Abstract
Purpose
To compare the astigmatic outcomes of phacoemulsification cataract surgery using temporal versus nasal clear corneal incisions.
Methods
In a clinical trial, consecutive patients with senile cataracts underwent phacoemulsification and implantation of a hydrophobic acrylic foldable intraocular lens through a horizontal clear corneal incision (temporal in right and nasal in left eyes). Outcome measures included keratometric astigmatism and surgically induced astigmatism (SIA) calculated by the vector analysis method using the Holladay-Cravy- Koch formula.
Results
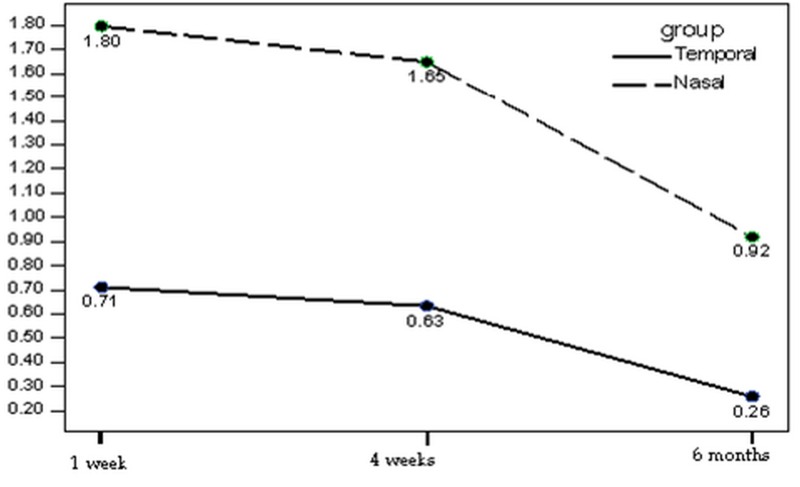
The nasal and temporal groups consisted of 20 eyes each. Mean preoperative keratometric astigmatism was 0.63±0.48 D and 0.38±0.39 D in the temporal and nasal incision groups respectively (P=0.09). Data on 10 eyes in each study group was available for the six-month analysis. Mean keratometric astigmatism was as follows in the temporal and nasal groups respectively: 0.85±0.47 D versus 1.95±0.45 D at 1 week (P<0.001), 0.73±0.46 D versus 1.79±0.55 D at 4 weeks (P<0.001), and 0.63±0.30 D versus 1.05±0.56 D at 6 months (P=0.053) after surgery. SIA at the same follow-up intervals was 0.71±0.20 D versus 1.80±0.22 D (P<0.001), 0.63±0.20 D versus 1.65±0.31 D (P<0.001) and 0.26±0.46 D versus 0.92±0.36 D (P=0.002) in the temporal versus nasal incision groups respectively.
Conclusion
Temporal clear corneal phacoemulsification induces significantly less astigmatism as compared to similar surgery using the nasal approach.
Keywords: Phacoemulsification, Cataract
INTRODUCTION
The two main determinants of the refractive state of the eye following phacoemulsification and intraocular lens implantation (PE+IOL) are IOL power and surgically induced astigmatism (SIA). Factors such as wound location and architecture, and IOL size are important predictors of SIA.1–4 According to numerous studies, temporal clear corneal incisions have been reported to produce minimal SIA5–12 while data on nasal incisions is less comprehensive. Surgeon position and comfort during the procedure is an important issue; most operating tables have not been designed for a surgeon to be positioned at the side of the patient's head for “temporal approach” surgery. For a right-handed surgeon, it might be easier to sit at the head of the operating table (the usual position) and construct the incision temporally in right eyes and nasally in left eyes (vice versa for left-handed surgeons). This study compares the short and intermediate term astigmatic outcomes of temporal versus nasal clear corneal phacoemulsification incisions with the surgeon positioned at the usual location at the head of the operating table.
METHODS
This prospective clinical trial included a consecutive series of patients with senile cataracts scheduled for PE+IOL. Exclusion criteria consisted of previous ocular surgery, presence of corneal pathology, pseudoexfoliation and with-the-rule (WTR) astigmatism exceeding 1 diopter (D). Patients with diabetes mellitus, connective tissue disease and those taking systemic steroids were also excluded.
All procedures were performed at Labbafinejad Medical Center, Tehran, Iran by two right-handed surgeons (MP and SY) using the same technique under retrobulbar anesthesia. The surgeon was positioned at the head of the operating table and used the horizontal meridian to construct the main phacoemulsification incision. A biplanar, 3.2 mm horizontal corneal incision (temporal in right eyes and nasal in left eyes) was constructed at the anterior edge of the limbal vessels. First a half-depth perpendicular groove incision was made using a 15° stab knife (Sharpoint, Surgical Specialties Corp., USA) followed by lamellar dissection 2.0 mm into clear cornea using a disposable 3.2 mm keratome (Sharpoint, Surgical Specialties Corp., USA). After phacoemulsification and cortex removal, a 6 mm hydrophobic acrylic foldable IOL (Alcon Acrysof SA60, Alcon Laboratories Inc. USA) was inserted using an injector system (Monarch, Alcon Laboratories Inc. USA), the anterior chamber was formed and the wound was checked for leakage and left unsutured.
Postoperative examinations were conducted 1, 2, 7 and 28 days, and 6 months after the procedure. Uncorrected visual acuity and bestcorrected visual acuity (BCVA) were measured and keratometry was performed at each followup visit. Main outcome measures included keratometric astigmatism and SIA calculated by the vector analysis formula using the Holladay-Cravy-Koch formula.13
With study power of 90%, a sample size of 13 eyes in each group was calculated to detect an inter-group difference of at least 0.4 D. To compensate for an expected 35% case loss after six months, the sample size was increased to 20 eyes in each group. Data were compared between the two study groups using Mann- Whitney and t-tests with statistical significance set at 5%.
RESULTS
Overall, 40 eyes of 34 consecutive patients with senile cataracts including 18 (53.9%) male and 16 (47.1%) female subjects with mean age of 62.2±7.5 (range 46 to 80) years underwent clear corneal phacoemulsification and intraocular lens implantation. Six subjects underwent bilateral surgery, consequently 20 right and 20 left eyes underwent temporal and nasal phacoemulsification. The two groups were comparable in terms of sex and mean age (P=0.52). Mean preoperative keratometric astigmatism was 0.63±0.48 D in the temporal and 0.38±0.39 D in the nasal group (P=0.09).
Data was available on all enrolled eyes for 1 and 4 week comparisons, but only 10 eyes in either study group were available for the 6 month analysis. Mean keratometric astigmatism 1 week, 4 weeks and 6 months postoperatively was 0.86±0.47 D versus 1.95±0.45 D (P<0.001), 0.73±0.46 D versus 1.79±0.55 D (P<0.001), and 0.63±0.30 D versus 1.05±0.56 D (P=0.053) in the temporal versus nasal groups respectively. The distribution of different types of astigmatism and detailed data on keratometric astigmatism are presented in Table 1.
Table 1.
Types of astigmatism
| Number (%) |
Total number | |||
|---|---|---|---|---|
| WTR | ATR | Neutral | ||
| Preoperative | ||||
| T | 6 (30%) | 10 (50%) | 4 (20%) | 20 |
| N | 8 (40%) | 5 (25%) | 7 (35%) | 20 |
| Postoperative | ||||
| 4 weeks | ||||
| T | 17 (85%) | 3 (15%) | 0 | 20 |
| N | 20 (100%) | 0 | 0 | 20 |
| 6 weeks | ||||
| T | 6 (60%) | 4 (40%) | 0 | 10 |
| N | 8 (80%) | 1 (10%) | 1 (10%) | 10 |
WTR, with-the-rule astigmatism; ATR, against-the-rule astigmatism; T, Temporal group; N, Nasal group.
SIA was 0.71±0.20 D versus 1.80±0.22 D (P<0.001), 0.63±020 D versus 1.65±0.31 D (P<0.001) and 0.26±0.46 D versus 0.92±0.36 D (P=0.002) one week, 4 weeks and 6 months postoperatively (Mann-Whitney test for all comparisons) in the temporal and nasal incision groups respectively (Fig. 1). In both groups the amount of SIA at sixth months was much lower than the initial visit (P<0.001). Despite the significant differences in keratometric and surgically induced astigmatism, BCVA was comparable in the study groups (Table 2).
Figure 1.
Mean surgically induced astigmatism (SIA)
Table 2.
Mean postoperative best-corrected visual acuity (logMAR)
| Mean±Standard deviation (No) |
P value | ||
|---|---|---|---|
| Temporal | Nasal | ||
| 4 weeks | 0.03 ± 0.07 (20) | 0.07 ± 0.16 (20) | 0.63 |
| 6 months | 0.03 ± 0.07 (10) | 0.06 ±0.11 (10) | 0.59 |
DISCUSSION
Horizontally oriented clear corneal incisions (temporal in right and nasal in left eyes) entail certain advantages; they avoid injury to the superior conjunctiva in eyes which may later need glaucoma surgery, the surgical technique is identical for right and left eyes, and the surgeon may be positioned at the head of the operating table in both circumstances. In patients with deep-set eyes the temporal approach in right eyes is advantageous if the surgeon is right-handed; for the left eye, nasal incisions avoid the prominent brow and also minimize the effect of Bell's phenomenon. The reverse conditions apply for left-handed surgeons. Many studies have demonstrated that temporal incisions induce the least amount of astigmatism.7,10,14 In this study we sought to determine whether nasal incisions lead to the same favorable astigmatic outcomes as temporal incisions.
This clinical trial compares two types of incisions lying on the same meridian: temporal incisions in right eyes versus nasal incisions in left eyes. Mean preoperative keratometric astigmatism was slightly higher in the temporal group which was of borderline statistical significance (P=0.09). This potential confounder does not appear to have significantly influenced the results of the study because final astigmatism was greater in the nasal group; furthermore, calculating SIA should have compensated for any baseline difference.
In the current study, SIA one week after phacoemulsification was 0.71 D and 1.80 D with temporal and nasal incisions respectively which is comparable to SIA figures of 0.62 D and 1.55 D for temporal and nasal incisions reported 2 weeks postoperatively by Kohnen and co-workers.8 SIA four weeks after surgery was 0.63 D and 1.65 D for temporal and nasal incisions respectively; Barequet et al5 reported very close figures of 0.74 D and 1.65 D at 6 weeks for temporal and nasal clear corneal incisions. We observed SIA of 0.26 D and 0.92 D six months after surgery for temporal and nasal incisions respectively which is comparable to Kohnen and associates8 figures of 0.47 D and 1.05 D after six months. Prior to surgery only 35% of eyes in our series had mild WTR astigmatism; by the end of the study, 75% of eyes had WTR astigmatism. In comparison, Barequet and associates7 reported 22.5% and 43.8% WTR astigmatism pre and postoperatively.
In our study SIA was significantly and consistently greater in the nasal approach (left eyes) at all visits which is similar to the results reported by Barequet et al5 and Kohnen et al.8 The observed inter-group difference in keratometric astigmatism and SIA diminished at the last visit, however longer follow-up is necessary to determine the behavior of temporal and nasal incisions over time. Explanations for the higher observed SIA in nasal incisions (left eyes) include closer proximity to the optical center of the cornea (the nasal limbus is closer to the visual axis) and that the right-handed surgeon should operate over the bulk of the patient's nose in the nasal approach for left eyes holding the phacoemulsification handpiece at a steeper angle leading to wound distortion and possibly burn.
One of the limitations of the current study was case loss during intermediate follow-up, such that data from only 20 eyes (10 in each group) was available for final analysis. We calculated keratometric astigmatism and SIA in patients who withdrew from the study at 1 and 4 weeks and noted the same pattern as other participants, we also compared the main outcome measures between lost cases and others at 1 and 4 weeks, and found no significant difference (P=0.92 and P=0.46 for keratometric and surgically induced astigmatism, respectively). Therefore it may be assumed that cases lost to follow-up probably have not significantly affected the results of the study.
In conclusion, the results of our study demonstrate that temporal clear corneal incisions seem to induce very low astigmatism and are suitable for astigmatically neutral eyes and those with low preoperative WTR astigmatism. On the other hand nasal clear corneal incisions seem to induce higher amounts of astigmatism and are therefore not suitable for patients with pre-existing WTR astigmatism. In some situations such as pre-existing against the rule astigmatism, the surgically induced astigmatism could be one of the advantages of incisions oriented on the horizontal meridian.
REFERENCES
- 1.Koch DD, Lindstrom RL. Controlling astigmatism in cataract surgery. Semin Ophthalmol. 1992;7:224–233. [Google Scholar]
- 2.Kohnen T. Corneal shape changes and astigmatic aspects of scleral and corneal tunnel incisions. J Cataract Refract Surg. 1997;23:301–302. doi: 10.1016/s0886-3350(97)80168-x. [DOI] [PubMed] [Google Scholar]
- 3.Kohnen T, Koch MJ. Refractive aspects of cataract surgery. Curr Opin Ophthalmol. 1998;9:55–59. doi: 10.1097/00055735-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Koch MJ, Kohnen T. Refractive cataract surgery. Curr Opin Ophthalmol. 1999;10:10–15. doi: 10.1097/00055735-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Shepherd JR. Induced astigmatism in small incision cataract surgery. J Cataract Refract Surg. 1989;15:85–88. doi: 10.1016/s0886-3350(89)80145-2. [DOI] [PubMed] [Google Scholar]
- 6.Gills JP, Sanders DR. Use of small incisions to control induced astigmatism and inflammation following cataract surgery. J Cataract Refract Surg. 1991;17 (Suppl):740–744. doi: 10.1016/s0886-3350(13)80695-5. [DOI] [PubMed] [Google Scholar]
- 7.Roman SJ, Auclin FX, Chong-Sit DA, Ullern MM. Surgically induced astigmatism with superior and temporal incisions in cases of with-the-rule preoperative astigmatism. J Cataract Refract Surg. 1998;24:1636–1641. doi: 10.1016/s0886-3350(98)80356-8. [DOI] [PubMed] [Google Scholar]
- 8.Simsek S, Yasar T, Demirok A, Cinal A, Yilmaz OF. Effect of superior and temporal clear corneal incision on astigmatism after sutureless phacoemulsification. J Cataract Refract Surg. 1998;24:515–518. doi: 10.1016/s0886-3350(98)80294-0. [DOI] [PubMed] [Google Scholar]
- 9.Lyhne N, Krogsager J, Corydon L, Kjeldgaard M. One year follow-up of astigmatism after 40 mm temporal clear corneal and superior scleral incisions. J Cataract Refract Surg. 2000;26:83–87. doi: 10.1016/s0886-3350(99)00323-5. [DOI] [PubMed] [Google Scholar]
- 10.Poort-van Nouhuijs HM, Hendrickx KH, van Marle WF, Boesten I, Beekhuis WH. Corneal astigmatism after clear corneal and corneoscleral incisions forcataract surgery. J Cataract Refract Surg. 1997;23:758–760. doi: 10.1016/s0886-3350(97)80287-8. [DOI] [PubMed] [Google Scholar]
- 11.Kohnen S, Neuber R, Kohnen T. Effect of temporal and nasal unsutured limbal tunnel incisions on induced astigmatism after phacoemulsification. J Cataract Refract Surg. 2002;28:821–825. doi: 10.1016/s0886-3350(01)01215-9. [DOI] [PubMed] [Google Scholar]
- 12.Barequet IS, Yu E, Vitale S, Cassard S, Azar DT, Stark WJ. Astigmatism outcomes of horizontal temporal versus nasal clear corneal incision cataract surgery. J Cataract Refract Surg. 2004;30:418–423. doi: 10.1016/S0886-3350(03)00492-9. [DOI] [PubMed] [Google Scholar]
- 13.Holladay JT, Cravy TV, Koch DD. Calculating the surgically induced refractive change following ocular surgery. J Cataract Refract Surg. 1992;18:429–443. doi: 10.1016/s0886-3350(13)80095-8. [DOI] [PubMed] [Google Scholar]
- 14.Anders N, Pham DT, Antoni HJ, Wollensak J. Postoperative astigmatism and relative strength of tunnel incisions: a prospective clinical trial. J Cataract Refract Surg. 1997;23:332–336. doi: 10.1016/s0886-3350(97)80175-7. [DOI] [PubMed] [Google Scholar]