relation to metabolic risk factors, indicating that although WC and waist-height ratio had higher associations, the abdominal and general adiposity measures can be considered equivalent.6
There were noticeably lower correlations between height and the measures of adiposity (Figure 1 and Figure 2) compared with the other anthropometric measurements when separated by sex. When stratified by sex, controlling for height is unnecessary because there is little or no correlation between height and adiposity. However, when the group is taken as a whole, height exhibits a negative correlation with percentage of fat (−0.54 in our data), which is not surprising because men tend to be taller with less body fat and women tend to be shorter with more body fat, as confirmed in the present study. The newly proposed BAI used height in the equation due to the moderate correlation (−0.52) between height and percentage of fat, which was the second highest correlation from a single measure when both sexes were analyzed together.1 It is unknown what the sex-specific correlations with height were in that study and how strong the confounding effect resulting from pooling both sexes was.
An underlying principle of using anthropometric measurements in a clinical setting is that they aim to reflect body fat, which in turn can be used to assess health risk. Yet for women, the present data indicated slightly lower and less consistent correlations between DXA-measured percentage of fat and CVD risk factors than between VAT or WC, for example, and CVD risk factors. In men, VAT was correlated with CVD risk factors, including glucose in both African American and white men and HDL-C level, triglyceride level, and blood pressure in white men. A prior investigation of body composition and health risk found that percentage of fat did not perform better than BMI or WC in predicting metabolic risk.6 The lack of relationship between BAI and the risk factors is particularly novel because the BAI has only recently been proposed as a new index of adiposity. Our current results, combined with previous results,17 show that the BAI is not a better indicator of body fat or health risk than established anthropometric measures. The overarching goal of anthropometric research is to identify the optimal measure that can be used for accurate identification and surveillance of adverse health outcomes. For this reason, the value of having an anthropometric measure or index that is related to percentage of fat alone must be questioned unless it can also be related to health outcomes or mortality. A circumspect approach may be to use BMI due to the large accumulation of data, which can be used for comparison and reference purposes, or to use WC as a single measure to assess the relationship between adiposity and cardiovascular health.
A strength of this study is the large biracial sample that allowed for any sex and race differences to be highlighted. A limitation when comparing anthropometric measurements with image-based adiposity measures is the site of measurement. Although standard clinical procedures were used in the present study, the site of measurement for WC, for example, and the location of an imaging section can affect the association between anthropometry and VAT or SAT.20 However, a systematic review of 120 studies revealed that measurement site of WC does not appear to affect its association with CVD, diabetes, or mortality risk.21 A further limitation of the present study was that information on participants' medications, such as those used to treat hyperlipidemia, was not available. Another weakness of this study is the temporal dispersion of the baseline visits of 15 years because population health changes have occurred during this period. For instance, the use of lipid-lowering medications has increased during this period, and thus this cohort's use of medications might alter the associations between anthropometry and biochemical CVD risk factors. This study relied on volunteers at a research clinic, and these results should be replicated using representative population samples to determine the generalizability of the results to the wider population.
Conclusion
In this study, several common anthropometric measures were moderately to highly and equally correlated with total body fat, CT-measured abdominal fat, and CVD risk factors in a sample of African American and white women and men. This comprehensive analysis provides evidence of the linkage between simple anthropometric measurements and the purported pathways between adiposity and health.
Acknowledgments
We gratefully acknowledge the contributions of Emily F. Mire, MS, and Connie D. Murla, BS, for data management and the many clinical scientists and staff of the Pennington Biomedical Research Center who have contributed data to the PCLS, particularly Donna H. Ryan, MD, Eric Ravussin, PhD, Frank L. Greenway, MD, Corby K. Martin, PhD, and George A. Bray, MD. We also acknowledge Jennifer Rood for her supervision of the chemistry analysis and Julia W. St Amant, RT (R), for her expert supervision of the CT acquisition and for the analysis of most of the CT data reported herein.
Footnotes
Grant Support: This research was supported by the Pennington Biomedical Research Center. Dr Heymsfield is funded, in part, by the George A. Bray, Jr. Endowed Super Chair in Nutrition; Dr Bouchard is funded, in part, by the John W. Barton, Sr. Chair in Genetics and Nutrition; and Dr Katzmarzyk is supported, in part, by the Louisiana Public Facilities Authority Endowed Chair in Nutrition. The PCLS is registered at ClinicalTrials.gov (identifier NCT00959270).
References
- 1.Bergman R.N., Stefanovski D., Buchanan T.A. A better index of body adiposity. Obesity (Silver Spring) 2011;19(5):1083–1089. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deurenberg P., Yap M., van Staveren W.A. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22(12):1164–1171. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 3.Smalley K.J., Knerr A.N., Kendrick Z.V., Colliver J.A., Owen O.E. Reassessment of body mass indices. Am J Clin Nutr. 1990;52(3):405–408. doi: 10.1093/ajcn/52.3.405. [DOI] [PubMed] [Google Scholar]
- 4.Després J.P., Prud'homme D., Pouliot M.C., Tremblay A., Bouchard C. Estimation of deep abdominal adipose-tissue accumulation from simple anthropometric measurements in men. Am J Clin Nutr. 1991;54(3):471–477. doi: 10.1093/ajcn/54.3.471. [DOI] [PubMed] [Google Scholar]
- 5.Bonora E., Micciolo R., Ghiatas A.A. Is it possible to derive a reliable estimate of human visceral and subcutaneous abdominal adipose tissue from simple anthropometric measurements? Metabolism. 1995;44(12):1617–1625. doi: 10.1016/0026-0495(95)90084-5. [DOI] [PubMed] [Google Scholar]
- 6.Bosy-Westphal A., Geisler C., Onur S. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes (Lond) 2006;30(3):475–483. doi: 10.1038/sj.ijo.0803144. [DOI] [PubMed] [Google Scholar]
- 7.Browning L.M., Hsieh S.D., Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev. 2010;23(2):247–269. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- 8.Emerging Risk Factors Collaboration Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leitzmann M.F., Moore S.C., Koster A. Waist circumference as compared with body-mass index in predicting mortality from specific causes. PLoS ONE. 2011;6(4):e18582. doi: 10.1371/journal.pone.0018582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calle E.E., Thun M.J., Petrelli J.M., Rodriguez C., Heath C.W., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 11.Katzmarzyk P.T., Bray G.A., Greenway F.L. Racial differences in abdominal depot-specific adiposity in white and African American adults. Am J Clin Nutr. 2010;91(1):7–15. doi: 10.3945/ajcn.2009.28136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedewald W.T., Levy R.I., Fredrickson D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 13.Grundy S.M., Cleeman J.I., Daniels S.R. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 14.Bouchard C. BMI, fat mass, abdominal adiposity and visceral fat: where is the 'beef'? Int J Obes (Lond) 2007;31(10):1552–1553. doi: 10.1038/sj.ijo.0803653. [DOI] [PubMed] [Google Scholar]
- 15.Rankinen T., Kim S.Y., Perusse L., Despres J.P., Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes Relat Metab Disord. 1999;23(8):801–809. doi: 10.1038/sj.ijo.0800929. [DOI] [PubMed] [Google Scholar]
- 16.Dobbelsteyn C.J., Joffres M.R., MacLean D.R., Flowerdew G. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors: The Canadian Heart Health Surveys. Int J Obes Relat Metab Disord. 2001;25(5):652–661. doi: 10.1038/sj.ijo.0801582. [DOI] [PubMed] [Google Scholar]
- 17.Barreira T.V., Harrington D.M., Staiano A.E., Heymsfield S.B., Katzmarzyk P.T. Body adiposity index, body mass index, and body fat in white and black adults. JAMA. 2011;306(8):828–830. doi: 10.1001/jama.2011.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith S.R., Lovejoy J.C., Greenway F. Contributions of total body fat, abdominal subcutaneous adipose tissue compartments, and visceral adipose tissue to the metabolic complications of obesity. Metabolism. 2001;50(4):425–435. doi: 10.1053/meta.2001.21693. [DOI] [PubMed] [Google Scholar]
- 19.Ashwell M., Cole T.J., Dixon A.K. Ratio of waist circumference to height is strong predictor of intra-abdominal fat. BMJ. 1996;313(7056):559–560. doi: 10.1136/bmj.313.7056.559d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross R., Shaw K.D., Rissanen J., Martel Y., de Guise J., Avruch L. Sex differences in lean and adipose tissue distribution by magnetic resonance imaging: anthropometric relationships. Am J Clin Nutr. 1994;59(6):1277–1285. doi: 10.1093/ajcn/59.6.1277. [DOI] [PubMed] [Google Scholar]
- 21.Ross R., Berentzen T., Bradshaw A.J. Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obes Rev. 2008;9(4):312–325. doi: 10.1111/j.1467-789X.2007.00411.x. [DOI] [PubMed] [Google Scholar]


