Summary
In the three decades since the eradication of smallpox and cessation of routine vaccination, the collective memory of the devastating epidemics caused by this orthopoxvirus has waned, and the human population has become increasingly susceptible to a disease that remains high on the list of possible bioterrorism agents. Research using surrogate orthopoxviruses in their natural hosts, as well as limited variola virus research in animal models, continues worldwide; however, interpretation of findings is often limited by our relative lack of knowledge about the naturally occurring disease. For modern comparative pathologists, many of whom have no first-hand knowledge of naturally occurring smallpox, this work provides a contemporary review of this historical disease, as well as discussion of how it compares with human monkeypox and the corresponding diseases in macaques.
Keywords: smallpox, monkeypox, variola, macaque
Introduction
Renewed interest in the development of medical countermeasures against smallpox, and to a lesser extent monkeypox, has led to an increased use of macaque models of both diseases. These models are used at all stages of the research process, from basic mechanistic investigations to regulatory safety and efficacy evaluations (Huggins et al., 2009; Jordan et al., 2009; Shao et al., 2009; Keasey et al., 2010; Zielinski et al., 2010; Estep et al., 2011; Hirao et al., 2011). In the USA, regulatory clearance of new countermeasures requires that the compound in question be tested in accordance with the ‘Animal Rule’ (FDA 21 CFR 601.90). Thus, an animal model that accurately recapitulates the human condition is needed for both the identification and testing of therapeutic targets. Macaques have been used in studies employing both variola virus and monkeypox virus delivered by different routes, yet it is largely unclear how the resultant systemic pathology compares with that of the naturally occurring disease. To this end, we provide a comprehensive review of the pathology of human smallpox and a detailed analysis of how it compares with human monkeypox and the various macaque models of smallpox and monkeypox.
Virology
The family Poxviridae is comprised of complex double-stranded DNA viruses whose replication cycle occurs exclusively within the cytoplasm of host cells. The family is divided further into two subfamilies, Chordopoxvirinae and Entomopoxvirinae based on the ability to infect vertebrate or insect cells, respectively. Variola virus (VARV) and monkeypox virus (MPXV) are classified in the Orthopoxvirus genus, one of eight genera within the Chordopoxvirinae subfamily. While VARV and MPXV are genetically and antigenically related, these viruses differ in sequence within regions encoding virulence and host-range factors near the genome termini (Shchelkunov et al., 2001). Comparative genomics of 45 epidemiologically varied VARV isolates indicate low sequence diversity (Esposito et al., 2006). However, comparison of VARV strain Japan 1951 (Harper masterseed) and MPXV strain Zaire 96-I-16 shows that the MPXV genome is 10,678 base pairs larger than that of VARV (Shchelkunov et al., 2001; Esposito et al., 2006). In addition, comparison of VARV strains India-1967 and Bangladesh-1975 with MPXV strains Zaire-96-I-16 and Congo-8 shows that the MPXV genomes have mutations that affect translation of two interferon resistance genes that encode proteins (C3L and E3L) that are intact in VARV (Shchelkunov et al., 2001). The MPXV genomes also encode a secreted interleukin (IL)-1β-binding protein which the VARV genomes do not (Shchelkunov et al., 2001). Deletion of this gene in vaccinia virus has been correlated with increased pathogenicity (Alcami and Smith, 1996). Genomic differences are important when one considers using MPXV as a surrogate model for VARV, particularly with respect to testing of vaccines and therapeutic countermeasures. Such variation could result in appreciable differences in pathogenesis in different hosts.
In addition to molecular differences, MPXV and VARV have dissimilar host ranges. Prior to eradication VARV was distributed worldwide throughout the human population only, and the lack of an animal reservoir contributed to the success of its eradication (Fenner et al., 1988c). MPXV is restricted to western and central Africa, which reflects, in part, the geographical distribution of its rodent reservoir hosts (Essbauer et al., 2010). Multiple ecological surveys have implicated African rodents, including Funisciurus spp., Heliosciurus spp. and Cricetomys spp., and not non-human primates, as the natural reservoir hosts of MPXV (Khodakevich et al., 1986, 1987, 1988; Hutin et al., 2001). In addition, an outbreak of monkeypox which occurred in the USA in 2003 was associated with the importation of rodents from Ghana, West Africa (Annonymous, 2003; Reed et al., 2004).
Smallpox in Man
Disease Classification and Clinical Progression
Human smallpox presented with varying clinical patterns, historically giving rise to numerous classifications for the types of disease. Early classifications, such as those by Curschmann (1875), were based primarily on the density of the rash. In the 20th century, Dixon divided the classification into nine clinical types and avoided use of the term ‘haemorrhagic’, favouring ‘fulminating’ instead (Dixon, 1962). Three of the nine subtypes were also based on the number of skin lesions. This method of classification proved to be impractical and was not useful prognostically. To simplify the classification system and make it more functional, Rao defined four types of smallpox: haemorrhagic, flat, ordinary and modified, that were further divided into 12 subtypes (Rao, 1972). This classification system was based on the observation that haemorrhagic smallpox was indeed a clinically and epidemiologically distinct form of the disease, and haemorrhages had prognostic value during diagnosis (Rao, 1972). Furthermore, he realized that in non-haemorrhagic cases, the number of lesions was not as significant as their nature and evolution. The World Health Organization (WHO) modified Rao’s classification system and divided the clinical forms of smallpox into five varieties: ordinary, modified, variola sine eruptione, flat and haemorrhagic. A summary of the major clinical and epidemiological features of the different forms of smallpox as defined by the WHO classification system is shown in Table 1.
Table 1.
Clinical classifications of human smallpox
| Disease type | Incidence | Vaccination status | Fever | Skin lesions | Subtypes | Case fatality rates |
|---|---|---|---|---|---|---|
| Ordinary | 88% | Unvaccinated | Yes | Many; vesiculopustular | Discrete | 9.3% |
| Semiconfluent | 37% | |||||
| Confluent | 62% | |||||
| Modified | NR | Vaccinated | No | Few; vesiculopustular | None | NR |
| Variola sine eruptione | NR | Vaccinated | Yes | None | None | NR |
| Flat | Rare | Unvaccinated | Yes | Erythema; flat vesicles with little fluid | None | 97% |
| Haemorrhagic | Rare | Unvaccinated | Yes | Erythema, petechia, ecchymoses | Early onset | 96% |
| Late onset |
NR, not reported
Ordinary smallpox was characterized by raised pustular lesions and was further divided into three subtypes based on lesion density: discrete (areas of normal skin between pustules), semiconfluent (lesions coalesced on the face) and confluent (lesions coalesced on the face and forearms) (Fenner et al., 1988a). In Rao’s report of 6,942 patients in Madras, ordinary smallpox comprised the majority of cases (88%) in unvaccinated patients. The case fatality rates among unvaccinated patients with discrete, semiconfluent and confluent subtypes were 9.3, 37, and 62%, respectively. Ordinary smallpox had an incubation period of 10–14 days. The pre-eruptive phase typically lasted 2–3 days and was marked by several common features including fever (100%), headache (90%), severe backache (90%) and vomiting (50%) (Rao, 1972). Fever (38.5–40.5 °C) fell by the time macules first appeared, rose a second time during vesicle, papule and pustule formation, and declined again during crust formation (Dixon, 1962; Rao, 1972; Fenner et al., 1988a).
Two milder variants of ordinary smallpox were modified smallpox and variola sine eruptione. Modified smallpox occurred in previously vaccinated individuals and was characterized by an accelerated clinical course without secondary fever (Fenner et al., 1988a). In addition, the lesions were superficial and fewer in number than ordinary smallpox (Dixon, 1962; Fenner et al., 1988a). Variola sine eruptione signified fever caused by VARV without development of skin lesions. It was also referred to as ‘contact fever’, a condition recognized in individuals who were vaccinated contacts of smallpox patients.
Flat smallpox and haemorrhagic smallpox represented rare but severe forms of the disease with 97 and 96% case fatality rates, respectively (Rao, 1972). In flat smallpox, distribution of lesions often did not conform to the typical centrifugal pattern of ordinary smallpox. Erythema resembling severe sunburn progressed to confluent or semiconfluent soft and velvety vesicles that remained flush with the skin surface (Dixon, 1962). The vesicles of flat smallpox contained little fluid, did not become umbilicated, and the epidermis frequently excoriated following slight trauma (Fenner et al., 1988a).
Haemorrhagic smallpox is divided into two subtypes: early and late (Bras, 1952; Fenner et al., 1988a). In both forms, widespread bleeding occurred in the skin and mucous membranes throughout the body. Cases of early haemorrhagic smallpox were relatively less common, comprising 36% of haemorrhagic cases reported by Rao (1972). Fever that could reach a peak of 41°C was accompanied by intense headache, backache, prostration, dyspnoea and chest pain (Rao, 1972; Koplan et al., 1975). By the second day of fever, generalized erythema and petechiae appeared, with areas of ecchymosis. The highest frequency of haemorrhages was in the skin and conjunctiva (Haviland, 1952; Rao, 1972). Bleeding from the gums and haematuria were also seen in 20 and 25% of patients, respectively (Rao, 1972). Death occurred swiftly and typically within 6 days of the onset of fever (Dixon, 1962; Rao, 1972). Early haemorrhagic smallpox had a propensity for adults (88% of Rao’s cases) and women, with pregnant women being particularly susceptible.
Late haemorrhagic smallpox was distinguished from the early type by the appearance of haemorrhages after vesiculopustular lesions developed. The course of the disease was rapidly progressive with high fever and death before day 12. In Rao’s report, late haemorrhagic smallpox constituted 64% of all haemorrhagic smallpox cases. Haemorrhage seen within the skin lesions originated in the dermis beneath pustules and not in the fluid within them (Ikeda, 1925; Bras, 1952; Roberts et al., 1965; Fenner et al., 1988a).
Clinical Pathology
Historically, clinical pathological evaluations of smallpox patients were rarely performed and relatively few data are available from cases of ordinary smallpox as compared with haemorrhagic smallpox. The available data are limited to complete blood counts and coagulation studies. Mild anaemia and leucocytosis are the only reported changes in ordinary smallpox and differential leucocyte values are not available (Koplan et al., 1975). In haemorrhagic smallpox, leucocytosis with lymphocytosis and neutropenia are reported consistently (Ikeda, 1925; Haviland, 1952). Despite the clinical presentation of haemorrhage in this form of the disease, anaemia was not found, presumably due to the acutely fatal disease course.
Thrombocytopenia is reported consistently in both ordinary and haemorrhagic smallpox (Ikeda, 1925; Haviland, 1952; McKenzie et al., 1965; Roberts et al., 1965; Mehta et al., 1967; Mitra and Bhattacharya, 1976). In ordinary smallpox, platelet counts reach a nadir during the vesicular stage and return to normal during the pustular stage (Ikeda, 1925; Roberts et al., 1965). In both early and late haemorrhagic smallpox, thrombocytopenia is severe and does not resolve prior to death. In addition, bleeding times are prolonged and clot retraction is abnormal or absent (McKenzie et al., 1965; Roberts et al., 1965; Mehta et al., 1967; Mitra and Bhattacharya, 1976). Coagulation studies in patients with haemorrhagic smallpox consistently reveal prolonged prothrombin, activated partial thromboplastin and thrombin times (McKenzie et al., 1965; Roberts et al., 1965; Mehta et al., 1967; Mitra and Bhattacharya, 1976). McKenzie et al. (19650 also evaluated activity of factors X, VII, and V in 39 patients with haemorrhagic smallpox and 21 patients with non-haemorrhagic smallpox. They found that factor X activity was normal in both forms of the disease, factor VII activity was mildly decreased in haemorrhagic smallpox, and factor V activity was markedly decreased in both forms of the disease (McKenzie et al., 1965). Together, these findings indicate that disseminated intravascular coagulation is the most likely cause of the haemorrhagic diathesis in haemorrhagic smallpox.
Gross Pathology
By today’s standards little is known about the systemic pathology of human smallpox. While the gross and microscopical appearance of the cutaneous and mucosal lesions is well described, descriptions of changes in other major organ systems are absent or incomplete and difficult to interpret. Importantly, often no distinction is made between lesions found in ordinary smallpox versus those found in haemorrhagic smallpox.
In 1904, Councilman et al. published autopsy findings from 54 cases, including 37 cases of ‘variola vera’ (ordinary smallpox), two cases of ‘variola pustulosa haemorrhagica’ (late haemorrhagic smallpox) and four cases of ‘purpura variolosa’ (early haemorrhagic smallpox) (Councilman et al., 1904). In 1952, Bras reported the pathological findings from 177 cases originating from a 1949 outbreak in Djakarta, Indonesia (Bras, 1952). Of these, 131 were diagnosed as ‘variola vera’, 11 were ‘variola pustulosa haemorrhagica’, 26 were ‘purpura variolosa’ and nine lacked specific diagnoses. Lillie (1930) reviewed numerous additional isolated reports in 1930. Unless otherwise noted, the pathology of human smallpox as presented here is taken from these seminal works (Councilman et al., 1904; Lillie, 1930; Bras, 1952). Summaries of the pathological changes found in ordinary and haemorrhagic human smallpox are shown in Tables 2 and 3, respectively. A summary of pathological changes reported, but not associated with a specific disease type is shown in Table 4.
Table 2.
Pathological findings specifically associated with ordinary smallpox in man
| Tissue | Lesion/Change |
|---|---|
| Skin/mucous membranes | Proliferative and necrotizing dermatitis with distinct maculopapular, vesiculopustular and desquamating stages |
| Spleen | Congestion and small haemorrhages |
| Lung | Bronchopneumonia, oedema, atelectasis |
| Liver | Hepatomegaly, congestion, lipidosis |
| Bone Marrow | Myeloid hyperplasia |
| Testis | Multifocal interstitial orchitis, seminiferous tubule degeneration, Azoospermia, arteritis, thrombosis, perivascular haemorrhage |
| Kidney | Multifocal lymphoplasmacytic and histiocytic interstitial nephritis |
Table 3.
Pathological findings specifically associated with haemorrhagic smallpox in man
| Tissue | Lesion/Change |
|---|---|
| Skin/mucous membranes | Erythema, petechia |
| Spleen | Congestion and small haemorrhages, infarction ± intralesional bacteria |
| Lung | Haemorrhage, oedema |
| Liver | Hepatomegaly, congestion, lipidosis |
| Bone Marrow | Necrosis ± intralesional bacteria |
| Testis | Multifocal interstitial orchitis, seminiferous tubule degeneration, arteritis, thrombosis, perivascular haemorrhage |
| Kidney | Pelvic and ureteral haemorrhage, multifocal lymphoplasmacytic and histiocytic interstitial nephritis |
Table 4.
Pathological findings in human smallpox not specifically associated with either the ordinary or haemorrhagic form of the disease
| Tissue | Lesion/Change |
|---|---|
| Spleen | Lymphohistiocytic splenitis, lymphoid hyperplasia |
| Lymph Node | Normal, hypertrophy, hyperaemia; oedema, congestion, lymphoid necrosis |
| Tonsil | Lymphoid necrosis |
| Liver | Hepatocellular necrosis, necrotizing hepatitis ± intralesional bacteria, endothelial hypertrophy and hyperplasia ± necrosis, acute subcapsular and parenchymal haemorrhage |
| Ovary | Multifocal lymphohistiocytic oophoritis, follicular epithelial necrosis |
| Uterus | Haemorrhage |
| Kidney | Acute glomerulonephritis |
| Bone | Pyogenic osteomyelitis, osteomyelitis variolosa |
| Central Nervous System | Meningoencephalomyelitis |
| Heart | Multifocal myocardial and subendothelial haemorrhages (rare), lymphohistiocytic and eosinophilic myocarditis and epicarditis (rare) |
Skin and Mucous Membranes
Orthopoxviral exanthema and enanthema are well described and have been studied extensively. Given the abundance of high quality literature describing the appearance and progression of these lesions, only a brief review will be provided here. The gross appearance and distribution of the lesions by disease type is discussed above. Histologically, the earliest change in ordinary smallpox is dilation of small capillaries and lymphatics within the superficial dermis and hypertrophy of the endothelial cells lining those vessels. At this time, a mild to moderate perivascular to interstitial lymphohistiocytic and plasmacytic superficial dermal infiltrate also appears. Subsequently, the epidermis overlying these areas becomes hyperplastic and keratinocytes within the stratum spinosum swell. Grossly, this corresponds to the maculopapular stage. Round to ovoid intracytoplasmic inclusions (2–8 μm diameter) may become visible within affected keratinocytes. Cell swelling progresses to hydropic (ballooning) degeneration and lysis of the keratinocytes results in intraepidermal vesicle formation. In many cases the vesicle is multiloculated. Lateral to the vesicle, epidermal hyperplasia continues resulting in acanthosis. Large numbers of neutrophils migrate from dermal capillaries and venules into the vesicle to form a discrete pustule. The progression from vesicle to pustule is not simultaneous across all lesions. During the healing stage, re-epithelialization with parakeratotic hyperkeratosis occurs and a crust is formed. Changes in the follicular epithelium resemble those in the epidermis. Sebaceous epithelium undergoes necrosis, granulation and replacement by fibrous connective tissue resulting in scar formation.
In early haemorrhagic smallpox, the cutaneous lesions resemble those of ordinary smallpox except that the initial vascular dilatation and congestion is more marked and sometimes accompanied by perivascular haemorrhage, resulting in the petechia seen grossly. In addition, because haemorrhagic smallpox is rapidly fatal, the epithelial lesions generally do not have time to progress through the maculopapular, vesiculopustular and crust stages. In late haemorrhagic smallpox, vesicles and pustules develop as in ordinary smallpox; however, congestion and haemorrhage within the underlying dermis is much more prominent.
The appearance and progression of epitheliocentric lesions in the mucous membranes lining the oropharynx, larynx, trachea and oesophagus are similar to those seen in the skin except that rupture of vesicles and pustules, and subsequent ulceration are more common; crusts do not occur. In some cases, the pustular stage is accompanied by pseudomembrane formation at the level of the pharynx. Healing generally occurs without scar formation. In early haemorrhagic disease, discrete mucosal lesions are not common, but similar to the skin, submucosal congestion and haemorrhage are seen.
Secondary Lymphoid Organs
Non-specific splenic changes are common in both ordinary and haemorrhagic smallpox. Throughout the historical literature, much attention is paid to the size of the spleen which appears to range from normal to mildly enlarged. Histologically, red pulp congestion with or without small haemorrhages is reported in both ordinary and haemorrhagic forms of the disease. The sinusoids are frequently described as being filled with macrophages accompanied by fewer lymphocytes, plasma cells and neutrophils. As in other organs, some authors emphasize a striking lack of neutrophils. Councilman et al. (1904) reported occasional intrahistiocytic intracytoplasmic inclusion bodies. The sinusoidal endothelium is often described as hypertrophic. In general, little distinction is made between the different disease types, except that splenic infarcts, with or without intralesional bacteria, are more commonly reported in cases of haemorrhagic smallpox. Bras (1952), specifies the presence of gram-positive bacteria in infarcted areas. Others describe focal areas of necrosis with large central masses of bacteria, but it is not clear whether this applies to cases of ordinary smallpox, haemorrhagic smallpox, or both. The white pulp is generally reported to be unremarkable, but a few authors describe some degree of lymphoid hyperplasia, and Councilman et al. (1904) describe what are likely to be prominent germinal centres.
Lymph node pathology in naturally occurring smallpox is poorly described. Councilman et al. (1904) note that in the pre-20th century literature ‘very little attention has been paid to the condition of the lymph nodes in variola’. In his case series, Bras (1952) reports that the lymph nodes were not examined regularly, and his description of them is limited to three sentences. Of the data available, the most commonly reported gross nodal changes are hypertrophy and hyperaemia; however, in many cases the lymph nodes are reportedly normal. Histologically, the enlargement, if present, appears to be due primarily to oedema and congestion. Councilman et al. (1904) specifically state that the ‘enlargement of the node is due more to oedema than cellular hyperplasia’. Sinus histiocytosis and multifocal haemorrhage with erythrophagocytosis and abundant fibrin and are also reported. As with the spleen, many authors also describe multiple foci of necrosis and lymphocytolysis, with or without bacteria; however, an association with a specific disease type is not always made. In a few reports, necrosis with intralesional bacteria is said to be more common with haemorrhagic disease.
Specific descriptions of tonsillar pathology are lacking. The tonsils are not mentioned by Councilman et al. (1904) or Lillie (1930). Bras (1952), describes multifocal lymphoid necrosis without reference to a specific disease type. In addition, typical epitheliocentric lesions as seen elsewhere in the oropharynx are present in the stratified squamous and specialized crypt epithelium of the tonsil.
Lungs
Much controversy exists over the character and aetiology of pulmonary lesions in human smallpox. Most authors agree that in ordinary smallpox, bronchopneumonia is the most common and serious complication and often the fulminant cause of death. The infiltrate is generally described as suppurative and in most reports, intralesional bacteria are common. Cocci, including streptococci, staphylococci and pneumococci are the most commonly implicated bacteria; however, it is not clear if these species-specific determinations are definitive or merely descriptive variants of coccoid bacteria. Councilman et al. (1904) report that blood cultures were performed in 11 cases; ‘Streptococcus pyogenes’ (n = 9), ‘Pneumococcus sp.’ (n = 1), and ‘Staphylococcus pyogenes aureus’ (n = 1) were recovered. Likewise, Lillie (1930) states that streptococci, staphylococci and pneumococci were ‘recovered culturally in all combinations’. In some cases, bacilli are also reported. Even so, the aetiology of the bronchopneumonia is often debated, largely due to the presence of a separate and distinct virus-associated bronchial lesion. In this case, the lesion is epitheliocentric, multifocal and appears to recapitulate the proliferative and necrotizing process seen in the skin and mucous membranes, much like the more common upper respiratory mucosal lesions (see Skin and Mucous Membranes). In some cases, bronchial epithelial intracytoplasmic inclusions are also reported. Thus, it is not clear whether the aetiology of the bronchopneumonia is purely bacterial or mixed bacterial–viral, where a secondary bacterial infection is superimposed on a primary viral lesion. Other commonly reported changes in ordinary smallpox include oedema and atelectasis. With late haemorrhagic disease, the lesions resemble those of ordinary smallpox, but are accompanied by multifocal acute haemorrhages. Pulmonary changes in acute onset haemorrhagic smallpox are limited to extensive haemorrhage and oedema.
Liver
Hepatomegaly is the most commonly reported hepatic change in both ordinary and haemorrhagic smallpox. It ranges from mild to marked, and histologically is most attributable to vascular congestion and macrovesicular hepatocellular degeneration (lipidosis). The lipidosis is generally found to be periportal, but panlobular distribution is also noted sometimes. Various forms of hepatocellular necrosis are also reported commonly. The mildest presentations involve either sporadic individual hepatocyte necrosis or small foci of necrosis without inflammation. More often, multifocal necrotizing hepatitis with central caseous necrosis is described. In these cases, the presence and role of bacteria is debated, with some authors reporting intralesional and intravascular cocci and others denying their presence. Intracytoplasmic and intranuclear hepatocellular inclusions are described rarely. Endothelial cell swelling and proliferation are described by many authors, and some also report endothelial necrosis and sloughing. Multifocal, acute, subcapsular and parenchymal haemorrhage is sometimes mentioned, but it is not clear if this change is limited to cases of haemorrhagic smallpox.
Bone Marrow
The nature of the bone marrow changes in smallpox has long been of interest. Myeloid hyperplasia is the predominant change reported in ordinary smallpox, while haematopoietic necrosis, with or without intralesional bacteria, occurs with haemorrhagic disease. Haemorrhage has been described in both forms of the disease, but is less common and milder in ordinary smallpox. Most authors, Bras (1952) being the only exception, report a striking reduction or absence of polymorphonuclear cells without reference to a specific disease type. Councilman et al. (1904) state that ‘the essential condition is that the marrow is incapable of transforming the mononuclear myelocytes into the polynuclear neutrophiles [sic]’. They go on to describe a reduction in the number of metamyelocytes. This suggests a maturation defect of the granulocyte line, but follow-up studies are lacking. In other organs, much emphasis is often placed on the relative lack of neutrophils, and in many cases bacterial colonization without a concomitant leucocytic reaction is described. It is unclear whether this represents post-mortem bacterial invasion or a true defect in the neutrophil response. Bras (1952) also reports this confounded observation; however, he states specifically that his examination of the bone marrow in 34 cases did not reveal a significant reduction in polymorphonuclear cells. Reduced numbers of megakaryocytes, and in some cases erythrocyte precursors, has been reported with haemorrhagic smallpox and correlates with the thrombocytopenia seen clinically.
Reproductive Organs
Smallpox-associated testicular lesions are reported commonly and with the exception of more severe haemorrhage in haemorrhagic smallpox, the lesions do not differ with disease type. Multifocal interstitial orchitis, with or without central necrosis, is the lesion reported most commonly. Many authors emphasize a temporal correlation between the development of testicular lesions and the progression of the cutaneous lesions. The inflammatory infiltrate is predominantly histiocytic and lymphocytic, although Bras (1952) also describes an eosinophilic component. Similarly, lymphohistiocytic epididymitis and prostatitis occur, but with much less frequency. In the testis, seminiferous tubule degeneration is common, but its distribution in relation to the interstitial inflammation is not described. Azoospermia is also reported in more advanced cases of ordinary smallpox. Arteritis, thrombosis and perivascular haemorrhage are additional commonly reported findings. Councilman et al. (1904) specifically describe a mononuclear endarteritis with endothelial hypertrophy. In some cases, discrete infarcts are reported.
Ovarian lesions are less common than testicular lesions; however, they are similar in character. Multifocal lymphohistiocytic oophoritis is found occasionally and may be accompanied by haemorrhage. Some authors describe degeneration and necrosis of the follicular epithelium associated with Graafian follicles; however, it is unclear if this is a smallpox-specific change or merely physiological follicular atresia. There are no reports of ovarian vascular lesions similar to the arteritis seen in the testis. Despite the high incidence of spontaneous abortion with variola infection, descriptions of uterine pathology are lacking. Endometrial haemorrhage is the only reported lesion, and no correlation with menstrual cycle phase, gestation or parturition is made.
Kidneys
Grossly, the only significant renal lesion is extensive pelvic and ureteral haemorrhage in cases of haemorrhagic smallpox. Histologically, most authors agree that regardless of disease type, multifocal lymphoplasmacytic and histiocytic interstitial nephritis with marked oedema and mild tubular epithelial degeneration and regeneration is the most common finding. Some authors also describe an eosinophilic component to the inflammatory infiltrate. Acute glomerulonephritis is reported less commonly. In a single case only, Keysselitz and Mayer (1909) report Guarnieri bodies (orthopoxvirus-specific intracytoplasmic inclusion bodies) within the renal tubular epithelium. In some cases, intralesional bacteria and fibrin thrombi are reported.
Bone and Joints
Clinically, osteomyelitis and/or arthritis were estimated to occur in 0.25–0.5% of smallpox patients (Cockshott and Macgregor, 1958). Very little information on the gross and histological appearance of this condition has been reported, but clinical and radiological studies indicate that two distinct osteoarticular manifestations occurred. The first was a pyogenic osteomyelitis associated with bacterial septicaemia. The second, termed ‘osteomyelitis variolosa’, was thought to be a VARV-associated lesion. In these cases, the lesions were most common in the elbows, radii, wrists, hands, ankles and feet; they were often bilateral; and they localized to the metaphyses and epiphyseal ossification centers (Cockshott and Macgregor, 1958). Osteomyelitis variolosa more commonly afflicted children <5 years of age (2–5% of VARV-infected children), and often resulted in permanent bony deformities and shortened limbs (Cockshott and Macgregor, 1958). The time to clinical onset ranged from 1 week to many years (Cockshott and Macgregor, 1958; Balaji, 2011). Unfortunately, detailed histopathological descriptions of osteomyelitis variolosa cannot be found. In 1893, Chiari created confusion by applying the term ‘osteomyelitis variolosa’ to foci of necrosis within the bone marrow (Chiari, 1893); however, it is now accepted that haematopoietic necrosis is an independent lesion distinct from the osteoarticular changes.
Other
Despite the well-known occurrence of vaccinia-associated postvaccinal encephalitis, the pathology of the central nervous system (CNS) in naturally-occurring smallpox is largely unknown. Councilman et al. (1904) do not mention the CNS. Bras (1952) states that in all of his cases the brain was examined grossly, and histopathological examinations were performed at the Laboratory for Neuropathology in Djakarta, but no results are reported. Lillie (1930) discusses the few reports available in the historical literature and findings are limited to a non-suppurative perivascular and interstitial encephalitis with demyelination and minimal meningitis. The lesions were reportedly most common in the cortex and non-existent in the medulla. Descriptions of spinal cord pathology are rare, but there is one report of perivascular mononuclear infiltration and meningeal haemorrhage.
Although mild, adrenal gland lesions were often noted. The most common change was small foci of lymphoplasmacytic inflammation within the medulla, and to a lesser extent, the zona reticularis. Some authors also report small foci of cellular degeneration and necrosis, although Bras (1952) states specifically that this change was not found in his cases. Congestion and medullary haemorrhage are also described.
Cardiac lesions as a result of variola infection were an infrequent occurrence. Multifocal myocardial and subendocardial haemorrhages were seen sometimes in haemorrhagic cases. Lymphohistiocytic and eosinophilic myocarditis and epicarditis are reported less frequently. Acute myocardial degeneration has also been reported, and Councilman et al. (1904) describe two cases in which locally extensive myocardial necrosis with intralesional bacteria were found.
Monkeypox in Man
Classification and Disease Course
Prior to the eradication of smallpox, human MPXV infections were likely misdiagnosed as VARV infections due to the prevalence of smallpox and the similarity of cutaneous disease presentation and progression. Monkeypox was not recognized as a disease distinct from smallpox until 1970 when the elimination of smallpox from the Democratic Republic of Congo revealed the continued occurrence of a smallpox-like disease (Fenner et al., 1988b). The clinical features of human monkeypox are similar to those of ordinary or modified smallpox, but disease severity varies among different virus strains. In general, strains originating from central Africa are more virulent than those originating from western Africa (Chen et al., 2005; Likos et al., 2005). Disease progression through the incubation period, pre-eruptive stage and rash is similar to smallpox, but the disease is milder with a lower case fatality rate (1.5–17%) (Jezek et al., 1987; Fenner et al., 1988b; Hutin et al., 2001; Huhn et al., 2005). In a review of 282 monkeypox patients in Zaire, the predominant type of skin lesion among non-vaccinated people was discrete (69%), followed by semiconfluent (23.4%) and confluent (7%) (Jezek et al.,1987). Similar trends were observed among patients with previous vaccination scars and no cases of haemorrhagic monkeypox were observed. Haemorrhagic monkeypox cases were not seen prior to the 2003 outbreak in the Midwestern USA where 2/34 patients developed haemorrhagic pustules, petechiae and/or purpura (Huhn et al., 2005); however, it is interesting to note that unlike haemorrhagic smallpox, the disease was mild with few lesions. Unlike smallpox, appreciable lymphadenopathy (particularly in the cervical and inguinal regions) is a prominent feature of monkeypox and occurs during the pre-eruptive stage (Breman et al., 1980; Jezek et al., 1987; Reed et al., 2004; Huhn et al., 2005). During the eruptive stage, ulcerative mucosal lesions result in tonsillitis, pharyngitis, laryngitis and subsequent dysphagia (Jezek et al., 1987; Reed et al., 2004; Sejvar et al., 2004; Huhn et al., 2005). Conjunctivitis, periorbital oedema and coughing (productive and non-productive) were also noted.
Clinical Pathology
Published serum biochemistry and haematology data from confirmed monkeypox cases are limited to the 2003 outbreak in the Midwestern USA (Huhn et al., 2005). Of 21 confirmed cases, 45% developed leucocytosis (9.13–26.8 × 109/l; reference range: 4.0–9.0 × 109/l); 50% developed mild to moderate hypoalbuminaemia (1.1–3.4 mg/dl; reference range: 3.5–5.5 mg/dl); and in 35% platelet counts were reduced (90–143 × 109/l; reference range: 150–400 × 109/l) (Huhn et al., 2005). All other parameters were within reference range or were clinically insignificant.
Gross Pathology
Due to the low case fatality rate and lack of necropsy examinations, little is known about the systemic pathology of human monkeypox. The cutaneous lesions have received the most attention, primarily through clinical examination and biopsy sampling (Stagles et al., 1985; Bayer-Garner, 2005). Grossly, the skin lesions assume a centrifugal distribution and progress through maculopapular, vesiculopustular and crusting stages that are indistinguishable from ordinary smallpox. Microscopical examination reveals all of the salient features of VARV infection including epidermal hyperplasia, ballooning degeneration of keratinocytes with intracytoplasmic inclusions, intraepidermal vesicles and pustules, and crust formation (Stagles et al., 1985; Bayer-Garner, 2005). Dermal changes are also similar to smallpox and include oedema and infiltration with lymphocytes, macrophages, and to a lesser extent, neutrophils and eosinophils. Ultrastructurally, intracytoplasmic immature and mature poxviral particles are readily apparent within keratinocytes (Stagles et al., 1985; Bayer-Garner, 2005).
Severe peripheral lymphadenopathy is often cited as the singular clinical feature which distinguishes monkeypox from smallpox (Arita et al., 1985; Jezek et al., 1987; Huhn et al., 2005; Parker et al., 2007). In some cases, the change is referred to specifically as lymphadenitis; however, no reports of the nodal histopathology can be found. This is unfortunate, and ironically, similar to smallpox with regard to the lack of information. The pathology of the internal organs in human monkeypox has not been described.
Smallpox in Macaques
Model Systems and Gross Pathology
Prior to the eradication of smallpox, little attention was paid to VARV infection in macaques. In 1906, Brinckerhoff and Tyzzer attempted to reproduce the disease in cynomolgus and pig-tailed macaques using seven different routes of inoculation: cutaneous, corneal and oral scarification; intratracheal; pulmonary; fomite and direct contact with a smallpox patient (Brinckerhoff and Tyzzer, 1906). In all cases, either subclinical or only mild disease developed. Later, as eradication efforts increased, isolated reports of naturally occurring smallpox in Old and New World primates raised concerns about the ability of these species to serve as natural reservoirs of the disease (Arita and Henderson, 1968). Studies were designed to test this possibility and most utilized a direct aerosol or indirect animal–animal or fomite–animal route of transmission that again resulted in only subclinical or mild disease (Hahon and Wilson, 1960; Hahon and McGavron, 1961; Noble and Rich, 1969; Noble, 1970). Notably, Westwood et al. (1966) administered an unknown dose of VARV (Higgins strain) via aerosol to rhesus macaques and observed a more pronounced clinical presentation than had previously been reported. Ultimately, non-human primates were determined to be an unlikely animal reservoir and studies were discontinued until the early 21st century when bioterrorism concerns intensified.
In 2004, Jahrling et al. revisited the potential of cynomolgus macaques to serve as an animal model of human smallpox. Using an intravenous (IV) route of administration and the Harper and India 7124 VARV strains, they found that 108 plaque-forming units (pfu) and 109 pfu produced clinical syndromes similar to ordinary and haemorrhagic smallpox, respectively (Jahrling et al., 2004). A follow-up study using the Harper strain and the same route of inoculation and doses revealed extensive details about the systemic pathology of ordinary and haemorrhagic smallpox in the cynomolgus macaque (Wahl-Jensen et al., 2011). Photomicrographs of the primary microscopical lesions seen in macaques with the ordinary and haemorrhagic forms of smallpox and monkeypox are shown in Fig. 1. The lesions were similar to those reported in the historical human literature and may help to clarify important differences between the two primary disease types. In the 108 pfu IV-injected cynomolgus macaque model (ordinary model), cutaneous lesions had a centrifugal distribution and progressed through typical maculopapular, vesiculopustular and crust stages that were grossly and histologically indistinguishable from their human ordinary smallpox counterparts. In the 109 pfu IV-injected cynomolgus macaque model (early haemorrhagic model), death occurred within 2–3 days post infection, and only very early stage cutaneous and mucosal lesions were present. Some animals developed a petechial rash similar to that seen in human early onset haemorrhagic disease. Splenic changes in the ordinary model were common and included diffuse congestion and expansion of the red pulp by large numbers of macrophages, lymphocytes and plasma cells. Mild lymphoid hyperplasia also developed. In the haemorrhagic model, the primary change was severe lymphoid depletion and necrosis accompanied by congestion, neutrophilic inflammation and intralesional coccoid bacteria. All of these splenic changes were reported in human smallpox, but the historical descriptions lack the clear distinction between disease types. There were also distinct differences in lymph node pathology in the ordinary and haemorrhagic models. In the ordinary model, lymphoid hyperplasia was the predominant change, while lymphoid necrosis was present in the haemorrhagic model. A similar pattern was present in the bone marrow with myeloid hyperplasia occurring in ordinary smallpox and haematopoietic necrosis occurring in haemorrhagic smallpox. Notably, this is also similar to what has been reported in the corresponding human conditions (Councilman et al., 1904; Bras, 1952). Additional findings that recapitulate the human disease accurately include lymphohistiocytic orchitis with seminiferous tubule degeneration, adrenocortical epithelial degeneration and necrotizing hepatitis with intralesional bacteria. Pulmonary changes were limited to acute interstitial pneumonia in the haemorrhagic model only and were attributed to secondary bacterial infection. Bronchopneumonia was not seen and may be a reflection of the route of administration. The macaque models of smallpox are summarized in Table 5.
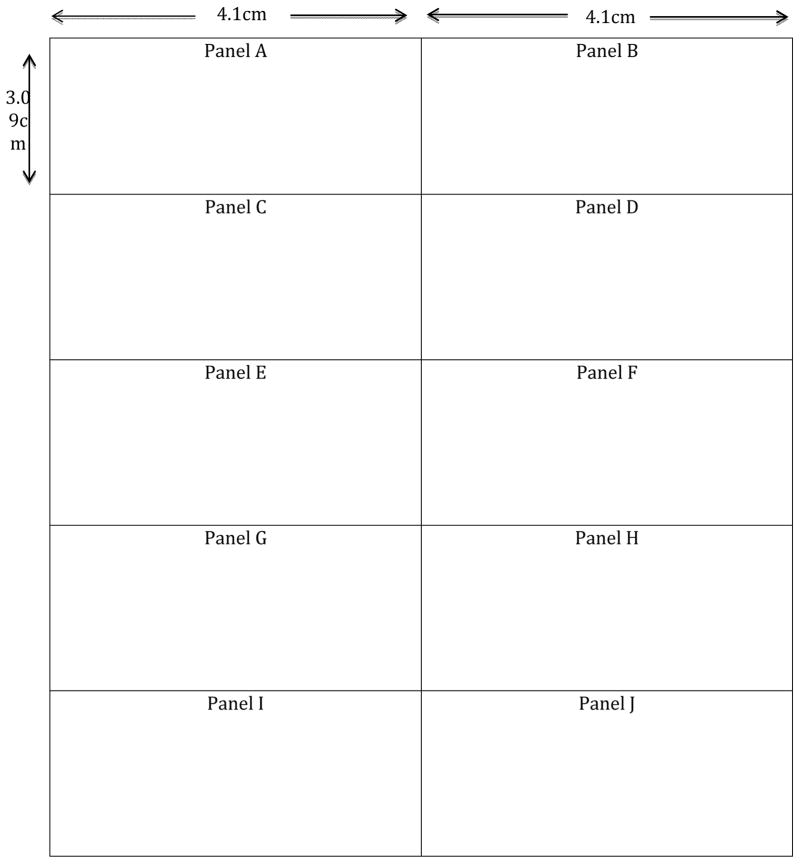
Fig. 1.
Primary lesions seen in ordinary (left) and haemorrhagic (right) smallpox and monkeypox in macaques. (A) Haired skin from a macaque with ordinary smallpox showing epidermal hyperplasia and intraepidermal vesiculation (*). A short expanse of normal non-hyperplastic epidermis is visible on the right. HE. Bar, 100um. (B) Haired skin from a macaque with haemorrhagic monkeypox showing focal haemorrhage in the subcutis (*); note the lack of proliferative and necrotizing epidermal lesions. HE. Bar, 200um. (C) Spleen from a macaque with ordinary monkeypox showing mild lymphoid hyperplasia as evidenced by scattered secondary follicles (*). HE. Bar, 200um. (D) Spleen from a macaque with haemorrhagic smallpox showing severe diffuse haemorrhage (red areas) and lymphoid necrosis (*). HE. Bar, 200um. (E) Lymph node from a macaque with ordinary smallpox showing marked lymphoid hyperplasia as evidenced by numerous secondary follicles (*). HE. Bar, 200um. (F) Lymph node from a macaque with haemorrhagic monkeypox showing multifocal follicular lymphoid necrosis (*). HE. Bar, 200um. (G) Bone marrow from a macaque with ordinary monkeypox showing diffuse myeloid hyperplasia. HE. Bar, 20um. (H) Bone marrow from a macaque with haemorrhagic smallpox showing haematopoietic necrosis (*) and haemorrhage (#). HE. Bar, 20um. (I) and (J) Testes from macaques with ordinary and haemorrhagic monkeypox, respectively, showing focal interstitial orchitis (*) and seminiferous tubule degeneration (#). HE. Bars, 100um.
Table 5.
Macaque models of smallpox
| Reference | Macaque species | n= | VARV (strain) | Inoculation dose | Route of inoculation | Disease type observed |
|---|---|---|---|---|---|---|
| Brinckerhoff and Tyzzer, 1906 |
M. cynomolgus M. nemestrina |
65 | VARV (unspecified strains collected from 10 patients with active smallpox) | Not specified | Cutaneous, corneal and oral scarification; intratracheal; pulmonary; fomite; direct smallpox patient contact | Mild ordinary or subclinical |
| Hahon and Wilson, 1960 | M. irus | 39 | VARV (strain not specified) | 5 × 104 IU | Aerosol | Mild ordinary |
| Hahon and McGavran, 1961 | M. irus | 5 | VARV (Yamada) | 1.8 × 106–3.4 ×106 IU | Aerosol | Mild ordinary |
| VARV (Lee) | 5.0 × 105–.0 ×106 IU | |||||
| Westwood et al., 1966 | M. mulatta (Indian origin) | 109 | VARV (Higgins) | Not specified | Aerosol | Ordinary |
| Noble and Rich, 1969 | M. irus | 22 | VARV (Harvey) | 5.0 × 106 pfu | Intranasal cage contact | Ordinary |
| Noble, 1970 | M. irus | 8 | VARV (Brazil Study 2) | 106 pfu | IN | Mild ordinary |
| VARV (Pakistan) | Not specified | IN | Mild ordinary | |||
| VARV (Utrecht 65–32) | 108 pfu | IN | Mild ordinary | |||
| VARV (Brazil Study 5) | 107 pfu | IM and IP | Mild to moderate ordinary | |||
| Jahrling et al., 2004 | M. fascicularis | 36 | VARV (Harper) | 108–109 pfu | IV | 106, 107, 108 pfu; ordinary |
| VARV (India 7124) | 106–109 pfu | IV | 109 pfu; haemorrhagic | |||
| Huggins et al., 2009 | M. fascicularis | 8 | VARV (Harper) | 108 pfu | IV | Unknown 108 pfu; ordinary |
| Wahl-Jensen et al., 2011 | M. fascicularis | 27 | VARV (Harper) | 108–109 pfu | IV | 109 pfu; ordinary or haemorrhagic |
IU, infectious units; IN, intranasal; IM, intramuscular; IP, intraperitoneal; IV, intravenous
Clinical Pathology
In 1962, Cheville et al. reported haematology data from macaques infected experimentally with VARV. They found that 3.2 × 107 pfu VARV (Yamada strain) administered IV to rhesus macaques (n = 2) produced mean total leucocyte counts of 10–15 × 109/l (reference range: 4.34–11.34 × 109/l), including 5.5–8.2 × 109/l lymphocytes (reference range: 1.34–3.53 × 109/l) over the course of infection; however, the mean total leucocyte baseline value obtained 6 days prior to inoculation was 12 × 109/l (Cheville et al., 1962). Huggins et al. (2009) reported that two cynomologus macaques inoculated IV with 108 pfu VARV (Harper strain) and not receiving antiviral treatment, had a circulating leucocytosis (23.9 ± 15.1 × 109/l; reference range: 7.1–21.7× 109/l) and hypoalbuminaemia (1.75 ± 0.49g/dl; reference range: 3.55–4.66 g/dl) at 11 days post inoculation (Huggins et al., 2009). No abnormalities in haematocrit, platelet count or mean corpuscular haemoglobin concentration, or the serum concentrations of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), blood urea nitrogen (BUN), creatinine or total protein were found. Jahrling et al. (2004) reported a more severe leucocytosis (up to 50 × 109/l) and monocytosis (>20%) in animals dying <6 days post inoculation (IV) with 108 or 109pfu VARV (Harper strain). Wahl-Jensen et al. (2011) evaluated two groups of cynomolgus macaques infected with either108pfu (n = 18) or 109pfu (n = 9) VARV (Harper strain). Haematological findings were similar in both groups and anaemia and leucocytosis (>30 ×109/l; reference range: 5–15×109/l) were the only significant changes. Similar to Huggins et al. (2009), and as in human monkeypox, hypoalbuminaemia (2–2.5 mg/dl; reference range: 2.6–4.2 mg/dl) was also seen.
Monkeypox in Macaques
Model Systems and Gross Pathology
Naturally occurring monkeypox in non-human primates was first reported in 1959 in a colony of cynomolgus macaques, and as no fatalities resulted, the only reported lesion was typical poxviral exanthema (von Magnus et al., 1959). In 1960, Prier and Sauer reported a naturally occurring outbreak involving both cynomolgus and rhesus macaques (Prier and Sauer, 1960). Clinical disease developed only in the cynomolgus macaques and although exact numbers were not reported, some fatalities occurred. Two disease presentations were described. The most common presentation was that of typical cutaneous disease with a tendency for the lesions to be haemorrhagic in fatal cases and in young animals. The second, less common presentation, included typical cutaneous lesions, ulcerative mucosal lesions, facial oedema and generalized lymphadenopathy. Histopathology was limited to the skin and lesions were indistinguishable from those found in human smallpox. Additional sporadic outbreaks in cynomolgus macaques were reported throughout the 1960s, but detailed pathological descriptions beyond the dermatopathology are lacking (Arita and Henderson, 1968).
Due to the inherent risks and difficulties of working with non-human primate models of smallpox, and in light of the zoonotic potential of MPXV, macaque models of monkeypox have been developed and are used commonly in vaccine and therapeutic drug studies (Huggins et al., 2009; Jordan et al., 2009; Shao et al., 2009; Zielinski et al., 2010; Hirao et al., 2011). As in the human condition, central African strains are more virulent than West African strains, and many models using different strains and different routes of infection have been explored (Chen et al., 2005; Likos et al., 2005). The most thorough description of the systemic pathology of monkeypox in the cynomolgus macaque was reported by Zaucha et al. (2001) who used a central African strain (Zaire) administered by aerosol via a head-only exposure chamber contained within a Class III biological safety cabinet; inhaled doses were 10,000–141,000 pfu. Primary gross findings included exanthema and enanthema, bronchopneumonia, pleuritis, peripheral lymphadenopathy, colitis and gastritis. Microscopical findings consistent with those described in human smallpox included typical cutaneous and mucosal lesions; fibrinonecrotic bronchopneumonia; necrotizing lymphadenitis, splenitis and tonsillitis; oesophagitis; necro-ulcerative gastroenteritis; necrotizing orchitis and oophoritis; and less commonly, necrotizing hepatitis. One animal developed concurrent bacterial septicaemia and myelitis with intralesional bacteria, also a reported finding in human smallpox. Immunohistochemical labelling for poxvirus antigen was positive in skin, oral mucosa, lung, trachea, larynx, lymph node, spleen, thymus, oesophagus, stomach, small intestine, colon, ovary and testis. Ultrastructurally, viral particles were found in skin, lung, lymph node, thymus and liver. In the bacteraemic animal only, the bone marrow was immunohistochemically and ultrastructurally positive. Additional studies that also used a central African strain administered either intratracheally or IV revealed similar findings (Stittelaar et al., 2005; Marriott et al., 2008; Goff et al., 2011). In the IV model, myocarditis and nephritis were also found. Recently, Nalca et al. (2010) reported divergent pathological findings in a cynomolgus macaque aerosol model (Zaire strain, 104–106 pfu). In that study, 13/18 animals reached endpoint criteria for humane destruction and widespread necrotizing lesions, similar to those described above, were found. The remaining five animals developed less severe disease in which lymphoid hyperplasia and plasmacytosis, as well as chronic pulmonary and dermal changes were seen; necrotizing lesions were not found.
Clinical Pathology
Limited haematological and serum biochemistry data are available from macaques infected experimentally with MPXV. Common findings that are consistent with human and/or macaque smallpox include leucocytosis, anaemia and hypoalbuminaemia (Zaucha et al., 2001; Hooper et al., 2004; Marriott et al., 2008; Huggins et al., 2009; Nalca et al., 2010). Occasional individual animals also developed elevated ALP, AST, BUN or creatinine concentrations (Hooper et al., 2004). Unlike human smallpox, thrombocytopenia has not been reported.
Discussion
Early natural disease investigations and modern bioterrorism concerns have resulted in the use of various macaque models of smallpox and monkeypox. The early- to mid-20th century macaque models paled in comparison with the human disease in both transmissibility and severity; and thus, cast doubt on whether VARV was the best orthopoxvirus species to use in a non-human primate. Monkeypox is generally a more severe disease in macaques, making it a seemingly good surrogate for smallpox in man; however, questions still remain as to whether monkeypox in macaques accurately recapitulates all aspects of human smallpox. More recent IV models using VARV or MPXV have been successful in producing a more severe clinical presentation, but the natural route of infection and primary viraemia are bypassed. Thus, a macaque model that replicates all aspects of human smallpox does not exist. However, many of the salient features of the disease can be consistently reproduced, and when used in carefully designed studies, they may provide important information about orthopoxvirus pathogenesis. Similarly, while no animal model can predict safety and efficacy of a medical countermeasure with 100% certainty, these models can help in situations where it is unethical to conduct testing in man.
An important, but often overlooked variable to consider in smallpox/monkeypox animal model development, is the major disease type (i.e. ordinary versus haemorrhagic). In human smallpox, the incidence, mortality and clinical presentation of ordinary smallpox differed dramatically from haemorrhagic smallpox. Yet, many reports utilizing a macaque model do not specifically classify the type of disease produced by their particular combination of host species, virus/strain, dose, route of inoculation, etc. Given that the pathogenesis of ordinary smallpox likely differs from haemorrhagic smallpox in many ways, it is important that basic research and immunopathogenesis studies define clearly the type of disease being investigated. Similarly, medical countermeasure studies should define clearly the type of disease being modelled, as there is no evidence to support the assumption that efficacy in ordinary smallpox equates to efficacy in haemorrhagic smallpox.
Another important variable in model development is the target population. Known risk factors in human smallpox include immunosuppression, chronic skin diseases and pregnancy. Next generation countermeasure development is often directed toward these at risk populations, yet few studies define the degree of risk among their animal research subjects. Given that retroviral and herpes B virus infections are common in many populations of macaques, these variables should be taken into consideration when designing animal model efficacy studies. Chronic skin diseases also occur in macaques, but they are often overlooked due to masking of the lesions by the natural hair coat.
The role of secondary bacterial infections in smallpox and monkeypox is poorly understood. Despite the documented incidence of staphylococcal, streptococcal and pneumococcal infections in fatal cases of human smallpox; and the reported observation of unspecified bacterial infections in experimentally-infected macaques; to date, no prospective studies have addressed this issue. The pathology findings suggest that systemic bacterial infections are more common in haemorrhagic smallpox, and it is possible that they occur exclusively in this form of the disease. If so, this would suggest that haemorrhagic smallpox may be the result of a secondary bacterial infection superimposed on the viral infection in an immunosuppressed host. Alternatively, a preexisting subclinical infection or peculiarities related to the host microbiome may allow for unabated viral spread. Prospective studies are needed to explore these possibilities further.
In summary, many important questions about naturally occurring smallpox remain unanswered. Some facets of smallpox pathogenesis, such as the natural route of infection, the site of primary viral replication and the role of concurrent bacterial infections, have been discussed in the literature for over 100 years, yet definitive answers are still lacking. In addition, our understanding of the systemic pathology of human smallpox is severely limited. Smallpox eradication occurred prior to the advent of modern molecular techniques, such as immunohistochemistry and in-situ hybridization, and the histopathological descriptions reported in the historical literature contain antiquated and imprecise terminology and interpretations; photomicrographs are strikingly absent. Carefully designed macaque models provide a means to fill these gaps using modern technology, and together with a solid study design, they may help to identify novel therapeutic targets. These models are also indispensable for testing the safety and efficacy of new vaccines and therapeutics, as well as for fulfilling regulatory requirements such as the ‘Animal Rule’ (FDA 21 CFR 601.90).
Acknowledgments
The authors wish to thank J. Kuhn, D. Perry, D. Ragland and A. Johnson for thoughtful discussions and critique; and L. Bollinger for technical assistance. JAC performed this work as an employee of Charles River Laboratories and VWJ as an employee of Tunnell Consulting, Inc., both subcontractors to Battelle Memorial Institute under its prime contract HHSN2722007000161 with NIAID.
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest with regard to the current submission.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anonymous. Update: multistate outbreak of monkeypox – Illinois, Indiana, Kansas, Missouri, Ohio and Wisconsin, 2003. Journal of the American Medical Association. 2003;290:325–327. [Google Scholar]
- Alcami A, Smith GL. A mechanism for the inhibition of fever by a virus. Proceedings of the National Academy of Sciences USA. 1996;93:11029–11034. doi: 10.1073/pnas.93.20.11029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arita I, Henderson DA. Smallpox and monkeypox in non-human primates. Bulletin of the World Health Organization. 1968;39:277–283. [PMC free article] [PubMed] [Google Scholar]
- Arita I, Jezek Z, Khodakevich L, Ruti K. Human monkeypox: a newly emerged orthopoxvirus zoonosis in the tropical rain forests of Africa. American Journal of Tropical Medicine and Hygiene. 1985;34:781–789. doi: 10.4269/ajtmh.1985.34.781. [DOI] [PubMed] [Google Scholar]
- Balaji D. Osteomyelitis variolosa: a case report. Journal of Orthopaedic Surgery (Hong Kong) 2011;19:120–122. doi: 10.1177/230949901101900128. [DOI] [PubMed] [Google Scholar]
- Bayer-Garner IB. Monkeypox virus: histologic, immunohistochemical and electron-microscopic findings. Journal of Cutaneous Pathology. 2005;32:28–34. doi: 10.1111/j.0303-6987.2005.00254.x. [DOI] [PubMed] [Google Scholar]
- Bras G. The morbid anatomy of smallpox. Documenta de Medicina Geographica et Tropica. 1952;4:303–351. [PubMed] [Google Scholar]
- Breman JG, Kalisa R, Steniowski MV, Zanotto E, Gromyko AI, et al. Human monkeypox, 1970–79. Bulletin of the World Health Organization. 1980;58:165–182. [PMC free article] [PubMed] [Google Scholar]
- Brinckerhoff WR, Tyzzer EE. Studies upon experimental variola in monkeys (Macacus cynomologus and M. nemestrinus) and in the orangutan (Simia Satyrus): Part II. Journal of Medical Research. 1906;14:263–320. [PMC free article] [PubMed] [Google Scholar]
- Chen N, Li G, Liszewski MK, Atkinson JP, Jahrling PB, et al. Virulence differences between monkeypox virus isolates from West Africa and the Congo basin. Virology. 2005;340:46–63. doi: 10.1016/j.virol.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheville NF, Marshall RG, Janssen RJ, Gerone PJ. The effect of 6-mercaptopurine on variola infections in rhesus monkeys. II. Hematological studies. Journal of Infectious Disease. 1962;111:163–166. doi: 10.1093/infdis/111.2.163. [DOI] [PubMed] [Google Scholar]
- Chiari H. Ueber osteomyelitis variolosa. Beitrage zur Pathologischen Anatomie und zur allgemeinen Pathologie. 1893;13:13–31. [PubMed] [Google Scholar]
- Cockshott P, Macgregor M. Osteomyelitis variolosa. Quarterly Journal of Medicine. 1958;27:369–387. [PubMed] [Google Scholar]
- Councilman WT, Magrath GB, Brinckerhoff WR. The pathological anatomy and histology of variola. Journal of Medical Research. 1904;11:12–135. [PMC free article] [PubMed] [Google Scholar]
- Curschmann H. Cyclopaedia of the Practice of Medicine. Sampson Low, Marston, Low & Searle; London: 1875. Smallpox; pp. 320–401. [Google Scholar]
- Dixon CW. Smallpox. J&A Churchill; London: 1962. pp. 5–56. [Google Scholar]
- Esposito JJ, Sammons SA, Frace AM, Osborne JD, Olsen-Rasmussen M, et al. Genome sequence diversity and clues to the evolution of variola (smallpox) virus. Science. 2006;313:807–812. doi: 10.1126/science.1125134. [DOI] [PubMed] [Google Scholar]
- Essbauer S, Pfeffer M, Meyer H. Zoonotic poxviruses. Veterinary Microbiology. 2010;140:229–236. doi: 10.1016/j.vetmic.2009.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estep RD, Messaoudi I, O’Connor MA, Li H, Sprague J, et al. Deletion of the monkeypox virus inhibitor of complement enzymes locus impacts the adaptive immune response to monkeypox virus in a nonhuman primate model of infection. Journal of Virology. 2011;85:9527–9542. doi: 10.1128/JVI.00199-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID. Smallpox and Its Eradication. WHO; Geneva: 1988a. The clinical features of smallpox; pp. 1–68. [Google Scholar]
- Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID. Smallpox and Its Eradication. WHO; Geneva: 1988b. Human monkeypox and other poxvirus infections in man; pp. 1287–1320. [Google Scholar]
- Fenner F, Henderson DA, Arita I, Jezek Z, Ladnyi ID. Smallpox and Its Eradication. WHO; Geneva: 1988c. Potential sources for a return of smallpox; pp. 1345–1370. [Google Scholar]
- Goff AJ, Chapman J, Foster C, Wlazlowski C, Shamblin J, et al. A novel respiratory model of infection with monkeypox virus in cynomolgus macaques. Journal of Virology. 2011;85:4898–4909. doi: 10.1128/JVI.02525-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahon N, McGavran GM. Air-borne infectivity of the variola-vaccinia group of poxviruses for the cynomolgus monkey, Macaca irus. Journal of Infectious Disease. 1961;109:294–298. doi: 10.1093/infdis/109.3.294. [DOI] [PubMed] [Google Scholar]
- Hahon N, Wilson BJ. Pathogenesis of variola in Macaca irus monkeys. American Journal of Hygiene. 1960;71:69–80. doi: 10.1093/oxfordjournals.aje.a120091. [DOI] [PubMed] [Google Scholar]
- Haviland JW. Purpura variolosa; its manifestations in skin and blood. Yale Journal of Biology and Medicine. 1952;24:518–524. [PMC free article] [PubMed] [Google Scholar]
- Hirao LA, Wu L, Satishchandran A, Khan AS, Draghia-Akli R, et al. Comparative analysis of immune responses induced by vaccination with SIV antigens by recombinant Ad5 vector or plasmid DNA in rhesus macaques. Molecular Therapeutics. 2011;18:1568–1576. doi: 10.1038/mt.2010.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper JW, Thompson E, Wilhelmsen C, Zimmerman M, Ichou MA, et al. Smallpox DNA vaccine protects nonhuman primates against lethal monkeypox. Journal of Virology. 2004;78:4433–4443. doi: 10.1128/JVI.78.9.4433-4443.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins J, Goff A, Hensley L, Mucker E, Shamblin J, et al. Nonhuman primates are protected from smallpox virus or monkeypox virus challenges by the antiviral drug ST-246. Antimicrobial Agents and Chemotherapy. 2009;53:2620–2625. doi: 10.1128/AAC.00021-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhn GD, Bauer AM, Yorita K, Graham MB, Sejvar J, et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clinical Infectious Disease. 2005;41:1742–1751. doi: 10.1086/498115. [DOI] [PubMed] [Google Scholar]
- Hutin YJ, Williams RJ, Malfait P, Pebody R, Loparev VN, et al. Outbreak of human monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerging Infectious Diseases. 2001;7:434–438. doi: 10.3201/eid0703.010311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda K. The blood in purpuric smallpox. Clinical review of forty-eight cases. Journla of the American Medical Association. 1925;84:1807–1813. [Google Scholar]
- Jahrling PB, Hensley LE, Martinez MJ, Leduc JW, Rubins KH, et al. Exploring the potential of variola virus infection of cynomolgus macaques as a model for human smallpox. Proceedings of the National Academy of Sciences USA. 2004;101:15196–15200. doi: 10.1073/pnas.0405954101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jezek Z, Szczeniowski M, Paluku KM, Mutombo M. Human monkeypox: clinical features of 282 patients. Journal of Infectious Disease. 1987;156:293–298. doi: 10.1093/infdis/156.2.293. [DOI] [PubMed] [Google Scholar]
- Jordan R, Goff A, Frimm A, Corrado ML, Hensley LE, et al. ST-246 antiviral efficacy in a nonhuman primate monkeypox model: determination of the minimal effective dose and human dose justification. Antimicrobial Agents and Chemotherapy. 2009;53:1817–1822. doi: 10.1128/AAC.01596-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keasey S, Pugh C, Tikhonov A, Chen G, Schweitzer B, et al. Proteomic basis of the antibody response to monkeypox virus infection examined in cynomolgus macaques and a comparison to human smallpox vaccination. PLoS One. 2010;5:e15547. doi: 10.1371/journal.pone.0015547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keysselitz G, Mayer M. Ueber zellveranderungen in inneren organen bei variola. Archiv Fuer Schiffs- und Tropen-Hygiene. 1909;13:75. [Google Scholar]
- Khodakevich L, Jezek Z, Kinzanzka K. Isolation of monkeypox virus from wild squirrel infected in nature. Lancet. 1986;1:98–99. doi: 10.1016/S0140-6736(86)90748-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khodakevich L, Jezek Z, Messinger D. Monkeypox virus: ecology and public health significance. Bulletin of the World Health Organization. 1988;66:747–752. [PMC free article] [PubMed] [Google Scholar]
- Khodakevich L, Szczeniowski M, Manbu ma D, Jezek Z, Marennikova S, et al. The role of squirrels in sustaining monkeypox virus transmission. Tropical and Geographical Medicine. 1987;39:115–122. [PubMed] [Google Scholar]
- Koplan JP, Monsur KA, Foster SO, Huq F, Rahaman MM, et al. Treatment of variola major with adenine arabinoside. Journal of Infectious Disease. 1975;131:34–39. doi: 10.1093/infdis/131.1.34. [DOI] [PubMed] [Google Scholar]
- Likos AM, Sammons SA, Olson VA, Frace AM, Li Y, et al. A tale of two clades: monkeypox viruses. Journal of General Virology. 2005;86:2661–2672. doi: 10.1099/vir.0.81215-0. [DOI] [PubMed] [Google Scholar]
- Lillie RD. Smallpox and vaccinia. The pathologic histology. Archives of Pathology. 1930;10:241–291. [Google Scholar]
- Marriott KA, Parkinson CV, Morefield SI, Davenport R, Nichols R, et al. Clonal vaccinia virus grown in cell culture fully protects monkeys from lethal monkeypox challenge. Vaccine. 2008;26:581–588. doi: 10.1016/j.vaccine.2007.10.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie PJ, Githens JH, Harwood ME, Roberts JF, Rao AR, et al. Haemorrhagic smallpox. 2. Specific bleeding and coagulation studies. Bulletin of the World Health Organization. 1965;33:773–782. [PMC free article] [PubMed] [Google Scholar]
- Mehta BC, Doctor RG, Purandare NM, Patel JC. Hemorrhagic smallpox. A study of 22 cases to determine the cause of bleeding. Indian Journal of Medical Science. 1967;21:518–523. [PubMed] [Google Scholar]
- Mitra M, Bhattacharya DK. Some observations on haemorrhagic smallpox (Type I) Journal of the Indian Medical Association. 1976;67:237–240. [PubMed] [Google Scholar]
- Nalca A, Livingston VA, Garza NL, Zumbrun EE, Frick OM, et al. Experimental infection of cynomolgus macaques (Macaca fascicularis) with aerosolized monkeypox virus. PLoS One. 2010;5 doi: 10.1371/journal.pone.0012880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble J., Jr A study of New and Old World monkeys to determine the likelihood of a simian reservoir of smallpox. Bulletin of the World Health Organization. 1970;42:509–514. [PMC free article] [PubMed] [Google Scholar]
- Noble J, Jr, Rich JA. Trsmission of smallpox by contact and by aerosol routes in Macaca irus. Bulletin of the World Health Organization. 1969;40:279–286. [PMC free article] [PubMed] [Google Scholar]
- Parker S, Nuara A, Buller RM, Schultz DA. Human monkeypox: an emerging zoonotic disease. Future Microbiology. 2007;2:17–34. doi: 10.2217/17460913.2.1.17. [DOI] [PubMed] [Google Scholar]
- Prier JE, Sauer RM. A pox disease of monkeys. Annals of the New York Academy of Science. 1960;85:951–959. doi: 10.1111/j.1749-6632.1960.tb50015.x. [DOI] [PubMed] [Google Scholar]
- Rao AR. Smallpox. Kothari Book Depot; Bombay: 1972. pp. 2–28. [Google Scholar]
- Reed KD, Melski JW, Graham MB, Regnery RL, Sotir MJ, et al. The detection of monkeypox in humans in the western hemisphere. New England Journal of Medicine. 2004;350:342–350. doi: 10.1056/NEJMoa032299. [DOI] [PubMed] [Google Scholar]
- Roberts JF, Coffee G, Creel SM, Gaal A, Githens JH, et al. Haemorrhagic smallpox. I. Preliminary haematological studies. Bulletin of the World Health Organization. 1965;33:607–613. [PMC free article] [PubMed] [Google Scholar]
- Sejvar JJ, Chowdary Y, Schomogyi M, Stevens J, Patel J, et al. Human monkeypox infection: a family cluster in the midwestern United States. Journal of Infectious Disease. 2004;190:1833–1840. doi: 10.1086/425039. [DOI] [PubMed] [Google Scholar]
- Shao L, Huang D, Wei H, Wang RC, Chen CY, et al. Expansion, reexpansion, and recall-like expansion of Vγ2Vδ2 T cells in smallpox vaccination and monkeypox virus infection. Journal of Virology. 2009;83:11959–11965. doi: 10.1128/JVI.00689-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shchelkunov SN, Totmenin AV, Babkin IV, Safronov PF, Ryazankina OI, et al. Human monkeypox and smallpox viruses: genomic comparison. FEBS Letters. 2001;509:66–70. doi: 10.1016/S0014-5793(01)03144-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stagles MJ, Watson AA, Boyd JF, More IA, McSeveney D. The histopathology and electron microscopy of a human monkeypox lesion. Transcripts of the Royal Society of Tropical Medicine and Hygiene. 1985;79:192–202. doi: 10.1016/0035-9203(85)90333-5. [DOI] [PubMed] [Google Scholar]
- Stittelaar KJ, van Amerongen G, Kondova I, Kuiken T, van Lavieren RF, et al. Modified vaccinia virus Ankara protects macaques against respiratory challenge with monkeypox virus. Journal of Virology. 2005;79:7845–7851. doi: 10.1128/JVI.79.12.7845-7851.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Magnus P, Andersen EK, Petersen KB, Birch-Andersen A. A pox-like disease in cynomolgus monkeys. Acta Pathologica Microbiologica Scandinavica. 1959;46:156–176. [Google Scholar]
- Wahl-Jensen V, Cann JA, Rubins KH, Huggins JW, Fisher RW, et al. Progression of pathogenic events in cynomolgus macaques infected with variola virus. PLoS One. 2011;6:e24832. doi: 10.1371/journal.pone.0024832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westwood JC, Boulter EA, Bowen ET, Maber HB. Experimental respiratory infection with poxviruses. I. Clinical virological and epidemiological studies. British Journal of Experimental Pathology. 1966;47:453–465. [PMC free article] [PubMed] [Google Scholar]
- Zaucha GM, Jahrling PB, Geisbert TW, Swearengen JR, Hensley L. The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis) Laboratory Investigation. 2001;81:1581–1600. doi: 10.1038/labinvest.3780373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielinski RJ, Smedley JV, Perera PY, Silvera PM, Waldmann TA, et al. Smallpox vaccine with integrated IL-15 demonstrates enhanced in vivo viral clearance in immunodeficient mice and confers long term protection against a lethal monkeypox challenge in cynomolgus monkeys. Vaccine. 2010;28:7081–7091. doi: 10.1016/j.vaccine.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]