Abstract
Retinopathy of prematurity is a potentially blinding condition. In this article we describe the surgical management for advanced stages of the disease (stages 4 and 5) Indications, options and alternative techniques are described through a review of articles and our personal experience.
Keywords: Retinopathy of Prematurity (ROP), Surgical Technique, Scleral Buckling; Vitrectomy
INTRODUCTION
Retinopathy of prematurity (ROP) is a preventable but potentially blinding condition.1 Premature infants have been screened at our center since 1997 and unfortunately, the overall incidence of ROP and that of advanced stages (4 and 5) of the disease are increasing.2–4 Despite improvements in screening protocols, peripheral laser ablation, microsurgical techniques and instrumentation, ROP still progresses to retinal detachment (RD) and blindness in 15% to 30% of all involved eyes.5,6 Advanced stages of ROP (4 and 5) usually require surgical intervention. 7 Premature infants with ROP need timely treatment because of the critical period of visual development.8
Several procedures have been described to treat ROP-associated RDs, including open-sky vitrectomy, scleral buckling, closed vitrectomy and lensectomy with or without scleral buckling, and more recently, lens sparing vitrectomy without scleral buckling.9 Herein we present a review on the options and techniques for surgical management of advanced stages of ROP and describe our experience in this regard.
SCLERAL BUCKLING
Scleral buckling is a well established technique for repair of RD and is also used for ROP related RDs. It mechanically reattaches the retina by counteracting the forces exerting traction on the retina.10 Although controversy exists on the choice of scleral buckling versus vitrectomy11–18 for stage 4 ROP, scleral buckling is still used particularly when traction exists anterior to the equator.19
The technique of scleral buckling in our patients involves placement of an encircling exoplant (2.5 mm # 240 solid silicone band) as close to the ridge as possible. The band is secured with intrascleral 5-0 polyester suture and tightened to achieve moderate-height buckle effect. Since subretinal fluid drainage is not routinely performed, anterior chamber paracentesis is usually needed to soften the eye.
Encircling buckles induce myopic refractive changes due to axial elongation and forward shift of the crystalline lens.20 The average induced myopia is −2.75 D in adults,21 but much greater in infants ranging from −9 to −11.0 D20,22 which is potentially amblyogenic. Division or removal of the exoplant is recommended when stable retinal reattachment is achieved22 to reduce the risk of intrusion and promote eye growth.11,16 We usually remove the exoplant after 6 months if retinal reattachment is stable or in cases of anisometropia, however it seems logical to delay exoplant removal in unstable situations. Concerns regarding amblyopia with scleral buckling have led to a preference for vitrectomy in stage 4 ROP.13,23
VITRECTOMY
Vitrectomy in advanced stages (4 or 5) of ROP may confer advantages; however it poses specific challenges to the surgeon.24,25 Vitrectomy may be performed in a closed or open system setting, the former is used more commonly. Open-sky vitrectomy allows direct access to posterior segment structures after removal of the cornea and lens. In this technique, the cornea is trephined and the lens is removed intracapsularly, allowing sharp dissection of retrolental membranes. During surgery, an ophthalmic viscosurgical device such as Healon is used to improve visualization, separate the retina and allow posterior dissection. Open-sky vitrectomy offers advantages of bimanual dissection through a large anterior incision and the possibility of surgery in eyes with cloudy corneas.26–28 Nowadays, closed system surgery is preferred; a three-port system permits the surgeon to switch hands in order to perform anterior dissection without the risk of transient hypotony.29 Vitrectomy can be performed with the aid of a contact lens, binocular indirect ophthalmomicroscope system, or by direct visualization using the operating microscope.
Vitrectomy in neonates differs from adults in several aspects:30 (1) the entry site should be through the pars plicata rather than pars plana;31,32 (2) the lens is relatively larger; (3) posterior vitreous detachment (PVD) cannot be achieved easily; (4) breaks are extremely poorly tolerated and are rarely repaired successfully; (5) cyclitic and pupillary membranes are common; (6) additional causes for structural failure include iridoretinal and retinal-retinal adhesions; (7) subretinal hemorrhage or exudation and retinal pigment epithelium degeneration may preclude favorable functional outcomes; and (8) maximal functional development may take years to achieve.
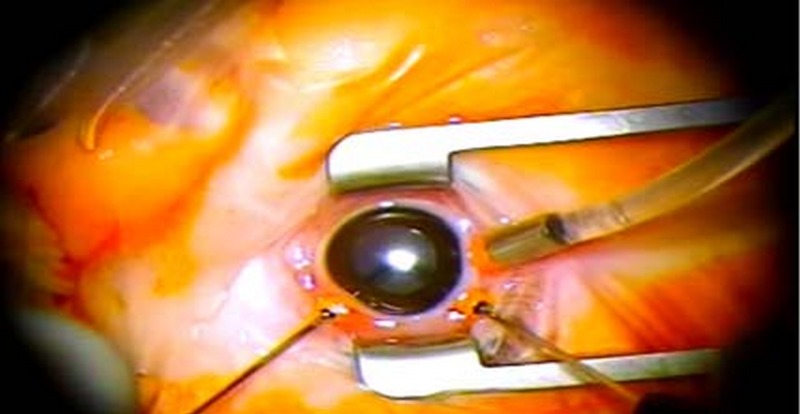
At the onset of operation, the patient undergoes full eye examination. If there is enough space to enter the globe through the pars plicata together with a free retrolental space, pars plicata vitrectomy is performed; otherwise limbal vitrectomy with lensectomy is preferred. Mechanical induction of PVD is not possible and only membranes causing traction should be released and segmented as far as possible using a vitrector (20-, 23- or 25-gauge) or scissors (horizontal or vertical). Extensive membranectomy is not possible and not recommended; we cut or remove membranes as much as possible and try to avoid iatrogenic breaks. We prefer a 23-gauge vitrectomy system because of its appropriate size and possibility of releasing peripheral tractions (Fig. 1). It may be difficult to remove all peripheral tractions by 25-gauge vitrectomy because of instrument flexibility which limits appropriate maneuvers. Once the tractions are relieved, retinal reattachment is achieved and intraocular tamponade is not routinely used. The patients are examined one day after surgery, weekly for 3 weeks, monthly up to 6 months, and every 6 months thereafter. In the case of partial reattachment, reoperations may be considered when persistent tractions exist.
Figure 1.
Twenty-three gauge vitrectomy in a patient with stage 5 retinopathy of prematurity.
In our recent experience, the operation is facilitated by the use of autologous plasmin (unpublished data). In future, enzyme assisted vitrectomy may become a basic component of ROP surgery. For preparation of autologous plasmin, blood is centrifuged at 4,000 rounds per minute for 15 minutes to obtain complete sedimentation; 1.5 ml of plasma is aspirated under aseptic conditions and transferred into a vial of streptokinase (750,000 IU) already incubated at 37°C for 15 minutes. The vial is shaken gently for 3 to 5 minutes and the solution is incubated at 37°C for 10 more minutes; 0.2 ml of this preparation is used for intravitreal injection 15 minutes prior to surgery during induction of anesthesia.33
DISCUSSION
Advantages of vitrectomy in stage 4 ROP include removing endogenous vasodilators and angiogenic factors such as vascular endothelial growth factor (VEGF) from the vitreous cavity in addition to releasing anteroposterior tractions. 19 Both scleral buckling11,16 and vitrectomy15,34 have been used to manage advanced ROP; in the past scleral buckling was the treatment of choice and vitrectomy was considered only if buckling had failed. Nowadays, primary vitrectomy is preferred for stage 4 ROP.5,35 Anatomic success rates vary depending on surgical technique (vitrectomy versus buckling) and stage of detachment (4A or 4B).16–18 Important drawbacks to scleral buckling which adversely affect the functional outcomes include lower anatomical success rates (60%–75%),11,12,15–17 need for a secondary procedure to divide or remove the encircling element,22 and induction of severe myopia and anisometropia with the resulting risk of amblyopia. Outcomes of vitrectomy in stage 4 ROP are more favorable13,18,19,29,36,37 (90% success with mean followup of 1 year) as compared to scleral buckling procedures.12–14,29,36,37 Although scleral buckling procedures may provide a greater anatomic success rate as compared to untreated eyes, studies have revealed that lens-sparing vitrectomy (LSV) may be superior to scleral buckling in terms of anatomical and functional success rates.12–15
Advantages of vitrectomy for advanced ROP with RD consist of addressing the traction directly without need for a second procedure, avoiding compression of anterior segment structures and anatomic distortion, and less induced myopia.38 In stage 4 ROP, initial LSV achieves retinal reattachment more often than scleral buckling with anatomic success rates of 82–97%.9,18,36,39 Vitreoretinal surgery is usually employed for treatment of stage 5 ROP.25 Despite relatively acceptable rates of retinal reattachment, functional outcomes have been poor.15,34,40–43 However, taking into account that untreated stage 5 ROP ends in blindness,43 vitreoretinal surgery is recommended.
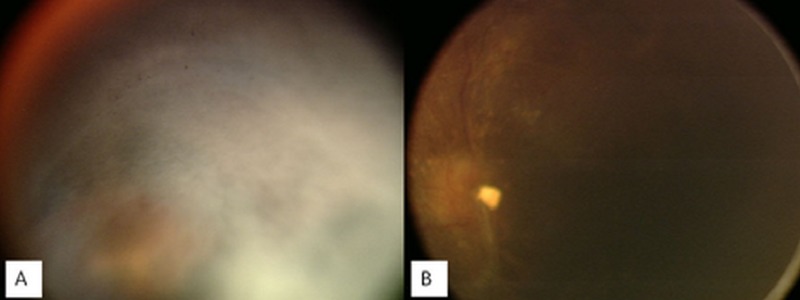
Our understanding of the indications, timing and techniques for surgical management of ROP continues to evolve.7 In our practice, vitrectomy is performed for stage 4 ROP and also for stage 5 in special situations. The choice of scleral buckling versus vitrectomy depends on the stage of ROP, retrolental involvement, vascular activity of the disease (existing plus disease or neovascularization) and presence of an exudative component. In stage 4 ROP, in case of anteroposterior traction and adequate retrolental space for releasing peripheral tractions without removing the lens, we prefer lens sparing vitrectomy; on the other hand with peripheral tractions we prefer scleral buckling. In stage 5 ROP, we routinely perform vitrectomy (Fig. 2) except in exudative forms, for which scleral buckling and intravitreal medications (anti-VEGF with or without corticosteroids) are preferred. Scleral buckling together with vitrectomy may be used for advanced cases of stage 5 ROP. Our algorithm for treatment of advanced stages of ROP is presented in (Figure 3.
Figure 2.
Pre- (A) and post-vitrectomy (B) fundus photographs in a patient with stage 5 retinopathy of prematurity.
Figure 3.
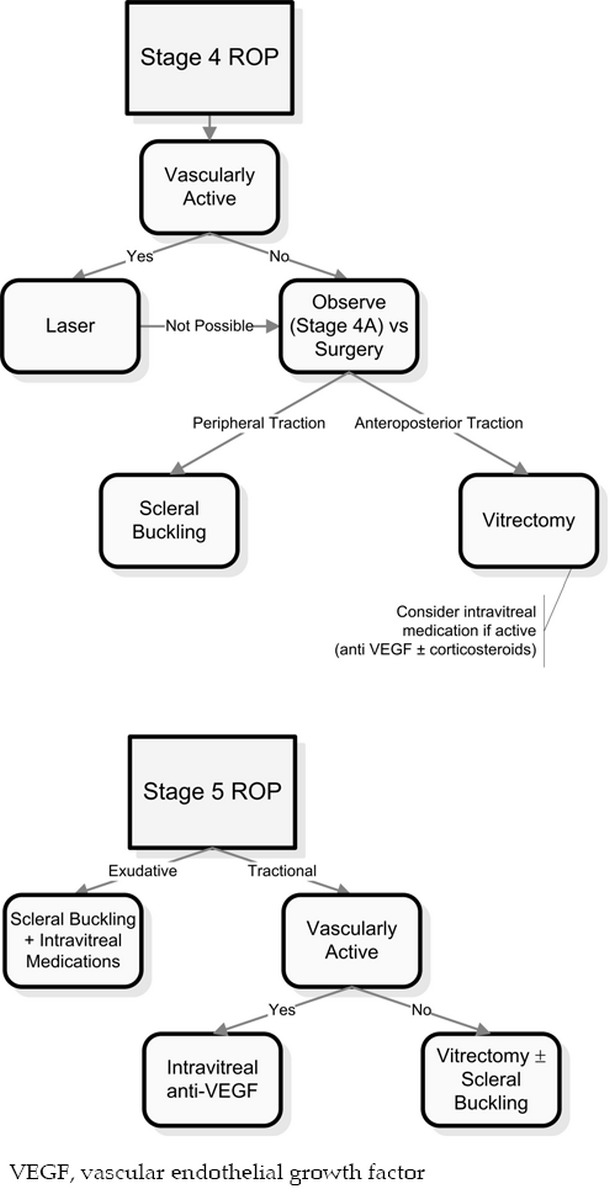
Our algorithm for management of advanced stages of retinopathy of prematurity.
In an unpublished study, we used combined procedures (scleral buckling and 25-gauge vitrectomy) in 21 eyes with stage 5 ROP. Retinal reattachment was achieved completely in 52.3% (success rate) and partially in 23.8% of eyes. Redetachment occurred in three eyes during one year. Success was correlated with disease activity and preoperative treatment (laser therapy or intravitreal bevacizumab). Final reattachment rate was 38%, which is consistent with some previous reports.25 Because of substantial heterogeneity in patient population and severity of the disease, it is difficult to compare the findings of different studies. Most studies include different stages of ROP and utilize different surgical techniques, which may explain differences in success rates.
Dilated vessels in the iris and retina indicate disease activity. We usually use intravitreal bevacizumab in vascularly active disease (unpublished data). Anti-VEGF pharmacotherapy may help as preoperative adjuvant treatment. Vascularly active disease is a significant risk factor for failure of retinal reattachment especially in stage 5 ROP and portends a poor prognosis.44 The poor visual outcome after lensectomy-vitrectomy procedures for RD due to ROP indicates that emphasis should be placed on prevention of RD in premature infants.40–42 Despite relatively acceptable rates of retinal reattachment in stage 5 ROP, functional outcome has been poor.15,23,34,40–42 Enzyme-assisted vitrectomy facilitates separation of the internal limiting membrane and posterior hyaloid membranes. 45 Tsukahara et al46 reported complete reattachment of the posterior pole in all six consecutively treated eyes with stage 5 ROP.
Similar to Lakhanpal et al,29 we manage ROP-related RDs through (1) observation, (2) scleral buckling alone, (3) vitrectomy alone, (4) vitrectomy plus scleral buckling, and (5) vitrectomy with lensectomy. The choice of technique depends on the location of the traction and the presence or absence of retinalens apposition.
REFERENCES
- 1.Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, et al. (International NO-ROP Group). Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115:e518–525. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- 2.Karkhaneh R, Riazi-Esfahani M, Lashay A, Chams H. A survey on visual impairment and blindness in children from retinopathy of prematurity. Iranian J Ophthalmol. 2003;15:101–105. [Google Scholar]
- 3.Mousavi SZ, Karkhaneh R, Riazi-Esfahani M, Mansouri MR, Roohipoor R, Galichi L, et al. Retinopathy of prematurity in infants with late retinal examination. J Ophthalmic Vis Res. 2009;4:24–28. [PMC free article] [PubMed] [Google Scholar]
- 4.Karkhaneh R, Mousavi SZ, Riazi-Esfahani M, Ebrahimzadeh SA, Roohipoor R, Kadivar M, et al. Incidence and risk factors of retinopathy of prematurity in a tertiary eye hospital in Tehran. Br J Ophthalmol. 2008;92:1446–1449. doi: 10.1136/bjo.2008.145136. [DOI] [PubMed] [Google Scholar]
- 5.Gibson DL, Sheps SB, Uh SH, Schechter MT, McCormick AQ. Retinopathy of prematurity induced blindness: birth weight-specific survival and the new epidemic. Pediatrics. 1990;86:405–412. [PubMed] [Google Scholar]
- 6.Lakhanpal RR, Sun RL, Albini TA, Holz ER. Anatomical success rate after primary three-port lens-sparing vitrectomy in stage 5 retinopathy of prematurity. Retina. 2006;26:724–728. doi: 10.1097/01.iae.0000244274.95963.1e. [DOI] [PubMed] [Google Scholar]
- 7.Hubbard GB 3rd. Surgical management of retinopathy of prematurity. Curr Opin Ophthalmol. 2008;19:384–390. doi: 10.1097/ICU.0b013e328309f1a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cats RP, Tan KF. Premature infants with and without regressed retinopathy of prematurity: comparison of long-term (6-10 years) ophthalmological morbidity. J Pediatr Ophthalmol Strabismus. 1989;26:271–275. doi: 10.3928/0191-3913-19891101-05. [DOI] [PubMed] [Google Scholar]
- 9.Hubbard GB 3rd, Cherwick DH, Burian G. Lenssparing vitrectomy for stage 4 retinopathy of prematurity. Ophthalmology. 2004;111:2274–2277. doi: 10.1016/j.ophtha.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 10.Ertzbischoff LM. A systematic review of anatomical and visual function outcomes in preterm infants after scleral buckle and vitrectomy for retinal detachment. Adv Neonatal Care. 2004;4:10–19. doi: 10.1016/j.adnc.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Greven C, Tasman W. Scleral buckling in stages 4B and 5 retinopathy of prematurity. Ophthalmology. 1990;97:817–820. doi: 10.1016/s0161-6420(90)32506-x. [DOI] [PubMed] [Google Scholar]
- 12.Noorily SW, Small K, de Juan E Jr, Machemer R. Scleral buckling surgery for stage 4B retinopathy of prematurity. Ophthalmology. 1992;99:263–268. doi: 10.1016/s0161-6420(92)31978-5. [DOI] [PubMed] [Google Scholar]
- 13.Maguire AM, Trese MT. Lens-sparing vitreoretinal surgery in infants. Arch Ophthalmol. 1992;110:284–286. doi: 10.1001/archopht.1992.01080140140042. [DOI] [PubMed] [Google Scholar]
- 14.Maguire AM, Trese MT. Visual results of lenssparing vitreoretinal surgery in infants. Pediatr Ophthalmol Strabismus. 1993;30:28–32. doi: 10.3928/0191-3913-19930101-08. [DOI] [PubMed] [Google Scholar]
- 15.Trese MT, Droste PJ. Long-term postoperative results of a consecutive series of stages 4 and 5 retinopathy of prematurity. Ophthalmology. 1998;105:992–997. doi: 10.1016/S0161-6420(98)96024-9. [DOI] [PubMed] [Google Scholar]
- 16.Trese MT. Scleral buckling for retinopathy of prematurity. Ophthalmology. 1994;101:23–26. doi: 10.1016/s0161-6420(94)31362-5. [DOI] [PubMed] [Google Scholar]
- 17.Hinz BJ, de Juan E Jr, Repka MX. Scleral buckling surgery for active stage 4A retinopathy of prematurity. Ophthalmology. 1998;105:1827–1830. doi: 10.1016/S0161-6420(98)91023-5. [DOI] [PubMed] [Google Scholar]
- 18.Capone A Jr, Trese MT. Lens-sparing vitreous surgery for tractional stage 4A retinopathy of prematurity retinal detachments. Ophthalmology. 2001;108:2068–2070. doi: 10.1016/s0161-6420(01)00809-0. [DOI] [PubMed] [Google Scholar]
- 19.Sears JE, Sonnie C. Anatomic success of lenssparing vitrectomy with and without scleral buckle for stage 4 retinopathy of prematurity. Am J Ophthalmol. 2007;143:810–813. doi: 10.1016/j.ajo.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Rubin ML. The induction of refractive errors by retinal detachment surgery. Trans Am Ophthalmol Soc. 1975;73:452–490. [PMC free article] [PubMed] [Google Scholar]
- 21.Smiddy WE, Loupe DN, Michels RG, Enger C, Glaser BM, deBustros S. Refractive changes after scleral buckling surgery. Arch Ophthalmol. 1989;107:1469–1471. doi: 10.1001/archopht.1989.01070020543036. [DOI] [PubMed] [Google Scholar]
- 22.Chow DR, Ferrone PJ, Trese MT. Refractive changes associated with scleral buckling and division in retinopathy of prematurity. Arch Ophthalmol. 1998;116:1446–1448. doi: 10.1001/archopht.116.11.1446. [DOI] [PubMed] [Google Scholar]
- 23.Quinn GE, Dobson V, Barr CC, Davis BR, Palmer EA, Robertson J, et al. Visual acuity of eyes after vitrectomy for retinopathy of prematurity: followup at 5 1/2 years. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology. 1996;103:595–600. doi: 10.1016/s0161-6420(96)30647-7. [DOI] [PubMed] [Google Scholar]
- 24.Cusick M, Charles MK, Agrón E, Sangiovanni JP, Ferris FL 3rd, Charles S. Anatomical and visual results of vitreoretinal surgery for stage 5 retinopathy of prematurity. Retina. 2006;26:729–735. doi: 10.1097/01.iae.0000244268.21514.f7. [DOI] [PubMed] [Google Scholar]
- 25.Trese MT. Visual results and prognostic factors for vision following surgery for stage V retinopathy of prematurity. Ophthalmology. 1986;93:574–579. doi: 10.1016/s0161-6420(86)33681-9. [DOI] [PubMed] [Google Scholar]
- 26.Hirose T, Katsumi O, Mehta MC, Schepens CL. Vision in stage 5 retinopathy of prematurity after retinal reattachment by open-sky vitrectomy. Arch Ophthalmol. 1993;111:345–349. doi: 10.1001/archopht.1993.01090030063040. [DOI] [PubMed] [Google Scholar]
- 27.Tasman W, Borrone RN, Bolling J. Open sky vitrectomy for total retinal detachment in retinopathy of prematurity. Ophthalmology. 1987;94:449–452. doi: 10.1016/s0161-6420(87)33432-3. [DOI] [PubMed] [Google Scholar]
- 28.Steidl SM, Hirose T. Subretinal organization in stage 5 retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2003;241:263–268. doi: 10.1007/s00417-003-0632-x. [DOI] [PubMed] [Google Scholar]
- 29.Lakhanpal RR, Sun RL, Albini TA, Holz ER. Anatomic success rate after 3-port lens-sparing vitrectomy in stage 4A or 4B retinopathy of prematurity. Ophthalmology. 2005;112:1569–1573. doi: 10.1016/j.ophtha.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 30.Tawansy KA, Samuel MA. Retinopathy of prematurity: practical surgical management in the new millennium. Tech Ophthalmology. 2004;2:60–67. [Google Scholar]
- 31.Aiello AL, Tran VT, Rao NA. Postnatal development of the ciliary body and pars plana. A morphometric study in childhood. Arch Ophthalmol. 1992;110:802–805. doi: 10.1001/archopht.1992.01080180074031. [DOI] [PubMed] [Google Scholar]
- 32.Dietl RH, Stefani FH. Topographic-surgical anatomy of the pediatric pars plana. Ophthalmologica. 1986;193:1–9. doi: 10.1159/000309671. [DOI] [PubMed] [Google Scholar]
- 33.Rizzo S, Pellegrini G, Benocci F, Belting C, Baicchi U, Vispi M. Autologous plasmin for pharmacologic vitreolysis prepared 1 hour before surgery. Retina. 2006;26:792–796. doi: 10.1097/01.iae.0000244266.83395.16. [DOI] [PubMed] [Google Scholar]
- 34.Mintz-Hittner HA, O’Malley RE, Kretzer FL. Longterm form identification vision after early, closed, lensectomy-vitrectomy for stage 5 retinopathy of prematurity. Ophthalmology. 1997;104:454–459. doi: 10.1016/s0161-6420(97)30292-9. [DOI] [PubMed] [Google Scholar]
- 35.Shah PK, Narendran V, Kalpana N, Tawansy KA. Anatomical and visual outcome of stages 4 and 5 retinopathy of prematurity. Eye. 2009;23:176–180. doi: 10.1038/sj.eye.6702939. [DOI] [PubMed] [Google Scholar]
- 36.Prenner JL, Capone A Jr, Trese MT. Visual outcomes after lens-sparing vitrectomy for stage 4A retinopathy of prematurity. Ophthalmology. 2004;111:2271–2273. doi: 10.1016/j.ophtha.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 37.Moshfeghi AA, Banach MJ, Salam GA, Ferrone PJ. Lens-sparing vitrectomy for progressive tractional retinal detachments associated with stage 4A retinopathy of prematurity. Ophthalmology. 2004;122:1816–1818. doi: 10.1001/archopht.122.12.1816. [DOI] [PubMed] [Google Scholar]
- 38.Gonzales CR, Boshra J, Schwartz SD. 25-Gauge pars plicata vitrectomy for stage 4 and 5 retinopathy of prematurity. Retina. 2006;26:S42–46. doi: 10.1097/01.iae.0000244288.63757.be. [DOI] [PubMed] [Google Scholar]
- 39.Hartnett ME, Srilakshmi M, Thompson HW, McColm JR. Comparison of retinal outcomes after scleral buckle or lens-sparing vitrectomy for stage 4 retinopathy of prematurity. Retina. 2004;24:753–757. doi: 10.1097/00006982-200410000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Zilis JD, deJuan E, Machemer R. Advanced retinopathy of prematurity The anatomic and visual results of vitreous surgery. Ophthalmology. 1990;97:821–826. [PubMed] [Google Scholar]
- 41.Kono T, Oshima K, Fuchino Y. Surgical results and visual outcomes of vitreous surgery for advanced stages of retinopathy of prematurity. Jpn J Ophthalmol. 2000;4:661–667. doi: 10.1016/s0021-5155(00)00282-3. [DOI] [PubMed] [Google Scholar]
- 42.Seaber JH, Machemer R, Eliott D, Buckley EG, deJuan E, Martin DF. Long-term visual results of children after initially successful vitrectomy for stage V retinopathy of prematurity. Ophthalmology. 1995;102:199–204. doi: 10.1016/s0161-6420(95)31035-4. [DOI] [PubMed] [Google Scholar]
- 43.Capone A Jr, Trese MT. Stage 5 retinopathy of prematurity: then and now. Retina. 2006;26:721–723. doi: 10.1097/01.iae.0000233654.23754.52. [DOI] [PubMed] [Google Scholar]
- 44.Lakhanpal RR, Fortun JA, Chan-Kai B, Holz ER. Lensectomy and vitrectomy with and without intravitreal triamcinolone acetonide for vascularly active stage 5 retinal detachments in retinopathy of prematurity. Retina. 2006;26:736–740. doi: 10.1097/01.iae.0000244257.60524.89. [DOI] [PubMed] [Google Scholar]
- 45.Uemura A, Nakamura M, Kachi S, Nishizawa Y, Asami T, Miyake Y, et al. Effect of plasmin on laminin and fibronectin during plasmin-assisted vitrectomy. Arch Ophthalmol. 2005;123:209–213. doi: 10.1001/archopht.123.2.209. [DOI] [PubMed] [Google Scholar]
- 46.Tsukahara Y, Honda S, Imai H, Kondo N, Fujii S, Yokoyama N, et al. Autologous plasmin-assisted vitrectomy for stage 5 retinopathy of prematurity: a preliminary trial. Am J Ophthalmol. 2007;144:139–141. doi: 10.1016/j.ajo.2007.03.020. [DOI] [PubMed] [Google Scholar]