Abstract
Background:
Addition of clonidine to ropivacaine (0.2%) can potentially enhance analgesia without producing prolonged motor blockade. The aim of the present study was to compare the post-operative pain relieving quality of ropivacaine 0.2% and clonidine mixture to that of plain ropivacaine 0.2% following caudal administration in children.
Methods:
In a prospective, double-blinded, randomized controlled trial, 30 ASA 1 pediatric patients undergoing infraumbilical surgery were randomly allocated to receive a caudal injection of either plain ropivacaine 0.2% (1 ml/kg) (group A) or a mixture of ropivacaine 0.2% (1 ml/kg) with clonidine 2 μg/kg (group B). Objective pain score and need for supplemental analgesics were compared during the 1st 24 hours postoperatively. Residual post-operative sedation and motor blockade were also assessed.
Results:
Significantly prolonged duration of post-operative analgesia was observed in group B (P<0.0001). Heart rate and blood pressure were not different in 2 groups. Neither motor blockade nor post-operative sedation varied significantly between the groups.
Conclusion:
The combination of clonidine (2 μg/kg) and ropivacaine 0.2% was associated with an improved quality of post-operative analgesia compared to plain 0.2% ropivacaine. The improved analgesic quality of the clonidine-ropivacaine mixture was achieved without causing any significant degree of post-operative sedation or prolongation of motor blockade.
Keywords: Caudal, clonidine, infra-umbilical surgery, paediatrics, ropivacaine
INTRODUCTION
Post-operative pain relief in children is very important since emotional component of pain is very strong in children. As pain is very difficult to assess in pediatric population very commonly, post-operative pain is undertreated in this age group. Caudal block is a well-accepted technique and proved to be a good alternative to general anesthesia in pediatric infra-umbilical surgeries. Usage of single local anesthetic agent via caudal route provides shorter duration of block[1] and requires often supplemental anesthetics. Ropivacaine, an amide local anesthetic, offers some advantages over bupivacaine e.g., less cardiac and neurological toxicity, less motor blockade and prolonged sensory analgesia.[2] Addition of adjuvants (opioids, ketamine etc.) prolongs the duration of block and are being increasingly used these days. Opioids carry risk of post-operative respiratory depression, and ketamine has the potential of neurotoxicity if inadvertently injected intrathecally.[3]
Clonidine, an a2 adrenergic agonist, prolongs analgesia without significant respiratory depression. The analgesic action of epidurally-administered clonidine is due to stimulation of descending noradrenergic medullospinal pathways inhibiting the release of nociceptive neurotransmitters in the dorsal horn of spinal cord.[4] The analgesic effect of clonidine is more pronounced after neuraxial injection, which suggests a spinal site of action and makes this route of administration preferable.[5,6]
Therefore, we did a prospective, randomized, double-blind trial to investigate the role of clonidine as an adjuvant to ropivacaine through caudal route in children on duration of post-operative analgesia and to find out if an addition of clonidine produces any unwanted effect.
METHODS
After obtaining proper informed consent from parents and approval of institutional ethical committee, 30 ASA grade I children, aged 2 to 11 years, weighing 5 to 30 kilograms, scheduled for lower abdominal, perineal, and lower limb surgeries, were included in the study. Patients having cardiovascular, neurological diseases, coagulopathy, infection or deformity of local site and where parents refused to give consent were excluded from the study.
30 children were randomly allocated into 2 equal groups. Group A received ropivacaine 0.2% 1 ml/kg via caudal route. Group B received ropivacaine 0.2% 1 ml/kg plus clonidine 2 μg/kg in the same route. Drug was prepared by a person unrelated to study, and volume of drug contributed by clonidine being insignificant blinding could be done easily.
All patients were premedicated with nasal midazolam spray 0.2 mg/kg, and parental separation was done after 20 minutes.
After transferring the patient into operating room, multichannel monitor was attached and baseline readings of heart rate (HR), oxygen saturation (SpO2), systolic blood pressure (SBP), diastolic blood pressure (DBP) were obtained. Patients were induced with gas mixture of nitrous oxide, oxygen, and halothane, and an intravenous access was achieved. Atropine 0.02 mg/kg, pentazocine 0.05 mg/kg were administered i.v. Caudal block was given in lateral position under all aseptic precaution with a 25 gauge i.m needle. After confirming the position of the needle, with Whoosh test, the allocated drug was given. Administering anesthesiologist was blinded to the composition of the drug. After making the patient supine, surgery was allowed once up to level T10 blockade was established. Intra-operatively HR, SBP, DBP were noted at 1 min,5 min, 10 min, 15 min30 min, 40 five min, and 60 min.
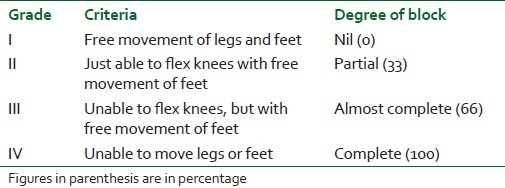
Post-operatively patients were observed in post-anesthesia care unit (PACU) for 24 hours Severity of pain was assessed with Children's Hospital Eastern Ontario Pain Scale (CHEOPS) at 0 hour, 4 hours, 8 hours, 12 hours, 16 hours, 20 hours and24 hours. Motor blockade was measured with Bromage scale [Table 1] at 0 hour, 1 hour, and 2 hours. Rescue analgesic was given with Pethidine 1 mg/kg i.m when CHEOPS score exceeded 4. Time of first rescue analgesic was recorded. Sedation or any other adverse events were also noted.
Table 1.
Bromage score
Statistical analysis
Data were collected separately from both the groups and fed in a Microsoft excel worksheet. Mean value and standard deviation were computed for age, weight, duration of surgery, duration of analgesia, HR, SBP, DBP. Then, the mean values of the 2 groups were compared by using unpaired student t test. P<0.05 was considered as statistically significant.
RESULTS
Patients in the 2 groups were comparable regarding age, weight, sex distribution, and duration of surgery [Table 2]. HR, SBP, and DBP as noted intra-operatively did not vary significantly between the 2 groups [Figures 1–3]. Motor blockade was comparable between the 2 groups [Figure 4]. Analgesia persisted for a longer duration in clonidine group (975±40.5 minutes) in comparison to plain ropivacaine group (466±0.94 minutes), which is statistically significant (P<0.0001) [Table 3]. In plain ropivacaine group, rescue was needed after average 8 hours post-operatively, and CHEOPS score diminished after receiving rescue analgesic, whereas rescue was needed after average 16 hours in ropivacaine plus clonidine group [Figure 5]. The 2 groups did not vary in respect to sedation or other adverse effect.
Table 2.
Showing demographic data and duration of surgery
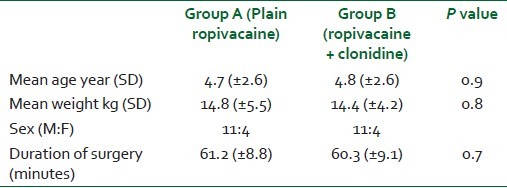
Figure 1.
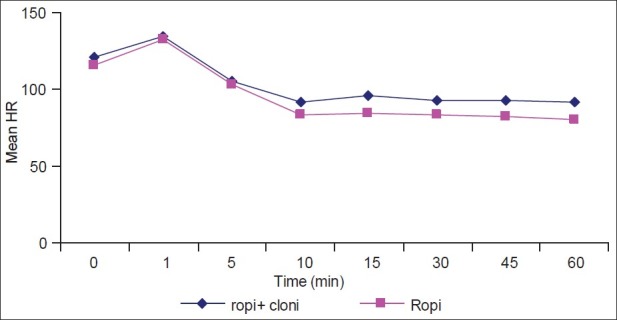
Intra-operative heart rate in two groups
Figure 3.
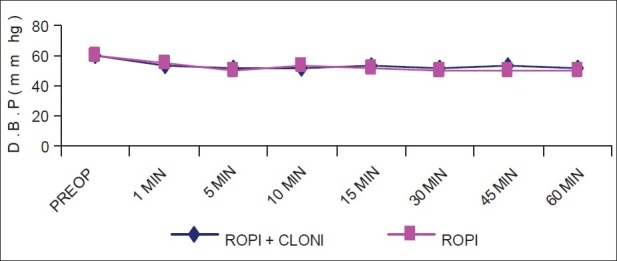
Intra-operative D.B.P in two groups
Figure 4.
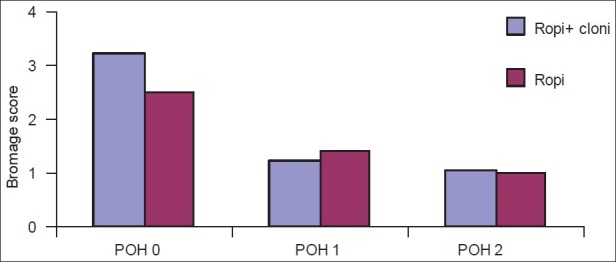
Post-operative motor blockade in two groups
Table 3.
Showing duration of analgesia
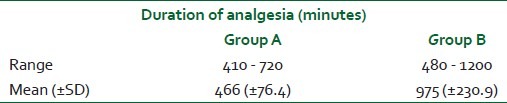
Figure 5.
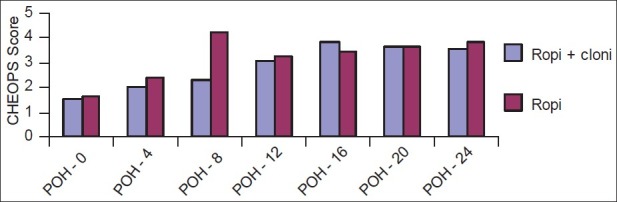
Post-operative pain score (CHEOPS) in two groups. CHEOPS: Children's hospital eastern ontario pain scale
Figure 2.
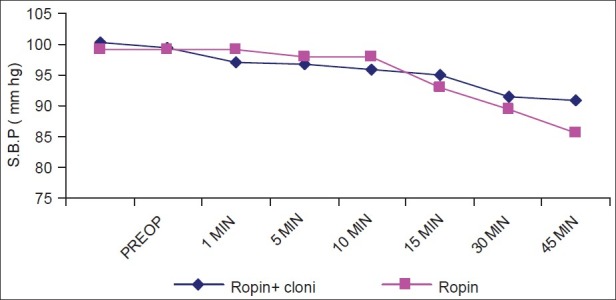
Intra-operative S.B.P in two groups
DISCUSSION
Caudal epidural block has been a popular technique to provide intra- and post-operative analgesia in children as it is easy to perform and safe. Ropivacaine is being increasingly used even in pediatric age group in caudal route because of its less motor blockade and systemic toxicity.[7,8] The limitation of the single shot caudal blockade is its finite and short duration, which reduces its utility as post-operative analgesic. To overcome this shortcoming, a trial was done with double caudal technique, but it was not found to be safe due to concern of toxicity from high volume[9] Therefore, there is a continuous search for an ideal adjuvant to prolong the duration of analgesia.
Clonidine is an alpha-2 adrenoceptor agonist, which was widely used as an anti-hypertensive in 70's and 80's, and presently it has been increasingly used for sedation, premedication, and as an adjuvant analgesic. It is also being used as an adjunct to local anesthetic in neuraxial block[10] Several pediatric studies involving caudal use of clonidine together with local anesthetics have indicated a spinal mechanism of action.[4,11–14] Co-administration of clonidine with local anesthetics has been shown to improve the quality of peripheral nerve blocks.[15–17]
Ivani G et al.[18] reported that 2 mg/kg of 0.2% ropivacaine is sufficient to obtain sensory block for lower abdominal or for genital surgery in children. Pharmacokinetic studies of ropivacaine show that 1 ml/kg 0.25% ropivacaine by caudal route produces a maximal plasma concentration of 0.72±0.24 mg/lit, which is much lower than the maximal-tolerated plasma concentration of ropivacaine in adult volunteers (2.2±0.8 mg/lit).[19,20] Therefore, we have chosen 0.2% 1 ml/kg ropivacaine.
In our study, we have seen that caudal ropivacaine alone provided excellent analgesia in the early post-operative period, but the effect wore off a few hours (466±0.94 minutes) after an operation, and supplemental analgesics were required. An addition of clonidine prolonged analgesia significantly (975±40.5 minutes).
There was no significant prolongation of motor blockade with addition of clonidine.
Regarding hemodynamics, we did not observe any significant difference in mean heart rate, SBP, DBP between the 2 groups, which corroborated to the study result obtained by Sukhminder Jit Singh Bajwah et al.[21]
No difference was found regarding post-operative sedation between 2 groups, which matched with other study.[21,22] No other adverse effect was noted in any patient of either group.
Da Conceicao and Coelho[23] reported a significantly shorter duration of motor block with 0.375% ropivacaine as compared to bupivacaine, which matched with our study (motor block <2 hours).
Bajwa SJ et al.[21] found in a study that caudal block with 0.25% of isobaric ropivacaine 0.5 ml/kg combined with 2 μg/kg of clonidine provides efficient analgesia intra-operatively and prolonged duration of analgesia post-operatively.
Koul A et al.[24] found significant prolongation of post-operative analgesia with an addition of clonidine with bupivacaine caudally.
Ivani G et al.[22] also showed in his study that combination of clonidine (2 μg/kg) and ropivacaine 0.1% is associated with an improved quality of post-operative analgesia compared to plain 0.2% ropivacaine.
The undesirable side effects of neuraxial clonidine are hypotension and bradycardia. Though some studies in adult patients have reported a decrease in mean arterial pressure (MAP) and heart rate (HR) within 15-30 minutes after an epidural injection, which lasted for 3 - 4 hrs before returning to baseline, others did not show any such hemodynamic alteration.[6,25,26]
The major limitation of our study being a single center study was that it was not feasible to validate our conclusion as the sample size was small (n = 15). Future study on larger number of patients could strongly prove the hypothesis.
CONCLUSION
In conclusion, this study suggests that addition of clonidine (2 μg/kg) as an adjuvant with 0.2% ropivacaine through caudal route increases the duration of post-operative analgesia without unnecessary prolongation of motor blockade or production of any other adverse effects.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Verghese ST, Hannallah RS. Postoperative pain management in children. Anesthesiol Clin North America. 2005;23:163–84. doi: 10.1016/j.atc.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Habre W, Bergesio R, Johnson C, Hackett P, Joyce D, Sims C, et al. Pharmacokinetics of ropivacaine following caudal analgesia in children. Paediatr Anaesth. 2000;10:143–7. doi: 10.1046/j.1460-9592.2000.00454.x. [DOI] [PubMed] [Google Scholar]
- 3.Malinovsky JM, Lepage JY, Cosian A, Mussini JM, Pinaudt M, Souron R. Is ketamine or its preservative responsible for neurotoxicity in rabbit? Anesthesiology. 1993;78:101–5. doi: 10.1097/00000542-199301000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Cook B, Dayle E. The use of additives to local anaesthetic solutions forcaudal epidural blockade. Paediatr Anaesth. 1996;6:353–9. doi: 10.1046/j.1460-9592.1996.d01-3.x. [DOI] [PubMed] [Google Scholar]
- 5.Bonnet F, Boico O, Rostaing S, Loriferne JF, Saada M. Clonidine induced analgesia in post operative patients; epidural versus intramuscular administration. Anesthesiology. 1990;72:423–7. doi: 10.1097/00000542-199003000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Eisenach J, Detweiter D, Hood D. Haemodynamic and analgesic action of epidurally administered clonidine. Anesthesiology. 1993;78:277–87. doi: 10.1097/00000542-199302000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Yildiz TS, Korkmaz F, Solak M, Toker K. Clonidine addition prolongs the duration of caudal analgesia. Acta Anaesthesiol Scand. 2006;50:501–4. doi: 10.1111/j.1399-6576.2005.00941.x. [DOI] [PubMed] [Google Scholar]
- 8.Tripi PA, Palmer JS, Thomas S, Elder JS. Clonidine increases duration of bupivacaine caudal analgesia for ureteroneocystostomy: A double-blind prospective trial. J Urol. 2005;174:1081–3. doi: 10.1097/01.ju.0000169138.90628.b9. [DOI] [PubMed] [Google Scholar]
- 9.Samuel M, Hampson-Evans D, Cunnington P. Prospective to a randomised double-blind controlled trial to assess efficacy of double caudal analgesia in hypospadias repair. J Pediatr Surg. 2003;37:168–74. doi: 10.1053/jpsu.2002.30247. [DOI] [PubMed] [Google Scholar]
- 10.Lonnqvist PA. Adjuncts to caudal block in children--Quo vadis? Br J Anaesth. 2005;95:431–3. doi: 10.1093/bja/aei221. [DOI] [PubMed] [Google Scholar]
- 11.Nishina K, Mikawa K, Shiga M, Obara H. Clonidine in paediatric anaesthesia. Paediatr Anaesth. 1999;9:187–202. [PubMed] [Google Scholar]
- 12.Jamali S, Monin S, Begon C, Dubousset AM, Ecoffey C. Clonidine in paediatric anaesthesia. Anesth Analg. 1994;78:663–6. doi: 10.1213/00000539-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Lee JJ, Rubin AP. Comparison of bupivacaine±clonidine mixture with plain bupivacaine for caudal analgesia in children. Br J Anaesth. 1994;72:258–62. doi: 10.1093/bja/72.3.258. [DOI] [PubMed] [Google Scholar]
- 14.Klimscha W, Chiari A, Michalek-Sauberer A, Wildling E, Lerche A, Lorber C, et al. The efficacy and safety of clonidine/bupivacaine combination in caudal blockade for pediatric hernia repair. Anesth Analg. 1998;86:54–61. doi: 10.1097/00000539-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Singelyn FJ, Gouverneur JM, Robert A. A minimum dose of clonidine added to mepivacaine prolongs the duration of anesthesia and analgesia after axillary brachial plexus block. Anesth Analg. 1996;83:1046–50. doi: 10.1097/00000539-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 16.El Saied AH, Steyn MP, Ansermino JM. Clonidine prolongs the effect of ropivacaine for axillary brachial plexus blockade. Can J Anaesth. 2000;47:962–7. doi: 10.1007/BF03024866. [DOI] [PubMed] [Google Scholar]
- 17.Ivani G, Conio A, de Negri P, Eksborg S, LoÈnnqvist PA. Spinal versus peripheral effects of adjunct clonidine: Comparison of the analgesic effect of a ropivacaine-clonidine mixture when administered as a caudal or ilioinguinal-iliohypogastric nerve blockade for inguinal surgery in children. Paediatr Anaesth. 2002;12:680–4. doi: 10.1046/j.1460-9592.2002.00935.x. [DOI] [PubMed] [Google Scholar]
- 18.Ivani G, Mereto N, Lampugnani E, Negri PD, Torre M, Mattioli G, et al. Ropivacaine in paediatric surgery: Preliminary results. Paediatr Anaesth. 1998;8:127–9. doi: 10.1046/j.1460-9592.1998.00246.x. [DOI] [PubMed] [Google Scholar]
- 19.Habre W, Bergesio R, Johnson C, Hackett P, Joyce D, Sims C. Plasma ropivacaine concentrations following caudal analgesia in children. Anesthesiology. 1998;89:A1245. doi: 10.1046/j.1460-9592.2000.00454.x. [DOI] [PubMed] [Google Scholar]
- 20.Knudsen K, Beckman Suurkula M, Blomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78:507–14. doi: 10.1093/bja/78.5.507. [DOI] [PubMed] [Google Scholar]
- 21.Bajwa SJ, Karun J, Bajwa SK, Bakshi G, Singh K, Panda A. Caudal ropivacaine-clonidine: A better post-operative analgesic approach. Indian J Anaesth. 2010;54:226–30. doi: 10.4103/0019-5049.65368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ivani G, De Negri P, Conio A, Amati M, Roero S, Giannone S, et al. Ropivacaine-clonidine combination for caudal blockade in children. Acta Anaesthesiol Scand. 2000;44:446–9. doi: 10.1034/j.1399-6576.2000.440415.x. [DOI] [PubMed] [Google Scholar]
- 23.Da Conceicao MJ, Coelho L. Caudal anaesthesia with 0.375% ropivacaine or 0.375% bupivacaine in paediatric patients. Br J Anaesth. 1998;80:507–8. doi: 10.1093/bja/80.4.507. [DOI] [PubMed] [Google Scholar]
- 24.Koul A, Pant D, Sod J. Caudal Clonidine in Day-Care Paediatric Surgery. Indian J Anaesth. 2009;53:450–4. [PMC free article] [PubMed] [Google Scholar]
- 25.Rauk RL, Eisenach JC, Jackson K, Young LD, Southern J. Epidural clonidine treatment for refractory reflex sympathetic dystrophy. Anesthesiology. 1993;79:1163–9. [PubMed] [Google Scholar]
- 26.Bernard JM, Kick O, Bonnet F. Comparison of intravenous and epidural clonidine for post operative patient controlled analgesia. Anesth Analg. 1995;81:706–12. doi: 10.1097/00000539-199510000-00009. [DOI] [PubMed] [Google Scholar]


