Abstract
Purpose:
Different adjuvants have been used to improve the quality and increase the duration of local anesthetics during various nerve block techniques. The current study was aimed to evaluate the effect of adding dexamethasone to bupivacaine on the quality and duration of transversus abdominis plane (TAP) block.
Methods:
Sixty adult patients undergoing elective open abdominal hysterectomy were randomly allocated to receive TAP block using 20 mL of bupivacaine hydrochloride 0.25% + 2 mL saline 0.9% (control group, n=30) or 20 mL of bupivacaine hydrochloride 0.25% + 2 mL dexamethasone “8 mg” (dexamethasone group, n=30). The primary outcome was postoperative pain, as evaluated by visual analog scale (VAS) for pain scoring at 1, 2, 4, 12, 24 and 48 h postoperatively, whereas the secondary outcomes were time to first analgesia (TFA), morphine consumption and the occurrence of nausea, vomiting or somnolence.
Results:
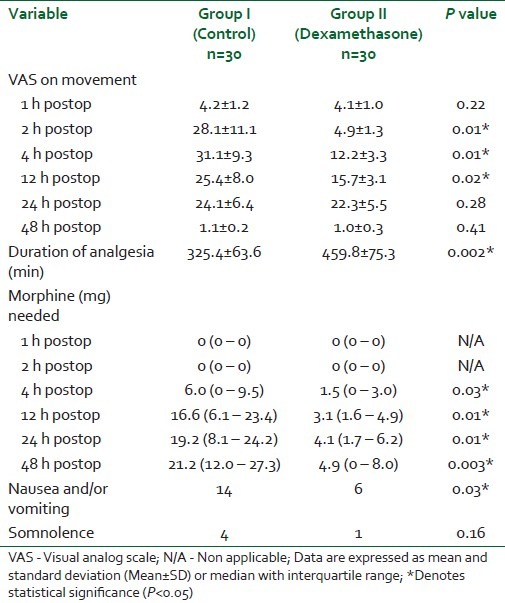
The pain VAS score was significantly lower at the postoperative 2 h (4.9 vs. 28.1, P=0.01), 4 h (12.2 vs. 31.1, P=0.01) and 12 h (15.7 vs. 25.4, P=0.02). Furthermore, TFA was significantly longer in the dexamethasone group (459.8 vs. 325.4 min, P=0.002), with lesser morphine requirements in the postoperative 48 h (4.9 vs. 21.2 mg, P=0.003) and lower incidence of nausea and vomiting (6 vs. 14, P=0.03). No complications attributed to the block were recorded.
Conclusion:
Addition of dexamethasone to bupivacaine in TAP block prolonged the duration of the block and decreased the incidence of nausea and vomiting.
Keywords: Bupivacaine, dexamethasone, transversus abdominis plane block
INTRODUCTION
A significant proportion of pain experienced by patients undergoing abdominal surgeries is related to somatic pain signals derived from the abdominal wall.[1] The anterior abdominal wall components (skin, muscles and parietal peritoneum) are supplied by sensory neurons derived from the anterior rami of spinal nerves T6 to L1, which include the intercostal nerves (T6 to T11), the subcostal nerve (T12) and the ilioinguinal and iliohypogastric nerves (L1). These neurons traverse through the neurofascial plane between the internal oblique and the transversus abdominis muscles.[2] Transversus abdominis plane (TAP) block is aimed to access these nerves in this neurofascial plane through the lumbar triangle of Petit.[3] This triangle is bounded anteriorly by the external oblique muscle and posteriorly by the latissimus dorsi muscle, whereas the base is formed by the iliac crest.[4]
Various adjuvants have been used to improve the quality and increase the duration of the local anesthetic action in different peripheral nerves and regional block techniques.[5,6] The analgesic effects of spinal and systemic corticosteroids in combination with local anesthetics have been approved in human studies.[7,8] Methyl prednisolone addition to local anesthetic has increased the duration of axillary brachial plexus block,[9] whereas dexamethasone microspheres have increased the block duration in both human and animal studies.[10–12] Furthermore, dexamethasone has been shown to possess antiinflamatory action.[13] The present placebo-controlled prospective, randomized and double-blinded study was aimed to assess the effect of adding dexamethasone to bupivacaine on the quality and duration of TAP block.
METHODS
The current prospective, randomized, double-blind, controlled clinical study was carried out after a written informed consent was obtained from all patients and institutional review board approval was obtained. Sixty ASA I or II adult patients undergoing elective open abdominal hysterectomy were included in the study. The operations were performed by the same surgical team through a transverse incision (bikini line) just above the pubic hairline. Exclusion criteria were refusal of the patients to give informed consent, preexisting coagulation disorders, morbid obesity, local infection at the site of the block or allergy to the drug under study. The patients were randomly allocated through sealed envelopes to get TAP block using 20 mL of bupivacaine hydrochloride 0.25% + 2 mL saline 0.9% (control group, n=30) or 20 mL of bupivacaine hydrochloride 0.25% + 2 mL dexamethasone “8 mg” (dexamethasone group, n=30). Randomization was done centrally by an independent statistician using a random number table generated by Microsoft Excel to ensure proper concealment of the study management from the patients and investigators until the release of the final statistical results. The injectate in both groups was prepared by an independent anesthesiologist not involved in patient care, TAP performance or data collection. The mean pH of the injectate was 5.8 in both groups. The patients were given 1–2 mg of midazolam iv as a premedication about 20 min before induction of general anesthesia. Standard monitoring included continuous electrocardiography (ECG), pulse oximetry, capnography and noninvasive blood pressure. General anesthesia was induced with propofol 1.5–2 mg/kg and fentanyl 3 μg/kg. Tracheal intubation was facilitated by administration of cis-atracurium 0.1 mg/kg. Anesthesia was maintained with isoflurane 1MAC, cis-atracurium 2 μg/kg/min and fentanyl 1 μg/kg/h, and no patients needed any additional narcotics during surgery. A single-injection ultrasound-guided TAP block was performed in all patients after induction of general anesthesia using a 38-mm broadband linear array ultrasound probe (5–10 MHz of a Hewlett-Packard 77020A ultrasound monitor [Andover, MA, USA]). With the patient in the supine position, the ultrasound probe was placed in the midaxillary line, in a transverse plane to the lateral abdominal wall between the lower costal margin and the iliac crest. The needle was then positioned in plane and directly under the ultrasound probe, and then advanced till it reached the plane between the internal oblique and transversus abdominis muscles (TAP). Upon reaching this plane, the local anesthetic solution was injected, which lead to expansion of the TAP, that appeared as a hypoechoic space. Careful aspiration was performed before injection to exclude vascular puncture. The TAP block was then performed on the opposite side, using the same technique and the same injectate. After surgery, the patients were transferred to the post anesthesia care unit. All patients were given acetaminophen 1 g iv every 6 h during first 24 h after surgery, then acetaminophen 1 g was given orally every 6 h for 4 days. Patients were given iv boluses of 1 mg morphine when needed as a patient-controlled analgesia (PCA) when visual analog scale (VAS) score at movement was more than 30 mm or on patient demand with a lock-out interval of 10 min and a maximum 4-h dose of 20 mg. Ondansetron 4 mg iv was administered in case of reported nausea and/or vomiting. Both the patients, anesthesiologists and the observers who recorded the postoperative data were blinded to the group assignment. The primary outcome was postoperative pain, as evaluated by VAS for pain scoring at 1, 2, 4, 12, 24 and 48 h postoperatively. The secondary outcomes were time to first analgesia (TFA), morphine consumption and the occurrence of nausea, vomiting or somnolence. Furthermore, any suspected adverse drug reactions were reported. The patients were instructed preoperatively about the use of the VAS for pain assessment on a 100-mm line (VAS; 0=no pain, 100=worst pain imaginable). Duration of analgesia was defined as the time interval from completion of local anesthetic administration till first need of rescue analgesic in the form of iv morphine using PCA.
Statistical analysis
Before the study, a power analysis was performed to determine the necessary number of patients in each group based on postoperative VAS score for pain. With a two-sided type I error of 5% and study power at 80%, it was estimated that 30 patients in each group would be enough to detect a 25% difference in the VAS score for pain based on detection of a 10-mm difference between the groups. The Kolmogorov-Smirnov test was used to verify normal distribution of continuous variables. Continuous variables are expressed as mean±standard deviation or median with interquartile range as appropriate. Statistical analysis was done by using Statistica version 6 (StatSoft Inc.; Tulsa, OK, USA; 2001) and GraphPad Prism version 4 (GraphPad Software Inc.; San Diego, CA, USA; 2005) software. Normally distributed continuous variables were compared using Student's unpaired “t”-test, whereas the Mann Whitney U test was used for comparison of morphine requirements. Categorical variables were compared by the Chi-square test or Fisher's exact test, as appropriate. All analyses were two-tailed and P<0.05 was considered statistically significant.
RESULTS
Both groups were comparable regarding the demographic data and operative characteristics [Table 1]. Addition of dexamethasone to bupivacaine during TAP block provided lower postoperative VAS for pain score, longer TFA (459.8±75.3 vs. 325.4±63.6 min, P=0.002), less morphine requirements (4.9 (0–8.0) vs. 21.2 (12.0–27.3) mg, P=0.003) during the postoperative 48 h and lower incidence of nausea and vomiting (6 vs. 14, P=0.03), whereas both groups were comparable regarding the incidence of somnolence (1 vs. 4, P=0.16) [Table 2].
Table 1.
Demographic data and operative characteristics in both groups
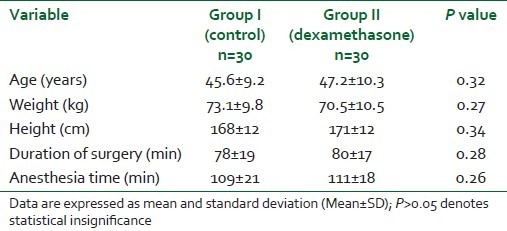
Table 2.
Characters of TAP block and postoperative pain in both groups
DISCUSSION
The current study showed that the addition of 8 mg dexamethasone to 20 mL bupivacaine 0.25% for TAP block on both sides resulted in a significant reduction of VAS pain score over the postoperative 48 h, with prolongation of TFA and reduction of postoperative morphine requirements. A variety of animal studies have reported the analgesic effect of corticosteroids by adding microspheres of corticosteroids to local anesthetics for peripheral nerve blockade.[10,12] Droger and colleagues have shown that dexamethasone incorporation into bupivacaine microspheres caused prolongation of the intercostal nerve blockade in sheep.[10] Castillo and coworkers reported that addition of dexamethasone microspheres to bupivacaine resulted in prolongation of sciatic nerve blockade in rats.[12] These studies have attributed the prolongation of the block duration to the antiinflammatory effect of steroids. However, it should be noticed that microsphere technology is designed to provide sustained and prolonged release of the drug in contrast to the aqueous solutions used in our study. Several animal studies have addressed neural safety of corticosteroid use for nerve block.[14–16] Repeated intrathecal injection of triamcinolone diacetate in a dose of 0.8 mg/kg in rats was not accompanied with any spinal neurotoxic effect.[14] In another animal study in sheep, the histopathologic effect of intrathecal injection of betamethasone was evaluated, approving its safety and suggesting its possible use in humans.[15] Sugita and coworkers[16] approved the safety and efficacy of intrathecal administration of dexamethasone more than 2000-times for approximately 200 cases with posttraumatic visual disturbance. In one study on human volunteers, addition of dexamethasone to bupivacaine microcapsules provided prolongation of the intercostal nerve blockade.[11] Use of oral dexamethasone succeeded in reducing pain and swelling following tooth extraction.[17] Another study reported analgesic and antiemetic effect of betamethason during ambulatory surgery, which was matching with our study in reducing both pain and vomiting.[18] Studies that used corticosteroids as an adjuvant with local anesthetics during peripheral or regional nerve blocks are lacking. Addition of dexamethasone to lidocaine 1.5% solution for axillary brachial plexus block resulted in longer sensory and motor blockade duration (sensory blockade duration was 242±76 vs. 98±33 min for control and motor blockade duration was 310±81 vs. 130±31 min for control).[19] In another study, 40 mg methyl prednisolone was added to a mixture of local anesthetic formed of 20 mL bupivacaine + 20 mL mepivacaine + 0.2 mL epinephrine for axillary brachial plexus block. It resulted in longer analgesia (23 vs. 16 h for control) and longer motor blockade duration (19 vs. 13 h for control).[9] Shrestha and coworkers[20] added 8 mg of dexamethasone to a mixture of lidocaine and bupivacaine for supraclavicular brachial plexus block. Dexamethasone provided a faster onset of action and longer duration of analgesia without any adverse effects. Parrington and colleagues[21] added 8 mg of dexamethasone to 30 mL mepivacaine 1.5% during supraclavicular brachial plexus blockade. The dexamethasone group showed a longer duration of analgesia: 332 (225–448 min) vs. 228 (207–263 min) min in the control group, whereas the onset times of sensory and motor blockade were similar in both groups. In another study,[22] Cummings III and coworkers reported longer analgesia when using ropivacaine or bupivacaine for interscalene blocks, with the effect being more potent with ropivacaine. However, the block duration was more prolonged with bupivacaine than with ropivacaine.
Several mechanisms have been suggested to explain the analgesic effect of corticosteroids. A direct effect on nerve membrane rather than an antiinflammatory action has been suggested as the corticosteroids were able to inhibit ectopic neural discharge originating in experimental neuromas.[23] Modulation of pain signals in the spinal cord has been suggested as intrathecal betamethasone produced rapid analgesia for pelvic and perineal cancer pain that lasted for 5 days.[24] Triggering vasoconstriction and antiallergic activity of topical steroids have been suggested through action on specific glucocorticoid receptors.[25,26] It should be emphasized that a blockade is not produced if steroids are used alone for regional blocks, but steroids may potentiate the action of local anesthetics through modulation of the function of potassium channels in the excitable cells.[27] In contradiction to our results, Tan and colleagues[28] reported failure of iv dexamethasone to potentiate the analgesic effect of intrathecal neostigmine; but, in our study, dexamethasone was not used intravenously other than for TAP block.
One limitation of the current study results from the fact that the beneficial effects of dexamethasone could be explained by its systemic absorption. Unfortunately, because a third group (perineural bupivacaine + intravenous dexamethasone) was not included in the design of the study, we were unable to answer this question.
In conclusion, the addition of dexamethasone 8 mg to bupivacaine 0.25% for TAP block provides prolongation of the duration of the block and decreases the incidence of postoperative nausea and vomiting that may have a great impact on patient comfort.
ACKNOWLEDGMENT
This study was supported by finance from Minoufiya University, Egypt. We pay great thanks to radiology department staff, Faculty of Medicine, Minoufiya University for cooperation and help in using the ultrasound machine.
Footnotes
Source of Support: Minoufiya University, Egypt
Conflict of Interest: None declared.
REFERENCES
- 1.Wall PD, Melzack R. Pain measurements in persons in pain. In: Wall PD, Melzack R, editors. Textbook of pain. 4th ed. Edinburgh, UK: Churchill Livingstone; 1999. pp. 409–26. [Google Scholar]
- 2.Tran TMN, Rozen W, Ashton M, Barrington M, Ivanusic J, Taylor G. Redefining the course of the intercostal nerves: A new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–33. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 3.Rafi A. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 4.Netter FH. Abdomen posterolateral abdominal wall. In: Netter FH, editor. Atlas of human anatomy summit. New Jersey, USA: The Ciba-Geigy Corporation; 1989. pp. 230–40. [Google Scholar]
- 5.Kapral S, Goolann G, Walt B, Likar R, Sladen RN, Weinstabl C, et al. Tramadol added to mepivacaine prolongs the duration of an axillary brachial plexus blockade. Anesth Analg. 1999;88:853–6. doi: 10.1097/00000539-199904000-00032. [DOI] [PubMed] [Google Scholar]
- 6.Pöpping DM, Elia N, Marret E, Wenk M, Tramèr MR. Clonidine as an adjuvant to local anesthetics for peripheral nerve and plexus blocks: A meta-analysis of randomized trials. Anesthesiology. 2009;111:406–15. doi: 10.1097/ALN.0b013e3181aae897. [DOI] [PubMed] [Google Scholar]
- 7.Glasser RS, Knego RS, Delashaw JB, Fessler RG. The perioperative use of corticosteroids and bupivacaine in the management of lumbar disc disease. J Neurosurg. 1993;78:383–7. doi: 10.3171/jns.1993.78.3.0383. [DOI] [PubMed] [Google Scholar]
- 8.Mirzai H, Tekin I, Alincak H. Perioperative use of corticosteroid and bupivacaine combination in lumbar disc surgery: A randomized controlled trial. Spine. 2002;27:343–6. doi: 10.1097/00007632-200202150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Stan T, Goodman E, Cardida B, Curtis RH. Adding methylprednisolone to local anesthetic increases the duration of axillary block. Reg Anesth Pain Med. 2004;29:380–1. doi: 10.1016/j.rapm.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Droger C, Benziger D, Gao F, Berde CB. Prolonged intercostals nerve blockade in sheep using controlled-release of bupivacaine and dexamethasone from polymer microspheres. Anesthesiology. 1998;89:969–74. doi: 10.1097/00000542-199810000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Kopacz DJ, Lacouture PG, Wu D, Nandy P, Swanton R, Landau C. The dose response and effects of dexamethasone on bupivacaine microcapsules for intercostals blockade (T9 to T11) in healthy volunteers. Anesth Analg. 2003;96:576–82. doi: 10.1097/00000539-200302000-00050. [DOI] [PubMed] [Google Scholar]
- 12.Castillo J, Curley J, Hotz J, Uezono M, Tigner J, Chasin M, et al. Glucocorticoids prolong rat sciatic nerve blockade in vivo from bupivacaine microspheres. Anesthesiology. 1996;85:1157–66. doi: 10.1097/00000542-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Skjelbred P, Lokken P. Postoperative pain and inflammatory reaction reduced by injection of a corticosteroid. Eur J Clin Pharmacol. 1982;21:391–6. doi: 10.1007/BF00542325. [DOI] [PubMed] [Google Scholar]
- 14.Abram SE, Marsala M, Yaksh TL. Analgesic and neurotoxic effects of intrathecal corticosteroids in rats. Anesthesiology. 1994;81:1198–205. doi: 10.1097/00000542-199411000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Latham JM, Fraser RD, Moore RJ, Blumbergs PC, Bogduk N. The pathologic effects of intrathecal betamethasone. Spine. 1997;22:1558–62. doi: 10.1097/00007632-199707150-00004. [DOI] [PubMed] [Google Scholar]
- 16.Sugita K, Kobayashi S, Yokoo A, Inoue T. Intrathecal steroid therapy for post-traumatic visual disturbance. Neurochirurgia (Stuttg) 1983;26:112–7. doi: 10.1055/s-2008-1053622. [DOI] [PubMed] [Google Scholar]
- 17.Baxendale BR, Vater M, Lavery KM. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia. 1993;48:961–4. doi: 10.1111/j.1365-2044.1993.tb07474.x. [DOI] [PubMed] [Google Scholar]
- 18.Aasboe V, Raeder JC, Groegaard B. Betamethasone reduces postoperative pain and nausea after ambulatory surgery. Anesth Analg. 1998;87:319–23. doi: 10.1097/00000539-199808000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–7. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 20.Shrestha BR, Maharjan SK, Tabedar S. Supraclavicular brachial plexus block with and without dexamethasone - A comparative study. Kathmandu Univ Med J (KUMJ) 2003;3:158–60. [PubMed] [Google Scholar]
- 21.Parrington SJ, O’Donnell D, Chan VW, Brown-Shreves D, Subramanyam R, Qu M, et al. Dexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2010;35:422–6. doi: 10.1097/AAP.0b013e3181e85eb9. [DOI] [PubMed] [Google Scholar]
- 22.Cummings KC, III, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–53. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 23.Devor MD, Gorvin-Lippmann R, Raber P. Corticosteroids suppress ectopic neural discharge originating in experimental neuromas. Pain. 1985;22:127–37. doi: 10.1016/0304-3959(85)90173-3. [DOI] [PubMed] [Google Scholar]
- 24.Taguchi H, Shingu K, Okuda H, Matsumoto H. Analgesia for pelvic and perineal cancer pain by intrathecal steroid injection. Acta Anaesthesiol Scand. 2002;46:190–3. doi: 10.1046/j.0001-5172.2001.00000.x-i1. [DOI] [PubMed] [Google Scholar]
- 25.Seidenari S, Di Nardo A, Mantovani L, Giannetti A. Parallel intraindividual evaluation of the vasoconstrictory action and the anti-allergic activity of topical corticosteroids. Exp Dermatol. 1997;6:75–80. doi: 10.1111/j.1600-0625.1997.tb00150.x. [DOI] [PubMed] [Google Scholar]
- 26.Marks R, Barlow JW, Funder JW. Steroid-induced vasoconstriction: glucocorticoid antagonist studies. J Clin Endocrinol Metab. 1982;54:1075–7. doi: 10.1210/jcem-54-5-1075. [DOI] [PubMed] [Google Scholar]
- 27.Pennington AJ, Kelly JS, Antoni FA. Selective enhancement of an A type potassium current by dexamethasone in a corticotroph cell line. J Neuroendocrinol. 1994;6:305–15. doi: 10.1111/j.1365-2826.1994.tb00587.x. [DOI] [PubMed] [Google Scholar]
- 28.Tan PH, Liu K, Peng CH, Yang LC, Lin CR, Lu CY. The effect of dexamethasone on postoperative pain and emesis after intra-thecal neostigmine. Anesth Analg. 2001;92:228–32. doi: 10.1097/00000539-200101000-00044. [DOI] [PubMed] [Google Scholar]


