Abstract
Background
The cumulative effect of solar ultraviolet (UV) radiation is responsible for the worldwide increase in non-melanoma skin cancer, a category that includes squamous cell carcinoma and its precursors (the actinic keratoses) as well as basal-cell carcinoma. Non-melanoma skin cancer is the most common type of cancer in areas of the world with a light-skinned population. The occupational exposure to UV radiation is high in many outdoor occupations; recent studies suggest that persons working in such occupations are more likely to develop non-melanoma skin cancer.
Methods
On the basis of a selective review of the literature, we present the current state of knowledge about occupational and non-occupational UV exposure and the findings of meta-analyses on the association of outdoor activity with non-melanoma skin cancer. We also give an overview of the current recommendations for prevention and for medicolegal assessment.
Results
Recent meta-analyses have consistently documented a significantly higher risk of squamous cell carcinoma of the skin among persons who work outdoors (odds ratio [OR] 1.77, 95% confidence interval [CI] 1.40–2.22, p<0.001). There is also evidence for an elevated risk of basal-cell carcinoma (OR 1.43, 95% CI 1.23–1.66, p = 0.0001), but the effect is of lesser magnitude and the study findings are not as uniform.
Conclusion
The association of occupational exposure to solar UV radiation with squamous cell carcinoma, including actinic keratosis, has been conclusively demonstrated. It follows that, in Germany, suspected non-melanoma skin cancer in persons with high occupational exposure to UV radiation should be reported as an occupational disease under § 9, paragraph 2 of the Seventh Book of the German Social Code (Sozialgesetzbuch, SGB VII). Preventive measures are urgently needed for persons with high occupational exposure to UV radiation.
Cutaneous squamous cell carcinomas and their precursor lesions, actinic keratoses, as well as basal cell carcinomas, are described as non-melanoma skin cancer (NMSC). These disorders are among the commonest forms of cancer in Western countries with an incidence of around 100 per 100 000 individuals in Europe (1, e1, e2). They are called NMSC or “white skin cancer” to distinguish them from melanoma or “black skin cancer”.
Most often affected are those with pale skin, especially light-sensitive individuals with Fitzpatrick skin types I and II (1, 2, e3).
There are no exact data from German-speaking countries on the incidence of actinic keratosis, also known as squamous cell carcinoma in situ, but studies from Great Britain show a prevalence of actinic keratoses in patients over 70 years of age of 34% in men and 18% in women (e4). The higher prevalence in men is partially explained by a greater exposure to sun, in part without protection, during the performance of outdoor work (e5).
In many work situations employees are exposed to natural UV radiation, often in significant (or considerable) amounts (3, 4). UV radiation is the single most important cause of squamous cell carcinoma and its precursors, as well as of basal cell carcinoma (e6).
UV-induced skin cancer is not yet recognized in Germany as an occupational disease in accordance with the Ordinance on Occupational Diseases (BKV, Berufkrankheitsverordnung) (5). There is active discussion at the present time about adding such diseases—specifically cutaneous squamous cell carcinoma and its precursors—to the list of recognized occupational diseases (Attachment 1 to the BKV). Until this is finalized, cutaneous malignancies caused by UV exposure can be designated as “quasi occupational diseases” under § 9, paragraph 2 of the Seventh Book of the German Social Code (Sozialgesetzbuch, SGB VII). A document known as the “Bamberger Code of Practice—Part 2” prepared by the Task Force for Occupational and Environmental Dermatology (ABD, Arbeitsgemeinschaft für Berufs- und Unweltdermatologie) and the German Social Accident Insurance (DGUV, Deutsche gesetzliche Unfallversicherung) provides guidance on assessing the causality and determining pension liability when the earning capacity has been reduced (6).
The goal of this review is to detail the role and relative importance of workplace factors in the development of squamous cell carcinoma and its precursors, as well as to update information on the quantification of UV exposure as well as the relation between occupational and recreational UV exposure. In addition, the current status of workplace protective measures, prevention and occupational disease evaluation is reviewed.
Methods
The epidemiologic evidence is derived from meta-analyses (7– 9) of the relationship between occupational solar UV exposure and squamous cell carcinoma (7, 8) or basal cell carcinoma, respectively (9). The systematic reviews were carried out according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group checklist (e7). The literature search was performed in MEDLINE (PubMed) using various groupings of MeSH terms for relevant key words (Meta-analyses [7 – 9]):
For study type: “risk“ OR “incidence“ OR “epidemiologic studies“ AND “carcinoma, squamous cell” OR “carcinoma, basal cell” OR “skin cancer” OR “skin neoplasm”.
For UV radiation exposure: “sunlight” OR “ultraviolet rays” OR “ultraviolet light”.
For work-related exposure: “occupational” OR “occupation” OR “outdoor work” OR “work” OR “workplace”.
In addition, the current dermatology and occupational dermatology guidelines and recommendations as well as new legal exposure standards and comparative dosimetry studies on UV exposure were all reviewed.
UV-induced cutaneous reactions and tumor induction
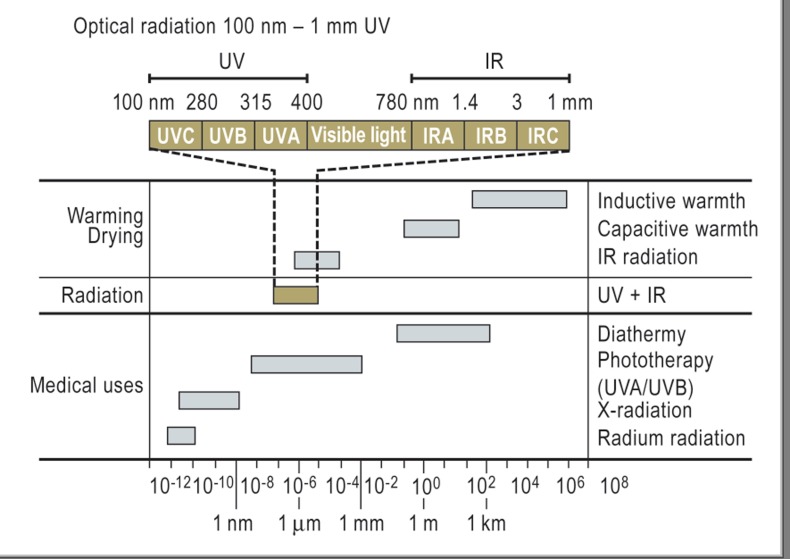
Ultraviolet radiation belongs to the group of optical radiation (wavelengths 100 nm to 1 mm). UV radiation falls in the range between 100 nm and 400 nm and is divided into UVC, UVB and UVA depending on wavelength (Figure 1). Because of the ozone layer, only UVA and UVB reach the earth’s surface; 95% of the natural UV radiation is in the UVA range. The biological reactions induced by UV radiation are complex and can only be touched upon here (review [e8]). Because of the absorption spectrum of the skin, UVA—even though it has less energy than UVB—penetrates deeper and causes not only epidermal damage but also dermal changes (Figure 2, Table). Nonetheless UVB has the most carcinogenic effect. UVA enhances the carcinogenic effect through immunosuppression (10) and by inducing the formation of reactive oxygen species (ROS). These in turn damage deoxyribonucleic acid (DNA), cell membranes and enzymes. The end result is damage to the epidermal keratinocytes and the dermal connective tissue (Figure 2) (review [e9].
Figure 1.
Spectrum of electromagnetic radiation; UV, ultraviolet; IR, infrared
Figure 2.
Cutaneous consequences of acute and chronic excessive UV exposure
Table. Benign clinical symptoms of chronic light damage (modified from Yaar 2007 [e9]—a selection).
| Benign clinical symptoms | Changes in the epidermis and dermis, especially in areas of maximum exposure* |
| Dry skin | Thickening of the skin barrier and changes in the epidermal proliferation rate |
Pigmentary changes:
|
Both increase and decrease in epidermal melanocytes, increase in dermal melanophages |
| Changes in the connective tissue – wrinkles and elastosis | Changes in the connective tissue, especially collagen and elastic fibers |
| Telangiectases Purpura (easy bruising) | Proliferation of small vessels often with atrophic walls, extravasation of erythrocytes and perivascular inflammation |
| Comedones (Favre-Racouchot disease) and sebaceous gland hyperplasia | Dilation and cornification of the superficial component of the sebaceous follicle, proliferation of sebaceous glands |
*Areas of maximum exposure: head and scalp (including helices, lower lip), décolleté, shoulders, backs of hands, forearms
The negative effects of UV radiation on the skin depend on the type, duration and intensity of the UV exposure and can lead to acute erythema (sunburn) or with cumulative exposure to the clinical picture of chronic actinic damage (extrinsic photoaging) (clinical symptoms see Table, Figure 2). Although there are various international methods to grade the severity of light damage (review [e11]), reliable data on the sensitivity and specificity and the role of certain markers such as solar elastosis are not available (11, 12). Exact dose-effect relationships based on spectrum and source of the UV radiation are not established for humans (13).
Squamous cell carcinoma and basal cell carcinoma secondary to occupational UV exposure
Type of tumor and form of UV exposure
There is active discussion currently on the relationship between occupational UV exposure and non-melanoma skin cancer (basal cell carcinoma and squamous cell carcinoma including precursor lesions). Although the development of some types of melanoma shows a certain dependence on UV exposure (14), there is insufficient data on occupational exposure so that at this time melanomas are not under consideration as tumors induced by occupational UV exposure.
The age-adjusted incidence of basal cell carcinoma in Germany is estimated as 80 new cases per 100 000 individuals (2, e6, e10). This locally destructive tumor does not metastasize and is usually surgically removed. It appears most often in body regions with marked UV exposure (see areas of marked exposure, Table), but also can occur on non-exposed areas (for example, retroauricular) so that a direct relationship to UV exposure is not regularly found in exposure studies (1, 15).
Squamous cell carcinoma has an age-adjusted incidence of 29 new cases per 100 000 individuals (1, e2, e10); tumors grow in a destructive way and can metastasize. Both squamous cell carcinomas and actinic keratoses, which are limited to the epidermis (carcinomata in situ), appear almost exclusively in areas with UV exposure, especially on the head and neck or on the décolleté, arms, backs of hands, and the vermilion of the lip (transitional epithelium). The transition from actinic keratosis to invasive squamous cell carcinoma is often difficult to establish (e11); thus the presence of actinic keratoses is an indication for therapy (16).
Exposure to UV radiation is the most important causative exogenous factor in the development of cutaneous squamous cell carcinoma (1). Other known exogenous factors include arsenic, tar and other carcinogens as well as ionizing radiation today play a lesser role in the development of skin cancer (e12).
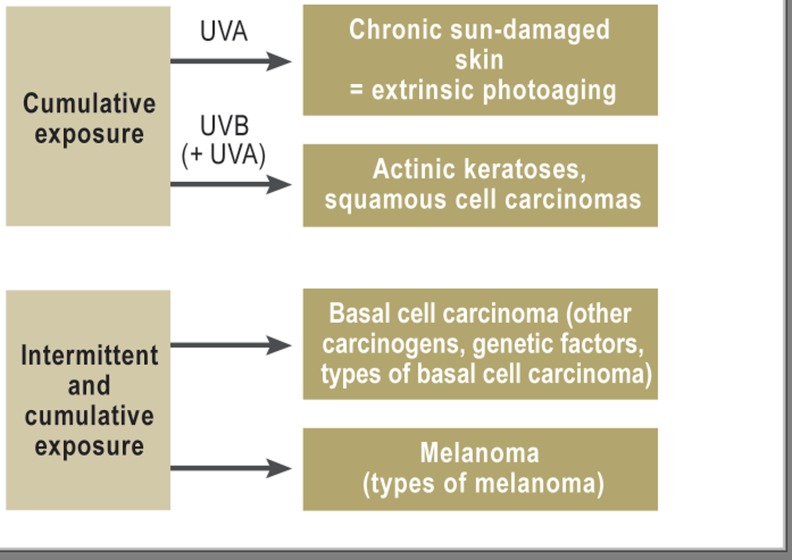
The currently accepted standard when describing UV exposure is to distinguish between cumulative continuous, intermittent, and mixed exposure patterns as well as identifying the peaks of exposure with resultant erythema (sunburns) (Figure 3).
Figure 3.
UV-induced skin damage and skin cancer
The relationship between UV exposure and cutaneous malignancies is probably different for the various tumor types. Squamous cell carcinoma generally develops following years of cumulative UV exposure. Here the increased risk following years of exposure is most easily identified (review [e1]. In addition, there is a clear correlation with the latitude at which one lives. For basal cell carcinoma, additional factors such as the intensity of sun exposure in childhood and adolescence may be relevant (2).
Epidemiology
Recent epidemiological studies (review [7, 8, e13]) show that cumulative occupational exposure leads to an increased risk for outdoor workers. The meta-analyses (7, 8) demonstrate that the published epidemiologic evidence consistently indicates a relevantly increased risk (pooled odds ratio of 1.77, 95% confidence interval 1.40–2.22 [p<0.001, variance = 0.131]) for the development of squamous cell carcinomas in individuals with high occupational UV exposure (outdoor workers). In this selective review, a total of 18 studies (6 cohort studies and 12 case-control studies) were identified that studied the relationship between occupational UV exposure and the risk of squamous cell carcinoma.
Sixteen studies describe a positive relationship between occupational UV exposure and the development of squamous cell carcinoma. The relationship was statistically significant in 12 studies. Occupational exposure was assessed differently in the various studies: Typical outdoor workers (farmers, foresters, construction workers, sailors) were compared with control groups consisting of either individuals who worked indoors with relatively little occupational UV exposure or else to the general population. Although the association was probably underestimated in some studies due to methodological weaknesses, one can state that the epidemiologic evidence points to an approximate doubling of the risk for squamous cell carcinoma in those individuals with extensive occupational UV exposure.
The evidence from the meta-analysis of the 24 studies (5 cohort and 19 case-control studies) also suggests a significant association between outdoor work and the risk of developing a basal cell carcinoma (pooled odds ratio of 1.43, 95% confidence interval 1.23–1.66 [p = 0.0001) [9]). The study results are less uniform than for squamous cell carcinoma and the effect is less clear (11 studies show a significant positive association, 5 studies show a non-significant increase, and 5 studies even show a non-significant risk reduction).
Dosimetric studies in selected occupational groups
Results from both international and national dosimetric studies are available. Numerous studies from Northern and Central Europe investigate increased UV exposure during outdoor work. In these studies the dose required to induce erythema (Her or erythema dose) is expressed as the SED (Standard Erythema Dose) (see Box) [e14]).
Box. Definitions and terms regarding UV radiation exposure.
Thieden and coworkers (17) showed with dosimetric studies that gardeners in Denmark had a 1.7 fold increased exposure on work days because of their occupation. Other publications have also proven that certain outdoor workers such as farmers, fishermen, policemen and sports teachers have an increased risk of skin cancer because of increased UV exposure (18). Newer more personalized dosimetric studies (3, 19, 20) show that, for example, construction workers have a 4.7-fold increased annual UV exposure compared to indoor workers. A markedly increased exposure can also be shown in mountain guides and ski teachers (21). Based on the work of Knuschke et al. (3) showing that the median estimated reference exposure of the German population as Her(Germany) = 130 SED yearly, then an outdoor worker has a 2- to 3-fold higher UV exposure.
Individual levels of solar UV exposure deviate from the mean depending on the type of outdoor work, the origination of the work place and the recreational activities. The causes of the variation are the duration and intensity of the UV exposure. The intensity varies with the work clothing, time of day, and season, as well as the latitude, elevation and albedo (reflection potential) of the work site.
Occupational disability laws, workplace protection, and prevention
Protection of employees and the current legal situation
The employer is already obligated under the German Occupational Safety and Health Act (Arbeitsschutzgesetz) to help employees avoid or minimize damage from excessive UV exposure through appropriate protective measures. However, there are no legal limits for the amount of exposure to natural UV radiation.
Regarding exposure to artificial UV radiation, since 2006 there has been an exposure limit, as stated in the Guideline 2006/25/EG of the European parliament (radiation Heff 30 J/m2 over 8 hours, see Box); this value for protection of employees from risks related to artificial optical radiation was adopted as German law on 19 July 2010 (22). The limit of exposure to artifical UV radiation was determined to avoid acute skin damage. Delayed effects were not considered in calculating this value.
Primary occupational prevention
Many studies have shown that inadequate sun protection measures are utilized by outdoor workers (review [23]).
UV exposure can be minimized in the workplace with a variety of technical, organizational and personal strategies (24) combined with adequate training (e15, e16). Examples of technical measures include:
the use of awnings
planning of work schedules to reduce work during high midday sun
optimal use of personal protective measures (clothing, hats, sun glasses)
use of sunscreens on uncovered skin surfaces.
Many randomized clinical studies have shown that the prophylactic use of sunscreens reduces the development of skin cancers—especially actinic keratoses and squamous cell carcinomas—but also melanomas (14, e17– e21). A long-term study over 4.5 years (e17) showed that the incidence of squamous cell carcinoma in individuals who used sunscreens was reduced by 40% in comparison to the control group. More recent studies have shown that one must pay very close attention to the amount of sunscreen applied. The solar protection factor is based on the application of 2 mg of sunscreen per cm2 of skin. On average only 0.5 mg/cm2 were applied—leading to an exponential decline in the degree of protection (e22). In addition, most of the chemical sunscreens protect against UVB but only a few provide adequate UVA coverage (for details see [25]).
Sunscreens cannot provide complete UV protection and should not mislead the employee into ignoring the use of physical protective measures (clothing) or reducing the duration of exposure.
Occupational disability laws and disability evaluation
The significantly increased incidence of skin cancer in outdoor workers and the epidemiologically and experimentally proven relationship between UV exposure and skin malignancies show that these disorders can result from occupational UV exposure. Today such diseases are recognized by the occupational disability insurance officials in Germany as “quasi occupational diseases“ according to § 9 paragraph 2 SGB VII.
Every physician, or more specifically every dermatologist in Germany who suspects that a skin cancer is due to occupational UV exposure should report this with an Occupational Disease Notification (Berufskrankheiten (BK)-Anzeige) (Form F6000 of the German Social Accident Insurance) to the responsible worker’s compensation agency. It seems likely that UV-induced squamous cell carcinoma including its precursors will be recognized as new occupational disease in the List of Occupational Diseases (BK-Liste). According to German law, a disorder can only be recognized as an occupational disease under § 9, paragraph 1 SGB VII and then be eligible for compensation if a certain occupational group is exposed to “a markedly higher degree than the rest of the population.”
Since UV exposure is ubiquitous, to determine the cause of a skin malignancy, the relation between occupational UV exposure and that experienced during vacation and recreational activity must be analyzed (12, 13). A multicenter study is currently developing methods to help analyze the non-occupational and occupational UV exposure and the resulting skin damage in individual cases. These instruments should enable a standardized, reproducible quantification of the light damage at sites of occupational and non-occupational exposure. In addition, it must document (primarily through history) the occupational/recreational exposure/damage from UV radiation (11, 12).
The issue of induction of skin cancers through occupational exposure to artifical UV radiation remains open. There are too few epidemiologic studies available to support this assertion.
| Her | Dose of radiation required to induce erythema, which takes into account the different wave lengths of solar radiation with their varying ability to cause erythema. Erythema weighting function ser(λ) after ISO 17166/CIE S 007 | |
| SED | Standard Erythema Dose | |
| Unit of the Her,1 SED = 100 J/m2: | ||
| 1.5–3 SED cause erythema in skin type II: | ||
| 6 SED cause marked erythema | ||
| 10 SED cause painful erythema | ||
| Heff | Effective radiation dose | |
|
||
|
||
| Heff 30 J/m2 in 8 hours | The UV-exposure limit according to national law in order to protect the employee from acute damage from artificial optical radiation in the workplace. | |
Key Messages.
Current studies show that outdoor workers have an increased risk for actinic keratoses and squamous cell carcinomas on skin sites with occupational UV exposure.
There also appears to be an increased risk for basal cell carcinoma—but the study results are less consistent and the effects less dramatic, so that this must remain a subject of further research.
At this time if the treating physician suspects an occupationally induced skin cancer, he or she should prepare an Occupational Disease Notification (BK-Anzeige) according to § 9 paragraph 2 SGB VII.
To insure uniform expertise and recognition of occupational disease, instruments must be developed to compare the doses of occupational and recreational UV exposure, as well as to judge the distribution and severity of sun-damage in occupationally and recreationally exposed skin sites as well as non-exposed sites.
Appropriate prevention measures should be employed to reduce the risk for outdoor workers; these include technical and organizational measures such as using awnings and minimizing midday sun exposure, as well as personal protective measures such as wearing appropriate clothing and headgear, and regularly using sunscreens.
Footnotes
Conflict of interest statement
Prof. Diepgen has received honoraria for advisory roles and lectures from Spirig Pharma and Leo Pharma.
Prof. Fartasch, Prof. Schmitt, and Prof. Drexler declare that no conflicts of interest exist.
References
- 1.Madan V, Lear JT, Szeimies RM. Non-melanoma skin cancer. Lancet. 2010;375:673–685. doi: 10.1016/S0140-6736(09)61196-X. [DOI] [PubMed] [Google Scholar]
- 2.Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer—the role of sunlight. Adv Exp Med Biol. 2008;624:89–103. doi: 10.1007/978-0-387-77574-6_8. [DOI] [PubMed] [Google Scholar]
- 3.Knuschke P, Unverricht I, Ott G, Janssen M. Personenbezogene Messung der UV-Exposition von Arbeitnehmern im Freien. Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. 2007 [Google Scholar]
- 4.Knuschke P, Unverricht I, Aschoff R, Cuevas M, Janssen M, Koch E. Untersuchung des Eigenschutzes der Haut gegen solare UV-Strahlung bei Arbeitnehmern im Freien. Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. 2010 [Google Scholar]
- 5.Blome O, Diepgen TL. Berufskrankheit Nr. 5103 der BKV? Teil 1. Dermatol Beruf Umwelt. 2007;55:167–176. [Google Scholar]
- 6.Diepgen T, Bernhard-Klimt C, Blome O, Brandenburg S, Dienstbach D, Drexler H. Bamberger Merkblatt Teil II. Dermatol Beruf und Umwelt. 2009 [Google Scholar]
- 7.Schmitt J, Diepgen T, Bauer A. Occupational exposure to non-artificial UV-light and non-melanocytic skin cancer - a systematic review concerning a new occupational disease. J Dtsch Dermatol Ges. 2010;8:250–264. doi: 10.1111/j.1610-0387.2009.07260.x. [DOI] [PubMed] [Google Scholar]
- 8.Schmitt J, Seidler A, Diepgen TL, Bauer A. Occupational ultraviolet light exposure increases the risk for the development of cutaneous squamous cell carcinoma: a systematic review and meta-analysis. Br J Dermatol. 2011;164:291–307. doi: 10.1111/j.1365-2133.2010.10118.x. [DOI] [PubMed] [Google Scholar]
- 9.Bauer A, Diepgen TL, Schmitt J. Is occupational solar ultraviolet irradiation a relevant risk factor for basal cell carcinoma? A systematic review and meta-analysis of the epidemiological literature. Br J Dermatol. 2011;165:612–625. doi: 10.1111/j.1365-2133.2011.10425.x. [DOI] [PubMed] [Google Scholar]
- 10.Schwarz T. Ultraviolet radiation–immune response. J Dtsch Dermatol Ges. 2005;3:11–18. doi: 10.1111/j.1610-0387.2005.04393.x. [DOI] [PubMed] [Google Scholar]
- 11.Baillie L, Askew D, Douglas N, Soyer HP. Strategies for assessing the degree of photodamage to skin: a systematic review of the literature. Br J Dermatol. 2011;165:735–742. doi: 10.1111/j.1365-2133.2011.10416.x. [DOI] [PubMed] [Google Scholar]
- 12.Diepgen T, Fartasch M. Instrumente zur Erfassung und Quantifizierung der Lichtschädigung. Dermatol Beruf Umwelt. 2011;59:55–56. [Google Scholar]
- 13.Wolf V, Kiesel J, Drexler H. Instrumente zur Expositionserfassung aus medizinischer Sicht. Dermatol Beruf Umwelt. 2011;59:57–59. [Google Scholar]
- 14.Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011;29:257–263. doi: 10.1200/JCO.2010.28.7078. [DOI] [PubMed] [Google Scholar]
- 15.Downs N, Parisi A. Measurements of the anatomical distribution of erythemal ultraviolet: a study comparing exposure distribution to the site incidence of solar keratoses, basal cell carcinoma and squamous cell carcinoma. Photochem Photobiol Sci. 2009;8:1195–1201. doi: 10.1039/b901741k. [DOI] [PubMed] [Google Scholar]
- 16.Deutsche Dermatologische Gesellschaft. Leitlinie Aktinische Keratose. www.awmf.org/Leitlinien/detail/II/013-041.html last accessed on. 2012. Jun 06,
- 17.Thieden E, Philipsen PA, Heydenreich J, Wulf HC. UV radiation exposure related to age, sex, occupation, and sun behavior based on time-stamped personal dosimeter readings. Arch Dermatol. 2004;140:197–203. doi: 10.1001/archderm.140.2.197. [DOI] [PubMed] [Google Scholar]
- 18.Ramirez C, Federman D, Kirsner RS. Skin cancer as an occupational disease: the effect of ultraviolet and other forms of radiation. Int J Derm. 2005;44:95 100. doi: 10.1111/j.1365-4632.2005.02301.x. [DOI] [PubMed] [Google Scholar]
- 19.Knuschke P, Kuriers M, Koch E, Kuhlisch W, Witte K. Mittlere UV- Expositionen der Bevölkerung. Schlussbericht BMBF- Vorhaben 07/UV-B54C/3. Technische Informationsbibliothek Hannover. 2004 F05B898. [Google Scholar]
- 20.Knuschke P, Janssen M, Ott G. Referenzbasis solarer UV-Expositionen zur Bewertung der Expositionslevel in der Bevölkerung und an Arbeitsplätzen im Freien. In: Kaase H, Serick F, editors. Licht und Gesundheit. Berlin: 2011. pp. 24–29. [Google Scholar]
- 21.Lichte V, Dennenmoser B, Dietz K, et al. Professional risk for skin cancer development in male mountain guides—a cross-sectional study. J Eur Acad Dermatol Venereol. 2010;24:797–804. doi: 10.1111/j.1468-3083.2009.03528.x. [DOI] [PubMed] [Google Scholar]
- 22.Bundesrat. Drucksache 262/10. 2010. Verordnung der Bundesregierung. Verordnung zur Umsetzung der Richtlinie 2006/25/EG zum Schutz der Arbeitnehmer vor Gefährdungen durch künstliche optische Strahlung und zur Änderung von Arbeitsschutzverordnungen. [Google Scholar]
- 23.Kutting B, Drexler H. UV-induced skin cancer at workplace and evidence-based prevention. Int Arch Occup Environ Health. 2010;83:843–854. doi: 10.1007/s00420-010-0532-4. [DOI] [PubMed] [Google Scholar]
- 24.Treier C, Schnauber H, Messinesis St, Hoffmann V, Aliferis K. Schriftreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin FB 903, Baua Dortmund/Berlin; 2000. Bremerhaven: Wirtschaftsverlag NW; 2000. Untersuchung der Außentätigkeit unter unmittelbarer Einwirkung von Sonnenstrahlen. [Google Scholar]
- 25.Elsner P, Holzle E, Diepgen T, et al. Recommendation: daily sun protection in the prevention of chronic UV-induced skin damage. J Dtsch Dermatol Ges. 2007;5:166–173. doi: 10.1111/j.1610-0387.2007.06099.x. [DOI] [PubMed] [Google Scholar]
- e1.Katalinic A, Kunze U, Schafer T. Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig-Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer) Br J Dermatol. 2003;149:1200–1206. doi: 10.1111/j.1365-2133.2003.05554.x. [DOI] [PubMed] [Google Scholar]
- e2.Trakatelli M, Ulrich C, del Marmol V, et al. Epidemiology of nonmelanoma skin cancer (NMSC) in Europe: accurate and comparable data are needed for effective public health monitoring and interventions. Br J Dermatol. 2007;156:1–7. doi: 10.1111/j.1365-2133.2007.07861.x. [DOI] [PubMed] [Google Scholar]
- e3.Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869–871. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- e4.Memon AA, Tomenson JA, Bothwell J, Friedmann PS. Prevalence of solar damage and actinic keratosis in a Merseyside population. Br J Dermatol. 2000;142:1154–1159. doi: 10.1046/j.1365-2133.2000.03541.x. [DOI] [PubMed] [Google Scholar]
- e5.Pukkala E, Martinsen JI, Lynge E, et al. Occupation and cancer - follow-up of 15 million people in five Nordic countries. Acta Oncol. 2009;48:646–790. doi: 10.1080/02841860902913546. [DOI] [PubMed] [Google Scholar]
- e6.Saladi RN, Persaud AN. The causes of skin cancer: a comprehensive review. Drugs Today (Barc.) 2005;41:37–53. doi: 10.1358/dot.2005.41.1.875777. [DOI] [PubMed] [Google Scholar]
- e7.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- e8.Maverakis E, Miyamura Y, Bowen MP, Correa G, Ono Y, Goodarzi H. Light, including ultraviolet. J Autoimmun. 2010;34:247–257. doi: 10.1016/j.jaut.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e9.Yaar M. Lim HW, Hönigsmann H, Hawk JLM, editors. The chronic effects of ultraviolet radiation on the skin: Photoaging Photodermatology. Informa Healthcare USA. 2007:91–106. chapter 7. [Google Scholar]
- e10.Naldi L, Diepgen TL. Lim HW, Hönigsmann H, Hawk JLM, editors. The epidemiology of skin cancer Photoaging. Informa Healthcare. 2007:119–137. [Google Scholar]
- e11.Braakhuis BJ, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH. A genetic explanation of Slaughter’s concept of field cancerization: evidence and clinical implications. Cancer Res. 2003;63:1727–1730. [PubMed] [Google Scholar]
- e12.Gawkrodger DJ. Occupational skin cancers. Occup Med. 2004;54:458–463. doi: 10.1093/occmed/kqh098. [DOI] [PubMed] [Google Scholar]
- e13.Radespiel-Troger M. Berufliche UV-Belastung und Hautkrebs. Zbl Arbeitsmed. 2011;61:112–115. [Google Scholar]
- e14.Kimlin MG, Tenkate TD. Occupational exposure to ultraviolet radiation: the duality dilemma. Rev Environ Health. 2007;22:1–37. doi: 10.1515/reveh.2007.22.1.1. [DOI] [PubMed] [Google Scholar]
- e15.Azizi E, Flint P, Sadetzki S, et al. A graded work site intervention program to improve sun protection and skin cancer awareness in outdoor workers in Israel. Cancer Causes Control. 2000;11:513–521. doi: 10.1023/a:1008970224998. [DOI] [PubMed] [Google Scholar]
- e16.Hall DM, McCarty F, Elliott T, Glanz K. Lifeguards’ sun protection habits and sunburns: association with sun-safe environments and skin cancer prevention program participation. Arch Dermatol. 2009;145:139–144. doi: 10.1001/archdermatol.2008.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e17.Green A, Williams G, Neale R, et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. Lancet. 1999;354:723–729. doi: 10.1016/S0140-6736(98)12168-2. [DOI] [PubMed] [Google Scholar]
- e18.Thompson SC, Jolley D, Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med. 1993;329:1147–1151. doi: 10.1056/NEJM199310143291602. [DOI] [PubMed] [Google Scholar]
- e19.Darlington S, Williams G, Neale R, et al. A randomized controlled trial to assess sunscreen application and beta carotene supplementation in the prevention of solar keratoses. Arch Dermatol. 2003;139:451–455. doi: 10.1001/archderm.139.4.451. [DOI] [PubMed] [Google Scholar]
- e20.van der Pols JC, Williams GM, Pandeya N, et al. Prolonged prevention of squamous cell carcinoma of the skin by regular sunscreen use. Cancer Epidemiol Biomarkers Prev. 2006;15:2546–2548. doi: 10.1158/1055-9965.EPI-06-0352. [DOI] [PubMed] [Google Scholar]
- e21.Green AC, Williams GM. Point: sunscreen use is a safe and effective approach to skin cancer prevention. Cancer Epidemiol Biomarkers Prev. 2007;16:1921–1922. doi: 10.1158/1055-9965.EPI-07-0477. [DOI] [PubMed] [Google Scholar]
- e22.Kim SM, Oh BH, Lee YW, Choe YB, Ahn KJ. The relation between the amount of sunscreen applied and the sun protection factor in Asian skin. J Am Acad Dermatol. 2010;62:218–222. doi: 10.1016/j.jaad.2009.06.047. [DOI] [PubMed] [Google Scholar]