Abstract
The current emphasis on preventive health care and wellness services suggests that measures of skills and competencies needed to effectively navigate the health care system need to be better defined. We take an expanded perspective of health literacy and define it as a set of skills used to organize and apply health knowledge, attitudes and practices relevant when managing one’s health environment. It is an emerging area of inquiry especially among adults and those with chronic conditions; however, it has been less studied among adolescent populations. To begin operationalizing this concept in a manner appropriate for teens in a health systems context, we explored knowledge, attitudes and practices related to health and preventive health care in 12 focus groups with publicly insured adolescents (N = 137), aged 13–17 years, as well as eight key informant interviews with physicians who serve publicly insured teens. Five dimensions emerged that provide a preliminary framework for an expanded definition of health literacy among adolescents. These include: (i) navigating the system, (ii) rights and responsibilities, (iii) preventive care, (iv) information seeking and (v) patient–provider relationship. This robust definition of health literacy contextualizes the concept in a health environment where individuals must be informed and skilled health care consumers.
Introduction
Access to and use of preventive health care services has become the norm in primary care in the United States over the past few decades, especially in the context of third-party payer and managed health care systems. However, among adolescent populations, use of preventive health care services has lagged [1] despite the development and promotion of the Annual Adolescent Well-Care Visit, a benefit covered by adolescent health insurance [2, 3]. At present, 92% of American adolescents have comprehensive health insurance [4]. In California where this study was conducted, 93% of adolescents have some form of health insurance [5].
Despite insurance coverage and availability of preventive health care benefits, data suggest that only 40.1% of publicly insured California adolescents attended a well-care visit in the previous year [6]. Additionally, adolescents with health insurance in California use the emergency room for health care at a rate higher (22.2%) than adolescents with no health insurance (18.7%) [5]. These data suggest that having health insurance alone does not ensure appropriate health care seeking behavior or health service utilization among adolescent populations. Rather, additional skills and competencies may be needed for this group of health care clients to effectively navigate the health care system and use health insurance benefits. We define these skills as components of an expanded definition of health literacy.
Many factors other than health insurance coverage influence the use of health care services among adolescent populations. Coker and colleagues [7] found that the clinician–patient relationship, geographic accessibility of services and perceptions of confidentiality were critical determinants in the appropriate and effective use of preventive health care services among adolescents. However, work in this field has focused primarily on identifying barriers to accessing health services as opposed to abilities and competencies needed to effectively navigate and utilize the system. Thus, to better understand an expanded, asset-based perspective of health literacy among generally healthy populations, we explored knowledge, attitudes and practices related to preventive and curative health care experiences and use among low-income adolescents who have publicly funded insurance in California.
Health literacy: history and conceptual definition
Traditionally, health literacy has been viewed as a derivative of literacy based upon skills in reading and numeracy [8, 9]. Past studies have found that in a health care setting, patients with low health literacy generally have lower levels of screening and medication adherence rates as well as poorer health outcomes [10–12]. This research relies on a narrow understanding of health literacy that emerged from clinical observations related to the gap between patient reading abilities and health education materials [13]. In this context, health literacy is viewed from a risk-factor perspective in that the medical encounter is tailored to patient literacy skills to maximize patient comprehension and ultimately successful treatment.
More recently, the definition of health literacy has expanded to take on a health promotion perspective. This perspective defines health literacy as the capacity to obtain, process and understand basic health information and services required to make informed decisions that will allow health-enhancing actions at the individual, social, and environmental levels [14–17]. In this sense, health literacy is viewed as an asset and a capacity that can be used to navigate through a complex health care system as well as in the broader health environment outside of the clinical context [18–21]. Parker and Ratzen [22] provide a framework that recognizes the dynamic nature of the construct, showing that health literacy occurs when the skills and abilities of those requiring health information and services are aligned with the demand and complexity of health information and services. However, the mechanisms through which the expanded definition of health literacy affects health behavior and health status remain less clear than the narrow definition, particularly in the health care setting [19, 23, 24].
Because of its origins in clinical care [13], health literacy emerged from empirical findings rooted in reading abilities and has not yet undergone theoretical development, making it more susceptible to conceptual drift. Many theories in health behavior posit that health knowledge is necessary but not sufficient for behavior change [25]. Concepts such as self-efficacy, motivation, intention and empowerment have been developed through theory in an attempt to predict and facilitate behavior change. Health literacy shares many similarities with these concepts, but must be defined distinctively so as not to risk being labeled as ‘new wine in old bottles’ [26]. For example, increased self-efficacy in an individual is likely to facilitate communication from patient to provider due to increased confidence. Health literacy, then, are the cognitive and social skills needed to communicate and articulate health needs and preferences. Additional theoretical development and application is needed to further advance the evolving concept of health literacy, particularly how it relates to other concepts of health behavior change.
Health literacy and adolescents
Despite an emerging interest in health literacy among adolescents [27–29], most studies have focused on adult populations. First, adults have higher health service utilization rates than adolescents, making them a higher priority when examining health literacy from a risk factor perspective. Because this perspective focuses on the clinical encounter, targeting higher utilizers of care such as adults does have a greater impact on health outcomes and health care expenditure. However, this neglects the impact of building health-literacy capacities among healthy, generally younger populations to mitigate or improve future health outcomes and expenditures.
Second, there is an assumption that adults serve as gatekeepers and guides for adolescents to help navigate the system. However, in a study examining the effect of parental health literacy on child health utilization among a population with asthma, parental health literacy was not associated with measures of child health care use [30]. Moreover, especially for first- and second-generation immigrant families who often must use public insurance, this may be an inaccurate assumption because these families may have limited history and interaction with the American health care system [31–34].
Moreover, there is a tendency to focus on barriers related to access and utilization of health services among adolescent populations, neglecting broader competencies that may facilitate the health care encounter. Studies have found that during preventive well-care visits, clinicians may not complete all recommended dimensions of the visit or may not discuss issues that are relevant to the adolescent patient [35–37]. Thus, health-literate adolesecents may be more equipped to ask questions and bring up health issues that are important to them.
Further limiting health-literacy research among adolescent populations is the lack of appropriate measures of the concept. The few standardized measures of health literacy either rely too heavily on a narrow definition of the concept or have not been adequately tested among adolescent populations [38–42]. However, a few studies have contextualized health literacy from an educational perspective and have begun to develop correlates of the concept [27, 29, 43]. Wu and colleagues have developed a classroom-based, health-literacy tool for adolescents that measures the ability to understand and evaluate health information [43]. However, it may be difficult to draw insights related to navigating health systems from measures developed for the classroom setting. Moreover, there is a tendency to develop ‘performance-based’ measures in educational settings that capture similar dimensions as traditional literacy-focused measures—validating such measures through correlations with a student’s grade point average and academic skills may bias findings towards the student’s general aptitude instead of broader health-literacy competencies.
In general, little is known about how an expanded understanding of health literacy varies among adolescents from a health systems perspective [28]. The lack of expanded measures of health literacy has to some extent hindered this area of research. Therefore, there is a need for studies to first, define, and second, reliably measure broader dimensions of the concept that are relevant to adolescents as well as other generally healthy populations [21].
The purpose of this article is to describe dimensions of an asset-based perspective of health literacy to better inform the operational understanding of how the expanded concept functions in the health systems environment. We will do so by exploring and describing through a health-literacy lens the interactions and experiences of adolescents when navigating the health care system. This effort is part of a larger study examining the effectiveness of an intervention focused on improving health literacy among adolescents. Additionally, practitioners, health plans and the public health community may be able to use our findings to better understand how adolescents consume health and health information, ultimately helping them tailor well-care visits as well as insurance benefits to meet the needs of this population.
Methods
Research design and sampling methodology
The goal of the larger, intervention-based study was to improve health literacy among publicly insured adolescents who are members of a large health plan; thus, our target population for the formative research process included low-income, publicly insured adolescents. Based on expert knowledge and existing networks with project staff, nine community sites from across California were identified through purposive sampling procedures as potential sites to conduct focus group discussions [44]. Sites consisted of community centers and clinics and were considered eligible for study participation if they provided services to eligible low-income adolescents. For this study, eligible low-income adolescents are defined as youth aged 13–17 years who are recipients of public health insurance, namely Medi-Cal (Medicaid) and Healthy Families (State Children’s Health Insurance Program).
Based on eligibility requirements as well as schedule availability, four sites were chosen to participate in winter 2010. The sites were dispersed across California, including one northern, two central and one southern. The geographic variation allows us to better generalize results to California adolescents, as opposed to one specific region of California adolescents.
Recruitment flyers were posted around each community site 1–2 weeks prior to focus group discussions. Flyers contained contact information of both the community site liaison as well as the project manager so that interested parents and adolescents could receive more information about the study. Consent and assent forms were distributed at the community site prior to focus group discussions and were made available in both English and in Spanish. Prior to focus group participation, completed consent forms were required from parents as well as assent forms from adolescents. A small incentive ($25 gift card) was used to facilitate recruitment and participation.
To supplement the focus group findings as well as to present a provider perspective, key informant interviews were conducted during the winter of 2010 with primary care physicians (PCPs) from across California. Thirty-six PCPs who were members of a large health plan in California were identified who met the eligibility criteria of serving a high number of publicly insured adolescents. Based on provider availability, eight PCPs consisting of seven pediatricians and one family medicine physician were interviewed by phone for 30 minutes by one trained project member.
Participants and procedure
Twelve focus group discussions were conducted across the four community sites during the winter of 2010; six focus groups were conducted with adolescents aged 13–14 years and six were conducted with adolescents aged 15–17 years. Each focus group included both males and females and consisted of 10–12 participants for a total of 137 adolescents. Focus groups were divided by age for two reasons: (i) middle school-aged adolescents are at different stages of maturity (both socially and physically) compared with high-school-aged adolescents and (ii) due to recruitment limitations, we would not have had enough participants in each discussion had we divided them based on both age and gender. Moreover, our focus group guides centered on preventive care and wellness visits and did not explicitly ask about reproductive health issues or other sensitive subjects. That said, we understand that reproductive health issues are at the forefront of teens’ health concerns; therefore, this is a limitation in our study [45].
All focus groups were conducted in English by trained moderators who attended a training that oriented them to procedures and script so as to minimize the variation in manner and style of discussion-leading. Two trained moderators were present at each focus group; one served as the discussion facilitator, whereas the other served as a silent note taker, recording non-verbal group observations as well as helping with logistics during the discussion.
The discussion guides for both the focus group and key informant interviews were developed based upon prior literature in the field that focused on adolescent interactions with the health care system and a patient-perspective of health literacy [18, 28]. Additionally, we used Andersen’s Behavioral Model and Access to Medical Care [46] as well as expert experience to design and solicit information about adolescent interactions with the health care system and health providers. Sample questions from the focus group guide and informant interview can be found in Table I.
Table I.
Sample themes and questions from the focus group guide and informant interviews
| Focus group guide |
| Going to the doctor |
|
| Health information |
|
| Rights and responsibilities |
|
| Informant interview |
| Doctor–patient relations |
|
| Adolescent preventive care |
|
| Health care utilization |
|
Parental consent and adolescent assent were obtained for all adolescent participants, as well as consents from each key informant. The UCLA Institutional Review Board approved the study.
Analysis
All focus groups and key informant interviews were recorded with audio equipment and later transcribed verbatim for coding purposes. Based on grounded theory, we used both open coding and theoretical coding procedures to allow for unanticipated, latent themes to emerge as well as to integrate existing models and theories of behavior change and health care interactions [46–49]. Using this coding process, a codebook was developed and organized in a framework of eleven families of codes. These were: Health Issues, Knowledge and Attitudes, Barriers, Benefits, Behaviors, Digital Knowledge, Digital Barriers, Digital Benefits, Digital Behavior, Website Development and Other.
The five study authors coded the 12 focus groups in pairs using Atlas.ti. This allowed us to individually annotate text data using the code families and ultimately converge the data to highlight similar as well as dissimilar annotations. Using a coding scheme based on these 11 families, we obtained a kappa of 0.849, indicating a strong agreement between coders [50]. Three study authors used the same coding scheme to code the key informant interviews. During an iterative process using a cross between selective and open coding methods [47], five dominant themes emerged from the family codes that provide the framework for reporting on how adolescents organize and apply health knowledge, attitudes, and practices within the health care setting. They include: (i) navigating the health care system, (ii) rights and responsibilities, (iii) preventive care, (iv) information-seeking and (v) patient–provider relationships.
Sociodemographics
The mean age of participants was 15.1 years and the gender representation was nearly equal across all focus groups, with just over 51% identifying as female. Adolescents who identified as Hispanic or Latino represented the largest racial category at just over 60%, reflecting California’s large Hispanic or Latino population relative to other states in the United States as well as enrollment patterns in government-sponsored health insurance programs in California [5]. Most adolescents indicated receiving Medi-Cal insurance (60%), demonstrating that a majority of our sample was from very low-income households. Table II describes the characteristics of the focus group participants.
Table II.
Descriptive statistics of the adolescent health literacy focus group participants (n = 137)
| Age, mean (SD) | 15.1 (1.5) |
| Gender, n (%) | |
| Male | 66 (48.2%) |
| Female | 71 (51.8%) |
| Race/ethnicity, n (%) | |
| African American | 34 (24.8%) |
| Asian American | 8 (5.8%) |
| Caucasian | 4 (2.9%) |
| Hispanic or Latino | 83 (60.6%) |
| Other or multi | 8 (5.8%) |
| Type of insurance, n (%) | |
| Medi-Cala | 82 (59.9%) |
| Healthy Familiesb | 22 (16.1%) |
| Other | 11 (8.0%) |
| None | 5 (3.6%) |
| Don’t know | 17 (12.4%) |
aEligibility for children aged 6–18 years in CA: income 100% of the Federal Poverty Level (FPL) or less.
bEligibility for children under the age of 19 in CA: income 250% of FPL or less.
Results
Results highlight interactions and experiences of adolescents’ knowledge, attitudes and practices relevant in the health care system and are framed through a health-literacy lens. That is, emphasis is placed on experiences and perceptions that relate to cross-cutting competencies within managed health care systems. We present both focus group and informant data together to help verify and validate our analysis. Thus, we are able to examine the consistency of findings generated by different data collection methods and sources (triangulation) [51].
Navigating the health care system
In most managed care systems, the PCP serves as the gateway for accessing the health care system. Without first seeing a PCP, referrals to other specialists or advanced medical care is difficult to access. Some of the adolescents in the focus groups were aware of this necessary step. As one adolescent explained:
If you have like a serious health problem … ? You go to your doctor … because you have your regular doctor. And when you tell them they can help you with the steps to get you help for that situation (South Central CA, 13–14 years).
The ability to make an appointment with a PCP is the next step in effectively navigating the health care system. In general, adolescents understood that making an appointment is the best way to see a doctor for non-emergency issues, limiting the amount of time spent in a waiting room.
When you call [your health care company] you press 4, you talk to a nurse practitioner first; and she asks you all your symptoms. And then she’s like – okay … can you come in at [specified time]? And when you come in, then, that’s when you get the real treatment (North CA, 15–17 years).
However, for some adolescents, parents served as the gatekeepers for their health care interactions, including scheduling appointments for the adolescents. One respondent remarked:
… it’s all my Mom’s, it’s her choice. She tells me I have an appointment; like, I think I’m going to go to my regular doctor, and then I go to another office (North Central CA, 15–17 years).
Participants also discussed difficulties in scheduling an appointment with their physician at a convenient time, or in a time frame they deem appropriate given the severity of their symptoms. In these instances, adolescents grappled with deciding whether the severity of the illness warranted an emergency room visit. One adolescent explained:
… with our doctor, you have to call, and then you have to make an appointment, and then sometimes they can’t take you till the next week. And you’re like, dude, I’m not going to be sick by next week (North CA, 15–17 years).
Physicians are also aware of difficulties in making appointments and how this may affect adolescent health care utilization. For the most part, difficulties arise from scheduling conflicts. One physician stated:
I think in getting appointments, sometimes because of their school schedule and other things in their lives, by the time they call to make an appointment for a physical our schedule is already full, and they end up waiting maybe a month.
Another important competency in navigating the health care system for adolescents is filling prescriptions. In general, adolescents understood the steps for filling a prescription at a pharmacy. Moreover, they were able to articulate their interaction with the pharmacist, particularly concerning medication guidelines and potential side effects. However, most interactions were described as one-way communication from pharmacist to adolescent with little to no dialogue. As one adolescent explained:
You go over there and get your prescription, get talked to about what the prescription is, they tell you when to take it, how to take it, what’s going to happen possibly (North CA, 15–17 years).
Rights and responsibilities
Another dimension to how adolescents understand and interact with the health care system deals with their understanding of rights and responsibilities as related to health and health care. Many of the respondents in our focus groups conveyed their understanding of responsibilities by describing their increasing role in maintaining their health. Two respondents commented:
Basically … my parents want me to take care of my own, due to the fact that I’m growing. So, when I know something’s wrong, I’ll just call and make an appointment. Then, I have to go there myself (North CA, 15–17 years).
You have to be responsible for your own health. The doctors help you out (North CA, 15–17 years).
During the health care encounter adolescents felt that it is their responsibility as well as their right to ask their doctor questions to help inform medical decisions, a key tenet of health literacy. One adolescent explained:
You have the right to ask as many questions as your brain can come up with (North CA, 13–14 years).
Moreover, when a teen is comfortable asking questions, it may also uncover misinformation or confusion on behalf of the adolescent as well as the desire to learn more. As one adolescent said, demonstrating confusion between blood sugar and blood pressure:
… . let’s say you have diabetes and you don’t know how to check up so your blood pressure won’t get too high, you need to ask [the doctor] how to make sure it doesn’t go up or how to keep it low (South Central CA, 15–17 years).
Helping adolescents understand their rights and responsibilities was also a focus for many of the physicians, particularly when related to sensitive health issues. One physician remarked:
We have to keep reminding them it’s okay for them to come alone for mental health illness issues or sexual health issues. Most of them are not aware of that.
Preventive care
Adolescents are a generally healthy population and may only access health care services during periods of wellness or for infrequent curative care visits. However, for many, preventive health care visits were not considered appropriate reasons to access health services. Many of the participants indicated the presence of illness or injury as a necessary reason to visit a doctor’s visit. As one participant explained:
I don’t see no point. It’s not that I don’t see no point, but why would you go if you’re not really sick, you know? (North CA, 15–17 years).
Physicians were also aware that preventive health services are low on the priority list for many adolescents, with the exception of annual sports physicals required for team memberships. One physician stated:
… they only pretty much come in when they need sports physicals or when they’re sick. Other than that, we really don’t see them. Yes, and urging them to come in routinely is a problem.
For some adolescents an annual well-care visit was seen in a positive light, albeit as an obligation for sports participation. One respondent commented:
I like going to the doctor − it’s worth it. It’s for your health. I like to stay healthy, because I like playing football … If I have to go, I’ll go (South Central CA, 13–14 years).
Preventive care was also mentioned in regard to screenings and tests associated with sexually transmitted infections (STIs). In general, participants understood that the absence of signs and symptoms does not necessarily mean that you are free of an STI, hence the need for a preventive health visit.
There’s new ones [diseases] out there … We’ve got to take care of ourselves, get checkups. Even if you’re not sexually active, you’ve got to get checked every six months (North CA, 15–17 years).
Information seeking
We define information seeking as the ability to seek out and critically evaluate relevant and appropriate information used to inform decisions. Adolescents in our focus groups described both passive and active ways in which they access information on health, health insurance and health care. Passive information was described as materials received from health providers, whereas active forms were described as information accessed over the Internet or by other means outside of the clinical setting.
Traditional, more passive methods used to disseminate health information, including pamphlets and booklets handed out at the doctor’s office, resonated less with adolescent populations—they are often thrown away. However, one adolescent explained how receiving information regarding health insurance benefits was important:
For me, they sent a paper; these are your benefits until you’re 18 or whatever. And I was like okay, that’s handy to know (North CA, 15–17 years).
Most of the adolescent respondents were comfortable using the Internet as a resource to find out information about their health. Adolescents, in general, were also aware that information on the Internet must be verified and that many sources are not reliable. As one said:
… go onto the Internet and you probably see … what’s wrong with you, they’ll [the Internet will] tell you some totally different thing (North CA, 13–14 years).
Physicians also commented that information presented to adolescents must be user friendly. That is, it is important for physicians to understand how teens access and use health information. One physician remarked:
Information [must be] in their own language, in their own media.
Patient–provider relationship
A final dimension that emerged from our focus group findings is the patient–provider relationship. Trust was a common theme discussed among adolescents in describing desirable qualities in a relationship with their doctor. As two respondents explained:
Build up trust with the doctor, like get the same person so you are not embarrassed to tell them anything, like a doctor friend (South Central CA, 15–17 years).
You don’t want your parents there when you’re talking about stuff you’ve done … That’s why I trust my doctors with information that I don’t want my parents to know (South Central CA, 13–14 years).
Comfort level was also an important issue for teens when describing the relationship with their physician. In many instances, the lack of comfort can serve as a barrier to accessing services or receiving a high level of care, particularly related to communicating one’s health needs. As one participant explained:
… sometimes I feel awkward, because I have a guy doctor right now, and … say for a girl you have to go get a pap smear, and it’s kind of … weird to ask him … I’m more comfortable with a girl [doctor] (North Central CA, 15–17 years).
There are various methods employed by physicians to build relationships with their patients to provide the highest quality of care. One physician described:
You know, I think it’s all about the rapport you make with them. So, we always excuse the parents, and first give them the five-minute spiel about how none of it’s going to leave the room. You kind of work your way into, start with the easy stuff, and then kind of work your way into the more serious issues.
Discussion
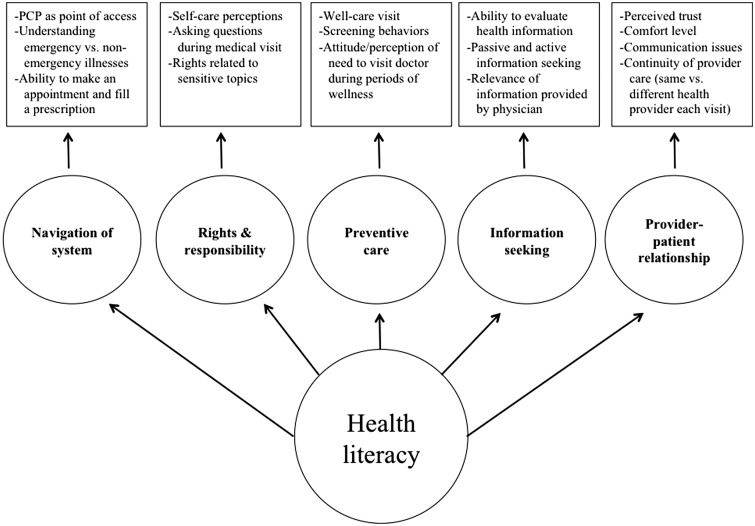
Our findings build upon prior literature by providing a framework for understanding and conceptualizing a robust definition of health literacy among adolescent populations, particularly concerning how they interact with the health care system. We have identified five domains for an expanded health-literacy concept that include: navigating the system, rights and responsibilities, preventive care, information seeking and patient–provider relationship. These domains help describe how our population organizes and applies cross-cutting competencies that include knowledge, attitudes and practices within the health care setting. Figure 1 displays our expanded model of the construct of health literacy with the five dimensions along with relevant practices that may help operationalize the concept.
Fig. 1.
Operationalizing an expanded definition of health literacy among adolescents.
As health literacy takes on a more robust definition, there is a need to develop multidimensional measures that capture the latent nature of the construct [21]. This in turn will allow researchers and practitioners to examine variations in health literacy among individuals and populations. Our conceptual model provides multiple domains as well as components of each dimension that may be used to develop measures of health literacy for adolescents and other generally healthy populations in the health care setting. The use of multiple items and multiple domains will better capture true variations in the underlying health-literacy construct. For example, in our population, navigating the health care system was described in terms of making the appointment with one’s regular doctor as well as overcoming scheduling difficulties. In some cases adolescents performed these duties themselves, whereas for others they relied on their parents to initiate contact with the system. This suggests that competencies related to this dimension will vary among adolescents. Ultimately, we can then examine whether different competency or skill levels are associated with varying health outcomes or health system experiences.
Adding to the prior literature, results from our focus groups and health provider interviews demonstrate the importance of further investigation of rights and responsibilities as a dimension of health literacy. The rights and responsibilities dimension was discussed in terms of knowledge related to health insurance benefits and also in terms of attitudes related to confidentiality and self-care practices. For many adolescents, understanding and articulating their rights and responsibilities as related to their health can be particularly challenging, especially if coupled with shifting roles and responsibilities within a family unit during adolescence. This dimension captures principles of self-efficacy and empowerment that are needed to manage one’s health environment, central components of an expanded definition of health literacy.
Furthermore, adolescents, like others, have learned to actively seek and obtain information about their health, especially using the Internet. Both focus group participants and physicians agreed that the Internet is a useful source from which to obtain health information, but also clearly stated that many facts, sources and sites offer conflicting views or advice. Central to an expanded definition of health literacy are the skills needed not only to find and access health information, but also to critically analyze and derive useful and correct information from a variety of information sources. The emerging field of e-health literacy has begun defining core competencies of searching for and evaluating health information in the digital age; however, the field is still developing the concept of e-health literacy and its measurement [52–55]; thus, findings from our study may contribute to the development of e-health literacy.
Our findings also highlight instances when competencies in health literacy could be used to overcome environmental and interpersonal barriers when interacting with the health care system. Adolescents whose appointment times conflict with school hours could reschedule or find other providers in their health plan who can better accommodate their schedule. Also, when discussing sensitive subjects with a provider, a health-literate adolescent may understand the role of confidentiality and thus will be more open to discussion. Additionally, a health-literate adolescent may be able to find and access appropriate and relevant health education materials when needed. The barriers reported by our participants are also supported by findings from previous studies [7, 56–59].
Educating insured teens about their health insurance benefits is also an important step in increasing their health literacy; however, as expressed by adolescents in the focus groups and supported in prior studies, other factors including attitudes and perceptions towards the need for well-care visits also influence behavior [7, 58]. Many of the adolescents did not understand the need to visit a health care provider unless they were sick or needed a sports physical. Moreover, very few view the health care system or health information as a resource to maintain their health during periods of wellness. Despite infrequent use or need of health-related services, a health-literate adolescent will have the skills needed to access health information or services when situations arise that warrant such action.
Limitations in our findings arise in the generalizability of results as we interviewed adolescents who mainly are recipients of public health insurance. In general, these youth come from low-income families that may have competing priorities different from higher income families when dealing with health and wellness. Measures developed based on these domains will need to be validated in other populations as health care needs may vary between populations. Furthermore, the State of California has traditionally been aggressive in the expansion of health insurance benefits to youth and children from low- and moderate-income families [60]; however, due to recent budget cuts, many public health insurance programs have revised eligibility criteria for coverage that may lead to inconsistent health insurance coverage among this population [61].
Another limitation to our findings is that they cannot be compared to findings of other research that used a narrow measure of health literacy. Measures such as the TOFHLA and REALM are not appropriate measures for this research as they rely too heavily on word recognition and assume that the ability to read or sound out words is necessary (and to some extent sufficient) to understand and negotiate the health care system. These measures do not capture the same skills as our expanded definition of health literacy, which focuses more on self-efficacy and issues related to managing one’s health environment. Thus, administering the REALM or TOFHLA during our focus groups would not have added to our findings as we investigated an asset-based perspective of health literacy, and further would have burdened our respondents with its test-like administration.
An additional limitation of our study is that all potential domains of an expanded health-literacy concept may not have emerged from our findings. Other relevant health-literacy competencies have been described elsewhere, including self-advocacy, assertiveness and application skills [18, 62, 63]. Furthermore, domains may manifest differently among different populations. The findings from this article are a stepping stone towards defining and developing relevant domains for an expanded operational definition of health literacy when applied to a health systems context.
Readers may also note that certain items or domains relevant to adolescent health care access are not included in our preliminary, operational definition of health literacy. Items such as awareness of health services available to adolescents or perceived ability to use a service for a specific health need are important concepts but are not included in our framework. This can be viewed as a limitation to our study and an inevitable challenge when conducting inductive research. However, we also argue that health-literate adolescents are able to use the appropriate channels (e.g., a primary care physician, the Internet, etc.) to access information and, ultimately, services based upon their needs.
Lastly, our findings and themes emerged through an iterative coding process based on prior health literacy literature as well as the expert knowledge and considerable field experience of the five authors. While analyzing the data, the dimensions of health literacy that emerged could have been assumed a priori. However, to minimize this bias, multiple authors coded each focus group and key informant interview independently and considerable effort was made to inductively create a framework based on empirical evidence.
Implications
Few published studies have defined and examined an expanded definition of health literacy among adolescents. As our findings suggest, expanding the definition to include navigation of the health care system, rights and responsibilities, preventive care, information seeking, and patient–provider relationships provides a more robust understanding of experiences between adolescents and the health care system.
Furthermore, our findings may be of particular interest to health care providers and health insurance companies as they provide insight into how adolescents view well-care visits and navigate the health care system more broadly. These stakeholders may wish to investigate strategies that increase health literacy and ultimately well-care visits among a generally healthy population, such as leveraging teachable moments including sports physicals and other school activities, or providing online scheduling and health information that may resonate more with this population. Using technology as a medium from which to build health-literacy skills may be a useful strategy in moving forward, particularly as access and use of the Internet and other mobile technologies becomes more ubiquitous in this population [64].
Despite lower rates of health care utilization among adolescents, adolescence can be a critical time for preventive interventions as shown in the alcohol and tobacco literature [65–68], leading to disease prevention and health promotion behaviors. Ultimately, understanding the framework and mechanisms from health literacy to health outcomes may improve patient-level interventions as well as inform system-wide changes for adolescent populations.
Further research that examines robust definitions of health literacy will help in the development of more appropriate measures of the concept that in turn can be used to gather better information. Moreover, this multidimensional construct becomes relevant in an era of health care reform where many will, for the first time, have health insurance, thus warranting the measurement of competencies in navigating and effectively utilizing a health care system that uses a managed care model.
Funding
Research Project Grant (R01) from the National Institute of Child Health and Human Development at the National Institutes of Health [5R01HD059756-02].
Conflict of interest statement
None declared.
References
- 1.Irwin CE, Adams SH, Park MJ, et al. Preventive care for adolescents: few get visits and fewer get services. Pediatrics. 2009;123:e565–72. doi: 10.1542/peds.2008-2601. [DOI] [PubMed] [Google Scholar]
- 2.American Medical Association. Guidelines for Adolescent Preventive Services (GAPS): Recommendations Monograph. Chicago: 1997. p. 7. Available at: http://www.ama-assn.org/ama1/pub/upload/mm/39/gapsmono.pdf. Accessed: 25 October 2011. [Google Scholar]
- 3.Duncan P, Pirretti AE. Bright futures for the busy clinical practice. Contemp Pediatr. 2009;22 no. 1. [Google Scholar]
- 4. Centers for Disease Control and Prevention. FastStats: Health Insurance Coverage. CDC National Center for Health Statistics, 2009. Available at: http://www.cdc.gov/nchs/fastats/hinsure.htm. Accessed: 24 March 2011.
- 5.UCLA Center for Health Policy Research. California Health Interview Survey 2009 Adolescent Public Use File. Center for Health Policy Research 2009. Available at: http://www.chis.ucla.edu/main/. Accessed: 25 October 2011. [Google Scholar]
- 6. HEDIS, Healthcare Effectiveness Data and Information Set: National Committee for Quality Assurance 2010. Available at: http://www.ncqa.org. Accessed: 24 March 2011.
- 7.Coker TR, Sareen HG, Chung PJ, et al. Improving access to and utilization of adolescent preventive health care: the perspectives of adolescents and parents. J Adolesc Health. 2010;47:132–43. doi: 10.1016/j.jadohealth.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Parker RM, Baker DW, Williams MV, et al. The test of functional health literacy in adults. J Gen Inter Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 9.Williams MV, Parker RM, Baker DW, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;275:1677–82. [PubMed] [Google Scholar]
- 10.Baker DW, Parker RM, Williams MV, et al. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87:1027–30. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeWalt DA, Berkman ND, Sheridan S, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Inter Med. 2004;19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gazmararian JA, Kripalani S, Miller MJ, et al. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Inter Med. 2006;21:1215–21. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. Philadelphia, PA: JB Lippincott Company; 1985. [Google Scholar]
- 14.Nielsen-Bohlman L, Panzer AM, Hamlin B, et al. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 15.U.S. Department of Health and Human Services. National Action Plan to Improve Health Literacy. vol. 15. Washington, DC: 2010. Available at: http://www.health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf. Accessed: 1 November 2011. [Google Scholar]
- 16.Nutbeam D. Advancing health literacy: a global challenge for the 21st century. Health Promot Int. 2000;15:183–4. [Google Scholar]
- 17.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–8. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 18.Jordan JE, Buchbinder R, Osborne RH. Conceptualising health literacy from the patient perspective. Patient Educ Couns. 2010;79:36–42. doi: 10.1016/j.pec.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Lee S-YD, Arozullah M, Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. 2004;58:1309–21. doi: 10.1016/S0277-9536(03)00329-0. [DOI] [PubMed] [Google Scholar]
- 20.Zarcadoolas C, Pleasant A, Greer DS. Understanding health literacy: an expanded model. Health Promot Int. 2005;20:195–203. doi: 10.1093/heapro/dah609. [DOI] [PubMed] [Google Scholar]
- 21.Pleasant A, McKinney J, Rikard RV. Health literacy measurement: a proposed research agenda. J Health Commun. 2011;16:11–21. doi: 10.1080/10810730.2011.604392. [DOI] [PubMed] [Google Scholar]
- 22.Parker R, Ratzan SC. Health literacy: a second decade of distinction for Americans. J Health Commun. 2010;15(Suppl 2):20–33. doi: 10.1080/10810730.2010.501094. [DOI] [PubMed] [Google Scholar]
- 23.Osborn CY, Paasche-Orlow MK, Bailey SC, et al. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011;35:118–28. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishikawa H, Yano E. Patient health literacy and participation in the health-care process. Health Expect. 2008;11:113–22. doi: 10.1111/j.1369-7625.2008.00497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glanz K, Rimer BK, Lewis FM. Health Behavior and Health Education: Theory, Research, and Practice, 3rd Edition. San Francisco: Jossey-Bass; 2002. [Google Scholar]
- 26.Tones K. Health literacy: new wine in old bottles? Health Educ Res. 2002;17:287–290. doi: 10.1093/her/17.3.287. [DOI] [PubMed] [Google Scholar]
- 27.Brown SL, Teufel JA, Birch DA. Early adolescents perceptions of health and health literacy. J Sch Health. 2007;77:7–15. doi: 10.1111/j.1746-1561.2007.00156.x. [DOI] [PubMed] [Google Scholar]
- 28.Manganello JA. Health literacy and adolescents: a framework and agenda for future research. Health Educ Res. 2008;23:840–7. doi: 10.1093/her/cym069. [DOI] [PubMed] [Google Scholar]
- 29.Wharf Higgins J, Begoray D, MacDonald M. A social ecological conceptual framework for understanding adolescent health literacy in the health education classroom. Am J Community Psychol. 2009;44:350–62. doi: 10.1007/s10464-009-9270-8. [DOI] [PubMed] [Google Scholar]
- 30.Shone LP, Conn KM, Sanders L, et al. The role of parent health literacy among urban children with persistent asthma. Patient Educ Couns. 2009;75:368–75. doi: 10.1016/j.pec.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coffman MJ, Shobe MA, Dmochowski J, et al. Health care access and utilization among Latino immigrants. Hisp Health Care Int. 2007;5:73–80. [Google Scholar]
- 32.Sanchez-Birkhead AC, Kennedy HP, Callister LC, et al. Navigating a new health culture: experiences of immigrant Hispanic women. J Immigr Minor Health. 2011;13:1168–74. doi: 10.1007/s10903-010-9369-x. [DOI] [PubMed] [Google Scholar]
- 33.Yu SM, Huang ZJ, Singh GK. Health status and health services utilization among US Chinese, Asian Indian, Filipino, and other Asian/Pacific Islander children. Pediatrics. 2004;113:101–7. doi: 10.1542/peds.113.1.101. [DOI] [PubMed] [Google Scholar]
- 34.Zanchetta MS, Poureslami IM. Health literacy within the reality of immigrants’ culture and language. Can J Public Health. 2006;97:S26–30. [PubMed] [Google Scholar]
- 35.Halpern-Felsher BL, Ozer EM, Millstein SG, et al. Preventive services in a health maintenance organization: how well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med. 2000;154:173–9. doi: 10.1001/archpedi.154.2.173. [DOI] [PubMed] [Google Scholar]
- 36.Klein JD, Wilson KM. Delivering quality care: adolescents’ discussion of health risks with their providers. J Adolesc Health. 2002;30:190–5. doi: 10.1016/s1054-139x(01)00342-1. [DOI] [PubMed] [Google Scholar]
- 37.Ma J, Wang Y, Stafford RS. U.S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36:441. doi: 10.1016/j.jadohealth.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 38.Davis TC, Wolf MS, Arnold CL, et al. Development and validation of the Rapid Estimate of Adolescent Literacy in Medicine (REALM-Teen): a tool to screen adolescents for below-grade reading in health care settings. Pediatrics. 2006;118:e1707–14. doi: 10.1542/peds.2006-1139. [DOI] [PubMed] [Google Scholar]
- 39.Yin HS, Forbis SG, Dreyer BP. Health literacy and pediatric health. Curr Probl Pediatr Adolesc Health Care. 2007;37:258–86. doi: 10.1016/j.cppeds.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 40.Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 41.Mancuso JM. Assessment and measurement of health literacy: an integrative review of the literature. Nurs Health Sci. 2005;11:77–89. doi: 10.1111/j.1442-2018.2008.00408.x. [DOI] [PubMed] [Google Scholar]
- 42.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu AD, Begoray DL, Macdonald M, et al. Developing and evaluating a relevant and feasible instrument for measuring health literacy of Canadian high school students. Health Promot Int. 2010;25:444–52. doi: 10.1093/heapro/daq032. [DOI] [PubMed] [Google Scholar]
- 44.Patton M. Qualitative Research & Evaluation Methods, 3rd Edition. Thousand Oaks, CA: Sage Publications; 2002. Designing Qualitative Studies; pp. 209–58. [Google Scholar]
- 45.Kreuger R, Casey M. Focus Groups: A Practical Guide for Applied Research 4th Edition. vol. 158. Los Angeles: Sage Publications; 2009. Focus Group Interviewing with Young People; pp. 155–162. [Google Scholar]
- 46.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. Available at: http://www.ncbi.nlm.nih.gov/pubmed/7738325. Accessed: 31 January, 2012. [PubMed] [Google Scholar]
- 47.Strauss AL. Qualitative Analysis for Social Scientists. Cambridge, UK: Cambridge University Press; 1987. Codes and Coding; pp. 55–81. [Google Scholar]
- 48.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 49.Basch CE. Focus group interview: an underutilized research technique for improving theory and practice in health education. Health Educ Behav. 1987;14:411–48. doi: 10.1177/109019818701400404. [DOI] [PubMed] [Google Scholar]
- 50.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 51.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Services Research. 1999;34 5 Part II. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1089059/pdf/hsresearch00022-0112.pdf. Accessed: 31 January 2012. [PMC free article] [PubMed] [Google Scholar]
- 52.Norman CD, Skinner HA. eHEALS: the eHealth Literacy Scale. J Med Internet Res. 2006;8:e27. doi: 10.2196/jmir.8.4.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Neuhauser L, Kreps GL. Rethinking communication in the e-health era. J Health Psychol. 2003;8:7–23. doi: 10.1177/1359105303008001426. [DOI] [PubMed] [Google Scholar]
- 54.Glasgow RE. eHealth evaluation and dissemination research. Am J Prev Med. 2007;32:S119–26. doi: 10.1016/j.amepre.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 55.Skopelja E, Whipple E, Richwine P. Reaching and teaching teens: adolescent health literacy and the internet. J Consum Health Internet. 2008;12:105–18. [Google Scholar]
- 56.Ginsburg KR, Menapace AS, Slap GB. Factors affecting the decision to seek health care: the voice of adolescents. Pediatrics. 1997;100:922–30. doi: 10.1542/peds.100.6.922. [DOI] [PubMed] [Google Scholar]
- 57.Klein JD, McNulty M, Flatau CN. Adolescents’ access to care: teenagers' self-reported use of services and perceived access to confidential care. Arch Pediatr Adolesc Med. 1998;152:676–82. doi: 10.1001/archpedi.152.7.676. [DOI] [PubMed] [Google Scholar]
- 58.Elliott BA, Larson JT. Adolescents in mid-sized and rural communities: foregone care, perceived barriers, and risk factors. J Adolesc Health. 2004;35:303–9. doi: 10.1016/j.jadohealth.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 59.Brown JD, Wissow LS. Discussion of sensitive health topics with youth during primary care visits: relationship to youth perceptions of care. J Adolesc Health. 2009;44:48–54. doi: 10.1016/j.jadohealth.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harbage P, Ryan J, Chan L. The Future of California’s SCHIP Program: Analyzing the Proposed Federal Legislation. Oakland, CA: 2007. Available at: http://www.chcf.org/~/media/MEDIA LIBRARY Files/PDF/C/PDF CHIPReauthorizationAnalysis.pdf http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/T/PDF%20TheFutureOfCAsSCHIPProgram.pdf. Accessed: 1 November 2011. [Google Scholar]
- 61.Harbage P. CHIP Reauthorization: Analysis of Potential Policy Changes for Healthy Families. Oakland, CA: 2010. Available at: http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/C/PDF%20CHIPReauthorizationAnalysis.pdf. Accessed: 1 November 2011. [Google Scholar]
- 62.Martin LT, Schonlau M, Haas A, et al. Patient activation and advocacy: which literacy skills matter most? J Health Commun. 2011;16(Suppl 3):177–90. doi: 10.1080/10810730.2011.604705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Levin-Zamir D, Peterburg Y. Health literacy in health systems: perspectives on patient self-management in Israel. Health Promot Int. 2001;16:87–94. doi: 10.1093/heapro/16.1.87. [DOI] [PubMed] [Google Scholar]
- 64.Lenhart A, Purcell K, Smith A, et al. Social Media & Mobile Internet Use Among Teens and Young Adults. Washington, DC: 3 February 2010: 1–37. Available at: http://www.pewinternet.org/~/media//Files/Reports/2010/PIP_Social_Media_and_Young_Adults_Report_Final_with_toplines.pdf. Accessed: 1 November 2011. [Google Scholar]
- 65.Christiansen BA, Smith GT, Roehling PV, et al. Using alcohol expectancies to predict adolescent drinking behavior after one year. J Consult Clin Psychol. 1989;57:93–9. doi: 10.1037//0022-006x.57.1.93. [DOI] [PubMed] [Google Scholar]
- 66.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 67.Pechacek TF, Murray DM, Luepker RV, et al. Measurement of adolescent smoking behavior: rationale and methods. J Behav Med. 1984;7:123–40. doi: 10.1007/BF00845351. [DOI] [PubMed] [Google Scholar]
- 68.Wang MQ, Fitzhugh EC, Eddy JM, et al. Family and peer influences on smoking behavior among American adolescents: an age trend. J Adolesc Health. 1995;16:200–3. doi: 10.1016/1054-139X(94)00097-X. [DOI] [PubMed] [Google Scholar]