Abstract
Purpose:
The main objective of this survey is to describe the current practice of thoracic anesthesia in the Middle Eastern (ME) region.
Methods:
A prospective online survey. An invitation to participate was e-mailed to all members of the ME thoracic-anaesthesia group. A total of 58 members participated in the survey from 19 institutions in the Middle East. Questions concerned ventilation strategies during one-lung ventilation (OLV), anesthesia regimen, mode of postoperative analgesia, use of lung isolation techniques, and use of i.v. fluids.
Results:
Volume-controlled ventilation was favored over pressure-controlled ventilation (62% vs 38% of respondents, P<0.05); 43% report the routine use of positive end-expiratory pressure. One hundred percent of respondents report using double-lumen tube (DLT) as a first choice airway to establish OLV. Nearly a third of respondents, 31.1%, report never using bronchial blocker (BB) in their thoracic anesthesia practice. Failure to pass a DLT and difficult airway are the most commonly cited indications for BB use. Regarding postoperative analgesia, the majority 61.8% favor thoracic epidural analgesia over other techniques (P<0.05).
Conclusions:
Our survey provides a contemporary snapshot of the ME thoracic anesthetic practice.
Keywords: Middle east, survey, thoracic anesthesia
INTRODUCTION
Thoracic anesthesia is a challenging subspecialty. In addition to the generic challenges of major surgery, the anesthetist is faced with the additional demands of establishing lung isolation. Hypoxemia associated with one-lung ventilation (OLV) has a reported incidence of 5-10%, while both the duration of OLV and high intraoperative ventilatory pressures are established risk factors for postoperative acute lung injury.[1,2]
Consequently, ventilator strategies have been developed seeking to maintain oxygenation during OLV while ameliorating postoperative lung injury. Such strategies include the use of positive end-expiratory pressure (PEEP) to the ventilated lung or continuous positive airway pressure to the collapsed lung, selection of pressure-controlled over volume-controlled ventilation (VCV), reducing the fraction of inspired oxygen (FiO2) and reducing tidal volume. The evidence base for such interventions is not conclusive with opinion and practice varying widely.[3–7] Choice of lung separation device is another important issue in anesthesia for general thoracic surgery. The commonest technique is the use of double-lumen endobronchial tube (DLT). Left-sided DLTs are widely used to achieve OLV in thoracic anesthesia, while the proximal take off of the right upper lobe bronchus makes positioning of a right-sided DLT more technically challenging. As a result, the use of right-sided DLT is the subject of some controversy; some have gone as far as to suggest that right-sided DLT should not be routinely used in thoracic anesthetic practice.[8,9] OLV can also be achieved with the use of bronchial blockers (BB), a technique which has been described as having a role in patients with a difficult airway.[10–12]
Provision of analgesia for thoracotomy is a further challenge to the thoracic anesthetist. Thoracic epidural analgesia (TEA) has long been considered the gold standard technique for post-thoracotomy pain relief. Recent studies however have reported that paravertebral block (PVB) is effective as TEA in treating post-thoracotomy pain and may be associated with a reduction in postoperative complications.[13–16] Shelley et al. recently conducted a survey of UK thoracic anesthesiologists exploring many of the above issues with interesting results.[17] We sought to carry out a similar survey among Middle Eastern (ME) thoracic anesthetists with the aim of describing the current practice of thoracic anesthesia in the region.
METHODS
Permission was obtained from Shelley et al. to use their survey protocol via the commercially available “Survey Monkey” software (www.surveymonkey.com).[17] An electronic invitation message was sent to all 129 members of the ME thoracic anesthesia group (http://health.groups.yahoo.com/group/thoracic-anaesthesia/). The thoracic anesthesia group was founded in November 1999 with the aim of providing a forum for the exchange of ideas and experiences pertinent to the practice of thoracic anesthesia in the ME region. Participants were requested to complete questions in the context of their “current routine ‘first choice’ practice when anesthetizing for lobectomy/pneumonectomy with one-lung ventilation… in the absence of any contraindications or special (patient) considerations.”
Questions concerned anesthetic technique, mode of ventilation during the period of OLV, regional analgesic technique (if any), adjunctive analgesia, perioperative fluid management, and choice of lung separation technique. Mann-Whitney test was used to compare continuous data and Chi Square test was used to compare categorical data. P<0.05 was considered statistically significant. Data analysis was carried out using SPSS software version 13.
RESULTS
A total of 58 members of the thoracic anesthesia group participated in the survey from 19 institutions in the Middle East. This corresponds to a response rate of 45%.
Anesthetic technique
For 84% of respondents, sevoflurane was the inhalational anesthetic of choice during OLV (P<0.05 compared with other agents). Only 16.9% of the respondents used total intravenous anesthesia with propofol during OLV.
Method of one-lung ventilation
VCV was favored over pressure-controlled ventilation (PCV) mode (62 vs 37.9%), though this difference was not statistically significant (P=0.8). Fifty-two percent of respondents reported that they ventilate with a target tidal volume (Vt) of 4-6 ml/kg body weight. Fifty-three percent of respondents reported the adoption of permissive approach to hypercapnia during OLV vs 47.2% who do not (not significant). The distribution of FiO2 chosen during the period of OLV (assuming hypoxia is not an issue) is bimodal. Fifty percent of the respondents report routinely ventilating with a FiO2 of 1, while 19% favor an FiO2 of between 0.4 and 0.5 [Figure 1]. Forty-three percent of respondents reported that they routinely use PEEP during OLV with the majority of those using 5 cm H2O PEEP.
Figure 1.
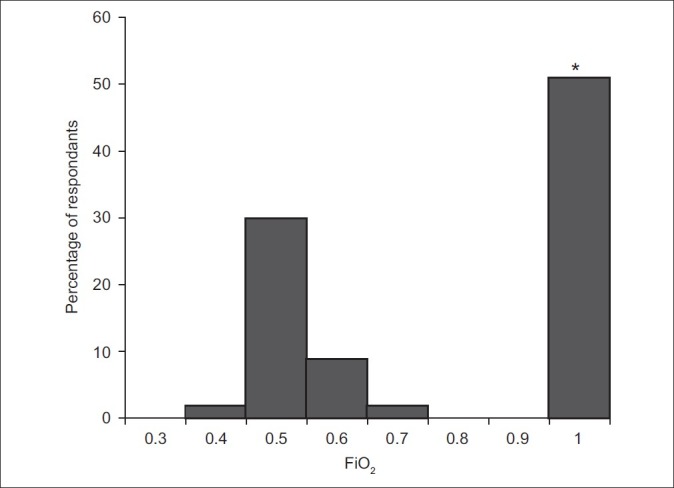
The range of FIO2 routinely used by respondents during the period of one-lung ventilation
Choice of lung separation technique
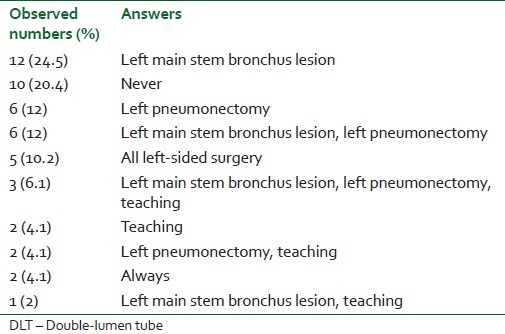
Forty-seven participants responded to the section on choice of lung separation technique. All reported that they use a DLT as first choice technique to establish OLV for open thoracotomy for lung resection. Fifty-four percent of respondents favor using left-sided DLTs for all pathologies. The most commonly cited indication for right-sided DLT use is for lesions of the left proximal main-stem bronchus [Tables 1 and 2].
Table 1.
Most common indications for using a left-sided DLT
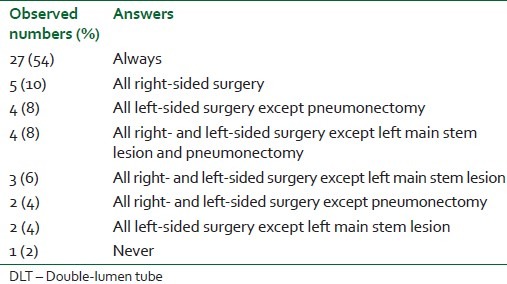
Table 2.
Most common indications for using a right-sided DLT
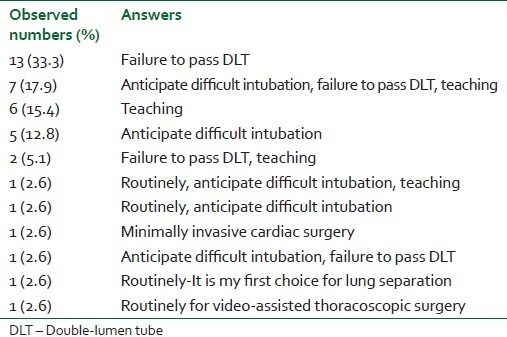
Nearly a third of respondents, 31%, report never using BB in their thoracic anesthetic practice. Of the 69% of respondents reporting use of BB, these are principally utilized in case of failure to pass a DLT and in patients with a difficult airway [Table 3].
Table 3.
Most common indications for using a bronchial blocker
Postoperative analgesia
TEA is favored by the majority of respondents [Table 4]. Fifty-eight percent of respondents report that they establish the epidural block before induction of general anesthesia. Bupivacaine was reported as the drug of choice for TEA in the majority of cases (89.7%), most commonly with fentanyl as an additive (96.2%). Only 9.1% reported the use of PVB as the preferred analgesic modality.
Table 4.
First choice regional analgesic technique for open thoracotomy and lung resection

Perioperative fluid management
Regarding intraoperative fluid management, 23% report using normal saline while 56% report using Lactated Ringer solution (the remainder reported using other types of fluids). Forty percent answered that they are using the fluids according to ml/kg body weight formula where 60% report liberal intraoperative fluid replacement. Assuming blood loss is not exceptional, the majority of respondents, 61%, report giving 1-2 l of fluids intraoperatively. However, 29% report giving 0.5-1 l of fluids intraoperatively. Seven and 2% of the respondents report giving 2-3 and >3 l of fluids intraoperatively, respectively.
DISCUSSION
Our results in this survey differ in many aspects from the survey conducted by Shelley et al. from United Kingdom (UK).[17] In our survey, most of the respondents were in favor of VCV in contradiction to the UK survey where the majority prefers using PCV mode during OLV. In both surveys, most of the participants were in favor of using PEEP during OLV. Definitive studies on the most effective ventilatory mode during OLV remain elusive. In a study comparing VCV vs PCV modes during OLV, Tugrul et al. demonstrated that PCV was associated with a statistically significant decrease in airway pressures and an improvement in oxygenation.[18] Though others have failed to demonstrate a similar improvement in oxygenation indices, the findings in terms of reduced airway pressure are consistent.[19,20] In light of concerns about acute lung injury, this alone has been sufficient for some to conclude that PCV is the preferred mode of ventilation during OLV.[21] Respondents from the ME also tended to favor administering a higher FiO2 during the period of OLV compared to UK respondents. This practice has recently been called into question in light of concerns over the potentially harmful effects of hyperoxia.[22]
Regarding the use of lung isolation techniques to achieve OLV, the majority of respondents to both surveys (ME and UK) favor the use of DLT. Left main bronchus lesions and left pneumonectomy were the most frequently cited indications for right-sided DLT in both surveys. In both surveys, most of the respondents reported rarely using BB to achieve OLV, though the majority will use them in cases of difficult airway. The use of BB for airway control and difficult airway management in thoracic anesthesia has recently been recommended by a panel of international experts.[23,24] None of the surveys was designed to explore what types of BB are in clinical use. TEA was the method of choice for perioperative pain relief in both surveys. Most of the respondents to the ME survey reported establishing and confirming the onset of epidural blockade prior to induction of anesthesia compared to few respondents to the UK survey. PVB is the second method of choice for post-thoracotomy pain relief in both surveys. There is growing evidence that PVB is a safe alternative to TEA for post-thoracotomy pain after lung resection.[25] Our results demonstrate the variety of thoracic anesthesia practices throughout the ME region. Although there was general agreement between the respondents to both surveys regarding the use of DLTs and BBs, there was clear differences in opinion between the two regions on other issues. The main differences appear to be in the conduct of OLV. We suggest that the differences in the practice of thoracic anesthesia between the two regions reflect a more “traditional” approach to thoracic anesthesia in the ME. This may reflect the absence of a subspecialty society, limited access to subspecialty continuing professional development, and limited training opportunities in the ME region. In contrast, the UK has a very active association of cardiothoracic anesthetists hosting biannual subspecialty educational meetings (www.acta.org.uk); in addition, fellowships/training programs for cardiothoracic anesthetic trainees are commonplace.
In conclusion, we have attempted to provide a broad overview of the current practice of thoracic anesthesia in the ME region. We believe significant inroads are being made by the ME thoracic anesthesia group, both in terms of education and training, but suggest more could be done to ensure that thoracic anesthesia practice in the ME remains up-to-date and develops in parallel with western contemporaries.
ACKNOWLEDGMENT
The author would like to thank all members the thoracic anesthesia group for their participation in this survey.
Thoracic-anaesthesia group collaborators
A. Members who mentioned their names and their institutes names: Mohamed Delvi, Waseem Hajjar, Sami Al-Nassar, Jumana Baaj, Badiah Abdulghani (College of Medicine, King Saud University, Riyadh, KSA), Abdulhadi Alsaflan (University of Dammam, KSA), Mussarat Afzal (King Fahad specialist Hospital, Dammam, KSA), Nasser Alkemyani (Sultan Qaboos University Hospital, Oman), Mohamed Abdulatif, Fawzia Aboelfetouh, Ezz El-Din Fikri Ismail, Mohamed Osman, Hisham Hosny (College of Medicine, Cairo University, Egypt), Khaled Abdullah (College of Medicine, Ain Shams University, Egypt), Mutlaq Althubaiti (Riyadh Military Hospital, KSA), Saad Al-Shamma (Al-yarmook Teaching Hospital, Baghdad-Iraq), Mohamed Moniem (Sharjah University Hospital, Sharjah, United Arab Emirates).
B. Members who mentioned only their institutes names: King Fahad Hospital (Almadinah Almunawarah, KSA), King Abdullah Medical City (Makah, KSA), Jordan University Hospital (Jordan), Kuwait University Hospital (Kuwait), International Medical Centre (Egypt), King Faisal Specialists Hospital (Riyadh, KSA), Suez Canal University Hospital (Ismailia, Egypt), Dr. Soliman Fakeeh Hospital (Jeddah, KSA), National guard Hospital (Riyadh, KSA), Arab Contractor Medical Centre (Cairo, Egypt).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Karazai W, Schwarzkopf K. Hypoxemia during one-lung ventilation. Anesthesiology. 2009;110:1402–1. doi: 10.1097/ALN.0b013e31819fb15d. [DOI] [PubMed] [Google Scholar]
- 2.Licker M, de Perrot M, Spiliopoulos A, Robert J, Diaper J, Chevalley C, et al. Risk factors for acute lung injury after thoracic surgery for lung cancer. Anesth Analg. 2003;97:1558–65. doi: 10.1213/01.ANE.0000087799.85495.8A. [DOI] [PubMed] [Google Scholar]
- 3.Ng A, Swanevelder J. Hypoxemia associated with one-lung anaesthesia: New discoveries in ventilation and perfusion. Br J Anaesth. 2011;106:761–3. doi: 10.1093/bja/aer113. [DOI] [PubMed] [Google Scholar]
- 4.Michelet P, Roch A, Brousse D, D’Journo XB, Bregeon F, Lambert D, et al. Effects of PEEP on oxygenation and respiratory mechanics during one-lung ventilation. Br J Anaesth. 2005;95:267–73. doi: 10.1093/bja/aei178. [DOI] [PubMed] [Google Scholar]
- 5.El-Tahan MR, El Ghoneimy YF, Regal MA, El Emam H. Comparative study of the non-dependent continuous positive pressure ventilation and high-frequency positive-pressure ventilation during one-lung ventilation for video-assisted thoracoscopic surgery. Interact Cardiovasc Thorac Surg. 2011;12:899–902. doi: 10.1510/icvts.2010.264911. [DOI] [PubMed] [Google Scholar]
- 6.Della Rocca G, Coccia C. Ventilatory management of one-lung ventilation. Minerva Anestesiol. 2011;77:534–6. [PubMed] [Google Scholar]
- 7.Montes FR, Pardo DF, Charrís H, Tellez LJ, Garzón JC, Osorio C. Comparison of two protective lung ventilatory regimes on oxygenation during one-lung ventilation: A randomized controlled trial. J Cardiothorac Surg. 2010;5:99–103. doi: 10.1186/1749-8090-5-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ehrenfeld JM, Walsh JL, Sandberg WS. Right- and left-sided Mallinckrodt double-lumen tubes have identical clinical performance. Anesth Analg. 2008;106:1847–52. doi: 10.1213/ane.0b013e31816f24d5. [DOI] [PubMed] [Google Scholar]
- 9.Cohen E. Con: Right-sided double-lumen endotracheal tubes should not be routinely used in thoracic surgery. J Cardiothorac Vasc Anesth. 2002;16:249–52. doi: 10.1053/jcan.2002.31092. [DOI] [PubMed] [Google Scholar]
- 10.Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol. 2010;23:12–7. doi: 10.1097/ACO.0b013e328331e8a7. [DOI] [PubMed] [Google Scholar]
- 11.Narayanaswamy M, McRae K, Slinger P, Dugas G, Kanellakos GW, Roscoe A, et al. Choosing a lung isolation device for thoracic surgery: A randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg. 2009;108:1097–101. doi: 10.1213/ane.0b013e3181999339. [DOI] [PubMed] [Google Scholar]
- 12.Ruetzler K, Grubhofer G, Schmid W, Papp D, Nabecker S, Hutschala D, et al. Randomized clinical trial comparing double-lumen tube and EZ-blocker for single-lung ventilation. Br J Anaesth. 2011;106:896–902. doi: 10.1093/bja/aer086. [DOI] [PubMed] [Google Scholar]
- 13.Elsayed H, McKevith J, McShane J, Scawn N. Thoracic epidural or paravertebral catheter for analgesia after lung resection: Is the outcome different? J Cardiothorac Vasc Anesth. 2012;26:78–82. doi: 10.1053/j.jvca.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 14.Davies R, Myles P, Graham J. A comparison of the analgesic efficacy and side effects of paravertebral vs epidural blockade for thoracotomy: A systematic review and meta-analysis of randomization trials. Br J Anaesth. 2006;96:418–26. doi: 10.1093/bja/ael020. [DOI] [PubMed] [Google Scholar]
- 15.Powell ES, Pearce AC, Cook D, Davies P, Bishay E, Bowler GM, et al. UKPOS co-ordinators. UK pneumonectomy outcome study (UKPOS): A prospective observational study of pneumonectomy outcome. J Cardiothorac Surg. 2009;4:41. doi: 10.1186/1749-8090-4-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grider JS, Mullet TW, Saha SP, Harned ME, Sloan PA. A randomized, double-blind trial comparing continuous thoracic epidural bupivacaine with and without opioid in contrast to a continuous paravertebral infusion of bupivacaine for post-thoracotomy pain. J Cardiothorac Vasc Anesth. 2012;26:83–9. doi: 10.1053/j.jvca.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Shelley B, Macfie A, Kinsella J. Anesthesia for thoracic surgery: A survey of UK practice. J Cardiothorac Vasc Anesth. 2011;25:1014–7. doi: 10.1053/j.jvca.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Tugrul M, Camci E, Karadeniz H, Sentürk M, Pembeci K, Akpir K. Comparison of volume-controlled with pressure-controlled ventilation during one-lung anaesthesia. Br J Anaesth. 1997;79:306–10. doi: 10.1093/bja/79.3.306. [DOI] [PubMed] [Google Scholar]
- 19.Unzueta MC, Casas JI, Moral MV. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for thoracic surgery. Anesth Analg. 2007;104:1029–33. doi: 10.1213/01.ane.0000260313.63893.2f. [DOI] [PubMed] [Google Scholar]
- 20.Pardos PC, Garutti I, Pineiro P, Olmedilla L, de la Gala F. Effects of ventilatory mode during one-lung ventilation on intraoperative and postoperative oxygenation in thoracic surgery. J Cardiothorac Vasc Anesth. 2009;23:770–4. doi: 10.1053/j.jvca.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Lohser J. Evidence-based management of one-lung ventilation. Anesthesiol Clin. 2008;26:241–72. doi: 10.1016/j.anclin.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Grocott H. Oxygen toxicity during one-lung ventilation: Is it time to re-evaluate our practice? Anesthesiol Clin. 2008;26:273–80. doi: 10.1016/j.anclin.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Merli G, Guarino A, Della Rocca G, Frova G, Petrini F, Sorbello M, et al. Recommendations for airway control and difficult airway management in thoracic anesthesia and lung separation procedures. Minerva Anestesiol. 2009;75:59–96. [PubMed] [Google Scholar]
- 24.Cohen E. Recommendations for airway control and difficult airway management in thoracic anesthesia and lung separation procedures. Are we ready for the challenge? Minerva Anestesiol. 2009;75:3–5. [PubMed] [Google Scholar]
- 25.Kaya FN, Turker G, Mogol EB, Bayrakter S. Thoracic paravertebral block for video-assisted thoracoscopic surgery: Single injection versus multiple injections. J Cardiothorac Vasc Anesth. 2012;26:90–4. doi: 10.1053/j.jvca.2011.09.008. [DOI] [PubMed] [Google Scholar]


