Abstract
Background:
Short implants are manufactured for use in atrophic regions of the jaws. Although many studies report on short implants as ≤10 mm length with considerable success, the literature regarding survival rate of ≤7 mm is sparse.
Purpose:
The purpose of this study was to systematically evaluate the publications concerning short dental implants defined as an implant with a length of ≤7 mm placed in the maxilla or in the mandible.
Materials and Methods:
A Medline and manual search was conducted to identify studies concerning short dental implants of length ≤7 mm published between 1991 and 2011. The articles included in this study report data on implant length ≤7 mm, such as demographic variables, implant type, location in jaws, observation time, prostheses and complications.
Results:
The 28 included studies represent one randomized controlled trial, 12 prospective studies and 10 retrospective studies. The survival rate of short implant was found to be increased from 80% to 90% gradually, with recent articles showing 100%.
Conclusion:
When severe atrophy of jaws was encountered, short and wide implants can be placed successfully.
Keywords: Short dental implants, survival rate, wide implant
INTRODUCTION
Edentulous patients seeking dental treatment to restore function and aesthetic appearance have traditionally received removable complete or partial dentures. However, the use of removable dentures may lead to a sense of patient insecurity, reduced chewing capacity and taste and low self-esteem.[1] Thus, the way of treatment turned toward implants because of the high success rate of dental implants, which has changed the quality of life for many patients. The success rate seems to be correlated to the amount and the quality of bone. Longer implants have been observed to score better than shorter ones.[2,3] When a problem of severe atrophy of jaws was encountered, there have been many different approaches in solving this condition by prosthetic reconstruction. The more-aggressive protocols call for bone grafting, followed by placement of endosseous implants.[4–7] In the setting of reduced alveolar bone height, the short dental implants have recently become available and offer the clinicians a pragmatic option to facilitate prosthetic restoration in the face of anatomic limitation.[8] Through the years, various types of standard Branemark implants (3.75 mm) have been introduced for the treatment of edentulous jaws, starting with the 10-mm long implant in 1971.[9] Owing to the need for rehabilitation of such increasing number of atrophic jaws, the 7-mm standard implant was introduced in 1979. From the beginning, this implant was used either alone or with longer implants in edentulous jaws, but, eventually, it was used in the treatment of partial edentulism as well.[10,11,12,13] When considering these implants in function, the 1-, 3-, 5- and 10-year results showed a preponderance of failures among the short implants.[14–16] In addition, to facilitate the replacement of a failing standard implant and to improve the success rate in compromised situations, wide-diameter implants were introduced.[17] The wide-diameter implant was first introduced to fulfill two indications: poor bone quality and/or quantity and replacement of a failing standard implant.[18] Some authors have found that wide-diameter implants were successful when the length of the implant was compromised for situations where residual alveolar height was less. Therefore, there was a relationship for shorter and wide-diameter implants. Reconstruction of the atrophic mandible using short implants without augmentation procedures yielded, after more than 10 years of follow-up, a cumulative implant survival rate of 92.3%.[19] As it is clear that the shortcoming of short implant was found to be improved by some means and paucity of data regarding review of ≤7 mm short implant studies, they need to be investigated thoroughly for their use. Thus, the aim of this review is to present a comprehensive view of ≤7 mm short implant studies.
MATERIALS AND METHODS
Studies to be included in this structured review had to fulfil the following inclusion criteria:
Relevant data on implant lengths and diameters
Implant survival rates were either clearly indicated or calculable from data reported in the paper or as percentage basis
Criteria for implant failure clearly defined
Implant placements in various sites of jaws with immediate or delayed loading
Human-derived data were reported
Complications before and after loading
Total number of short implants with their lengths and diameters
Combination with or without long implants.
No restrictions were placed concerning study design, and randomized and non-randomized clinical trials, cohort studies, case control studies and case reports were considered for inclusion in the review. A Medline search was performed to identify clinical articles published between 1991 and 2011. The following search terms were used: “dental/oral implant” and “length,” “diameter,” “shape” and “short dental implant,” wide diameter implant, implant size <10, <8 <7 mm etc, reduced alveolar height implants, compromised implants. In addition, a manual search of the following journals from 1991 to 2011 was performed: Clinical Oral Implant Research, International Journal of Oral and Maxillofacial Implants, Clinical Implant Dentistry and Related Research, Journal of Periodontology, Journal of Clinical Periodontology, International Journal of Periodontics and Restorative Dentistry, Quientessence International. A further manual search was conducted through the bibliographies of all relevant papers and review articles. The review looks on certain key aspects of short implants that will be helpful in deciding whether to use or not when they are really indicated. Thus, the data obtained from each article was divided into six tables:
A demographic data and the type of study [Table 1]
Type of implants, total number used and their dimensions [Table 2]
Location of implants in the jaws, type and quality of bone, type of surgery and augmentation [Table 3]
Number of short implants and their dimensions [Table 4]
Type of prosthesis, loading, follow-up and survival rate [Table 5]
Time of failure, complications before/after loading and crestal bone loss [Table 6] and
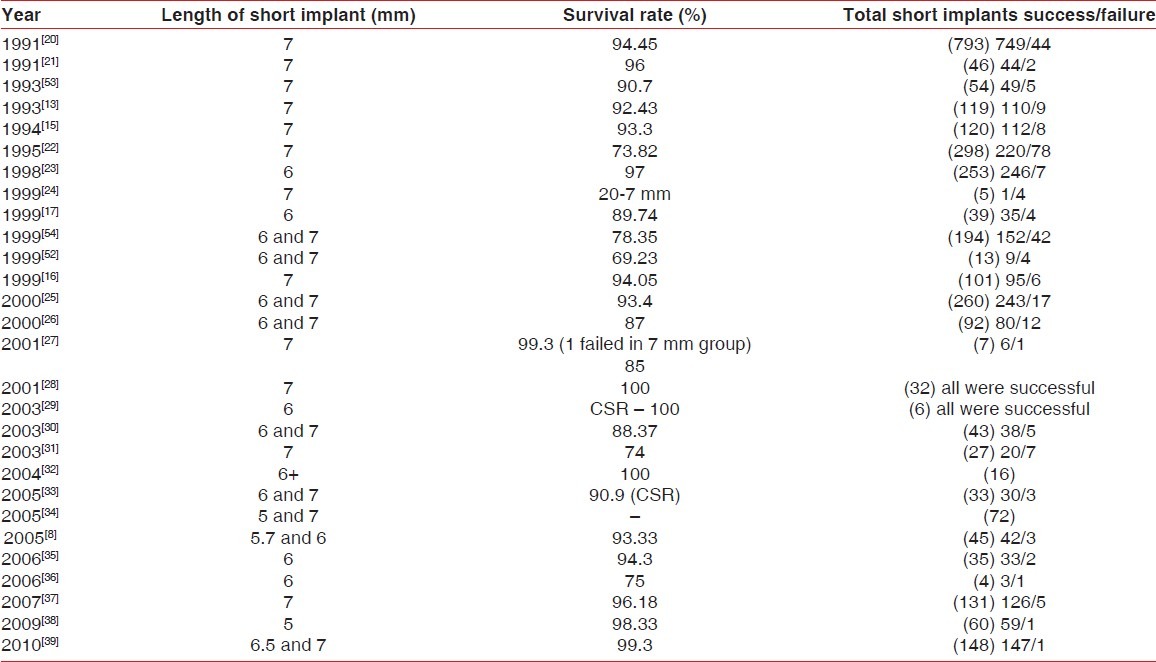
Overall success rate of short implants as per each article [Table 7].
Table 1.
Demographic data and type of study
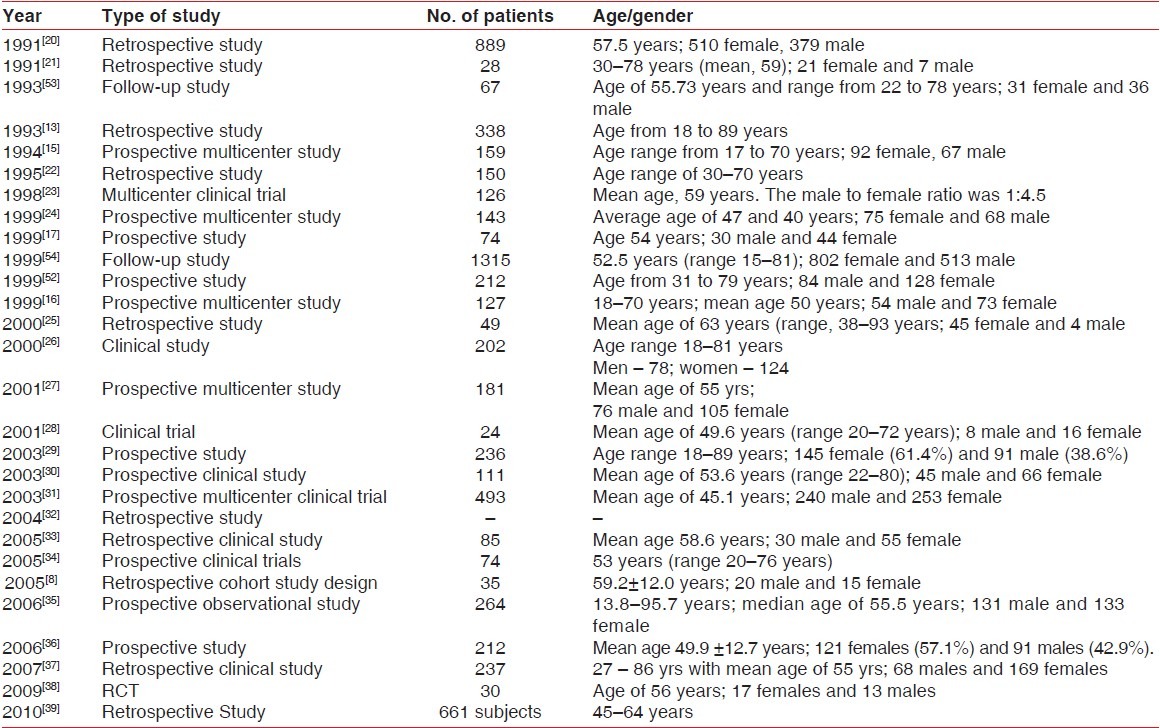
Table 2.
Type of implants, total number used and their dimensions
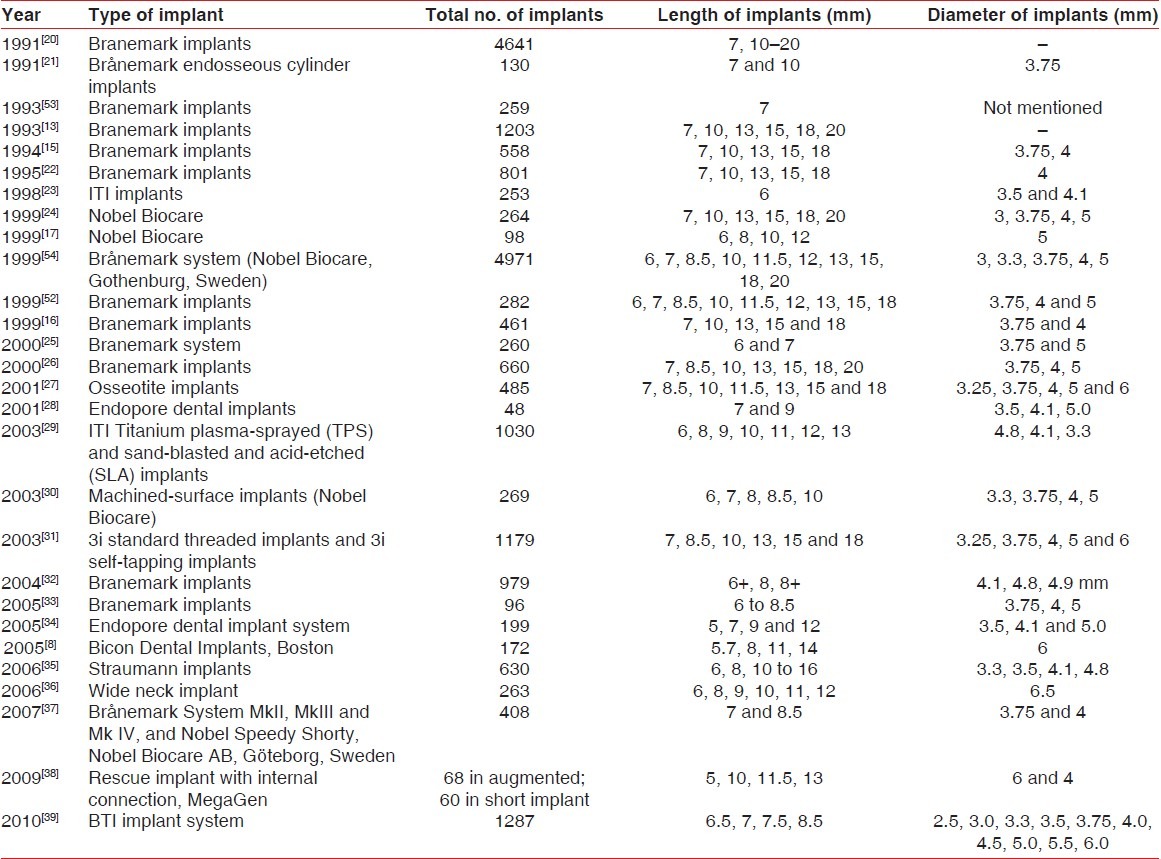
Table 3.
Location of implants in the jaws, type and quality of bone, type of surgery and augmentation
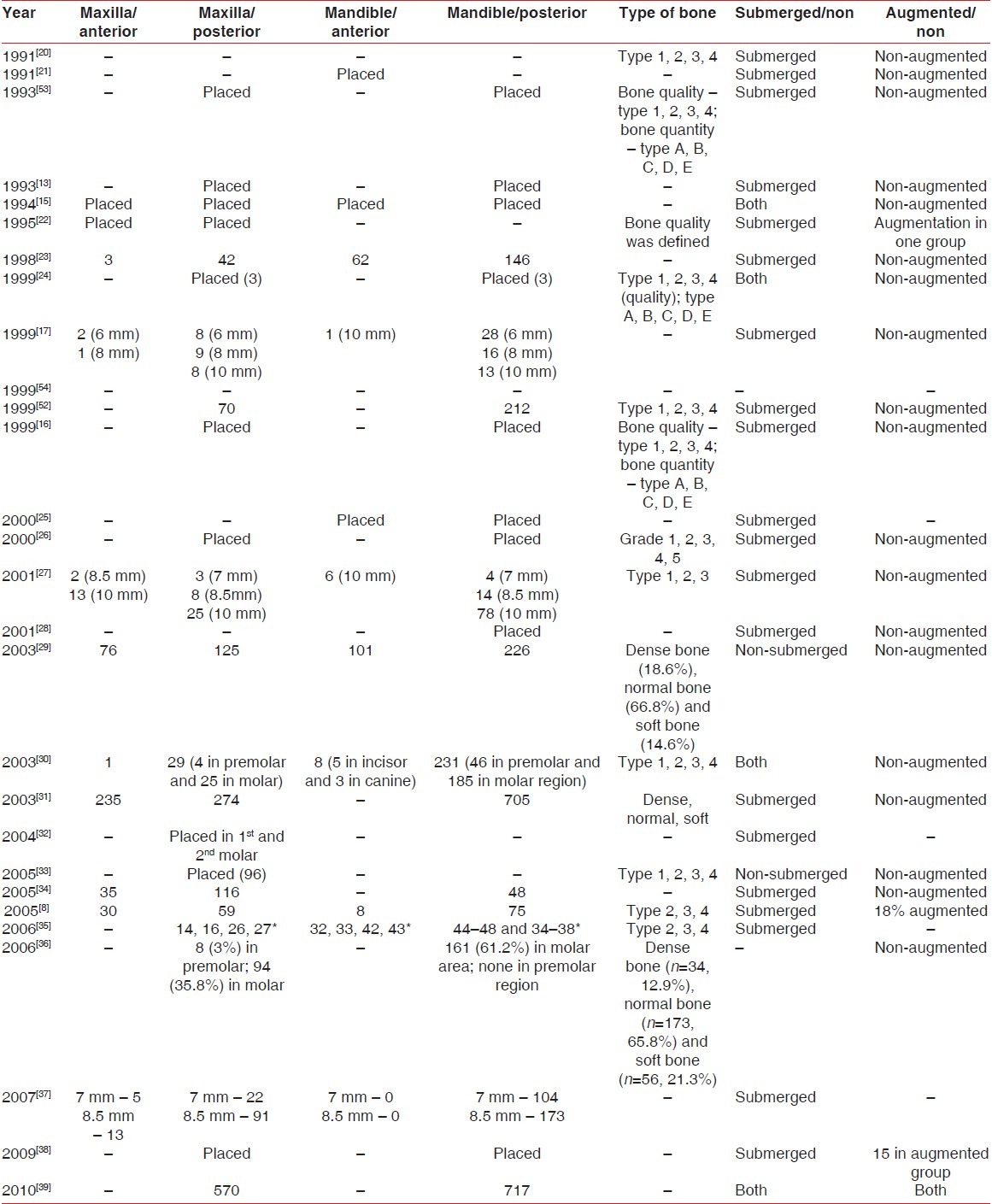
Table 4.
The number of short implants and their dimensions
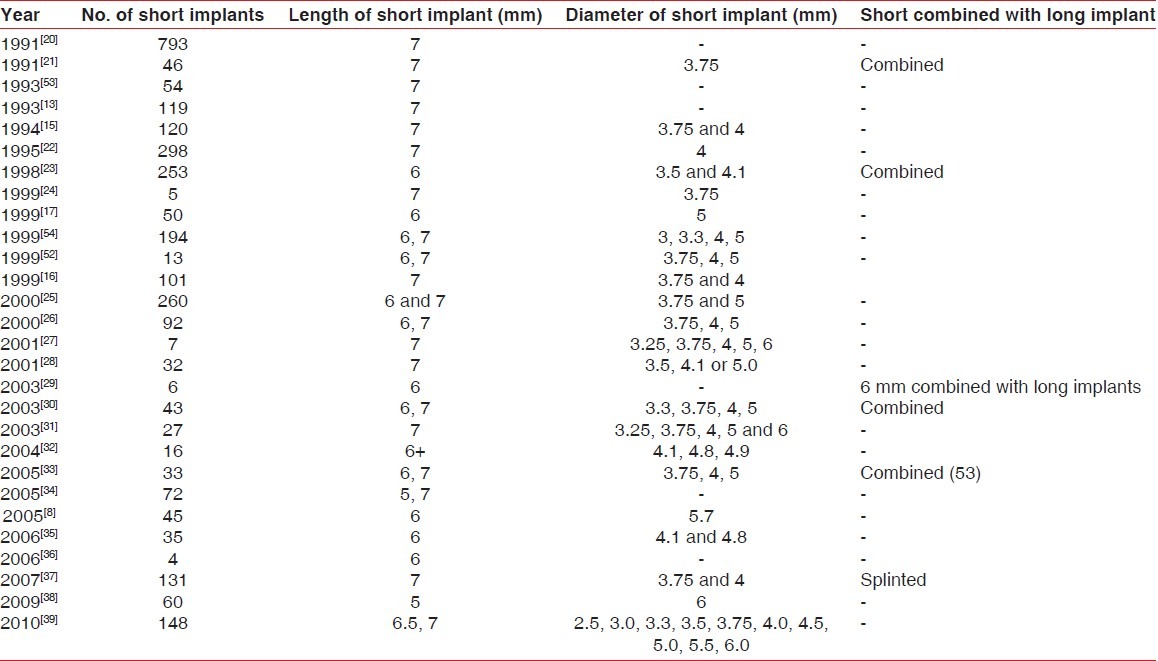
Table 5.
Type of prosthesis, loading, follow-up and survival rate
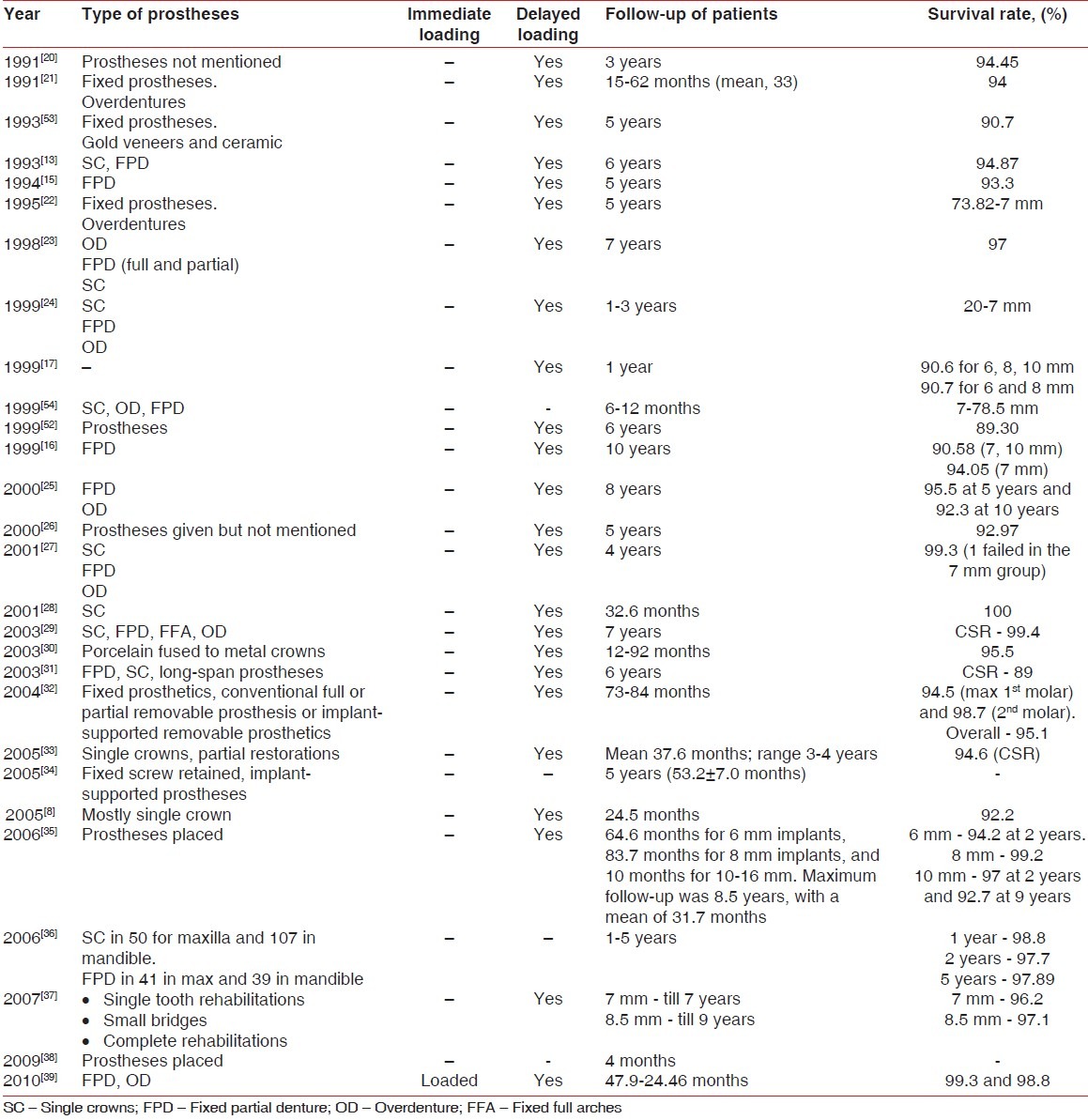
Table 6.
Time of failure, complications before/after loading and crestal bone loss
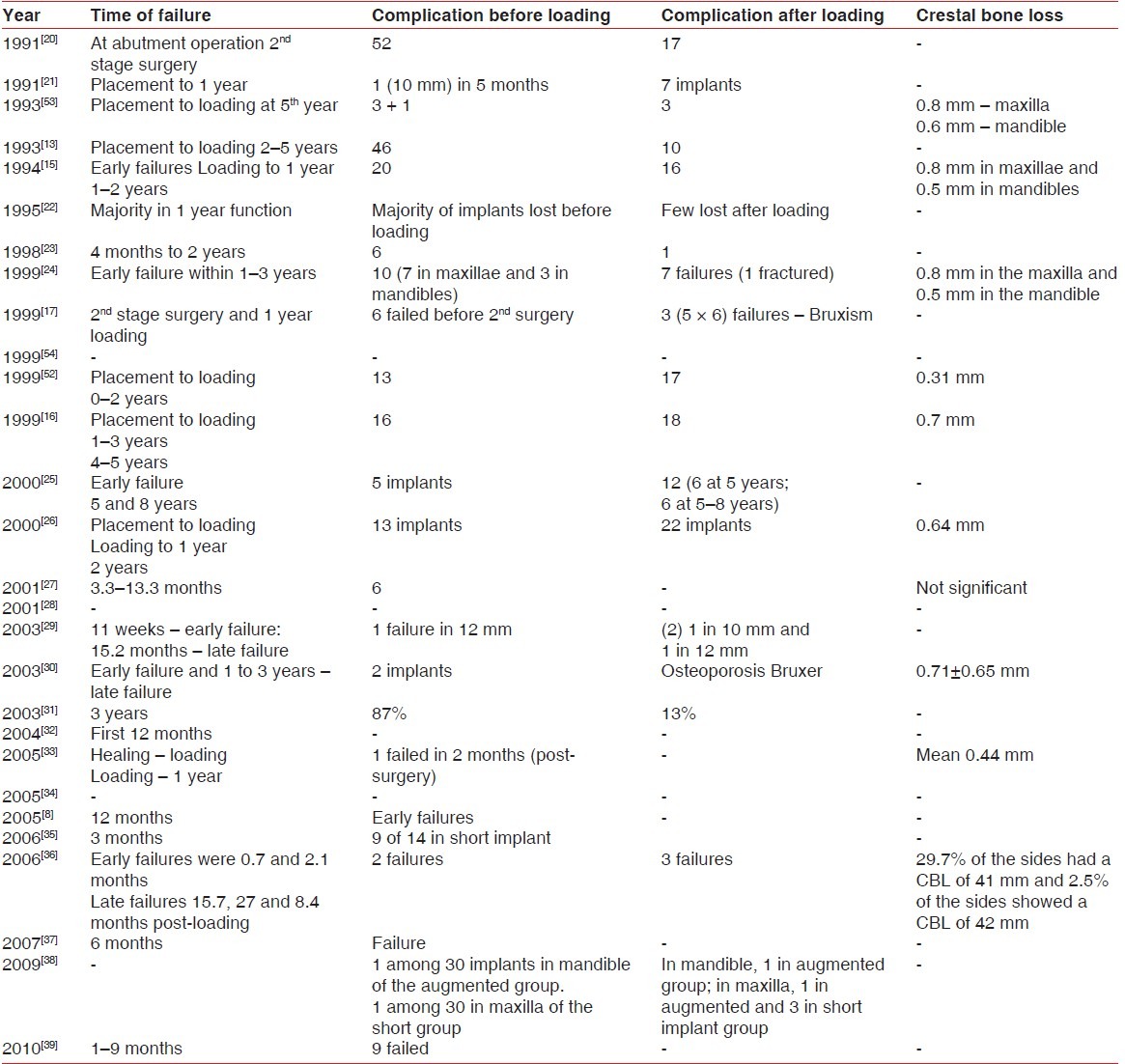
Table 7.
Overall success rate of short implants as per each article
DISCUSSION
This review presents a comprehensive view of short implants from 1991 to 2011. In the present study, data on short implants from 12 prospective, non-randomized, non-controlled trials, 10 retrospective, non-randomized, non-controlled trials, one randomized controlled trial and the rest from clinical follow-up studies are presented. The data in this review has been published in peer-reviewed scientific journals and are therefore judged reliable. A metaanalysis was not performed as data from the included reports were not standardized and, therefore, a descriptive analysis is presented. In this study, short implants were reviewed from 1991 to 2011 by dividing the data into six tables, and the description of each study is as follows. In a retrospective study, implants were placed central (closest to midline, terminal the most posteriorly inserted) and intermedial (all implants between central and terminal), and it did not include fixture failure after prostheses. The overall failure of the implants was attributed to the following reasons: placement of implant in soft bone and not achieving the primary stability at the time of placement, maxillary region, advanced resorption of maxilla and mandible and overheating of surgical site due to high bone density. The authors reported that the 7-mm implant had the highest failure rate both in the maxilla and in the mandible in completely edentulous patients, and they attributed the failure rate to the length of the implant as small bone volumes were present for fixture insertion. They also stressed the fact that majority of the 7-mm fixtures still became integrated and, subsequently, supported prosthetic restorations, whereas in partially edentulous patients, the authors reported no relationship between implant length and early failures.[20] In another retrospective study, implants were placed anterior to the mental foramen, implant-supported prostheses given for a minimum of 1 year. There was bicortical implant placement in the study. The failure of the 7-mm implant was due to distal implants, and they were rigidly connected to the fixed prostheses and were not engaged to the inferior cortical border of the bone. They attributed this to excess occlusal forces as the distal most implants carry a large load and the implants were mobile because they were not engaged to the inferior cortical border. Shortcomings of the study were retrospective design, inclusion of small sample size and limited long-term follow-up. They concluded that short implants can be used successfully in atrophic mandibles even without bone augmentation procedures.[21] A prospective multicentre study was conducted in 1985 with a total of 159 edentulous patients with 558 implants. They used the Applegate Kennedy classification to classify jaws into class 1, 2 and 4. A standard surgical procedure was followed. A clear correlation was noted with implant length failure, and most failures were represented by short implants of standard diameter whereas the implants of wider diameter seemed to achieve better results than the standard ones. Implant loss was higher in the maxilla, particularly in type 4 bone quality, and most losses occurred in the early loading periods. This study relates implant length and maxillary bone quality for their failure.[15] A retrospective study from 1985 to 1988 conducted on 150 patients, dividing them into four groups, i.e. bone-grafted group (BG), resorption group (SR), intermediate group (IM) and fixed prosthesis (FP). The FP group revealed best value and the BG group was the worst. Most failed implants were found in the SR group (28.7%), least in the FP group (7.6%), and the IM and BG group recorded 20%. Authors noted that implant failure decreased over time in all test groups except the grafted one. Therefore, the BG group must be followed longer before full knowledge can be obtained regarding the potential of that procedure. Authors concluded that even though failure rate was more for the SR group, it was acceptable because grafting would not have been a realistic treatment alternative; so, to reach the survival level of about 70% after 5 years of clinical function must therefore be regarded as acceptable.[22] A multicenter clinical trial was carried out for a 6-year period on 126 patients. The type of implant used was ITI ( International team of Implantologists )and the surface characteristic was TPS (Titanium,Plasma-Sprayed ). There were five losses out of seven implants in the maxillary molar and in the premolar sites. Implants were lost due to periimplantitis, bone loss without inflammation and infection. Authors stated that implant length of <8 mm is not acceptable. All lost implants (six out of seven) were in the maxilla. They remarked that implant design and implant-bone interface play an important role, and the plasma-sprayed implant surface might have compensated for the shorter implant length. Authors stressed that placing of short implants in extremely atrophic mandible and maxilla will create unfavorable crown root ratio, resulting in large prosthetic restorations that are heavy, aesthetically unsatisfying and uncomfortable for the patient. Therefore, they advocated augmentation of severely atrophic mandible as well as maxilla. They concluded that 6 mm implants can be used successfully with patients with minimal bone height, preferably used in combination with longer implants.[23] A prospective multicenter study was carried out in which five (7 mm) implants with 3.75 mm diameter were used and were immediately placed. A total of three implants were placed in the maxilla, and all implants were lost. Two were placed in the mandible and one was lost. Authors concluded an 80% failure rate for the 7-mm implant in this study. They attributed failures to immediate placement of short implant in extraction socket.[24] A prospective study used 6-12-mm length implants. A total of four implants were lost, one each in the maxillary and mandibular premolar and molar areas. The CSR (Cumulative Success Rate ) was found to be 91.8%. The losses were due to placement in type 4 bone, mechanical overload and periimplantitis.[17] In a prospective multicenter study, 127 patients were involved according to Kennedy's class I or II. The follow-up period was 10 years. The study presented only survival and not the success rate, as the prostheses were removed at 10 years, to assess individual implant stability. Authors stated that the tendency for higher failure rate was seen for restorations supported by four or more implants than those supported by two to three units.[16] A retrospective study conducted on 49 patients with edentulous mandible and bone resorption was shape E and quality 1 according to Lekholm and Zarb. None of the 5 mm × 6 mm implants were lost in the present study, which may be coincidental or because of their limited number. They recommended this treatment procedure without hesitation for severely resorbed mandible.[25] A clinical study involved patients with the age range of 18-81 years receiving 660 posterior maxillary implants. Quality and quantity of bone was assessed using computed tomography scans. The Lekholm and Zarb system of bone classification was modified to include additional variations of Type 4A, Type 4B, Type 4C and Type 5, and they were described as follows: Type 4A only crestal bone (inferior cortical bone), Type 4B both inferior and superior cortical bone, Type 4C superior cortical bone, Type 5 no cortical bone superiorly and inferiorly. The failure of wider implant was 5% versus 7% for the 3.75 mm implant. Authors stated that the quantity and quality of bone did not have influence on the success rate, as a lower success rate was seen in type 4 bone where quality was concerned. According to bone quantity, there was a 7% failure in grade 4 and 6% failure in grades 1, 2 and 3. The authors stated that a sufficient number of implants have to be placed to support the occlusal load. Therefore, the authors recommended the use of wide and double implants posteriorly for successful implant placement.[26] Osseotite implants were used in a prospective study for patients who were 18 years and above with a two-stage surgery and evaluated up to 5 years. Bone density was divided into normal and soft. One implant failed in the posterior maxilla during preloading due to mobility (soft bone). Authors attributed lower failure rate to the dual etched microtextures surface compared with machined implant surface.[27] Clinical investigations in a study regarding Endopore implants that were placed in patients with an age range of 22-72 years showed that the 7-mm length implants were 32 in number with no failures. Authors attributed success to the large surface area provided by the implant design, which is three- to four-times that of machined threaded implants and porous surface implant, and it allows for three-dimensional mechanical interlock with the bone for the in-growth of the bone, and this interface effectively resists interfacial shear forces and also tensile forces created by the transverse component of occlusal loading. The functional time was 32.6 months.[28] In a study, authors used ITI implants and made a special emphasis on short implants. Combination of overdentures, full-arch fixed partial denture and single crowns were given for the patients in this study. In the present study, there were no failures in short implants. Authors recommend that the use of short and roughened ITI implants is predictable for their success.[29] A total of 111 patients with an age range of 22-80 years and their edentulism classified according to the Applegate Kennedy classification were enrolled in a study. Failure rates were attributed to osteoporotic bone and dense bone overheating.[30] 1179 3i self-tapping machined implants with external hex were incorporated on 493 patients with a 5-year follow-up. There was a 26% failure for the 7 mm implants in this study. Authors attributed failures to poor quality of bone. Short implants failed at a higher rate (11%) than long implant (6.9%), and more failures were noted in the posterior maxilla.[31] Short implant used in this study was 4.1/7 mm dimensions with 84 months follow-up. A total of 16 short implants with 15 implants in the maxillary 1 st molar and one in the maxillary 2 nd molar sites were placed. All types of implants such as TPS/sandblasted/acid etched/SLS surface were used, with survival of 100%. Authors stated that short implants may be successfully employed in the replacement of missing single maxillary molars.[32] A retrospective study was carried out on resorbed maxillae for 85 patients. Ninety-six short Branemark implants (6-8.5 mm) were installed by a one-stage procedure with delayed loading (3-6 months). The bone quality ranged from type 1 to type 4. Of the 96 implants, 42 were TiUnite surface and 54 were machined surface implants. Among the 7 mm implants, a total of three implants were lost, of which one was TiUnite and two implants were machined. All were placed in the maxilla, and failed within 6 months. They reported inferior results for machined implants compared with oxidised implants, but the difference was statistically non-significant. Authors stated that use of short implants is of greater simplicity and safety compared with bone augmentation procedures and severely resorbed maxilla.[33] A prospective clinical trial was conducted on 74 patients with mean age around 53 years (range 20-76 years). All implants were placed using a two-stage surgical protocol. Endopore dental implant system was used. Long implants showed greater crestal bone loss than short ones. Likewise, splinted implants showed more crestal bone loss than non-splinted ones. Those implants with c/r ratios equal to or less than 1.0 had an average functional time of nearly 5 years, while those with c/r ratios >2.0 on average had been functioning only approximately 3 years. The c/r ratios for the implants used in these two trials were assessed and categorized, and it was found that the majority of the implants had a c/r ratio of between 1.0 and 2.0, with an average of 1.5. Authors stated that this might have been considered unfavorable for long-term implant survival, given the generally recommended c/r ratio of 0.5.[34] A study was conducted in a private practice on 264 patients with the age group of 13.8-95.7 years (median age of 55.5 years) using Straumann implants. More than half of the 6 mm implants were placed in relatively poor quality (type 4) bone. The implant types for 6 mm were solid screw standard (4.1 mm), Solid-screw esthetic SLA (4.1 mm), Solid-screw standard SLA (4.1 mm), Wide-body implants (4.8 mm) and wide body SLA and wide neck SLA. In this study, splinting was applied to implants placed in adjacent sites, irrespective of implant lengths. Among 35 of the 6 mm implants, two failed, and implant losses were observed in sites with type 4 bone.[35] A prospective 5-year life table analysis was carried out on wide neck (WN) ITI implants placed in a private practice for 212 patients, with 263 implants of 4.8 mm diameter placed in the posterior regions. The quality of bone analyzed in this study was dense bone, normal bone and soft bone. The total numbers of short implants used in this study were four, with length of 6 mm and diameter of 4.8 mm. The failure of implant was due to placement in soft bone, and the reason was that he was bruxer and smoker. Unfortunately, no conclusion could be drawn on the reliability of the 6 mm implant in this indication because of the limited number of implants (only four implants). When short implants were placed in soft bone, i.e. with two combined risks, the survival rate was still 95.8%.[36] A retrospective clinical trial was conducted with 272 implants that had machined surfaces, while 136 implants had oxidized surfaces (TiUniteTM, Nobel Biocare AB). There was a total of 5 years follow-up. Of the five failed implants, two were located in the maxillary anterior and one in the maxillary posterior region, and two were placed in the mandibular posterior region. All implant losses occurred during the first 6 months of healing, before prosthetic loading, and all had machined surfaces. In most cases, the bone was rather soft, being in the maxilla. Authors stated that the cumulative survival rate of 96% for 7-mm implants after 5 years indicates that short implants used in both jaws may be a viable concept with comparable survival rates to longer implant.[37] A randomized controlled trial combined 5 mm long, 6 mm wide implant with 10 mm length implant, with a partial fixed prosthesis on them, and was carried out on non-smokers, light smokers and heavy smokers. The follow-up was 5 years with two-stage surgery in a total of 30 patients. Patients were divided into two groups, namely: short implant group and augmented group. One implant was failed due to less torque placement (<25 Ncm). Authors stated that the large implant diameter might have played an important role in the success, although this is just a hypothesis and not a fact, which therefore needs to be investigated with proper clinical trials.[38] A retrospective study stated that the initial evidence suggesting high predictability of short implants has been reinforced by the different biomechanical studies addressing that maximum bone stress is practically independent of implant length and that implant width is more important than the additional length. A total of 1287 implants was placed in 661 consecutive patients: inclusion criteria was bone densitometry >400 and primary stability ranged between 45 and 60 Ncm. Short implants placed were 382. Only one implant of 7 mm was lost, which was placed in the mandible in a one-stage protocol connected with long implant placed with high torque (60 Ncm) pushed out by the tongue.[39]
The vertical bone augmentation procedure has the potential to increase the number, length and diameter of the implants, and it is quite predictable for immediate loading, enabling a stable long-term prognosis to the implant-supported reconstruction, whereas the demerits are type of graft material to be used as autogenous being gold standard, which will not be always the choice with donor site morbidity and graft resorption, and requires higher cost to the patient.[40]
The placement of short implants is no less efficacious than placement of implants of 10 mm or longer[41] ; however, according to a retrospective study, immediate loading of threaded implants of 10 mm or shorter with a rough surface should be performed with caution.[42] But, investigations of immediate loading of implants of length (≤7 mm) as per this review are not found. It seemed prudent to follow a two-stage implant placement approach when using short implants, as this approach has been linked with higher success rates. However, according to a review,[43] there is no significant difference in failure rates between single-stage and two-stage implants. In a metaanalysis study,[44] the single-stage approach might be preferable in partially edentulous patients, as it avoided one surgical intervention and shortened treatment times, while a two-stage submerged approach could be indicated when an implant had not obtained optimal primary stability, especially in fully edentulous patients. A surgical protocol may not play a key role in the prognosis of short implants.
Early loading refers to final crowns within 3 (within 1 to a couple of weeks) weeks from surgery in occlusion.[45] In delayed loading, endosseous dental implants remain covered and free from loading for a period of 3 months in the mandible and 6 months in the maxilla to allow implant-bone integration.[46] A study has demonstrated the possibility of early loading of SLActive implants inserted with simultaneous osteotome sinus floor elevation without the use of grafting material. SLActive implants allow early loading protocols of 3-4 weeks, as it maintains its chemical purity and high surface activity and increasing early cellular activity and bone apposition.[47] But, the study used 10 mm as implant length, and there are no studies for early loading of 7 mm short implants. All the articles stated in this review are delayed loading, contributing the maximum survival rate undoubtedly.
The crown/root ratio, especially when using short implants, has been considered as one of the prosthetic factors that may increase the risk of biomechanical complication because of overloading/non-axial loading, ultimately resulting in crestal bone loss. Authors[34,48] demonstrated that C/I ratio for short implants was not a complicating factor, such as affecting crestal bone levels.
A study reports on the success of using four 5.0×5.0 mm Bicon implants in a 56-year-old patient with partial edentulism. The success of this case study suggests a potential for decreasing the frequency of complications, such as inferior alveolar canal perforation, and of being able to provide dental implants to individuals who have inadequate alveolar bone levels for conventionally longer implants.[49] A retrospective study evaluated various implant surface factors associated with Bicon implant survival for single-tooth restoration in the healthy individual. Among the many factors that may influence the failure rate of TPS and HA-coated Bicon implants, installation depth played an especially significant role in the success of HA-coated Bicon implants, and implant length was an important prognostic factor for the TPS-treated implants.[50] A retrospective study was designed to estimate the 1- and 5-year survival of Bicon® dental implants and to identify risk factors associated with implant failure in an objective, statistically valid manner. The overall 1- and 5-year survival of the Bicon® implant system was 95.2% and 90.2%, respectively. The results of these analyses suggest that the overall survival of the Bicon dental implant is comparable with other current implant systems.[51]
Twenty-eight short implant articles are presented in this study. A total of 3046 short implants were placed, four articles documented the placement in the maxillary region, three articles documented in the mandibular region and 21 articles documented both. Regarding augmentation procedures, 20 dealt with non-augmentation, three reported on augmentation procedures and the rest did not specify anything. Branemark implants were used by 17 studies, two articles on Straumann implants, two on ITI implant systems, one on Bicon implants and one on Endopore implants. Of the 28 articles, 17 articles dealt with 7 mm length, 11 considered on 6 mm either alone or in combination with longer implants and two articles documented 5 mm length implants. The observation period of the articles ranged from a minimum of 4 months to a maximum of 7 years. Nine articles have taken the Lekholm and Zarb classification of bone qualities.[15,16,21–23,25,27,36,52] The survival rates for short implant are as follows: from 1991 to 1995, it was 82.45-98.48%; 1996 to 2000, 80-95.5%; 2001 to 2011, it was found to be 98-100%. The causes for the failures according to authors from 1991 to 2000 were small bone volumes, distal implants with excessive occlusal forces,[21] maxilla,[15,52] short and standard diameter implant; from 2001 to 2011, the reason was soft bone, smooth machined implants and osteoporotic bone.[30] The striking aspect was implants with a sintered porous surface geometry (Endopore) that can be suitable for restoring edentulous spaces as they yielded 100% survival.[28] Implants with rougher surface implants, i.e. sand-blasted and acid-etched implants, showed favorable results compared with machined surface,[27,29] and the failure rate was higher with standard-diameter short implants compared with wide-diameter short implants.[26] Authors gave information regarding immediate placement not on immediate loading, whereas there are no articles either on immediate loading or immediate placement of short implants (≤7 mm).[29]
SUMMARY AND CONCLUSION
This structured review has identified 28 articles with data regarding implant length <7 mm, of which nine articles are dedicated to short implants, 21 articles include wide-diameter implants and other are the usual ones. Short implants could be a preferable choice as the treatment becomes faster and cheaper, and these are associated with less morbidity than vertical bone augmentation. Even when the residual bone height over the mandibular canal is 5–7 mm, these short ones achieved better results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ostman PO. Immediate ⁄ early loading of dental implants. Clinical documentation and presentation of a treatment concept. Periodontol 2000. 2008;47:90–112. doi: 10.1111/j.1600-0757.2007.00244.x. [DOI] [PubMed] [Google Scholar]
- 2.Quirynen M, Naert I, Van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Branemark system. Clin Oral Implants Res. 1992;3:104–11. doi: 10.1034/j.1600-0501.1992.030302.x. [DOI] [PubMed] [Google Scholar]
- 3.Sennerby L, Roos J. Surgical determinants of clinical success of osseointegrated oral implants: A review of the literature. Int J Prosthodont. 1998;11:408–20. [PubMed] [Google Scholar]
- 4.Schliephake H, Neukam FW, Wichmann M. Survival analysis of endosseous implants in bone grafts used for the treatment of severe alveolar ridge atrophy. J Oral Maxillofac Surg. 1997;55:1227–33. doi: 10.1016/s0278-2391(97)90173-7. [DOI] [PubMed] [Google Scholar]
- 5.Bell RB, Blakey GH, White RP, Hillebrand DG, Molina A. Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg. 2002;60:1135–41. doi: 10.1053/joms.2002.34986. [DOI] [PubMed] [Google Scholar]
- 6.Kahnberg KE, Nilsson P, Rasmusson L. LeFort I osteotomy with interpositional bone grafts and implants for rehabilitation of the severely resorbed maxilla: A 2-stage procedure. Int J Oral Maxillofac Implants. 1999;14:571–8. [PubMed] [Google Scholar]
- 7.Smedberg JI, Johansson P, Ekenback D, Wannfors D. Implants and sinus-inlay graft in a 1-stage procedure in severely atrophied maxillae: Prosthodontic aspects in a 3-year follow-up study. Int J Oral Maxillofac Implants. 2001;16:668–74. [PubMed] [Google Scholar]
- 8.Gentile MA, Chuang SK, Dodson TB. Survival estimates and risk factors for failure with 6 × 5.7 implants. Int J Oral Maxillofac implants. 2005;20:930–7. [PubMed] [Google Scholar]
- 9.Lekholm U. The Branemark implant technique. A standardized procedure under continuous development. In: Laney WR, Tolman DE, editors. Chicago: Quintessence; 1992. pp. 194–9. Tissue Integration in Oral, Orthopedic and Maxillofacial Reconstruction. [Google Scholar]
- 10.Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. A long-term follow up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5:347–59. [PubMed] [Google Scholar]
- 11.Jemt T, Lekholm U, Adell R. Osseointegrated implants in the treatment of partially edentulous patients: A preliminary study on 876 consecutively placed fixtures. Int J Oral Maxillofac Implants. 1989;4:211–7. [PubMed] [Google Scholar]
- 12.Van Steenberghe D, Lekholm U, Bolender C, Folmer T, Henry P, Herrmann I, et al. The applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: A prospective multicenter study on 558 fixtures. Int J Oral Maxillofac Implants. 1990;5:272–81. [PubMed] [Google Scholar]
- 13.Nevins M, Langer B. The successful application of osseointegrated implants to the posterior jaw: A long-term retrospective study. Int J Oral Maxillofac Implants. 1993;8:428–32. [PubMed] [Google Scholar]
- 14.Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Branemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991;6:270–6. [PubMed] [Google Scholar]
- 15.Lekholm U, Van Steenberghe D, Herrmann I. Osseointegrated implants in the treatment of partially edentulous jaws: A prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1994;9:627–35. [Google Scholar]
- 16.Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, et al. Survival of the Branemark implant in the partially edentulous jaw.A 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999;14:639–45. [PubMed] [Google Scholar]
- 17.Renouard F, Arnoux JP, Sarment DP. Five-mm-Diameter Implants without a Smooth Surface Collar: Report on 98 Consecutive Placements. Int J Oral Maxillofac Implants. 1999;14:101–7. [PubMed] [Google Scholar]
- 18.Langer B, Langer L, Hermann I, Erug M. The wide implant: A solution for special bone situations and rescue for the compromised implant. Part I. Int J Oral Maxillofac Implants. 1993;8:400–8. [PubMed] [Google Scholar]
- 19.Davies JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998;13:391–401. [PubMed] [Google Scholar]
- 20.Friberg B, Jemt T. Early failures in 4,641 consecutively placed branemark dental implants: A study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants. 1991;6:142–6. [PubMed] [Google Scholar]
- 21.Triplett RG, Mason ME, Alfonso WF, McAnear JT. Endosseous cylinder implants in severely atrophic mandibles. Int J Oral Maxillofac Implants. 1991;6:264–9. [PubMed] [Google Scholar]
- 22.Jemt T, Lekholm U. Implant treatment in edentulous maxillae: A 5-Year follow-up report on patients with different degrees of jaw resorption. Int J Oral Maxillofac Implants. 1995;10:303–11. [PubMed] [Google Scholar]
- 23.Ten Bruggenkate CM, Asikainen P. Short (6-mm) nonsubmerged dental implants: Results of a multicenter clinical trial of 1 to 7 years. Int J Oral Maxillofac Implants. 1998;13:791–8. [PubMed] [Google Scholar]
- 24.Grunder U, Polizzi G. A 3-year prospective multicenter follow-up report on the immediate and delayed-immediate placement of implants. Int J Oral Maxillofac Implants. 1999;14:210–6. [PubMed] [Google Scholar]
- 25.Friberg B, Grondahl K, Lekholm U, Branemark PI. Long-term Follow-up of Severely Atrophic Edentulous Mandibles Reconstructed with Short Branemark Implants. Clin Implant Dent Relat Res. 2000;2:184–9. doi: 10.1111/j.1708-8208.2000.tb00116.x. [DOI] [PubMed] [Google Scholar]
- 26.Bahat O. Brånemark System Implants in the Posterior Maxilla: Clinical Study of 660 Implants Followed for 5 to 12 Years. Int J Oral Maxillofac Implants. 2000;15:646–53. [PubMed] [Google Scholar]
- 27.Testori T, Wiseman L. A Prospective Multicenter Clinical Study of the Osseotite Implant: Four-Year Interim Report. Int J Oral Maxillofac Implants. 2001;16:193–200. [PubMed] [Google Scholar]
- 28.Deporter D, Pilliar RM. Managing the posterior mandible of partially edentulous patients with short, porous-surfaced dental implants: Early data from a clinical trial. Int J Oral Maxillofac Implants. 2001;16:653–8. [PubMed] [Google Scholar]
- 29.Nedii R, Bischof M. A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants. Results from a private practice. Clin Oral Implants Res. 2004;15:150–7. doi: 10.1111/j.1600-0501.2004.00978.x. [DOI] [PubMed] [Google Scholar]
- 30.Tawil G, Younan R. Clinical evaluation of short, machined-surface implants followed for 12 to 92 Months. Int J Oral Maxillofac Implants. 2003;18:894–901. [PubMed] [Google Scholar]
- 31.Weng D. A prospective multicenter clinical trial of 3i machined-surface implants: Results after 6 years of follow-up. Int J Oral Maxillofac Implants. 2003;18:417–23. [PubMed] [Google Scholar]
- 32.Fugazzotto PA. Success and failure rates of 9 mm or shorter implants in the replacement of missing maxillary molars when restored with individual crowns: Preliminary results 0 to 84 months in function.A retrospective study. J Periodontol. 2004;75:327–32. doi: 10.1902/jop.2004.75.2.327. [DOI] [PubMed] [Google Scholar]
- 33.Renouard F, Nisand D. Short implants in the severely resorbed maxilla: A 2-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S104–10. doi: 10.1111/j.1708-8208.2005.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 34.Rokni S. DDS1/Reynaldo Todescan.An assessment of crown-to-root ratios with short sintered porous-surfaced implants supporting prostheses in partially edentulous patients. Int J Oral Maxillofac Implants. 2005;20:69–76. [PubMed] [Google Scholar]
- 35.Arlin ML. Short dental implants as a treatment option: Results from an observational study in a single private practice. Int J Oral Maxillofac Implants. 2006;21:769–76. [PubMed] [Google Scholar]
- 36.Bischof M, Nedir R, Najm SA. A five-year life-table analysis on wide neck ITI implants with prosthetic evaluation and radiographic analysis: Results from a private practice. Clin Oral Implants Res. 2006;17:512–20. doi: 10.1111/j.1600-0501.2006.01271.x. [DOI] [PubMed] [Google Scholar]
- 37.Maló P, de Araújo Nobre M. Short implants placed one-stage in maxillae and mandibles: A retrospective clinical study with 1 to 9 years of follow-up. Clin Implant Dent Relat Res. 2007;9:15–21. doi: 10.1111/j.1708-8208.2006.00027.x. [DOI] [PubMed] [Google Scholar]
- 38.Felice P, Checchi V. Bone augmentation versus 5-mm dental implants in posterior atrophic jaws. Four-month post-loading results from a randomised controlled clinical trial. Eur J Oral Implantol. 2009;2:267–81. [PubMed] [Google Scholar]
- 39.Anitua E, Orive G. Short implants in maxillae and mandibles: A retrospective study with 1 to 8 years of follow-up. J Periodontol. 2010;81:819–26. doi: 10.1902/jop.2010.090637. [DOI] [PubMed] [Google Scholar]
- 40.Nissan J, Ghelfan O, Mardinger O, Calderon S, Chaushu G. Efficacy of Cancellous Block Allograft Augmentation Prior to Implant Placement in the Posterior Atrophic Mandible. Clin Implant Dent Relat Res. 2011;13:279–85. doi: 10.1111/j.1708-8208.2009.00219.x. [DOI] [PubMed] [Google Scholar]
- 41.Kotsovilis S, Fourmosis I, Karoussis IK, Bamia C. A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol. 2009;80:1700–18. doi: 10.1902/jop.2009.090107. [DOI] [PubMed] [Google Scholar]
- 42.Strietzel FP, Karmon B, Lorean A, Fischer PP. Implant-Prosthetic Rehabilitation of the Edentulous Maxilla and Mandible with Immediately Loaded Implants: Preliminary Data from a Retrospective Study, Considering Time of Implantation. Int J Oral Maxillofac Implants. 2011;26:139–47. [PubMed] [Google Scholar]
- 43.Sun HL, Huang C, Wu YR, Shi B. Failure Rates of Short (≤10 mm) Dental Implants and Factors Influencing Their Failure: A Systematic Review. Int J Oral Maxillofac Implants. 2011;26:816–25. [PubMed] [Google Scholar]
- 44.Esposito M, Grusovin MG, Chew YS, Coulthard P, Worthington HV. One-stage versus two-stage implant placement.A Cochrane systematic review of randomised controlled clinical trials. Eur J Oral Implantol. 2009;2:91–9. [PubMed] [Google Scholar]
- 45.Degidi M, Piattelli A. Immediate functional and nonfunctional loading of dental implants: A 2 to 60 month follow up study of 646 Titanium implants. J Periodontol. 2003;74:224–41. doi: 10.1902/jop.2003.74.2.225. [DOI] [PubMed] [Google Scholar]
- 46.Branemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399–410. doi: 10.1016/s0022-3913(83)80101-2. [DOI] [PubMed] [Google Scholar]
- 47.Markoviæ A, Coliæ S, Draziæ R, Gaciæ B, Todoroviæ A, Stajciæ Z. Resonance Frequency Analysis as a Reliable Criterion for Early Loading of Sandblasted/Acid-Etched Active Surface Implants Placed by the Osteotome Sinus Floor Elevation Technique. Int J Oral Maxillofac Implants. 2011;26:718–24. [PubMed] [Google Scholar]
- 48.Blanes RJ. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions.A systematic review? Clin Oral Implants Res. 2009;20(suppl):67–72. doi: 10.1111/j.1600-0501.2009.01762.x. [DOI] [PubMed] [Google Scholar]
- 49.Yi YS, Emanuel KM, Chuang SK. Short (5.0 × 5.0 mm) Implant Placements And Restoration With Integrated Abutment Crowns. Implant Dent. 2011;20:125–30. doi: 10.1097/ID.0b013e31820fb67e. [DOI] [PubMed] [Google Scholar]
- 50.Lee EH, Ryu SM, Kim JY, Cho BO, Lee YC, Park YJ, et al. Effects of Installation Depth on Survival of an Hydroxyapatite-Coated Bicon Implant for Single-Tooth Restoration. J Oral Maxillofac Surg. 2010;68:1345–52. doi: 10.1016/j.joms.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 51.Vehemente VA, Chuang SK, Daher S, Muftu A, Thomas B. Dodson (2002) Risk factors affecting dental implant survival. J Oral Implantol. 2002;28:74–81. doi: 10.1563/1548-1336(2002)028<0074:RFADIS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 52.Becker W, Becker BE. Long term evaluation of 282 implants in maxillary and mandibular molar postions: A prospective study. J periodontal. 1999;70:896–901. doi: 10.1902/jop.1999.70.8.896. [DOI] [PubMed] [Google Scholar]
- 53.Jemt T. Fixed-implant-supporting prostheses in the edentulous jaw. Clin Oral Implants Res. 1993;4:142–7. doi: 10.1034/j.1600-0501.1994.050304.x. [DOI] [PubMed] [Google Scholar]
- 54.Snauwaert K, Duyck J, van Steenberghe D. Time dependent failure rate and marginal bone loss of implant supported prostheses: A 15-year follow-up study. Clin Oral Investig. 2000;4:13–20. doi: 10.1007/s007840050107. [DOI] [PubMed] [Google Scholar]


