Abstract
Purpose
To describe the clinical and pathological features of a case of hydrogel intraocular lens (IOL) calcification.
Case Report
A 48-year-old man underwent explantation of a single-piece hydrophilic acrylic intraocular lens in his left eye because of decreased visual acuity and milky white opalescence of the IOL. The opacified lens was exchanged uneventfully with a hydrophobic acrylic IOL. Gross examination of the explanted IOL disclosed opacification of the optic and haptics. Full-thickness sections of the lens optic were stained with hematoxylin and eosin (H&E), von Kossa and Gram Tworts’. Microscopic examination of the sections revealed fine and diffuse basophilic granular deposits of variable size within the lens optic parallel to the lens curvature but separated from the surface by a moderately clear zone. The deposits were of high calcium content as evident by dark brown staining with von Kossa. Gram Tworts’ staining disclosed no microorganisms.
Conclusion
This report further contributes to the existing literature on hydrogel IOL calcification.
Keywords: Lenses, Intraocular
INTRODUCTION
Intraocular lens (IOL) calcification is an uncommon complication following cataract surgery. Calcification of ophthalmic devices is considered rare but has been observed in silicone scleral buckles, the intracameral portion of Molteno implants, and IOLs.1,2 Clinical observations of calcification of hydrogel IOLs were first reported in 1987.3 Multiple factors are involved in the pathogenesis of this phenomenon including IOL material, host environment, packageing and surgical instruments such as forcepsrelated impressions.3–5 Although generally considered as a privileged site, the intraocular environment does not preclude calcification. The potential for IOL calcification must be considered when evaluating the long-term biocompatibility of lens material.3 Herein, we present the clinicopathologic features of a case of hydrophilic acrylic IOL calcification with a good visual outcome following uneventful IOL exchange.
CASE REPORT
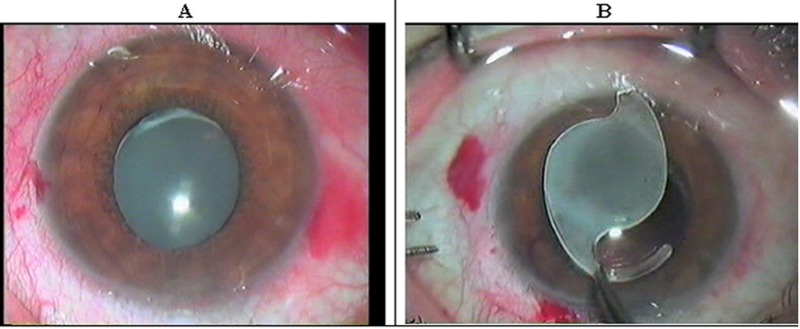
A 48-year-old man underwent uneventful phacoemulsification and implantation of a single piece hydrophilic acrylic posterior chamber IOL (ACRL-C160, Ophthalmed, California, USA) using hydroxypropyl-methylcellulose viscoelastic material (Viscel, Corneal Co. Ltd, France) in his left eye in 2003. One month after surgery, best corrected visual acuity was 20/25 and the IOL was well positioned within the capsular bag. Other examinations were unremarkableand there was no systemic disorder. Four years later, the patient complained of glare sensation and markedly decreased visual acuity in the operated eye down to 20/60. Diffuse and milky opalescence of the IOL was visible on slitlamp biomicroscopy. IOL explantation and exchange with a three-piece hydrophobic acrylic IOL (Acrysof MA60, Alcon Laboratories, Fort Worth, USA) was performed.
The explanted IOL (Fig. 1) underwent microscopic examination at the Eye Bank pathology laboratory. After gross examination, the IOL was bisected; one half was directly stained with von Kossa without any tissue processing and mounted on a slide using DPX mountant. The other half was processed and embedded in a paraffin block. Full-thickness cross sections of the paraffin blocked lens optic were prepared and stained with hematoxylin and eosin (H&E), von Kossa and Gram Tworts’.
Figure 1.
Diffuse milky opalescence of the intraocular lens before (A) and after (B) explantation.
A section of a cornea with band keratopathy and a section from a cornea with confirmed bacterial keratitis were used as positive control slides for von Kossa and Gram Tworts’ staining methods respectively. The stained sections were examined by an Olympus BX40 light microscope with an attached Olympus DP12 camera (Olympus Optical Co, Ltd, Japan).
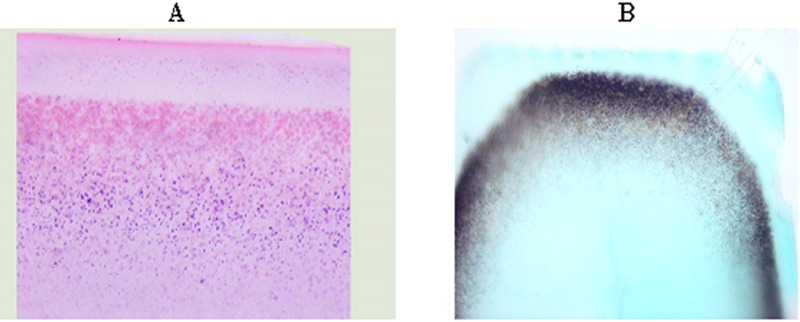
Gross examination of the IOL disclosed opacification of the optic and haptics. Microscopic examination of the H&E-stained sections revealed fine and diffuse basophilic granular deposits of variable size within the lens optic parallel to the lens curvature (Fig. 2A), separated with a moderately clear zone from the optic surface. The deposits were of high calcium content which appeared dark brown with von Kossa staining (Fig. 2B). Gram Tworts’ stained sections were negative for microorganisms. Examination of the non-processed half of the IOL stained with von Kossa also disclosed diffuse dark brown deposits within the haptics and optic.
Figure 2.
(A) Basophilic granular deposits of variable size within the intraocular lens material (Hematoxylin and Eosin, ×400). (B) The calcium-containing deposits appear dark brown with von Kossa staining and are separated by a moderately clear zone from the optic surface (× 400).
DISCUSSION
Delayed calcification of an IOL is a rare multifactorial phenomenon which occurs secondary to both lens material and host environment factors and starts at the surface progressing over time into the lens matrix.3 Based on clinical and microscopic findings of more than 400 explanted IOLs, Neuhann et al6 identified 3 major types of IOL calcification: (1) primary IOL calcification due to a variety of reasons including improper formulation of the polymer, IOL fabrication, faulty packaging, forcepsrelated impressions and certain Viscoelastic substances; (2) secondary calcification which most likely occurs due to an abnormal milieu such as blood-aqueous barrier dysfunction; and (3) pseudocalcification in which other pathology is mistaken for calcification. Since there was no evidence of underlying systemic disease or blood-aqueous barrier dysfunction in the patient presented herein and due to interprettation of pathologic findings based on positivecontrol results for calcium, the IOL calcification may be regarded as a primary phenomenon.
The prevalence of IOL opacification three years after implantation of Hydroview IOLs (Bausch & Lomb, Rochester, USA) was reported to be 14.5% while 21.8% of eyes with opacification were asymptomatic.7 Both early and delayed-onset IOL calcifications have been reported. Bucher and coauthors2 described calcification of an IOL one day after surgery. In another report, IOL calcification occurred 4 to 26 months after cataract surgery.4 The time to symptomatic opacification was 48 months in our patient. Yu et al4,8 reported a maximum of 10 Snellen lines of visual loss (mean loss of 2.8 Snellen lines) in eyes with calcified hydrogel IOLs. Loss of visual acuity in our case was 6 Snellen lines.
The presence of calcium on explanted IOLs can be confirmed by staining with Alizarin red9 and von Kossa.5 The pathologic findings in our case were similar to those reported by Werner et al10 in the form of multiple fine granular deposits of variable size within the lens optics, distributed parallel to anterior and posterior curvatures of the optic with a clear zone beneath the optic surface. Energy dispersive Xray spectroscopy (EDS) on the internal substance of the opacified IOLs and optical coherence tomography (OCT) have recently been reported as new methods for detecting calcification of hydrogel IOLs.11,12 To our knowledge, no microorganism has ever been reported in calcified IOLs.13 In the current study, we also found no organisms with Gram Tworts’ staining.
IOL calcification is an uncommon indication for IOL exchange, with only a few case reports.9,14,15 Meticulous dissection of the IOL from the capsular bag with a viscoelastic material is the key to successful explantation. Intraoperative complications include rupture of the posterior capsule and zonular dehiscence.8 In summary, this report describes the clinicopathologic features of calcification of a hydrophilic acrylic IOL and a successful outcome after IOL exchange.
REFERENCES
- 1.Bucher P. Calcification of an IOGEL 1003 lens. Eur J Implant Refract Surg; Foldable Technology Symposium; 1994. pp. 6–175. [Google Scholar]
- 2.Bucher PJ, Buchi ER, Daicker BC. Dystrophic calcification of an implanted hydroxyethylmetacrylate intraocular lens. Arch Ophthalmol. 1995;113:1431–1435. doi: 10.1001/archopht.1995.01100110091031. [DOI] [PubMed] [Google Scholar]
- 3.Buchen SY, Cunanan CM, Gwon A, Weinschenk JI, Gruber L, Knight PM. Assessing intraocular lens calcification in an animal model. J Cataract Refract Surg. 2001;27:1473–1484. doi: 10.1016/s0886-3350(01)00842-2. [DOI] [PubMed] [Google Scholar]
- 4.Yu AKF, Kwan KYW, Chan DHY, Fong DY. Clinical features of 46 eyes with calcified hydrogel intraocular lenses. J Cataract Refract Surg. 2001;27:1596–1606. doi: 10.1016/s0886-3350(01)01038-0. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi RH, Werner L, Pandey SK, Peng Q, Arthur S, Izak AM, et al. Intraocular lens-related opacifications: in front of, on, within, between, and behind the intraocular lens. In: Stienert RF, editor. Cataract surgery: Technique, Complications, and Management. 2nd ed. Philadelphia: Elsevier Science; 2004. pp. 443–467. [Google Scholar]
- 6.Neuhann IM, Kleinmann G, Apple DJ. A new classification of calcification of intraocular lenses. Ophthalmology. 2008;115:73–79. doi: 10.1016/j.ophtha.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 7.Balasubramaniam C, Goodfellow J, Price N, Kirkpatrick N. Opacification of the Hydroview H60M intraocular lens: total patient recall. J Cataract Refract Surg. 2006;32:944–948. doi: 10.1016/j.jcrs.2006.02.047. [DOI] [PubMed] [Google Scholar]
- 8.Yu AKF, Ng ASY. Complications and clinical outcomes of intraocular lens exchange in patients with calcified hydrogel lenses. J Cataract Refract Surg. 2002;28:1217–1222. doi: 10.1016/s0886-3350(02)01357-3. [DOI] [PubMed] [Google Scholar]
- 9.Apple DJ, Werner L, Escobar-Gomez M, Pandey SK. Deposits on the optical surface of Hydroview intraocular lenses [letter] J Cataract Refract Surg. 2000;26:796–797. doi: 10.1016/s0886-3350(00)00517-4. [DOI] [PubMed] [Google Scholar]
- 10.Werner L, Apple DJ, Kaskaloglu M, Pandey SK. Dense opacification of the optical component of a hydrophilic acrylic intraocular lens: a clinicopathologic analysis of 9 explanted lenses. J Cataract Refract Surg. 2001;27:1485–1492. doi: 10.1016/s0886-3350(01)00841-0. [DOI] [PubMed] [Google Scholar]
- 11.Macky TA, Werner L, Soliman MM, Pandey SK, Izak AM, Apple DJ. Opacification of two hydrophilic acrylic intraocular lenses 3 months after implantation. Ophthalmic Surg Laser Imaging. 2003;34:197–202. [PubMed] [Google Scholar]
- 12.Hatou S, Inoue M, Kurosaka D, Hida YR, Shinoda K, Oguchi Y. Evaluation of calcification of a hydrogel intraocular lens by optical coherence tomography. J Cataract Refract Surg. 2004;30:1590–1592. doi: 10.1016/j.jcrs.2003.11.048. [DOI] [PubMed] [Google Scholar]
- 13.Apple DJ, Rabb MF. Ocular Pathology: clinical applications and self assessment. 6th ed. St Louis: Mosby; 1998. [Google Scholar]
- 14.Yu AKF, Shek TWH. Hydroxyapatite formation on implanted hydrogel intraocular lenses. Arch Ophthalmol. 2001;119:611–614. doi: 10.1001/archopht.119.4.611. [DOI] [PubMed] [Google Scholar]
- 15.Fernando GT, Crayford BB. Visually significant calcification of hydrogel intraocular lenses necessitating explantation. Clin Exp Ophthalmol. 2000;28:280–286. doi: 10.1046/j.1442-9071.2000.00331.x. [DOI] [PubMed] [Google Scholar]